Abstract
Context
Some evidence suggests that treating vascular risk factors and performing mentally stimulating activities may delay cognitive impairment onset in older adults. Exposure to a complex neighborhood environment may be one mechanism to help delay cognitive decline.
Evidence acquisition
PubMed, Web of Science, and ProQuest Dissertation and Theses Global database were systematically reviewed, identifying 25 studies published from February 1, 1989 to March 5, 2016 (data synthesized, May 3, 2015–October 7, 2016). The review restricted to quantitative studies focused on: (1) neighborhood social and built environment and cognition; and (2) community-dwelling adults aged ≥45 years.
Evidence synthesis
The majority of studies were cross-sectional, U.S.-based, and found at least one significant association. The diversity of measures and neighborhood definitions limited the synthesis of findings in many instances. Evidence was moderately strong for an association between neighborhood SES and cognition and modest for associations between neighborhood demographics, design, and destination accessibility and cognition. Most studies examining effect modification found significant associations, with some evidence for effect modification of the neighborhood SES–cognition association by individual-level SES. No studies had low risk of bias and many tested multiple associations that increased the chance of a statistically significant finding. Considering the studies to date, the evidence for an association between neighborhood characteristics and cognition is modest.
Conclusions
Future studies should include longitudinal measures of neighborhood characteristics and cognition, examine potential effect modifiers such as sex and disability, and study mediators that may help elucidate the biological mechanisms linking neighborhood environment and cognition.
CONTEXT
At least 10% of older adults (aged ≥65 years) have mild cognitive impairment1 and approximately 5 million Americans have Alzheimer disease dementia (AD),2 conditions that will increase in incidence with the projected rise in population of older adults.3,4 To date, no effective treatments are available to ameliorate or cure AD, the most common neurodegenerative cause of cognitive impairment. However, some research suggests that treating vascular risk factors and performing cognitively stimulating activities may delay the onset of cognitive impairment5 and reduce AD pathology.6 Exposure to complex, stimulating neighborhood environments may be one mechanism that delays cognitive impairment.7
Recently, studies have started examining how the neighborhood social environment (SE) and built environment (BE) may affect cognition in older adults. The BE encompasses the physical aspects of living and work environments, including the placement and configuration of roads, homes, commercial buildings, and public spaces; whereas the SE includes human-centered characteristics, such as demographics, SES, social disorder, and social climate. A literature review of neighborhood environment and health in older adults8 found that neighborhood SES (NSES) was more frequently associated with health than neighborhood BE measures, and the only study of cognition found that living in neighborhoods with less educated residents was associated with worse cognition.9 In another systematic review focused on community environment and cognition in older adults,10 the authors also found that lower community SES was frequently associated with worse cognition.
The same mechanisms that link the neighborhood environment and physical activity, blood pressure, obesity, depression, and quality of life11–15 may explain associations between the neighborhood environment and cognition. The mechanisms may relate to the neighborhood’s impact on personal mobility, one’s sense of security and safety, potential for chance interactions, exercise and social engagement, access to healthy foods and green space, and exposure to pollution, crime, and social deprivation. For older adults, the neighborhood may become more important with increasingly less time in motorized transportation and more time in the neighborhood.16 The neighborhood environment’s impact on health may be intensified by physical disability or difficulty navigating and interacting in the neighborhood due to normal cognitive aging.7 Additionally, the neighborhood may play a strong role in determining the social ties and social participation among older adults,17,18 which can affect psychological health and well-being.
Approximately 80% of the U.S. population lived in urban areas in 201019 and more than 90% of older adults would like to age in place, staying in their homes and neighborhoods for as long as possible.20 Compared with the SE, the BE is more directly targeted by city and regional planning efforts and has been studied less in relation to cognition in older adults. Therefore, this study aimed to systematically review publications on the neighborhood SE and BE and cognition in older adults, with added emphasis on the BE and effect modification (e.g., differential impact on vulnerable populations), two areas that were mentioned only briefly in a 2014 review of community environment and cognition.21
EVIDENCE ACQUISITION
Neighborhoods were defined as geographic areas smaller than towns, cities, or counties and were delineated using administrative boundaries, circumscribed areas (e.g., 0.5 miles around home), or perceived geographic boundaries. The environment surrounding the home was chosen to represent the social and physical exposures likely to affect older adults frequently.
Neuropsychological tests are one means of evaluating cognitive functioning, and have been designed to measure global cognition as well as various cognitive domains (e.g., memory, language).22 In this review, cognition could have been determined by a clinician or assessed using brief cognitive measures such as the Mini Mental State Exam (MMSE) or domain-specific neuropsychological tests.
Search Criteria
PubMed, Web of Science (all databases), and ProQuest Dissertation and Theses Global database were systematically reviewed for papers and dissertations published through March 5, 2016 (resulted in publications from February 1, 1989). The following keywords were searched: (built environment or neighborhood environment or neighborhood level or walkability) AND (cognition or cognitive function or cognitive decline or cognitive impairment or dementia or Alzheimer or Alzheimer’s or demented or cognitive or memory). Given these search criteria, results were likely to include studies of the BE, SE, or both.
Screening Procedure
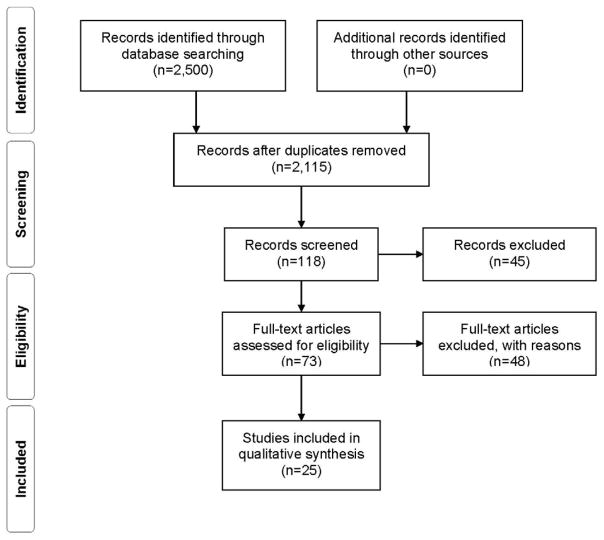
Downloaded 2,500 unscreened citations meeting search criteria.
Eliminated duplicates (n=385).
Eliminated unrelated titles (n=1,997).
Eliminated abstracts not in English or not covering topic of interest (n=45).
Eliminated full-text publications (n=48) not in English, not quantitative, or not focused on: community-dwelling adults aged ≥45 years, neighborhood-level characteristics, or the neighborhood–cognition association.
Methods
The SE findings were synthesized into four categories: SES (e.g., income), demographics (e.g., race/ethnicity), social disorder (e.g., crime), and social climate/social ties (e.g., social support). The BE findings were grouped according to the “5D’s” previously proposed to influence travel behavior23: density (e.g., population density, density of social destinations), diversity (e.g., land use mix), design (e.g., intersection density, presence of sidewalks), destination accessibility (e.g., distance to nearest store), and distance to transit (e.g., nearest bus stop). The “5D” categories allow for a synthesis using terminology that is frequently used in neighborhood research and relatable to city planners. Data were synthesized between May 3, 2015 and October 7, 2016.
The studies were too disparate to evaluate whether they met the epidemiologic criteria for causality. Instead, the risk of bias by participant selection, confounding of the neighborhood–cognition association, and missing data (all variables) was determined using the Risk Of Bias in Non-randomized Studies - of Interventions (ROBINS-I) tool,24–26 which helped assess the strength of evidence to date. Additionally, six criteria were developed to evaluate the neighborhood measures (did not provide validity/reliability, used one or more perceived measure, and used one or more composite measure) and cognitive measures (did not provide validity/reliability, used one or more composite measure, and no longitudinal measure used). Bias can occur if perceived measures of the neighborhood relate to cognition28 or if the neighborhood or cognitive measures are associated with measurement error29,30 (e.g., invalid measures,31 composite measure27). Each domain (e.g., selection) was evaluated for risk of bias (low=1, moderate=2, serious=3, critical=4), and overall risk of bias was calculated by a simple average of the domain scores.
EVIDENCE SYNTHESIS
The final sample included 25 studies9,17,32–54 (Figure 1). Six non-U.S. studies were from the Netherlands, United Kingdom (UK), Japan, and Singapore.32,37,41,45,50,53 The majority focused on adults aged ≥65 years (36% included <65-year-olds) and 80% included minorities. Appendices 1–5 outline study details.
Figure 1.
Sample size flow diagram.
Research Methods
Sixty-eight percent of samples originated from cohort studies, with the remaining based on clinical trials or other observational studies. Seventy-six percent of samples were population-based or randomly sampled. Eleven32,37,38,45,47,49–54 studies used the MMSE, five studies9,17,35,40,43 used the Telephone Interview for Cognitive Status, five used domain-specific cognitive measures,39,42,44,48,51 and four used composite cognitive measures.33,34,36,41 Eighty-four percent of studies used continuous measures of cognition instead of categorical/dichotomous measures, and ten studies used longitudinal cognitive measures.33,36,40,43–47,51,52
Most studies focused on objective neighborhood measures, with only four33,34,45,54 including perceived measures (i.e., neighborhood social disorder, neighborhood climate, number of friendly neighbors, neighborhood homogeneity, distance to community resources). Almost half of the studies (n=12) used U.S. Census tracts to define neighborhoods, with the remaining using U.S. Census block groups, neighborhood perceptions, alternative definitions such as city-defined boundaries, or other regional definitions (e.g., UK enumeration district).
Neighborhood Social Characteristics and Cognition
Twenty-two studies examined the association between neighborhood SE and cognition.9,17,32–35,38–50,52–54
Neighborhood SES
Eight of 15 studies found that lower NSES was associated with worse cognition (Table 1), with 78% of cross-sectional and 17% of longitudinal studies finding a significant association. The majority (n=13) of studies developed composite measures of NSES based on components such as the proportion with no high school degree or living in poverty. All SES measures were based on objective data sources such as the U.S. Census.
Table 1.
Findings for Studies Examining Neighborhood Social Characteristics and Cognition Among Older Adults
| Author (year) | Study design | SESa | Demographicsb | Psychosocial disorderc | Social climate/social tiesd |
|---|---|---|---|---|---|
|
| |||||
| n=15 | n=8 | n=5 | n=2 | ||
| Aneshensel et al. (2011) | Cross-sectional | + | NS | ||
| Basta et al. (2008) | Cross-sectional | + | |||
| Boardman (2012) | Longitudinal | NS | + | ||
| Brown (2009) | Cross-sectional | + | |||
| Clarke (2012) | Cross-sectional | + | + | NS | |
| Espino (2001) | Cross-sectional | + | |||
| Glass (2009) | Cross-sectional | NS | |||
| Kovalchik (2015) | Longitudinal | NS | |||
| Lang (2008) | Cross-sectional | + | |||
| Lee (2011) | Cross-sectional | + | |||
| Magaziner (1989) | Cross-sectional | NS | |||
| Martinez (2007) | Longitudinal | NS | + | ||
| Meyer (2015) | Longitudinal | NS | NS | ||
| Murayama (2013) | Longitudinal | NS | |||
| Rej (2015) | Longitudinal | NS | |||
| Sheffield (2009) | Longitudinal | + | + | ||
| Shih (2011) | Cross-sectional | NS | |||
| Sisco (2012) | Cross-sectional | + | |||
| Wee (2012) | Cross-sectional | + | |||
| Wight (2006) | Cross-sectional | + | |||
| Wu (2015) | Cross-sectional | NS | NS | ||
| Zeki Al Hazzouri (2011) | Longitudinal | NS | |||
| Total significant studies | 8 of 15 | 4 of 8 | 2 of 5 | 1 of 2 | |
Notes: + = At least one statistically significant association between neighborhood characteristic and cognition; NS = association between neighborhood characteristic and cognition was not statistically significant.
Includes composite measures of SES and measures of income or wealth, employment, and education.
Includes measures of age, race/ethnicity, and perceived homogeneity with neighbors.
Includes measures such as presence of graffiti and crime.
Includes measures of neighboring, social support/acts, and social ties in neighborhood (e.g., number of friends in neighborhood).
Neighborhood demographics
Four of eight studies found that neighborhood demographics were associated with cognition (Table 1). Living in a neighborhood with a greater percentage of adults aged ≥65 years35 and fewer Hispanics38 or African Americans43 was associated with better cognition. Conversely, a greater percentage of Mexican Americans was associated with decreased odds of cognitive decline.47 Two of four longitudinal studies43,47 of neighborhood race (African American, Hispanic, or minority) found a significant association with cognition. Perceived homogeneity of neighbor characteristics was not associated with cognitive decline in a Japanese sample.45
Psychosocial disorder and social climate
Two of five studies33,42 (one cross-sectional, one longitudinal) found that greater psychosocial disorder was associated with worse cognition (Table 1). In two cross-sectional studies on social climate, positive acts of neighboring were associated with better cognition,34 but perceptions of friendly neighbors or the number of children, relatives, and friends in the neighborhood was not associated with cognition.54
Neighborhood Built Environment and Cognition
Six studies examined neighborhood BE and cognition,35,36,43,51,53,54 using a wide variety of neighborhood definitions (i.e., city block, U.S. Census tract, U.S. Census block group, perceived neighborhood, 0.5-mile radius around home, UK Lower-layer Super Output Area), and data sources (i.e., block observations, city-based geographic data, audit, participant report, U.S. Census, map data, UK neighborhood statistics).
Density
One of three cross-sectional studies53 examining density found an association with cognition (Table 2). Neighborhood area dedicated to natural environment (hence, lower population density) was associated with worse cognition in an English sample53; however, increased neighborhood park area was not associated with cognition in a U.S.-based sample.35 The single study examining population density and cognition found no association.43
Table 2.
Findings for Studies Examining Neighborhood Built Environment Characteristics and Cognition Among Older Adults
| Author (year) | Study design | Built environment categories
|
||||
|---|---|---|---|---|---|---|
| Densitya n=3 |
Designa n=2 |
Destinationa n=3 |
Diversitya n=1 |
Distance to transita n=1 |
||
| Clarke (2012) | Cross-sectional | NS | NS | |||
| Clarke (2015) | Longitudinal | + | + | + | ||
| Magaziner (1989) | Cross-sectional | + | ||||
| Martinez (2007) | Longitudinal | NS | ||||
| Watts (2015) | Longitudinal | + | ||||
| Wu (2015) | Cross-sectional | + | + | |||
| Total significant studies | 1 out of 3 | 2 out of 2 | 2 out of 3 | 1 out of 1 | 1 out of 1 | |
Notes: + = At least one statistically significant association between neighborhood characteristic and cognition; NS = association between neighborhood characteristic and cognition was not statistically significant.
Density: e.g., population density, density of social destinations; Diversity: e.g., land use mix, business types in the neighborhood; Design: e.g., intersection density, presence of sidewalks; Destination accessibility: e.g., distance to nearest store; Distance to transit: e.g., distance to nearest bus stop.
Design
Both studies of neighborhood design found an association with longitudinal measures of cognition (Table 2). Neighborhoods in poor condition (deterioration of public spaces) but not those lacking pedestrian facilities were associated with accelerated cognitive decline.36 Additionally, greater street connectivity was associated with faster cognitive decline using one measure (fewer turns needed to reach all other streets in network) but slower cognitive decline using another (greater paths/streets connected to each street).51
Destination accessibility
Three studies (two cross-sectional, one longitudinal) examined the association between neighborhood destination accessibility and cognition (Table 2). An increased distance to community resources54 and presence of a community center,36 but not presence of recreational centers and institutions (e.g., schools),35 were associated with better cognition.
Diversity of land uses and distance to transit
Neighborhood diversity of land uses was associated with lower odds of dementia,53 and the presence of a neighborhood transit stop was associated with slower cognitive decline36 (Table 2).
Effect Modification of Neighborhood Environment–Cognition Association
Thirteen studies investigated effect modification9,17,32–35,37,39–42,49,54 of the association between neighborhood characteristics and cognition.
Four of five cross-sectional studies found that individual-level SES modified the association between neighborhood SE and cognition.9,17,32,37,49 Having low personal SES and living in a low-SES neighborhood was associated with worse cognition in two studies.9,17 By contrast, two studies found that the association between NSES and cognition was strongest when personal SES did not match NSES (i.e., low personal SES, high NSES; high personal SES, low NSES).32,37 In addition, a higher percentage of African Americans was cross-sectionally associated with worse cognition in those with lower education and better cognition in those with higher education.17
Three of six studies of the neighborhood SE and one study of the neighborhood BE found effect modification by individual-level demographics.17,34,35,40,41,49 Individual-level race was not an effect modifier of the longitudinal association between neighborhood racial composition and cognition40 or the cross-sectional association between NSES and cognition.49 Sex did not modify the association between neighborhood social climate (e.g., social ties) and cognition.34 However, higher NSES was associated with better cognition among younger participants49 and in all but <70-year-old men41 in two cross-sectional studies. Finally, the presence of institutional resources (e.g., community center) was cross-sectionally associated with better cognition among whites but worse cognition among African Americans.35
Both studies examining effect modification by apolipoprotein E e4 carrier status (APOE-e4; risk factor for AD) found significant associations.33,42 The first found that although APOE-e4 genotype was associated with faster cognitive decline, the association was strongest when psychosocial disorder was low.33 The second, cross-sectional study found that APOE-e4 carriers in the least psychosocially hazardous neighborhoods had cognitive levels similar to APOE-e4 non-carriers, and APOE-e4 carriers in the most psychosocially hazardous neighborhoods had worse cognition compared with APOE-e4 non-carriers in neighborhoods with lower psychosocial hazards.42
Three studies examined effect modification by other individual-level factors.35,39,54 Neighborhoods with a higher percentage of older adults were associated with better cognition among those living 6–10 years in their neighborhood but worse cognition among those living >10 years in their neighborhood.35 The association between community resources (e.g., number of children in neighborhood) and cognition did not differ among those who lived with others versus lived alone.54 Finally, the association between higher tibia lead levels and worse cognition was stronger in those with higher versus lower neighborhood psychosocial disorder.39
Risk of Bias
Selection bias
Eight studies used sampling weights or propensity scores to reduce the risk of selection bias,9,17,33,35,40–43 and 11 studies demonstrated a lack of overlap (by >2 years) between the dates in which the neighborhood and cognitive measures were collected.9,17,33,36,38,39,41,43,46,47,52 Based on the ROBINS-I evaluation criteria, 19 studies had a moderate risk and six studies had a moderate to serious risk of selection bias (Table 3).
Table 3.
Potential Risk of Bias in the 25 Reviewed Papers
| Paper | Domains
|
Overall risk of biasd | ||||
|---|---|---|---|---|---|---|
| Selectiona | Confoundinga | Missing dataa | Neighborhood measure(s)b | Cognitive measure(s)c | ||
| Aneshensel et al.17 | Moderate | Moderate | NA | Moderate | Low | Moderate |
| Basta et al.24 | Moderate | Serious | Low | Moderate | Moderate | Moderate |
| Boardman et al.25 | Moderate | Serious | NA | Moderate | Moderate | Moderate |
| Brown et al.26 | Moderate | Serious | NA | Moderate | Moderate | Moderate |
| Clarke et al.27 | Moderate | Moderate | NA | Low | Moderate | Moderate |
| Clarke et al.28 | Moderate-serious | Moderate | NA | Low | Moderate | Moderate |
| Deeg et al.29 | Moderate | Serious | NA | Moderate | Moderate | Moderate |
| Espino et al.30 | Moderate-serious | Serious | NA | Moderate | Moderate | Moderate |
| Glass et al.31 | Moderate-serious | Serious | NA | Moderate | Moderate | Moderate |
| Kovalchik et al.32 | Moderate | Moderate | NA | Low | Low | Low-moderate |
| Lang et al.33 | Moderate | Serious | NA | Moderate | Serious | Moderate-serious |
| Lee et al.34 | Moderate | Moderate | NA | Moderate | Serious | Moderate |
| Magaziner et al.46 | Moderate | Serious | NA | Serious | Moderate | Moderate-serious |
| Martinez et al.35 | Moderate | Moderate | NA | Low | Low | Low-moderate |
| Meyer et al.36 | Moderate | Serious | NA | Moderate | Low | Moderate |
| Murayama et al.37 | Moderate | Moderate-serious | NA | Moderate | Low | Moderate |
| Rej et al.38 | Moderate-serious | Critical | NA | Low | NA | Moderate-serious |
| Sheffield et al.39 | Moderate-serious | Moderate | Low-moderate | Moderate | Low | Moderate |
| Shih et al.41 | Moderate | Moderate | Low-moderate | Moderate | Low | Moderate |
| Sisco et al.40 | Moderate | Serious | NA | Moderate | Moderate | Moderate |
| Watts et al.43 | Moderate | Serious | NA | Low | Low | Moderate |
| Wee et al.42 | Moderate | Moderate | NA | Moderate | Low | Moderate |
| Wight et al.9 | Moderate | Moderate | Low-moderate | Low | Low | Low-moderate |
| Wu et al.45 | Moderate | Moderate-serious | NA | Moderate | Moderate | Moderate |
| Zeki al Hazzouri et al.44 | Moderate-serious | Serious | Moderate | Low | Low | Moderate |
Three criteria were developed to evaluate neighborhood measures: (1) Did not provide validity/reliability; (2) Used ≥1 perceived neighborhood measure; (3) Used ≥1 composite neighborhood measure.
Three criteria were developed to evaluate cognitive measures: (1) Did not provide validity/reliability; (2) Used ≥1 composite measure of cognition; (3) Did not use longitudinal measure.
The overall risk of bias was calculated by a simple average of the scores for the specific domains (Low=1, Moderate=2, Serious=3, Critical=4).
NA, not applicable
Confounding
Ten studies controlled for covariates (i.e., age, sex, race/ethnicity, income, education, married) hypothesized to be related to neighborhood characteristics and cognitive measures, and therefore were determined to have a moderate risk of residual confounding (Table 3).9,17,35,40,42,43,47,49,50,55 The study with a critical risk for residual confounding did not adjust for any covariates, and the 14 remaining studies with moderate to serious risk did not adjust for at least one covariate.
Missing data
Twenty studies failed to delineate missing data on the neighborhood characteristics, cognitive measures, or covariates, and therefore were not assessed for risk owing to missing data. Five studies9,32,47,49,52 used statistical methods or sensitivity analyses to account for missing data, and among these, one study had a low risk of bias due to missing data because few data were missing32 (Table 3). Three studies were determined to have low to moderate risk because some evidence suggested that the results were not robust to missing data.9,47,49 The fifth study showed that the results were not robust to missing data, and was categorized as moderate risk.52
Neighborhood measures
Eight studies met one or fewer of the criteria developed to evaluate the neighborhood measures (low risk of bias due to the neighborhood measure), 16 met two criteria (moderate risk), and one54 met all three criteria (serious risk) (Table 3).
Cognitive measures
Eleven papers met one or fewer of the criteria developed to evaluate the cognitive measures (low risk of bias due to the cognition measure), 12 met two criteria (moderate risk), and two 41,42 met all three criteria (serious risk).
DISCUSSION
More than half of the 25 reviewed studies found associations between neighborhood characteristics and cognition. The studies provided moderately strong evidence for an association between NSES and cognition and modest evidence for associations between neighborhood demographics, design, and destination accessibility and cognition. Similarly, most studies investigating effect modifiers found significant associations, with some evidence for effect modification of the association between NSES and cognition by individual-level SES. In addition, some evidence suggested that individual-level demographics and APOE-e4 genotype modify the association between the neighborhood SE and cognition. Although few studies examined effect modification, and the neighborhood measures and effect modifiers were too variable, the significant findings suggest that studies of effect modification may be a fruitful line of research. Considered together, no studies were found to have low risk of bias, the effect sizes were often small, and many of the studies tested multiple neighborhood–cognition associations that increased the chance of a statistically significant finding. Additionally, the combinations of neighborhood measures examined were inconsistent across the studies, and thus did not allow for a more thorough critique. Therefore, the evidence for an association between neighborhood characteristics and cognition is modest to date.
Lower NSES was associated with worse cognition after controlling for personal SES, a strong predictor of mortality and AD risk.56,57 NSES has been associated with multiple health outcomes58–60 and may be independently associated with cognition by affecting an individual’s social interactions and level of social isolation,61,62 which indirectly affect health. Few longitudinal studies found significant associations; thus, it is possible that NSES is associated with lifelong disparities in cognition but not late-life differences in cognitive decline. Nonetheless, social isolation is a plausible mechanism for the observed associations between lower NSES and worse cognition, and should be examined as a potential mediator in future studies.
Controlling for individual- and neighborhood-level SES and race may not fully account for the psychosocial impact of racism and segregation that can influence health.17,63 Only 27% of the reviewed studies examining NSES controlled for neighborhood racial composition; therefore, future studies will need to develop valid measures of and control for segregation, which may be independently associated with worse cognition.
Having lower personal SES and living in higher-SES neighborhoods may cause social isolation, leading to poorer well-being and health consistent with the local social inequality model.37,64 By contrast, low-SES individuals who have better cognition when living in higher-SES neighborhoods are consistent with the collective resources model, in which they benefit from increased material and social resources.64 Two studies supported the collective resources model9,17 and two supported the local social inequality model32,37; thus, there is insufficient evidence to conclude if either of these models are at play, and additional research is needed on the interaction between individual- and neighborhood-level SES.
The reviewed studies demonstrated inconsistent associations between neighborhood psychosocial hazards and cognition. The only longitudinal study found a significant association with cognitive decline, but it used perceived measures to construct a composite measure of neighborhood psychosocial hazards. Perceived measures represent individual-based assessments that may be laden with other subjective influences, and composite measures can be associated with measurement error and lack specificity, which hinders the ability to pinpoint the causal mechanisms. The remaining studies were cross-sectional and used different objective measures of neighborhood psychosocial hazards. Overall, future studies of psychosocial hazards and cognition would benefit from using longitudinal measures of cognition and psychosocial hazard measures that are objective and measured individually. Additionally, future studies could examine potential mediators such as social engagement, isolation, well-being, and mental health, which would help support a mechanism by which any observed associations can be explained by social engagement/isolation.
A majority of the BE studies found significant associations. Cognition was associated with neighborhoods with a community center or transit stop, public spaces in poor condition, distance to community resources, street connectivity, land use mix, and area dedicated to the natural environment. Only a single study examined potential modifiers of the BE–cognition association, finding that number of years living in the neighborhood modifies the cross-sectional association between neighborhood percentage of older adults and cognition. Overall, the BE studies to date provide suggestive evidence for an association between neighborhood design and destination accessibility and cognition. However, given this nascent field of research, new studies are needed to refine the BE and neighborhood measures, examine longitudinal measures of cognition, examine potential mediators and moderators, and elucidate the associated causal mechanisms.
Quality of Studies
The majority of studies were at moderate to serious risk of bias due to selection, residual confounding, and missing data. New studies should use methods such as sampling weights or propensity scores to reduce selection bias and use techniques such as multiple imputation to address bias due to missing data. Additionally, future studies should effectively measure and control for individual characteristics that are likely associated with the neighborhood characteristics and cognition to reduce the possibility of residual confounding, which may help explain the studies finding associations in unexpected directions.
Most of the studies defined neighborhoods using administrative boundaries set by national or local governments (e.g., U.S. Census tracts). Although this may allow for more consistent neighborhood definitions across studies, Census tracts are typically employed out of convenience, which ignores the potential that different neighborhood definitions may be more appropriate based on the neighborhood measure of interest and the proposed biological mechanism responsible for its association with cognition.28 In addition, individuals living at the edge of a Census tract may be misclassified, if they typically walk in the neighboring Census tract. New studies can build upon the previous work, transitioning from using administrative boundaries to other measures such as of the 0.5-mile area around a participant’s home, which may better reflect the nearby places and the distances an older adult would walk.
The employed neighborhood measures had a number of other weaknesses. Firstly, the characteristics measured to date may be only rough proxies of the neighborhood qualities associated with improved or worsened cognition. For example, population density could serve as a proxy for BE characteristics such as destination accessibility or SE characteristics such as chance social interactions. Secondly, 44% of the studies used neighborhood data collected at a different time than the cognitive data, which may result in bias related to measurement error. Lastly, all of the studies failed to account for longer-term neighborhood exposures that may be more important that late-life neighborhood exposures. For instance, if an individual lived for many years in a dense urban environment and recently moved to the suburbs, simply using measurements of the current suburban environment would inaccurately reflect lifelong neighborhood exposures. Any association with cognition under these conditions would be hard to disentangle without additional information about residential history. Considering these weaknesses, much more work is needed to understand the neighborhood constructs that affect cognition, the ideal time points in which they should be measured, and the best ways to measure them.
The existing studies failed to address regional context, specifically the potential influence of nearby neighborhoods and the comparability of findings across regions. Neighborhoods that border a residence may influence study findings, if for instance, the affluence or disadvantage of surrounding neighborhoods decreases or increases accessibility to social destinations or community resources. Overall context of the town, city, or metropolitan area may be important to consider, as exemplified by a study finding that a neighborhood’s regional location mattered more for neighborhood walking for commuting compared with the neighborhood’s BE.65 Additionally, the studies could have provided more thorough evaluations of the reasons why the neighborhood measures included may have limited external validity. For example, the variability of the neighborhood measures may not be comparable across cities, metropolitan regions, or countries, and certain neighborhood features (e.g., availability of walking paths) may have more influence than others based on regional cultural norms.
Most of the studies used brief cognitive tests (e.g., MMSE), which do not effectively measure particular cognitive domains that could assist in determining the biological mechanism by which the neighborhood environment relates to cognition. For example, if the neighborhood environment is hypothesized to influence cognition via the mechanism of social engagement, tests previously associated with social engagement (e.g., perceptual speed test66) would be preferred over non-specific screening instruments such as the MMSE.
Limitations
This review is not without limitations. It was difficult to assess the strength of the evidence and causality given the limited studies to date, the variability of neighborhood and cognitive measures, and the cross-sectional study designs. Inconsistent findings may be due to the fact that no studies examined early-life neighborhood exposures, which have been associated with cognition.67–70 Although the searched databases are comprehensive and cover a broad range of disciplines, this review may have missed some papers. In addition, the review could be affected by positive publication bias. Lastly, the method used to evaluate bias due to the neighborhood and cognitive measures has not been validated, but nonetheless provided a means of assessing the strength of the measures.
CONCLUSIONS
Few studies have examined associations between cognition and the neighborhood SE and BE. A large majority of the reviewed studies found at least one significant association, suggesting that the neighborhood environment may be associated with cognition. Although the published studies are a good starting point, future studies will need to use standardized BE measures and replicate and expand upon previous findings by including longitudinal measures of cognition; considering longer-term neighborhood exposures; considering the impact of moves, residential tenure, and time spent in and around the neighborhood; and considering the potential for individual-level effect modifiers and mediators. Finally, because the existing studies did not provide adequate evaluation or support for particular causal mechanisms, future studies are needed to tease apart and test the causal mechanisms by design.
Supplementary Material
Acknowledgments
Lilah Besser conceived of the study idea, performed the systematic review, and wrote and revised the first draft of the manuscript. Noreen McDonald, Walter Kukull, and Daniel Rodriguez helped with the study design, interpretation of findings, and editing of the manuscript.
No financial disclosures were reported by the authors of this paper.
References
- 1.Langa KM, Levine DA. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA. 2014;312(23):2551–2561. doi: 10.1001/jama.2014.13806. https://doi.org/10.1001/jama.2014.13806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alzheimer’s Association. [Accessed August 22, 2014];Alzheimer’s Disease Facts and Figures. 2014 www.alz.org/downloads/facts_figures_2014.pdf.
- 3.Administration for Community Living. [Accessed August 22, 2015];Administration on Aging - Aging Statistics. www.aoa.acl.gov/Aging_Statistics/index.aspx.
- 4.U.S. Census. [Accessed August 22, 2015];An Aging Nation: The Older Population in the United States - Population Estimates and Projections. www.census.gov/prod/2014pubs/p25-1140.pdf.
- 5.Nelson L, Tabet N. Slowing the progression of Alzheimer’s disease; what works? Ageing Res Rev. 2015;23(Pt B):193–209. doi: 10.1016/j.arr.2015.07.002. https://doi.org/10.1016/j.arr.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Vemuri P, Lesnick TG, Przybelski SA, et al. Effect of intellectual enrichment on AD biomarker trajectories: Longitudinal imaging study. Neurology. 2016;86(12):1128–1135. doi: 10.1212/WNL.0000000000002490. https://doi.org/10.1212/WNL.0000000000002490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cassarino M, Setti A. Environment as ‘Brain Training’: A review of geographical and physical environmental influences on cognitive ageing. Ageing Res Rev. 2015;23(Pt B):167–182. doi: 10.1016/j.arr.2015.06.003. https://doi.org/10.1016/j.arr.2015.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. https://doi.org/10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wight RG, Aneshensel CS, Miller-Martinez D, et al. Urban neighborhood context, educational attainment, and cognitive function among older adults. Am J Epidemiol. 2006;163(12):1071–1078. doi: 10.1093/aje/kwj176. https://doi.org/10.1093/aje/kwj176. [DOI] [PubMed] [Google Scholar]
- 10.Wu YT, Prina AM, Brayne C. The association between community environment and cognitive function: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2015;50(3):351–362. doi: 10.1007/s00127-014-0945-6. https://doi.org/10.1007/s00127-014-0945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallis JF, Saelens BE, Frank LD, et al. Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med. 2009;68(7):1285–1293. doi: 10.1016/j.socscimed.2009.01.017. https://doi.org/10.1016/j.socscimed.2009.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li F, Harmer P, Cardinal BJ, et al. Built environment and 1-year change in weight and waist circumference in middle-aged and older adults: Portland Neighborhood Environment and Health Study. Am J Epidemiol. 2009;169(4):401–408. doi: 10.1093/aje/kwn398. https://doi.org/10.1093/aje/kwn398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Renalds A, Smith TH, Hale PJ. A systematic review of built environment and health. Fam Community Health. 2010;33(1):68–78. doi: 10.1097/FCH.0b013e3181c4e2e5. https://doi.org/10.1097/FCH.0b013e3181c4e2e5. [DOI] [PubMed] [Google Scholar]
- 14.Mair C, Diez Roux AV, Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62(11):940–946. doi: 10.1136/jech.2007.066605. https://doi.org/10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 15.Koohsari MJ, Badland H, Sugiyama T, Mavoa S, Christian H, Giles-Corti B. Mismatch between perceived and objectively measured land use mix and street connectivity: associations with neighborhood walking. J Urban Health. 2015;92(2):242–252. doi: 10.1007/s11524-014-9928-x. https://doi.org/10.1007/s11524-014-9928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levasseur M, Généreux M, Bruneau JF, et al. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: results from a scoping study. BMC Public Health. 2015;15:503. doi: 10.1186/s12889-015-1824-0. https://doi.org/10.1186/s12889-015-1824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aneshensel CS, Ko MJ, Chodosh J, Wight RG. The urban neighborhood and cognitive functioning in late middle age. J Health Soc Behav. 2011;52(2):163–179. doi: 10.1177/0022146510393974. https://doi.org/10.1177/0022146510393974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.James BD. Doctoral dissertation. Ann Arbor: The Johns Hopkins University; 2009. Social engagement and cognitive decline in older adults: Pathways and neighborhood context. [Google Scholar]
- 19.U.S. Census. [Accessed November 23, 2016];Census Urban and Rural Classification and Urban Area Criteria. 2010 www.census.gov/geo/reference/ua/urban-rural-2010.html.
- 20.AARP Public Policy Institute. [Accessed November 23, 2016];Aging in Place: A State Survey of Livability Policies and Practices. http://assets.aarp.org/rgcenter/ppi/liv-com/ib190.pdf.
- 21.Wu YT, Prina AM, Brayne C. The association between community environment and cognitive function: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2015;50(3):351–362. doi: 10.1007/s00127-014-0945-6. https://doi.org/10.1007/s00127-014-0945-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reed BR, Mungas DM, Kramer JH, et al. Profiles of neuropsychological impairment in autopsy-defined Alzheimer’s disease and cerebrovascular disease. Brain. 2007;130(Pt 3):731–739. doi: 10.1093/brain/awl385. https://doi.org/10.1093/brain/awl385. [DOI] [PubMed] [Google Scholar]
- 23.Ewing R, Cervero R. Travel and the Built Environment: A Meta-Analysis. J Am Plann Assoc. 2010;76(3):265–294. https://doi.org/10.1080/01944361003766766. [Google Scholar]
- 24.Sterne JAC, Higgins J, Reeves BC on behalf of the development group for ACROBAT-NRSI. [Accessed October 2, 2016];A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI). Version 1.0.0. 2014 Sep 24; www.riskofbias.info.
- 25.Sterne J, Hernán N, Reeves B, et al. [Accessed October 2, 2016];The Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) assessment tool. 2016 https://sites.google.com/site/riskofbiastool/
- 26.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. https://doi.org/10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bollen KA, Bauldry S. Three Cs in measurement models: causal indicators, composite indicators, and covariates. Psychol Methods. 2011;16(3):265–284. doi: 10.1037/a0024448. https://doi.org/10.1037/a0024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Diez Roux AV. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. https://doi.org/10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 29.Spiegelman D. Evaluating Public Health Interventions: 4. The Nurses’ Health Study and Methods for Eliminating Bias Attributable to Measurement Error and Misclassification. Am J Public Health. 2016;106(9):1563–1566. doi: 10.2105/AJPH.2016.303377. https://doi.org/10.2105/AJPH.2016.303377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brownson RC, Hoehner CM, Day K, Forsyth A, Sallis JF. Measuring the built environment for physical activity: state of the science. Am J Prev Med. 2009;36(4 Suppl):S99–123. doi: 10.1016/j.amepre.2009.01.005. https://doi.org/10.1016/j.amepre.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gay JL, Smith J. Validity of a scale assessing the built environment for physical activity. Am J Health Behav. 2010;34(4):420–431. doi: 10.5993/ajhb.34.4.4. https://doi.org/10.5993/AJHB.34.4.4. [DOI] [PubMed] [Google Scholar]
- 32.Basta NE, Matthews FE, Chatfield MD, Brayne C MRC-CFAS. Community-level socio-economic status and cognitive and functional impairment in the older population. Eur J Public Health. 2008;18(1):48–54. doi: 10.1093/eurpub/ckm076. https://doi.org/10.1093/eurpub/ckm076. [DOI] [PubMed] [Google Scholar]
- 33.Boardman JD, Barnes LL, Wilson RS, Evans DA, Mendes de Leon CF. Social disorder, APOE-E4 genotype, and change in cognitive function among older adults living in Chicago. Soc Sci Med. 2012;74(10):1584–1590. doi: 10.1016/j.socscimed.2012.02.012. https://doi.org/10.1016/j.socscimed.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown SC, Mason CA, Spokane AR, Cruza-Guet MC, Lopez B, Szapocznik J. The relationship of neighborhood climate to perceived social support and mental health in older Hispanic immigrants in Miami, Florida. J Aging Health. 2009;21(3):431–459. doi: 10.1177/0898264308328976. https://doi.org/10.1177/0898264308328976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clarke PJ, Ailshire JA, House JS, et al. Cognitive function in the community setting: the neighbourhood as a source of ‘cognitive reserve’? J Epidemiol Community Health. 2012;66(8):730–736. doi: 10.1136/jech.2010.128116. https://doi.org/10.1136/jech.2010.128116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clarke PJ, Weuve J, Barnes L, Evans DA, Mendes de Leon CF. Cognitive decline and the neighborhood environment. Ann Epidemiol. 2015;25(11):849–854. doi: 10.1016/j.annepidem.2015.07.001. https://doi.org/10.1016/j.annepidem.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Deeg D, Fleur Thomese GC. Discrepancies between personal income and neighborhood status: effects on physical and mental health. Eur J Ageing. 2005;2(2):98–108. doi: 10.1007/s10433-005-0027-4. https://doi.org/10.1007/s10433-005-0027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Espino DV, Lichtenstein MJ, Palmer RF, Hazuda HP. Ethnic differences in Mini-Mental State Examination (MMSE) scores: Where you live makes a difference. J Am Geriatr Soc. 2001;49(5):538–548. doi: 10.1046/j.1532-5415.2001.49111.x. https://doi.org/10.1046/j.1532-5415.2001.49111.x. [DOI] [PubMed] [Google Scholar]
- 39.Glass TA, Bandeen-Roche K, McAtee M, Bolla K, Todd AC, Schwartz BS. Neighborhood psychosocial hazards and the association of cumulative lead dose with cognitive function in older adults. Am J Epidemiol. 2009;169(6):683–692. doi: 10.1093/aje/kwn390. https://doi.org/10.1093/aje/kwn390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kovalchik SA, Slaughter ME, Miles J, Friedman EM, Shih RA. Neighbourhood racial/ethnic composition and segregation and trajectories of cognitive decline among U.S. older adults. J Epidemiol Community Health. 2015;69(10):978–984. doi: 10.1136/jech-2015-205600. https://doi.org/10.1136/jech-2015-205600. [DOI] [PubMed] [Google Scholar]
- 41.Lang IA, Llewellyn DJ, Langa KM, Wallace RB, Huppert FA, Melzer D. Neighborhood deprivation, individual socioeconomic status, and cognitive function in older people: analyses from the English Longitudinal Study of Ageing. J Am Geriatr Soc. 2008;56(2):191–198. doi: 10.1111/j.1532-5415.2007.01557.x. https://doi.org/10.1111/j.1532-5415.2007.01557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee BK, Glass TA, James BD, Bandeen-Roche K, Schwartz BS. Neighborhood psychosocial environment, apolipoprotein E genotype, and cognitive function in older adults. Arch Gen Psychiatry. 2011;68(3):314–321. doi: 10.1001/archgenpsychiatry.2011.6. https://doi.org/10.1001/archgenpsychiatry.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martinez DM. Doctoral Dissertation. Ann Arbor: University of California Los Angeles; 2007. Racial disparities in cognitive performance over time among older adults: A multilevel analysis of neighborhood effects. [Google Scholar]
- 44.Meyer OL, Sisco SM, Harvey D, et al. Neighborhood Predictors of Cognitive Training Outcomes and Trajectories in ACTIVE. Res Aging. doi: 10.1177/0164027515618242. In press. Online December 13, 2015. https://doi.org/10.1177/0164027515618242. [DOI] [PMC free article] [PubMed]
- 45.Murayama H, Nishi M, Matsuo E, et al. Do bonding and bridging social capital affect self-rated health, depressive mood and cognitive decline in older Japanese? A prospective cohort study. Soc Sci Med. 2013;98:247–252. doi: 10.1016/j.socscimed.2013.09.026. https://doi.org/10.1016/j.socscimed.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 46.Rej S, Begley A, Gildengers A, Dew MA, Reynolds CF, Butters MA. Psychosocial Risk Factors for Cognitive Decline in Late-Life Depression: Findings from the MTLD-III Study. Can Geriatr J. 2015;18(2):43–50. doi: 10.5770/cgj.18.134. https://doi.org/10.5770/cgj.18.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sheffield KM, Peek MK. Neighborhood context and cognitive decline in older Mexican Americans: results from the Hispanic Established Populations for Epidemiologic Studies of the Elderly. Am J Epidemiol. 2009;169(9):1092–1101. doi: 10.1093/aje/kwp005. https://doi.org/10.1093/aje/kwp005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sisco SM, Marsiske M. Neighborhood Influences on Late Life Cognition in the ACTIVE Study. J Aging Res. 2012;2012:435826. doi: 10.1155/2012/435826. https://doi.org/10.1155/2012/435826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shih RA, Ghosh-Dastidar B, Margolis KL, et al. Neighborhood socioeconomic status and cognitive function in women. Am J Public Health. 2011;101(9):1721–1728. doi: 10.2105/AJPH.2011.300169. https://doi.org/10.2105/AJPH.2011.300169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wee LE, Yeo WX, Yang GR, et al. Individual and Area Level Socioeconomic Status and Its Association with Cognitive Function and Cognitive Impairment (Low MMSE) among Community-Dwelling Elderly in Singapore. Dement Geriatr Cogn Dis Extra. 2012;2(1):529–542. doi: 10.1159/000345036. https://doi.org/10.1159/000345036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Watts A, Ferdous F, Moore KD, Burns JM. Neighborhood Integration and Connectivity Predict Cognitive Performance and Decline. Gerontol Geriatr Med. 2015:1. doi: 10.1177/2333721415599141. https://doi.org/10.1177/2333721415599141. [DOI] [PMC free article] [PubMed]
- 52.Zeki Al Hazzouri A, Haan MN, Osypuk T, Abdou C, Hinton L, Aiello AE. Neighborhood socioeconomic context and cognitive decline among older Mexican Americans: results from the Sacramento Area Latino Study on Aging. Am J Epidemiol. 2011;174(4):423–431. doi: 10.1093/aje/kwr095. https://doi.org/10.1093/aje/kwr095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu YT, Prina AM, Jones AP, et al. Community environment, cognitive impairment and dementia in later life: results from the Cognitive Function and Ageing Study. Age Ageing. 2015;44(6):1005–1011. doi: 10.1093/ageing/afv137. https://doi.org/10.1093/ageing/afv137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Magaziner J, Cadigan DA. Community resources and mental health of older women living alone. J Aging Health. 1989;1(1):35–49. doi: 10.1177/089826438900100103. https://doi.org/10.1177/089826438900100103. [DOI] [PubMed] [Google Scholar]
- 55.Clarke P, George LK. The role of the built environment in the disablement process. Am J Public Health. 2005;95(11):1933–1939. doi: 10.2105/AJPH.2004.054494. https://doi.org/10.2105/AJPH.2004.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guralnik JM, Land KC, Blazer D, Fillenbaum GG, Branch LG. Educational status and active life expectancy among older blacks and whites. N Engl J Med. 1993;329(2):110–116. doi: 10.1056/NEJM199307083290208. https://doi.org/10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- 57.Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11(11):1006–1012. doi: 10.1016/S1474-4422(12)70191-6. https://doi.org/10.1016/S1474-4422(12)70191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Propper C, Jones K, Bolster A, Burgess S, Johnston R, Sarker R. Local neighbourhood and mental health: evidence from the UK. Soc Sci Med. 2005;61(10):2065–2083. doi: 10.1016/j.socscimed.2005.04.013. https://doi.org/10.1016/j.socscimed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 59.Poortinga W, Dunstan FD, Fone DL. Perceptions of the neighbourhood environment and self rated health: a multilevel analysis of the Caerphilly Health and Social Needs Study. BMC Public Health. 2007;7:285. doi: 10.1186/1471-2458-7-285. https://doi.org/10.1186/1471-2458-7-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jaffe DH, Eisenbach Z, Neumark YD, Manor O. Individual, household and neighborhood socioeconomic status and mortality: a study of absolute and relative deprivation. Soc Sci Med. 2005;60(5):989–997. doi: 10.1016/j.socscimed.2004.06.047. https://doi.org/10.1016/j.socscimed.2004.06.047. [DOI] [PubMed] [Google Scholar]
- 61.Menec VH, Shooshtari S, Nowicki S, Fournier S. Does the relationship between neighborhood socioeconomic status and health outcomes persist into very old age? A population-based study. J Aging Health. 2010;22(1):27–47. doi: 10.1177/0898264309349029. https://doi.org/10.1177/0898264309349029. [DOI] [PubMed] [Google Scholar]
- 62.de Jong Gierveld J, Keating N, Fast JE. Determinants of Loneliness among Older Adults in Canada. Can J Aging. 2015;34(2):125–136. doi: 10.1017/S0714980815000070. https://doi.org/10.1017/S0714980815000070. [DOI] [PubMed] [Google Scholar]
- 63.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2008;98(9 Suppl):S29–37. doi: 10.2105/ajph.98.supplement_1.s29. https://doi.org/10.2105/AJPH.98.Supplement_1.S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? Int J Epidemiol. 2003;32(3):357–366. doi: 10.1093/ije/dyg084. https://doi.org/10.1093/ije/dyg084. [DOI] [PubMed] [Google Scholar]
- 65.Cho G-H, Rodriguez DA. Neighborhood design, neighborhood location, and three types of walking: results from the Washington DC area. Environ Plann B Plann Des. 2015;42(3):526–540. https://doi.org/10.1068/b130222p. [Google Scholar]
- 66.Krueger KR, Wilson RS, Kamenetsky JM, Barnes LL, Bienias JL, Bennett DA. Social engagement and cognitive function in old age. Exp Aging Res. 2009;35(1):45–60. doi: 10.1080/03610730802545028. https://doi.org/10.1080/03610730802545028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sampson RJ, Sharkey P, Raudenbush SW. Durable effects of concentrated disadvantage on verbal ability among African-American children. Proc Natl Acad Sci U S A. 2008;105(3):845–852. doi: 10.1073/pnas.0710189104. https://doi.org/10.1073/pnas.0710189104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Richards JL, Chapple-McGruder T, Williams BL, Kramer MR. Does neighborhood deprivation modify the effect of preterm birth on children’s first grade academic performance? Soc Sci Med. 2015;132:122–131. doi: 10.1016/j.socscimed.2015.03.032. https://doi.org/10.1016/j.socscimed.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.McCulloch A, Joshi HE. Neighbourhood and family influences on the cognitive ability of children in the British National Child Development Study. Soc Sci Med. 2001;53(5):579–591. doi: 10.1016/s0277-9536(00)00362-2. https://doi.org/10.1016/S0277-9536(00)00362-2. [DOI] [PubMed] [Google Scholar]
- 70.Krishnadas R, McLean J, Batty GD, et al. Socioeconomic deprivation and cortical morphology: psychological, social, and biological determinants of ill health study. Psychosom Med. 2013;75(7):616–623. doi: 10.1097/PSY.0b013e3182a151a7. https://doi.org/10.1097/PSY.0b013e3182a151a7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.