Abstract
A 37-year-old woman underwent surgery to remove bilateral vulvar masses. The masses were firm, non-tender, and immobile. Pathologic finding was a well-delineated creamy grayish mass with a homogenous grayish solid surface and mild edema, chronic inflammatory infiltration, and focal dilation of the ducts with squamous metaplasia. The diagnosis was hyperplastic and hypertrophied Bartholin’s gland. Hyperplasia is a rare etiology for an enlarged Bartholin’s gland. Clinical presentation of Bartholin’s gland nodular hyperplasia is rather specific, although inflammatory lesion is the most common cause of swelling of the Bartholin’s gland in all age groups. Bartholin’s hyperplasia should be considered in cases with a solid mass. Total surgical excision is required for diagnosis. Only a few cases of Bartholin’s gland hyperplasia have been reported in the literature. Our patient has been receiving regular follow-up examination and there is no evidence of dyspareunia, perineal pain, and recurrent disease 12 months after surgery.
Keywords: Bartholin’s gland, Hyperplasia, Lymphadenitis
What’s Known
Because Bartholin’s gland hyperplasia is very rare, we should consider it as an etiologic differential diagnosis.
What’s New
Only a few cases of Bartholin’s gland hyperplasia have been reported in the literature.
Hyperplasia is a rare etiology for an enlarged Bartholin’s gland.
Introduction
The bilateral Bartholin glands, also termed greater vestibular glands, are major glands that measure 0.5 to 1 cm in diameter. Each duct is about 1.5-2 cm long and opens distal to the hymeneal ring; one at 5 and the other at 7 o’clock on the vestibule.1 These glands are normally impalpable.2 Lesions of the Bartholin’s gland are most often due to benign diseases such as cysts and abscess, whereas malignant lesion is rare.3 Bartholin’s gland lesions can be classified as cysts, abscess, hyperplasia, adenoma, adenomyoma, carcinoma, and soft tissue mesenchymal lesions.3 Only a few cases of Bartholin’s gland hyperplasia have been reported in the literature. Hyperplasia is a rare etiology for an enlarged Bartholin’s gland.
Clinical presentation of Bartholin’s gland nodular hyperplasia is rather specific. Most of the cases arise as a slightly painful, rapidly enlarging, cherry-red, regular or irregular, firm or cyst-like lesion of the lower part of the major or minor labium. If ulceration is present, entry dyspareunia can be associated. No discharge, dysuria, or vulvar sensitivity has been reported. Nodular hyperplasia can be bilateral.4,5
We present a case of bilateral hyperplastic Bartholin’s gland masses in a patient with perineal pain. Written informed consent was obtained from the patient for the publication of this case report.
Case Presentation
We introduce a 37-year-old woman whose chief complaints were perineal pain and dyspareunia 1-year before surgery. She did not feel any masses in the perineal area. Genital examination was performed. Inspection was normal and palpation revealed bilateral firm, fix, and non-tender masses in vestibular gland region. We performed a 1-2 cm incision just about the bulged point of the masses, excised masses from adjacent tissue and totally removed both masses and did marsupialization. Grossly, the specimen consisted of well-delineated creamy grayish mass with elastic consistency measuring 4×3×2.5 cm and 4.5×1.7×1.7 cm (figure 1). The cut section revealed a homogenous grayish solid surface and the representative section submitted in 4 blocks. No necrosis or hemorrhage was seen. Microscopic examination showed hyperplastic and hypertrophied Bartholin’s gland revealing mild edema, chronic inflammatory infiltrate, and focal dilation of ducts with squamous metaplasia (figure 2). The diagnosis was hyperplasic and hypertrophied Bartholin’s gland with chronic adenitis. There was no evidence of malignancy.
Figure 1.

Intraoperative findings shows solid masses arising from bilateral vaginal wall in vestibular gland region.
Figure 2.
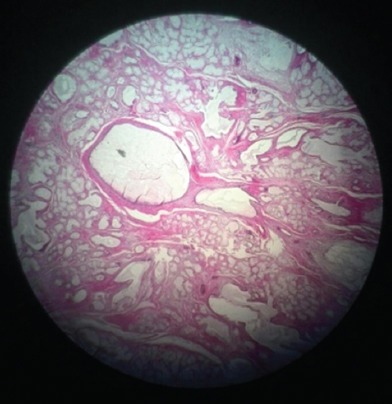
Pathologic feature shows hyperplastic and hypertrophied Bartholin’s glands, edema, chronic inflammatory infiltrate, focal dilation of ducts with squamous metaplasia, and increased number of acini.
Discussion
Although inflammatory lesion is the most common cause of swelling of the Bartholin’s gland in all age groups, Bartholin’s hyperplasia should be considered in cases with a solid mass. Total surgical excision is required for diagnosis.3 Several labia and vaginal lesions can imitate Bartholin’s gland diseases. In such situations, differential diagnosis should be considered for the abscess or mass. Differential diagnosis includes different types of cysts (inclusion, Gartner, Skene’s, sebaceous, vestibular mucosa, canal of Nuck), leiomyoma fibroma, hernia, hidradenoma, hematomas, lipoma, endometriosis, syringoma, accessory breast tissue, folliculitis, urethral diverticula, hidradenitis suppurativa, chancroid, gonorrhea, syphilis, vaginitis, warts or Bartholin’s gland cyst, abscess or cancer.6
Nodular hyperplasia, adenoma, adenomyoma can sometimes cause Bartholin’s gland enlargement and differential diagnosis between these anatomo-pathological types can be difficult based on a simple clinical examination. Malignancies of Bartholin’s gland, on the other hand, include various types of carcinomas.7 Nodular hyperplasia can be defined as a proliferation of mucinous acini with a preserved duct-acini ratio, as seen in a normal gland, without capsulation and with a lobulated or irregular contour. On the other hand, adenoma can be diagnosed if the proliferation of glands, tubules, and acini is random or diffuse and sharply circumscribed or capsulated. Differential diagnosis between nodular hyperplasia and adenoma is very important for the well-defined malignant potential of the latter one.
Browsing recent literature, there is no mention of the prevalence and incidence of Bartholin’s gland nodular hyperplasia since only 36 cases are reported in the modern English-language literature.
Santos and Kennarson reported 10 cases of nodular hyperplasia (NH). Grossly, NHs were solid, tan, and unencapsulated. Histologically, the NHs were composed of the proliferation of mucus-secreting acini with preservation of the normal duct to acinar relationship. Chronic inflammation and squamous metaplasia were present.2
Hyun-soo et al. reported a 40-year-old woman with the complaint of nonspecific discomfort in the perineal region for one month without any other symptom such as vaginal discharge, dysparunia or pruritus. Physical examination revealed bilateral firm and tender masses with the clinical diagnosis of Bartholin’s gland cyst. Pathologic findings were consistent with Bartholin’s gland hyperplasia.8
Jahromi et al. reported Bartholin’s gland hyperplasia, which was removed incidentally during anterior-posterior colporhaphy. Two ill-defined, lobulated surface, solid masses with diameters of 3×2.2×1.5 cm and 3.2×2.5×1.5 cm were removed. Microscopic examination showed increased number of acini with preserved duct-acinar relationship. There was no evidence of inflammation. The hyperplasia could result from hormonal alterations. In this report, the patient had used OCP for 4 years, which may have had stimulatory effect on Bartholin’s gland.9
Koeing and Tavassoli reported 17 cases with NH. The mean age of these patients was 35 years. These lesions were solid or solid and cystic, had maximal dimension of 2-3 cm, and were frequently thought to be Bartholin’s cysts on clinical examination. Varying degree of inflammation and sqamous metaplasia of the duct was common in NH. In their report, they concluded that NH occurs in younger patients and is often associated with inflammation or obstruction of Bartholin’s duct.10
Kazakov and Carik studied 2 cases of hyperplasia of the Bartholin’s gland. In one case, there was a squamous metaplasia and in the other case, a monoclonal pattern was found suggesting that the lesion may be a process rather than a simple reactive hyperplasia.11
Fiori et al. reported a 50-year-old woman with a history of recurrent episodes of Bartholinities over several years. They described a case in which total excision of Bartholin’s gland was performed and that resulted in a diagnosis of nodular hyperplasia.7
Wal and Antonello reported 3 cases of hyperplasia of the Bartholin’s gland. The first case was a 35-year-old woman with a complaint of a hardened nodule in her right labium without local inflammatory signs. The second case was a 45-year-old woman with a painless 2 cm diameter fibrous nodule in the right labium. The last case was a 38-year-old woman with a left-sided swelling of the vulva. Pathologic findings were consistent with Bartholin’s gland hyperplasia.12 A mass must be classified as adenoma if it presents disrupted ductal/acinar architecture; diffuse or disorganized acinar and ductal proliferation; encapsulation or circumscribed margin.12 Based on literature review, the average age of the patients was approximately 36 years old. The youngest and the oldest patients reported with NH were 19 and 56 years old, respectively. Inflammatory or infectious process can induce hyperplasia due to chronic cellular lesion mechanism. Surgical intervention and local trauma can also act as etiological factors to glandular proliferation, as it was reported on the minor vestibular glands. Hyperplasia can also result from hormonal milieu alteration.12
The histopathology finding in our case was chronic inflammation and focal dilation of the duct with squamous metaplasia. Hyperplasia of Bartholin’s gland is a rare benign lesion and there are a few female cases of different age groups in the literature. The treatment of choice for bilateral Bartholin’s hyperplasia is a complete excision to exclude malignant neoplasm, such as squamous cell carcinoma, adenocarcinoma, or adenoid cyst carcinoma, which rarely arises in Bartholin’s gland.8 Follow-up studies on benign solid tumors of Bartholin’s gland have demonstrated an excellent prognosis. Our patient has been receiving regular follow-up examination and there is no evidence of dysparunia, perineal pain, and recurrent disease 12 months after surgery.
Conflict of Interest: None declared.
References
- 1.Bloom S, Corton MM, Spong CY, Dashe J, Leveno K. Williams Obstetrics. 24th ed. New York: McGraw-Hill Education; 2014. p. 1376. [Google Scholar]
- 2.Santos LD, Kennerson AR, Killingsworth MC. Nodular hyperplasia of Bartholin’s gland. Pathology. 2006;38:223–8. doi: 10.1080/00313020600696223. [DOI] [PubMed] [Google Scholar]
- 3.Kurtoğlu E, Kaya R, Arpacı H, Topak N, Cemgil Arıkan D. Nodular Hyperplasia of the Bartholin’s Gland. Journal of Clinical and Analytical Medicine. 2015;6:219–21. [Google Scholar]
- 4.Argenta PA, Bell K, Reynolds C, Weinstein R. Bartholin’s gland hyperplasia in a postmenopausal woman. Obstet Gynecol. 1997;90:695–7. doi: 10.1016/S0029-7844(97)00409-2. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Harosh S, Cohen I, Bornstein J. Bartholin’s gland hyperplasia in a young woman. Gynecol Obstet Invest. 2008;65:18–20. doi: 10.1159/000106500. [DOI] [PubMed] [Google Scholar]
- 6.Lee MY, Dalpiaz A, Schwamb R, Miao Y, Waltzer W, Khan A. Clinical Pathology of Bartholin’s Glands: A Review of the Literature. Curr Urol. 2015;8:22–5. doi: 10.1159/000365683. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fiori E, Ferraro D, Borrini F, De Cesare A, Leone G, Crocetti A, et al. Bartholin’s gland hyperplasia. Case report and a review of literature. Ann Ital Chir. 2013;84:1–4. [PubMed] [Google Scholar]
- 8.Hyun-Soo K, Gou-Young K, Sung-Jig L, Eun-Hee Y, Youn-Wha K. Bilateral Bartholin’s Gland Hyperplasia Associated with Bartholin’s Gland Cyst: A Brief Case Report. Korean J Pathol. 2008;42:314–6. [Google Scholar]
- 9.Akbarzadeh Jahromi M, Sari Aslani F, Samsami Dehghani A, Mahmoodi E. Bartholin’s Gland Bilateral Nodular Hyperplasia: A Case Report Study. Iran Red Crescent Med J. 2014;16:e8146. doi: 10.5812/ircmj.8146. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koenig C, Tavassoli FA. Nodular hyperplasia, adenoma, and adenomyoma of Bartholin’s gland. Int J Gynecol Pathol. 1998;17:289–94. doi: 10.1097/00004347-199810000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Kazakov DV, Curik R, Vanecek T, Mukensnabl P, Michal M. Nodular Hyperplasia of the Bartholin Gland: A Clinicopathological Study of Two Cases, Including Detection of Clonality by HUMARA. Am J Dermatopathol. 2007;29:385–7. doi: 10.1097/DAD.0b013e31806f54b3. [DOI] [PubMed] [Google Scholar]
- 12.Wal R, Antonello ML. Nodular hyperplasia of Bartholin’s gland: case reports and literature review. J Bras Patol Med Lab. 2011;47:555–9. [Google Scholar]


