Abstract
Objectives
To determine the association between neighborhood domestic violence and small-for-gestational-age (SGA) birth and to examine if there is a differential impact of neighborhood domestic violence on SGA births by race in a high crime community.
Methods
This analysis includes all birth records issued in New Orleans, Louisiana from 2011–2012 geocoded by census tract (N=177 census tracts, N=8,322 women). Hierarchical modeling and ecologic spatial analysis were used to examine the area-effect of neighborhood domestic violence on SGA births, independent of individual-level predictors and accounting for the propensity to live in high domestic violence neighborhoods.
Results
Tests for spatial autocorrelation reveled area-level clustering and overlap of SGA and domestic violent rates. Pregnant women living in high domestic violence areas were more likely to give birth to an SGA infant compared to women in low-domestic violence areas (OR=1.04, 95%CI: 1.01, 1.08), net of the effects of individual-level factors and propensity scores.
Conclusion
Neighborhood-level attributes including rates of domestic violence may increase women’s risk for SGA birth, highlighting a policy-relevant and potentially amenable exposure.
Keywords: neighborhood effects, domestic violence, small for gestational age births, hierarchical modeling, spatial analysis, propensity scores
INTRODUCTION
In the United States, Black women experience disproportionately higher rates of adverse birth outcomes relative to other women. Black women are 1.5 times more likely than White women to give birth to a small-for-gestational-age (SGA) infant, twice as likely to have a pre-term birth (PTB), and three times as likely to give birth to a low birth weight (LBW) infant.1,2 Differences in individual-level characteristics (i.e., socioeconomic status, education, health behaviors, and access to medical care) do not fully explain these racial disparities in birth outcomes.3–5 Efforts to understand why risk differences persist are increasingly focused on broader, contextual factors beyond individual characteristics, with the understanding that the environment in which people live, work, and grow can influence health.6–11 Previous explorations of neighborhood-level determinants of adverse birth outcomes have predominantly focused on socioeconomic indicators such as poverty and unemployment rates, median household income, and the concentration of economic disadvantage that occurs in racially segregated areas.9,12 While area-level socioeconomic disparities have been consistently associated with adverse birth outcomes, socioeconomic conditions alone fail to capture the multiple ways in which neighborhood context influences racial disparities in women’s health,10,13 and there is a need to better understand the mechanisms through which neighborhood conditions may impact birth outcomes.7
Stress is a commonly cited pathway through which exposure to disadvantage is thought to have a deleterious effect on birth outcomes.14 Research focused on physiological stress pathways demonstrates that chronic exposure to stress may lead to excess circulating corticotrophin-releasing hormone and cortisol, which in turn, may stunt fetal growth.1,14 Additionally, chronic stress exposure can lead to dysfunction of maternal cardiometabolic processes, contributing to the pathogenesis of intrauterine growth restriction, which may lead to SGA birth.1,14,15 Given the established relationship between stress and adverse perinatal outcomes,16–18 violent crime – and fear of crime – may be an important source of neighborhood stress for women and their children and may play a role in perinatal health. Neighborhood violence has been associated with health outcomes such as higher rates of smoking, depression, and lower rates of physical activity.13,19 Previous studies on crime and reproductive health have linked high crime neighborhoods to higher rates of LBW and SGA in Chicago,20,21 and higher rates of PTB in North Carolina13. A recent systematic review concluded that exposure to neighborhood disadvantage – including crime – significantly increased women’s risk for an adverse birth outcome.7 It has been hypothesized that persistent exposure to violent crime induces stress response, which predisposes pregnant women to adverse birth outcomes. However, several studies have found that the impact of neighborhood context on birth outcomes differs by maternal race. One study found that living in neighborhoods with the highest and second highest quartiles of crime rates compared with the lowest quartile was associated with increased odds of preterm birth for Black women only.22 Two other studies found that living in less deprived or higher income neighborhoods increased the risk of preterm birth for Black women but not for White women;13,23 yet, another study found that living in areas of high concentrated disadvantage were associated with adverse birth outcomes for White women, but not for Black women.9,11 Reasons underlying the differential impact by race remain unclear but may be related to larger structural forces, including structural racism, exposure over the life-course, or even more proximal neighborhood conditions as well as differences in coping with stress.24
One form of violence that has yet to be examined at an aggregate level in relation to birth outcomes is domestic violence. Domestic violence is common in the U.S., including violence against children as well as intimate partner violence (IPV). The lifetime IPV prevalence rate reported by women is 25%, and considering more common forms of IPV, such as emotional and psychological abuse, it is believed that 1 in 3 women worldwide will be abused in her lifetime.25 Violence during pregnancy may lead to pregnancy complications or adverse birth outcomes through direct or indirect mechanisms26–28 and may be responsible for increased fetal deaths in affected pregnancies at a rate of 16.0 per 1000.27 The prevalence of IPV is disproportionately high among young Black women,29 with rates reported as high as 40%, and may be a significant source of stress among pregnant women.30
In addition to variation in the types of neighborhood violence examined, key methodological considerations in the research on neighborhood conditions and adverse birth outcomes have been limited. Selection bias is a problematic feature of many previous studies on neighborhood context and birth outcomes, and methods to minimize the effects of such bias propensity score matching has rarely been done in studies examining neighborhood influences on adverse birth outcomes.21 Selection bias occurs from social sorting mechanisms whereby individuals choose where to live. Propensity score methods are one approach to reduce such bias, making exposure groups more comparable; however, it is impossible to fully remove the effect of selection bias.31 It is important to consider that individuals do not randomly chose where to live and those living in high deprivation and crime stricken areas may be different from those who do not live in such areas. These differences may be related to birth outcomes and if not accounted for can confound the exposure-outcome association.
Previous studies have not only failed to address potential selection bias, but also spatial autocorrelation of adjacent neighborhoods (i.e. exposure clustering), which can also produce biased results.13,21 In all but one study21 on neighborhood effects and birth outcomes, neighborhoods are assumed to be independent entities, ignoring the broader spatial context in which neighborhood effects are embedded. The social environment of adjacent neighborhoods can influence outcomes, suggesting that neighborhood interdependence and proximity should be considered in statistical analysis. Failing to account for spatial autocorrelation when spatial dependency is present can lead to an overestimation in significance levels of contextual effects and incorrect inferences about the exposure-outcome relationship. Given the variability in race-stratified findings and the lack of research that has used robust empirical analysis (i.e., accounting for structural confounding and spatial dependence), further evidence building is warranted not only to determine the impact between exposure to neighborhood domestic violence and adverse birth outcomes, but also whether the impact of such exposure—as a more proximal consequence of deprived or impoverished areas—may explain racial disparities in birth outcomes.
This study examines the association and spatial distribution of neighborhood-level domestic violence rates and adverse birth outcomes among non-Hispanic (NH) Black and NH White women in New Orleans, Louisiana. The objectives of this analysis were twofold: (1) to determine the contribution of neighborhood domestic violence on SGA births, accounting for spatial autocorrelation, propensity to live in high domestic violence neighborhoods, and individual-level characteristics, and (2) to examine if there was differential impact of neighborhood domestic violence on SGA births by race. We hypothesized that after controlling for individual-level variables, women living in neighborhoods with high domestic violence rates would be more likely to experience a SGA birth compared to women living in neighborhoods with low domestic violence rates.
METHODS
Individual-level measures
Data included in this analysis came from multiple sources. Individual-level data on mothers and infants included the 2011–2012 Louisiana Vital Statistics computer-registry of birth certificate data. This data included information on birth weight (grams), gestational age (weeks), maternal education (less than high school, high school graduate, some higher education, bachelor’s degree or higher), maternal racial identification (NH Black, NH White), maternal age (continuous), health insurance status (private, Medicaid, other), women, infants, and children (WIC) program status, smoking during pregnancy, previous birth outcome events, parity, and maternal address at time of birth. The primary outcome of interest, SGA, was defined as an infant with birth weight below the 10th percentile of weight for a given gestational age. We additionally explored associations with preterm birth (<37 weeks gestation) and LBW (<2,500 g). For this study, and due to the population distribution in New Orleans (33% White, 60% Black), the sample was restricted to NH White and NH Black women (n=8,322).
Neighborhood-level measures
Neighborhood definitions were based on the 2010 Census TIGER/Line Shapefile for Louisiana census tract boundaries. Orleans parish is comprised of 177 census tracts. Of the 177 census tracts, 4 were excluded from statistical analysis due to low population estimates (i.e. < 500 individuals), leaving a total of 173 census tracts. The New Orleans Police Department provided domestic violence data based on incidents of 911 calls reporting domestic events by census tract, including aggravated assault, aggravated battery, domestic disturbance, simple assault and simple battery. The neighborhood domestic violence rate was calculated by summing the counts of domestic violence calls in each census tract and dividing the total sum by the 2012 population of that census tract for a rate per 1,000 residents. Analysis was based on a 10-unit increase in the rate of neighborhood domestic violence per 1000 population.
Geocoding
Maternal residential address and crime locations were geocoded using ArcGIS software (ESRI Inc, Redlands, CA) and then aggregated to the census tract level. Over 80% of addresses were matched with the New Orleans Parish TIGER shape file from the 2010 census. Addresses that could not be geocoded were recorded as missing. Addresses that could not be geocoded were P.O. Boxes or state highway addresses. The final analytic sample of births with women georeferenced data was 8,082.
Statistical analysis
Bivariate analysis identified racial differences in maternal characteristics, census tract variables, and SGA using chi-square analysis, two-sample t tests, and crude hierarchical logistic regression models as appropriate. Crude bivariate associations between neighborhood domestic violence and PTB and LBW were detected, however, associations were nullified for both PTB and LBW in adjusted models. We assessed the impact of neighborhood domestic violence rate on SGA births by fitting hierarchical logistic regression models, with individuals (first level, n= 8,082) nested within census tracts (second level, n=173). This method partitions the variance of components at both the individual and neighborhood level. Partitioning the variance accounts for the variance in individual-level outcomes that can be explained by differences between neighborhoods, also known as the intraclass correlation (ICC).32 The ICC was calculated using the following formula: Vneighborhood/Vneighborhood + Vindividual, where Vneighborhood =variance between neighborhood and Vindividual = variance within neighborhoods or between individuals. Since the outcome variable is binary, the ICC was calculated using Snijders formula where Vstudent = Π2/3.32,33 Because of the limitations of the ICC for non-linear outcomes, the median odds ratio (MOR) was also calculated.33
To account for potential differences between women living in neighborhoods with high and low domestic violence rates (selection bias),34 propensity for living in a high domestic violence neighborhood (those with a domestic violence rate above the 75th percentile of sample distribution) was estimated by a regression model including maternal age, education, smoking status, Medicaid enrollment, and number of previous live births.
All predictor variables were centered at their means to improve model fit and interpretability. SAS version 9.4 was used for analysis including the PROC GLIMMIX command for hierarchical models. Modeling proceeded as follows: (1) an empty model that is the function of the neighborhood-level random intercept; (2) a crude bivariate multi-level model including the individual-level outcome and the main neighborhood-level predictor; (3) a multilevel model including the individual-level outcome, the main neighborhood-level predictor, propensity score, and other individual-level measures; (4) a multi-level model including a test for interaction between neighborhood domestic violence and race to identify potential racial heterogeneity in the association between domestic violence and SGA; and (5) race-stratified multivariate models.
Spatial analyses included Moran’s I tests for global and local clustering and spatial regression. Spatial weights were applied based on a queen contiguity matrix. Local Indicators of Spatial Autocorrelation (LISA) maps were used to detect the presence of spatial clustering of tract-level SGA and domestic violence rates. LISA analysis identifies areas of high and low spatial clustering that are surrounded by neighboring areas with high or low spatial clustering (i.e. high-high cluster). To quantify the presence of spatial autocorrelation, ordinary least squares (OLS), the reference model, and a spatially lagged regression model of SGA on domestic violence were calculated and compared for model fit. The OLS and spatially lagged residuals were mapped using LISA cluster analysis as a diagnostic check for remaining spatial autocorrelation.35 Spatial analysis was conducted in ArcGIS and Geoda. Finally, to evaluate the robustness of the association between SGA birth and the neighborhood-level predictors, a sensitivity analysis was conducted by restricting the sample to term births (those occurring at >37 weeks of gestation) to assess the effect of domestic violence on infant size at birth independent of preterm delivery.36 The results of the sensitivity analysis limited to term births (7064) were consistent with the findings of the primary analysis.
RESULTS
Table 1 summarizes descriptive statistics for individual and area-level variables by race and SGA status. Overall, 14.2% of births were SGA, and the proportion of SGA births was significantly higher for NH Black mothers (16.5%) compared to NH White mothers (7.4%). Among all mothers, 3.2% smoked during pregnancy and 57.7% had a previous live birth. At time of delivery, 68.1% of mothers were on public insurance (Medicaid) and 49.0% on WIC. Relative to non-SGA births, the proportion of mothers on Medicaid and WIC was statistically significantly higher for SGA births (81.1% vs. 66.4%; 56. 7% vs. 47.5%). More than 75% of White mothers had bachelor’s-level education (or higher) compared to only 10.1% of Black mothers. At the neighborhood-level, the average rate of SGA was 142.0 per 1,000 population of pregnant women in each tract and the average domestic violence rate per tract was 33.8 per 1000 population. Neighborhood-level domestic violence was crudely associated with SGA (p<0.0001).
Table 1.
Individual and area-level maternal and birth characteristics by race and SGAa New Orleans, LA 2011–2012
| Total N=8,082 |
White N=2,290 |
Black N=5,792 |
SGA N=1,151 |
No SGA N=6,931 |
|||
|---|---|---|---|---|---|---|---|
| Individual characteristics | |||||||
| Small for gestational age (%) | 14.2 | 7.4 | 16.9 | * | -- | -- | -- |
| Low birth weight (%) | 12.0 | 6.5 | 14.1 | * | -- | -- | -- |
| Pre-term birth (%) | 12.5 | 8.4 | 14.2 | * | -- | -- | -- |
| Mother’s age- mean (SD) | 27 (5.8) | 31 (5.3) | 25 (5.7) | * | 26 (6.1) | 28 (6.1) | * |
| Race (%) | |||||||
| Black | 71.7 | -- | -- | -- | 16.9 | 83.1 | * |
| White | 28.3 | -- | -- | -- | 7.4 | 92.6 | |
| Education (yrs) (%) | |||||||
| less than high school | 20.9 | 3.0 | 28.2 | 26.8 | 20.0 | ||
| high school completed | 26.0 | 6.9 | 33.8 | 33.3 | 24.8 | * | |
| some higher education | 23.6 | 14.1 | 27.4 | 22.9 | 23.7 | ||
| bachelor degree or higher | 29.5 | 75.8 | 10.0 | 17.0 | 24.2 | ||
| WIC b (%) | 49.0 | 13.58 | 62.9 | * | 56.7 | 47.5 | * |
| Medicaid (%) | 68.1 | 22.1 | 87.5 | * | 81.1 | 66.4 | * |
| Smoking during pregnancy (%) | 3.2 | 2.55 | 3.5 | * | 5.9 | 2.7 | * |
| Previous reported adverse birth outcome event (%) | 9.5 | 10.18 | 9.35 | 9.2 | 9.6 | ||
| Previous live birth (%) | 57.7 | 44.6 | 62.9 | * | 53.4 | 58.3 | * |
| Area-level characteristics (census tracts N=173) | |||||||
| Average rate per 1,000 Population (sd) | |||||||
| Neighborhood domestic violence | 33.8 (24.1) | ||||||
| Neighborhood SGA | 142.0 (66.8) | ||||||
Note. p-value (two-sided):
p<0.05.
SGA, Small for Gestational Age.
WIC, Women, Infant, and Children federal program.
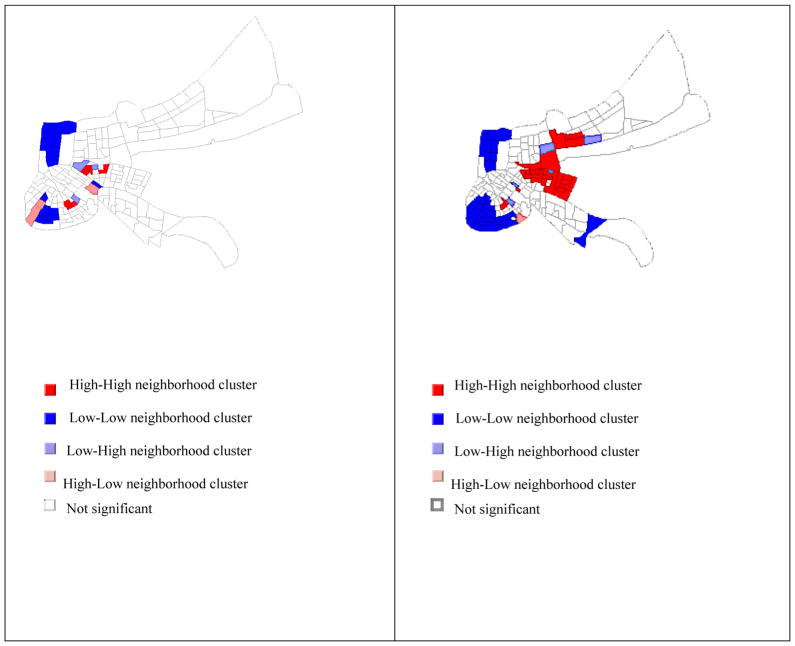
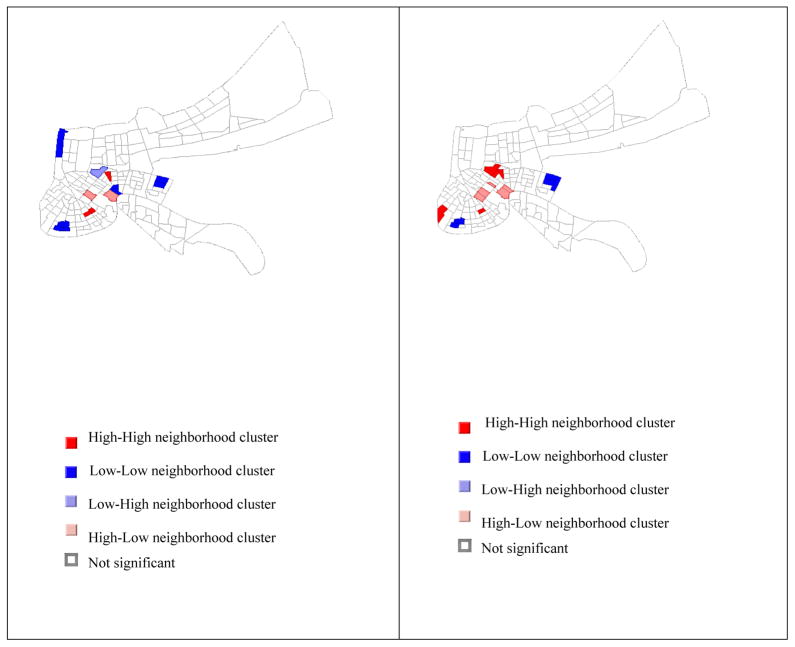
The crude Moran’s I of tract-level SGA and domestic violence rates were 0.13 and 0.48 and both p<0.05, indicating significant global clustering of overall tract-level domestic violence and SGA rates. Figures 1a–b display maps for statistically significant areas of spatial clusters of crude SGA birth and domestic violence rates. High-high clusters (red) and low-low clusters (blue) indicate the presence of positive local spatial autocorrelation. The high-low (light red) and low-high (light blue) locations are spatial outliers and indicate negative local spatial autocorrelation. Figure 1a shows that SGA birth is spatially clustered, although not as much as domestic violence. Figure 1b is dominated by large high-high and low-low clusters, indicating that neighborhoods with high levels of domestic violence are also surrounded by neighborhoods with high levels of domestic violence and neighborhoods with low levels of domestic violence are surrounded by neighborhoods with low levels of domestic violence. Figure 1c presents the amount of SGA clustering after adjusting for domestic violence rates. Adjusting for domestic violence substantially reduced the amount of residual autocorrelation in SGA rates (Moran’s I=0.04). The reduction in variance explained is evident in the LISA map, where statistically significant clusters of high SGA rates were reduced after adjusting for domestic violence. Adjusting for other individual covariates in the model further decreased the amount of spatial autocorrelation as shown in Figure 1d.
Figure 1.
a. LISA cluster map of crude SGA birth rates. b. LISA cluster map of crude domestic violence rates. c. LISA cluster map of adjusted model residuals of tract-level SGA rates, adjusted for neighborhood domestic violence. d. LISA cluster map of adjusted model residuals of tract-level SGA rates, adjusted for neighborhood domestic violence and other individual-level covariates.
Table 2 presents the results of multilevel logistic models predicting SGA with domestic violence as the main neighborhood-level predictor. In the empty model, while most of the variance in SGA was explained by factors at the individual-level, 4.0% was attributable to neighborhood differences in SGA. The residual heterogeneity between neighborhoods (MOR=1.4) also suggests that area-level differences in SGA are present. In Model 1, which included neighborhood domestic violence, a statistically significant relationship was observed, with a 11% increase in the likelihood of an SGA birth for a 10-unit increase in the neighborhood domestic violence rate (OR= 1.11; 95% CI: 1.08,1.15). Compared to the empty model, the reduction in the ICC due to the addition of neighborhood domestic violence (Model 1) indicates that 2% of the variance partitioned to the neighborhood-level and (50%) of total variance of the model were explained by the addition of domestic violence. The addition of propensity scores and other individual-level covariates (Model 2) explained an additional 57% of the variance partitioned to the neighborhood-level. The reduction in unexplained neighborhood-level variance after addition of propensity scores and individual variables to the model indicates that a large portion of the variance partitioned to the neighborhood-level is due to the composition or grouping of residents with similar individual characteristics. Nonetheless, the estimate associated with domestic violence remained statistically significant (OR=1.04, 95% CI: 1.01, 1.08).
Table 2.
Hierarchical logistic regression models of SGAa births and tract-level and individual-level predictors (N=173 tracts, N=8,082)
| Empty Model | Model 1 | Model 2b | |
|---|---|---|---|
|
| |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Individual-level variables | |||
| Age (years) | 1.01 (0.99, 1.03) | ||
| Education | 1.01 (0.91, 1.12) | ||
| Medicaid (no=ref) | 1.04(0.75, 1.45) | ||
| Total cigarettes smoked during pregnancy | 1.01 (1.00, 1.02) * | ||
| Number of previous live births | 0.84 (0.76, 0.92) * | ||
| Race (White=ref) | 1.84 (1.46, 2.32) * | ||
| Tract-level variables | |||
| Domestic violence rate | 1.11 (1.08, 1.15) * | 1.04 (1.01, 1.08) * | |
| Random effects | |||
| Variance between neighborhoods | 0.14 | 0.07 | 0.03 |
| Variance between individuals | 3.29 | 3.29 | 3.29 |
| Intraclass correlation coefficient (ICC)c | 4.0% | 2.0% | 0.54% |
| Median odds ratio (MOR)d | 1.4 | 1.3 | 1.2 |
| −2 Res Log Likelihood | 39847.0 | 39984.1 | 40125.7 |
| Akaike information criterion (AIC) | 1963.57 | 1954.65 | |
| Moran’s I | 0.13* | 0.04 | 0.02 |
| R-squared | 0.12 | 0.22 | |
Note. p-value (two-sided):
p<0.05.
SGA, Small for Gestational Age.
Models adjusted for propensity score calculated on living in a high violent crime area.
ICC, intraclass correlation coefficient calculated using the formula of Snijders and Boskers.32
Because of limitations of the ICC for non-linear outcomes, the median odds ratio (MOR) was calculated.33
A significant test for interaction in the full model suggested that the association between neighborhood domestic violence and likelihood of SGA birth might vary by race (B=−0.08, p-value=0.04), with a potentially stronger impact for Black women. To further examine racial differences of domestic violence exposure and SGA births, Model 2 was run for Blacks and Whites separately (Table 3). Among Black women, odds of SGA birth were 1.03 (95% CI: 1.00, 1.07) per 10-unit increase of neighborhood domestic violence exposure. Among White women, odds of SGA birth were 1.06 (95% CI: 0.97, 1.16) per 10-unit increase of neighborhood domestic violence exposure. The amount of SGA clustering at the neighborhood-level in the adjusted models was also substantially different by race (ICC=0.37% in Blacks versus 1.41% in Whites). Domestic violence rate explained approximately 45% of the variance at the neighborhood level among Whites and 25% of neighborhood level variance in SGA among Blacks.
Table 3.
Race-stratified hierarchical logistic regression models of SGAa births and tract-level and individual-level predictors (N=173 tracts, N=8082)
| Blacksb (N=5792) | Whitesb (N=2290) | |
|---|---|---|
|
| ||
| OR (95% CI) | OR (95% CI) | |
| Individual-level variables | ||
| Age (years) | 1.00 (0.98, 1.03) | 1.06 (1.02, 1.10) * |
| Education | 1.02 (0.90, 1.16) | 1.11 (0.91, 1.35) |
| Medicaid (no=ref) | 0.96 (0.65, 1.43) | 0.58 (0.27, 1.28) |
| Total cigarettes smoked during pregnancy | 1.01 (1.00, 1.02) * | 1.04 (1.02, 1.06) * |
| Number of previous live births | 0.87 (0.78, 0.97) * | 0.63 (0.49, 0.80) * |
| Tract-level variables | ||
| Domestic violence rate | 1.03 (1.00, 1.07) * | 1.06 (0.97, 1.16) |
| Random effects | ||
| Variance between neighborhoods | 0.01 | 0.03 |
| Variance between individuals | 3.29 | 3.29 |
| Intraclass correlation coefficient (ICC)c | 0.37% | 1.41% |
| Median odds ratio (MOR)d | 1.1 | 1.2 |
| −2 Res Log Likelihood | 27576.8 | 40125.7 |
Note. p-value (two-sided):
p<0.05.
SGA, Small for Gestational Age.
Models adjusted for propensity score calculated on living in a high violent crime area.
ICC, intraclass correlation coefficient calculated using the formula of Snijders and Boskers.32
Because of limitations of the ICC for non-linear outcomes, the median odds ratio (MOR) was calculated.33
DISCUSSION
We used hierarchical modeling and spatial analysis to examine the association and spatial dependence between neighborhood domestic violence on SGA births in an urban city characterized by high rates of crime and large racial disparities in adverse birth outcomes. Unadjusted results suggest that living in neighborhoods characterized by high domestic violence rates are associated with increased odds of SGA birth (OR=1.11; 95% CI: 1.08, 1.15), compared with living in low domestic violence neighborhoods. After adjusting for propensity scores and other individual-level covariates including race, associations were attenuated but remained statistically significant (p<0.05). Finding an effect of neighborhood domestic violence after adjusting for individual-level attributes is consistent with other neighborhood effects research 7 and the inclusion of propensity scores allowed for improved control of confounding, and in turn, better estimation of the exposure-outcome relationship.
The impact of domestic violence on SGA births only marginally differed by race. Racially stratified models revealed that among Black women, those living in areas with high domestic violence rates, irrespective of other individual-level characteristics, were 3% more likely to have an SGA birth compared to Black women living in areas with low domestic violence rates (p<0.05). White women exposed to neighborhoods with high domestic violence rates were 6% more likely to have an SGA birth compared to White women living in areas with low domestic violence rates, after controlling for other factors; yet, the findings were not statistically significant. Even though there appeared to be greater variance in SGA heterogeneity (i.e., lower ICC) among Black women, neighborhood domestic violence played a significant role and explained 25% of the variance in SGA. This finding is consistent with several other studies on adverse birth outcomes and neighborhood-level risk factors, such that neighborhood effects among Black women are greater and more variable than among White women.13 A possible explanation for the small within racial group difference could be due to unmeasured confounding among Whites, such that observable differences in high domestic violence and low domestic violence neighborhoods on SGA births were minimized7,11. Nonetheless, findings on neighborhood-level risk factors and adverse birth outcomes remain inconsistent. Other studies have found that living in areas characterized as high risk puts White women but not Black women at an increased risk of preterm birth.11,13,20 The reasons for these inconsistencies could be due to variability in the measurement of neighborhood risk and the methodologies used. Furthermore, these studies did not account for spatial autocorrelation or propensity to be exposed, which could bias the results. Of the few that have employed propensity score methods, significant differences were detected among Blacks, but not Whites.34
The mechanisms through which neighborhood domestic violence influences birth outcomes are unclear. Literature suggests that exposure and proximity to toxic and violent environments can increase stress and decrease physical activity, which in turn, may impact birth outcomes.13,19,37 It has also been suggested that chronic exposure to an abusive environment results in higher stress levels, which may lead to an increased use of nicotine, alcohol, prescription and illicit drug use, and in turn, may have an indirect effect on birth outcomes during pregnancy. Associations between maternal stress, chronic exposure to stressful life events, and poor birth outcomes have been detected. Another possible mechanism through which violence may influence birth outcomes is health behavior and mental health.13
This study contributes to the growing body of neighborhood-effects literature, with the added strength of accounting for the conditional probability of living in high domestic violence areas and consideration of spatial clustering. Results from previous studies may have been biased by not accounting for the conditional probability of high violence exposure. The substantial reduction of the ICC with the addition of propensity scores to the model demonstrates the relevance in controlling for differential probabilities for living in high violence areas. Further, the inclusion of spatial analytics provides insight into the spatial dynamics of adverse birth outcomes by showing that spatial effects on adjusted SGA birth rates (i.e., lagged residual) were reduced after adjusting for domestic violence rates.
Our findings also highlight the importance of examining area-level factors that are more proximal along the potential causal pathway than overall poverty or neighborhood disadvantage. Domestic violence is a more proximal risk factor along the causal pathway to adverse birth outcomes because it represents an immediate vulnerability to women’s health. Direct physical violence mechanisms such as abdominal trauma can lead to abruption placenta and fetal loss, maternal hemorrhage, and early onset of labor and delivery.38 Exposure to abusive environments may also lead to intermediate risks such as elevated physical and physiological stress, which in turn, may lead to diminished fetal growth and early onset of labor. While we did not have individual-level measures of domestic violence, even the neighborhood-level marker is some indication of the level of violence in the homes of residents. Such violence, even at the neighborhood-level, is still likely more proximal to adverse birth outcomes as it is likely related to more distal issues of neighborhood deprivation, power and racism that may impact feelings of hopelessness and aggression.37,39 Finally, by examining more proximal determinants, such as domestic violence, we can better identify the degree to which specific area-level attributes drive the association with poor birth outcomes, highlighting a policy-relevant and actionable exposure.
Despite the strengths of our study, there are several limitations. The choice of individual-level confounders was limited to those collected reliably on the birth record. Due to the cross-sectional nature of the data, we were not able to determine the length of time women resided in a neighborhood, and therefore, could not determine the duration of exposure. We assumed that women resided in the same neighborhood for the duration of the pregnancy. Further, although the findings indicate a clear association between objective neighborhood domestic violence rates and birth outcomes, they say little about individual perception of violence, which could differentially impact birth outcomes. Another limitation is associated with the use of 911 calls of reported domestic violence events.24 It is difficult to know the degree to which the reported event was actually a substantiated domestic violence case. A final limitation is known as the modifiable areal unit problem (MAUP),13 which arises from aggregating point-based measures of spatial phenomena to arbitrarily defined geographic areas and the use of census-based administrative units as a proxy for neighborhood. Although census tract boundaries are a relatively small unit of aggregation, they provide only a rough measure of neighborhood context, and in turn, could lead to incorrect specification of neighborhood-level exposures. Nevertheless, other studies have found using census tracts and block groups as the most useful unit of analysis for birth outcome studies.2,6,13
CONCLUSION
Our findings suggest that residing in neighborhoods with high domestic violence rates may increase the odds of having a SGA infant, irrespective of individual-level characteristics, and may be a factor in explaining Black-White disparities in SGA birth. This association highlights the role contextual factors have in shaping birth outcomes, including neighborhoods as critical spaces that influence reproductive health outcomes. Strong relationships and social bonds have been shown to reduce neighborhood crime rates and intimate partner violence through informal social control processes.40 Policies and interventions should focus on building community social cohesion, reducing social isolation, and changing social norms to promote men’s involvement in fatherhood and reproductive health. Additionally, to address the impact of neighborhood-level factors such as neighborhood domestic violence and crime on birth outcomes, more knowledge on how violent environments influence health is required. Future research should examine the multiple physiological pathways through which domestic violence and crime may operate to drive differences in birth outcomes and examine the mechanisms underlying racial heterogeneity in neighborhood-level risk.
Highlights.
Living in neighborhoods with high domestic violence rates is associated with increased odds of small for gestational age (SGA) births, net of the effects of individual-level variables and the propensity to live in high domestic violence areas.
Spatial analysis detected global clustering of tract-level small for gestational age (SGA) births and domestic violence rates.
The impact of domestic violence on small for gestational age (SGA) births only marginally differed by race, with a potentially stronger impact for Black women.
Acknowledgments
The authors would like to acknowledge the Frost Foundation, the Louisiana Department of Health and Vital Statistics, the National Institutes of Health (NIH; P60AA009803-RC5 to Dr. Theall), and the Health Resources and Services Administration (HRSA/MCHB; T03MC07649).
Footnotes
CONTRIBUTIONS
All authors were responsible for the study concept and design. E. Felker-Kantor analyzed the data and wrote the manuscript. K. Theall and M. Wallace advised on the data analysis plan and reviewed and revised the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFRENCES
- 1.Wallace M, Mendola P, Danping L, Grantz K. Joint Effects of Structural Racism and Income Inequality on Small for Gestation Age Birth. American Journal of Public Health. 2015;105(8) doi: 10.2105/AJPH.2015.302613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Culhane J, Elo I. Neighborhood context and reproductive health. American journal of obstetrics and gynecology. 2005;192:s22–29. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- 3.Ananth C, Demissie K, Kramer M, Vintzileos A. Small-for-gestational-age births among black and white women: temporal trends in the United States. Am J Public Health. 2003;93(4):577–579. doi: 10.2105/ajph.93.4.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nepomnyaschy L. Socioeconomic gradients in infant health across race and ethnicity. Matern Child health J. 2009;13(6):720–731. doi: 10.1007/s10995-009-0490-1. [DOI] [PubMed] [Google Scholar]
- 5.McDermott J, Drews C, Adams M, Hill H, Berg C, McCarthy B. Does inadequate prenatal care contribute to growth retardation among second-born African-American babies. Am J Epidemiol. 1999;150(7):706–713. doi: 10.1093/oxfordjournals.aje.a010073. [DOI] [PubMed] [Google Scholar]
- 6.Wentz A, Messer L, Nguyen T, Boone-Heinonen J. Small and large size for gestational age and neighborhhod deprivation measured within increasing proximity to homes. Health and Place. 2014;(30):98–106. doi: 10.1016/j.healthplace.2014.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Metcalfe A, Lail P, Ghali W, Sauve R. The association between neighbourhoods and adverse birth outcomes: a systematic review and meta-analysis of multi-level studies. Paediatr Perinat Epidemiol. 2011;25(3):236–245. doi: 10.1111/j.1365-3016.2011.01192.x. [DOI] [PubMed] [Google Scholar]
- 8.Kawachi I, Berkman L. Neighborhoods and Health. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 9.O’Campo P, Burke J, Culhane J, et al. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. Am J Epidemiol. 2008;167(2):155–163. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- 10.Witt W, Park H, Wisk L, et al. Neighborhood disadvantage, Preconception Stressful Life Events, and Infant Birht Weight. American Journal of Public Health. 2015;105(5) doi: 10.2105/AJPH.2015.302566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ncube CN, Enquobahrie DA, Albert SM, Herrick AL, Burke JG. Association of neighborhood context with offspring risk of preterm birth and low birthweight: A systematic review and meta-analysis of population-based studies. Soc Sci Med. 2016;153:156–164. doi: 10.1016/j.socscimed.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. American Journal of Public Health. 2001;91(11):1808–1814. doi: 10.2105/ajph.91.11.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Messer L, Kaufman J, Dole N, Herring A, Laraia B. Violent crime exposure classfication and adverse birth outcomes: a geographically-defined cohort study. International Journal of Health Geographics. 2006;5(22) doi: 10.1186/1476-072X-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uchino B. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 15.Weetman A. The immunology of pregnancy. Thyroid. 1999;9(7):643–646. doi: 10.1089/thy.1999.9.643. [DOI] [PubMed] [Google Scholar]
- 16.Wilson D, Kirtland K, Ainsworth B, Addy C. Socioeconomic status and perceptions of access and safety for physical activity. Annals of Behavioral Medicine. 2004;28:20–28. doi: 10.1207/s15324796abm2801_4. [DOI] [PubMed] [Google Scholar]
- 17.Gomez J, Johnson B, Selva M. Violent crime and outdoor physical activity among inner-city youth. Preventative Medicine. 2004;39:876–881. doi: 10.1016/j.ypmed.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 18.Chandola T. The fear of crime and area differences in health. Health and Place. 2001;2001(7):105–116. doi: 10.1016/s1353-8292(01)00002-8. [DOI] [PubMed] [Google Scholar]
- 19.Masi C, Hawkley L, Piotrowski Z, Pickett K. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Social Science & Medicine. 2007 doi: 10.1016/j.socscimed.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 20.Collins J, David R. Urban violence and African-American pregnancy outcome: an ecologic study. Ethnicity and Disease. 1997;7:184–190. [PubMed] [Google Scholar]
- 21.Morenoff J. Neighborhood mechanisms and the spatial dynamics of birthweight. American Journal of sociology. 2003;(108):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- 22.Messer L, Kaufman J, Dole N, Herring A, Laraia B. Neigborhood crime, deprivation, and preterm birth. Ann Epidemiol. 2006;16(6):455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Kaufman J, Dole N, Savitz D, Herring A. Modeling community-level effects on preterm birth. Annals of Epidemiology. 2003;13:377–384. doi: 10.1016/s1047-2797(02)00480-5. [DOI] [PubMed] [Google Scholar]
- 24.Rutter M, Nikapota A. Culture, Ethnicity, Society, and Psychopathology. In: Rutter MTE, editor. Child and Adolescent Psychiatry. Oxford, United Kingdom: Blackwell Science Inc; 2002. pp. 277–286. [Google Scholar]
- 25.Heise L, Ellsberg M, Gottemoeller M. Ending violence against women. Popul Rep. 1999;XXVVII (4)(11) [Google Scholar]
- 26.Petersen R, Gamararian J, AS, Rowley D, Goodwin M, Saltzman L. Violence and adverse pregnancy outcomes: A review of the literature and directions for future research. American Journal of Preventative Medicine. 1997;3:366–373. [PubMed] [Google Scholar]
- 27.Boy A, Salihu H. Intimate partner violence and birth outcomes: a systematic review. International journal of fertility and women’s medicine. 2004;49(4):159–164. [PubMed] [Google Scholar]
- 28.Shah PS, Jyotsna S. Maternal exposure to domestic violence and pregnancy and birthoutcomes: a systematic review and meta-analyses. Journal of Women’s Health. 2010;19(11):2017–2031. doi: 10.1089/jwh.2010.2051. [DOI] [PubMed] [Google Scholar]
- 29.Raiford J, Wingood G, Diclemente R. Prevalence, incidence, and predictors of dating violence: A longitudinal study of African American female adolescents. Journal of Women’s Health. 2007;16(6):822–832. doi: 10.1089/jwh.2006.0002. [DOI] [PubMed] [Google Scholar]
- 30.Malik S, Sorenson S, Aneshensel C. Community and dating violence among adolescents: perpetration and victimization. J Adolesc Health. 1997;21(5):291–302. doi: 10.1016/S1054-139X(97)00143-2. [DOI] [PubMed] [Google Scholar]
- 31.Oakes J. Advancing neighbourhood-effects research-selection, inferential support, and structural confounding. Int J Epidemiol. 2006;35(3):643–647. doi: 10.1093/ije/dyl054. [DOI] [PubMed] [Google Scholar]
- 32.Snijders T, Boskers R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. London: Sage; 1999. [Google Scholar]
- 33.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clsutering in multilevel logistic regression to investigate contxtual phenomena. J Epidemiology Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ma X, Fleischer N, Liu J, Hardin J, Zhao G, Liese A. Neighborhood deprivation and preterm birth: an application of propensity score matching. Ann Epidemiol. 2015;25(2):120–125. doi: 10.1016/j.annepidem.2014.11.021. [DOI] [PubMed] [Google Scholar]
- 35.Anslein L. Exploring spatial data with GeoDa: a workbook. Santa Barbara, CA: 2005. [Google Scholar]
- 36.Martin J, Hamilton B, Ventura S, Osterman M, Mathews T. Births: final data for 2011. Natl Vital Stat Rep. 2013;62(1):1–69. [PubMed] [Google Scholar]
- 37.O’Campo P, Xue S, Wang M, Caughy M. Neighborhood risk factors for low birth weight in Baltimore: a multilevel analysis. American Journal of Public Health. 1997;87:1113–1118. doi: 10.2105/ajph.87.7.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Newberger E, Barkan S, Liberman E. Abuse of Pregnant Women and Adverse Birth Outcomes. JAMA. 1992;267(17):2370–2372. [PubMed] [Google Scholar]
- 39.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39(7):887–903. doi: 10.1016/0277-9536(94)90202-x. [DOI] [PubMed] [Google Scholar]
- 40.Li Q, Kirby R, Sigler R, Hwang S, LaGory M, Goldenberg R. A Multilevel Analysis of Individual, Household, and Neighborhood Correlates of Intimate Partner Violence Among Low-Income Pregnant Women in Jefferson County, Alabama. American Journal of Public Health. 2010;100(3):531–539. doi: 10.2105/AJPH.2008.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]