Abstract
Background
Recently reported prevalences of myopia in primary school children vary greatly in different regions of the world. This study aimed to estimate the prevalence of refractive errors in an unselected urban population of young primary school children in eastern Sydney, Australia, between 1998 and 2004, for comparison with our previously published data gathered using the same protocols and other Australian studies over the last 30 years.
Methods
Right eye refractive data from non-cycloplegic retinoscopy was analysed for 1,936 children aged 4 to 12 years who underwent a full eye examination whilst on a vision science excursion to the Vision Education Centre Clinic at the University of New South Wales. Myopia was defined as spherical equivalents equal to or less than -0.50 D, and hyperopia as spherical equivalents greater than +0.50 D.
Results
The mean spherical equivalent decreased significantly (p < 0.0001) with age from +0.73 ± 0.1D (SE) at age 4 to +0.21 ± 0.11D at age 12 years. The proportion of children across all ages with myopia of -0.50D or more was 8.4%, ranging from 2.3% of 4 year olds to 14.7% of 12 year olds. Hyperopia greater than +0.50D was present in 38.4%. A 3-way ANOVA for cohort, age and gender of both the current and our previous data showed a significant main effect for age (p < 0.0001) but not for cohort (p = 0.134) or gender (p = 0.61).
Conclusions
Comparison of our new data with our early 1990s data and that from studies of over 8,000 Australian non-clinical rural and urban children in the 1970's and 1980's provided no evidence for the rapidly increasing prevalence of myopia described elsewhere in the world. In fact, the prevalence of myopia in Australian children continues to be significantly lower than that reported in Asia and North America despite changing demographics. This raises the issue of whether these results are a reflection of Australia's stable educational system and lifestyle over the last 30 years.
Background
The prevalence of myopia is currently receiving worldwide attention as many recent studies report dramatic increases over the last 20 years [1,2]. Myopia and its aetiology is an interesting example of the intertwining of 'nature and nurture' with both genetics and life-style environment as important issues [3]. There is strong evidence indicating that genetic inheritance is a major contributor, both from the examination of prevalences across different racial backgrounds [4], from family pedigrees [5] and from twin studies [6]. However, there is increasing evidence suggesting that high heritability does not preclude rapid environmentally-induced increases in prevalence [7], rather, inherited factors are likely to both drive the susceptibility and resistance to environmentally-induced myopia [6,8].
Despite much research interest over the last half century, there have been surprisingly few well-designed epidemiological studies of refractive error with large numbers of randomly selected younger school children to form the basis of valid world wide comparisons of the earliest stages of development of myopia [3,9,10]. However, a group sponsored by the World Health Organisation in 2001 has devised a protocol to be used during studies of refractive error across different cultural and ethnic settings: the 'Refractive Error Study in Children' (RESC) [11].
In general, estimates of the prevalence of myopia have shown less increase in the Western world than in Asia, and less increase in rural than in urban populations [1,10,12-16]. Five very large studies across two decades and involving over 10,000 children in Taiwan are very important for understanding the changing prevalence of myopia in young Asian children (1.8% in 1986 rising to 12% in 1995 for 6 year olds, 40% rising to 56% for 12 year olds) [2]. A similar change is also reflected in Singaporean studies of myopia in military conscripts aged 17 years (26% to 83% from the late 1970s to the late 1990s as reviewed by [1]), of whom notably 82% were Chinese [17].
It has often been suggested that myopia is more prevalent in ethnic Chinese (reviewed [18]), but only relatively recent studies compare the prevalence of myopia in young ethnic Chinese children living either in China and in other countries [1,12,15,18-22]. For younger Chinese children aged around 5–7 years, the prevalence of myopia was found to range from under 5% in rural China [14,23] to 24% in Chinese Malays [20] and 30% in urban Hong Kong [19,22]. For older Chinese children aged 11–12 years, the prevalence ranged from 23% of rural Chinese[14,23] to 40% in urban China[12], 47% of Chinese Malays [20] and 57% in urban Hong Kong [22]. Japan has a similarly high prevalence of myopia in young school children estimated in recent times to be 43.5% of 12 year olds [24].
By comparison, the epidemiology of refractive error for young Australian school children is relatively well documented and presents a very different profile. A number of studies were carried out in the early 1970s and the 1980s on relatively large groups of unselected primary school children from the socio-economic extremes (generally aged 5 to 12 years), and indicated a prevalence of myopia ranging from approximately 3% to 13% (see Table 1) [25-29]. Two of those early studies investigated children largely from underprivileged, rural, families [26,27], and the other was of children from several, middle to upper socio-economic class private schools [25]. One smaller study was carried out in the mid 1980s on children from a representative selection of government schools in Brisbane [29], and would therefore have investigated children from a broader range of backgrounds. Interestingly, this latter study was the only Australian study to have determined refractive error under cycloplegia, yet yielded the highest prevalence of myopia. Thus, it has been difficult to determine whether the prevalence of myopia has increased in young school children in Australia as reported elsewhere. The majority of Australian residents are of Caucasian extraction living a very western lifestyle, leading one to expect the prevalence of myopia to be similar to that found in US or Europe. Yet, studies suggest that the prevalence of myopia in Australian primary school children is low by world standards [10].
Table 1.
Prevalence of myopia in Australia school children.
| Authors | Year | N | Place | Ages | Method | Criterion | Prevalence % |
| Robbins & Bailey [25] | 1975 | 1,243 | Private schools | 4, 8, 12 | Non-cycloplegic retinoscopy | Myopia≥-0.50D "suspected of having myopia" |
5.6% 4 yrs 6.4% 12 yrs |
| Amigo, McCarthy & Pye [26] | 1976 | 1,166 | Rural underprivileged | 7 to 12 | Non-cycloplegic retinoscopy | "any tendency for myopia" | 3.4% |
| Walters [27] | 1981 1982 1983 |
2,055 1,187 1,722 |
Rural underprivileged | 4 to 14 | Non-cycloplegic retinoscopy | Myopia≥-0.50D | 4.40% 3.03% 2.67% |
| Macfarlane [29] | 1987 | 877 | Representative government schools | 6 to 11 | Cycloplegic retinoscopy | Not stated | 13% |
| Junghans et al [30] | Early 1990s | 2,535 | 14 government & church schools | 4 to 12 | Non-cycloplegic retinoscopy | Myopia≥-0.50D | 2.0% 4 yrs 10.9% 12 yrs Mean 6.5% |
In 2003 we reported the relative proportions of refractive errors in a large unselected primary school population of 2,535 children drawn from a very broad range of socio-economic backgrounds in Sydney, the largest city in Australia, in the early 1990s [30]. The children attended fourteen primary schools and two preschools. As in the earlier studies, the proportion of children with myopia greater than -0.50 DS spherical equivalence, as determined by non-cycloplegic retinoscopy, was found to be low by world standards (1.0% of 4 year olds rising to 8.3% of 12 year olds). We have now analysed the prevalence of refractive error in a new similar group of 1,936 children unselected primary school children drawn generally from the same area as our first study.
Methods
The study design is a retrospective examination of records of the Vision Education Centre (VEC) [31] school vision screenings (so named because parents were not present to ratify history) conducted in the Clinic of the School of Optometry and Vision Science, UNSW. Approvals for the study and permission to approach schools were obtained from the Committee for Use of Humans in Research at the University of New South Wales (UNSW), Sydney, Australia. The protocols adhered to the tenets of the Declaration of Helsinki. Parents or guardians were provided with an information sheet and requested an outline of known symptoms. Signed consent was required prior to a child's participation.
Sampling and recruitment
Permission was obtained from the NSW Department of Education and the NSW Catholic Education Office to approach all schools in the eastern region of Sydney (some thirty coeducational primary schools) to send entire classes to the VEC. A flyer was sent describing the VEC science excursion and age-appropriate eye examination, inviting Years 1, 3 and 5 particularly to participate.
The group of 1,936 children examined came from the eastern suburbs along the southern beaches of Sydney, and may be thought of as randomly selected with little likelihood of bias to the data as individual classes were free to respond. Children were drawn from twelve government and non-government primary schools and one pre-school and attended the clinic only once. During the 1996 Australian Bureau of Statistics census 14,785 children aged 4 to 12 years were recorded in this region (Randwick and Waverley precincts of Eastern Sydney) who came from a very broad range of ethnic and socio-economic backgrounds present, where 37 different languages might be spoken in the home [32]. This was reflected in the children attending VEC. Census data indicate approximately 9% of the children in the current study were likely to be of Asian origin [32], a figure supported by our interpretation of family name for each child [30]. Participation in the eye examinations was typically well over 90% for each class, with teachers reporting non-participation to be predominantly due to illness on the day. Less than 3% of parents intentionally prevented participation, even if eye care had previously been sought. This particularly high participation rate was largely due to the attraction of a an age-appropriate student-centred hands-on science lesson about eyes and vision [31] delivered alongside the eye examination.
Clinical examination
The comprehensive optometric examination by experienced paediatric practitioners included all age-appropriate tests meeting Australian Optometric Competency Standards, except that parents/guardians were not present to ratify history. Refractive error was determined by non-cycloplegic retinoscopy with optical fogging while the child maintained fixation on a distant non-accommodative (6 metre) target. In most cases refractive status was confirmed by subjective refraction. Other tests included letter visual acuity at 6 m and 33 cm, cover test for strabismus, motilities, saccades, pupil reactions, near point of convergence, heterophoria, stereopsis, accommodative facility, colour vision and ophthalmoscopy.
Justification of choice of testing procedures
Cycloplegic retinoscopy was not undertaken for many reasons including the fact that VEC studies started prior to the 2000 convention suggesting use of cycloplegic retinoscopy for studies of refractive error prevalence [11]. Secondly, the VEC visit was meant as an excursion and the children had to return to normal classes with near work demands after the morning outing. Thirdly, it was important for comparison purposes to use refractive data procured under the same conditions as that used for the earlier groups of children. Fourthly, an initial evaluation without cycloplegia is necessary in order to understand daily function. Fifthly, non-cycloplegic retinoscopy was only one component of the exam. Outcomes regarding a decision to refer would not alter for most children had a cycloplegic refraction been carried out, as several other near function tests that would also indicate the possible existence of latent hyperopia or pseudo-myopia were included. Lastly, the degree of refractive error may in fact be influenced by cycloplegia (see Discussion for elaboration [33-38]).
Autorefractors were not employed as hand-held versions were unavailable when the first cohort was seen. Equally as important, there is no convincing evidence that the proportion of myopes identified in the sample would have changed [39].
Comparison with earlier data
To compare the estimated prevalence of myopia in this urban population of 'Australian children' over the last decade, this more recent 2000s data set was analysed against data from an earlier cohort of 2,322 children with similar demographics seen in the early 1990's, using the same testing protocols and seen at the same venue [30]. The optometric results of that earlier cohort have previously been reported [40], and it was noted that 7.1% of those children were already wearing spectacles [30], indicating that our recruitment procedure did not preclude children already under the care elsewhere. The data for any child examined in both cohorts was deleted from the earlier data set to avoid bias in the analysis. The mean date of assessment for this last 2000s cohort was September 2000, and for the early 1990s cohort was June 1992. Thus, the average gap between assessments of children from the two cohorts was 8 years and 3 months.
Statistical analyses
Data was analysed by Analysis of Variance ANOVA (StatView software). Only refractive data from right eyes was used for the current refractive class analysis, as the correlation between right and left eye refractions was extremely high (p < 0.0005). The preferred criterion to define myopia in this study is that used clinically in Australia: a spherical equivalent equal to or more minus than -0.50 D. However, as myopia more minus than -0.50 D has occasionally been used to define myopia in epidemiological studies [13,19,41], analyses using the criterion 'myopia more minus than -0.50 D' were also performed for comparison. Hyperopia was defined as spherical equivalents greater than +0.50 D. Thus, emmetropia for this study was defined as refractions in the range -0.25 to +0.50 dioptres spherical equivalence inclusive. Means are quoted with the associated standard error.
Results
The records of 1,936 children aged 4 to 12 years from a non-clinical unselected population examined during the six years from March 1998 to May 2004 were analysed retrospectively to estimate the prevalence of different types of refractive error. Primary schools of their own choice sent more children from years 1, 3, and 5, which resulted in unequal numbers of children in each of the age groups. There were 925 boys and 951 girls, and the relative numbers for both males and females in each age group are shown in Table 2. For 59 children, the gender was not indicated on the record card and could not be inferred with certainty from the given name. The data not associated with gender has only been included in analyses entitled 'All' as shown in Tables 2 and 3. Mean age was 8.36 years. The relative proportions of the different classifications of refractive error for all children combined (including those of unknown gender) for each age group are shown in Table 2.
Table 2.
Estimated prevalence of refractive error (%) by age in children aged 4 to 12 years.
| Age | Myopia | Emmetropia | Hyperopia | N | |||||
| More than -3.75 | -0.50 to -3.75 | of -0.50 | -0.25 to +0.50 | +0.75 to +1.25 | More than +1.25 | Female | Male | All | |
| 4 | 0.0 | 2.3 | 0.0 | 43.2 | 50.0 | 4.5 | 24 | 16 | 44 |
| 5 | 0.4 | 1.5 | 1.2 | 49.8 | 41.3 | 5.8 | 121 | 129 | 259 |
| 6 | 0.0 | 1.7 | 0.7 | 47.6 | 43.4 | 6.6 | 145 | 133 | 286 |
| 7 | 0.0 | 2.5 | 2.5 | 54.8 | 33.1 | 7.0 | 72 | 80 | 157 |
| 8 | 1.0 | 5.6 | 0.5 | 49.0 | 29.6 | 14.3 | 100 | 85 | 196 |
| 9 | 0.8 | 6.5 | 1.5 | 56.3 | 29.7 | 5.3 | 133 | 128 | 263 |
| 10 | 2.4 | 9.0 | 2.4 | 54.7 | 27.8 | 3.8 | 149 | 88 | 212 |
| 11 | 0.5 | 10.9 | 2.1 | 58.0 | 24.5 | 4.0 | 146 | 189 | 376 |
| 12 | 2.1 | 11.2 | 1.4 | 57.3 | 22.4 | 5.6 | 61 | 77 | 143 |
Table 3.
Mean estimated prevalence of myopia and hyperopia in children aged 4 to 12 years.
| Female | Male | All | ||||
| Refractive Category: | N | % | N | % | N | % |
| Myopia ≤-4 | 8 | 0.8 | 8 | 0.9 | 15 | 0.8 |
| Myopia -3.75≤x≤-0.75 | 58 | 6.1 | 58 | 6.3 | 118 | 6.1 |
| Myopia of -0.50 | 11 | 1.2 | 17 | 1.8 | 29 | 1.5 |
| Emmetropia -0.25≤x≤0.50 | 504 | 53.0 | 501 | 54.2 | 1030 | 53.2 |
| Hyperopia +0.75≤x≤+1.25 | 320 | 33.6 | 282 | 30.5 | 624 | 32.2 |
| Hyperopia ≥+1.50 | 50 | 5.3 | 59 | 6.4 | 120 | 6.2 |
| Total | 951 | 100 | 925 | 100 | 1936 | 100 |
The mean spherical equivalent refraction of all 1,936 children was +0.45 ± 0.02 DS, however it should be noted that there is a preponderance of children aged 5–6, 9 and 11 years old corresponding with Years 1, 3, and 5 of primary school. Overall, there was no significant difference in spherical equivalent refractive error between girls and boys (p = 0.697). In general, mean refraction demonstrates a highly significant shift towards less hyperopia with increasing age (p < 0.0001) from 0.73 ± 0.1DS for 4 year olds to 0.21 ± 0.11 for 12 year olds, however this is more noticeable after the age of 9 years as seen in Fig. 1. With increasing age, more children are found in the emmetropic category and fewer in the low hypermetropic category.
Figure 1.

Histogram of mean right eye spherical equivalent refractive error by age and gender ('2000s' data). Error bars represent standard error.
A summary of the relative proportions of myopia and hyperopia for this cohort of children of all ages seen during the six years ('2000s' data) is given in Table 3. The majority of children screened are emmetropic by our criteria: 53.0% averaged across all ages. The proportion of children manifesting moderate to high degrees of hypermetropia (≥+1.50 DS) is 6.2% across all ages. Only 6.9% of children of all ages had refractive errors more minus than -0.50 DS, ranging from 2.3% of 4 year olds to 13.3% of 12 year olds (Fig. 2). If the more liberal definition of myopia is applied (myopia equal to or more minus than -0.50), then 8.4% of all children were myopic (ranging from 2.3% of 2 year olds to 14.7% of 12 year olds). Only 0.8% of the 1,936 children were more than -4.00 DS myopic.
Figure 2.
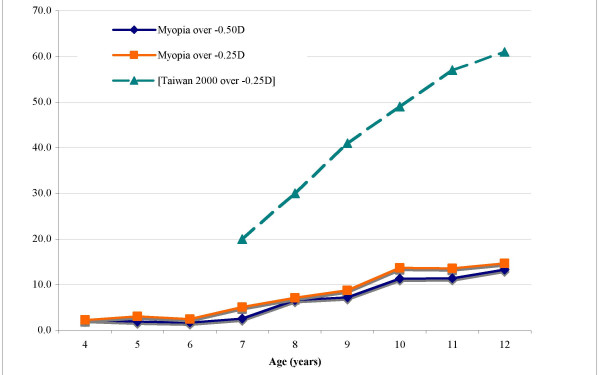
Line graphs of the percentage Sydney children with myopia by age using the alternate criteria of more minus than -0.50 D spherical equivalence (blue line) or more minus than -0.25DS spherical equivalence (orange line), and, the percentage of Taiwanese children seen in the year 2000 more minus than -0.25D (aqua dashed line) taken from Lin et al, Ann Acad Med 2004 33:27–33.
Comparison with previous data
The number of children per age group for the two cohorts is shown in Fig. 3, and notably, the age profile differs slightly between cohorts, though the mean age of 8.37 years for the earlier cohort was similar to that of this later cohort. The mean and standard error for right eye spherical equivalent refractive error by age is shown for each cohort in Fig. 4.
Figure 3.
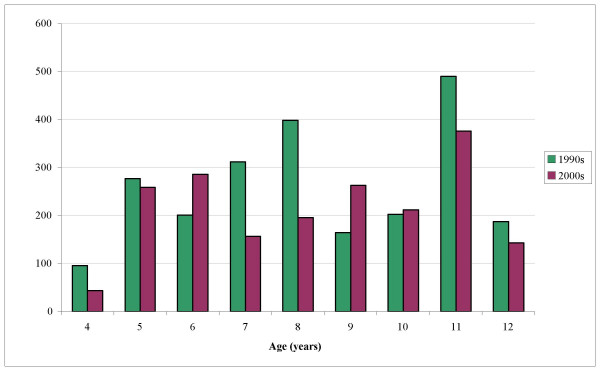
Histogram of the number of children in each age group for data from the current study (2000s) and the previously reported early 1990s data [30].
Figure 4.
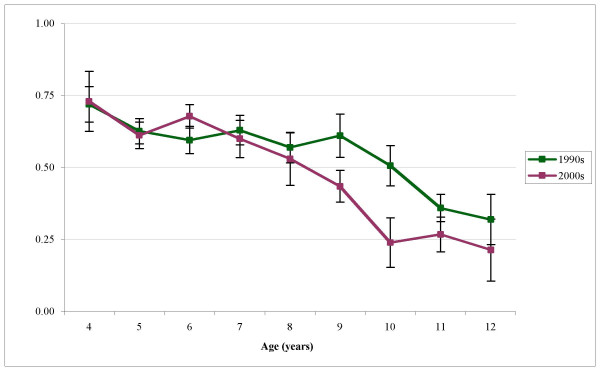
The mean right eye spherical equivalent refractive error by age for data from the current study and the previously reported early 1990s data [30]. Error bars represent standard error.
A three-way analysis of variance was carried out for cohort, age and gender. There was a main effect for age (p < 0.0001), but no main effect for either cohort (p = 0.134) or gender (p = 0.61). However, there were age/gender/cohort interactions that indicate a trend towards an increasing shift away from the hyperopic refraction in the later cohort.
Discussion
An analysis of the prevalence of refractive errors in young school children in eastern Sydney during the last thirteen years has been presented. The latest data gathered from 1,936 unselected primary school-aged children in the last 6 years, indicates that the prevalence of myopia remains quite low compared to that reported for the western world and Asia, especially as refractive error was established by non-cycloplegic retinoscopy (as will be discussed later). These findings are not significantly different (p = 0.13) to our previous report [30] indicating that 6.5% of 2,535 unselected children aged 4 to 12 years seen in the early 1990s were myopic by at least 0.50 D. Notably, those children were of similar socio-economic and ethnic status drawn from the same region of Sydney and seen at the same Centre using the same testing protocol.
Therefore, if we take the total 4,258 children seen since 1990, the relative frequency of refractive error across all is: 54.2% emmetropic by our criteria, 32.3% low to moderate hyperopes, 5.3% myopic greater than -0.50D spherical equivalence and 7.4% myopic by at least -0.50 DS. The number with myopia of at least -4.00 DS was an extremely small 0.6%.
The prevalence of myopia in Sydney primary school children compared to the rest of the world
As alluded to in the introduction, the proportion of Sydney children with myopia is dramatically less than in Asia. Indeed, the proportion appears significantly lower than in the USA [41] and Canada [42] (4% and 6% of 6 year olds respectively, or 20% of 12 year olds in USA), but higher than urban India with only 4.4% of all school children under 16 years myopic [13] and higher particularly than in other less developed countries [10].
In the past, a lack of internationally accepted definitions for 'myopia' has hampered valid comparisons across the various studies [10]. Commonly the criteria 'greater than -0.50 DS' or 'at least -0.50 DS' are employed. However, our separate analyses using both of these criteria only resulted in a difference of 1.5% of all children included as myopic, in keeping with other dual analyses [13,41], and is low either way when compared with Asia or North America.
Comparison across studies is also difficult when only an 'overall' mean refraction is presented covering all children in a study, due to the well known increasing prevalence of myopia with age. Indeed, the comparison of data from our own two data sets is confounded to some extent by the slightly different age profiles for each cohort. However, in neither cohort was the age range nor mean significantly different, so the similar proportion of myopes is not unexpected.
Comparison of refractive error with and without a cycloplegic agent
The question of optimal ocular conditions for comparison of the prevalence of refractive errors remains controversial. A cycloplegic agent is typically proposed as the gold standard [3,43,44] in the belief that it will eliminate ciliary muscle action or spasm, and thus unmask latent hyperopia or pseudomyopia. Thus, the use of a cycloplegic would be firstly predicted to lead to a decrease in the prevalence of myopia, and an increase in the prevalence of hyperopia. However, as a cycloplegic also leads to associated mydriasis and the introduction of unpredictable spherical aberrations, it is arguable that cycloplegia will induce unpredictable errors. In fact, Gao et al [38] in 2002 reported significant changes in the refractive components of children's eyes under conditions of deep cycloplegia and mydriasis that were greatest in hyperopic eyes and smallest in myopic eyes, adding no definitive evidence as to the relative efficacy of cycloplegia.
Thus there appears to be no scientific concurrence regarding the efficacy of cycloplegia for studies on the prevalence of myopia [35-37], with several major studies electing to use cycloplegia (see review in [10,9,11]) and others not [18-21,23,42,45]. Presumably this design variability exists because there is no decisive evidence indicating a difference between refractions determined with and without a cycloplegic agent in eyes that have a myopic refraction. In general, a more positive retinoscopic finding is reported under cycloplegia, though considerable individual variation is seen including a myopic shift in some [33,35-37,46]. Not surprisingly, the differences noted decreased both with age and with less positive refraction.
As our refractive data was derived from non-cycloplegic retinoscopy we readily concede that mean refractive error may be less hyperopic than if a cycloplegic had been used. However, we suggest that as the influence of a cycloplegic is uncertain and is of least concern for myopes, the estimated prevalence of myopia will not be significantly altered by our decision to not use a cycloplegic. In support of this notion are new conference data from Rose et al [47,48] reporting refractive status ascertained by cycloplegic autorefraction in over 1,000 children aged 6–7 years from across the same city of Sydney. They reported values of 'around 3%' for the prevalence of myopia of at least 0.50D [47], and then the value of 1.5% for myopia of 'approximately 0.50D' [48] with a participation rate between 73 and 80%. From Table 2 it can be seen that 2.4% of our 6 year olds in the current study were at least 0.50D myopic – a value that is strikingly similar.
Demographics versus lifestyle
Worldwide patterns of the prevalence of myopia suggest significant differences are likely to be due to the different demographics and lifestyles [1,10,49]. Zadnik [41] concedes that the increase in numbers of myopic children in the US Orinda study may be due to changing ethnic demographics. The apparent slight increase in myopia in Australia reported in the current study may also be in part accounted for by our changing ethnic demographics in urban areas. However demographics and ethnic compositions are unlikely to be responsible for the large changes reported in Asian and some other western countries [1,50].
Whatever way it is argued, our results indicate little evidence for an epidemic of myopia although there is a developmental trend towards an earlier decrease in hyperopia to the point of myopia. Thus, the question of whether it is a matter of lifestyle, or perhaps familial environmental stress, or more, remains. Certainly, the education system and housing has changed little in Australia the last 30 years. By comparison, most Asian children participating in myopia epidemiological studies reportedly are more likely to live in high-rise residential blocks [17] and have strong demands at school to memorize along with parental and peer pressure to do well, and for some, a competitive entrance examination to enter school [19,51].
Conclusions
It is concluded that despite some differences in methodology across earlier studies, the prevalence of myopia in young Australian school children does not appear to have increased significantly over the last 30 years if one allows for the change in ethnic demographics. It is also proposed that an explanation for the large increase in prevalence of myopia reported in other countries must include questions relating to lifestyle in addition to genetic propensity.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
SC conceived and designed the study, jointly analysed the results and worked the drafts through to the final version. BJ coordinated the study, collated the clinic records, jointly analysed the results, researched the background for the paper, prepared the draft manuscript and was responsible for presentation. Both authors read and approved the manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Supported by a University of New South Wales GoldStar Grant to BM Junghans.
Contributor Information
Barbara M Junghans, Email: b.junghans@unsw.edu.au.
Sheila G Crewther, Email: s.crewther@latrobe.edu.au.
References
- Seet B, Wong TY, Tan DT, Saw SM, Balakrishnan V, Lee LK, Lim AS. Myopia in Singapore: taking a public health approach. Br J Ophthalmol. 2001;85:521–526. doi: 10.1136/bjo.85.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LLK, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med. 2004;33:27–33. [PubMed] [Google Scholar]
- Saw SM, Katz J, Schien OD, Chew SJ, Chan TK. Epidemiology of myopia. Epidem Rev. 1996;18:175–187. doi: 10.1093/oxfordjournals.epirev.a017924. [DOI] [PubMed] [Google Scholar]
- Curtin BJ. The Myopias. Basic Science and Clinical Management. Philadelphia , Harper and Row; 1985. [Google Scholar]
- Pacella R, McLellan J, Grice K, Del Bono EA, Wiggs JL, Gwiazda JE. Role of genetic factors in the etiology of juvenile-onset myopia based on a longitudinal study of refractive error. Optom Vis Sci. 1999;76:381–386. doi: 10.1097/00006324-199906000-00017. [DOI] [PubMed] [Google Scholar]
- Lyhne N, Sjolie AK, Kyvik KO, Green A. The importance of genes and environment for ocular refraction and its determiners: a population based study among 20-45 year old twins. Br J Ophthalmol. 2001;85:1470–1476. doi: 10.1136/bjo.85.12.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose KA, Morgan IG, Smith W, Mitchell P. High heritability of myopia does not preclude rapid changes in prevalence. Clin Exp Ophthalmol. 2002;30:168–172. doi: 10.1046/j.1442-9071.2002.00521.x. [DOI] [PubMed] [Google Scholar]
- Saw SM, Chua WH, Hong CY, Wu HM, Chan WY, Chia KS, Stone RA, Tan D. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci. 2002;43:332–339. [PubMed] [Google Scholar]
- Zadnik K, Mutti DO, Friedman NE, Adams AJ. Initial cross-sectional results from the Orinda Longitudinal Study of Myopia. Optom Vis Sci. 1993;70:750–758. doi: 10.1097/00006324-199309000-00012. [DOI] [PubMed] [Google Scholar]
- Working group on myopia prevalence and progression . Myopia: prevalence and progression. Washington D.C. , National Research Council; 1989. [Google Scholar]
- Negrel AD, Maul E, Pokharel GP, Zhao J, Ellwein LB. Refractive Error Study in Children: sampling and measurement methods for a multi-country survey.[comment] Am J Ophthalmol. 2000;129:421–426. doi: 10.1016/S0002-9394(99)00455-9. [DOI] [PubMed] [Google Scholar]
- Yap M, Wu M, Wang SH, Lee FL, Liu ZM. Environmental factors and refractive error in Chinese children. Clin Exp Optom. 1994;77:8–14. [Google Scholar]
- Dandona R, Dandona L, Naduvilath TJ, Srinivas M, McCarty CA, Rao GN. Refractive errors in an urban population in Southern India: the Andhra Pradesh Eye Disease Study. Invest Ophthalmol Vis Sci. 1999;40:2810–2818. [PubMed] [Google Scholar]
- Zhang MZ, Saw SM, Hong RZ, Fu ZF, Yang H, Shui YB, Yap MK, Chew SJ. Refractive errors in Singapore and Xiamen, China--a comparative study in school children aged 6 to 7 years. Optom Vis Sci. 2000;77:302–308. doi: 10.1097/00006324-200006000-00010. [DOI] [PubMed] [Google Scholar]
- Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB. Refractive Error Study in Children: results from Shunyi District, China. Am J Ophthalmol. 2000;129:427–435. doi: 10.1016/S0002-9394(99)00452-3. [DOI] [PubMed] [Google Scholar]
- Dandona R, Dandona L, Srinivas M, Sahare P, Narsaiah S, Munoz SR, Pokharel GP, Ellwein LB. Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615–622. [PubMed] [Google Scholar]
- Wu HM, Seet B, Saw SM, Lim TH, Chia KS. Does education explain ethnic differences in myopia prevalence? A population based study of young adult males in Singapore. Optom Vis Sci. 2001;78:234–239. doi: 10.1097/00006324-200104000-00012. [DOI] [PubMed] [Google Scholar]
- Lam CS, Edwards M, Millodot M, Goh WS. A 2-year longitudinal study of myopia progression and optical component changes among Hong Kong schoolchildren. Optom Vis Sci. 1999;76:370–380. doi: 10.1097/00006324-199906000-00016. [DOI] [PubMed] [Google Scholar]
- Lam CSY, Goh WSH. The incidence of refractive errors among school children in Hong Kong and its relationship with the optical components. Clin Exp Optom. 1991;74:97–103. [Google Scholar]
- Chung KM, Mohidin N, Yeow PT, Tan LL, O'Leary D. Prevalence of visual disorders in Chinese schoolchildren. Optom Vis Sci. 1996;73:695–700. doi: 10.1097/00006324-199611000-00004. [DOI] [PubMed] [Google Scholar]
- Edwards MH. The development of myopia in Hong Kong children between the ages of 7 and 12 years: a five-year longitudinal study. Ophthalmic Physiol Opt. 1999;19:286–294. doi: 10.1046/j.1475-1313.1999.00445.x. [DOI] [PubMed] [Google Scholar]
- Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, Lai RY, Chew SJ. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–1075. doi: 10.1167/iovs.03-1151. [DOI] [PubMed] [Google Scholar]
- Yap MK, Cho J, Woo G. A survey of low vision patients in Hong Kong. Clin Exp Optom. 1990;73:19–22. [Google Scholar]
- Matsumura H, Hirai H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv Ophthalmol. 1999;44:S109–115. doi: 10.1016/S0039-6257(99)00094-6. [DOI] [PubMed] [Google Scholar]
- Robbins HG, Bailey IL. The organisation and findings of a school vision screening service. Aust J Optom. 1975;58:392–401. [Google Scholar]
- Amigo G, McCarthy A, Pye D. Visual characteristics of an underprivileged group of Australian children. Aust J Optom. 1976;59:188–197. [Google Scholar]
- Walters J. Portsea Modified Clinical Technique: results from an expanded optometric screening protocol for children. Aust J Optom. 1984;67:176–186. [Google Scholar]
- Nathan J, Kiely PM, Crewther SG, Crewther DP. Disease-associated visual image degradation and spherical refractive errors in children. American Journal of Optometry & Physiological Optics. 1985;62:680–688. doi: 10.1097/00006324-198510000-00003. [DOI] [PubMed] [Google Scholar]
- Macfarlane DJ, Fitzgerald WJ, Stark DJ. The prevalence of ocular disorders in 1000 Queensland primary school children. ANZ J Ophthalmol. 1987;15:161–174. doi: 10.1111/j.1442-9071.1987.tb00066.x. [DOI] [PubMed] [Google Scholar]
- Junghans BM, Crewther SG. The prevalence of myopia among primary school children in eastern Sydney. Clin Exp Optom. 2003;86:339–345. doi: 10.1111/j.1444-0938.2003.tb03130.x. [DOI] [PubMed] [Google Scholar]
- Junghans BM, Crewther SG. The Vision Education Centre: a multi-level educational tool. J Optom Ed. 1992;17:82–86. [Google Scholar]
- Ethnic Affairs Commission of NSW . The people of New South Wales: Statistics from the 1996 census. Sydney , NSW Government; 1998. pp. 149–151. [Google Scholar]
- Young FA, Leary GA, Baldwin WR, West DC, Box RA, Harris E, Johnson C. Comparison of cycloplegic and non-cycloplegic refractions of Eskimos. Am J Optom Arch Am Acad Optom. 1971;48:814–824. doi: 10.1097/00006324-197110000-00003. [DOI] [PubMed] [Google Scholar]
- Ludlum WM, Weinberg SS, Twarowski CJ, Ludlum DP. Comparison of cycloplegic and non-cycloplegic ocular component measurement in children. Am J Optom Arch Am Acad Optom. 1972;49:805–818. doi: 10.1097/00006324-197210000-00001. [DOI] [PubMed] [Google Scholar]
- Hiatt RL, Braswell R, Smith L, Patty JW. Refraction using mydriatic, cycloplegic and manifest techniques. Am J Ophthalmol. 1973;76:739–744. doi: 10.1016/0002-9394(73)90571-0. [DOI] [PubMed] [Google Scholar]
- Schultz L. Variations in refractive change induced by cyclogyl upon children with differing degrees of ametropia. Am J Optom Phsyiol Opt. 1975;52:482–484. doi: 10.1097/00006324-197507000-00006. [DOI] [PubMed] [Google Scholar]
- Chan OYC, Edwards M. Comparison of cycloplegic and noncycloplegic retinoscopy in Chinese pre-school children. Optom Vi Sci. 1994;71:312–318. doi: 10.1097/00006324-199405000-00002. [DOI] [PubMed] [Google Scholar]
- Gao L, Zhou X, Kwok AKH, Yu N, Ma L, Wang J. The change in ocular refractive components after cycloplegia in children. Jpn J Ophthalmol. 2002;46:293–298. doi: 10.1016/S0021-5155(02)00479-3. [DOI] [PubMed] [Google Scholar]
- Chat SW, Edwards MH. Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in children. Ophthalmic Physiol Opt. 2001;21:87–100. [PubMed] [Google Scholar]
- Junghans B, Kiely P, Crewther D, Crewther S. Referral rates for a functional vision screening among a large cosmopolitan sample of Australian children. Ophthal Physiol Opt. 2002;22:10–25. doi: 10.1046/j.1475-1313.2002.00010.x. [DOI] [PubMed] [Google Scholar]
- Zadnik K. The Glenn A. Fry Award Lecture (1995). Myopia development in childhood. Optom Vis Sci. 1997;74:603–608. [PubMed] [Google Scholar]
- Robinson BE. Factors associated with the prevalence of myopia in 6-year-olds. Optom Vis Sci. 1999;76:266–271. doi: 10.1097/00006324-199905000-00011. [DOI] [PubMed] [Google Scholar]
- Curtin BJ. Adult myopia. Acta Ophthalmol. 1988;185S:78–79. doi: 10.1111/j.1755-3768.1988.tb02670.x. [DOI] [PubMed] [Google Scholar]
- Mutti DO, Zadnik K, Egashira S, Kish L, Twelker JD, Adams AJ. The effect of cycloplegia on measurement of ocular components. Invest Ophthalmol Vis Sci. 1994;35:515–527. [PubMed] [Google Scholar]
- Garner LF, Meng CK, Grosvenor TP, Mohidin N. Ocular dimensions and refractive power in Malay and Melanesian children. Ophthalmic Physiol Opt. 1990;10:234–238. doi: 10.1016/0275-5408(90)90004-I. [DOI] [PubMed] [Google Scholar]
- Suryakumar R, Bobier WR. The manifestation of noncycloplegic refractive state in pre-school children is dependent on autorefractor design. Optom Vis Sci. 2003;80:578–586. doi: 10.1097/00006324-200308000-00012. [DOI] [PubMed] [Google Scholar]
- Rose K, Mai TQ, Smith W, Morgan IG, Mitchell P. Prevalance of myopia in school-aged children: comparative data from Sydney and Vietnam. In: XVI International Congress of Eye Reserch: Sydney, Australia. Academic Press; 2004. [Google Scholar]
- Rose K, Smith W, Morgan IC, Mitchell P. Preliminary results from the Sydney Myopia Study. In XVICER Satellite meeting on the Eye and Brain and Myopia: 4 - 7 September 2004; Fraser Island, Australia. 2004. [Google Scholar]
- Baldwin WR. A review of statistical studies of relations between myopia and ethnic, behavioral, and physiological characteristics. Am J Optom Phsyiol Opt. 1981;58:516–527. doi: 10.1097/00006324-198107000-00002. [DOI] [PubMed] [Google Scholar]
- Villarreal MG, Ohlsson J, Abrahamsson M, Sjostrom A, Sjostrand J. Myopisation: the refractive tendency in teenagers. Prevalence of myopia among young teenagers in Sweden. Acta Ophthalmologica Scand. 2000;78:177–181. doi: 10.1034/j.1600-0420.2000.078002177.x. [DOI] [PubMed] [Google Scholar]
- Goldschmidt E, Lam CS, Opper S. The development of myopia in Hong Kong children. Acta Ophthalmol Scand. 2001;79:228–232. doi: 10.1034/j.1600-0420.2001.790303.x. [DOI] [PubMed] [Google Scholar]


