Summary
Background
Human immunodeficiency virus infection and obesity are pro‐inflammatory conditions that, when occurring together, may pose a synergistic risk for diabetes and cardiovascular disease.
Purpose
The aim of the current study was (i) to document the prevalence of obesity in HIV+ patients treated at the Miriam Hospital Immunology Center (Providence, RI) and (ii) to investigate the relationship between obesity and comorbidities.
Methods
The study population consisted of 1,489 HIV+ adults (70% men; average age 48 ± 11 years) treated between 01/01/2012 and 06/30/2014. Separate logistic regressions tested the associations between overweight and obesity and comorbid diagnoses (diabetes, hypertension and cardiovascular disease), as compared with normal weight. Covariates included age, gender and smoking status.
Results
Approximately 37% of patients were overweight (body mass index 25.0–29.9), and an additional 28% were obese (body mass index ≥30.0). Obesity was associated with higher odds of comorbid diabetes (OR = 3.26, CI = 1.98–5.39) and hypertension (OR = 2.11, CI = 1.49–2.98). There was no significant association between obesity and the presence of cardiovascular disease (OR = 1.12, CI = 0.66–1.90). Overweight was associated only with higher odds of comorbid diabetes (OR = 1.72; CI = 1.02–2.88).
Conclusion
Our findings demonstrate a heightened risk of comorbidities in overweight and obese HIV+ patients. Future studies should investigate whether weight loss interventions for this population can reduce cardiovascular and metabolic risk factors as they do in other populations.
Keywords: AIDS, HIV, human immunodeficiency virus
Introduction
During the height of the US AIDS epidemic, hundreds of thousands of Americans died from opportunistic infections and wasting after acquiring the human immunodeficiency virus (HIV). For many, the letters ‘HIV’ still conjure images of extreme, unwanted weight loss, although the prognosis for most Americans living with HIV today is quite different. Individuals treated with effective combined antiretroviral therapy (cART) are now living with HIV as a chronic condition and, strikingly, many are obese 1, 2, 3.
Nearly 1.2 million Americans are living with HIV, and approximately 50,000 are infected annually 4. The condition disproportionately affects African Americans, Latinos and men who have sex with men (MSM) of all races and ethnicities; in 2010, two‐thirds of new infections occurred in MSM, and the estimated rates of infection among African Americans and Latinos were eight times and three times the rates in Caucasians respectively 5. New infections are highest among young people (31% of new cases occurred in 25‐ to 34‐year‐olds and 26% in 13‐ to 24‐year‐olds) 5. However, in 2012, 25% of Americans living with HIV were 55 years or older 6. HIV infection continues to be one of the most stigmatizing health conditions 7 and often co‐occurs with other highly stigmatized conditions, including substance abuse and psychiatric illness 8.
Obesity among HIV+ adults with access to care is recognized among infectious disease researchers and clinicians. Over the past decade, papers demonstrating this phenomenon have been published in journals including Antiviral Therapy 9, AIDS Patient Care and STDs 2, 10, the Journal of Acquired Immunodeficiency Syndromes 1 and Open Forum Infectious Diseases 11. A recent study in Medicine reported that in a nationally representative sample of over 4,000 HIV+ adults with access to care, two in five women and one in five men were obese 3.
The combination of HIV infection and obesity may result in an additive or synergistic risk for diabetes and cardiovascular disease (CVD), among other chronic medical conditions, owing to the pro‐inflammatory nature of both conditions. Inflammation associated with HIV infection results from replication of HIV, replication of comorbid viral infections (e.g. cytomegalovirus and Epstein–Barr virus), loss of regulatory immune cells and microbial translocation across damaged gut mucosa 12, 13. In obesity, the visceral adipose tissue releases increased concentrations of pro‐inflammatory adipokines (e.g. TNF‐α, IL‐6) and decreased concentrations of anti‐inflammatory adipokines (e.g. adiponectin). Chronic inflammation in obesity may also be due, in part, to changes in gut microbiota and intestinal permeability 14. Higher rates of alcohol, smoking and illicit drug abuse 12, abnormally low functional aerobic capacity 15 and chronic use of cART for decades 12 may further exacerbate the risk of diabetes and CVD in HIV+ individuals.
We conducted a cross‐sectional investigation of the HIV+ population treated at the Miriam Hospital Immunology Center, Rhode Island, with the goal of (i) documenting the prevalence of obesity in the centre's HIV+ population and (ii) examining the relationship between obesity and comorbidities. Our data provide a unique opportunity to examine these issues on a statewide basis because this centre sees 94% of all HIV+ individuals in the state of Rhode Island who are engaged in care. The full spectrum of patients with HIV in the state, based on age, race/ethnicity, risk group and comorbidity status, are seen at this centre, and 93% of these patients have well‐controlled HIV.
Methods
Study population
The study population consisted of all HIV+ adults treated in the Immunology Center at the Miriam Hospital, a major teaching hospital of the Alpert Medical School of Brown University, in Providence, Rhode Island, between 01/01/2012 and 06/30/2014. The Institutional Review Board approved this study.
Data extraction
Patient demographics, diagnoses and laboratory tests from office visits between 01/01/2012 and 06/30/2014 were extracted and de‐identified from the Immunology Center Database and Electronic Clinical Works. ‘Active’ patients who had at least one medical visit during the extraction period were included in our analyses. ‘Inactive’ patients (e.g. deceased, transferred care) and patients who were pregnant during the extraction period were excluded. Demographics included age at the end of the extraction period, gender, race, ethnicity, HIV transmission group (MSM vs. non‐MSM), body mass index (BMI; calculated from objectively measured height and weight) and smoking status. Laboratory data consisted of CD4 count and HIV plasma viral load. BMI was calculated based on the most recent office visit, and CD4 count and viral load data were extracted from the most recent laboratory test. Diagnoses (as listed in patient medical records) included diabetes, hypertension and CVD (which included CVD, chronic heart failure, coronary artery disease and peripheral vascular disease).
Data analysis
Descriptive statistics determined the frequencies, means and standard deviations. Chi‐squared tests compared demographic and laboratory categories (age, gender, race, ethnicity, HIV transmission group, smoking status, CD4 count, viral load) by BMI category (normal weight [BMI 18.5–24.9], overweight [BMI 25.0–29.9], obese [BMI ≥30]). Separate logistic regressions tested the associations between overweight and obesity and comorbid diagnoses (diabetes, hypertension and CVD), as compared with normal weight. Analyses controlled for age (continuous), gender and smoking status. Transgendered patients (n = 6) were not included in regression analyses to allow for model convergence. All analyses were conducted by using sas version 9.4.
Results
A total of 1,489 HIV+ patients were included in this study. The average patient age was 48 (SD = 11) years, and 43% of the patients were 50 years or older. The majority of patients were men (70%, n = 1,047), of whom 60% (n = 627) identified as MSM. Most patients were being effectively treated with cART (93% CD4 > 200 cells μL−1, 85% plasma viral load ≤ 75 copies mL−1). Demographic characteristics, by overweight and obesity status, are displayed in Table 1. As shown in Figure 1, approximately 37% of patients were overweight (BMI 25.0–29.9), and an additional 28% were obese (BMI ≥30.0).
Table 1.
Demographics by obesity status in HIV+ patients (n = 1,459) treated at the Immunology Center at the Miriam Hospital (Providence, Rhode Island)
| Variable | All patients* | Normal weight | Overweight | Obese | P value |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| All patients | 1,459 (100.0) | 486 (33.3) | 553 (37.9) | 420 (28.8) | — |
| Gender | <0.0001 | ||||
| Male | 1,029 (70.5) | 365 (75.1) | 426 (77.0) | 238 (56.7) | |
| Female | 424 (29.1) | 118 (24.3) | 126 (22.8) | 180 (42.9) | |
| Transgender | 6 (0.4) | 3 (0.6) | 1 (0.2) | 2 (0.5) | |
| Age | 0.0146 | ||||
| <30 years | 113 (7.8) | 49 (10.1) | 36 (6.5) | 28 (6.7) | |
| 31–40 years | 247 (16.9) | 80 (16.5) | 108 (19.5) | 59 (14.1) | |
| 41–50 years | 474 (32.5) | 145 (29.8) | 175 (31.7) | 154 (36.7) | |
| 51–60 years | 480 (32.9) | 158 (32.5) | 187 (33.8) | 135 (32.1) | |
| 61–70 years | 122 (8.4) | 40 (8.2) | 42 (7.6) | 40 (9.5) | |
| >70 years | 23 (1.6) | 14 (2.9) | 5 (0.9) | 4 (1.0) | |
| HIV transmission group (men, only) | 0.1580 | ||||
| MSM | 626 (60.1) | 231 (63.3) | 255 (59.9) | 132 (55.5) | |
| Non‐MSM | 411 (39.9) | 134 (36.7) | 171 (40.1) | 106 (44.5) | |
| Race | 0.2460 | ||||
| Caucasian | 852 (58.4) | 287 (59.1) | 331 (59.9) | 234 (55.7) | |
| African American | 453 (31.1) | 145 (29.8) | 160 (28.9) | 148 (35.2) | |
| All others | 154 (10.6) | 54 (11.1) | 62 (11.2) | 38 (9.1) | |
| Ethnicity | 0.5346 | ||||
| Hispanic | 359 (24.6) | 115 (23.7) | 145 (26.2) | 99 (23.6) | |
| Non‐Hispanic | 1,100 (75.4) | 371 (76.3) | 408 (73.8) | 321 (76.4) | |
| Smoking status | 0.0003 | ||||
| Smoker | 596 (40.9) | 233 (47.9) | 198 (35.8) | 165 (39.3) | |
| Non‐smoker | 863 (59.2) | 253 (52.1) | 355 (64.2) | 255 (60.7) | |
| CD4 cell count (cells μL−1) | 0.0233 | ||||
| <200 | 102 (7.0) | 47 (9.7) | 34 (6.2) | 21 (5.0) | |
| 201–500 | 457 (31.4) | 161 (33.2) | 163 (29.6) | 133 (31.7) | |
| >500 | 895 (61.6) | 277 (57.1) | 353 (64.2) | 265 (63.3) | |
| HIV RNA load (copies mL−1) | 0.9179 | ||||
| ≤75 | 1,241 (85.2) | 414 (85.2) | 472 (85.5) | 355 (84.7) | |
| 76–1,000 | 108 (7.4) | 35 (7.2) | 38 (6.9) | 35 (8.4) | |
| >1,000 | 108 (7.4) | 37 (7.6) | 42 (7.6) | 29 (6.9) |
All patients’ excludes underweight patients (BMI <18.5, n = 30). Normal weight = BMI 18.5–24.9; overweight = BMI 25–29.9; obese = BMI ≥30.
BMI, body mass index; MSM, men who have sex with men.
Figure 1.
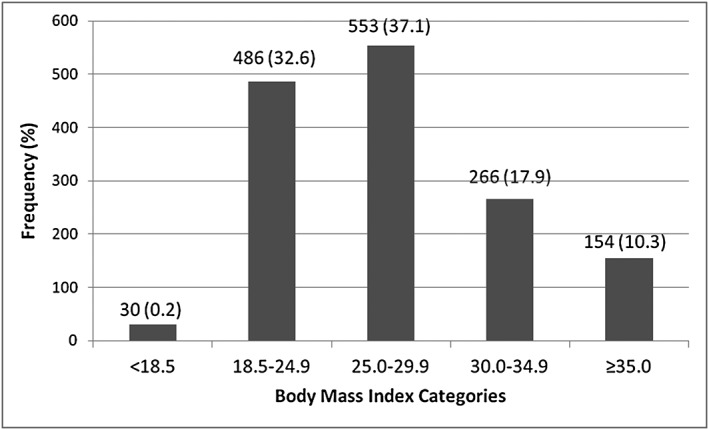
Distribution of body mass index among HIV+ patients (n = 1,489) treated at the Immunology Center at the Miriam Hospital (Providence, Rhode Island).
Obesity was associated with higher odds of comorbid diabetes (OR = 3.26, CI = 1.98–5.39) and hypertension (OR = 2.11, CI = 1.49–2.98) as compared with normal weight. There was no significant association between obesity and presence of CVD (OR = 1.12, CI = 0.66–1.90). Overweight was associated with higher odds of comorbid diabetes (OR = 1.72, CI = 1.02–2.88) but not hypertension (OR = 1.36, CI = 0.97–1.91) or CVD (OR = 0.87, CI = 0.52–1.47).
Discussion
Among HIV+ patients receiving care at the Miriam Hospital Immunology Center in Providence, Rhode Island, greater than one in four HIV+ patients was obese and two‐thirds were either overweight or obese. Our findings are in line with data from a number of US and international cohorts reporting comorbid obesity and HIV infection 1, 2, 9, 10, 11. Further, this percentage closely mirrors the rate of obesity and overweight in Rhode Island (26% obese, 63% overweight or obese) 16.
In the current study, the odds of having diabetes were three times greater in obese patients than in normal weight patients; being overweight also significantly increased the risk of diabetes but to a lesser extent. The odds of having hypertension were two times greater in obese patients than in normal weight patients. Of note, the current study used a cross‐sectional design, and, thus, we cannot infer directionality in these relationships. There were no differences in risk of CVD in this study population, but other studies have shown elevated CVD risk 12. We recognize that our cross‐sectional design limits our ability to fully capture CVD risk, as these diagnoses may emerge in older adulthood.
Two other findings from the current study warrant brief discussion. First, obesity in this cohort was more prevalent in women than in men. Nationally, nearly one in four HIV+ Americans are women, with African–American and Hispanic/Latino women being disproportionately affected 4. As African–American and Latino women have the highest rates of obesity 17, future research on the health risks of obesity and the effects of weight loss may be particularly warranted in this subpopulation of people living with HIV. Although the prevalence was lower, it is important to note that more than 20% of male patients in our sample were also obese.
Second, almost half (43%) of the patients in the Miriam Hospital Center were aged 50+ years at the time of our study, whereas only 15% were 50+ years when the cohort was examined 10 years earlier (data not shown). The increasing age of the HIV+ population in combination with obesity compounds the risk of health problems such as hypertension, diabetes and CVD.
Our findings raise the question of whether weight loss interventions with HIV+ populations can reduce cardiovascular and metabolic comorbidities as they do in non‐infected populations. To date, there is no evidence to suggest that weight loss is indicated in this population. There have been a number of exercise and nutrition interventions with HIV+ individuals in recent years 18, but few have focused specifically on weight loss 19. In 2006, Engelson et al. investigated the effects of weight loss on body composition and metabolic risk factors in 18 obese, HIV+ women 20. The 12‐week intervention consisted of weekly nutrition education classes and supervised exercise (aerobic and resistance) three times per week. Despite significant weight loss (average 6.7 kg), mean fasting glucose, insulin and insulin sensitivity did not improve, nor were there changes in fasting lipids, tissue plasminogen activator or plasminogen activator inhibitor 1. Similarly, in a study with 30 HIV+ individuals, Terry et al. 21 found that weight losses (average 2 kg) resulting from a low‐lipid diet and aerobic exercise intervention did not produce changes in glucose, triglycerides, total cholesterol or HDL cholesterol. These findings stand in marked contrast to the effects of weight loss on cardiovascular and metabolic risk factors in non‐HIV+ populations 22, 23. Further research is thus clearly warranted to determine whether interventions lead to weight loss and subsequently whether weight loss leads to improved health in this population. Because of the prior history of wasting in HIV+ patients and the persistence of HIV even in virally suppressed patients, it will also be important to determine the effects of weight loss on lean body mass and CD4 counts.
In the era of HIV as a chronic condition, HIV+ individuals effectively treated with cART are facing different health challenges compared with HIV+ patients of the 1980s and 1990s. In the current study, more than one in four HIV+ patients was obese, and two‐thirds were overweight or obese. Research examining the relationship between weight loss and risk factor changes in this population is needed to determine whether weight loss should be encouraged in these individuals.
Conflict of Interest Statement
This work was made possible by the National Heart, Lung and Blood Institute and the Lifespan/Tufts/Brown Center for AIDS Research, supported by the National Institute of Allergy and Infectious Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institute of Allergy and Infectious Diseases. The authors have no conflicts of interest to disclose.
Funding
This work was made possible by the National Heart, Lung and Blood Institute (T32 HL076134) and the Lifespan/Tufts/Brown Center for AIDS Research, supported by the National Institute of Allergy and Infectious Diseases (P30AI042853).
Authors’ contributions
E. J. W., F. S. G. and K. E. R. developed ideas for the manuscript and wrote the initial rough draft; K. M. B. built on the initial rough draft to develop the version submitted; F. S. G. conducted the data analyses and was involved in the writing process throughout; R. R. W. and E. J. W. provided oversight for data analyses and were involved in the writing process throughout. All authors approved of the submitted version.
Becofsky, K. M. , Wing, E. J. , Wing, R. R. , Richards, K. E. , and Gillani, F. S. (2016) Obesity prevalence and related risk of comorbidities among HIV+ patients attending a New England ambulatory centre. Obesity Science & Practice, 2: 123–127. doi: 10.1002/osp4.38.
References
- 1. Amorosa V, Synnestvedt M, Gross R et al. A tale of 2 epidemics – the intersection between obesity and HIV infection in Philadelphia. J Acquir Immune Defic Syndr 2005; 39: 557– 561. [PubMed] [Google Scholar]
- 2. Crum‐Cianflone N, Tejidor R, Medina S, Barahona I, Ganesan A. Obesity among patients with HIV: the latest epidemic. AIDS Patient Care STDS 2008; 22: 925–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thompson‐Paul AM, Wei SC, Mattson CL et al. Obesity among HIV‐infected adults receiving medical care in the United States: data from the cross‐sectional Medical Monitoring Project and National Health and Nutrition Examination Survey. Medicine (Baltimore) 2015; 94: e1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bradley H, Hall HI, Wolitski RJ et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV – United States, 2011. MMWR Morb Mortal Wkly Rep 2014; 63: 1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention . Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. HIV Surveillance Supplemental Report 2012; 17/4.
- 6. Centers for Disease Control and Prevention . Monitoring selected national HIV prevention and care objectives by using HIV surveillance data – United States and 6 dependent areas – 2013. HIV Surveillance Supplemental Report 2015; 20/2.
- 7. Shacham E, Rosenburg N, Onen NF, Donovan MF, Overton ET. Persistent HIV‐related stigma among an outpatient US clinic population. Int J STD AIDS 2015; 26: 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Durvasula R, Miller TR. Substance abuse treatment in persons with HIV/AIDS: challenges in managing triple diagnosis. Behav Med 2014; 40: 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tate T, Willig AL, Willig JH et al. HIV infection and obesity: where did all the wasting go? Antivir Ther 2012; 17: 1281– 1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boodram B, Plankey MW, Cox C et al. Prevalence and correlates of elevated body mass index among HIV‐positive and HIV‐negative women in the Women's Interagency HIV Study. AIDS Patient Care STDS 2009; 23: 1009– 1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hasse B, Iff, M ., Ledergerber, B et al. Obesity trends and body mass index changes after starting antiretroviral treatment: the Swiss HIV Cohort Study. Open Forum Infect Dis 2014; 1(2): doi: 10.1093/ofid/ofu040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet 2013; 382: 1525– 1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pathai S, Bajillan H, Landay AL, High KP. Is HIV a model of accelerated or accentuated aging? J Gerontol A Biol Sci Med Sci 2014; 69: 833– 842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cox AJ, West NP, Cripps AW. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol 2015; 3: 207–215. [DOI] [PubMed] [Google Scholar]
- 15. Hand GA, Phillips KD, Dudgeon WD et al. Moderate intensity exercise training reverses functional aerobic impairment in HIV‐infected individuals. AIDS Care 2008; 20: 1066– 1074. [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention . 2012. State Nutrition, Physical Activity, and Obesity Profile: Rhode Island. URL http://www.cdc.gov/obesity/stateprograms/fundedstates/pdf/rhode‐island‐state‐profile.pdf (access January 20, 2016).
- 17. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 2012; 307: 491– 497. [DOI] [PubMed] [Google Scholar]
- 18. Botros D, Somarriba G, Neri D, Miller TL. Interventions to address chronic disease and HIV: strategies to promote exercise and nutrition among HIV‐infected individuals. Curr HIV/AIDS Rep 2012; 9: 35–‐363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cofrancesco J, Jr , Freedland E, McComsey G. Treatment options for HIV‐associated central fat accumulation. AIDS Patient Care STDS 2009; 23: 5– 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Engelson ES, Agin D, Kenya S et al. Body composition and metabolic effects of a diet and exercise weight loss regimen on obese, HIV‐infected women. Metabolism 2006; 55: 1327– 1336. [DOI] [PubMed] [Google Scholar]
- 21. Terry L, Sprinz E, Stein R et al. Exercise training in HIV‐1‐infected individuals with dyslipidemia and lipodystrophy. Med Sci Sports Exerc 2006; 38: 411– 417. [DOI] [PubMed] [Google Scholar]
- 22. Wing RR, Lang W, Wadden TA et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care 2011; 34: 1481– 1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lau DC, Teoh H. Benefits of modest weight loss on the management of type 2 diabetes mellitus. Can J Diabetes 2013; 37: 128– 134. [DOI] [PubMed] [Google Scholar]


