Abstract
Introduction
The prognostic impact of the number of examined lymph nodes (ELNs) in different histological subtypes of cervical cancer remains unclear. We aimed to assess the impact of the number of ELNs in stage IA2–IIA cervical cancer with different histological subtypes.
Methods
Data of patients with stage IA2–IIA squamous cell carcinoma (SCC) and adenocarcinoma (AC) of the uterine cervix between 1988 and 2013 were retrieved from the Surveillance, Epidemiology, and End Results program. Univariate and multivariate Cox regression analyses were performed to analyze the effect of number of ELNs on cause-specific survival (CSS) and overall survival (OS).
Results
The final data set identified 11,830 patients including 7,920 (66.9%) women with SCC and 3,910 (33.1%) with AC. The median number of ELNs was 19. The multivariate analysis indicated that the number of ELNs was an independent prognostic factor influencing CSS and OS, both as a continuous or a categorical variable. Patients with a higher number of ELNs had better survival outcomes. In SCC subtype, the number of ELNs was also the independent prognostic factor of CSS and OS in node-positive patients, but not in patients with node-negative disease. In AC patients, ELN count was not an independent predictor of CSS and OS regardless of lymph node status.
Conclusion
The number of ELNs is an independent prognostic factor in patients with stage IA2–IIB cervical cancer. A higher number of ELNs is associated with better survival outcomes, especially in the node-positive SCC subtype.
Keywords: cervical cancer, early stage, SEER, histological subtype, nodal positive, prognosis
Introduction
Cervical cancer is one of the most common malignancies in women and has become an important disease that threatens women’s health.1,2 Radical hysterectomy is the main local treatment of early stage cervical cancer, and pelvic lymphadenectomy is an important surgical procedure during radical hysterectomy. Several studies have found that the number of examined lymph nodes (ELNs) could predict precise lymph node staging in lung, gastric, rectal, and ovarian cancer, and patients with a higher number of ELNs show better survival.3–6 However, for patients with cervical cancer, extensive lymphadenectomy may lead to more postoperative complications and damage the patient’s immune system.7,8
The status of lymph node is not considered in the current International Federation of Gynecology and Obstetrics (FIGO) staging system. However, more studies have found that a higher number of positive lymph nodes (PLNs) was associated with worse prognosis.9,10 Theoretically, a higher number of ELNs could accurately assess lymph node status, which may reduce the risk of occult lymph node metastases. Previous studies have found that a higher number of ELNs was associated with better survival in patients with node-positive disease.11,12 However, several studies have shown that extensive lymphadenectomy did not improve survival.13–15 In addition, a population-based study found that a higher number of ELNs was associated with better survival outcomes in patients with node-negative cervical cancer.16 Therefore, the clinical value of ELN count in cervical cancer remains controversial.
Squamous cell carcinoma (SCC) and adenocarcinoma (AC) are the most common histological subtypes of cervical cancer, which show differences in epidemiology, etiology, molecular characterization, and prognosis.17–19 To the best of our knowledge, there are no studies investigating the prognostic impact of the number of ELNs in different histological subtypes of cervical cancer. In this study, we aimed to investigate the prognostic value of the number of ELNs in cervical cancer using the Surveillance, Epidemiology, and End Results (SEER) database and further analyzed whether the results were affected by histological subtypes.
Materials and methods
Patients
We included patients diagnosed with FIGO stage IA2–IIA SCC and AC of the uterine cervix after hysterectomy and lymphadenectomy between 1988 and 2013 based on the SEER program.20 Patients with unknown ELN count and PLN count were excluded. We obtained the permission to access the SEER research data files with the reference number 14239-Nov2015. The Clinical Research Ethics Committee of the First Affiliated Hospital of Xiamen University approved this study. This study did not include any interactions with human subjects or use personally identifiable information, therefore, the ethics committee did not require that written informed consent be obtained.
Demographic and clinicopathological factors
The demographic and clinicopathological factors including age, year of diagnosis, ethnicity, FIGO stage, grade, histological subtypes, number of PLNs and ELNs, and radiotherapy were collected from the SEER database. The FIGO stage IA2–IIA category included stages IA2, IB not otherwise specified (NOS), IB1, IB2, and IIA in the SEER database. The number of PLNs was classified as 0, 1, 2, 3, and >4. The number of ELNs was classified according to previous studies as follows: 1–10, 11–20, 21–30, and >30.13,16 The primary endpoints of this study were cause-specific survival (CSS) and overall survival (OS).
Statistical analysis
All statistical analyses were completed using the SPSS package (version 21.0; IBM Corporation, Armonk, NY, USA). The Pearson’s χ2 test was used to compare the frequency distributions between categorical variables. Analysis of variance was used to compare the continuous variables in patients. Survival rates were determined by using Kaplan–Meier method and log-rank test. Univariate and multivariate Cox proportional hazard analyses were performed to identify the prognostic factors of CSS and OS. The impact of ELNs in the multivariate Cox proportional hazard model was evaluated by using continuous variables or categorical variables in two models. All the prognostic variables that were found to be significant in the univariate analysis were included in the multivariate analysis. A p-value of <0.05 was considered significant in all the analyses.
Results
The demographic and clinicopathological characteristics are summarized in Table 1. A total of 11,830 patients were included in this study, and 8,825 (74.6%) patients were diagnosed after 2000. The median age was 43 years (range, 9–90 years). Among them, 66.9% (7,920) and 33.1% (3,910) of patients were diagnosed with SCC and AC, respectively. Regarding the FIGO stage, 1,573 (13.3%), 9,528 (80.5%), and 729 (6.2%) patients were in stage IA2, IB, and IIA, respectively.
Table 1.
Patients’ demographic and clinicopathological characteristics
| Characteristic | n | 1–10 ELNs (%) | 11–20 ELNs (%) | 21–30 ELNs (%) | >31 ELNs (%) | p-value |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| Median ± SD | 43.0±12.2 | 44.0±13.1 | 43.0±12.3 | 43.0±11.7 | 42.0±11.0 | <0.001 |
| Year of diagnosis | ||||||
| 1988–1999 | 3,005 | 484 (20.4) | 1,045 (23.7) | 818 (27.0) | 658 (32.8) | <0.001 |
| 2000–2013 | 8,825 | 1,890 (79.6) | 3,373 (76.3) | 2,216 (73.0) | 1,346 (67.2) | |
| Ethnicity | ||||||
| White | 9,417 | 1,823 (76.8) | 3,530 (79.9) | 2,445 (80.6) | 1,619 (80.8) | <0.001 |
| Black | 1,030 | 286 (12.0) | 383 (8.7) | 227 (7.5) | 134 (6.7) | |
| Other | 1,302 | 250 (10.5) | 472 (10.7) | 337 (11.1) | 243 (12.1) | |
| Unknown | 81 | 15 (0.6) | 33 (0.7) | 25 (0.8) | 8 (0.4) | |
| Grade | ||||||
| G1 | 1,542 | 298 (12.6) | 582 (13.2) | 405 (13.3) | 257 (12.8) | 0.435 |
| G2 | 4,532 | 887 (37.4) | 1,716 (38.8) | 1,157 (38.1) | 772 (38.5) | |
| G3–4 | 4,005 | 806 (34.0) | 1,472 (33.3) | 1,020 (33.6) | 707 (35.3) | |
| Unknown | 1,751 | 383 (16.1) | 648 (14.7) | 452 (14.9) | 268 (13.4) | |
| FIGO stage | ||||||
| IA2 | 1,573 | 348 (14.7) | 653 (14.8) | 372 (12.3) | 200 (10.0) | <0.001 |
| IB NOS | 4,746 | 883 (37.2) | 1,685 (38.1) | 1,241 (40.9) | 937 (46.8) | |
| IB1 | 4,015 | 769 (32.4) | 1,571 (35.6) | 1,057 (34.8) | 618 (30.8) | |
| IB2 | 767 | 187 (7.9) | 257 (5.8) | 185 (6.1) | 138 (6.9) | |
| IIA | 729 | 187 (7.9) | 252 (5.7) | 179 (5.9) | 111 (5.5) | |
| Histological type | ||||||
| SCC | 7,920 | 1,557 (65.5) | 2,952 (66.8) | 2,030 (66.9) | 1,361 (67.9) | 0.760 |
| AC | 3,910 | 797 (33.5) | 1466 (33.2) | 1004 (33.1) | 643 (32.1) | |
| Radiotherapy | ||||||
| Yes | 8,205 | 1,522 (64.1) | 3,110 (70.4) | 2,161 (71.2) | 1,412 (70.5) | <0.001 |
| No | 3,625 | 852 (35.9) | 1308 (29.6) | 873 (28.8) | 592 (29.5) | |
| Marital status | ||||||
| Unmarried | 5,065 | 1,015 (42.8) | 1,909 (43.2) | 1,332 (43.9) | 809 (40.4) | 0.001 |
| Married | 6,326 | 1,264 (53.2) | 2,316 (52.4) | 1,604 (52.9) | 1,142 (57.0) | |
| Unknown | 439 | 95 (4.0) | 193 (4.4) | 98 (3.2) | 53 (2.6) | |
| Number of PLNs (n) | ||||||
| 0 | 10,018 | 2,021 (85.1) | 3,772 (85.4) | 2,558 (84.3) | 1,667 (83.2) | <0.001 |
| 1 | 853 | 175 (7.4) | 307 (6.9) | 230 (7.6) | 141 (7.0) | |
| 2 | 442 | 106 (4.5) | 159 (3.6) | 108 (3.6) | 69 (3.4) | |
| 3 | 214 | 31 (1.3) | 88 (2.0) | 53 (1.7) | 42 (2.1) | |
| >4 | 303 | 41 (1.7) | 92 (2.1) | 85 (2.8) | 85 (4.2) |
Abbreviations: AC, adenocarcinoma; ELNs, examined lymph nodes; FIGO, International Federation of Gynecology and Obstetrics; G1, well differentiated; G2, moderately differentiated; G3, poorly differentiated; G4, undifferentiated; NOS, not otherwise specified; PLNs, positive lymph nodes; SCC, squamous cell carcinoma; SD, standard deviation.
The median number of ELNs was 19. A total of 2,374 (20.1%), 4,418 (37.3%), 3,034 (25.6%), and 2,004 (16.9%) patients were categorized as having 1–10, 11–20, 21–30, and >30 ELNs, respectively. A total of 1,812 (15.3%) patients were with node-positive disease, and the median number of PLNs was two (range, 1–43) in patients with node-positive disease.
Patients who were younger, diagnosed after 2000, white ethnicity, IB NOS stage, received radiotherapy, and married had a higher number of ELNs. The probability of a higher number of PLNs was higher in patients with more ELNs. The clinicopathological data among the four groups were not significantly different for histological subtypes and grade (Table 1).
The median time of follow-up was 86 months (range, 1–311 months). The 5- and 10-year CSS were 91.6% and 89.1%, respectively, and the 5- and 10-year OS were 89.3% and 83.9%, respectively.
The univariate analysis showed that ELN as a continuous variable or as a categorical variable was the significant prognostic factor in CSS and OS (Table 2). The results of multivariate analysis showed that ELN was an independent prognostic factor for both CSS and OS as a continuous or a categorical variable (Table 3). Patients with a higher number of ELNs had a better survival. In the subgroup analysis of patients with node-positive disease, the number of ELNs was also an independent prognostic factor for survival. However, the number of ELNs was not associated with survival outcomes in node-negative patients (Table 3). Age, year of diagnosis, ethnicity, FIGO stage, grade, histological subtypes, number of PLNs, and radiotherapy were also independent prognostic factors for survival in the multivariate analysis.
Table 2.
Univariate analysis on prognostic factors of survival
| Characteristics | CSS
|
OS
|
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Age (years) (continuous variable) | 1.013 | 1.008–1.018 | <0.001 | 1.038 | 1.034–1.042 | <0.001 |
| Year of diagnosis | ||||||
| 1988–1999 | 1 | 1 | ||||
| 2000–2013 | 0.863 | 0.759–0.982 | 0.025 | 0.919 | 0.828–1.020 | 0.113 |
| Ethnicity | ||||||
| White | 1 | 1 | ||||
| Black | 1.564 | 1.304–1.876 | <0.001 | 1.463 | 1.266–1.690 | <0.001 |
| Other | 1.232 | 1.026–1.478 | 0.025 | 1.091 | 0.941–1.264 | 0.251 |
| Grade | ||||||
| G1 | 1 | 1 | ||||
| G2 | 2.514 | 1.865–3.389 | <0.001 | 2.145 | 1.735–2.652 | <0.001 |
| G3–4 | 4.657 | 3.478–6.234 | <0.001 | 3.366 | 2.733–4.146 | <0.001 |
| FIGO stage | ||||||
| IA2 | 1 | 1 | ||||
| IB NOS | 4.378 | 3.164–6.057 | <0.001 | 2.389 | 1.976–2.888 | <0.001 |
| IB1 | 2.878 | 2.037–4.067 | <0.001 | 1.883 | 1.518–2.336 | <0.001 |
| IB2 | 10.481 | 7.291–15.067 | <0.001 | 5.339 | 4.173–6.831 | <0.001 |
| IIA | 11.678 | 8.230–16.572 | <0.001 | 6.062 | 4.866–7.551 | <0.001 |
| Histological type | ||||||
| SCC | 1 | 1 | ||||
| AC | 0.922 | 0.809–1.051 | 0.223 | 0.831 | 0.748–0.924 | 0.001 |
| Radiotherapy | ||||||
| No | 1 | 1 | ||||
| Yes | 3.690 | 3.267–4.168 | <0.001 | 2.641 | 2.404–2.902 | <0.001 |
| Marital status | ||||||
| Unmarried | 1 | 1 | ||||
| Married | 0.792 | 0.702–0.895 | <0.001 | 0.666 | 0.606–0.732 | <0.001 |
| Number of PLNs (n) | ||||||
| 0 | 1 | 1 | ||||
| 1 | 3.335 | 2.804–3.966 | <0.001 | 2.281 | 1.962–2.650 | <0.001 |
| 2 | 3.887 | 3.133–4.822 | <0.001 | 2.783 | 2.309–3.355 | <0.001 |
| 3 | 5.361 | 4.146–6.933 | <0.001 | 3.439 | 2.720–4.349 | <0.001 |
| >4 | 7.071 | 5.770–8.665 | <0.001 | 4.775 | 3.984–5.723 | <0.001 |
| Number of PLNs (continuous variable) | 1.139 | 1.126–1.153 | <0.001 | 1.132 | 1.119–1.145 | <0.001 |
| Number of ELNs (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.785 | 0.670–0.920 | 0.003 | 0.823 | 0.726–0.932 | 0.002 |
| 21–30 | 0.756 | 0.636–0.899 | 0.002 | 0.774 | 0.676–0.887 | <0.001 |
| >30 | 0.793 | 0.656–0.958 | 0.016 | 0.746 | 0.641–0.867 | <0.001 |
| Number of ELNs (continuous variable) | 0.993 | 0.988–0.999 | 0.012 | 0.992 | 0.988–0.996 | <0.001 |
Abbreviations: AC, adenocarcinoma; CI, confidence interval; CSS, cause-specific survival; ELNs, examined lymph nodes; FIGO, International Federation of Gynecology and Obstetrics; G1, well differentiated; G2, moderately differentiated; G3, poorly differentiated; G4, undifferentiated; HR, hazard ratio; NOS, not otherwise specified; PLNs, positive lymph nodes; SCC, squamous cell carcinoma; OS, overall survival.
Table 3.
Multivariate analyses of impact of examined lymph node count on survival according to different lymph node status
| Number of ELNs | CSS
|
OS
|
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Entire group (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.848 | 0.723–0.996 | 0.044 | 0.885 | 0.781–1.003 | 0.056 |
| 21–30 | 0.777 | 0.652–0.926 | 0.005 | 0.816 | 0.711–0.936 | 0.004 |
| >30 | 0.758 | 0.625–0.919 | 0.005 | 0.77 | 0.661–0.898 | 0.001 |
| Number of ELNs (continuous variable) | 0.991 | 0.986–0.997 | 0.001 | 0.992 | 0.988–0.996 | <0.001 |
| Node-negative (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.968 | 0.785–1.193 | 0.759 | 0.93 | 0.800–1.081 | 0.343 |
| 21–30 | 0.914 | 0.725–1.151 | 0.442 | 0.86 | 0.729–1.015 | 0.074 |
| >30 | 0.975 | 0.759–1.252 | 0.841 | 0.875 | 0.727–1.052 | 0.155 |
| Number of ELNs (continuous variable) | 0.999 | 0.992–1.005 | 0.664 | 0.996 | 0.991–1.001 | 0.127 |
| Node-positive (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.711 | 0.553–0.913 | 0.008 | 0.826 | 0.654–1.042 | 0.107 |
| 21–30 | 0.536 | 0.486–0.833 | 0.001 | 0.763 | 0.595–0.979 | 0.033 |
| >30 | 0.525 | 0.387–0.712 | <0.001 | 0.593 | 0.448–0.785 | <0.001 |
| Number of ELNs (continuous variable) | 0.981 | 0.973–0.990 | <0.001 | 0.985 | 0.978–0.992 | <0.001 |
| SCC subtype (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.846 | 0.699–1.027 | 0.086 | 0.86 | 0.742–0.996 | 0.044 |
| 21–30 | 0.785 | 0.638–0.967 | 0.023 | 0.828 | 0.706–0.971 | 0.02 |
| >30 | 0.685 | 0.541–0.867 | 0.002 | 0.727 | 0.607–0.872 | 0.001 |
| Number of ELNs (continuous variable) | 0.992 | 0.987–0.996 | 0.001 | 0.99 | 0.984–0.996 | 0.001 |
| Node-negative SCC (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 1.042 | 0.809–1.341 | 0.751 | 0.923 | 0.774–1.101 | 0.373 |
| 21–30 | 0.951 | 0.719–1.258 | 0.725 | 0.868 | 0.715–1.052 | 0.149 |
| >30 | 0.962 | 0.709–1.304 | 0.802 | 0.854 | 0.689–1.059 | 0.151 |
| Number of ELNs (continuous variable) | 0.999 | 0.991–1.007 | 0.827 | 0.996 | 0.991–1.002 | 0.211 |
| Node-positive SCC (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.623 | 0.464–0.838 | 0.002 | 0.739 | 0.563–0.971 | 0.030 |
| 21–30 | 0.600 | 0.439–0.820 | 0.001 | 0.735 | 0.553–0.978 | 0.034 |
| >30 | 0.415 | 0.285–0.605 | <0.001 | 0.493 | 0.351–0.693 | <0.001 |
| Number of ELNs (continuous variable) | 0.976 | 0.966–0.987 | <0.001 | 0.981 | 0.972–0.989 | <0.001 |
| AC subtype (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.835 | 0.621–1.122 | 0.232 | 0.956 | 0.750–1.218 | 0.715 |
| 21–30 | 0.774 | 0.559–1.073 | 0.125 | 0.796 | 0.606–1.046 | 0.102 |
| >30 | 0.949 | 0.676–1.334 | 0.765 | 0.92 | 0.688–1.231 | 0.577 |
| Number of ELNs (continuous variable) | 0.996 | 0.987–1.005 | 0.373 | 0.996 | 0.988–1.003 | 0.260 |
| Node-negative AC (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.844 | 0.578–1.233 | 0.382 | 1 | 0.748–1.336 | 1.000 |
| 21–30 | 0.843 | 0.561–1.268 | 0.412 | 0.841 | 0.610–1.159 | 0.290 |
| >30 | 1.057 | 0.680–1.645 | 0.804 | 0.99 | 0.692–1.417 | 0.957 |
| Number of ELNs (continuous variable) | 0.998 | 0.986–1.011 | 0.804 | 0.997 | 0.987–1.006 | 0.51 |
| Node-positive AC (n) | ||||||
| 1–10 | 1 | 1 | ||||
| 11–20 | 0.811 | 0.501–1.315 | 0.396 | 0.931 | 0.588–1.474 | 0.760 |
| 21–30 | 0.663 | 0.381–1.155 | 0.147 | 0.715 | 0.420–1.219 | 0.218 |
| >30 | 0.853 | 0.496–1.467 | 0.566 | 0.905 | 0.539–1.519 | 0.705 |
| Number of ELNs (continuous variable) | 0.994 | 0.979–1.009 | 0.441 | 0.996 | 0.982–1.010 | 0.604 |
Abbreviations: AC, adenocarcinoma; CI, confidence interval; CSS, cause-specific survival; ELNs, examined lymph nodes; HR, hazard ratio; SCC, squamous cell carcinoma; OS, overall survival.
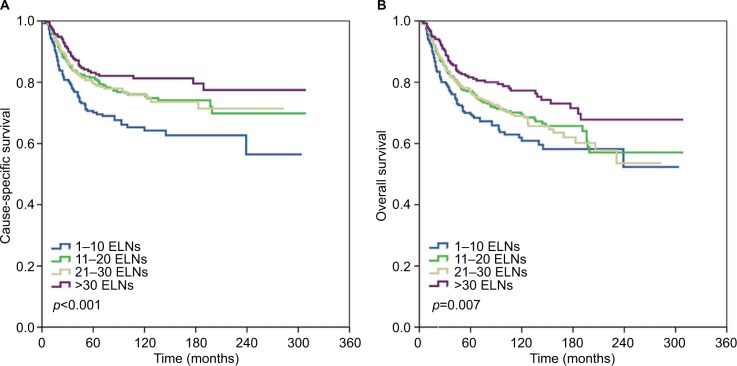
The prognostic value of the number of ELNs in patients with SCC and AC was further analyzed. The ELN count was not significantly different between SCC and AC (p=0.760). However, more patients had a higher number of PLNs in SCC subtype, whereas AC patients were more likely to have node-negative disease (p<0.001). In SCC subtype, the results of multivariate analysis showed that the number of ELNs as a continuous or a categorical variable was also an independent prognostic factor for CSS and OS in the entire cohort and in the node-positive subset, but not in the node-negative patients (Table 3; Figure 1). However, ELN count was not an independent predictor of CSS and OS regardless of lymph node status (Table 3).
Figure 1.
Impact of examined lymph node (ELN) count on cause-specific survival (A) and overall survival (B) in node-positive cervical squamous cell carcinoma.
Discussion
In this study, we investigated the prognostic impact of ELN count of early stage cervical cancer patients in a population-based study. Our results indicated that ELN count was an independent prognostic factor for survival outcomes, especially in patients with a node-positive disease. The subgroup analysis showed similar results in patients with SCC subtype, while ELN count had no prognostic value in AC patients.
Currently, the therapeutic value of extensive lymphadenectomy in patients with cervical cancers remains controversial. A study by Lim et al found that a more extensive lymphadenectomy (>40 ELNs) improved survival in patients with tumors sized >4 cm.21 However, other studies found that the ELN count had no effect on survival.13–15 In this study, we found that a higher number of ELNs was associated with better survival in patients with early stage cervical cancer.
Although the lymph node status has not been included in the FIGO staging system, several studies have suggested that a higher number of PLNs was an unfavorable prognostic factor for survival.9,10 Our study also found that patients with a higher number of PLNs had worse prognosis and that the risk of lymph node involvement (>4) was significantly increased in patients with >30 ELNs. Therefore, a higher number of ELNs may reduce the risk of occult lymph node metastases.
The effect of number of ELNs on survival of patients with cervical cancer according to different lymph node status remains controversial. A previous SEER study suggested that more extensive lymphadenectomy improved survival in node-negative patients and had no prognostic value in node-positive patients (from 1988 to 2005).16 In our study, subgroup analyses found that ELN count was the independent prognostic factor in node-positive patients but not in patients with node-negative disease. Our results were contrary to the findings of Shah et al,16 which may be due to the difference in sample size (11,830 vs 5,222, respectively). In addition, 48.0% of patients in the Shah et al16 study were diagnosed after 2000, and 76.4% of patients in our study were diagnosed after 2000, which differences in the use of adjuvant therapy may exist according to the year of diagnosis. Although there were contrary findings between the two SEER studies, our results were similar to previous studies.11,12 Mao et al also found that there was no prognostic effect of ELN count in node-negative patients.22
The epidemiology, etiology, clinicopathological and molecular characteristics, treatment response, and prognosis of SCC are significantly different compared to AC of the uterine cervix.17–19 However, the incidence of AC has increased in recent decades. In our study, 33.1% of patients were diagnosed with cervical AC, which was higher than a previous SEER study (20%).23 Several studies have shown that radiotherapy was the main local treatment in cervical SCC, while more cervical AC patients received primary surgery.24,25 Therefore, the higher incidence of AC in our study was related to difference in the study population. Previous studies indicated that there was no significant difference in lymph node status between SCC and AC.26,27 In this study, the ELN count was not significantly different between SCC and AC. However, more patients had a higher number of PLNs in SCC subtype, whereas AC patients were more likely to have node-negative disease. However, the SCC subtype had a higher number of PLNs compared with AC group.
The effect of ELN count on the survival of patients with SCC and AC is not well determined. Our subgroup analysis found that ELN count was the independent prognostic factor in node-positive SCC subtype. In addition, the ELN count had no prognostic value in AC patients regardless of nodal status. To the best of our knowledge, our study was the first to identify the prognostic value of ELN count in cervical cancer with different histological subtypes.
The extent of lymphadenectomy may be individualized based on accurate assessment of lymph node status. Previous studies have found that advanced FIGO stage, large tumor size, deep stromal invasion, involvement of the parametrium, and lymphovascular invasion could predict lymph node metastasis in cervical cancer.28,29 In addition, positron emission tomography/computer tomography (PET/CT) and magnetic resonance imaging (MRI) have higher sensitivity and specificity in predicting lymph node metastasis.30,31 However, the accuracy of PET/CT decreases for nodal size <5 mm and micrometastasis.30,31 PET/MRI-diffusion weighted imaging may be a valuable imaging technique for nodal staging in patients with cervical and endometrial cancer, but further studies are required to investigate its potential clinical utility.32
An increasing number of studies have found that sentinel lymph node (SLN) biopsy is an important indicator evaluating pelvic nodal status in cervical cancer, with excellent detection rates and high sensitivity.33,34 SLN biopsy without pelvic lymphadenectomy is considered safe in cervical cancer patients with negative SLNs.35,36 Several studies have found that indocyanine green SLN mapping in cervical cancer provided higher overall and bilateral detection rates compared with current standard of care37–39 and removed up to three SLNs which may be enough to accurately assess the lymph node staging in cervical cancer patients.40 The current National Comprehensive Cancer Network guidelines recommended the SLN technique for early stage cervical cancer with tumor size <2 cm.41 Our study found that the number of ELNs has no effect on survival in node-negative cervical cancer. Therefore, combined with the current SLN biopsy technology, pelvic lymphadenectomy may be avoided in node-negative cervical cancer.
Our study has several limitations that need to be acknowledged. First, inherent bias could not be avoided in retrospective studies. Second, the SEER program lacks data concerning several pathological factors including lymphovascular invasion, stromal invasion, and postoperative complications among the ELNs groups, which may cause bias to analysis. In addition, the extents of lymphadenectomy (pelvic, inguinal, or para-aortic) were not clearly defined because there is no detailed record in the SEER database. Third, there was no information regarding whether or not chemotherapy has been given. Fourth, the period of this study spanned about 25 years, and the adjuvant treatment of early stage cervical cancer has changed in recent decades,42 which may have potentially impacted the survival outcomes.
Conclusion
In patients with stage IA2–IIB cervical cancer, the number of ELNs is an independent prognostic factor of survival. A higher number of ELNs is associated with better survival outcomes, especially in the node-positive SCC subtype. Further studies are required to determine the optimal extent of lymphadenectomy in cervical cancer with different histological subtypes.
Acknowledgments
This work was supported by grants from the Natural Science Foundation of Fujian Province (numbers 2015J01550 and 2013D001), the Foundation Medical Innovation Foundation of Fujian Province (number 2015-CXB-34), and the Foundation for Young Scholar of Fujian Provincial Health Department (number 2014-ZQN-ZD-31). The authenticity of this article has been validated by uploading the key raw data onto the Research Data Deposit (RDD) public platform (www.researchdata.org.cn), with the approval RDD number as RDDA2017000184.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- 3.Liang W, He J, Shen Y, et al. Impact of examined lymph node count on precise staging and long-term survival of resected non-small-cell lung cancer: a population study of the US SEER database and a Chinese multi-institutional registry. J Clin Oncol. 2017;35(11):1162–1170. doi: 10.1200/JCO.2016.67.5140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woo Y, Goldner B, Ituarte P, et al. Lymphadenectomy with optimum of 29 lymph nodes retrieved associated with improved survival in advanced gastric cancer: a 25,000 patient international database study. J Am Coll Surg. 2017;224(4):546–555. doi: 10.1016/j.jamcollsurg.2016.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall MD, Schultheiss TE, Smith DD, et al. Impact of total lymph node count on staging and survival after neoadjuvant chemoradiation therapy for rectal cancer. Ann Surg Oncol. 2015;22(Suppl 3):S580–S587. doi: 10.1245/s10434-015-4585-1. [DOI] [PubMed] [Google Scholar]
- 6.Kleppe M, van der Aa MA, Van Gorp T, Slangen BF, Kruitwagen RF. The impact of lymph node dissection and adjuvant chemotherapy on survival: a nation wide cohort study of patients with clinical early-stage ovarian cancer. Eur J Cancer. 2016;66:83–90. doi: 10.1016/j.ejca.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Chen GD, Lin LY, Wang PH, Lee HS. Urinary tract dysfunction after radical hysterectomy for cervical cancer. Gynecol Oncol. 2002;85(2):292–297. doi: 10.1006/gyno.2002.6614. [DOI] [PubMed] [Google Scholar]
- 8.Zullo MA, Manci N, Angioli R, Muzii L, Panici PB. Vesical dysfunctions after radical hysterectomy for cervical cancer: a critical review. Crit Rev Oncol Hematol. 2003;48(3):287–293. doi: 10.1016/s1040-8428(03)00125-2. [DOI] [PubMed] [Google Scholar]
- 9.Kasuya G, Ogawa K, Iraha S, et al. Postoperative radiotherapy for uterine cervical cancer: impact of lymph node and histological type on survival. Anticancer Res. 2013;33(5):2199–2204. [PubMed] [Google Scholar]
- 10.Horn LC, Hentschel B, Galle D, Bilek K. Extracapsular extension of pelvic lymph node metastases is of prognostic value in carcinoma of the cervix uteri. Gynecol Oncol. 2008;108(1):63–67. doi: 10.1016/j.ygyno.2007.08.086. [DOI] [PubMed] [Google Scholar]
- 11.Kim HS, Kim JH, Chung HH, et al. Significance of numbers of metastatic and removed lymph nodes in FIGO stage IB1 to IIA cervical cancer: primary surgical treatment versus neoadjuvant chemotherapy before surgery. Gynecol Oncol. 2011;121(3):551–557. doi: 10.1016/j.ygyno.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 12.Pieterse QD, Kenter GG, Gaarenstroom KN, et al. The number of pelvic lymph nodes in the quality control and prognosis of radical hysterectomy for the treatment of cervical cancer. Eur J Surg Oncol. 2007;33(2):216–221. doi: 10.1016/j.ejso.2006.09.037. [DOI] [PubMed] [Google Scholar]
- 13.Suprasert P, Charoenkwan K, Khunamornpong S. Pelvic node removal and disease-free survival in cervical cancer patients treated with radical hysterectomy and pelvic lymphadenectomy. Int J Gynaecol Obstet. 2012;116(1):43–46. doi: 10.1016/j.ijgo.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Ditto A, Martinelli F, Lo Vullo S, et al. The role of lymphadenectomy in cervical cancer patients: the significance of the number and the status of lymph nodes removed in 526 cases treated in a single institution. Ann Surg Oncol. 2013;20(12):3948–3954. doi: 10.1245/s10434-013-3067-6. [DOI] [PubMed] [Google Scholar]
- 15.Xie XZ, Song K, Cui B, et al. Clinical and pathological factors related to the prognosis of chinese patients with stage Ib to IIb cervical cancer. Asian Pac J Cancer Prev. 2012;13(11):5505–5510. doi: 10.7314/apjcp.2012.13.11.5505. [DOI] [PubMed] [Google Scholar]
- 16.Shah M, Lewin SN, Deutsch I, et al. Therapeutic role of lymphadenectomy for cervical cancer. Cancer. 2011;117(2):310–317. doi: 10.1002/cncr.25408. [DOI] [PubMed] [Google Scholar]
- 17.Fujiwara K, Monk B, Devouassoux-Shisheboran M. Adenocarcinoma of the uterine cervix: why is it different? Curr Oncol Rep. 2014;16(12):416. doi: 10.1007/s11912-014-0416-y. [DOI] [PubMed] [Google Scholar]
- 18.Gien LT, Beauchemin MC, Thomas G. Adenocarcinoma: a unique cervical cancer. Gynecol Oncol. 2010;116(1):140–146. doi: 10.1016/j.ygyno.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 19.Zhou J, Wu SG, Sun JY, et al. Comparison of clinical outcomes of squamous cell carcinoma, adenocarcinoma, and adenosquamous carcinoma of the uterine cervix after definitive radiotherapy: a population-based analysis. J Cancer Res Clin Oncol. 2017;143(1):115–122. doi: 10.1007/s00432-016-2246-9. [DOI] [PubMed] [Google Scholar]
- 20.Surveillance, Epidemiology, and End Results (SEER) Program ( www.seer.cancer.gov) SEER#x0002A;Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2015 Sub (1973-2013 varying) - Linked To County Attributes - Total U.S., 1969-2014 Counties. National Cancer Institute, DCCPS, Surveillance Research Program; [Accessed January 25, 2017]. released April 2016, based on the November 2015 submission. Available from: https://seer.cancer.gov/data. [Google Scholar]
- 21.Lim S, Cho K, Lee S, et al. Effect of number of retrieved lymph nodes on prognosis in FIGO stage IB-IIA cervical cancer patients treated with primary radical surgery. J Obstet Gynaecol Res. 2017;43(1):211–219. doi: 10.1111/jog.13171. [DOI] [PubMed] [Google Scholar]
- 22.Mao S, Dong J, Li S, Wang Y, Wu P. Prognostic significance of number of nodes removed in patients with node-negative early cervical cancer. J Obstet Gynaecol Res. 2016;42(10):1317–1325. doi: 10.1111/jog.13058. [DOI] [PubMed] [Google Scholar]
- 23.Adegoke O, Kulasingam S, Virnig B. Cervical cancer trends in the United States: a 35-year population-based analysis. J Womens Health (Larchmt) 2012;21(10):1031–1037. doi: 10.1089/jwh.2011.3385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vinh-Hung V, Bourgain C, Vlastos G, et al. Prognostic value of histopathology and trends in cervical cancer: a SEER population study. BMC Cancer. 2007;7:164. doi: 10.1186/1471-2407-7-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou J, Wu SG, Sun JY, et al. The effect of local treatment modalities in patients with early-stage adenocarcinoma of the uterine cervix: a population-based analysis. Int J Surg. 2017;41:16–22. doi: 10.1016/j.ijsu.2017.03.024. [DOI] [PubMed] [Google Scholar]
- 26.Winer I, Alvarado-Cabrero I, Hassan O, et al. The prognostic significance of histologic type in early stage cervical cancer – a multi-institutional study. Gynecol Oncol. 2015;137(3):474–478. doi: 10.1016/j.ygyno.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 27.Noh JM, Park W, Kim YS, et al. Comparison of clinical outcomes of adenocarcinoma and adenosquamous carcinoma in uterine cervical cancer patients receiving surgical resection followed by radiotherapy: a multicenter retrospective study (KROG 13–10) Gynecol Oncol. 2014;132(3):618–623. doi: 10.1016/j.ygyno.2014.01.043. [DOI] [PubMed] [Google Scholar]
- 28.Sakuragi N. Up-to-date management of lymph node metastasis and the role of tailored lymphadenectomy in cervical cancer. Int J Clin Oncol. 2007;12(3):165–175. doi: 10.1007/s10147-007-0661-2. [DOI] [PubMed] [Google Scholar]
- 29.Zhou J, Ran J, He ZY, et al. Tailoring pelvic lymphadenectomy for patients with stage IA2, IB1, and IIA1 uterine cervical cancer. J Cancer. 2015;6(4):377–381. doi: 10.7150/jca.10968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi HJ, Ju W, Myung SK, Kim Y. Diagnostic performance of computer tomography, magnetic resonance imaging, and positron emission tomography or positron emission tomography/computer tomography for detection of metastatic lymph nodes in patients with cervical cancer: meta-analysis. Cancer Sci. 2010;101(6):1471–1479. doi: 10.1111/j.1349-7006.2010.01532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mayoral M, Paredes P, Domènech B, et al. 18F-Fdg PET/CT and sentinel lymph node biopsy in the staging of patients with cervical and endometrial cancer. Role of dual-time-point imaging. Rev Esp Med Nucl Imagen Mol. 2017;36(1):20–26. doi: 10.1016/j.remn.2016.07.003. Spanish, with English abstract. [DOI] [PubMed] [Google Scholar]
- 32.Stecco A, Buemi F, Cassarà A, et al. Comparison of retrospective PET and MRI-DWI (PET/MRI-DWI) image fusion with PET/CT and MRI-DWI in detection of cervical and endometrial cancer lymph node metastases. Radiol Med. 2016;121(7):537–545. doi: 10.1007/s11547-016-0626-5. [DOI] [PubMed] [Google Scholar]
- 33.Diab Y. Sentinel lymph nodes mapping in cervical cancer a comprehensive review. Int J Gynecol Cancer. 2017;27(1):154–158. doi: 10.1097/IGC.0000000000000853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lécuru F, Mathevet P, Querleu D, et al. Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: results of the SENTICOL study. J Clin Oncol. 2011;29:1686–1691. doi: 10.1200/JCO.2010.32.0432. [DOI] [PubMed] [Google Scholar]
- 35.Lennox GK, Covens A. Can sentinel lymph node biopsy replace pelvic lymphadenectomy for early cervical cancer? Gynecol Oncol. 2017;144(1):16–20. doi: 10.1016/j.ygyno.2016.08.337. [DOI] [PubMed] [Google Scholar]
- 36.Niikura H, Okamoto S, Otsuki T, et al. Prospective study of sentinel lymph node biopsy without further pelvic lymphadenectomy in patients with sentinel lymph node-negative cervical cancer. Int J Gynecol Cancer. 2012;22(7):1244–1250. doi: 10.1097/IGC.0b013e318263f06a. [DOI] [PubMed] [Google Scholar]
- 37.Buda A, Papadia A, Zapardiel I, et al. From Conventional Radiotracer Tc-99(m) with blue dye to indocyanine green fluorescence: a comparison of methods towards optimization of sentinel lymph node mapping in early stage cervical cancer for a laparoscopic approach. Ann Surg Oncol. 2016;23(9):2959–2965. doi: 10.1245/s10434-016-5227-y. [DOI] [PubMed] [Google Scholar]
- 38.Imboden S, Papadia A, Nauwerk M, et al. A comparison of radio colloid and indocyanine green fluorescence imaging, sentinel lymph node mapping in patients with cervical cancer undergoing laparoscopic surgery. Ann Surg Oncol. 2015;22(13):4198–4203. doi: 10.1245/s10434-015-4701-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ruscito I, Gasparri ML, Braicu EI, et al. Sentinel node mapping in cervical and endometrial cancer: indocyanine green versus other conventional dyes – a meta-analysis. Ann Surg Oncol. 2016;23(11):3749–3756. doi: 10.1245/s10434-016-5236-x. [DOI] [PubMed] [Google Scholar]
- 40.Papadia A, Imboden S, Gasparri ML, Siegenthaler F, Fink A, Mueller MD. Endometrial and cervical cancer patients with multiple sentinel lymph nodes at laparoscopic ICG mapping: how many are enough? J Cancer Res Clin Oncol. 2016;142:1831–1836. doi: 10.1007/s00432-016-2193-5. [DOI] [PubMed] [Google Scholar]
- 41.National Comprehensive Cancer Network NCCN Clinical Practice Guidelines in Oncology. Cervical Cancer. Version 1.2017 [updated October 10, 2016] [Accessed May 28, 2017]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf.
- 42.Peters WA, 3rd, Liu PY, Barrett RJ, 2nd, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000;18(8):1606–1613. doi: 10.1200/JCO.2000.18.8.1606. [DOI] [PubMed] [Google Scholar]