Abstract
Purpose
Computed tomography (CT) use in emergency departments represents a significant contribution to pediatric patients’ exposure to ionizing radiation. Here, we evaluate whether ultralow-dose chest CT can be diagnostically adequate for other diagnoses and whether model-based iterative reconstruction (MBIR) can improve diagnostic adequacy compared to adaptive statistical iterative reconstruction (ASIR) at ultralow doses.
Methods
Twenty children underwent chest CTs; 10 standard-dose reconstructed with ASIR and 10 ultralow-dose reconstructed with ASIR and MBIR. Four radiologists assessed images for their adequacy to exclude 5 hypothetical diagnoses: foreign body, fracture, lung metastasis, pulmonary infection, and interstitial lung disease. Additionally, pairwise comparison for subjective image quality was used to compare ultralow-dose chest CT with ASIR and MBIR. Radiation dose and objective image noise measures were obtained.
Results
For exclusion of an airway foreign body, the adequacy of ultralow-dose CT was comparable to standard-dose (p=0.6). For the remaining diagnoses, ultralow-dose CT was inferior to standard-dose (p=0.03−<0.001). MBIR partially recovered the adequacy of ultralow-dose CT to exclude pulmonary infection (p=0.017), but was suboptimal for the other diagnoses. Image noise was significantly lower with MBIR compared to ASIR in ultralow-dose CT (p<0.001), although subjective preference showed only a slight advantage of MBIR (58% versus 42%).
Conclusions
Ultralow-dose chest CT may be adequate for airway assessment, but suboptimal for the evaluation parenchymal lung disease. Although MBIR improves objective and subjective image quality, it does not completely restore the diagnostic adequacy of ultralow-dose CT when compared to standard-dose CT.
Keywords: chest CT, ultralow-dose CT, pediatric CT, airway foreign body
Introduction
Radiation exposure is an important consideration in pediatric imaging as lifetime cancer risk may be increased in children undergoing examinations using ionizing radiation such as computed tomography (CT) [1, 2]. Several initiatives, including Image Gently®, have brought increased attention to this subject and, in recent years, use of pediatric CT in the US has declined. However, CT remains valuable tool in diagnosing and characterizing pediatric disease especially in the emergency setting [3–5]. In cases where CT is warranted, one of the key strategies to control radiation exposure is dose reduction. While traditionally achieved at the expense of image quality, recent technological developments have enabled dose reduction at equivalent image quality. Adaptive statistical iterative reconstruction (ASIR) is one such iterative reconstruction technique that reduces image noise and mitigates artifacts. Reduced-dose CT with ASIR has been shown to provide similar diagnostic quality to regular-dose chest CT while allowing significant dose reduction [6–8]. Model based iterative reconstruction (MBIR) is a recently FDA-approved second generation iterative reconstruction technique that takes into account three-dimensional system optics as well as data statistics thus leading to improved artifact reduction and spatial resolution compared to ASIR[9, 10]. Several studies have demonstrated similar, if not better, objective and subjective quality with MBIR over ASIR in reduced-dose adult and pediatric CT [11–15]. Some have suggested that ultralow-dose CT with MBIR may be of utility in selected clinical indications [16]. The purpose of our study was twofold. First, we evaluated the diagnostic adequacy of ultralow-dose chest CT, reconstructed with both ASIR and MBIR, and standard-dose chest CT, reconstructed with ASIR, in several clinical scenarios. Second, we used subjective and objective parameters of image quality to compare MBIR to ASIR in ultralow-dose chest CT. Our primary hypothesis was that ultralow-dose chest CT would be sufficient to exclude certain diagnoses, both common and uncommon, in pediatric chest imaging. Our secondary hypothesis was that MBIR would improve this diagnostic confidence.
Methods
Patient population
Chest CT images of twenty children seen at our institution between August 2012 and January 2014 were selected for evaluation. Of this selection, 10 were ultralow-dose chest CTs obtained as part of the work-up of pectus excavatum and 10 were standard-dose chest CTs obtained for a variety of indications. The included standard-dose chest CTs were specifically selected to be within a similar age range to that of the pectus excavatum ultralow-dose chest CTs and to demonstrate no apparent pathology. This retrospective study was compliant with Health Insurance Portability and Accountability Act guidelines and was approved by the Institutional Review Board. The requirement for informed consent was waived.
Imaging and Reconstruction Technique
All studies were performed on a 64-channel multi detector-row scanner (Discovery CT750 HD, GE Healthcare). Standard-dose CTs were reconstructed with ASIR and ultralow-dose CTs were reconstructed both with ASIR and MBIR. Detailed CT scanning parameters are shown in Table 1. The volume CT dose index (CTDIvol) in milligrays and dose-length product (DLP) in milligrays × cm were obtained from the CT scanner to quantify dose reduction. Radiation dose parameters were converted to size specific dose estimate (SSDE) using the method described by the American Association of Physicists in Medicine report 204 with anteroposterior thickness and lateral width measured on scout CT images in order to provide a more accurate representation of the effective radiation dose by the pediatric patient [18, 19].
Table 1.
Patient characteristics and CT scanning parameters
| Standard-dose | Ultralow-dose | |
|---|---|---|
| Boys/Girls | 6/4 | 10/0 |
| Mean age (years) | 13.3 (10–18) | 14.5 (12–18) |
| Mean body surface area (m2) | 1.40 (1.07–1.9) | 1.56 (1.29–1.94) |
| Detector configuration (rows × mm) | 64 × 0.625 | 64 × 0.625 |
| Tube potential (kVp) | 100 | 80 |
| Bow tie filter | Body (medium) | Body (medium) |
| Tube current (mA) | 150–200 | 20 |
| Tube current modulation | Smart mA (x-y-z modulation) | Off |
| Noise index | 13–22 | N/A |
| Gantry rotation time (s) | 0.5 | 0.5 |
| Acquisition mode | Helical | Helical |
| Helical Pitch | 1.375:1 | 1.375:1 |
| Display field of view (mm) | 300 | 300 |
| Axial image thickness (mm) | 3 | 3 |
| Breath Hold | Inspiration | Expiration |
| Reconstruction method (% blend) | ASIR (30%) | ASIR (30%) and MBIR (N/A) |
ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction.
Interpretation
Four board-certified radiologists including two fellowship-trained pediatric radiologists (10 and 3 years experience after residency) and two fellowship-trained chest radiologists (5 and 4 years experience after residency) assessed all series for subjective image quality. Evaluation was carried out on a 15-inch MacBook Pro Laptop (Apple Computer, Cupertino CA) with screen resolution of 1440 × 900. A laptop was chosen instead of a PACS workstation, because a laptop facilitated side-by-side pairwise comparisons of images from different patients and different studies. Interpretation was performed individually in a dark room that simulated radiology reading room conditions. Clinical data was removed and the scan parameters and reconstruction method were not provided to the reader.
A Microsoft PowerPoint (Microsoft, Redmond, WA) module was prepared for comparison of the standard-dose ASIR, ultralow-dose ASIR, and ultralow-dose MBIR images in five hypothetical common diagnostic scenarios: 1) airway foreign body, 2) fracture, 3) metastatic involvement of the lung, 4) pulmonary infection, and 5) interstitial lung disease. Single axial images of the chest coned in to the right lung base with lung window setting (window width, WW: 1500 HU, window length, WL: −500 HU) were used for evaluation of lung parenchyma, axial images of the whole chest at the carina with lung window setting were used for evaluation of the central airways, and axial images of the whole chest at the mid-thoracic level with bone window setting (WW: 950 HU, WL: 450 HU) were used for the evaluation of bone. Thirty images were evaluated (10 standard-dose CT, 10 ultralow-dose CT with ASIR, and 10 ultralow-dose CT with MBIR). Each image was shown to the reader five different times, each time asking the reader about their diagnostic confidence with one of the five different hypothetical diagnoses. The reader was required to ascertain, in “yes or no” format, whether the selected image was of diagnostic adequacy to confidently exclude the five hypothetical diagnoses. Pulmonary metastasis and infection were defined to the reader as a 5 mm solid or ground glass nodule, respectively. This resulted in a total of 150 images shown to the reader, in randomized order.
Another module was prepared for pairwise comparison of the ultralow-dose ASIR and MBIR images using axial slices at the level of the carina with lung window setting. Pairwise comparison was composed of 190 side-by-side comparisons of the 20 different (10 with ASIR, 10 with MBIR) axial slices with two images per slide in a manner previously described [20]. The comparisons were ordered randomly and included every unique comparison. The reader was asked to determine one of three possibilities with regards to evaluating lung parenchyma: a) image on right is better, b) image on left is better, or c) no difference between the two images. Figure 1 provides a graphical representation of subjective interpretation that was performed.
Fig. 1.
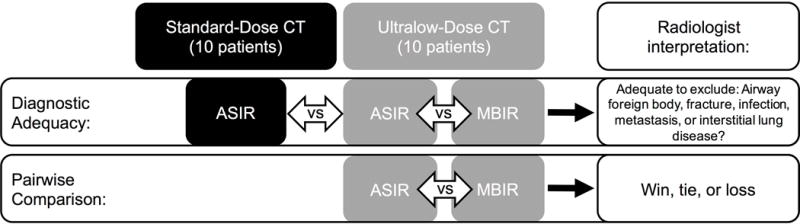
Chart shows subjective evaluation schemes used in our study. ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction
An ovoid region of interest (ROI) was drawn at four standard locations: anterior mediastinum, pectoralis musculature, axillary fat, and paraspinal musculature. ROIs of identical size were placed at the same anatomic location for the CT datasets and noise (standard deviation, SD) and mean CT number (HU) measurements were recorded.
Statistics
Student’s t-test was performed to compare children’s age and body surface area. Subjective evaluation of diagnostic adequacy was analyzed with Cochrane’s Q test and post-hoc McNemar test. Inter-reader agreement was assessed with free marginal multirater kappa. Agreement on the basis of kappa values was classified as: poor (≤0.2), fair (0.21-0.4), moderate (0.41-0.6), good (0.61-0.8), and very good (0.81-1.0). Subjective pairwise comparison between reconstruction methods of ultralow-dose CT was performed with Student’s t-test. Interobserver agreement was assessed with intraclass correlation coefficient. Objective measures of radiation dose and noise were compared with one-way analysis of variance and post-hoc Tukey test where applicable. Statistical significance was accepted at the 95% confidence level (p value < 0.05) for all measures.
Results
Patient characteristics
There was no significant difference in patient age or body surface area between the two groups (p = 0.5 and 0.13, respectively, Table 1). There was, however, a difference in gender composition: in the standard dose group, there were 6 boys and 4 girls, whereas in the ultralow-dose group there were only boys.
Subjective measurement
Evaluation for diagnostic adequacy of standard- and ultralow-dose chest CT was based on whether or not the reviewer viewed the image as adequate to exclude the diagnosis of airway foreign body, fracture, lung metastasis, pulmonary infection, or interstitial lung disease. Figure 2 shows axial chest CT images with the three scanning protocols evaluated in this study. Results are summarized and depicted in Table 2 and Figure 3, respectively. Of note, as ultralow-dose CT was performed at expiration as part of our pectus excavatum protocol, care was taken to select axial images for interpretation without or with minimal atelectasis.
Fig. 2.
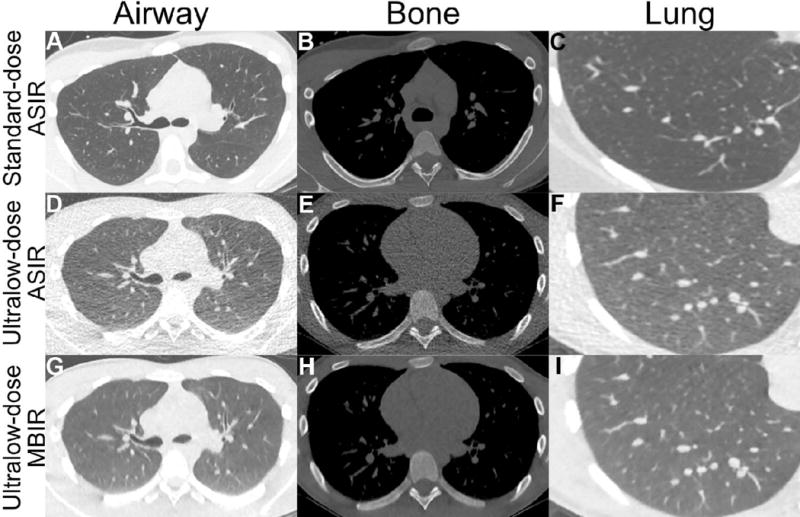
10-year-old boy who underwent a standard-dose chest CT that was reconstructed with ASIR (A–C) and a 12-year-old boy who underwent an ultralow-dose chest CT that was reconstructed with ASIR (D–F) and MBIR (G–I). Application of MBIR reduces image noise and also creates a “waxy” appearance (G–I). ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction
Table 2.
Percentage of diagnostic confidence per indication by CT protocol
| Standard-dose ASIR | Ultralow-dose ASIR | Ultralow-dose MBIR | |
|---|---|---|---|
| Airway Foreign Body | 100 | 97.5 | 97.5 |
| Fracture | 100 | 82.5 | 77.5 |
| Metastasis | 92.5 | 77.5 | 75 |
| Pulmonary Infection | 100 | 67.5 | 85 |
| Interstitial Lung Disease | 100 | 60 | 60 |
ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction.
Fig. 3.
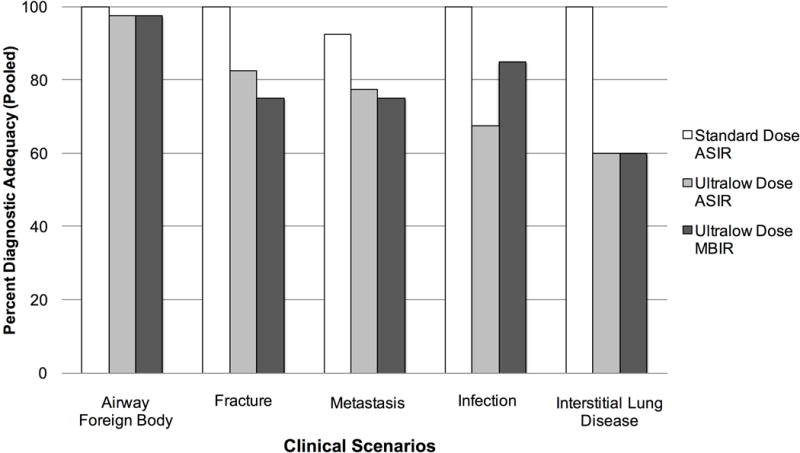
Radiologist diagnostic adequacy for detection of pathology by CT dose and reconstruction method. ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction
There was no significant difference in the ability of readers to confidently exclude airway foreign body between standard-dose chest CT, ultralow-dose chest CT with ASIR, and ultralow-dose chest CT with MBIR (p = 0.37). A clinical imaging example of an airway foreign body not identified on radiographs, but well seen with ultralow-dose chest CT and confirmed with bronchoscopy is depicted in Figure 4. The readers were not able to confidently exclude fracture, metastasis, pulmonary infection, or interstitial lung disease in ultralow-dose CT with both ASIR and MBIR. In these clinical queries, the diagnostic adequacy of ultralow-dose chest CT with both ASIR and MBIR was suboptimal in comparison to standard-dose CT (studies were deemed adequate in 60–85% of the ultralow-dose CTs versus 93–100% in the standard-dose CTs, p ≤ 0.002). In the evaluation for pulmonary infection, MBIR improved diagnostic adequacy over ASIR (85% versus 67.5%, p = 0.008). There was no significant difference among ultralow-dose chest CT reconstruction methods for the other four diagnoses. Interobserver agreement was good to very good in standard-dose chest CT (k = 0.77 - 1). Interobserver agreement in ultralow-dose chest CT was moderate to very good for airway foreign body, fracture and metastasis (k = 0.43 - 0.9) and poor to moderate in ultralow-dose chest CT with ASIR and MBIR for pulmonary infection and interstitial lung disease (k = 0 – 0.5).
Fig. 4.
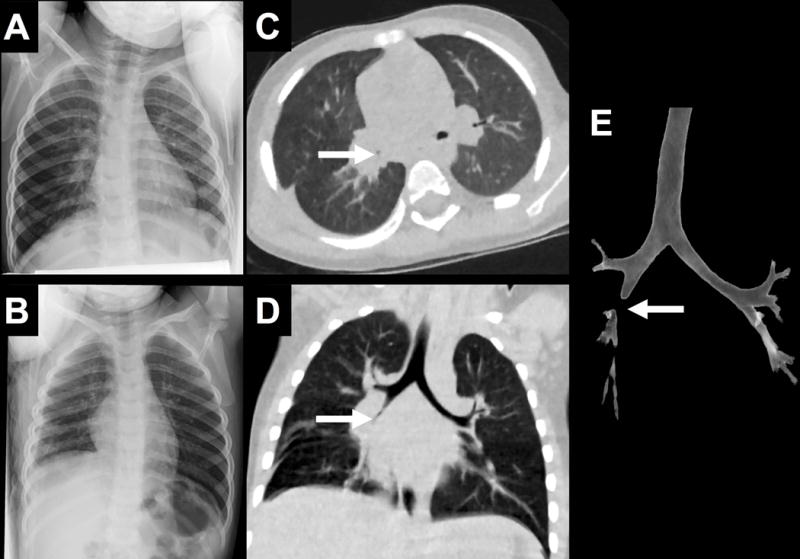
2-year-old boy with cough and exertional wheeze underwent frontal (not shown), left lateral (A) and right lateral decubitus (B) radiograph without evidence of foreign body or air trapping, respectively. Ultralow-dose chest CT reconstructed with MBIR (C, D) demonstrates occlusion of the right bronchus intermedius that is also depicted on 3D volumetric reformat of the central airways (E, white arrows). MBIR = Model Based Iterative Reconstruction
Overall, pairwise evaluation of ultralow-dose chest CT reconstructed with MBIR compared to ASIR revealed a slight advantage of MBIR, preferred in 58% of cases compared to 42% for ASIR (p < 0.01). Additionally, for all ultralow-dose CT comparison pairs, reconstruction with MBIR was preferred over reconstruction with ASIR. However, when taking into account readers as groups, the pediatric radiologists preferred MBIR to ASIR in 69% of the comparisons whereas the thoracic radiologists preferred ASIR to MBIR in 53% of the comparisons (p = 0.5). Intraclass correlation coefficient was 0.52, indicating moderate correlation between the readers.
Objective measurement
Detailed objective image quality measures are displayed in Table 3. There was a significant difference in the image noise at all sampled ROIs between standard-dose and ultralow-dose chest CT with both reconstruction methods (p < 0.01). For the ultralow-dose CT, objective image noise was significantly lower with MBIR compared to ASIR (p < 0.01). In post-hoc tests, image noise in ultralow-dose chest CT with MBIR was significantly lower than with ASIR (p < 0.01) and no significant difference was noted between standard-dose and ultralow-dose chest CT with ASIR (p > 0.05).
Table 3.
Attenuation (HU) in selected ROIs and study dose descriptors displayed as mean ± standard deviation
| Standard-dose ASIR | Ultralow-dose ASIR | Ultralow-dose MBIR | |
|---|---|---|---|
| Pectoralis | 28.9 ± 18.6 | 77.3 ± 18.2 | 20.0 ± 3.6 |
| Anterior mediastinum | 35.0 ± 21.2 | 82.9 ± 21.5 | 22.1 ± 4.7 |
| Axilla | 41.0 ± 20.9 | 78.7 ± 21.2 | 26.2 ± 4.9 |
| Paraspinal | 40.1 ± 20.4 | 108.3 ± 19.2 | 24.9 ± 5.3 |
| DLP (mGy × cm) | 96.8 ± 50.6 | 7.5 ± 2.9 | |
| CTDIvol (mGy) | 3.2 ± 1.4 | 0.2 ± 0.08 | |
| SSDE (mGy) | 4.9 ± 2.0 | 0.4 ± 0.1 | |
ASIR = Adaptive Statistical Iterative Reconstruction, MBIR = Model Based Iterative Reconstruction.
There was a significant difference in mean DLP and CTDIvol between standard-dose and ultralow-dose (p < 0.01). Compared to standard-dose CT, there was a 93% decrease in CTDIvol for ultralow-dose CT and mean patient SSDE was also reduced by 93% in ultralow-dose CT compared to standard-dose CT.
Discussion
The goal of this preliminary study was to evaluate the diagnostic adequacy of ultralow-dose pediatric chest CT with MBIR compared to ultralow-dose and standard-dose examinations with ASIR. We found that ultralow-dose CT with MBIR allowed readers to exclude airway foreign body, but not fracture or parenchymal lung disease. In pairwise comparisons of ultralow-dose CT, reconstruction with MBIR was preferred to ASIR. Additionally, we support prior studies demonstrating that ultralow-dose CT with MBIR allows for a significant reduction in radiation dose while preserving objective quality.
Our primary hypothesis: that our ultralow-dose protocol, originally intended for evaluating pectus excavatum, would be sufficient for certain pulmonary indications, was supported. Our secondary hypothesis was supported to a lesser extent, as the addition of MBIR did not completely restore the loss of diagnostic confidence that resulted from the dose reduction. MBIR is among a new generation of iterative reconstruction techniques shown to recover objective and subjective image quality in reduced-dose CT [13–15, 21, 22]. To date no study has evaluated the diagnostic adequacy of ultralow-dose chest CT in specific clinical scenarios. Our results show that ultralow-dose chest CT with MBIR is only equivalent to standard-dose chest CT in the evaluation of foreign body. Readers could not confidently exclude fracture or parenchymal lung disease in ultralow-dose chest CT reconstructed with either ASIR or MBIR. Although MBIR was able to recover diagnostic adequacy relative to ASIR in ultralow-dose CT for pulmonary infection, there was no significant improvement with MBIR for any of the other diagnoses.
Our findings support a prior study demonstrating a threshold limit of dose reduction at which diagnostic confidence falls below acceptable levels [23]. We suggest that ultralow-dose CT with MBIR may play an indication-specific role in pediatric imaging. As such, we propose an indication-specific prospective study in which patients are initially scanned using ultralow-dose CT protocol and subsequently receive standard-dose CT if further imaging is needed. However, depending on the required frequency of the standard-dose follow up, this may not be feasible given current concerns with radiation exposure, particularly in the pediatric population.
Overall, our readers favored MBIR to ASIR (58%) in pairwise comparison of ultralow-dose CT reconstruction methods. However, the pediatric radiologists preferred MBIR (69%) and the thoracic radiologists preferred ASIR (53%). Among the pediatric radiologists we recorded almost-perfect interobserver agreement, whereas among the thoracic radiologists agreement was only fair. Of note, at our institution MBIR has been applied to pediatric CT for two years whereas MBIR is not widely adopted for use in adult CT. Our comparison of MBIR to ASIR suggests that reader experience with reconstruction technique is an influential factor in determining preference. Here, we chose to include both adult and pediatric radiologists as in routine practice, particularly in the emergency setting, adult radiologists may be interpreting pediatric studies.
Similarly with MBIR, differences in image texture, in particular “smoothing” and a more “plastic-like appearance,” are well-described phenomena that may affect qualitative perception and alter clinical interpretation [14, 16, 24]. We attribute our observed variation in preference and agreement between pediatric and thoracic radiologists to the differences in their exposure to MBIR. We advise that future comparisons include readers familiar with all reconstruction methods.
Objectively, ultralow-dose CT with MBIR yields less image noise than both ultralow-dose and standard-dose chest CT with ASIR. Our results are consistent with several phantom and human studies [13–15, 22]. Along with this, we found that ultralow-dose CT permits a 93% reduction in both the CTDIvol and SSDE. Ultralow-dose CT results in effective doses within the range of posteroanterior and lateral chest radiographs (0.05 – 0.24 mSv) [25]. These measures show that ultralow-dose CT with MBIR restores image quality and may improve disease detection while decreasing the harmful potential effects of ionizing radiation exposure. However, in light of our qualitative assessment findings we suggest that objective metrics alone may not be sufficient to assess the clinical utility of reduced-dose CT.
While our study focused on the reader’s confidence to exclude findings on CT images, the provided example of an ultralow-dose chest CT in the setting of an airway foreign body suggests a potential clinical application. In the selected case, chest radiographs were unable to demonstrate an airway foreign body or secondary signs thereof, whereas the site of obstruction was readily identified with ultralow-dose chest CT. In current clinical practice, algorithms for management of suspected foreign body aspiration call for chest radiographs to be performed prior to CT, if CT is to be performed at all [26,27]. Given the comparable effective dose to two-view chest radiographs, our study invites future work to prospectively evaluate the use of ultralow-dose chest CT as the first-line imaging modality in the setting of suspected airway foreign body.
Our study has some limitations to consider. First, our results are dependent on the scanner system used, in particular the vendor-specific iterative reconstruction techniques of ASIR and MBIR. Despite this, we believe the approach, findings, and recommendations maintain significant general relevance. Second, our sample size was relatively small due to the low frequency of pectus excavatum. A larger, multicenter study may overcome this problem. Third, our study was retrospective and the clinical scenarios were hypothetical in nature. Although the ultralow-dose images were deemed insufficient, they may be diagnostic in the presence of disease. We propose further investigation with a prospective study for patients suspected to have airway foreign body, comparing the diagnostic ability of ultralow-dose CT, standard-dose CT, and bronchoscopy. Fourth, subjective evaluation is likely to have been affected by the lack of true blinding due to the differing appearance of reconstruction methods as well as the relative unfamiliarity of the thoracic radiologists with MBIR. Finally, we chose to evaluate the images on a non-PACS computer unintended for clinical diagnostic work in order to simplify the data blinding and ease of reader evaluation. While this choice may have decreased reader confidence in interpreting the images, the non-PACS monitor resolution was above that of the full-size CT images.
Conclusion
Ultralow-dose chest CT results in an effective radiation dose comparable to posteroanterior and lateral chest radiographs and may be adequate for the exclusion of an airway foreign body, but suboptimal for the evaluation of parenchymal lung disease. Although MBIR improves objective and subjective image quality in ultralow-dose CT, it does not reach diagnostic quality comparable to that of a standard-dose CT.
Acknowledgments
US Department of Health and Human Services - National Institutes of Health - National Institute of Biomedical Imaging and Bioengineering (2T32EB001631-11)
Footnotes
Disclosures: None
This study was compliant with Health Insurance Portability and Accountability Act guidelines and was approved by the Institutional Review Board. The requirement for informed consent was waived.
References
- 1.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 2.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. The Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strauss KJ, Goske MJ, Kaste SC, et al. Image Gently: Ten Steps You Can Take to Optimize Image Quality and Lower CT Dose for Pediatric Patients. American Journal of Roentgenology. 2010;194:868–873. doi: 10.2214/AJR.09.4091. [DOI] [PubMed] [Google Scholar]
- 4.Townsend BA, Callahan MJ, Zurakowski D, Taylor GA. Has Pediatric CT at Children’s Hospitals Reached Its Peak? American Journal of Roentgenology. 2010;194:1194–1196. doi: 10.2214/AJR.09.3682. [DOI] [PubMed] [Google Scholar]
- 5.Miglioretti DL, Johnson E, Williams A, et al. The Use of Computed Tomography in Pediatrics and the Associated Radiation Exposure and Estimated Cancer Risk. JAMA Pediatr. 2013;167:700–707. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marin D, Nelson RC, Schindera ST, et al. Low-Tube-Voltage, High-Tube-Current Multidetector Abdominal CT: Improved Image Quality and Decreased Radiation Dose with Adaptive Statistical Iterative Reconstruction Algorithm—Initial Clinical Experience. Radiology. 2010;254:145–153. doi: 10.1148/radiol.09090094. [DOI] [PubMed] [Google Scholar]
- 7.Singh S, Kalra MK, Hsieh J, et al. Abdominal CT: Comparison of Adaptive Statistical Iterative and Filtered Back Projection Reconstruction Techniques. Radiology. 2010;257:373–383. doi: 10.1148/radiol.10092212/-/DC1. [DOI] [PubMed] [Google Scholar]
- 8.Singh S, Kalra MK, Do S, et al. Comparison of hybrid and pure iterative reconstruction techniques with conventional filtered back projection: dose reduction potential in the abdomen. J Comput Assist Tomogr. 2012;36:347–353. doi: 10.1097/RCT.0b013e31824e639e. [DOI] [PubMed] [Google Scholar]
- 9.Willemink MJ, de Jong PA, Leiner T, et al. Iterative reconstruction techniques for computed tomography Part 1: Technical principles. Eur Radiol. 2013;23:1623–1631. doi: 10.1007/s00330-012-2765-y. [DOI] [PubMed] [Google Scholar]
- 10.Koc G, Courtier JL, Phelps A, et al. Computed tomography depiction of small pediatric vessels with model-based iterative reconstruction. Pediatr Radiol. 2014;44:787–794. doi: 10.1007/s00247-014-2899-y. [DOI] [PubMed] [Google Scholar]
- 11.Vardhanabhuti V, Loader RJ, Mitchell GR, et al. Image Quality Assessment of Standard- and Low-Dose Chest CT Using Filtered Back Projection, Adaptive Statistical Iterative Reconstruction, and Novel Model-Based Iterative Reconstruction Algorithms. American Journal of Roentgenology. 2013;200:545–552. doi: 10.2214/AJR.12.9424. [DOI] [PubMed] [Google Scholar]
- 12.Katsura M, Sato J, Akahane M, et al. Comparison of pure and hybrid iterative reconstruction techniques with conventional filtered back projection: image quality assessment in the cervicothoracic region. European Journal of Radiology. 2013;82:356–360. doi: 10.1016/j.ejrad.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Shuman WP, Green DE, Busey JM, et al. Model-Based Iterative Reconstruction Versus Adaptive Statistical Iterative Reconstruction and Filtered Back Projection in Liver 64-MDCT: Focal Lesion Detection, Lesion Conspicuity, and Image Noise. American Journal of Roentgenology. 2013;200:1071–1076. doi: 10.2214/AJR.12.8986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang W, Lee JM, Lee K, et al. Assessment of a model-based, iterative reconstruction algorithm (MBIR) regarding image quality and dose reduction in liver computed tomography. Invest Radiol. 2013;48:598–606. doi: 10.1097/RLI.0b013e3182899104. [DOI] [PubMed] [Google Scholar]
- 15.Smith EA, Dillman JR, Goodsitt MM, et al. Model-based Iterative Reconstruction: Effect on Patient Radiation Dose and Image Quality in Pediatric Body CT. Radiology. 2014;270:526–534. doi: 10.1148/radiol.13130362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miéville FA, Berteloot L, Grandjean A, et al. Model-based iterative reconstruction in pediatric chest CT: assessment of image quality in a prospective study of children with cystic fibrosis. Pediatr Radiol. 2013;43:558–567. doi: 10.1007/s00247-012-2554-4. [DOI] [PubMed] [Google Scholar]
- 17.Lambert J, MacKenzie JD, Cody DD, Gould R. Techniques and tactics for optimizing CT dose in adults and children: state of the art and future advances. J Am Coll Radiol. 2014;11:262–266. doi: 10.1016/j.jacr.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 18.Boone JM, Strauss KJ, Cody DD, et al. Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. College Park (MD): American Association of Physicists in Medicine (AAPM) 2011:28. AAPM report; no. 204. [Google Scholar]
- 19.Brink JA Morin RL. Size-specific Dose Estimation for CT: How Should It Be Used and What Does It Mean? Radiology. 2012;265:666–668. doi: 10.1148/radiol.12121919. [DOI] [PubMed] [Google Scholar]
- 20.Phelps AS, Naeger DM, Courtier JL, et al. Pairwise Comparison Versus Likert Scale for Biomedical Image Assessment. American Journal of Roentgenology. 2015;204:8–14. doi: 10.2214/AJR.14.13022. [DOI] [PubMed] [Google Scholar]
- 21.Katsura M, Matsuda I, Akahane M, et al. Model-based iterative reconstruction technique for ultralow-dose chest CT: comparison of pulmonary nodule detectability with the adaptive statistical iterative reconstruction technique. Invest Radiol. 2013;48:206–212. doi: 10.1097/RLI.0b013e31827efc3a. [DOI] [PubMed] [Google Scholar]
- 22.Newell JD, Jr, Fuld MK, Allmendinger T, et al. Very low-dose (0.15 mGy) chest CT protocols using the COPDGene 2 test object and a third-generation dual-source CT scanner with corresponding third-generation iterative reconstruction software. Invest Radiol. 2015;50:40–45. doi: 10.1097/RLI.0000000000000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Callahan MJ, Kleinman PL, Strauss KJ, et al. Pediatric CT Dose Reduction for Suspected Appendicitis: A Practice Quality Improvement Project Using Artificial Gaussian Noise—Part 1, Computer Simulations. American Journal of Roentgenology. 2015;204:W86–W94. doi: 10.2214/AJR.14.12964. [DOI] [PubMed] [Google Scholar]
- 24.Yoon MA, Kim SH, Lee JM, et al. Adaptive statistical iterative reconstruction and Veo: assessment of image quality and diagnostic performance in CT colonography at various radiation doses. J Comput Assist Tomogr. 2012;36:596–601. doi: 10.1097/RCT.0b013e31826092be. [DOI] [PubMed] [Google Scholar]
- 25.Mettler FA, Jr, Huda W, Yoshizumi TT, Mahesh M. Effective Doses in Radiology and Diagnostic Nuclear Medicine: A Catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 26.Giannoni CM, Guillerman RP. Computed Tomography for the Evaluation of Suspected Airway Foreign Bodies. Clinical Pediatric Emergency Medicine. 2015;16(4):230–234. doi: 10.1016/j.cpem.2015.11.004. [DOI] [Google Scholar]
- 27.Hitter A, Hullo E, Durand C, Righini CA. Diagnostic value of various investigations in children with suspected foreign body aspiration: review. European annals of otorhinolaryngology, head and neck diseases. 2011;128(5):248–252. doi: 10.1016/j.anorl.2010.12.011. [DOI] [PubMed] [Google Scholar]


