Abstract
Background and Objectives:
Inappropriate antimicrobial prescribing is highly reported in dentistry. The objective of the study was to see the effect of dental qualification and practice settings on antimicrobial prescribing practices among dental practitioners in Delhi and National Capital Region (NCR) of India.
Materials and Methods:
A self-designed and pretested questionnaire was given to 667 dental practitioners holding degrees of graduation, postgraduation, and those pursuing postgraduation, working in academic institutions and private clinics in NCR of India. Data were analyzed using statistical software Stata version 12.0. Chi-square and logistic regression tests were used for analysis.
Results:
Out of total 539 responded, 66.4% of the practitioners prescribed by brand name and 27.8% by generic name. Amoxicillin + clavulanic acid (27.4%) was the first choice. Only 26% of the practitioners asked for antimicrobial susceptibility testing. Space infections (91.9%), impacted third molar extractions (89.7%), and periodontal abscess (88.1%) were the conditions where antimicrobials were most frequently prescribed. However, 60.9% and 53.3% of the practitioners also prescribed antimicrobials for acute pulpitis and dry socket, respectively. For prophylaxis in medical conditions, amoxicillin was the first choice. In case of history of allergy to penicillin, 52.3% of the practitioners prescribe erythromycin whereas 14.6% prescribe amoxicillin. The adverse drug reporting culture was negligible, and only 14.3% of the practitioners were aware of the Pharmacovigilance Program of India. Level of qualification had a significant effect on prescribing (P < 0.05).
Interpretation and Conclusion:
Frequent irrational prescribing of antimicrobials used in odontogenic conditions warrants an urgent and continued need for guidelines as well as educational intervention programs in dentistry. This will improve the quality of antimicrobial prescribing practices in dentistry.
Keywords: Antibiotics, dentistry, generic, National Capital Region, pharmacovigilance, prescription pattern
INTRODUCTION
Antimicrobials, when used rationally, for appropriate indications, can be lifesaving. However, prescribing antimicrobials for unwarranted conditions have adverse consequences, for example, development of resistance, adverse drug reactions (ADRs), and drug interactions. In dentistry, antimicrobials should be prescribed for the control of existing local or systemic infections and not for merely relieving pain due to inflammation.[1] Prophylactic antimicrobials are required in only few associated systemic conditions.[2]
Dental practitioners account for nearly 7% of prescribed antimicrobials.[3] Culture sensitivity is seldom carried out in dentistry, and the antimicrobial prescriptions are mostly empirical and at times excessive.[4,5,6,7] Examples of dental conditions where antimicrobials are not required yet commonly prescribed are acute periapical infections, acute pulpitis, dry socket, chronic inflammatory periodontal conditions, periodontal abscess, dentinal hypersensitivity, and cracked tooth.[8,9,10,11] As the essential therapeutic and prophylactic role of antimicrobials is linked with current threat of antimicrobial resistance, it is important to emphasize on appropriate antimicrobial prescription.
The present study was carried out to assess if the qualification and practice settings have any influence on antimicrobial prescribing practices of dental practitioners in Delhi and National Capital Region (NCR) of India.
MATERIALS AND METHODS
This was a cross-sectional study performed among dental practitioners of Delhi and NCR of India.
Study approval
The study was approved by the Institutional Ethics Committee of All India Institute of Medical Sciences (IESC/T-422/28.11.2014).
Study tool
A questionnaire was designed, consisted of open-ended and closed-ended questions, and pretested in twenty dental practitioners who were not the part of the study. The changes suggested by practitioners were included in the final version of questionnaire. In the initial version of the questionnaire, choices for antimicrobials were given, and the results were inconsistent. Hence, instead of choices, open-ended questions were added to evaluate the type of antimicrobials. The validated questionnaire was used to assess the pattern of prescribing, i.e., by brand name or generic, choice of antimicrobials in various dental conditions, use for prophylaxis, and the attitude of the dentist toward culture sensitivity.
Study duration
Duration of the study was 12 months, conducted from December 2014 to November 2015.
Study site and participants
Sample size was estimated based on the results of the previous study[12] on the prevalence of acceptable knowledge among practitioners just passed was found to be 375 (prevalence = 42.2%) with 95% confidence interval and 5% level of significance. Since this was a trend finding regional study involving extensive personal survey, our statistician opined for such number and geographical distribution.
Academic dental institutes (5) and private dental clinics (860) in cities under National Capital Territory of India, i.e., Bahadurgarh, Delhi, Faridabad, Ghaziabad, and Gurgaon were approached. From academic dental institutions, 420 dental practitioners were approached, and total of 388 practitioners agreed to participate. Of 860 registered practicing dentists in private clinics, only 279 agreed to participate. Dentists with master's degree in dentistry and having only bachelor's degree were included in the study.
A prior appointment was taken from the practitioners; questionnaire was given to them personally, and the response was collected at the same time. Each interview took about 30–40 min though it was much difficult for practitioners to spare time.
Statistical analysis
Statistical analysis was done with Stata version 12.0 by StataCorp, USA, using Chi-square test, Fisher's exact test, and univariate logistic regression to see the antimicrobial prescribing habits in relation to level of qualification and type of practice setting in different dental conditions.
RESULTS
Demographic characteristics
Out of 667 dental practitioners, 539 (80.8%) responded. The only reason given by dentists for not participating was nonavailability of time and long waiting list of patients. There were 119 practitioners from Delhi and 420 practitioners from NCR. There were 41% males and 59% females with mean age of 27.9 ± 7.0 years. By qualification, there were 24% graduates, 30% postgraduates, and 46% pursuing postgraduation. Responders from academic institutions were 68% while from private clinics were 32%. Response to close-ended questions was >95% but was variable for open-ended questions.
Prescription pattern of antimicrobials
Out of 539 practitioners, 535 responded, 358 (66.4%) reported prescribing by brand name, 150 (27.8%) by generic name, and 27 (5.19%) by both. The interaction revealed a lack of clarity in understanding of the terms “brand” and “generic.” All participants mentioned multiple sources of updating their information on antimicrobials, journals/books (56.9%) followed by senior practitioners (41.4%), conferences/CMEs/workshops (33.4%), and pharmaceutical representatives (29.2%).
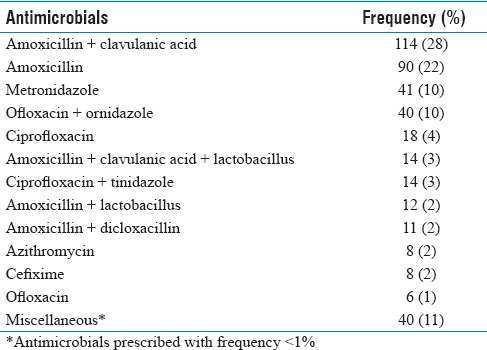
Of 539 practitioners, 416 practitioners responded to the question on choice of antimicrobials. Most of the practitioners prescribe amoxicillin + clavulanic acid (27.4%) followed by amoxicillin (21.6%) and metronidazole (10%) [Table 1]. A wide range of antimicrobials were prescribed either as single medicine formulation (47.3%) and fixed dose combination (FDC) (52.7%). Most commonly prescribed FDC are amoxicillin + clavulanic acid (58.1%) and ofloxacin + ornidazole (18.9%).
Table 1.
Frequency of antimicrobials prescribed by dental practitioners
Dental practitioners with postgraduate degree or pursuing postgraduation prescribed by brand name (72.5%–73.5%) significantly (P = 0.03) less frequently as compared with only graduate degree holders (85.5%). The difference between graduates and postgraduates was statistically significant (P = 0.03) in prescribing by brand name and generic. There was no significant association in prescribing brand and generic with respect to practice settings (P = 0.17).
Five dental conditions were selected where antimicrobial prescribing may (periodontal abscess, impacted third molar with periapical infection, and space infections) or may not be required (acute pulpitis and dry socket). The pattern of prescribing antimicrobials in these conditions was assessed [Table 2 and Figure 1].
Table 2.
Influence of practice setting and qualification on antimicrobial prescribing in various dental conditions
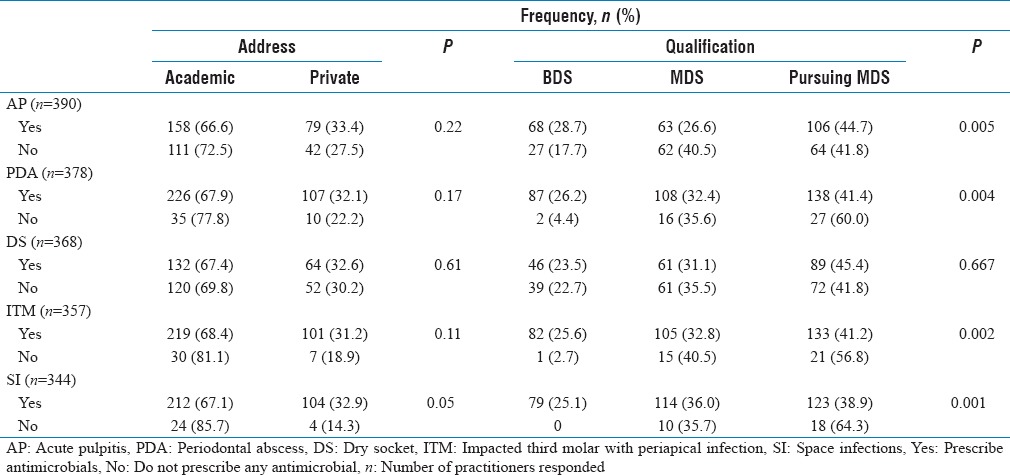
Figure 1.
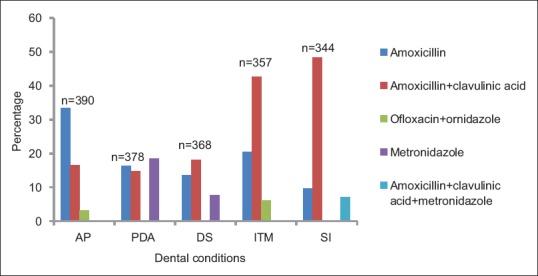
Three most preferred antimicrobials in different dental conditions. AP: Acute pulpitis, PDA: Periodontal abscess, DS: Dry socket, ITM: Impacted third molar with periapical infections, SI: Space infections, n: number of practitioners responded for each situation
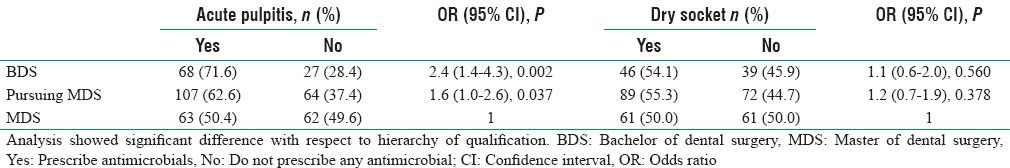
To study the influence of qualification (graduates vs. postgraduates vs. pursuing postgraduation) and practice setting (academic vs. private) on prescribing antimicrobials in acute pulpitis and dry socket, univariate logistic regressions analysis was done. The analysis revealed that antimicrobial prescribing in acute pulpitis was significantly more by those pursuing postgraduation (P = 0.037) and graduates (P = 0.002) as compared to postgraduates. In case of dry socket, although the odds of prescribing antimicrobials (odds ratio: 1.1) were more among graduates and those pursuing postgraduation, result was not significant (P = 0.560) [Table 3]. Except for prescribing in space infections (P = 0.05), no significant association was seen with respect to practice settings of practitioners.
Table 3.
Univariate logistic regression analysis of the influence of qualification (bachelor of dental surgery vs. pursuing master of dental surgery vs. master of dental surgery) on antimicrobial prescription in acute pulpitis and dry socket
In case of history of penicillin allergy, erythromycin (52.3%) was their first choice followed by cephalexin (23.8%), amoxicillin (14.6%), metronidazole (10.3%), and doxycycline (7.5%). For oral candidiasis, the choice of antimicrobials was clotrimazole (47.1%) followed by amphotericin B (39.6%), acyclovir (11.2%), and amoxicillin + clavulanic acid (6.8%). For acute herpetic gingivostomatitis, acyclovir (73.5%), amoxicillin + clavulanic acid (19.2%), clotrimazole (4.5%), and abacavir (3.5%) were prescribed.
Antimicrobial prophylaxis in dental patients
Among all, 405 (75.1%) practitioners were giving prophylactic antimicrobials for infective endocarditis and 320 (59.4%) responded for associated diabetes. Amoxicillin (35% and 17%) and amoxicillin + clavulanic acid (13% and 8%) were the choice for prophylaxis in infective endocarditis and diabetes mellitus, respectively.
Statistically significant difference was found in prescribing antimicrobials for controlled diabetes condition in relation to qualification (postgraduates prescribe more than graduates, P = 0.036) but not with practice settings (P = 0.35). Culture sensitivity and antimicrobial susceptibility testing, in patients not responding to prescribed antimicrobials, was done by 25.7% practitioners.
Attitude toward adverse drug reactions monitoring and reporting
When asked whether their patients report in case of any ADR, 172 (32.2%) said always, 275 (51.5%) rarely, whereas 86 (16.1%) said patients never report the ADR. Majority of the practitioners (467 [87.7%]) reported that <20% of patients experience ADRs.
Out of 539 practitioners, 348 (67.9%) practitioners inform patients of antimicrobial-related possible ADRs before prescription. Practitioners were asked to write the antimicrobials-related frequent adverse effects about which they inform patients, only 157 (29.0%) responded, and gastritis (50 [31.6%]), diarrhea (35 [22.3%]), and allergy (29 [18.5%]) were the most frequent ADRs communicated to the patients. In the presence of an ADR, 69.1% practitioners change the medicine or the dose (6.3%), 46.3% practitioners go for symptomatic relief, and 9.3% practitioners report to concerned authorities.
The Pharmacovigilance Program of India (PvPI) was known to only 14.3% practitioners, and among these, 4.2% practitioners correctly knew about the reporting system and the National Coordinating Centre of PvPI.
DISCUSSION
Dental infections usually do not require antimicrobials as most conditions are treatable by operative intervention. Conditions which may require antimicrobials include space infections, acute necrotizing ulcerative gingivitis, aggressive periodontitis, and periodontal abscess. Yet, inappropriate antimicrobial prescribing has been reported from different parts of the world.[12,13,14,15,16,17]
This study investigated the prescription pattern of antimicrobials among dental practitioners in India. The results show that prescribing did not differ significantly between academic and private practice settings. Postgraduate dental practitioners prescribed antimicrobials more rationally. The trend of higher antimicrobial prescribing by graduates was also reported in a previous Indian study;[5] however, an Iranian study did not show any difference in prescribing behavior with qualification.[18]
A wide range of antimicrobials were prescribed. More than two-third practitioners prescribe by brand name. Although no such study is available in dental context, similar trends have been reported in general medicine prescribing.[16,17] This is despite promotion of generic prescribing by government and the World Health Organization.[19,20] Thus, there is a need for greater emphasis on rational antimicrobial prescribing, especially in dental graduate curriculum.
When asked to mention three preferred antimicrobials, 15% practitioners listed same antimicrobials under different brand names which indicate lack of awareness regarding brand and generic names as well as higher possibility of medication errors. This further stresses the importance of generic prescribing.
Majority of the participants prescribed FDCs. Amoxicillin + clavulanic acid was most frequently prescribed which is rational.[21,22,23] The second most commonly prescribed FDC was ofloxacin + ornidazole which is not considered rational due to the difference in antimicrobial spectrum, pharmacokinetic and pharmacodynamic profile, and increased risk of ADR with the combination.[23,24] Few practitioners also prescribed cloxacillin and dicloxacillin with amoxicillin and cefixime. These combinations have no established synergistic effect.[23,24] Incidentally, a large number of FDCs with questionable rationality are available in Indian market. The practitioners must exercise the academic wisdom not to use irrational FDCs. Not prescribing such FDCs will be the best auto-correction strategy.
Amoxicillin + clavulanic acid, amoxicillin, and metronidazole were the most commonly prescribed antimicrobials. Similar trend was reported by Hamoudi et al.[10] In case of patients allergic to penicillins, more than 80% responses were appropriate, but it was disappointing to note that some would prescribe amoxicillin (another penicillin) to such allergic patients.
Dental conditions that require antimicrobials are few. These include space infections, acute necrotizing ulcerative gingivitis, aggressive periodontitis, and periodontal abscess which are often associated with signs of systemic involvement such as elevated body temperature and lymphadenopathy.[7] Acute pulpitis and dry socket are not indications for antimicrobial therapy, yet in our study, one-third to half of the practitioners prescribed antimicrobials for these conditions. Some may prescribe antibacterials for oral candidiasis (fungal infection) and acute herpetic gingivostomatitis (viral infection) as well. It is possible that some specific reason could be there to prescribe a particular antimicrobial which could not be captured by us in interview.
Prescribing drugs in hospitals where medicines are given free and not free may influence the trend. It can be done in extended study focusing more number of both type of hospital setups that is public and private hospitals.
Antimicrobial prophylaxis is recommended for patients with existing heart disease but not for controlled diabetes mellitus.[2,25] In this study, majority of practitioners responded prescribing in infective endocarditis. However, more than one-third practitioners recommend prophylaxis for diabetic patients otherwise controlled on oral hypoglycemic.
The present study reveals that although dental practitioners come across ADRs, they do not report them and do not actively seek ADRs. Some studies were carried out in India to assess the knowledge of health-care practitioners regarding pharmacovigilance have revealed variable levels of awareness and ADR reporting.[26,27] PvPI has been targeting health-care professionals since its inception. However, reporting by dental practitioners has not been assessed. Pharmacovigilance and ADRs were included in the study to sensitize the dental practitioners for ADR reporting. We observed that most dental practitioners were not even aware of the term pharmacovigilance. Knowledge of PvPI has been included as an additional knowledge and attitude assessment as what they do if any adverse reaction to antibiotic is observed. This would also indirectly improve their rational prescribing.
Few developed countries have antimicrobial prescribing guidelines for dental conditions such as Scottish Dental Clinical Effectiveness Programme Medicine Prescribing for Dentistry, National Guideline Clearinghouse, and National Institute of Health and Clinical Excellence, however, in India no such guidelines exist. Better prescribing trend is expected in developed and more regulated countries. A future multicountry study can address this issue.
The Indian Council of Medical Research has initiated antimicrobial stewardship program which aims to restrict inappropriate use of antimicrobials, optimize selection, dose, route and duration of the treatment for best outcomes, minimizing detrimental adverse events, excessive costs, and emergence of resistance. The team involved in this program mainly consists of infectious disease physician, clinical pharmacologist/pharmacist, clinical microbiologist, infection control nurse, and the hospital administrator.[28] We recommend inclusion of dental practitioners as part of the stewardship program.
Antimicrobial overprescribing is common in dentistry and is an important contributor to antimicrobial resistance. The present study indicates high irrational antimicrobial prescribing in dentistry. This emphasizes the need for developing national guidelines for antimicrobial use in dental conditions. Practicing such guidelines will go a long way in controlling antimicrobial resistance. Academic institutes and dental organizations should take lead to effectively catalyze the training and awareness for rational use of antimicrobials in dental practice.
Limitation of the study
The results of the study would have been more convincing if analysis of antimicrobial prescriptions issued by practitioners was done to come to an evidence-based conclusion.
CONCLUSION
Antimicrobial overprescribing is common in dentistry and is a major contributor to antimicrobial resistance. The present study indicates a high incidence of irrational antimicrobial prescribing in dentistry. The lack of awareness observed in the study emphasizes the need for developing national guidelines for antimicrobial use in dental conditions. Practicing such guidelines will go a long way in controlling antimicrobial resistance. Academic institutes and relevant dental organizations should take lead to effectively catalyze the training and awareness for rational use of antimicrobials in dental practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Cope A, Francis N, Wood F, Mann MK, Chestnutt IG. Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults. Cochrane Database Syst Rev. 2014;6:CD010136. doi: 10.1002/14651858.CD010136.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, et al. Prevention of infective endocarditis: Guidelines from the American Heart Association: A guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007;116:1736–54. doi: 10.1161/CIRCULATIONAHA.106.183095. [DOI] [PubMed] [Google Scholar]
- 3.Spencer RC. The path of least resistance. J Antimicrob Chemother. 1999;43:437–8. [Google Scholar]
- 4.Chitturi RT, Ramesh V, Priyanka R, Senthilnathan N, Elanagai R. The role of dental surgeons in combating medicine resistance: A study in South India. Int J Nutr Pharmacol Neurol Dis. 2014;4(Suppl S1):12–6. [Google Scholar]
- 5.Garg AK, Agrawal N, Tewari RK, Kumar A, Chandra A. Antibiotic prescription pattern among Indian oral healthcare providers: A cross-sectional survey. J Antimicrob Chemother. 2014;69:526–8. doi: 10.1093/jac/dkt351. [DOI] [PubMed] [Google Scholar]
- 6.Karibasappa GN, Sujatha A. Antimicrobial resistance – A concern for dentists? IOSR J Dent Med Sci. 2014;3:112–8. [Google Scholar]
- 7.Dar-Odeh NS, Abu-Hammad OA, Al-Omiri MK, Khraisat AS, Shehabi AA. Antibiotic prescribing practices by dentists: A review. Ther Clin Risk Manag. 2010;6:301–6. doi: 10.2147/tcrm.s9736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fedorowicz Z, van Zuuren EJ, Farman AG, Agnihotry A, Al-Langawi JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev. 2013;12:CD004969. doi: 10.1002/14651858.CD004969.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Noroozi AR, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: Comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:30–5. doi: 10.1016/j.tripleo.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 10.Hamoudi NM, Fuoad SA, Aziz Z, Saddeq M. Antibiotic utilization pattern in dental practice in Ajman, UAE: A prospective study. J Adv Sci Res. 2013;4:17–20. [Google Scholar]
- 11.Newman MG, Takei H, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. 11 edition. Saunders; 2011. [Google Scholar]
- 12.Al-Huwayrini L, Al-Furiji S, Al-Dhurgham R, Al-Shawaf M, Al-Muhaiza M. Knowledge of antibiotics among dentists in Riyadh private clinics. Saudi Dent J. 2013;25:119–24. doi: 10.1016/j.sdentj.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gour PR, Kohli S, Advani U, Kulshreshtha S, Jain A, Parakh R. Prescription pattern of antimicrobial agents by dental practitioners: A questionnaire based study. Int J Basic Clin Pharmacol. 2013;2:311–4. [Google Scholar]
- 14.Rachmawati MW, Yoshida N, Tsuboi H, Kimura K. Investigation of antimicrobial use at a dental teaching hospital in Yogyakarta, Indonesia: A review from guidelines. Pharmacol Pharm. 2014;5:524–31. [Google Scholar]
- 15.Lewis MA. Why we must reduce dental prescription of antibiotics: European Union Antibiotic Awareness Day. Br Dent J. 2008;205:537–8. doi: 10.1038/sj.bdj.2008.984. [DOI] [PubMed] [Google Scholar]
- 16.Tamuno I. Prescription pattern of clinicians in private health facilities in Kano, Northwestern Nigeria. Asian Pac J Trop Dis. 2011;1:235–8. [Google Scholar]
- 17.Babalola CP, Awoleye SA, Akinyemi JO, Kotila OA. Evaluation of prescription pattern in Osun state (Southwest) Nigeria. J Public Health Epidemiol. 2011;3:94–8. [Google Scholar]
- 18.Kia SJ, Behravesh M, Khalighi SF. Evaluation of medicine prescription pattern among general dental practitioners in Rasht, Iran. J Dentomaxillofac Radiol Pathol Surg. 2012;1:18–23. [Google Scholar]
- 19.Medical Council of India. [Last accessed on 2016 Mar 10]. Available from: http://www.mciindia.org/tools/announcement/Circular_Ethics_21.01.2013.pdf .
- 20.The Rational Use of Medicines. Report of the Conference of Experts Nairobi; 25-29 November. 1985. [Last accessed on 2016 Mar 10]. Available from: http://www.who.int/medicines/en/
- 21.Bratton TA, Jackson DC, Nkungula-Howlett T, Williams CW, Bennett CR. Management of complex multi-space odontogenic infections. J Tenn Dent Assoc. 2002;82:39–47. [PubMed] [Google Scholar]
- 22.Sulejmanagic N, Sulejmanagic H, Ljutovic Z, Salihagic D, Sijercic M. Combined application of amoxicillin and clavulanic acid after oral surgical interventions. Bosn J Basic Med Sci. 2005;5:61–8. doi: 10.17305/bjbms.2005.3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gautam CS, Saha L. Fixed dose drug combinations (FDCs): Rational or irrational: A view point. Br J Clin Pharmacol. 2008;65:795–6. doi: 10.1111/j.1365-2125.2007.03089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balat JD, Gandhi AM, Patel PP, Dikshit RK. A study of use of fixed dose combinations in Ahmedabad, India. Indian J Pharmacol. 2014;46:503–9. doi: 10.4103/0253-7613.140581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Academy on Pediatric Dentistry Clinical Affairs Committee; American Academy on Pediatric Dentistry Council on Clinical Affairs. Guideline on antimicrobial prophylaxis for dental patients at risk for infection. Pediatr Dent 2008. 2009;30(7 Suppl):215–8. [PubMed] [Google Scholar]
- 26.Arulmani R, Rajendran SD, Suresh B. Adverse drug reaction monitoring in a secondary care hospital in South India. Br J Clin Pharmacol. 2008;65:210–6. doi: 10.1111/j.1365-2125.2007.02993.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desai CK, Iyer G, Panchal J, Shah S, Dikshit RK. An evaluation of knowledge, attitude, and practice of adverse drug reaction reporting among prescribers at a tertiary care hospital. Perspect Clin Res. 2011;2:129–36. doi: 10.4103/2229-3485.86883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandy SJ, Michael JS, Veeraraghavan B, Abraham OC, Bachhav SS, Kshirsagar NA. ICMR programme on antibiotic stewardship, prevention of infection and control (ASPIC) Indian J Med Res. 2014;139:226–30. [PMC free article] [PubMed] [Google Scholar]


