Abstract
Background
Cadaver dissection for anatomy training provides an opportunity to understand the precise nature of human tissues with their clinical and structural relationships. This study assessed the effectiveness of this practical educational intervention for teaching applied facial anatomy on the knowledge and confidence of aesthetic physicians.
Methods and materials
A total of 168 aesthetic physicians underwent facial applied anatomy training for 2 days at The Academia, Singapore. The 2-day course encompassed detailed facial anatomy of neurovasculature, fat compartments, ligaments, and muscles followed by simulated practice of safer injection techniques. To enable quality interaction between the participants and the faculties, the delegates were divided into four groups. Academic impact of the program was evaluated by a pre-course and post-course multiple choice question (MCQ) test. Participants, also completed a paper-based feedback on their knowledge, skills, and confidence in performing nonsurgical facial aesthetic procedures. Different sets of MCQs were utilized for pre-course post-course test to avoid any recall bias.
Results
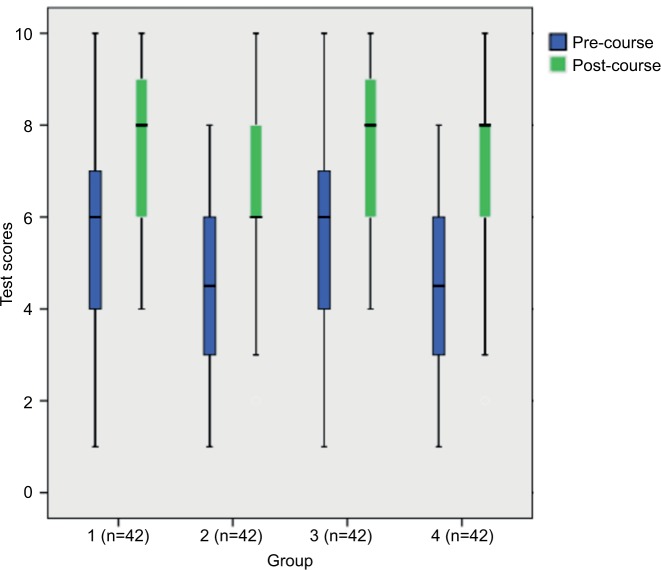
All 168 participants completed the test and were included in the analysis. Mean pre-course and post-course test scores were 4.8 (standard deviation [SD] 1.9) and 7.6 (SD 1.7), respectively (p<0.001 vs pre-course test). All the four groups showed improvement in their facial anatomy knowledge based on the comparison of pre-course and post-course test results (p<0.001). The average post-course test score in all the groups from baseline significantly improved. However, there was no statistical difference in pre-course and post-course test evaluation between the groups (p=0.32).
Conclusion
Our results showed that cadaver anatomy training improved applied facial anatomy knowledge for most of the aesthetic practitioners, which may enhance their confidence in performing nonsurgical facial aesthetic procedures.
Keywords: MCQ, facial anatomy, non-surgical, anatomy teaching, simulation, anatomy knowledge, pre-course test, post-course test
Introduction
Strong knowledge of anatomy is an essential component of a safe and effective procedural practice. Cadaver dissection has been considered the principle teaching method of anatomy for the last 400 years.1,2 It comprises understanding of the relationship between patients’ symptoms and pathology, appreciation of the three-dimensional perspectives of structures,1,3 identification of anatomical variations,4 and exposure to more realistic tactile features compared to technologically supported synthetic training models.5–7 However, in recent times, cadaver dissection-based teaching has significantly declined due to the adoption of integrated medical curricula worldwide, the significant cost and required time, and religious restrictions.8,9 The permanence of basic science knowledge learned in medical school has been a source of concern for as long as this knowledge has been included in the curriculum. More specifically, there is a common belief among physicians and medical educators that a significant percentage of the basic science knowledge attained in the preclinical years in medical school is lost during the final, predominantly clinical, years.10,11 Studies have shown that residents fail to recall a considerable proportion of apparent anatomical knowledge in the transition from their pre-clinical years to practice.12–14 Due to the effectiveness and safety of nonsurgical aesthetic procedures in reducing the signs of facial aging, increasing numbers of people are opting to undergo nonsurgical facial aesthetic procedures worldwide.15 Understanding facial anatomy further enhances the aesthetic practitioners’ knowledge of the aging process, to provide a better treatment plan for an optimal clinical outcome.16,17 Furthermore, intravascular complications associated with injectables have been shown to be mainly related to a lack of facial anatomy knowledge and awareness.18 The importance of facial anatomy knowledge has been discussed by many experts.19 A global consensus on avoidance of aesthetic procedure-related complications has also echoed the importance of detailed facial anatomy knowledge to prevent devastating complications.20 Increased usage of botulinum toxin and dermal fillers in facial aesthetic procedures has brought with it a renewed interest in elaborate facial anatomy, previously a relatively low priority in medical school. For many aesthetic practitioners whose last experience with gross anatomy was during their early preclinical years, refreshing this knowledge is necessary for safe and optimal clinical outcome.21 The aim of this research was to evaluate the impact of cadaver dissection on facial anatomy learning among experienced aesthetic practitioners. The hypothesis of this study was that enhancing facial anatomy knowledge, specifically, the vasculature, fat compartments, ligaments, and muscles, through a cadaveric dissection of the face would increase anatomical knowledge needed to perform safe and effective nonsurgical facial aesthetic procedures.
Methods and materials
Participants
The study was approved by the Ethics Committee of the Faculty of Medical Science, Anglia Ruskin University, Chelmsford, UK. The study cohort comprised 168 aesthetic physicians who attended a 2-day applied facial anatomy course with fresh cadaver dissection at The Academia, Singapore. Participation in the workshop was by invitation, and the delegates were from China, India, Indonesia, Malaysia, Taiwan, Thailand, Turkey, and Singapore. Participants’ mean experience of practicing aesthetic medicine since primary medical qualification was 7.6 years (standard deviation [SD] 3.8); 36% of participants were men, and 64% were women.
Course structure
An instructional curriculum was developed in consultation with dermatologists and aesthetic plastic surgeons globally recognized for their interest in non-surgical facial aesthetics. The course was delivered over 2 days. Day 1 was focused on cadaveric dissection and day 2 was focused on live demonstration of safer injection techniques linked to anatomical correlation, with active audience participation. Each session had a logical sequence of teaching activities, which included lectures on the relevant anatomical areas with an emphasis on critical neurovasculature, fat compartments, ligaments and muscles of the upper, mid and lower third of the face. This was followed by task-driven, facilitator-led small group functional anatomy dissection and simulated practice of safer injection techniques with a variety of dermal fillers delineating the depth and location of the injection (Table 1).
Table 1.
Course structure
| Day 1 | Day 2 |
|---|---|
| Pre-course MCQ test Review of facial anatomy (lecture) Cadaveric dissection: Divided into lower, middle, and upper thirds of the face with special attention to: • Fat compartments • Neuro-vasculature • Ligaments • Muscles |
Review of facial anatomy (lecture) Live demonstration • Surface marking • Injection technique (with active audience participation) |
| Simulated practice of safer injection techniques with a variety of dermal fillers, delineating the depth and location of injection | Post-course MCQ test Feedback |
Abbreviation: MCQ, multiple choice question.
Course delivery
Participants (n=168) were organized into four groups, each headed by a lead faculty. Each group was further subdivided into smaller units of 7 with a table demonstrator to encourage discussion, active interaction, feedback, and reflection. This two-tier strategy was incorporated to maximize the tutor intervention as it keeps the group tasked focused when members in the group are new to one another and complex task needs to be achieved.22
Assessment materials
Measurement of knowledge retention has been debated in the literature. There is no single agreed measure of knowledge retention, but rather several different methods, which may not always yield equivalent results. Open-ended (recall) and true-false (recognition) questions are most commonly used in educational contexts to measure retention. However, multiple choice questions (MCQs) enable the testing of both recall and recognition.23 Hence, a formal 10-minute test was administered before the course (pre-course) and the day following the dissection session (post-course). The test comprised 10 MCQs with four stem answers focused on facial anatomy (Figure S1). These questions were randomly selected from a list of 40 questions prepared and validated by a panel of five dermatologists and aesthetic plastic surgeons, each with >20 years of clinical and academic experience. Participants were given different sets of MCQs during pre- and post-course test to avoid any recall bias.
Participants were also asked to complete a paper-based feedback on their knowledge, skills, and confidence in performing nonsurgical facial aesthetic procedures after the course using a 5-point Likert scale (0= strongly disagree, 5= strongly agree).
Statistical analysis
Descriptive statistics were computed including frequency, mean, and SD. Primary outcome measures were the pre-course and post-course test scores. The data were normally distributed at baseline but skewed at the subsequent time points. The analysis compared scores from consecutive time points to determine whether there was an improvement. The measures of the central tendency for assessment score were presented as median with interquartile ranges.
The Wilcoxon signed-rank test was utilized as it compares two related samples or repeated data (in this case, the pre-course and post-course test scores). All p-values were two-tailed, and due to the multiple testing of the items, statistical significance was set at p≤0.001.
IBM SPSS statistics for Windows, Version 20.0 (IBM Corporation, Armonk, NY, USA) was used to analyze quantitative data.
Results
Mean pre-course and post-course test scores were 4.8 (SD 1.9) and 7.6 (SD 1.7), respectively. All four groups showed improvement in their facial anatomy knowledge (p<0.001) based on the comparison of pre-course and post-course test results (Figure 1). The average post-course test score in each of the groups was higher than the pre-course test score. There was no significant difference (p=0.32) in pre-course and post-course test evaluation scores between the groups (Table 2).
Figure 1.
Box plot showing pre-course and post-course test scores in each group.
Table 2.
Wilcoxon signed rank test
| Post-course test – pre-course test | Difference group | Pre-course test group | Post-course test group | |
|---|---|---|---|---|
| Z | −9.233a | −0.995b | −9.312a | −11.209a |
| Asymptotic significance (two-tailed) | 0.000 | 0.320 | 0.000 | 0.000 |
Notes:
Based on negative ranks;
based on positive ranks.
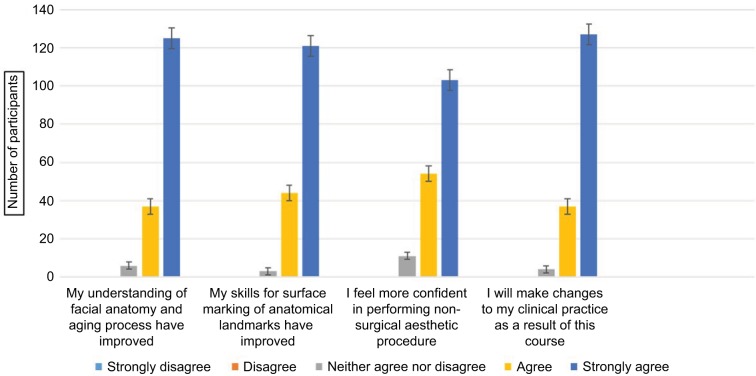
Participant feedback
All 168 students in the dissection course completed an anonymous feedback. Participants’ response revealed that the course strengthened the ability of physicians to carry out nonsurgical aesthetic procedure independently in a less stressful environment, by increasing their understanding of facial anatomy (n=162; 96.42%), skills for surface making (n=165; 98.21%), and confidence (n=157; 93.4%). All physician attendees rated the program as extremely useful and that they would apply the learnings into their clinical practices (n=164; 97%) (Figure 2).
Figure 2.
Participants’ feedback.
Examples of the participants’ comments included: “invaluable experience to learn facial anatomy after medical school” and “best and much-needed refresher training for every physician.”
Additional comments revealed that some participants found the course to be very intensive, with a lack of sufficient breaks (n=14; 8%), while others expressed that it would have been useful to have additional time for more detailed dissection (n=19; 11%).
Discussion
Overall, this program objectively demonstrated that the cadaver dissection course could significantly improve the facial anatomical knowledge of aesthetic physicians. Since multiple educational modalities were incorporated in a sequential fashion, it is not possible to discern which intervention had the most significant effect. The goal was to impart facial anatomy knowledge that would have an expected impact on injection competency and safety, thereby minimizing unintended complications.
Our findings here support the intuitive belief that cadaver dissection is a valuable educational tool for the understanding of facial anatomy and may promote safe patient outcomes after nonsurgical aesthetic treatment.
Cadaver dissection has been an essential part of medical education for centuries and has been consistently utilized to teach anatomy to medical students and practitioners. This method has been shown to establish practical insights within the framework of human anatomy teaching.24 Moreover, dissection familiarizes students not only with the anatomical details but also with anatomical variations, and an appreciation for fully exposed structures that could potentially be damaged during invasive treatment.2 Conventional teaching, including lectures and practical gross anatomy, allows the practitioners to express, assess and reflects on their learning, and has been found to be objectively achievable, unambiguous, and clinically relevant.25 Most physicians who have undergone this training perceived the experience of cadaver dissections as a way of enhancing reverence toward the human body.1,26,27
Limitations
This research has several limitations. First, we conducted the study without any control group at a single anatomy center; however, in this quasi experimental intervention study, we incorporated a pre-course test; post-course test design without non-equivalent control group as pre-course test itself can act as a control group.28,29 Moreover, participants were invited to attend the workshop; there was an expectation of gaining additional knowledge and skill, hence allocating a proportion of them into a control would have been a disadvantage to some. Second, we did not assess the students’ self-study or motivation, which may have impacted their baseline scores. Third, we did not record repeated measure effects or evaluate their long-term retention of this acquired knowledge. Fourth, although the participants performed simulated procedural skills, they were not assessed formally. However, we ensured that the procedures were thoroughly demonstrated, deconstructed and subject to feedback given by the group demonstrators.
Conclusion
Procedure-oriented and replicable cadaver dissection-based anatomy training improves the knowledge, understanding, and confidence of aesthetic physicians, thereby theoretically enhancing patient safety. It can be concluded that facial anatomy training should remain a key component of postgraduate and continued medical education for aesthetic physicians, with cadaver dissection as its core teaching method.
Supplementary material
Example of multiple choice questions.
Abbreviation: Q, question.
Acknowledgments
We would like to thank Dr Greg Goodman, Associate Professor, Monash University, Melbourne, VIC, Australia, and Dr Arthur Swift, Clinical Lecturer, McGill University, Montréal, QC, Canada, for comments that greatly improved the manuscript.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ. 2010;3(2):83–93. doi: 10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- 2.Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg Engl. 2007;89(2):104–107. doi: 10.1308/003588407X168244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Azer SA, Eizenberg N. Do we need dissection in an integrated problem-based learning medical course? Perceptions of first- and second-year students. Surg Radiol Anat. 2007;29(2):173–180. doi: 10.1007/s00276-007-0180-x. [DOI] [PubMed] [Google Scholar]
- 4.Korf HW, Wicht H, Snipes RL, et al. The dissection course - necessary and indispensable for teaching anatomy to medical students. Ann Anat. 2008;190(1):16–22. doi: 10.1016/j.aanat.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Gunderman RB, Wilson PK. Viewpoint : exploring the human interior : the roles of cadaver dissection and radiologic imaging in teaching anatomy. Acad Med. 2005;80(8):745–749. doi: 10.1097/00001888-200508000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Rizzolo LJ, Stewart WB, O’Brien M, et al. Design principles for developing an efficient clinical anatomy course. Med Teach. 2006;28(2):142–151. doi: 10.1080/01421590500343065. [DOI] [PubMed] [Google Scholar]
- 7.Ellis MS, Nelson JT, Kartchner JZ, Yousef KA, Adamas-rappaport WJ, Amini R. Cadaver-based abscess model for medical training. Adv Med Educ Pract. 2017;8:85–88. doi: 10.2147/AMEP.S124648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lockwood AM, Roberts AM. The anatomy demonstrator of the future: an examination of the role of the medically-qualified anatomy demonstrator in the context of tomorrow ’ s doctors and modernizing medical careers. Clin Anat. 2007;459(October 2006):455–459. doi: 10.1002/ca.20427. [DOI] [PubMed] [Google Scholar]
- 9.Drake RL, Mcbride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;259(December):253–259. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy WB, Kelley PR, Jr, Saffran M. Use of NBME examinations to assess retention of basic science knowledge. J Med Educ. 1981;56(3):167–173. doi: 10.1097/00001888-198103000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Norman G. The essential role of basic science in medical education: the perspective from psychology. Clin Investig Med. 2000;23(1):47–51. [PubMed] [Google Scholar]
- 12.Glenn C, Hamilton FN. Clinical anatomy for medical student. J Emerg Med. 1997 Mar;3:71–74. [Google Scholar]
- 13.Custers EJ, Ten Cate OT. Very long-term retention of basic science knowledge in doctors after graduation. Med Educ. 2011;45(4):422–430. doi: 10.1111/j.1365-2923.2010.03889.x. [DOI] [PubMed] [Google Scholar]
- 14.Custers EJ. Long-term retention of basic science knowledge: a review study. Adv Heal Sci Educ. 2010;15(1):109–128. doi: 10.1007/s10459-008-9101-y. [DOI] [PubMed] [Google Scholar]
- 15.De Aquino MS, Haddad A, Ferreira LM. Assessment of quality of life in patients who underwent minimally invasive cosmetic procedures. Aesthetic Plast Surg. 2013;37(3):497–503. doi: 10.1007/s00266-012-9992-0. [DOI] [PubMed] [Google Scholar]
- 16.Oh S-R, Priel A, Korn BS, Kikkawa DO. Applied anatomy for the aesthetic surgeon. Curr Opin Ophthalmol. 2010;21(5):404–410. doi: 10.1097/ICU.0b013e32833ce990. [DOI] [PubMed] [Google Scholar]
- 17.Shaw RB, Katzel EB, Koltz PF, et al. Aging of the facial skeleton: aesthetic implications and rejuvenation strategies. Plast Reconstr Surg. 2011;127(1):374–383. doi: 10.1097/PRS.0b013e3181f95b2d. [DOI] [PubMed] [Google Scholar]
- 18.Emer J, Levy L. Complications of minimally invasive cosmetic procedures: prevention and management. J Cutan Aesthet Surg. 2012;5(2):121. doi: 10.4103/0974-2077.99451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gladstone HB, Cohen JL. Adverse effects when injecting facial fillers. Semin Cutan Med Surg. 2007;26(1):34–39. doi: 10.1016/j.sder.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Signorini M, Liew S, Sundaram H, et al. Global aesthetics consensus: avoidance and management of complications from hyaluronic acid fillers-evidence- and opinion-based review and consensus recommendations. Plast Reconstr Surg. 2016;137(6):961e–971e. doi: 10.1097/PRS.0000000000002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lempp HK. Perceptions of dissection by students in one medical school: beyond learning about anatomy. A qualitative study. Med Educ. 2005;39(3):318–325. doi: 10.1111/j.1365-2929.2005.02095.x. [DOI] [PubMed] [Google Scholar]
- 22.McCrorie P. Teaching and leading small groups. In: Swanwick T, editor. Understanding Medical Education: Evidence, Theory and Practice. Oxford: John Wiley & Sons, Ltd; 2013. [Google Scholar]
- 23.Arzi HJ, Ben-Zvi R, Ganiel U. Forgetting versus savings: the many facets of long-term retentione. Sci Educ. 1986;70(2):171–188. [Google Scholar]
- 24.Özcan S, Huri E, Tatar İ, et al. Impact of cadaveric surgical anatomy training on urology residents knowledge: a preliminary study. Turkish J Urol. 2015;41(2):83–87. doi: 10.5152/tud.2015.87422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dissabandara LO, Nirthanan SN, Khoo TK, Tedman R. Role of cadaveric dissections in modern medical curricula: a study on student perceptions. Anat Cell Biol. 2015;48(3):205–212. doi: 10.5115/acb.2015.48.3.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell EL, Sevdalis N, Arora S, et al. From the society for clinical vascular surgery a fresh cadaver laboratory to conceptualize troublesome anatomic relationships in vascular surgery. J Vasc Surg. 2012;55(4):1187–1195. doi: 10.1016/j.jvs.2011.09.098. [DOI] [PubMed] [Google Scholar]
- 27.Robinson AG, Metten S, Guiton G, Berek J. Using fresh tissue dissection to teach human anatomy in the clinical years. Acad Med. 2004;79(7):711–716. doi: 10.1097/00001888-200407000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Regehr G. In: International Handbook of Research in Medical Education. Norman GR, Van der Vleuten CPM, Newble DI, et al., editors. Dordrecht: Kluwer Academic Publishers; 2002. [Google Scholar]
- 29.Eliopoulos GM, Harris AD, Bradham DD, et al. The use and interpretation of quasi-experimental studies in infectious diseases. Clin Infect Dis. 2004;38(11):1586–1591. doi: 10.1086/420936. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Example of multiple choice questions.
Abbreviation: Q, question.