Abstract
Aims
The majority of post-acute hip fracture rehabilitation in the US is delivered in skilled nursing facilities (SNFs). Currently, there are limited guidelines that equip occupational and physical therapy practitioners with a summary of what constitutes evidence-based high quality rehabilitation. Thus, this study aimed to identify rehabilitation practitioners' perspectives on the practices that constitute high quality hip fracture rehabilitation.
Methods
Focus groups were conducted with 99 occupational and physical therapy practitioners working in SNFs in southern California. Purposive sampling of facilities was conducted to capture variation in key characteristics known to impact care delivery for this patient population (e.g., financial resources, staffing, patient case-mix). Questions aimed to elicit practitioners' perspectives on high quality hip fracture rehabilitation practices. Each session was audio-recorded and transcribed. Data were systematically analyzed using a modified grounded theory approach.
Results
Seven themes emerged: objectives of care; first 72 hours; positioning, pain, and precautions; use of standardized assessments; episode of care practices; facilitating insight into progress; and interdisciplinary collaboration.
Conclusions
Clinical guidelines are critical tools to facilitate clinical decision-making and achieve desired patient outcomes. The findings of this study highlight the practitioners' perspective on what constitutes high quality hip fracture rehabilitation. This work provides critical information to advance the development of stakeholder-driven rehabilitation clinical guidelines. Future research is needed to verify the findings from other stakeholders (e.g., patients), ensure the alignment of our findings with current evidence, and develop measures for evaluating their delivery and relationship to desired outcomes.
Keywords: hip fracture, occupational therapy, physical therapy, post-acute care, qualitative
Introduction
In the United States, 90% of patients that experience a hip fracture are discharged to a post-acute care (PAC) facility for rehabilitation after an average of 6 days in the hospital [1, 2]. The majority of patients are admitted to a skilled nursing facility (SNF) for PAC [3, 4], instead of going home with home health care or receiving care in an inpatient rehabilitation facility. The focus of PAC rehabilitation, across patient populations, is to support continued medical and functional recovery to facilitate a safe return to the community [3]. Achievement of this desired patient goal requires collaboration between the patient, caregiver and all members of the care team including physicians, nursing, social workers, and rehabilitation.
Regrettably, outcomes for this hip fracture population are suboptimal. Few patients return to their prior level of independence and long-term institutionalization is common [5-8]. As efforts to improve patient outcomes expand from a focus on acute hospitals to include PAC settings, there is growing scrutiny of the quality of the rehabilitation services[9]. Within the US and other industrialized countries indicators of healthcare quality include hospital readmissions and achieving a safe community transition (e.g. successful community discharge).[10, 11] Efforts to optimize these outcomes are focusing on the care processes that are delivered, as they are the easiest to modify and directly linked to outcomes. This approach is drawn from Donabedian's framework of healthcare quality, which postulates that efforts to optimize patient outcomes are driven by the healthcare setting (i.e. organizational structure) and providers' delivery of evidence-based effective care processes—high quality care.[12-15] As a result, there is an urgent need to identify what constitutes high quality PAC rehabilitation practice and ensure its delivery within the clinical setting.
Existing evidence emphasizes a collaborative multiple discipline approach and documents effective interventions after hip fracture [16-20]. For example, guidelines delineate parameters to guide surgeons, nurses, and physicians during the acute phase of a hip fracture, including timing of surgery, anesthesia, surgical procedures, and then concludes with recommendations for comprehensive rehabilitation[10]. Further, the evidence emphasizes the importance of physician oversight and nursing care during the post-operative phase to address medical recovery, pain management, delirium and fall prevention, and wound healing; occupational and physical therapy are then included. [18, 21-25] Yet, the care processes that reflect their contribution to the care team are not described. To begin to address this gap, rehabilitation evidence has evaluated the timing, intensity, and setting of occupational and physical therapy services on desired patient outcomes as well as document the benefit of specific interventions such as intensive exercise, early mobilization, pre-discharge home assessment, or retraining in activities of daily living.[5, 19, 26, 27] Yet, as part of the care team, there are few clinical guidelines delineating the collective rehabilitation practices that reflect high quality occupational and physical therapy beyond discipline specific evaluations.[28]
Consequently, occupational and physical therapy practitioners are ill-equipped to implement the constellation of evidence-based practices known to enhance outcomes after hip fracture. This gap in our knowledge is particularly concerning given pervasively poor patient outcomes in this patient population [5-7] and the growing emphasis on optimizing patient outcomes by delivering high quality care. Furthermore, PAC facilities are financially incentivized to enhance care delivery and improve patient outcomes or face penalties for poor outcomes [29-31]. Thus, as part of the care team, there is a need to identify what practices constitute high quality rehabilitation. The purpose of this study is to capture perspectives of rehabilitation practitioners, specifically those of occupational and physical therapy, on the hip fracture practices that constitute high quality rehabilitation.
Methods
Study design
In-depth semi-structured focus groups were conducted with occupational therapists (OTs), occupational therapy assistants (OTAs), physical therapists (PTs), and physical therapy assistants (PTAs) working in SNFs in southern California. Ethics approval was obtained from the [blinded for review] Institutional Review Board.
Sampling and recruitment
A purposive sample of SNFs located in Los Angeles County was recruited to participate in the study. Guided by Donabedian's framework, facilities were selected that differ across key organizational characteristics (e.g., total number of beds, staffing levels) and patient characteristics (e.g., socioeconomic status, medical complexity) that have been associated with care quality [12, 32-36] to promote the exploration of care practices that are characteristic of high quality rehabilitation. Sample selection data were derived from the Medicare Nursing Home Compare website, a government-run site providing publicly available information on care quality and organizational characteristics of facilities that receive Medicare and Medicaid payments in the US (https://data.medicare.gov/data/nursing-home-compare). From a list of facilities in LA County, SNF administration was contacted regarding participation in the study. Each approached facility agreed to participate. We then worked with rehabilitation administration to schedule a convenient date and time to be on site. Each facility hosted the research team for one focus group. Prior to the event, facilities were given fliers to advertise the focus group as well as an email providing an overview of the study, which was disseminated to staff.
To participate in the focus group, rehabilitation practitioners had to: (1) be licensed OT, OTA, PT, or PTA; (2) have at least one year of clinical experience working with hip fracture patients; and (3) be employed in the respective facility. Lunch was provided to participants, and upon completion of the focus group, the rehabilitation department was given a $50 gratuity gift card as a token of appreciation.
Data collection
All focus groups were conducted between July and August 2014. One researcher facilitated the focus groups and at least one research assistant attended each session to take notes. The length of the focus groups ranged between 30 minutes and 75 minutes. A total of 13 focus groups were conducted with an average of 7 (±3) participants per group and 99 participants overall. A semi-structured guide that had been previously piloted was used for all focus groups. Questions explored the practitioners' experiences and perceptions of delivering high quality hip fracture rehabilitation and sought out discrete examples to augment their perspectives. For example, participants were asked to think about an entire rehabilitation stay and to identify five practices that every patient admitted with a hip fracture should experience? Participants also completed a brief questionnaire detailing their age (in years), sex (male or female), race/ethnicity (Asian, Black, White, or Other), clinical discipline (OT or PT), length of professional experience (in years), tenure in current facility (in years), and full-time employee status (yes or no).
Data analysis
The focus groups were audio-recorded and transcribed verbatim with all identifying information removed. Each transcript was verified for accuracy. We used a grounded theory approach to analyze the transcripts, which involves three steps of coding (open, axial, and selective).
During open coding, participants' statements and clinical examples were labeled with a word or phrase that succinctly represented the topic area of discussion.[37] After coding the first focus group transcript, the team convened to discuss the codes and their respective coding decisions. Based on comparisons across team members' coding decisions and discussions about which codes most accurately categorize the focus group data, an initial set of codes was generated and used to inform research team members' independent open coding of the second focus group transcript. Subsequently, the team met to discuss the coding of the second transcript, which entailed discussing new codes and refining initial codes as needed to better categorize the focus group data. On all subsequent transcripts, three team members independently coded each transcript, and then the entire team met to discuss the coding process, the codes, and emerging themes and subthemes. After completing initial coding for the 13 transcripts, all data were imported into ATLAS.ti, and the codes that were developed during open coding were applied to all data.
After completing open coding, the research team examined the coded text and related categories of information (i.e., segments of coded text) in a process called axial coding.[37] Specifically, using the Donabedian model, we linked categories to help integrate the structure, process, and outcomes of hip fracture rehabilitation. Categories were linked in a set of relationships that denote causal conditions, contexts, intervening conditions, action/interaction strategies, and consequences. For example, several practices were identified as constituent of high quality rehabilitation particularly when deployed within the first 72 hours in the SNF.
In the final stage of coding—selective coding—major categories were organized around a central explanatory concept or core category.[37] Our core category, high quality hip fracture rehabilitation, was chosen a-priori as it addresses our core research question. Analysis was considered to be complete when theoretical saturation occurred, that is, when no new or relevant data emerged regarding a category, when category development was dense, and when the relationships between categories was well established and validated.
We used constant comparative analysis throughout the three-stage coding process to assure codes and themes were robust, which entailed making comparisons of the coded text within and across focus groups. [38]Transcripts were then reread to verify that the codes were present in the data. Successively, candidate themes and subthemes were reviewed and verified in the data to finalize themes and identify negative case examples that refuted emerging themes. When cases or concepts were identified to refute the candidate themes, the team discussed and amended the themes accordingly. To further verify findings, all 13 participating facilities were invited to participate in one of five web-based interactive meetings in which the preliminary themes and subthemes were presented and feedback was solicited to verify findings. Participants verified all themes.
Results
Table 1 presents the characteristics of the 99 practitioners who participated in the focus groups. Forty-nine percent (n=48) were OT practitioners, 50.5% were PT practitioners (n=49), and two participants did not disclose their discipline. Seven themes emerged that describe high quality hip fracture rehabilitation: (1) objectives of care, (2) the first 72 hours, (3) positioning, pain, and precautions, (4) use of standardized assessments, (5) episode of care processes, (6) facilitating insight into progress, and (7) interdisciplinary collaboration. Each theme is summarized and supported with quotes, which serve as examples of how these practices have been used in clinical practice. To indicate which of the 13 focus groups the quote was extracted from, an FG and number (e.g., FG-8) is used.
Table 1. Focus group participant characteristics.
| Focus Group | Age mean(SD) | Race, % | Female, % | Provider, % | Years of experience, mean (SD) | Years in the facility, mean (SD) | Full-time employee, % | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Asian | Black | White | Othera | OT | PT | ||||||
| All FGs (N=99) | 38.3(9.2) | 42.4 | 2 | 44.4 | 8.1 | 69.7 | 49.5 | 50.5 | 10.7(10.3) | 2.9(3.2) | 89.9 |
|
| |||||||||||
| FG 1 (n=9) | 36(5.4) | 22.2 | 0 | 66.7 | 11.1 | 66.7 | 44.4 | 55.6 | 10.3(7.1) | 3.9(2.3) | 88.9 |
| FG 2 (n=4) | 35(8.5) | 50 | 0 | 50 | 0 | 75 | 50 | 50 | 5.3(4.2)b | 4.1(3.9) | 100 |
| FG 3 (n=10) | 39.5(12.5) | 20 | 0 | 60 | 10 | 60 | 40.0c | 50.0c | 9.1(7.8) | 4.9(3.4) | 90 |
| FG 4 (n=8) | 32.6(4.8)d | 75 | 0 | 25 | 0 | 75 | 50.0c | 37.5c | 6.9(4.3) | 3.4(3.6) | 100 |
| FG 5 (n=10) | 38.5(6.1) | 20 | 20 | 50 | 10 | 60 | 50 | 50 | 9.9(8.3) | 1.5(2.3) | 90 |
| FG 6 (n=1) | 41 | 0 | 0 | 0 | 100 | 100 | 100 | 0 | 18 | 0.5 | 100 |
| FG 7 (n=7) | 41.3(11.3) | 28.6 | 0 | 71.4 | 10 | 71.4 | 42.9 | 57.1 | 13.3(8.5) | 5.4(4.8) | 100 |
| FG 8 (n=13) | 38.7(11.7)d | 38.5 | 0 | 38.5 | 7.7 | 61.5 | 46.2 | 53.8 | 6.4(7.9) | 0.5(0.4) | 100 |
| FG 9 (n=8) | 45(9.3)d | 37.5 | 0 | 50 | 12.5 | 75 | 50 | 50 | 17.4(13.5) | 3.5(3.5) | 100 |
| FG 10 (n=8) | 37(9.9)d | 87.5 | 0 | 0 | 12.5 | 87.5 | 62.5 | 37.5 | 9.1(9.7) | 1.1(0.5) | 87.5 |
| FG 11 (n=7) | 37.5(11.8)d | 57.1 | 0 | 14.3 | 0 | 57.1 | 57.1 | 42.9 | 10.2(8.9)b | 2.2(1.5) | 57.1 |
| FG 12 (n=7) | 41.1(6.1) | 57.1 | 0 | 42.9 | 0 | 71.4 | 42.9 | 57.1 | 13.9(6.5) | 4.3(4.9) | 71.4 |
| FG 13 (n=7) | 34.1(6.7) | 42.9 | 0 | 28.6 | 14.3 | 85.7 | 42.9 | 57.1 | 9(6.9) | 2.9(1.8) | 85.7 |
Other = participants who identified as other and participants who selected more than one race.
Two participants were missing data on type of providers, n=97.
One participant was missing data on years of experience, n=98.
Full time employee = yes was a full time employee.
Objectives of care
Participants emphasized that the objective of rehabilitation is to get the patient back home. However, they clarified that it is not just about whether or not the patient returns to the community; rather, high quality care reflects the facilitation of a safe discharge home. This includes maximizing independence and equipping the patient (and caregivers) with knowledge and skills to get home and stay home—safely. To this end, the patient and caregiver need to be equipped with skills to recognize symptoms that may indicate a change in medical or functional status, such as a urinary tract infection, surgical infection, or change in fall risk. Additionally, preventing subsequent falls and fractures was consistently described as an objective of rehabilitation. Embedded within this overarching goal, as the practitioners emphasized, is the importance of helping the patient come to terms with his or her “new self.”
One participant described a common occurrence in PAC rehabilitation in which patients view themselves as the person they were prior to the fracture without insight into current functional limitations or recognition of what facility staff are providing in terms of support with self-care. For example, a study participant explained:
“They [patients] start to think they can do this and that, once they get to their own environment.” (FG-6)
If not addressed, this mismatch between what the patient could do before the fracture, what the patient can do with PAC staff assistance, and what they envision they can do at home poses risks, as another participant explained:
“Some patients will be like, ‘Oh no, I'm doing fine [here]. Oh yeah, I'm going to do this at home,’ and then I ask, ‘Okay, do you have this grab bar in your bathroom like we have here?’ And they go, ‘Oh, wait, at home, I might not be able to.’” (FG-2)
The practitioner's role was described as assisting the patient and caregiver to reconcile the individual's capacity before the fracture with the “new self” so patients can understand abilities, limitations, and need for supports to safely engage in meaningful activities within their home environment.
The first 72 hours
A theme arose regarding the first 72 hours after a patient's discharge from the hospital to PAC with a hip fracture diagnosis, distinguishing this time frame from the rest of the PAC stay. The practitioners' initial interactions with the patient and family were identified as pivotal exchanges that lay the foundation for the entire stay. Not only were OT and PT evaluations conducted, but this was also a time to build relationships with the patient and family, who may be experiencing a stressful and chaotic transition from the hospital to PAC. Creating a collaborative and trustful relationship with the patient and family during the first 72 hours was described as high quality care:
“Developing trust is huge. If they don't trust you, they will not do anything for you.” (FG-12)
Practitioners also described the importance of orienting the patient and family to the facility and the rehabilitation process so they knew what to expect throughout the stay.
“Educating them a lot… explaining why they're here; how long that might be. [Emphasizing] the shared goal is to go home, and be back to their [prior] level.” (FG-2)
This would include discussing findings of the evaluation, collaborating on care planning, and initiating mobility while reinforcing hip precautions and weight bearing status.
Several focus groups discussed the importance of talking with the certified nursing assistants (CNAs) and the charge nurse after completing the initial rehabilitation evaluation to foster interdisciplinary care. In the US, CNAs are the care providers who assist patients with the majority of self-care tasks in SNFs. As overseers of patient care, the charge nurse communicates patient updates and recommendations to nursing on the next shift as well as the physician overseeing the plan of care. The intent of this initial communication with nursing was to convey the OT/PTs' evaluation findings, recommendations for assisting the patient (e.g., toilet transfers), and strategies to prevent adverse events (e.g., accidental falls), particularly in the first 72 hours.
The 3 P's: Pain, Positioning, & Precautions
To promote recovery while increasing functional abilities, the 3 P's—pain, positioning, and precautions—were identified as a core area for high quality hip fracture rehabilitation. Practitioners acknowledged that pain after surgical repair of a hip fracture is common and can slow recovery, limiting participation in rehabilitation. Practitioners stated that their role in pain management included: collaborating with patients and nursing staff to identify optimal times for rehabilitation based on pain medication schedules; monitoring pain during therapy sessions; and working with the care team, particularly the nurse and physician, when pain interferes with the patient's ability to participate in therapy. Practitioners also described the importance of integrating alternative strategies and positioning into treatment sessions to mitigate pain:
“I've encouraged patients to bring in some relaxing music or [try] meditation and basic breathing techniques. We complement [medications] with other ways to manage their pain.” (FG-11)
Positioning was closely tied to compliance with precautions and addressing pain, including working with the patient to identify body positions that mitigate pain while aligning with precautions.
Depending on surgical approach for the hip fracture repair, the patient may have to comply with hip precautions to avoid dislocation. As the patient begins to engage in self-care tasks and functional mobility, they must learn how to move in a new way:
“PTs, [best practice is to] first do bed mobility. If there is a hip replacement, make sure that patient knows their precautions. Focus on the bed mobility because that's the first barrier to getting out from the bed.” (FG-13)
The participants emphasized high quality hip fracture rehabilitation should include educating, training, and reinforcing the integration of the hip precautions and weight bearing limitations in the context of the patient's daily activities in order to establish new routines:
“They're used to doing it [getting dressed] a certain way; [rehab has to] show them there's a different way to do it and really getting them used to that.” (FG-2)
Use of standardized assessments
Evaluating patient risk and abilities with standardized assessments served multiple purposes and was described by participants as a marker of high quality care. Focus group participants discussed augmenting required clinical documentation with assessments to demonstrate need for intervention and progress to the patient, caregiver, and insurance companies. Three common assessment areas were fall risk, balance, and cognition. Use of standardized assessments provided quantifiable and normative standards, with which OT and PT practitioners supported their clinical recommendations during the collaborative process of making healthcare decisions with the patient, caregiver, and interdisciplinary team. Assessing fall risk and balance were used to facilitate conversations about an individual's risk of subsequent falls and opportunities for altering that risk. Due to the interplay between cognitive ability and engagement in functional tasks, results of standardized cognitive assessments were used to guide treatment approaches (e.g., facilitating compliance with weight bearing during mobility and dressing), educate caregivers during training sessions, and inform discharge recommendations (e.g., 24 hour supervision, assistance with medications).
Episode of care practices
A series of clinical practices was identified as critical and necessary for patients in hip fracture rehabilitation to achieve a safe community discharge. As reflected in Figure 1, activities of daily living (ADLs) retraining, environmental safety assessments, community mobility, navigating stairs, fall prevention, and health management strategies (e.g., symptoms of medical status changes) are among the practices that participants consistently labeled as reflecting high quality care. Further, it was emphasized that discharge planning must start at admission and continue throughout the stay to address the patient's cumulative functional and medical needs in order to achieve a safe community discharge. This ongoing process was described as being informed by the other care practices reflected in the figure, which is why discharge planning is reflected in the figure as encapsulating the other processes. Practitioners suggested these practices be addressed throughout the stay by means of education, training, handouts, skill-building, and teach-back sessions with patients, family, and staff:
Figure 1.
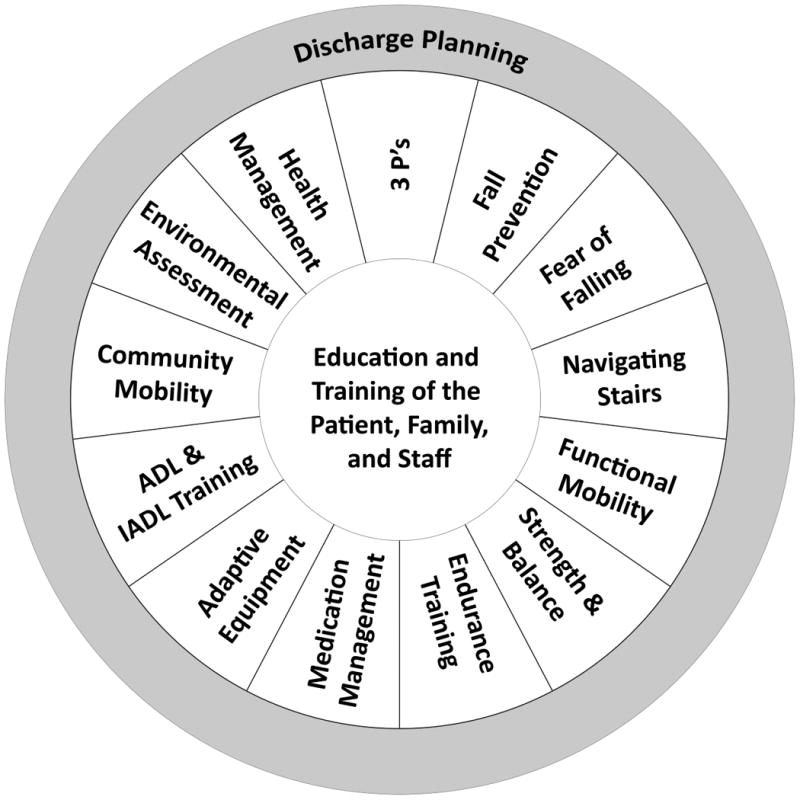
Episode of Care Practices Note: These are practices that practitioners suggested be addressed throughout the PAC stay by means of education, training, handouts, skill-building, and teach-back sessions with patients, family, and staff.
“You really want the family to come in [for training] so they feel confident when they are by themselves at home [with the patient] so that they'll be able to do it.” (FG-2).
Practitioners frequently described using in-person training to model a behavior or skill, capitalizing on hand-over-hand assistance and providing verbal cues to build efficacy.
In discussing environmental assessments, practitioners across focus groups consistently pointed out two distinctive times at which conducting the assessment was crucial: near the time of the PAC admission and in preparation for community discharge. Such distinction was made to emphasize the importance of examining the person-environment fit in each setting (in the facility and again in the community) and reconciling any discrepancy between the environment and the patient's abilities, precautions, risk, and needs.
“If it's a dementia patient, we might not want them in a low bed [because the patient] might be more likely to dislocate [the hip] on their way out of bed. So, communicating [to nursing] that patient is not a low bed [candidate], so that you get the right one [strategy to prevent the dislocation and potential fall].” (FG-5)
Participants described the optimal approach for the environmental assessment of the patient's home would be a home visit. Yet, acknowledging that a home visit is not always possible, practitioners in several facilities described alternative approaches they use, including Skype/Facetime with a caregiver to get a virtual-tour of the home, asking the caregiver to complete the Center for Disease Control home safety checklist, or having the caregiver take pictures of the home environment. These approaches could then inform recommendations and guide remaining treatment sessions to address specific needs of the patient prior to discharge:
“the patient has a four-inch threshold to step over, so we'll try to simulate the best we can. We want to address anything that they're having a tough time with.” (FG-1)
Community mobility was explained in the context of facilitating a safe community transition to prevent adverse events. The practitioners described a variety of patient scenarios, such as needing to access transportation (e.g., car, public bus) to go to a doctor's appointment. To minimize dislocation of the hip, ensure compliance with hip precautions, and accommodate a patient's limitation, the practitioner, patient, and caregiver need to discuss appropriate means of community mobility and problem-solve barriers. Practitioners emphasized high quality care integrated modeling and hands-on patient and caregiver practice for community mobility training (e.g., car transfer training).
During the patient's rehabilitation stay, nurses dispensed the medications based on a physician-prescribed medication schedule. However, in preparation for going home, OTs frequently found it important to address the patient's medication routine. Medication management was seen as collaborative effort with the nurses, patient, and caregiver, to ensure the medication schedule prescribed by the physician was integrated into the patient's daily routine. OTs frequently described using the results of the standardized cognitive assessment(s) to guide their clinical approaches. For individuals with impaired cognition, the practitioners described working with both the patient and caregiver to identify strategies for integrating medications schedules into their daily routine. Alternatively, if the patient had cognitive impairment but no caregiver(s), participants emphasized the importance of making recommendations to the interdisciplinary care team to ensure services are setup to support a safe discharge, including assistance with medication compliance.
Facilitating insight into progress
To support the patient's recognition of his or her “new self,” practitioners emphasized the importance of highlighting functional progress to the patient. Failure to facilitate the patient's insight into their abilities can result in the patient engaging in activities they can no longer complete safely, as they did prior to the hip fracture, thereby increasing risk of poor outcomes. Practitioners shared examples in which they informally initiated conversations with the patient about their progress during a treatment session, at the end of a session, and weekly during goal review.
“Pointing out that progress, [which] they don't realize. They go, ‘we're doing terrible, I can't do this.’ But, look how far you walked yesterday and look how you're doing today. Making sure they realize it, because they may not feel like they're making progress, but we see it.” (FG-2)
Interdisciplinary collaboration
In PAC, where care focuses on patients' medical and functional recovery, OT and PT practitioners work with other disciplines to achieve patients' goals. Interdisciplinary collaboration was frequently described as a key element of high quality care and also a give-and-take dynamic. One focus group participant shared,
“as therapists, we are information gatherers, and then [sharing] that information to nursing, or whoever's going to use it.” (FG-7)
Alternatively, another participant stated the importance of receiving information from other disciplines during the morning standup meeting:
“the charge nurses from each station will… give their 24-hour report. The CNAs also give an update on how they [the patients] did in the morning.” (FG-7)
Examples of interdisciplinary communication included sharing information about medications, weight bearing status, or the patient's change in assistance level outside the therapy room.
As conveyers of information, the practitioners used training sessions to communicate recommended approaches to both the patient and staff. However, the approaches to training differed across various facilities, from spur-of-the-moment training with the CNAs and patient to formal in-service training with all CNAs on the unit. Interdisciplinary communication was consistently seen as critical to delivering high quality care.
Discussion
By identifying practitioners' perspectives on the care practices that constitute high quality rehabilitation, this study addresses a gap in the literature. Previous literature has examined the effect of a single rehabilitation intervention or identified the importance of occupational and physical therapy as part of the care team [16-20], but there is a dearth of evidence detailing the cumulative OT and PT care processes that constitute PAC rehabilitation. Seven themes emerged from focus groups with rehabilitation practitioners, reflecting common perceptions on the goals and domains that make up high quality hip fracture rehabilitation: objectives of care; the first 72 hours; positioning, pain, and precautions; use of standardized assessments; episode of care practices; facilitating insight into progress; and interdisciplinary collaboration.
Practitioners in this study consistently described the goal of care as safely getting the patient home without re-hospitalization. Despite the commonly used dichotomous outcome measure of community discharge [39], which focuses solely on whether the patient goes home or not, practitioners in this study had a broader goal of PAC rehabilitation. In alignment with readmission prevention efforts in the US and internationally, practitioners defined community discharge as getting home and staying there, thereby avoiding a readmission for at least 30 days [40]. The practices that these study participants went on to describe, were situated within this goal of getting the patient home and equipping the patient and caregiver with the knowledge and skills to stay home.
Toward this end, participants described a patient-centered approach to discharge planning. They emphasized that discharge planning started at admission and took into account the patients' as well as the caregivers needs and abilities, both physical and cognitive, to promote independence and minimize risk of adverse events, which aligns with the broader care transition literature [41-46]. Taking this patient-centered approach addresses a gap described in previous studies, which has emphasized caregivers' feelings of being excluded from discharge planning and being ill-equipped to manage caregiving responsibilities post-discharge [47-50]. Furthermore, study participants consistently described interdisciplinary collaboration as a high priority. OT and PT frequently described reinforcing the efforts of other disciplines (e.g. nursing and physicians) to facilitate medical and medication self-management when working with patients and caregivers during therapy sessions. This collaborative, yet complementary approach is consistent with effective acute care community transition programs.[41] For example, within the context of medication management, OTs described supporting nursing and physician efforts by utilizing results of the standardized cognitive assessment to inform most effective approaches. This has been supported by previous work detailing OTs efforts to assess and develop interventions related to the client's functional cognition, physical capacity, memory, and other issues to improve the client's ability to manage medications prescribed by the physician.[51, 52] Additionally, participants identified other practices that are not reflected in existing care transition initiatives, but are necessary to prevent readmissions for this rehabilitation population, such assessing fear of falling, and fostering health management in the context of changes in medical and functional status that may occur after PAC discharge. These concepts have each been identified as risk factors for adverse outcomes and therefore are areas to target for discharge planning and prevention of adverse events [53-55].
Persistent pain has been associated with poor outcomes after hip fracture [56] and is more common during movement than at rest [57]. Given the intent of rehabilitation, focus group participants emphasized the importance of assessing and addressing pain from the perspective of functional improvement throughout the PAC stay. In an effort to optimize pain management, interdisciplinary communication and collaboration was described to be essential. In particular, conveying changes in a patient's pain level during functional activities was perceived to be how OT and PT could support physicians and nursing efforts to manage pain. This additional information can assist physicians in care decisions related to polypharmacy, preventing adverse events (e.g. fall risk), and the patient's plan of care, which is consistent with the broader literature detailing the role of nursing and physician in hip fracture recovery. Due to the pervasiveness of chronic pain and its negative impact of limiting activity [58], as recorded in prior research [59, 60], practitioners also described the importance of equipping patients and caregivers with other coping strategies for pain between medication doses.
Promoting functional recovery was consistently described as a primary rehabilitation aim. While practitioners saw themselves as team members contributing to the patients' risk assessment, they approached the patients' issues from the context of optimizing function. Similarly, the practitioners described their relationships with CNAs as mutually supportive. The two most commonly conveyed and valued interchanges occurred when a patient had a change in functional status. The CNA was described as the individual who knew the patient best and could update the practitioner with information that may be used to guide the plan of care. Alternatively, practitioners described instances in which they would inform the CNA of the patient's increased level of independence, which meant the CNA could provide less assistance with a functional task. Due to the constantly changing functional status of this PAC population, such communication between members of the care team was seen as essential to achieving optimal patient outcomes.
Rehabilitation patients and caregivers are challenged with maintaining a delicate balance between regaining independence and managing risk of adverse events within the context of their situated perspectives [61]. Throughout the rehabilitation stay, a patient's perceived abilities, limitations, and autonomy evolve. They may experience functional recovery and increased independence in ADLs and instrumental activities of daily living, but often the new functional ability is less than the patient's prior abilities. Thus, patients have to reconcile the incompatibility of their physical capacity with the perceptions of the individual they expect to be [62]. As patient advocates, practitioners described their efforts to resolve this mismatch between the patient's perceived self and post-fracture abilities by empowering the “new self” and promoting the patient's quality of life. Similar experiences have been described in the stroke rehabilitation literature [50].
Limitations
Limitations of this study are noted. This study does not capture the perspectives of rehabilitation practitioners working in other PAC settings, patients, caregivers, or other members of the PAC team. Future work is needed to capture the priorities of other stakeholders and identify their perspective on the role of OT and PT as part of the care team, as they work collectively to delivery high quality care. Furthermore, this study did not evaluate the extent to which these practices are implemented. The focus groups were conducted in the US within one geographic region; while efforts were made to capture a diverse range of facilities with different resources, patient case-mix, and organizational characteristics associated with quality, the findings may not be generalizable to other geographic regions or other countries. However, similar policy drivers are in place throughout the US and European countries and as such results can still be applied in broad terms.
Despite these limitations, this study has contributed to the literature by addressing what constitutes high quality rehabilitation in the context of multidisciplinary post-operative hip fracture care from the practitioners' perspective. While this study is only the first step towards equipping practitioners with the tools necessary to develop clinical guidelines and enhance patient outcomes, it lays the foundation for subsequent efforts. Future research is needed to verify these findings from the perspective of other stakeholders (e.g., patients), ensure their alignment with current evidence, and develop measures for evaluating their implementation and relationship to desired outcomes.
Conclusion
Currently, rates of readmissions and failed community care transitions are suboptimal for patients experiencing a hip fracture. However, the current shortcomings of our knowledge on the constellation of OT and PT best practices limit efforts to enhance these outcomes. Thus, if patient outcomes are going to be optimized, high quality rehabilitation must be defined and delivered. Our findings suggest that there is a core set of practices that OT and PT practitioners perceive to constitute high quality hip fracture rehabilitation. These practices have been situated within the context of an interdisciplinary team, in which all disciplines work together to achieve the patient's desired goals. This work provides critical information that can advance the development of stakeholder-driven rehabilitation guidelines and quality measures, thereby laying a foundation for future research quantifying the role of rehabilitation practitioners in hip fracture care. Further, the methodology employed in this study emphasized the importance of participatory research and qualitative grounded theory on under researched areas like this.
Implications for Rehabilitation.
This study highlights occupational and physiotherapy therapy practitioners' perspectives on the cumulative best practices that reflect high quality care, which should be delivered during hip fracture rehabilitation.
While this study was limited to two professions within the broader interdisciplinary team, consistently occupational and physiotherapy therapy practitioners situated their role and practices within the team, emphasizing that high quality care was driven by collaboration among all members of the team as well as the patient and caregivers.
Future research needs to evaluate the (1) frequency at which these practices are delivered and the relationship to patient-centered outcomes and (2) perspectives of rehabilitation practitioners working in other PAC settings, patients, caregivers, as well as the other members of the interdisciplinary PAC team.
Acknowledgments
We are grateful to all skilled nursing facilities that allowed us to be guests into their building and the rehabilitation practitioners for sharing their time and thoughts with this research team. We would also like to thank Kezia Rusli for her assistance with data management.
Declaration of interest: Dr. Leland was receiving funding from the National Center Medical Rehabilitation Research (NICHD) and the National Institute Neurological Disorders and Stroke (K12 HD055929) during the data collection phase of this study and Agency for Healthcare Research and Quality during the analysis and manuscript development phase of the study (K01 HS 022907-01A1).
Footnotes
Author Contributions: Natalie Leland contributed to study conception and design, acquisition of data, analysis and interpretation of data, and drafting the article.
Michael Lepore contributed to drafting the article, critical revision of the article, and final approval of the version to be published.
Carin Wong contributed to acquisition of data, analysis and interpretation of data, and revision of the article.
Karen Crum contributed to the study concept and design, acquisition of data, and revision of the article.
Heather Gillies contributed to analysis and interpretation of data.
Lynn Freeman and Sun Hwa Chang contributed to drafting the article and critical revision of the article.
Paul Nash contributed to drafting the article, critical revision of the article, and final approval of the version to be published.
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Guarantor of Submission: The corresponding author is the guarantor of submission.
References
- 1.Gage B, Morley M, Potelle J, Ingber M. Assistant Secretary for Planning and Evaluation (ASPE) US Department of Health and Human Services. Waltham, MA 02451: RTI International; 2011. Post-Acute Care Episodes Expanded Analytic File: Data Chart Book. [Google Scholar]
- 2.Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Med Care. 2010 Sep;48:776–84. doi: 10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leland NE, Gozalo P, Christian TJ, Bynum J, Mor V, Wetle TF, et al. An Examination of the First 30 Days After Patients are Discharged to the Community From Hip Fracture Postacute Care. Medical Care. 2015 doi: 10.1097/MLR.0000000000000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nguyen-Oghalai TU, Kuo YF, Zhang DD, Graham JE, Goodwin JS, Ottenbacher KJ. Discharge setting for patients with hip fracture: trends from 2001 to 2005. J Am Geriatr Soc. 2008;56:1063–1068. doi: 10.1111/j.1532-5415.2008.01688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaupre LA, Binder EF, Cameron ID, Jones CA, Orwig D, Sherrington C, et al. Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol. 2013 Dec;27:771–788. doi: 10.1016/j.berh.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaupre LA, Binder EF, Cameron ID, Jones CA, Orwig D, Sherrington C, et al. Maximising functional recovery following hip fracture in frail seniors. Best Practice & Research Clinical Rheumatology. 2013;27:771–788. doi: 10.1016/j.berh.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beaupre LA, Carson JL, Noveck H, Magaziner J. Recovery of Walking Ability and Return to Community Living within 60 Days of Hip Fracture Does Not Differ Between Male and Female Survivors. Journal of the American Geriatrics Society. 2015 doi: 10.1111/jgs.13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burns A, Younger J, Morris J, Baldwin R, Tarrier N, Pendleton N, et al. Outcomes following hip fracture surgery: a 2-year prospective study. Am J Geriatr Psychiatry. 2014 Aug;22:838–44. doi: 10.1016/j.jagp.2013.01.047. [DOI] [PubMed] [Google Scholar]
- 9.MEDPAC. Report to the Congress: Medicare payment policy. Medicare Payment Advisory Commission 1934-1296. 2015 [Google Scholar]
- 10.N. I. f. H. a. C. Excellence. The management of hip fracture in adults : NICE Clinical Guidelines 124. 2014 Mar; [Google Scholar]
- 11.“IMPACT Act H.R. 4994, ” ed, 2014.
- 12.Donabedian A. Evaluating the quality of medical care. The Milbank Memorial Fund Quarterly. 1966;44:166–206. [PubMed] [Google Scholar]
- 13.Blumenthal D, Jena AB. Hospital value-based purchasing. J Hosp Med. 2013 May;8:271–7. doi: 10.1002/jhm.2045. [DOI] [PubMed] [Google Scholar]
- 14.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health, and cost. Health Affairs. 2008;27:759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 15.Eldar R. A conceptual proposal for the study of the quality of rehabilitation care. Disability and Rehabilitation. 2000;22:163–169. doi: 10.1080/096382800296854. [DOI] [PubMed] [Google Scholar]
- 16.Beaupre LA, Binder EF, Cameron ID, Jones CA, Orwig D, Sherrington C, et al. Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol. 2013 Dec;27:771–88. doi: 10.1016/j.berh.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Handoll HHG, Sherrington C, Mak JCS. Interventions for improving mobility after hip fracture sugery in adults. Cochrane Database of Systematic Reviews. 2011 doi: 10.1002/14651858.CD001704.pub4. [DOI] [PubMed] [Google Scholar]
- 18.Colon-Emeric CS. Postoperative management of hip fractures: interventions associated with improved outcomes. Bonekey Rep. 2012;1:241. doi: 10.1038/bonekey.2012.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009 Feb;90:246–62. doi: 10.1016/j.apmr.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 20.Crotty M, Unroe K, Cameron ID, Miller M, Ramirez G, Couzner L. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev. 2010 doi: 10.1002/14651858.CD007624.pub3. CD007624. [DOI] [PubMed] [Google Scholar]
- 21.Titler MG, Herr K, Brooks JM, Xie XJ, Ardery G, Schilling ML, et al. Translating research into practice intervention improves management of acute pain in older hip fracture patients. Health Services Research. 2009;44:264–287. doi: 10.1111/j.1475-6773.2008.00913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Basu N, Natour M, Mounasamy V, Kates S. Geriatric hip fracture management: keys to providing a successful program. European Journal of Trauma and Emergency Surgery. 2016:1–5. doi: 10.1007/s00068-016-0685-2. [DOI] [PubMed] [Google Scholar]
- 23.Flikweert ER, Izaks GJ, Knobben BA, Stevens M, Wendt K. The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial. BMC Musculoskelet Disord. 2014;15:188. doi: 10.1186/1471-2474-15-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson H. Multi-disciplinary care of the patient with acute hip fracture: How to optimise the care for the elderly, traumatised patient at and around the time of the fracture to ensure the best short-term outcome as a foundation for the best long-term outcome. Best Pract Res Clin Rheumatol. 2013 Dec;27:717–30. doi: 10.1016/j.berh.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 25.Mak JC, Cameron ID, March LM, National H, Medical Research C. Evidence-based guidelines for the management of hip fractures in older persons: an update. Med J Aust. 2010 Jan 4;192:37–41. doi: 10.5694/j.1326-5377.2010.tb03400.x. [DOI] [PubMed] [Google Scholar]
- 26.Johnston K, Barras S, Grimmer-Somers K. Relationship between pre-discharge occupational therapy home assessment and prevalence of post-discharge falls. Journal of Evaluation in Clinical Practice. 2010;16:1333–1339. doi: 10.1111/j.1365-2753.2009.01339.x. [DOI] [PubMed] [Google Scholar]
- 27.Di Monaco M, Vallero F, De Toma E, De Lauso L, Tappero R, Cavanna A. A single home visit by an occupational therapist reduces the risk of falling after hip fracture in elderly women: a quasi-randomized controlled trial. J Rehabil Med. 2008 Jun;40:446–50. doi: 10.2340/16501977-0206. [DOI] [PubMed] [Google Scholar]
- 28.Riemen AH, Hutchison JD. The multidisciplinary management of hip fractures in older patients. Orthop Trauma. 2016 Apr;30:117–122. doi: 10.1016/j.mporth.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. N Engl J Med. 2015 Mar 5;372:897–9. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 30.Leland NE, Mallinson T, Gage B. Value-Based Payment: Ensuring Rehabiliation Priorities are Reflected in Quality Measures. Archives of Physical Medicine and Rehabilitation. 2014;95:e100. [Google Scholar]
- 31.VanLare JM, Conway PH. Value-based purchasing—national programs to move from volume to value. New England Journal of Medicine. 2012;367:292–295. doi: 10.1056/NEJMp1204939. [DOI] [PubMed] [Google Scholar]
- 32.Gozalo P, Leland NE, Christian TJ, Mor V, Teno JM. Volume Matters: Returning Home After Hip Fracture. Journal of the American Geriatrics Society. 2015 doi: 10.1111/jgs.13677. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leland NE, Gozalo P, Teno J, Mor V. Falls in Newly Admitted Nursing Home Residents: A National Study. Journal of the American Geriatrics Society. 2012;60:939–945. doi: 10.1111/j.1532-5415.2012.03931.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. The Milbank Quartery. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castle NG. Nursing home caregiver staffing levels and quality of care: a literature review. J Applied Gerontology. 2008;27:375–405. [Google Scholar]
- 36.Castle NG, Anderson RA. Caregiver staffing in nursing homes and their influence on quality of care: Using dynamic panel estimation methods. Medical care. 2011;49:545–552. doi: 10.1097/MLR.0b013e31820fbca9. [DOI] [PubMed] [Google Scholar]
- 37.Strauss AC, J . Techniques and Procedures for Developing Grounded Theory. London: Sage; 1998. Basics of Qualitative Research. [Google Scholar]
- 38.Strauss AL. Qualitative Analysis for Social Scientists. Cambridge: Cambridge University Press; 1987. [Google Scholar]
- 39.Reistetter TA, Graham JE, Deutsch A, Granger CV, Markello S, Ottenbacher KJ. Utility of functional status for classifying community versus institutional discharges after inpatient rehabilitation for stroke. Arch Phys Med Rehabil. 2010 Mar;91:345–50. doi: 10.1016/j.apmr.2009.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.U.S. Congress. Improving Medicare Post Acute Care Transformation Act. (IMPACT Act of 2014) PUBLIC LAW 113-185. 2014 doi: 10.5014/ajot.2017.715001. [H.R 4994] [DOI] [PubMed] [Google Scholar]
- 41.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166:1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 42.Naylor MD, Bowles KH, McCauley KM, Maccoy MC, Maislin G, Pauly MV, et al. High-value transitional care: translation of research into practice. J Eval Clin Pract. 2013 Oct;19:727–33. doi: 10.1111/j.1365-2753.2011.01659.x. [DOI] [PubMed] [Google Scholar]
- 43.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–684. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- 44.Muir SW, Yohannes AM. The impact of cognitive impairment on rehabilitation outcomes in elderly patients admitted with a femoral neck fracture: a systematic review. J Geriatr Phys Ther. 2009;32:24–32. doi: 10.1519/00139143-200932010-00006. [DOI] [PubMed] [Google Scholar]
- 45.Allen J, Koziak A, Buddingh S, Liang J, Buckingham J, Beaupre LA. Rehabilitation in patients with dementia following hip fracture: A systematic review. Physiotherapy Canada. 2012;64:190–201. doi: 10.3138/ptc.2011-06BH. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Buddingh S, Liang J, Allen J, Koziak A, Buckingham J, Beaupre LA. Rehabilitation for long-term care residents following hip fracture: a survey of reported rehabilitation practices and perceived barriers to delivery of care. J Geriatr Phys Ther. 2013 Jan-Mar;36:39–46. doi: 10.1519/JPT.0b013e3182569b4f. [DOI] [PubMed] [Google Scholar]
- 47.Chen L, Xiao LD, De Bellis A. First-time stroke survivors and caregivers' perceptions of being engaged in rehabilitation. J Adv Nurs. 2015 Sep 24; doi: 10.1111/jan.12819. [DOI] [PubMed] [Google Scholar]
- 48.Mackenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs, knowledge, satisfaction and competence in caring. Disabil Rehabil. 2007 Jan 30;29:111–21. doi: 10.1080/09638280600731599. [DOI] [PubMed] [Google Scholar]
- 49.Lawler K, Taylor NF, Shields N. Involving family members in physiotherapy for older people transitioning from hospital to the community: a qualitative analysis. Disabil Rehabil. 2015;37:2061–9. doi: 10.3109/09638288.2014.996673. [DOI] [PubMed] [Google Scholar]
- 50.Dowswell G, Lawler J, Dowswell T, Young J, Forster A, Hearn J. Investigating recovery from stroke: a qualitative study. Journal of Clinical Nursing. 2000;9:507–515. doi: 10.1046/j.1365-2702.2000.00411.x. [DOI] [PubMed] [Google Scholar]
- 51.Sanders MJ, Van Oss T. Using daily routines to promote medication adherence in older adults. Am J Occup Ther. 2013;67:91–9. doi: 10.5014/ajot.2013.005033. [DOI] [PubMed] [Google Scholar]
- 52.Association AOT. Role of occupational therapy in assessing functional cognition. 2016 [Google Scholar]
- 53.Mahoney JE, Palta M, Johnson J, Jalaluddin M, Gray S, Park S, et al. Temporal association between hospitalization and rate of falls after discharge. Arch Intern Med. 2000;160:2788–2795. doi: 10.1001/archinte.160.18.2788. [DOI] [PubMed] [Google Scholar]
- 54.Mahoney JE, Sager M, Dunham NC, Johnson J. Risk of falls after hospital discharge. J Am Geriatr Soc. 1994;42:269–274. doi: 10.1111/j.1532-5415.1994.tb01750.x. [DOI] [PubMed] [Google Scholar]
- 55.Luger MF, Muller S, Kammerlander C, Gosch M, Luger TJ. Predictors of Postoperative Cognitive Decline in Very Old Patients With Hip Fracture: A Retrospective Analysis. Geriatr Orthop Surg Rehabil. 2014 Dec;5:165–72. doi: 10.1177/2151458514548577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pidemunt G, Pérez-Prieto D, Ginés-Cespedosa A, Suils-Ramon J, Puig-Verdié L, Cáceres E, et al. Persistent pain and depression after hip fracture strongly correlate with poor outcomes. European Orthopaedics and Traumatology. 2015;6:399–404. 2015/12/01. [Google Scholar]
- 57.Feldt KS, Oh HL. Pain and hip fracture outcomes for older adults. Orthopaedic Nursing. 2000;19 doi: 10.1097/00006416-200019060-00008. [DOI] [PubMed] [Google Scholar]
- 58.Herrick C, Steger-May K, Sinacore DR, Brown M, Schechtman KB, Binder EF. Persistent pain in frail older adults after hip fracture repair. J Am Geriatr Soc. 2004;52:2062–2068. doi: 10.1111/j.1532-5415.2004.52566.x. [DOI] [PubMed] [Google Scholar]
- 59.Abou-Setta AM, Beaupre LA, Rashiq S, Dryden DM, Hamm MP, Sadowski CA, et al. Comparative effectiveness of pain management interventions for hip fracture: a systematic review. Ann Intern Med. 2011 Aug 16;155:234–45. doi: 10.7326/0003-4819-155-4-201108160-00346. [DOI] [PubMed] [Google Scholar]
- 60.Pellino TA, Gordon DB, Engelke ZK, Busse KL, Collins MA, Silver CE, et al. Use of nonpharmacologic interventions for pain and anxiety after total hip and total knee arthroplasty. Orthop Nurs. 2005 May-Jun;24:182–90. doi: 10.1097/00006416-200505000-00005. quiz 191-2. [DOI] [PubMed] [Google Scholar]
- 61.Haggqvist B, Stenvall M, Fjellman-Wiklund A, Westerberg K, Lundin-Olsson L. “The balancing act”--licensed practical nurse experiences of falls and fall prevention: a qualitative study. BMC Geriatr. 2012;12:62. doi: 10.1186/1471-2318-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wood JP, Connelly DM, Maly MR. ‘Getting back to real living’: a qualitative study of the process of community reintegration after stroke. Clinical Rehabilitation. 2010;24:1045–1056. doi: 10.1177/0269215510375901. [DOI] [PubMed] [Google Scholar]


