Abstract
Objective
Although most people will experience a traumatic event, only some will develop significant psychological symptoms in the aftermath. In the current study, we utilize a preexisting longitudinal study located in Long Island to examine the impact of Hurricane Sandy on internalizing symptoms in a large sample of children. We focused on temperamental fear and a biomarker of risk for anxiety, the error-related negativity (ERN). The ERN is a negative deflection in the event-related potential (ERP) occurring when individuals make mistakes and is increased in anxious individuals.
Method
The final sample consisted of 223 children who had undergone an observational assessment of fear at age 3 and an electroencephalogram assessment of the ERN at age 6. At the age 9 assessment, internalizing symptoms were assessed, and then again after the hurricane (approximately 65 weeks later).
Results
A significant three-way interaction between fearfulness, hurricane stressors, and the ERN in predicting post-hurricane increases in internalizing symptoms suggested that children who were high in fear at age 3 and experienced elevated hurricane stressors were characterized by subsequent increases in internalizing symptoms, but only when they were also characterized by an increased ERN at age 6.
Conclusion
These findings support a diathesis-stress model, suggesting that early temperament and pre-stressor biological markers confer risk for increased psychological symptoms following environmental stressors.
Keywords: biomarker, error-related negativity, anxiety, trauma, developmental psychopathology
INTRODUCTION
Although most people will experience a traumatic event at some point in their lives, only a subset will develop significant psychological symptoms in the aftermath; approximately 5 – 10%.1–3 Given that epidemiologic studies suggest that an enduring stress response is not an inevitable consequence of trauma, there has been substantial interest in identifying pre-trauma factors that may confer risk for trauma-related increases in symptomatology.4–6
Natural disasters are a unique occasion to explore such factors, given that exposure to such events is typically unrelated to pre-trauma individual differences. In 2012, Hurricane Sandy hit New York State and surrounding regions, impacting 60 million people. The hurricane destroyed 200,000 homes, cost an estimated $50 billion in damages, and resulted in 113 US deaths.7 We recently utilized a pre-existing longitudinal study located in Long Island, New York8 to examine the impact of Hurricane Sandy stressors on anxiety symptoms in a large sample of children. Adjusting for pre-Sandy symptoms, higher levels of stress from Hurricane Sandy predicted elevated levels of anxiety symptoms, but only in children characterized by increased temperamental fear measured 7 years prior to the hurricane when children were 3 years old.9 These findings support a diathesis-stress model, suggesting that temperament plays an important and enduring role in the development of psychopathology in the context of stressful life events.
In the current study, we build on these findings and examine to what extent pre-hurricane neural biomarkers may interact with temperamental risk to predict increases in symptoms after the hurricane. Although some work in adults has identified neural biomarkers of risk that predict increases in post-trauma anxiety,10–13 very little work has yet focused on biomarkers that confer risk for post-trauma anxiety symptoms in children.14 The significance of this gap is underscored in the literature, which denotes that anxiety frequently onsets early in life15–17 and often results in chronic impairment through adulthood.18–20 Additionally, some research suggests that children may be particularly vulnerable to the impact of environmental adversity.21 Understanding early biomarkers that may confer risk for the development of anxiety in response to stressful life events may be important for understanding the etiopathogenesis of anxiety and additionally may have considerable implications for the implementation and development of psychiatric intervention and prevention strategies.
One promising biomarker of anxiety is an event-related potential (ERP), the error-related negativity (ERN).22,23,24 The ERN, which is a negative deflection in the ERP occurring when participants make mistakes during a speeded response task,25,26 has been found to be increased in individuals with anxiety in over 40 studies to date.23,24 Additionally, unaffected first-degree relatives of individuals with obsessive-compulsive disorder (OCD) are characterized by an increased ERN.27,28 The ERN appears to be trait-like, demonstrating excellent test-retest reliability in children and adults for up to 2 years,29,30 and has been shown to be moderately heritable 45 – 60%.31 The ERN has also been shown to prospectively predict the onset of new anxiety disorders in young children, while controlling for baseline symptoms,22 suggesting that an increased ERN may be a viable early-emerging biomarker of risk for anxiety. Similarly, two prospective studies found that among children high in early temperamental behavioral inhibition, an increased ERN predicted anxiety later in development.32,33 For example, Lahat et al. (2014) found an interaction between early childhood behavioral inhibition (BI, assessed at 24 and 36 months of age) and the ERN measured at age 7 in predicting symptoms of social phobia in children 2 years later, such that children characterized by high BI and an increased ERN were particularly at risk for developing anxiety.
The current study sought to extend these findings to examine whether the ERN and temperamental fear may confer risk for stress-induced increases in anxiety symptoms. This question was addressed in an ongoing longitudinal sample that was exposed to Hurricane Sandy and had pre-hurricane assessments of temperamental fear, ERN, and internalizing symptoms. Temperamental fearfulness was assessed when the children were three years old via laboratory-based observations; three years later, when the children were approximately 6 years old, the ERN was measured while children completed a Go-NoGo task. Children returned to the lab 3 years later (around age 9), and mothers reported on child internalizing and externalizing symptoms. Approximately 8 weeks after Hurricane Sandy hit Long Island, children’s mothers completed a questionnaire assessing exposure to hurricane-related stressors as well as children’s internalizing and externalizing symptoms. We have previously shown that higher levels of hurricane-related stress predicted increases in anxiety symptoms, but only among children characterized by increased temperamental fear. We seek to extend those findings by testing the hypothesis that an increased ERN would also relate to increased vulnerability and that the children who are at highest risk for hurricane-related increases in internalizing symptoms are characterized by both high fear and high ERN. We begin by examining broad internalizing symptoms, as well as a comparable model utilizing externalizing symptoms in order to examine specificity. We hypothesized that neither fear nor the ERN would predict increases in post-hurricane externalizing symptoms. However, we hypothesized that an elevated ERN would relate to increased vulnerability for increases in internalizing symptoms that would be driven by post-hurricane increases in anxiety symptoms.
METHOD
The sample for the current study consisted of 223 children (initially between the ages of 3.00 – 4.09 years, SD = .26) and their mothers from a larger longitudinal study of 559 children (for details, see8). Participants were recruited through a commercial mailing list and screened to select children with no significant medical problems or developmental disabilities and who had at least one English-speaking biological parent who could participate in the study. As part of this longitudinal study, mothers and children were assessed at three-year intervals (i.e., at approximately 3 years of age, 6 years of age, and 9 years of age). An additional 50 children were added at the age 6 assessment to increase the diversity of the sample.
Of the total sample, 446 had completed age 9 assessments prior to hurricane Sandy, and these families were contacted to complete a post-Sandy assessment. Eighty-one percent (362 families) agreed to participate. Of these families, 15 were excluded because they were not on Long Island when Hurricane Sandy occurred, and 15 were excluded because they entered the study at age 6 and didn’t have laboratory measures from age 3. Of the 332 remaining children, 223 had adequate ERN data from the age 6 assessment. In order to be included in ERN analyses, participants had to have at least 6 artifact-free error trials,30,34 which led to the exclusion of 74 children. Thirty-four children had not completed the age 6 electroencephalogram (EEG) assessment, and ERP data from one participant was lost due to technical error. Children who participated in the current study did not differ from the larger sample on any of the study variables (pre- or post-Sandy internalizing Child Behavior Checklist [CBCL] symptoms, total hurricane Sandy stressors, age 6 ERN, or age 3 fear), all ps > .10.
The final sample thus consisted of 223 children (95 female). The average age at the first assessment was 3.57 years, SD = .26. The average age at the second assessment was 6.13 years, SD = .38. The average age at the third assessment was 9.19 years, SD = .32. Children’s post-hurricane symptoms were assessed an average of 8.39 weeks, SD = 1.39 after Hurricane Sandy occurred, which was an average of 64.97 weeks, SD = 32.59 since their age 9 assessment. Overall, 91% of the children were Caucasian and non-Hispanic. All of the families in the current study lived in Federal Emergency Management Agency (FEMA)-declared disaster zones.
Procedure
During the first assessment, participants completed the Laboratory Temperament Assessment Battery (Lab-TAB; Goldsmith HH, Reilly J, Lemery KS, Longley S, Prescott A, Preschool Laboratory Temperament Assessment Battery [Unpublished instrument], University of Wisconsin, 1995), which provided a measure of temperamental fear. During the second assessment, when children were approximately 6 years old, they completed a Go-NoGo task while EEG was recorded to measure the ERN. At the third assessment, when children were approximately 9 years old, mothers completed the CBCL,35 as a measure of their children’s internalizing and externalizing symptoms. Six weeks after Hurricane Sandy, mothers were contacted and asked to complete the CBCL again, in addition to a measure of hurricane-related stress. This study was approved by the local institutional review board.
Measures
Child fearfulness
At age 3, children participated in 12 age-appropriate episodes from the Lab-TAB (Goldsmith HH et al., 1995) that were designed to elicit a range of temperamentrelevant behaviors and emotions described in detail.8 During each videotaped episode, instances of facial, vocal, and bodily fear were rated on a four-point intensity scale and then summed across each episode. These ratings were then averaged across the 12 episodes to yield a composite score for fear (α = .63). Interrater reliability of the fear composite, assessed using the intraclass correlation coefficient (ICC), was .64 (n = 35).
Internalizing and externalizing symptoms pre- and post-Sandy
At the age 9 and post-Sandy evaluations, children’s internalizing and externalizing symptoms were assessed via mother’s reports on the CBCL.35 The CBCL is a 113-item parent-report checklist assessing emotional and behavioral problems in children. In the current study, we focused on composite internalizing and externalizing symptoms. At the age 9 assessment, items were rated for the past 6 months. In the post-Sandy assessment, mothers were asked to rate symptoms in the period since Hurricane Sandy (an average of 8.39 weeks).
Hurricane Sandy stressors
Approximately 6 weeks after the hurricane, mothers were asked to complete a 13-item web-based questionnaire on the effects of the hurricane on families and children.9,36,37 The items were drawn from previous questionnaires developed for Hurricane Katrina38 and Hurricane Ike.39 The first 8 items were rated on a 5-point scale (1 = not at all affected, 5 = extremely affected), and included damage to home, safety threatened, financial hardship, children fear for their safety, life disrupted by the hurricane, difficulty finding gasoline, difficulty getting food, water, or warmth, and children quarreling or complaining more than usual. Items 9 and 10 were rated on duration (1 = 0 days, 5 = 2 weeks or more) and included loss of power and school closure. Items 11 – 13 were rated as present or absent and included questions regarding injury or robbery, applying to FEMA or the Red Cross, and being evacuated from the home. To create an overall sum of exposure severity, non-dichotomous items were scored 1 = present and 0 = absent using a cutoff score determined through a combination of statistical and clinical considerations to distinguish a subgroup of participants with significant levels of stress on each item (for detailed description, see9). Total scores ranged from 0 – 11, M = 2.28, SD = 2.18, and the scale showed adequate internal consistency (α = .73).
Error-related brain activity
At age 6, children were administered a Go/No-Go task with Presentation software (Neurobehavioral Systems, Inc.) to measure the ERN previously described.40,41 The stimuli were green equilateral triangles presented in one of four different orientations for 1,200 ms in the middle of the monitor. On 60% of the trials, triangles were vertically aligned and pointed up, 20% were vertically aligned and pointed down, 10% were tilted slightly to the left, and 10% were tilted slightly to the right. Children were told to respond to upward-pointing triangles by pressing a button, and to withhold a response to all other triangles. Following the presentation of the triangle and prior to the start of the next trial, a small gray fixation cross was displayed in the middle of the monitor for a random interval that ranged from 300 to 800 ms. Children completed four blocks of 60 trials each.
The Active Two system (Biosemi, Amsterdam, Netherlands) was used to acquire EEG data, and 32 Ag/AgCI-tipped electrodes were used with a small amount of electrolyte gel (Signa Gel; Bio-Medical Instruments Inc., Warren, Michigan) at each electrode position. All data were sampled at 512 Hz. The ground electrode during acquisition was formed by the common mode sense active electrode and the driven right leg passive electrode.
Data was processed offline with Brain Vision Analyzer (Brain Products, Gilching, Germany). EEG data was re-referenced to the nose and high and low pass filtered at 0.1 Hz and 30 Hz, respectively. EEG segments of 1,500 ms were extracted from the continuous EEG, beginning 500 ms prior to responses. Data was then corrected for eye movements and blinks,42 and artifacts were rejected if any of the following criteria were met: a voltage step of more than 50 microvolts between data points, a voltage difference of 300 microvolts within a single trial, or a voltage difference of less than 0.5 microvolts within 100 ms intervals. After this, data were visually inspected for remaining artifacts. ERP averages were created for error and correct trials and a baseline of the average activity from −500 to −300 ms prior to the response was subtracted from each data point.
ERP and behavioral results in the full sample have been previously reported.41 The error-related negativity (ERN) and correct-related negativity (CRN) were scored as the average voltage in the window between 0 ms and 100 ms after response commission on error and correct trials, respectively; the CRN and ERN were quantified at Fz, where error-related brain activity was maximal. The delta ERN (ΔERN), thought to reflect error-specific activity, was calculated by subtracting the CRN from the ERN.
All statistical analyses were conducted using SPSS (Version 17.0) General Linear Model software, with Greenhouse-Geisser correction applied to p values with multiple-df, repeatedmeasures comparisons when necessitated by violation of the assumption of sphericity. We utilized a nonparametric bootstrapping method43 to conduct moderation analyses. To test interactions, we used an SPSS macro,44 which provided an estimate using 5,000 bootstrap samples. We examined a model wherein Age 9 (pre-Sandy) CBCL internalizing symptoms were controlled for and the three-way interaction between temperamental fearfulness × Hurricane Sandy stressors × age 6 ΔERN was entered predicting post-Sandy CBCL internalizing symptoms in children. In this model, all main effects and two-way interactions were included as well (i.e., fear × stressors, fear × ΔERN, stressors × ΔERN). We then examined the same model, this time utilizing age 9 CBCL externalizing symptoms (pre- and post-Sandy).
RESULTS
Descriptive Statistics and Bivariate Correlations
As previously reported,40,41,45 the ERP response was more negative following errors than correct responses (F[1,222] = 90.08, p < .001; Figure 1). Means and standard deviations as well as Pearson correlations are presented for all main study variables in Table 1. Hurricane stressors related to post-hurricane internalizing symptoms (r[221] = .16, p < 05). Additionally, prehurricane internalizing symptoms predicted post-hurricane internalizing symptoms (r[221] = .56, p < .01), as well as post-hurricane externalizing symptoms (r[.221] = .31, p < .01). Similarly, pre-hurricane externalizing symptoms predicted post-hurricane externalizing symptoms (r[221] = .59, p <01), as well as post-hurricane internalizing symptoms (r[221] = .38, p < .01). Neither child fearfulness nor the ΔERN was significantly related to any other study variables (all ps > .05). Additionally, neither gender nor child age (at any of the assessments) related to any of the study variables (all ps > .05).
Figure 1.
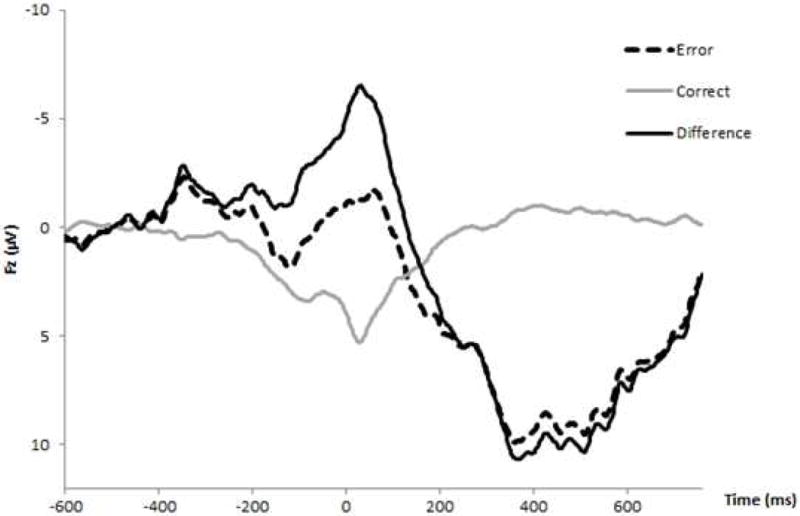
Response-locked event-related potential (ERP) waveform for correct and error trials, as well as the difference wave (error minus correct) for the entire sample at Fz.
Table 1.
Pearson Correlation Coefficients, as well as Means and Standard Deviations (SD) for the Difference Error-Related Negativity (ΔERN) Temperamental Fearfulness, Hurricane Stressors, Pre- and Post-Hurricane Internalizing and Externalizing Symptoms
| 1 | 2 | 3 | 4 | 5 | 6 | Mean | SD | |
|---|---|---|---|---|---|---|---|---|
| 1. ΔERN | – | −5.19 | 8.16 | |||||
| 2. Age 3 fearfulness | .09 | – | −.02 | 1.01 | ||||
| 3. Hurricane stressors | −.07 | .06 | – | 2.28 | 2.18 | |||
| 4. Pre-hurricane Internalizing symptoms | −.07 | .11 | −.01 | – | 3.97 | 4.97 | ||
| 5. Post-hurricane internalizing symptoms | .02 | .09 | .16* | .56** | – | 2.15 | 3.27 | |
| 6. Pre-hurricane externalizing symptoms | −.00 | .09 | −.00 | .54** | .38** | – | 4.61 | 5.32 |
| 7. Post-hurricane externalizing symptoms | .10 | .06 | .04 | .31** | .59** | .63** | 2.43 | 4.56 |
Predicting Post-Hurricane Increases in Internalizing Symptoms
We examined a model wherein baseline age 9 (pre-Sandy) CBCL internalizing symptoms were entered as a covariate and the three-way interaction between temperamental fearfulness × hurricane stressors × ΔERN was entered predicting post-Sandy CBCL internalizing symptoms in children, as well as all main effects and two-way interactions. Results are displayed in Table 2. The overall model was significant (F[8, 214] = 15.37, p < .001), accounting for 36% of the variance. In this model, there was a main effect of pre-hurricane internalizing symptoms (β = .37, SE = .04, t = 10.05, p < .001, 95% CI: .29 to .44) and hurricane stressors (β = .26, SE = .10, t = 2.48, p < .01, 95% CI: .05 to .46) in predicting post-hurricane internalizing symptoms. No other main effects nor any two-way interactions reached significance (all ps > .10).
Table 2.
Results From a Model Wherein Baseline Age 9 (Pre-Sandy) Child Behavior Checklist (CBCL) Internalizing Symptoms Were Entered as a Covariate and the Three-Way Interaction Between Temperamental Fearfulness × Hurricane Stressors × Difference Error-Related Negativity (ΔERN) Was Entered Predicting Post-Sandy CBCL Internalizing Symptoms in Children, as well as all Main Effects and Two-Way Interactions
| Post-hurricane internalizing symptoms | |||
|---|---|---|---|
| Variables entered | B | SE (N = 223) | t |
| Pre-hurricane internalizing symptoms | .37 | .04 | 10.05** |
| Hurricane stressors | .26 | .10 | 2.48** |
| Fear | .00 | .22 | .01 |
| ΔERN | .01 | .02 | .56 |
| Fear × hurricane stressors | −.03 | .10 | −.33 |
| Fear × ΔERN | −.02 | .02 | −.74 |
| Hurricane stressors × ΔERN | −.01 | .01 | −.55 |
| Fear × hurricane stressors × ΔERN | −.02 | .01 | −2.42** |
| Overall model: total R-squared | .36** | ||
| R-squared increase due to 3- way interaction | .02** | ||
Note: SE = standard error.
p < .05,
p < .01
However, this was qualified by a significant three-way interaction between temperamental fearfulness, hurricane stressors, and the ΔERN in predicting changes in child internalizing symptoms after Hurricane Sandy (β = −.02, SE = .01, t = −2.42, p < .01, 95% CI: − .04 to −.01). Post hoc analyses suggested that the two-way interaction between child fearfulness and stressors was significant only among children with a larger ΔERN (β = .25, SE = .10, t = 2.44, p < .01, 95% CI: .05 to .45), such that children who were higher in temperamental fear at age 3 and experienced elevated hurricane Sandy stressors were characterized by subsequent increases in internalizing symptoms, but only when they were also characterized by an increased ΔERN at age 6. Using the Johnson-Neyman technique for identifying regions of significance, the two-way interaction between fear and stressors was significant only among children characterized by an ΔERN with values between −30 and −12 (between 1 and 3 SDs more negative than the mean; all ps < .01). As depicted in Figure 2, children rated as fearful in the lab whose mothers were perceived to be impacted by hurricane stressors had significant increases in symptoms, but only when they also had a large ΔERN (shown on the top; based on a median split). Among children with a small ΔERN (shown on the bottom; based on a median split), there is no significant interaction between temperamental fearfulness and hurricane stressors in predicting change in internalizing symptoms. When child age and gender were entered into the model as covariates, the pattern of results did not change, i.e., there was a significant three-way interaction between fear, hurricane stressors, and the ΔERN in predicted changes in child internalizing symptoms (β = −.02, SE = .01, t = −2.39, p < .01, 95% CI: −.04 to −.01).
Figure 2.
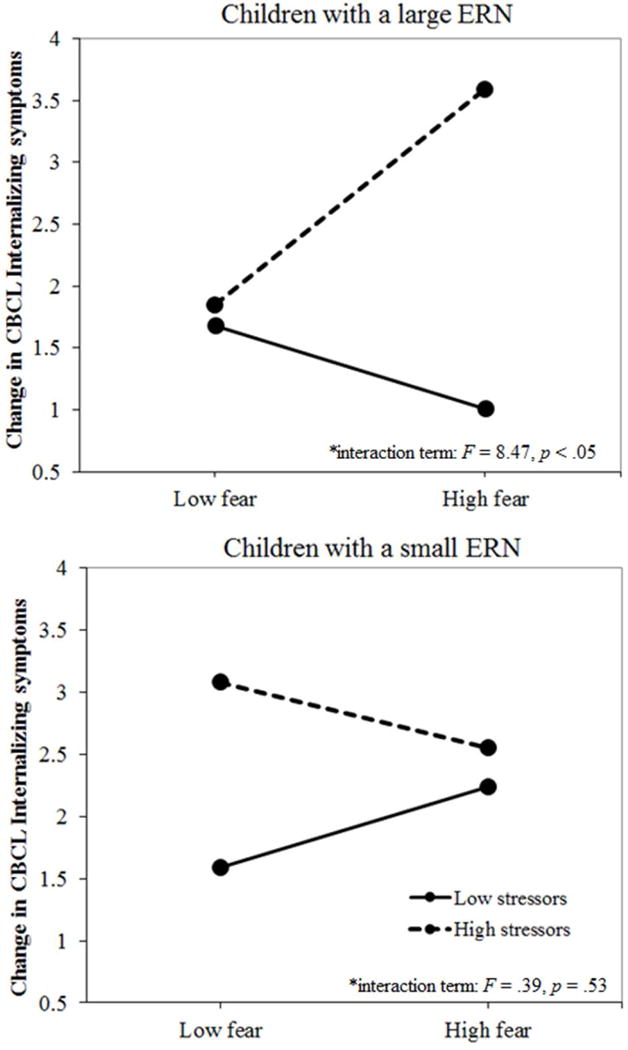
The three-way interaction between the difference error-related negativity (ΔERN), temperamental fearfulness, and hurricane stressors in predicting post-hurricane increases in internalizing symptoms. Note: Fearful children were impacted by hurricane stressors, but only when they also have a large ΔERN (shown on the top; based on a median split), F(1,105) = 8.47, p < .05. Amongst children with a small ΔERN (shown on the bottom; based on a median split), there is no significant interaction between temperamental fearfulness and hurricane stressors in predicting changes in internalizing symptoms, F(1,105) = .39, p = .53. CBCL = Child Behavior Checklist.
To further examine this interaction and determine specificity, we repeated the same model three times, with each of the subscales within the internalizing composite (anxious/depressed, withdrawn/depressed, and somatic complaints) entered as both the pre- and post-hurricane symptom scales. When we did this, the three-way interaction between fear, stressors, and the ΔERN significantly predicted changes in the anxious/depressed subscale (β = − .01, SE = .01, t = −2.38, p < .01, 95% CI: −.03 to −.01). However, the three-way interaction predicting changes in either withdrawn/depressed symptoms or somatic complaints was not significant (both ps > .10).
Predicting Post-Hurricane Increases in Externalizing Symptoms
Finally, we examined a model wherein baseline age 9 (pre-Sandy) CBCL externalizing symptoms were entered as a covariate and the three-way interaction between temperamental fearfulness × hurricane stressors × ΔERN was entered predicting post-Sandy CBCL externalizing symptoms in children, as well as all two-way interactions. The overall model was significant (F[8, 214] = 19.70, p < .001), accounting for 42% of the variance. In this model, there was a main effect of pre-hurricane externalizing symptoms (β = .54, SE = .05, t = 12.06, p < .001, 95% CI: .45 to .63). However, there was no main effect of hurricane stressors on changes in externalizing symptoms (β = .10, SE = .14, t = 0.76, p = .44, 95% CI: −.17 to .38). Additionally, no other main effects, nor any two-way interactions or the three-way interaction, reached significance (all ps > .10).
DISCUSSION
The current study examined the ERN in conjunction with temperamental fear as prospective predictors of increased symptoms following exposure to Hurricane Sandy in a large sample of children. Results suggested that children who were high in fear at age 3 and experienced elevated hurricane stressors were characterized by subsequent increases in internalizing symptoms, but only when they were also characterized by an increased ERN at age 6. These findings support a moderated diathesis-stress model, suggesting that the combination of early temperament and the ERN confers risk for increased psychological symptoms following environmental stressors. These findings build upon previous work in this sample that found an interaction between early temperamental fearfulness and hurricane stressors in predicting increases in anxiety symptoms.9
The current findings were consistent with previous work that has examined the ERN in conjunction with early childhood temperament in relation to developmental increases in anxiety.32,33 For example, Lahat et al. (2014) found that children characterized by high BI (at 24 and 36 months of age) and an increased ERN (at 7 years old) were particularly at risk for developing anxiety symptoms (at 9 years old). This is consistent with the current findings in that early temperamental fear and increased ERN in middle childhood predicted risk for subsequent increases in anxiety symptoms in later childhood. Results from the current study extended previous work by examining stress-mediated increases in anxiety symptoms following a natural disaster – suggesting that temperament, neural biomarkers, and environmental stressors all contribute to developmental trajectories leading to anxious outcomes.
To examine specificity of this effect, we confirmed that temperamental fear, the ERN, and their interaction did not predict stress-related changes in children’s externalizing symptoms. Collectively, these analyses support interactions between temperamental fear and the ERN as unique markers for risk related to anxious symptoms. Additionally, we completed follow-up analyses examining the subscales within the internalizing composite. We found that while the model was significant in predicting increases in the anxious/depressed subscale, the model did not reach significance predicting changes in the withdrawn/depressed or somatic complaints subscales. Given that the anxious/depressed subscale uniquely indexes anxiety symptoms and has been shown to be strongly associated with clinical anxiety diagnoses,46 findings suggest that temperamental fearfulness and increased childhood ERN may be risk factors for environmentally induced increases specific to internalizing psychopathology with a significant component of anxiety. Future studies should explore whether these factors confer risk for stress-induced increases in specific types of anxiety.
Moreover, although fearful temperament is an important risk factor for anxiety disorders, only a subset of fearful children end up actually developing an anxiety disorder.47,48 In light of this, there has been great interest in identifying markers and further characterizing these heterogeneous developmental pathways. The present findings suggest that the ERN and stress further moderate the path from fearful temperament to anxious outcomes. Future studies should explore other environmental, biological, and cognitive processes that may characterize the pathway from fearful temperament to anxiety disorders.
The current findings add to previous work examining biomarkers that confer risk for increases in symptoms following trauma or stressful life events.14 Other biomarkers of risk include: skin conductance,10,11 heart rate,12 glucocorticoid receptor pathway components,13 and amygdala reactivity to threat.49–51 The current study adds to these findings by examining a neural biomarker measured early in development (children were 6 years old). Additionally, the biomarker was not measured proximally to the environmental stressor: Hurricane Sandy hit Long Island approximately 4 years after the ERN was measured. These findings suggest that error-related neural activity may be a relatively trait-like vulnerability marker that is established early in the course of development, and thereby may be an important target of early intervention.
It should be noted that in the current study, elevations in symptoms were measured 6 weeks after Hurricane Sandy. Presumably, stressors during this time were ongoing (e.g., cleanup, assessing damage, etc.) and elevations in anxiety symptoms may be expected and adaptive. Therefore, interpreting increases in symptoms during this time as pathological may not be appropriate. Future studies should explore to what extent the ERN can predict who will experience prolonged and maladaptive increases in anxiety symptoms following a stressful life event. Additionally, it should be noted that while the current study focused on stressful life events, future work should examine whether a similar pattern of results is found in relation to traumatic events.
One limitation of the current study includes the concern that post-hurricane psychological symptoms were assessed at the same time as hurricane-related stress, and both were reported by mothers. While this introduces the possibility of shared method and informant variance between symptoms and stressors, it would not account for the interaction between temperament and ERN in predicting changes in symptoms. Another limitation is that we were unable to complete diagnostic interviews following Hurricane Sandy. Hence, we do not know if children in the current study would have met criteria for posttraumatic stress disorder following the hurricane and to what extent our current findings would extend to this diagnostic category. Additionally, the current sample largely consisted of English-speaking Caucasian, middle-class children. It is unknown to what extent the current findings would generalize to a less homogeneous population. And, considering that children growing up in families with low socioeconomic status are particularly likely to encounter environmental adversity,52 it is important for future work to explore markers of risk for environmentally induced increases in psychopathology in more diverse samples and in response to other types of trauma.
Acknowledgments
This study was funded by a National Institute of Mental Health (NIMH) grant (R01 MH069942).
This study was presented in a symposium at the Society for Psychophysiological Research (SPR), Minneapolis, 2016.
Drs. Kotov and Klein served as the statistical experts for this research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Meyer, Danielson, Danzig, Bhatia, Black, Bromet, Carlson, Hajcak, Kotov, and Klein report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Alexandria Meyer, Florida State University, Tallahassee.
Carla Kmett Danielson, Medical University of South Carolina, Charleston.
Allison P. Danzig, Kaiser Permanente - South San Francisco.
Vickie Bhatia, Ralph H. Johnson VA Medical Center, Charleston, SC.
Sarah R. Black, The Ohio State University, Columbus.
Evelyn Bromet, Stony Brook University, Stony Brook, NY.
Gabrielle Carlson, Stony Brook University, Stony Brook, NY.
Greg Hajcak, Stony Brook University, Stony Brook, NY.
Roman Kotov, Stony Brook University, Stony Brook, NY.
Daniel N. Klein, Stony Brook University, Stony Brook, NY.
References
- 1.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 2.deRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno GA. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation Psychology. 2010;55:1–11. doi: 10.1037/a0018601. [DOI] [PubMed] [Google Scholar]
- 3.North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. Jama. 2013;310(5):507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- 4.Masten AS, Narayan AJ. Child development in the context of disaster, war, and terrorism: Pathways of risk and resilience. Annu Rev Psychol. 2012;63:227–57. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pfefferbaum B, Noffsinger MA, Wind LH, Allen JR. Children’s coping in the context of disasters and terrorism. Journal of loss and trauma. 2014;19(1):78–97. doi: 10.1080/15325024.2013.791797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.La Greca AM, Lai BS, Joormann J, Auslander BB, Short MA. Children’s risk and resilience following a natural disaster: Genetic vulnerability, posttraumatic stress, and depression. J Affect Disord. 2013;151:860–867. doi: 10.1016/j.jad.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 7.Neria Y, Shultz JM. Mental health effects of Hurricane Sandy: Characteristics, potential aftermath, and response. JAMA. 2012;308(24):2571–2572. doi: 10.1001/jama.2012.110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olino TM, Klein DN, Dyson MW, Rose SA, Durbin CE. Temperamental emotionality in preschool-aged children and depressive disorders in parents: associations in a large community sample. J Abnorm Psychol. 2010;119(3):468–78. doi: 10.1037/a0020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kopala-Sibley D, Danzig A, Kotov R, et al. Negative Emotionality and its Facets Moderate the Effects of Exposure to Hurricane Sandy on Children’s Post-Disaster Depression and Anxiety Symptoms. J Abnorm Psychol. 2016;125(4):471–81. doi: 10.1037/abn0000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guthrie RM, Bryant RA. Auditory startle response in firefighters before and after trauma exposure. American Journal of Psychiatry. 2005;16(2):283–290. doi: 10.1176/appi.ajp.162.2.283. [DOI] [PubMed] [Google Scholar]
- 11.Pole N, Neylan TC, Otte C, Henn-Hasse C, Metzler TJ, Marmar CR. Prospective prediction of posttraumatic stress disorder symptoms using fear potentiated auditory startle responses. Biological psychiatry. 2009;65(3):235–240. doi: 10.1016/j.biopsych.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Orr SP, Lasko NB, Macklin ML, Pineles SL, Chang Y, Pitman RK. Predicting post-trauma stress symptoms from pre-trauma psychophysiologic reactivity, personality traits and measures of psychopathology. Biology of mood & anxiety disorders. 2012;2:8. doi: 10.1186/2045-5380-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Zuiden M, Geuze E, Willemen HL, et al. Glucocorticoid receptor pathway components predict posttraumatic stress disorder symptom development: a prospective study. Biol Psychiatry. 2012;71:309–316. doi: 10.1016/j.biopsych.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 14.Weems CF. Biological correlates of child and adolescent responses to disaster exposure: a bioecological model. Current psychiatry reports. 2015;17(7):1–7. doi: 10.1007/s11920-015-0588-7. [DOI] [PubMed] [Google Scholar]
- 15.Beesdo K, Pine DS, Lieb R, Wittchen HU. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch Gen Psychiatry. 2010;67:47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- 16.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 18.Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? J Child Psychol Psychiatry. 2007;48(12):1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- 19.Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: The great smoky mountains study. J Am Acad Child Adolesc Psychiatry. 2014;53:21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wittchen HU, Lieb R, Pfister H, Schuster P. The waxing and waning of mental disorders: evaluating the stability of syndromes of mental disorders in the population. Compr Psychiatry. 2000;41(2 Suppl 1):122–132. doi: 10.1016/s0010-440x(00)80018-8. [DOI] [PubMed] [Google Scholar]
- 21.Manly JT, Kim JE, Rogosch FA, Cicchetti D. Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Dev Psychopathol. 2001;13:759–82. [PubMed] [Google Scholar]
- 22.Meyer A, Hajcak G, Torpey-Newman DC, Kujawa A, Klein DN. Enhanced error-related brain activity in children predicts the onset of anxiety disorders between the ages of 6 and 9. J Abnorm Psychol. 2015;124:266–74. doi: 10.1037/abn0000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moser JS, Moran TP, Schroder HS, Donnellan MB, Yeung N. On the relationship between anxiety and error monitoring: a meta-analysis and conceptual framework. Frontiers in human neuroscience. 2013;466(7):1–19. doi: 10.3389/fnhum.2013.00466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hajcak G. What we’ve learned from mistakes. Curr Dir Psychol Sci. 2012;21:101–106. [Google Scholar]
- 25.Falkenstein M, Hohnsbein J, Hoormann J, Blanke L. Effects of crossmodal divided attention on late ERP components. II. Error processing in choice reaction tasks. Electroencephalography and Clinical Neurophysiology. 1991;78(6):447–455. doi: 10.1016/0013-4694(91)90062-9. [DOI] [PubMed] [Google Scholar]
- 26.Gehring WJ, Goss B, Coles MGH, Meyer DE, Donchin E. A Neural System for Error Detection and Compensation. Psychological Science. 1993;4(6):385–390. [Google Scholar]
- 27.Riesel A, Endrass T, Kaufmann C, Kathmann N. Overactive error-related brain activity as a candidate endophenotype for Obsessive-Compulsive Disorder: Evidence from unaffected first-degree relatives. Am J Psychiatry. 2011;168(3):317–324. doi: 10.1176/appi.ajp.2010.10030416. [DOI] [PubMed] [Google Scholar]
- 28.Carrasco M, Harbin SM, Nienhuis JK, Fitzgerald KD, Gehring WJ, Hanna GL. Increased Error-Related Brain Activity In Youth With Obsessive-Compulsive Disorder And Unaffected Siblingseased Error-Related Brain Activity In Youth With Obsessive-Compulsive Disorder And Unaffected Siblings. Depression and Anxiety. 2013;30(1):39–46. doi: 10.1002/da.22035. [DOI] [PubMed] [Google Scholar]
- 29.Weinberg A, Hajcak G. Longer term test–retest reliability of error-related brain activity. Psychophysiology. 2011;48(10):1420–1425. doi: 10.1111/j.1469-8986.2011.01206.x. [DOI] [PubMed] [Google Scholar]
- 30.Meyer A, Bress J, Proudfit GH. Psychometric Properties of the Error-Related Negativity in Children and Adolescents. Psychophysiology. 2014;51(7):602–610. doi: 10.1111/psyp.12208. [DOI] [PubMed] [Google Scholar]
- 31.Anokhin AP, Golosheykin S, Heath AC. Heritability of frontal brain function related to action monitoring. Psychophysiology. 2008;45(4):524–534. doi: 10.1111/j.1469-8986.2008.00664.x. [DOI] [PubMed] [Google Scholar]
- 32.Lahat A, Lamm C, Chronis-Tuscano A, Pine DS, Henderson HA, Fox NA. Early behavioral inhibition and increased error monitoring predict later social phobia symptoms in childhood. J Am Acad Child Adolesc Psychiatry. 2014;53:447–455. doi: 10.1016/j.jaac.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McDermott JM, Perez-Edgar K, Henderson HA, Chronis-Tuscano A, Pine DS, Fox NA. A history of childhood behavioral inhibition and enhanced response monitoring in adolescence are linked to clinical anxiety. Biological Psychiatry. 2009;65(5):445–448. doi: 10.1016/j.biopsych.2008.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olvet DM, Hajcak G. The stability of error-related brain activity with increasing trials. Psychophysiology. 2009;46(5):957–961. doi: 10.1111/j.1469-8986.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 35.Achenbach TM, Edelbrock C. Child behavior checklist. Burlington, VT: University of Vermot; 1981. [Google Scholar]
- 36.Kopala-Sibley D, Kotov R, Bromet E, et al. Personality diatheses and Hurricane Sandy: effects on post-disaster depression. Psychological medicine. 2016;46:865–75. doi: 10.1017/S0033291715002378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kujawa A, Hajcak G, Danzig AP, et al. Neural reactivity to emotional stimuli prospectively predicts the impact of a natural disaster on psychiatric symptoms in children. Biol Psychiatry. 2015;80:381–9. doi: 10.1016/j.biopsych.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Galea S, Brewin CR, Gruber M, et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of general psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Norris FH, Sherrieb K, Galea S. Prevalence and consequences of disaster-related illness and injury from Hurricane Ike. Rehabilitation Psychology. 2010;55(3):221–30. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- 40.Meyer A, Hajcak G, Torpey DC, et al. Increased error-related brain activity in six-year-old children with clinical anxiety. Journal of abnormal child psychology. 2013;41(8):1257–1266. doi: 10.1007/s10802-013-9762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Torpey DC, Hajcak G, Kim J, Kujawa A, Klein DN. Electrocortical and behavioral measures of response monitoring in young children during a Go/No-Go task. Dev Psychobiol. 2011;54:139–150. doi: 10.1002/dev.20590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gratton G, Coles MGH, Donchin E. A new method for off-line removal of ocular artifact. Electroencephalography and Clinical Neurophysiology. 1983;55(4):468–484. doi: 10.1016/0013-4694(83)90135-9. [DOI] [PubMed] [Google Scholar]
- 43.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate behavioral research. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 45.Torpey DC, Hajcak G, Kim J, et al. Error-related brain activity in young children: associations with parental anxiety and child temperamental negative emotionality. J Child Psychol Psychiatry. 2013;54:854–862. doi: 10.1111/jcpp.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aschenbrand SG, Angelosante AG, Kendall PC. Discriminant validity and clinical utility of the CBCL with anxiety-disordered youth. J Clin Child Adolesc Psychol. 2005;34(4):735–746. doi: 10.1207/s15374424jccp3404_15. [DOI] [PubMed] [Google Scholar]
- 47.Buss KA, Kiel EJ. Temperamental risk factors for pediatric anxiety disorders. In: Buss KA, Kiel EJ, editors. Pediatric Anxiety Disorders: A Clinical Guide. New York: Springer; 2013. pp. 47–68. [Google Scholar]
- 48.Lahat A, Hong M, Fox NA. Behavioural inhibition: Is it a risk factor for anxiety? Int Rev Psychiatry. 2011;23:248–257. doi: 10.3109/09540261.2011.590468. [DOI] [PubMed] [Google Scholar]
- 49.Admon R, Lubin G, Stern O, et al. Human vulnerability to stress depends on amygdala’s predisposition and hippocampal plasticity. Proc Natl Acad Sci U S A. 2009;106:14120–14125. doi: 10.1073/pnas.0903183106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McLaughlin KA, Busso DS, Duys A, et al. Amygdala response to negative stimuli predicts PTSD symptom onset following a terrorist attack. Depression and anxiety. 2014;31(10):834–842. doi: 10.1002/da.22284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Swartz JR, Knodt AR, Radtke SR, Hariri AR. A neural biomarker of psychological vulnerability to future life stress. Neuron. 2015;85(3):505–511. doi: 10.1016/j.neuron.2014.12.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Evans GW. The environment of childhood poverty. Am Psychol. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]


