The association of maculopathy with advanced glaucomatous cupping is known, but controversy remains over the origin of fluid.1–3 Reports using enhanced depth imaging have demonstrated a track communicating from cavities posterior to the lamina cribrosa to the peripapillary retina, and these cavities presumably consist of cerebrospinal fluid (CSF).2,3
The protein composition of a fluid can identify its origin. To our knowledge, there have been no previous reports on proteomic analysis of fluid from maculopathy associated with optic nerve excavation. We present a case of advanced glaucomatous cupping in which macular schisis fluid was analyzed for protein content.
Report of a Case
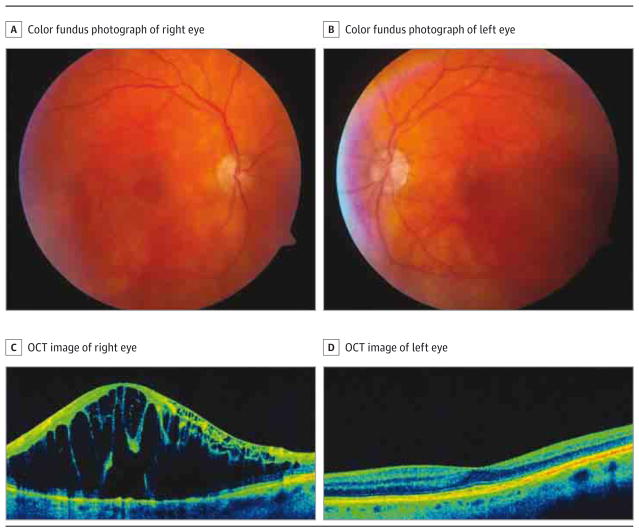
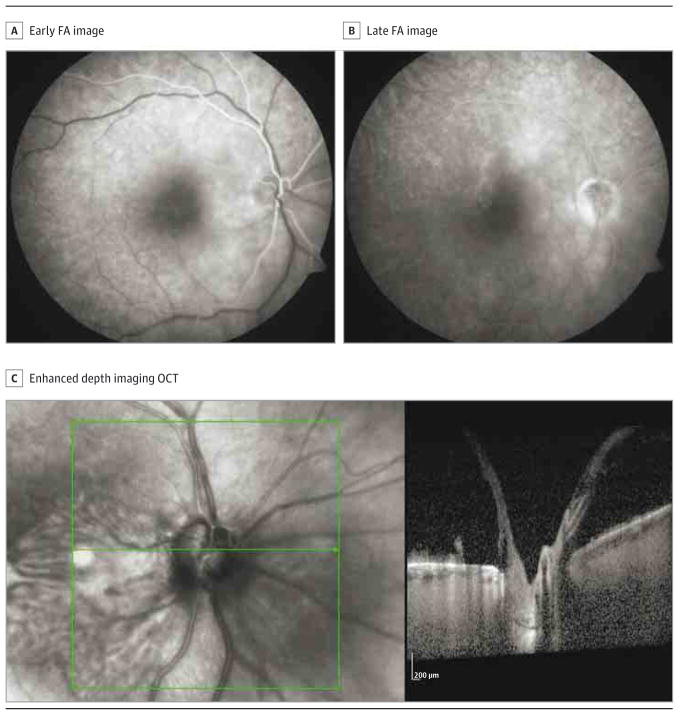
A patient with low-tension glaucoma and advanced cupping presented with progressive loss of vision in her right eye (visual acuity decreased from 20/30 to counting fingers). Fundus examination revealed macular schisis (Figure 1). Enhanced depth imaging optical coherence tomography did not demonstrate an obvious track or visible defect in the lamina cribrosa, and fluorescein angiography did not demonstrate retinal or choroidal leakage (Figure 2).
Figure 1. Color Fundus Photographs and Optical Coherence Tomography (OCT) of the Right and Left Eyes.
A–D, Color fundus photographs of the right (A) and left (B) eyes, and OCT images of the right (C) and left (D) eyes. C, The right eye demonstrates glaucomatous excavation with a large macular schisis cavity on OCT. D, The left eye also shows glaucomatous changes but normal macular architecture.
Figure 2. Fluorescein Angiograms (FAs) and Enhanced Depth Imaging Optical Coherence Tomography (OCT) of the Right Eye.
A and B, Early (A) and late (B) FAs show normal transit time as well as absence of vascular obstruction or vessel leakage. C, Enhanced depth imaging OCT through the optic nerve demonstrates a fluid cavity without visible defect in the lamina cribrosa or communication between the optic nerve and schisis pocket.
Undiluted vitreous was collected at the beginning of vitrectomy surgery before the infusion cannula was opened. A complete vitrectomy was performed, followed by air-fluid exchange. The surface of the macula was then repeatedly dried under air until pooling ceased. A retinotomy superotemporal to the fovea was made with diathermy, a clean 25-gauge soft tip was inserted into the cavity, and viscous fluid was aspirated with visible flattening of the cavity. Endolaser was applied in a limited pattern around the optic nerve, and the air was exchanged with 20% sulfur hexafluoride gas. Approximately 30 μL of undiluted schisis fluid was extracted and immediately stored at −80°C for later analysis. Samples were digested with trypsin prior to proteomic analysis.
Results
Two-dimensional liquid chromatography tandem mass spectrometry4 identified approximately 240 unique proteins in the collected vitreous sample. Peptides derived from opticin, beta-crystallin B2, and alpha-crystallin B were detected and are unique to vitreous (not seen in CSF).5 Because of the small volume of schisis fluid, a more targeted analysis was performed and identified approximately 80 proteins. Opticin, beta-crystallin B2, and a large number of other vitreous proteins were detected in the schisis fluid. No CSF-unique proteins were found.
Discussion
Several theories regarding the mechanism behind maculopathy due to optic nerve abnormalities have been proposed. Accumulation of macular fluid due to transudate from poorly developed peri-papillary choroidal vasculature, liquefied vitreous, and CSF have all been reported as putative sources of macular fluid.3 Several reports using enhanced depth imaging have demonstrated a track extending from the peripapillary retina to cystic cavities posterior to the lamina cribrosa, providing indirect support forCSF,2,3 but no such connection has been confirmed histologically or after subarachnoid injection of india ink in a dog model.6
Proteomic analysis of macular fluid collected in this case confirms the presence of vitreous, which to our knowledge is the first direct clinical evidence that liquefied vitreous can enter the intraretinal or subretinal space (presumably through an optic nerve defect). While vitreous could have contaminated our aspirate, meticulous drying of the retina and direct aspiration of the cavity under air were done to reduce this possibility. While there is no consensus on the treatment of chronic maculopathy, reported methods or combinations thereof include the following: vitrectomy, peripapillary laser, application of fibrin sealant, macular scleral buckling, removal of the internal limiting membrane, internal drainage, and long-acting tamponade. Verification of the source of fluid might influence therapeutic approaches but should be weighed against additional risks.
In conclusion, this detailed proteomic analysis of macular schisis fluid associated with advanced glaucomatous cupping suggests that vitreous was the source of fluid. These findings may have important implications for the management of similar future cases.
Acknowledgments
Funding/Support: This work was supported by an unrestricted grant from Research to Prevent Blindness to the Department of Ophthalmology and Visual Sciences, Vanderbilt University School of Medicine. Dr Kuchtey was supported by grant 5R01EY020894 from the National Eye Institute.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Previous Presentation: This paper was presented in part at the 38th Annual Meeting of the Macula Society; February 25, 2015; Scottsdale, Arizona.
Author Contributions: Drs Patel and Kim had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Patel, Kim, Schey, Rose, Kuchtey.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Patel, Ling, Kim, Schey, Kuchtey.
Critical revision of the manuscript for important intellectual content: Patel, Kim, Schey, Rose, Kuchtey.
Obtained funding: Kim.
Administrative, technical, or material support: Kim, Schey, Rose.
Study supervision: Kim, Kuchtey.
References
- 1.Zumbro DS, Jampol LM, Folk JC, Olivier MM, Anderson-Nelson S. Macular schisis and detachment associated with presumed acquired enlarged optic nerve head cups. Am J Ophthalmol. 2007;144(1):70–74. doi: 10.1016/j.ajo.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 2.Spaide RF. Serous detachment of the macula associated with advanced glaucomatous cupping. Ophthalmic Surg Lasers Imaging Retina. 2014;45(6):598–600. doi: 10.3928/23258160-20141118-18. [DOI] [PubMed] [Google Scholar]
- 3.Gowdar JP, Rajesh B, Giridhar A, Gopalakrishnan M, Hussain R, Thachil T. An insight into the pathogenesis of optic disc pit-associated maculopathy with enhanced depth imaging. JAMA Ophthalmol. 2015;133(4):466–469. doi: 10.1001/jamaophthalmol.2014.6093. [DOI] [PubMed] [Google Scholar]
- 4.Washburn MP, Wolters D, Yates JR., III Large-scale analysis of the yeast proteome by multidimensional protein identification technology. Nat Biotechnol. 2001;19(3):242–247. doi: 10.1038/85686. [DOI] [PubMed] [Google Scholar]
- 5.Aretz S, Krohne TU, Kammerer K, et al. In-depth mass spectrometric mapping of the human vitreous proteome. Proteome Sci. 2013;11(1):22. doi: 10.1186/1477-5956-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown GC, Shields JA, Patty BE, Goldberg RE. Congenital pits of the optic nerve head, I: experimental studies in collie dogs. Arch Ophthalmol. 1979;97(7):1341–1344. doi: 10.1001/archopht.1979.01020020083020. [DOI] [PubMed] [Google Scholar]