Introduction
Obesity and cigarette smoking are two of the main causes of premature death and disability in the United States (US) and are important health issues that affect adolescents who can benefit from interventions early in life. Smoking harms nearly every organ of the body and is causally linked to many chronic diseases including cancer and cardiovascular disease [1]. Type 2 diabetes rates have been steadily increasing with the rise in childhood obesity [2]. While rates of cigarette smoking among adolescents have been steadily declining since 1999, adolescent obesity rates have quadrupled since the 1980s [3,4]. The National Health and Nutrition Examination Survey (2013–2014) found that approximately 21 percent of youth ages 12–19 years in the United States are obese; a prevalence rate 3-fold higher than two decades ago [4]. A greater percent of adult women are obese than men (38.3% among women, 34.3% among men), but sex differences in adolescents are small [4,5].
Adolescence is a crucial period in which health behaviors are established that continue into adulthood [6]. Cigarette smoking is initiated primarily during adolescence; approximately eighty percent of adult smokers begin smoking before the age of 18 [3]. A longitudinal study by Chen and colleagues found that smoking rates, as measured by the number of days smoked in the last 30 days and the average number of cigarettes smoked, are higher among females during the ages of 11–14, with males having higher rates at ages 18 and older [7]. Research indicates that early health behaviors related to obesity such as physical activity levels and food preference tend to track from childhood into early adulthood, but the relationship of BMI and smoking longitudinally is understudied [8].
The 2012 Surgeon General’s report indicates that the average BMI for smokers under age 18 is typically the same or higher than nonsmokers, but there is not an established relationship between smoking and body weight in children and young adults. However, differences in weight were found between smokers and nonsmokers among those ages 35 and older, which may be attributed to the relatively lower weight gain among smokers over time [3]. The Surgeon General’s report concluded that “the evidence is suggestive but not sufficient to conclude that smoking by adolescents and young adults is not associated with significant weight loss, contrary to young people’s beliefs” [3]. Generally, cross-sectional research indicates that adult current smokers have a lower body mass index (BMI) than never and former smokers [9,10], which may be in part due to the effects of nicotine on metabolism, as biologically, nicotine serves as an appetite suppressant and mechanistically is related to weight control by reducing hunger and increasing satiety [11]. Research among a cohort of adult men in the United Kingdom found that smokers had a lower BMI than nonsmokers but over time, former smokers eventually reverted back to BMI levels similar to nonsmokers [12]. There may be sex differences to consider as research indicates that smoking initiation among females is associated with overweight status and trying to lose weight but not among males [13]. These sex differences in initiation may influence the relationship of smoking and body weight in young adulthood.
A growing body of literature has addressed the association of smoking and obesity among adolescents and young adults, but results have been mixed [12,14–17]. A Finnish study found that smoking during adolescence increased adult obesity risk, but another study found no significant reductions in body weight among United States adolescents three years following smoking initiation [15,17]. Despite extensive research addressing youth obesity and smoking separately [3], to our knowledge, only two studies have looked at the relationship of these two issues from adolescence into young adulthood longitudinally in the US [18,19]. One longitudinal research study utilizing a community-based sample of youth in upstate New York indicated that youth smoking is related to lower BMI in young adulthood [18]. However, another study using a nationally representative sample of youth found that overweight status during adolescence was associated with greater levels of smoking in young adulthood [19]. The first study used a convenience sample, whereas the second study, which used nationally representative data, looked at obesity over time and the relationship to smoking in young adulthood, rather than smoking over time. The conflicting longitudinal evidence from these studies highlights a potentially interesting and important relationship between smoking during adolescence and body weight in young adulthood that needs to be further examined. The current study helps fill this gap in the literature by addressing smoking over time and the relationship to BMI in young adulthood and is important for understanding the potential interplay between these two pressing health issues and their associated health risks.
This study examines the relationship between cigarette smoking and weight status in a large nationally representative sample of youth as they develop into young adults. The purpose of the current study is to examine the association of smoking behavior trajectories (early establishers, late establishers, former smokers, nonsmokers), beginning in adolescence with BMI in young adulthood. Consistent with prior research in this area [18], we hypothesize that youth who report smoking during adolescence will have a lower BMI as young adults than nonsmokers. In addition, we hypothesize that longer life-course exposure to smoking will be associated with lower BMI, given the impact of nicotine on weight status. Given differences in smoking initiation and rates [7,13], and BMI by sex [20], we also hypothesize that sex differences in these relationships will be found.
Methods
Study Design
This research utilizes data from the National Longitudinal Study of Adolescent to Adult Health (Add Health) [21]. Add Health is the largest and most comprehensive longitudinal study of adolescents into young adulthood in the US [22]. Wave I participants were in grades 7–12 (1995–1996), with subsequent follow up in 1996 (Wave II), 2001–2002 (Wave III) and 2007–2008 (Wave IV). Add Health collected data from 80 high schools and 52 middle schools across the country to be representative of all US schools in regards to region of the country, urbanicity, size and type of school, and ethnicity [22]. Further details regarding the study are provided elsewhere [22]. This study was deemed exempt by the NIH Office of Human Subjects Research Protections.
Participants
In Wave I, respondents (n=20,745) were questioned in both the home and schools. Respondents were questioned in the home in Wave II (n=14,738), Wave III (n=15,197), and Wave IV (n=15,701). Participants who reported being pregnant (n=518) or identified as active duty military (n=350) in Wave IV were excluded from the analyses. Individuals providing current cigarette smoking status at only one wave were excluded as it was not possible to create a trajectory based on data from only one time point (n=1606). The study sample (n=13,361) was generated after accounting for missing data using listwise deletion.
Measures
Smoking Measures
Current Cigarette Smoking Status
Cigarette smoking was measured by the question “During the past 30 days, on how many days did you smoke cigarettes?” Respondents with greater than zero days were categorized as current smokers for that wave; respondents with zero days were categorized as nonsmokers for that wave.
Early Initiation
A variable for early initiation was created based on responses to items in Waves I and II. In Wave I, participants were asked, “How old were you when you smoked a whole cigarette for the first time?”. Those who reported first smoking before the age of 14 were classified as early initiators. Respondents who first reported smoking at Wave II, and were younger than 14 at that time, were also coded as early initiators.
Smoking Trajectories
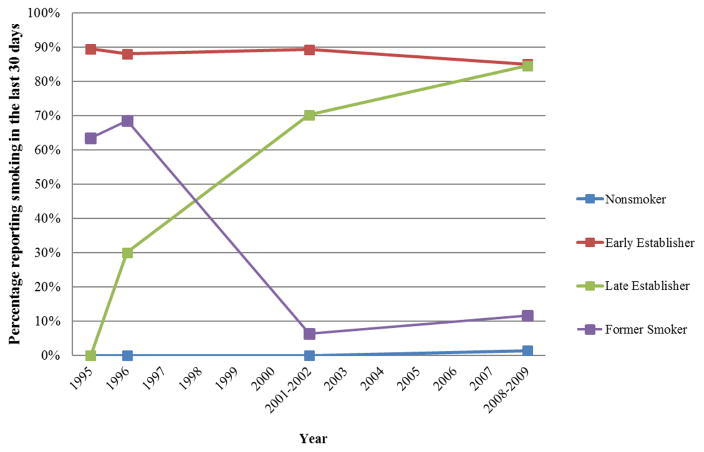
To characterize patterns of smoking across the life course, a series of repeated-measures latent class analyses (RMLCA) were conducted using current cigarette smoking status at all four waves and age of initiation in order to produce four trajectories of cigarette use based on the lowest Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) values [23]. A four class solution was found to have the lowest AIC (62.38) and BIC (245.02) values. These classes were labeled as: 1) early establishers, 2) late establishers, 3) former smokers, and 4) nonsmoker (see Figure 1). Most respondents who were identified by the RMCLA in the early establishers trajectory reported smoking in Waves I–IV, and started before the age of 14. Those identified in the late establisher category were likely to report smoking after Wave I, and after the age of 14. Most of the respondents identified as former smokers reported smoking prior to Wave IV, but were no longer smoking by Wave IV, with the exception of 276 participants who responded to smoking in Wave IV. Finally, those identified in the nonsmoker category had a low probability of reporting smoking at Waves 1–IV. These classes of trajectories served as the primary independent variable for this study and are shown in Figure 1.
Figure 1. Developmental trajectories of cigarette smoking from adolescence into young adulthood and likelihood of smoking at each wave*.
*The nonsmoker category created by the RMCLA included 694 participants who responded yes to smoking in Wave IV only.
Weight Status
The main outcome of BMI (kg/m2) at Wave IV was calculated using self-reported weight and height. Waist circumference (WC) at Wave IV was measured in centimeters (cm) by interviewers at the superior border of the iliac crest, providing a secondary measure of weight status [24]. To adjust for the initial weight status in adolescence, BMI was calculated using self-reported weight and height at Wave I. BMI at Waves II and III was also calculated for cross-sectional analyses.
Demographics
Covariates included from Wave I include self-reported sex, race/ethnicity, and parental household income. Racial/ethnic categories based on Add Health defined categories included: Hispanic, Non-Hispanic White, Non-Hispanic Black, Asian, and Other [25]. Four categories (less than $25,000, $25,000 to less than $50,000, $50,000 to less than $75,000, and more than $75,000) were created for parental household income in line with previous literature [26]. Missing data for household income was coded as a separate category; 22% of the sample had not reported household income. Young adult educational attainment at Wave IV was also included as a covariate and was categorized as: less than high school, high school, some college/technical school, college, and graduate/professional school.
Data analysis
All data were weighted according to procedures outlined in Add Health documents [27]. Univariate analyses were conducted to produce overall and sex stratified sample characteristics. Weighted cross-sectional bivariate analyses for BMI at each wave using trajectories as the independent variable predicted BMI at each wave, providing information regarding differences in BMI at various stages of development by smoking trajectory. Post-hoc pairwise comparisons assessed differences in mean BMI at each wave by smoking trajectory. Stepwise linear regression analysis was used to assess the relationship between smoking trajectory and BMI at Wave IV. A final multivariable linear regression model using BMI at Wave IV adjusted for demographic covariates. All data analyses were conducted using Stata 14.
Results
Demographic and sample characteristics are shown in Table 1. Using weighed data, our sample was reflective of young adults nationally during this time period, with approximately 49% male, and 70% Non-Hispanic White. At Wave I, mean age was 15.5, and average BMI was 22.5 with no statistically significant differences between males and females. At Wave IV, mean age was 28.4, and average BMI was 28.2, with no statistically significant differences between males and females. Most participants reported more than a secondary school education, with at least some college or technical school (43%), completing college (20%), or having a graduate/professional degree (11%). Over 44% of the participants in the analytic sample were identified as nonsmokers. An additional 23% were identified as early establishers, 21% were identified as late establishers, and 12% were identified as former smokers.
Table 1.
Sample characteristics, weighted (n=13361)*
| Variable Name | Total sample N (%) or mean (SD) |
Male N (%) or mean (SD) |
Female N (%) or mean (SD) |
|---|---|---|---|
| Smoking trajectory | |||
| Nonsmoker | 6404 (44%) | 2810 (21%) | 3594 (23%) |
| Early establisher | 2802 (23%) | 1334 (11%) | 1468 (12%) |
| Late establisher | 2514 (21%) | 1619 (14%) | 895 (7%) |
| Former Smoker | 1641 (12%) | 724 (5%) | 917 (7%) |
|
| |||
| BMI (avg.) (Wave I) | 22.53 (4.56) | 22.76 (4.57) | 22.28 (4.53) |
|
| |||
| BMI (avg.) (Wave IV) | 28.18 (6.82) | 28.27 (5.90) | 28.09 (7.77) |
| Waist Circumference (avg.) (Wave IV) (cm) | 98.01(17.13) | 99.75 (15.16) | 96.10 (18.98) |
|
| |||
| Age (Wave I) | 15.47 (1.80) | 15.56 (1.78) | 15.38 (1.80) |
| Age (Wave IV) | 28.40 (0.11) | 28.50 (0.11) | 28.30 (0.11) |
|
| |||
| Race/Ethnicity | |||
| Non-Hispanic White | 7538 (70%) | 3711(36%) | 3827 (35%) |
| Non-Hispanic Black/African American | 2656 (14%) | 1194 (7%) | 1462 (7%) |
| Hispanic/Latino | 2127 (11%) | 1047 (6%) | 1080 (5%) |
| Asian | 779 (3%) | 409 (2%) | 370 (1%) |
| Other | 261 (2%) | 126 (1%) | 135 (1%) |
|
| |||
| Parental household income (Wave I) | |||
| Less than $25,000 | 2872 (22%) | 1364 (11%) | 1508 (11%) |
| $25,000 to less than $50,000 | 3413 (27%) | 1703(14%) | 1710 (13%) |
| $50,000 to less than $75,000 | 2361 (18%) | 1192 (10%) | 1169 (9%) |
| $75,000 to less than $100,000 | 1487 (11%) | 740 (6%) | 747 (5%) |
| Missing | 3228 (22%) | 1488 (11%) | 1740 (11%) |
|
| |||
| Young adult educational attainment (Wave IV) | |||
| Less than high school | 1039 (9%) | 626 (6%) | 413 (3%) |
| High School | 2150 (17%) | 1241 (11%) | 909 (6%) |
| Some college/technical school | 5839 (43%) | 2769 (21%) | 3070 (21%) |
| College | 2672 (20%) | 1227 (10%) | 1445 (10%) |
| Grad/professional school | 1661 (11%) | 624 (5%) | 1037 (7%) |
Excludes women who are pregnant at Wave IV and individuals on active military duty at Wave IV. Waist circumference was missing for an additional n=119 participants.
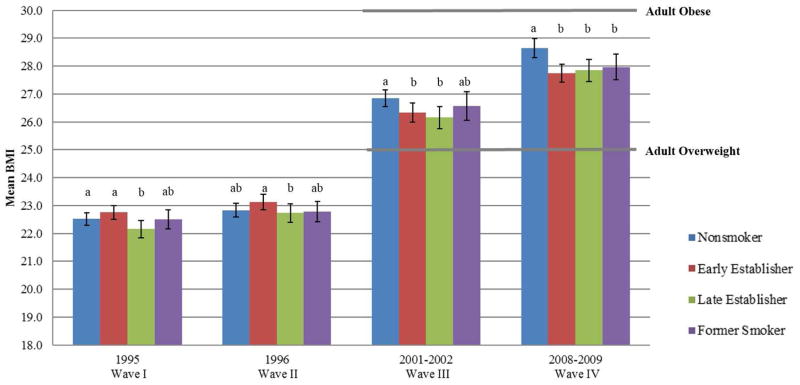
The bivariate relationship of mean BMI with smoking trajectory at each wave is displayed in Figure 2. For all trajectories, mean BMI increased over time from Waves I–IV. In Wave I, late establishers had a statistically significantly lower BMI than nonsmokers and early establishers. In Wave II, late establishers had statistically significantly lower BMI than early establishers, but did not differ from nonsmokers. In Wave III, both early and late establishers had a statistically significant lower BMI than nonsmokers. By Wave IV, all participants in smoking trajectories, including former, had a statistically significant lower BMI than nonsmokers.
Figure 2. Bivariate and pairwise comparisons of BMI from Waves I–IV by smoking trajectory*.
*Trajectories sharing a letter within each wave in the group label are not statistically different (p<0.05).
Multivariable linear regression predicting Wave IV BMI was conducted, adjusting for demographic covariates (Table 2). There was a significant association of smoking trajectory with BMI in Wave IV in adjusted models for all smoking trajectories compared to nonsmokers: early establishers had a lower BMI by 1.27 (CI: −1.56, −0.98), followed by late establishers (β= −0.84; CI: −1.16, −0.52), and former smokers (β= −0.63; CI: −0.93, −0.34). Males reported a lower BMI (β= −0.28; CI: −0.53, −0.03) than females. Greater age was associated with a lower BMI (β= −0.28; CI: −0.35, −0.20). Baseline BMI was positively associated with young adult BMI (β= 1.07; CI: 1.03, 1.10). Participants with higher parental incomes (greater than $50,000) were more likely to have a lower BMI than those in the lowest income category. Those reporting some college or technical school had a higher BMI (β= 0.51; CI: 0.08, 0.95), than those reporting less than high school, but respondents with a college degree (β= −0.61; CI: −1.10, −0.11), or graduate/professional degree (β= −1.09; CI: −1.62, −0.56) reported statistically significantly lower BMIs than those reporting less than high school. Differences in BMI also emerged between groups by race/ethnicity, as seen in Table 2.
Table 2.
Regression of BMI at Wave IV (2008–2009) based on latent class analysis smoking trajectory (n=13361)*
| Full Multivariate Model | Male | Female | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| β* | (95% Confidence Interval) | β* | (95% Confidence Interval) | β* | (95% Confidence Interval) | |
| Smoking trajectory | ||||||
| Nonsmokers | Reference | Reference | Reference | |||
| Early establishers | −1.27*** | (−1.56, −0.98) | −1.26*** | (−1.67, −0.86) | −1.31*** | (−1.71, −0.88) |
| Late establishers | −0.84*** | (−1.16, −0.52) | −1.02*** | (−1.40, −0.65) | −0.49 | (−1.03, 0.06) |
| Former smoker | −0.63*** | (−0.93, −0.34) | −0.58** | (−1.01, −0.15) | −0.63** | (−1.08, −0.19) |
|
| ||||||
| BMI (Wave I) | 1.07*** | (1.03, 1.10) | 0.96*** | (0.92, 1.00) | 1.19*** | (1.14, 1.24) |
|
| ||||||
| Sex | ||||||
| Female | Reference | ----- | ----- | ----- | ----- | |
| Male | −0.28* | (−0.53, −0.03) | ----- | ----- | ----- | ----- |
|
| ||||||
| Age (Wave IV) | −0.28*** | (−0.35, −0.20) | −0.31*** | (-0.40, -0.21) | −0.23*** | (−0.34, −0.13) |
|
| ||||||
| Race/Ethnicity | ||||||
| White | Reference | Reference | Reference | |||
| Black/African American | 0.28 | (−0.08, 0.64) | −0.16 | (−0.62, 0.29) | 0.59* | (0.10, 1.09) |
| Hispanic/Latino | 0.07 | (−0.33, 0.48) | 0.32 | (−0.21, 0.85) | −0.31 | (−0.94, 0.32) |
| Asian | −0.78*** | (−1.19, −0.37) | −0.10 | (−0.68, 0.49) | −1.47*** | (−2.09, −0.85) |
| Other | 0.27 | (−0.61, 1.14) | 1.12 | (−0.11, 2.34) | −0.50 | (−1.52, 0.53) |
|
| ||||||
| Parental income (Wave I) | ||||||
| Household income less than $25,000 | Reference | Reference | Reference | |||
| $25,000 to less than $50,000 | −0.23 | (−0.60, 0.14) | −0.57* | (−1.03, −0.11) | 0.25 | (−0.27, 0.78) |
| $50,000 to less than $75,000 | −0.46* | (−0.82, −0.10) | −0.50* | (−0.95, −0.05) | −0.40 | (−0.92, 0.12) |
| More than $75,000 | −0.63** | (−1.03, −0.23) | −0.54 | (−1.11, 0.03) | −0.71** | (−1.25, −0.16) |
|
| ||||||
| Young adult educational attainment (Wave IV) | ||||||
| Less than high school | Reference | Reference | Reference | |||
| High School | 0.38 | (−0.04, 0.80) | 0.09 | (−0.45, 0.63) | 0.72 | (−0.09, 1.52) |
| Some college/technical school | 0.51* | (0.08, 0.95) | 0.45 | (−0.07, 0.97) | 0.45 | (−0.28, 1.19) |
| College | −0.61* | (−1.10, −0.11) | −0.39 | (−0.00, 0.21) | −0.96** | (−1.76, −0.15) |
| Grad/professional school | −1.09*** | (−1.62, −0.56) | −0.58 | (−1.23, 0.07) | −1.50*** | (−2.32, −0.69) |
Adjusted models controlling for age, race/ethnicity, parental income, and adolescent BMI at Wave I and educational status at Wave IV. The full multivariate model also controls for sex. Excludes women who are pregnant at Wave IV and individuals on active military duty at Wave IV.
p<0.05,
p<0.01,
p<0.001
In order to further test the relationship of smoking trajectories to weight status, waist circumference was used as a secondary outcome measure (Table 3). In the full model controlling for demographic covariates, early establishers reported a 2.20 cm smaller WC than nonsmokers (CI: −3.05, −1.36). Waist circumference was also lower among late establishers (β=−1.08; CI: −2.06, −0.10) and former smokers (β =−1.05; CI: −1.85, −0.24) compared to nonsmokers. Participants with higher parental incomes (greater than $50,000) were more likely to have a smaller WC than those in the lowest income category. Greater educational attainment was associated with a significantly lower WC for both college (β= −2.78; CI: −4.09, −1.47) and graduate/professional school (β= −3.83; CI: −5.24, −2.42). Sex stratified models further revealed differences by groups by race/ethnicity and educational attainment (Table 3).
Table 3.
Regression of Waist Circumference (cm) at Wave IV (2008–2009) based on latent class analysis smoking trajectory (n=13242)*
| Full Multivariate Model | Male | Female | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| β* | (95% Confidence Interval)* | β* | (95% Confidence Interval)* | β* | (95% Confidence Interval)* | |
| Smoking trajectory | ||||||
| Nonsmokers | Reference | Reference | Reference | |||
| Early establishers | −2.20*** | (−3.05, −1.36) | −2.35*** | (−3.55, −1.17) | −2.13*** | (−3.31, −0.94) |
| Late establishers | −1.08* | (−2.06, −0.10) | −1.67** | (−2.73, −0.61) | 0.05 | (−1.66, −0.77) |
| Former smoker | −1.05* | (−1.85, −0.24) | −0.94 | (−2.25, 0.37) | −1.04 | (−2.16, 0.08) |
|
| ||||||
| BMI (Wave I) | 2.32*** | (2.23, 2.41) | 2.13*** | (2.02, 2.24) | 2.53*** | (2.41, 2.66) |
|
| ||||||
| Sex | ||||||
| Female | Reference | --- | --- | --- | --- | --- |
| Male | 2.50*** | (1.79, 3.20) | --- | --- | --- | --- |
|
| ||||||
| Age (Wave IV) | −0.56*** | (−0.76, −0.36) | −0.62*** | (−0.86, −0.37) | −0.48** | (−0.79, −0.17) |
|
| ||||||
| Race/Ethnicity | ||||||
| White | Reference | --- | Reference | --- | Reference | --- |
| Black/African American | −1.02* | (−2.00, −0.04) | −1.83** | (−3.20, −0.47) | −0.31 | (−1.73, 1.11) |
| Hispanic/Latino | −1.30* | (−2.34, −0.25) | 0.07 | (−1.29, 1.43) | −2.87** | (−4.67, −1.29) |
| Asian | −4.57*** | (−6.06, −3.07) | −4.41*** | (−6.27, −2.54) | −4.58*** | (−6.69, −2.48) |
| Other | −1.74 | (−4.18, 0.70) | 0.62 | (−3.03, 4.28) | −3.74** | (−6.30, −1.19) |
|
| ||||||
| Parental income (Wave I) | ||||||
| Household income less than $25,000 | Reference | --- | Reference | --- | Reference | --- |
| $25,000 to less than $50,000 | −0.27 | (−1.30, 0.75) | −0.88 | (−2.25, 0.48) | 0.76 | (−0.67, 2.19) |
| $50,000 to less than $75,000 | −1.11* | (−2.11, −0.11) | −0.80 | (−2.08, 0.48) | −1.38 | (−3.01, 0.25) |
| More than $75,000 | −0.69 | (−1.87, 0.49) | −0.11 | (−1.75, 1.52) | −1.26 | (−3.08, 0.56) |
|
| ||||||
| Young adult educational attainment (Wave IV) | ||||||
| Less than high school | Reference | --- | Reference | --- | Reference | --- |
| High School | 0.62 | (−0.68, 1.91) | −0.01 | (−1.57, 1.56) | 1.49 | (−0.77, 3.75) |
| Some college/technical school | 0.50 | (−0.69, 1.68) | 0.87 | (−0.61, 2.34) | −0.46 | (−2.42, 1.49) |
| College | −2.78*** | (−4.09, −1.47) | −1.44 | (−3.09, 0.22) | −4.67*** | (−6.75, −2.59) |
| Grad/professional school | −3.83*** | (−5.24, −2.42) | −1.71 | (−3.66, 0.24) | −5.87*** | (−7.98, −3.77) |
Adjusted models controlling for age, race/ethnicity, parental income, and adolescent BMI at Wave I and educational status at Wave IV. The full multivariate model also controls for sex. Excludes women who are pregnant at Wave IV and individuals on active military duty at Wave IV.
p<0.05,
p<0.01,
p<0.001
Discussion
In a nationally representative cohort followed from adolescence into young adulthood, we found that the mean BMI increased over time as a whole, for all trajectories, regardless of current cigarette smoking status, which is consistent with the national secular trends in obesity [20]. We found a significantly lower BMI at Wave IV among all smoking trajectories compared to nonsmokers when controlling for sex, baseline BMI, age, race/ethnicity, parental income, and educational status at Wave IV; however, the magnitude of this difference was small. This relationship was also found for WC in young adulthood when adjusting for covariates. We found support for our hypothesis that there is a significant longitudinal relationship of smoking through adolescence into young adulthood on young adult weight status, such that participants in smoking trajectories had a lower BMI in young adulthood than nonsmokers. Our findings are consistent with previous research by Brook et al. [18], but conflict with research by Lanza et al. [19], which may be a result of the differing approaches and research focuses. Similar to our approach, Brook at al. examined smoking trajectories and the association to weight status in young adulthood [18]; whereas, Lanza et al. assessed obesity as a predictor of latent classes and the association with smoking in young adulthood [19]. Our study extends findings from Brook et al. to a nationally representative sample.
Smoking and obesity are the leading causes of cancer and other serious health problems, and together may be additive or synergistic in their negative health effects. Research shows that tobacco smoke is a strong risk factor for cancer. Lung cancer is the leading cause of cancer mortality in the U.S., with an estimated 158,080 deaths expected to occur in 2016; approximately 80% of lung cancer deaths are attributable to smoking. Other types of cancer, including cancers of the esophagus, stomach, pancreas, kidney, bladder and colon/rectum, are also related to smoking [28]. For certain cancers such as lung, liver, and pancreatic, excess body weight and smoking have a synergistic effect, causing a greater risk than of the individual risk factors [29]. Approximately 500,000 additional cases of cancer in the United States are projected by 2030 as a result of the rise in obesity rates [30]. Research indicates that even minor reductions in BMI can be beneficial for overall health. For example, among overweight and obese individuals with type 2 diabetes, a small (5–10%) reduction of their body weight can lead to improvements in glycemic control, blood pressure, and cholesterol levels [31]. For a male of average height (69.3 inches) and weight (195.5 lbs.) in the US [32], a 1 point reduction in BMI is equivalent to 7 lbs. Research indicates that a reduction 1% of weight (equivalent to 2.2 lbs. for an adult of average age) across the US population would prevent 73,000–127,000 new cases of cancer [30]. Although individuals with smoking histories had slightly lower BMIs and waist circumference at Wave IV than nonsmokers, BMI for each trajectory was well above the threshold for being overweight and the negligible differences in BMI between trajectories are unlikely to produce any health benefits, especially considering smoking history. The risk of smoking and obesity on health outcomes need to be collectively weighed, while understanding that potential synergistic or additive risks may lead to a greater burden of disease.
This study found differences in the relationship of smoking and weight status (BMI & WC) for men and women. Men in all smoking trajectories had a lower BMI than nonsmokers. Women had similar findings, however late establishers did not have a significantly lower BMI than nonsmokers. Men who were early and late establishers had a smaller WC compared to nonsmokers, however only women who were early establishers had a lower WC compared to nonsmokers. Given sex differences for late establishers, more research is needed to explain why these differences emerged. Female late establishers may be struggling with weight reduction, as indicated in the literature [33]. Additionally, smoking initiation in adolescents has been related to female adolescents who reported daily dieting, and dieting is more of a concern for females adolescents than males [34]. However, more research is needed to confirm this hypothesis among our sample and to better understand women who are late establishers.
There are some limitations with this study. First, the Add Health study did not include all variables of interest to us and some measures were not included at each wave. Several measures, including current cigarette smoking status, were based on self-reported data; cotinine levels or carbon monoxide expulsion levels, would have strengthened these analyses. However, Add Health ensured confidentiality, thus increasing accuracy on self-reported measures [35]. Additionally, there may be selection bias due to attrition; however, this is unlikely given the large sample size and nationally weighted analyses. The Wave IV response rate (80.3%) is comparable to other national studies and non-response bias was minimal in Add Health [35]. Furthermore, this study utilizes one measure of cigarette smoking at each time point; duration and intensity of smoking are not captured in these analyses. Waist circumference was not measured in Wave I, so BMI was used as a proxy to control for baseline weight status in the adjusted WC model. Additionally, since cigarette smoking status was only measured at four time points, trajectory patterns may not account for changes to smoking status between waves. Similarly, weight status fluctuations are not captured in these analyses. Examining potential contextual and neighborhood variables that may be related to both weight status and smoking, such as aspects of the built environment related to the retail environment around schools, which may impact both smoking initiation and weight status among youth, would have strengthened our understanding [36].
Despite these limitations, our study adds significantly to the literature. First, this study builds on previous literature by characterizing the relationship of developmental trajectories of cigarette smoking to weight status from adolescence through young adulthood in a nationally representative cohort [18]. The longitudinal nature of the study also allows for a more nuanced understanding of smoking behaviors across the lifespan from adolescence through young adulthood, building on previous cross-sectional studies assessing the association of smoking and weight status at various stages of the lifecourse [3]. Consistent findings utilizing both calculated BMI based on self-reported data and measured WC as endpoints further strengthen this study, since waist circumference was measured and not self-reported, which indicates that the self-reported data used to generate BMI are likely to be valid measures, and the relationship found in this study holds, regardless of the measure used for weight status.
Overall, our results have implications for future research and interventions concerning cigarette smoking and both weight status and weight control in adolescents and young adults. We see that smoking does not protect from obesity, as the population level weight status increased for all trajectory groups. In order to better understand the relationship of smoking status and weight status, it is important to further research related health behaviors, including various smoking behaviors, physical activity, and eating behaviors, as well as sociodemographic characteristics. The variability in these individual level characteristics can provide insight, and further advance the field of addressing multiple health behaviors. Furthermore, research has found that unhealthy behaviors tend to cluster together, increasing the risk of both obesity and tobacco related cancers [37]. Policy level influences also need to be considered, given the impact of the tobacco and food industries on health [38]. Interventions at the policy and individual level need to focus especially on youth and the transition period to young adulthood, and address multiple behaviors of smoking and weight status related risk such as physical activity and eating behaviors simultaneously in order to reduce smoking initiation and encourage healthy weight management. Efforts to assist adolescents to never start smoking and avoid weight gain are both critical to reducing the negative public health outcomes. Additionally, clinical implications need to be considered regarding the relationship of smoking and weight status that was found in this study and should utilize the gold standard cessation and obesity reduction guidelines concurrently [39,40]. Since our study finds that young adults in all trajectories were on average overweight, clinicians need to better advise all overweight patients to reduce their weight status regardless of smoking status to improve population health. Both tobacco use and obesity need to be studied concurrently in order to better understand potential additive and/or synergistic effects among youth and young adults in the US.
Implications and Contribution Summary Statement.
Weight gain throughout adolescence into young adulthood is prevalent across all smoking behavior trajectories. Smoking throughout adolescence has a modest association with lowered weight gain into young adulthood. These results have implications for both research and interventions to help youth and young adults avoid both smoking and obesity.
Acknowledgments
Minal Patel is currently a Cancer Prevention Postdoctoral Fellow at the National Cancer Institute. The opinions expressed in this manuscript are the authors’ own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Abbreviations
- Add Health
National Longitudinal Study of Adolescent to Adult Health
- AIC
Akaike Information Criterion
- BIC
Bayesian Information Criterion
- BMI
body mass index
- cm
centimeters
- RMLCA
repeated-measures latent class analyses
- US
United States
- WC
Waist circumference
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.US Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. p. 17. [Google Scholar]
- 2.Goran MI, Ball GD, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. The Journal of Clinical Endocrinology & Metabolism. 2003;88(4):1417–1427. doi: 10.1210/jc.2002-021442. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. p. 2. [Google Scholar]
- 4.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutrition Journal. 2008;7(1):1. doi: 10.1186/1475-2891-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance—United States, 2013. MMWR. 2014;63(Suppl 4):1–168. [PubMed] [Google Scholar]
- 7.Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. Journal of Adolescent Health. 2012;50(2):154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelder SH, Perry CL, Klepp K-I, Lytle LL. Longitudinal tracking of adolescent smoking, physical activity, and food choice behaviors. American Journal of Public Health. 1994;84(7):1121–1126. doi: 10.2105/ajph.84.7.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plurphanswat N, Rodu B. The association of smoking and demographic characteristics on body mass index and obesity among adults in the US, 1999–2012. BMC Obesity. 2014;1(1):1. doi: 10.1186/s40608-014-0018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sneve M, Jorde R. Cross-sectional study on the relationship between body mass index and smoking, and longitudinal changes in body mass index in relation to change in smoking status: The Tromsø Study. Scandinavian Journal of Public Health. 2008;36(4):397–407. doi: 10.1177/1403494807088453. [DOI] [PubMed] [Google Scholar]
- 11.Audrain-McGovern J, Benowitz N. Cigarette smoking, nicotine, and body weight. Clinical Pharmacology & Therapeutics. 2011;90(1):164–168. doi: 10.1038/clpt.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munafò MR, Tilling K, Ben-Shlomo Y. Smoking status and body mass index: a longitudinal study. Nicotine & Tobacco Research. 2009;11(6):765–771. doi: 10.1093/ntr/ntp062. [DOI] [PubMed] [Google Scholar]
- 13.Cawley J, Markowitz S, Tauras J. Lighting up and slimming down: the effects of body weight and cigarette prices on adolescent smoking initiation. Journal of health economics. 2004;23(2):293–311. doi: 10.1016/j.jhealeco.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Fidler JA, West R, Van Jaarsveld CH, Jarvis MJ, Wardle J. Does smoking in adolescence affect body mass index, waist or height? Findings from a longitudinal study. Addiction. 2007;102(9):1493–1501. doi: 10.1111/j.1360-0443.2007.01910.x. [DOI] [PubMed] [Google Scholar]
- 15.Saarni SE, Pietiläinen K, Kantonen S, Rissanen A, Kaprio J. Association of smoking in adolescence with abdominal obesity in adulthood: a follow-up study of 5 birth cohorts of Finnish twins. American Journal of Public Health. 2009;99(2):348–354. doi: 10.2105/AJPH.2007.123851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stice E, Martinez EE. Cigarette smoking prospectively predicts retarded physical growth among female adolescents. Journal of Adolescent Health. 2005;37(5):363–370. doi: 10.1016/j.jadohealth.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Cooper TV, Klesges RC, Robinson LA, Zbikowski SM. A prospective evaluation of the relationships between smoking dosage and body mass index in an adolescent, biracial cohort. Addictive Behaviors. 2003;28(3):501–512. doi: 10.1016/s0306-4603(01)00258-1. [DOI] [PubMed] [Google Scholar]
- 18.Brook DW, Zhang C, Brook JS, Finch SJ. Trajectories of cigarette smoking from adolescence to young adulthood as predictors of obesity in the mid-30s. Nicotine & Tobacco Research. 2010 doi: 10.1093/ntr/ntp202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lanza HI, Grella CE, Chung PJ. Adolescent obesity and future substance use: Incorporating the psychosocial context. Journal of Adolescence. 2015;45:20–30. doi: 10.1016/j.adolescence.2015.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Harris K, Udry J. Inter-university Consortium for Political and Social Research (ICPSR) [distributor] 2013. National Longitudinal Study of Adolescent Health (Add Health), 1994–2008: Core Files [Restricted Use] [Google Scholar]
- 22.Harris KM, Halpern CT, Whitsel E, et al. The National Longitudinal Study of Adolescent Health: Research Design. Carolina Population Center, University of North Carolina; Chapel Hill, NC: 2009. [Google Scholar]
- 23.Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. Vol. 718. John Wiley & Sons; 2013. [Google Scholar]
- 24.Entzel P, Whitsel EA, Richardson A, et al. Add Health Wave IV Documentation. Carolina Population Center, University of North Carolina; Chapel Hill: 2009. Cardiovascular and anthropometric measures. [Google Scholar]
- 25.Carolina Population Center, University of North Carolina at Chapel Hill. Program Code for Race. http://www.cpc.unc.edu/projects/addhealth/faqs/aboutdata/index.html#RACE2016.
- 26.Lui CK, Chung PJ, Ford CL, Grella CE, Mulia N. Drinking behaviors and life course socioeconomic status during the transition from adolescence to adulthood among whites and blacks. Journal of Studies on Alcohol and Drugs. 2015;76(1):68–79. [PMC free article] [PubMed] [Google Scholar]
- 27.Chen P, Chantala K. Guidelines for analyzing Add Health data. Carolina Population Center, University of North Carolina; Chapel Hill: 2014. [Google Scholar]
- 28.American Cancer Society. Cancer Facts & Figures 2014. Atlanta: 2014. [Google Scholar]
- 29.Meyer J, Rohrmann S, Bopp M, Faeh D. Impact of smoking and excess body weight on overall and site-specific cancer mortality risk. Cancer Epidemiology Biomarkers & Prevention. 2015;24(10):1516–1522. doi: 10.1158/1055-9965.EPI-15-0415. [DOI] [PubMed] [Google Scholar]
- 30.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 31.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fryar CD, Gu Q, Ogden CL. Anthropometric reference data for children and adults: United States, 2007–2010. Vital and Health Statistics. Series 11. 2012;(252):1–48. [PubMed] [Google Scholar]
- 33.Klesges RC, Klesges LM. Cigarette smoking as a dieting strategy in a university population. International Journal of Eating Disorders. 1988;7(3):413–419. [Google Scholar]
- 34.Potter BK, Pederson LL, Chan SS, Aubut J-AL, Koval JJ. Does a relationship exist between body weight, concerns about weight, and smoking among adolescents? An integration of the literature with an emphasis on gender. Nicotine & Tobacco Research. 2004;6(3):397–425. doi: 10.1080/14622200410001696529. [DOI] [PubMed] [Google Scholar]
- 35.Harris KM. The add health study: design and accomplishments. Chapel Hill: Carolina Population Center, University of North Carolina at Chapel Hill; 2013. [Google Scholar]
- 36.McCarthy WJ, Mistry R, Lu Y, Patel M, Zheng H, Dietsch B. Density of tobacco retailers near schools: effects on tobacco use among students. American Journal of Public Health. 2009;99(11):2006–2013. doi: 10.2105/AJPH.2008.145128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mistry R, McCarthy WJ, Yancey AK, Lu Y, Patel M. Resilience and patterns of health risk behaviors in California adolescents. Preventive Medicine. 2009;48(3):291–297. doi: 10.1016/j.ypmed.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Moodie R, Stuckler D, Monteiro C, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. The Lancet. 2013;381(9867):670–679. doi: 10.1016/S0140-6736(12)62089-3. [DOI] [PubMed] [Google Scholar]
- 39.Fiore M. Treating tobacco use and dependence: 2008 update: Clinical practice guideline. Diane Publishing; 2008. [Google Scholar]
- 40.Jensen MD, Ryan DH, Donato KA, et al. Executive summary: Guidelines (2013) for the management of overweight and obesity in adults. Obesity. 2014;22(S2):S5–S39. doi: 10.1002/oby.20821. [DOI] [PubMed] [Google Scholar]