Abstract
Background
Parents of children with critical congenital heart defects (PCCHDs) may be at high risk for mental health morbidity; however, the literature is not well characterized. Given that compromised parental mental health can lead to long‐term cognitive, health‐related, and behavioral problems in children, a systematic review of this literature could provide informed recommendations for continued research and enhance the care of families of children living with critical congenital heart defects.
Methods and Results
We conducted a systematic review using the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines that resulted in 30 studies on the mental health of PCCHDs. The literature revealed that PCCHDs are at an elevated risk for psychological problems, particularly in the immediate weeks and months following cardiac surgery. Up to 30% of PCCHDs have symptoms consistent with a diagnosis of posttraumatic stress disorder, with over 80% presenting with clinically significant symptoms of trauma; 25% to 50% of PCCHDs reported clinically elevated symptoms of depression and/or anxiety, and 30% to 80% reported experiencing severe psychological distress. There was high variability in measurements used to assess study outcomes, methodological quality, and sociocultural composition of the parents included in the studies.
Conclusions
There is an urgent need for additional research on the severity, course, persistence, and moderators of these mental health problems over time, and for the development and testing of screening approaches and interventions that can be feasibly delivered in the context of ongoing pediatric cardiac care.
Keywords: caregiver, congenital cardiac defect, congenital heart disease, mental disorder, psychology and behavior
Subject Categories: Mental Health, Congenital Heart Disease
Introduction
Congenital heart defects (CHDs) are the most common birth defect in the United States, affecting nearly 40 000 (1%) births per year.1 Of these children, 25% have “critical” CHDs (CCHDs), requiring one or more cardiac surgeries in the first year of life.1 The survival of children with CCHDs has improved considerably over the past decade, allowing them to survive complicated surgeries and go on to have near‐normal life expectancy.2, 3 However, these biomedical advances have not been accompanied by a concurrent increase in our understanding of the psychological impact of CCHDs on the families of which these children are a part.
Parents of children with CCHDs (PCCHDs) are at high risk for mental health morbidity—coping with their children's medical appointments and cardiac procedures, long and multiple hospitalizations, digestive and/or feeding issues, and increased risk for major respiratory illnesses—all of which amount to extensive financial, emotional, and familial costs.4 Most children with CCHDs will have at least one cardiac procedure in the postpartum period, a time when parents, especially mothers, are most vulnerable for mental health problems.5, 6, 7 This risk is exacerbated substantially when parenting a child who experiences a major illness or acute injury that requires significant medical intervention and/or time in an intensive care unit (ICU).8 For example, while the prevalence of postpartum depression is 10% to 15% for women in the general population,9 it can increase to 39% among mothers of children who spend time in the neonatal ICU after birth.10 Trauma is also common, with approximately one third of parents of children hospitalized in the ICU developing acute stress disorder (ASD),10, 11 10% to 20% developing posttraumatic stress disorder (PTSD),10, 12 and a prevalence of trauma symptoms approaching 84%.12
It is well established that compromised parental mental health, if untreated, can adversely affect a parent's ability to care for his or her child and can lead to long‐term cognitive, health‐related, and behavioral problems in children.13, 14, 15, 16 As described in Abidin's theoretical model of parenting stress, the mental health of a parent can result in dysfunctional parent‐child interactions, which may subsequently influence parenting behavior and result in maladaptive child outcomes.17 This dynamic is of particular concern in the postpartum period given that the quality of parent‐child emotional attachment during this earliest phase of life is crucial for subsequent physical and psychological development.18
The psychological health of PCCHDs is not well characterized. While there is a growing body of research on familial impact,19, 20 coping,19 well‐being,21 and level of stress22 among these parents, we could not find a published review that focused explicitly on the mental health needs of CHD parents whose children require surgical intervention (ie, are “critical”)—this being an important distinction in CHD care as non‐CCHDs do not involve the invasive surgical treatments and associated hospitalizations that are characteristic of more severe CHDs. A systematic review of this literature would allow for informed recommendations to guide policy, clinical care, and ongoing research. Indeed, the field of pediatric oncology has recently acknowledged the importance of psychological support for affected parents, publishing a set of standards for psychosocial care in the field that include a strong recommendation for early and ongoing assessment of parental mental health needs.23 No such standards exist in the field of pediatric cardiology despite a precedent for the importance of psychological variables in research and clinical practice of adult cardiology.24 To address this knowledge gap, we conducted a systematic review of the published literature on the psychological health of PCCHDs using guidelines from the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA).25
Methods
Eligibility Criteria
Articles were required to meet the following criteria: (1) published on any date before January 1, 2016, in an English‐language journal; (2) included a sample of parents with a child who had cardiac surgery for a CHD; and (3) included a quantitative assessment of psychological functioning of the parents. All study designs (eg, longitudinal, cross‐sectional) and time points since cardiac surgery had occurred were included. Review articles and qualitative studies were excluded as well as studies in which: (1) psychological assessments were only reported for the children, and (2) the sample was exclusively of parents of children who had undergone surgery for heart transplantation given the unique long‐term nature of posttransplant medical care and the stressors associated with it.26
Data Sources and Search Strategy
An electronic search of peer‐reviewed, English‐language articles published prior to January 1, 2016, was conducted using PubMed, PsycINFO, and CINAHL databases. In consultation with a librarian, the following Boolean search strategy was created: (parent OR caregiver OR mother OR father) AND (CHD OR congenital heart defect OR cardiovascular surgical procedures OR cardiac surgical procedures OR open heart surgery OR pediatric heart surgery), AND (child OR infant), AND (anxiety OR depression OR trauma OR stress OR psychological OR distress OR emotional OR quality of life OR psychosocial). Reference lists of relevant articles were examined for additional citations, including the reference lists of previously published reviews on familial impact,19, 20 distress,22 well‐being,21 and coping19 among CHD parents.
Study Selection and Data Abstraction
After articles were identified according to the search terms, titles and abstracts were screened for eligibility. If eligibility could not be determined via the title or abstract, full‐text versions of articles were further screened for eligibility until the final number of articles was determined for inclusion in the systematic review (Figure). Two independent reviewers (S.W.K. and A.A.) read and abstracted the following data from each article included in the review: (1) authors, year, journal; (2) study location; (3) study design; (4) description of the sample of parents; (5) description of comparison group of parents (if any); (6) description of the sample of CHD children; (7) cardiac procedure(s); (8) age at cardiac surgery; (9) time since surgery at time of assessment; (10) psychological outcomes assessed; (11) measure(s) used to assess psychological functioning; and (12) results. Each reviewer independently created a table with these data and the tables were subsequently compared and inconsistencies resolved through ongoing discussion.
Figure 1.
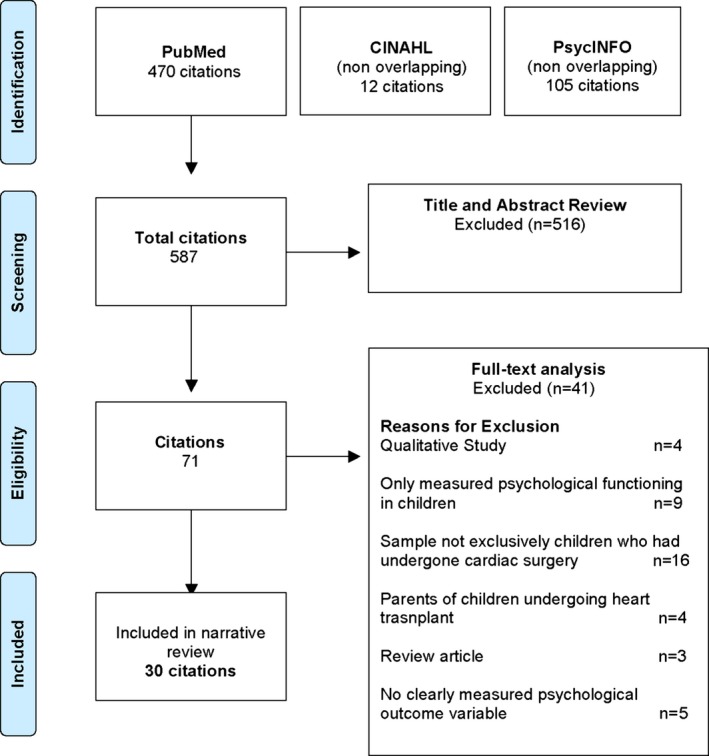
Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow diagram. Adapted from: Moher et al.25 CINAHL indicates cumulative index to nursing and allied health literature.
Assessment of Risk of Bias
Risk of bias assessments are typically used to evaluate the strength of a body of evidence in order to determine “the risk that the study results reflect bias in study design or execution.”27 Despite the availability of many tools for this purpose, there is no consensus on the “best approach” or “preferred tool” for a risk of bias assessment.27 Given our topic and the variety of observational study designs included in our review, we adapted the Agency for Healthcare Research and Quality design‐specific criteria in order to assess for risk of bias in 4 domains: (I) selection bias, (II) attrition and participation bias, (III) reporting bias, and (IV) detection bias (Table 1). Levels of risk were defined as follows: (1) low risk of bias=study satisfied all items in domains I–IV; (2) medium risk of bias=study was insufficient in at least one domain (score of 0 in domains I–III or score of 1 in domain IV), and (3) high risk of bias=study was insufficient in >1 domain. In an effort to account for risk of bias in the narrative review of these results, only studies with a low or medium risk are described and the results are also stratified by study design. A full list of studies reviewed, stratified by risk of bias categorization, and inclusive of descriptive information and results are presented in Table 2.
Table 1.
Assessment of Risk of Bias
| Risk of Bias Domain | Criterion |
|---|---|
| I. Selection bias | (1) Does the design or analysis control or account for >1 important confounding or modifying variables through matching, stratification, multivariable analysis, or other approaches? (Yes=1; No=0) |
| II. Attrition and participation bias | (2) If attrition (dropout, loss to follow‐up) or high rate of refusal was a concern, were missing data or characterization of refusers handled appropriately (eg, imputation, descriptions of reasons for refusal and/or drop‐out, comparison of refusers vs nonrefusers)? |
| III. Reporting bias | (3) Were potential outcomes prespecified by the researchers? Are all prespecified outcomes reported? |
| IV. Detection bias | (4) Were the outcomes assessed/defined using valid and reliable measures, implemented consistently across all study participants? |
| (5) Were confounding variables assessed using valid and reliable measures, implemented consistently across study participants? |
Table 2.
Summary of Studies Included in the Systematic Review (N=30)
| First Author (Year) | Study Location | Design | Sample | Mental Health Category | Measures | Results | Risk of Bias Assessment |
|---|---|---|---|---|---|---|---|
| Cantwell‐Bartl (2013)30 | Australia | Cross‐sectional |
N=29 parents 55% mothers |
Trauma | PTSD module of SCID | 83% of PCCHDs met criteria for diagnosis of ASD or PTSD at time of hospital discharge for surgery. | Low |
| Franck (2010)32 | UK | Longitudinal |
N=326 parents 56% mothers |
Parenting stress | Parent Stressor Scale: Infant Hospitalization | Parenting stress was highest before surgery and decreased slightly over time until an increase at 15 days postsurgery. Parents of infants with CHDs had greater parenting stress than parents of older children with CHDs. | Low |
| Franich‐Ray (2013)33 | Australia | Cross‐sectional |
N=132 parents 58% mothers |
Trauma | ASDS |
35% of mothers and 18% of fathers met criteria for ASD when assessed 1 month posthospital discharge from surgery. 83% of all parents reported at least one trauma symptom. |
Low |
| Gronning‐Dale (2013)35 | Norway | Longitudinal | N=60 parents | Stress/distress | Subjective Well‐Being Index |
Mothers of CCHD had significantly lower subjective well‐being than controls when assessed at 6 and 36 months postpartum. Severity of CHD was a contributing factor in overall score; Parents of children with mild to moderate CHDs did not differ from controls. |
Low |
| Hearps (2014)37 | Australia | Cross‐sectional |
N=39 parents 72% mothers |
Anxiety/depression stress/distress | Psychosocial Assessment Tool |
38% of PCCHDs reported psychosocial risk at a clinical level. 51% of mothers and fathers reported excessive worry (the most commonly endorsed item) and 25.6% of mothers and fathers reported having experienced sadness or depression. |
Low |
| Helfricht (2008)39 | Switzerland | Longitudinal |
N=233 parents 58% mothers |
Trauma | PDS |
16.4% of mothers and 13.3% of fathers met diagnostic criteria for acute PTSD at hospital discharge. 14.9% of mothers and 9.5% of fathers met diagnostic criteria for PTSD when assessed again 6 months postsurgical repair. |
Low |
| Landolt (2011)41 | Switzerland | Longitudinal |
N=232 58% mothers |
Trauma stress/distress | PDS Medical Outcomes Study Short‐Form 36 |
25% of mothers and 26% of fathers reported PTSD 1 month postsurgery. PTSD was associated with higher probability of low MHRQoL. MHQoL was significantly lower than population norms for mothers upon discharge from the hospital. MHRQoL changed significantly over time and, by 6 months postcardiac surgery, scores were higher than population norms for both mothers and fathers. |
Low |
| Menahem (2008)43 | Australia | Longitudinal |
N=39 parents 74% mothers |
Anxiety/depression | STAI |
Levels of anxiety and emotional distress in PCCHDs prior to surgery were significantly higher than published norms. Levels of anxiety returned to normative values 12 months postsurgery. |
Low |
| Rogers (1984)44 | US | Longitudinal | N=20 mothers | Anxiety/depression stress/distress | Profile of mood states Psychosocial Adjustment to Illness Scale |
Prior to surgery, no difference between PCCHDs and controls. PCCHDs reported significantly more symptoms of depression and distress compared with controls 1 week postsurgery. Levels of distress remained significantly higher among PCCHDs compared with controls at 2 months postsurgery; levels of depression were not significantly different at 2 months postsurgery. |
Low |
| Solberg (2011a)46 | Norway | Longitudinal | N=242 mothers | Anxiety/depression | EPDS |
29% of CCHD mothers reported clinically significant symptoms of depression. CCHD mothers were 2.45 times more likely to have depression compared with mothers of children with mild or moderate CHDs at 6 months postpartum. |
Low |
| Solberg (2011b)47 | Norway | Longitudinal | N=162 mothers | Anxiety/depression | Hopkins Symptom Checklist |
Depression and anxiety symptoms increased at both 6 and 18 months postpartum. Severity of CHD has prolonged effects on symptoms and results in overall higher depression scores. |
Low |
| Solberg (2012c)48 | Norway | Longitudinal | N=141 mothers | Anxiety/depression | Hopkins Symptom Checklist |
Mothers of CHD infants are at overall increased risk for symptoms of depression from pregnancy through 36 months postpartum. Mothers of children with CCHDs reported more symptoms of anxiety and depression at 36 months postpartum compared with controls. |
Low |
| Spijkerboer (2007)49 | The Netherlands | Cross‐sectional |
N=161 parents 62% mothers |
Stress/distress | GHQ | PCCHDs exhibited significantly lower levels of distress compared with controls. | Low |
| Utens (2002)52 | The Netherlands | Longitudinal |
N=150 parents 50% mothers |
Anxiety/depression | GHQ | PCCHDs reported more distress and anxiety precardiac surgery when compared with parents of children who underwent catheterization, and controls; however these symptoms tended to decrease over time and PCCHDs scored lower than the control group on anxiety and depression when assessed 18 months postsurgery. | Low |
| Visconti (2002)55 | US | Cross‐sectional | N=143 parents | Parenting stress | PSI | PCCHDs reported significantly less stress and more social support than a normative sample 3 years postcardiac surgery. | Low |
| Vrijmoet‐Wiersma (2009)56 | The Netherlands | Cross‐sectional |
N=196 58% mothers |
Anxiety/depression stress/distress parenting stress |
STAI GHQ PSI |
Mothers had significantly higher anxiety scores on the STAI compared with a normative reference group; no significant differences were found for fathers. Both mothers and fathers scored comparable to instrument reference groups on the generic stress questionnaire of the GHQ. Parenting stress levels on the PSI were comparable to normative reference groups. |
Low |
| Wray (2004)57 | UK | Longitudinal |
N=102 parents 53% mothers |
Stress/distress | GHQ |
65% of mothers and 48% of fathers reported being distressed immediately prior to surgery. PCCHDs had significantly higher rates of distress than parents of healthy children. PCCHDs experienced significant decreases in distress over time compared with no changes in parents of healthy children. |
Low |
| Bevilacqua (2013)28 | Italy | Cross‐sectional | N=38 couples | Anxiety/depression stress/distress | GHQ |
46% of mothers and 20% of fathers were reported to be depressed. 82% of mothers and 61% of fathers reported psychological distress. PCCHDs had significantly lower mental health component scores compared with controls. |
Medium |
| Brosig (2007)29 | US | Cross‐sectional | N=26 parents | Parenting stress | PSI | Parenting stress was significantly lower for PCCHDs compared with controls. | Medium |
| DeMaso (1991)31 | US | Cross‐sectional | N=99 mothers | Parenting stress | PSI |
Mean score on PSI was significantly different from the comparative mean for “normal healthy children. PSI scores were positively and significantly correlated with child behavior problems. |
Medium |
| Guan (2014)36 | China | Cross‐sectional | N=29 parents 66% mothers | Anxiety/depression | GHQ |
Mothers of CCHDs reported higher levels of anxiety and depression compared with controls up to 5 years postsurgical repair. Maternal anxiety was 4 times more likely if behavioral problems in the child were reported. No significant differences were noted in fathers. |
Medium |
| Helfricht (2009)38 | Switzerland | Longitudinal |
N=61 parents 57% mothers |
Trauma | ASDS |
25% of PCCHDs were diagnosed with ASD when assessed at 3 weeks postsurgical repair. ASDS scores were significantly correlated with measures of anxiety and depression. ASDS scores were significantly predictive of PTSD 6 months posttrauma. |
Medium |
| Jordan (2014)40 | Australia | Cross‐sectional | N=97 mothers | Anxiety/depression | EPDS | Maternal depression was significantly associated with boding difficulties and feelings of attachment towards the CHD infant. | Medium |
| Majnemer (2006)42 | Canada | Longitudinal |
N=49 parents 82% mothers |
Parenting stress | PSI |
27% of PCCHDs were classified as having high parenting stress. If the child was cyanotic prior to first surgery, the odds of high parenting stress 5 years postsurgery increased by a factor of 4.5 (95% CI, 1.05–19.02). |
Medium |
| Sarajuuri (2012)45 | Finland | Cross‐sectional |
N=54 parents 56% mothers |
Parenting stress | PSI | PCCHDs reported significantly more parenting stress than healthy controls. | Medium |
| Tallon (2015)50 | Australia | Cross‐sectional | N=91 mothers | Anxiety/depression stress/distress | Depression Anxiety Stress Scale |
30% of mothers reported some level of stress, 25% reported “abnormal” levels of anxiety, and 20% reported symptoms of depression. Severity of CHD corresponded to higher levels of depression in mothers. |
Medium |
| Torowicz (2010)51 | US | Cross‐sectional | N=129 mothers | Parenting stress | PSI | Parenting demands of infants with critical CHD, regardless of single‐ventricle and biventricular physiology, were a source of increased parenting stress when compared with healthy controls (P<0.05). | Medium |
| Uzark (2003)53 | US | Cross‐sectional |
N=80 parents 86% mothers |
Parenting stress | PSI |
PCCHDs experience greater levels of parenting stress than population norms. 25% of PCCHDs experience clinically significant levels of parenting stress. |
Medium |
| Van Horn (2001)54 | US | Longitudinal | N=38 mothers | Anxiety/depression | How “depressed” and “anxious” on 7‐point scale |
At initial interviews, maternal anxiety was classified in high range; depressed mood determined in moderate‐high range. At follow‐up, symptoms of anxiety and depression significantly decreased. |
Medium |
| Gardner (1996)34 | UK | Longitudinal | N=20 mothers | Stress/distress | GHQ | CHD mothers were significantly more distressed than controls 2 days before surgery, but were indistinguishable from controls 6 months postsurgery. | High |
Risk of bias based on 5‐item, 4‐domain, risk of bias assessment. Low risk=score=1 in domains I–IV; medium risk=study was insufficient in 1 domain (score=0 in domains I–III or score=1 in domain IV); high risk=study was insufficient in >1 domain (score of 0 or 1 in domain IV) in >1 domain. ASD indicates acute stress disorder; ASDS, Acute Stress Disorder Scale; CHDs, congenital heart defects; EPDS, Edinburgh Postnatal Depression Scale; GHQ, General Health Questionnaire; MHRQoL, mental health–related quality of life; PCCHDs, parents of children with critical congenital heart defects; PDS, Posttraumatic Stress Diagnostic Scale; PSI, Parenting Stress Index; PTSD, posttraumatic stress disorder; SCID, Structured Clinical Interview for DSM‐IV; STAI, State Trait Anxiety Inventory.
Results
Study Characteristics
A total of 30 articles were included in the review after reading 587 abstracts/titles and reviewing 71 full‐text articles (Figure). Of these articles, 14 were cross‐sectional and 16 were longitudinal; 17 of the studies were classified as having a low risk of bias, 12 were categorized as having a medium risk of bias, and 1 was categorized as having a high risk of bias. The studies were published in a variety of cardiac, nursing, pediatric, and social science journals with samples of parents from the following countries: the United States (n=7), Australia (n=6), Switzerland (n=3), Norway (n=4), The Netherlands (n=3), the United Kingdom (n=3), Canada (n=1), China (n=1), Finland (n=1), and Italy (n=1). The publication dates of the articles ranged from 1984 to 2015, with the majority (73%) published in the past 10 years. This time frame is consistent with biomedical progress in the field, which saw major breakthroughs in surgical treatment throughout the late 1970s, 1980s, and early 1990s, resulting in significant increases in survival.3
Summary of Key Findings
Table 2 provides descriptive information for the studies.28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57 The review is organized according to the following areas of mental health: (I) trauma, (II) depression and anxiety, (III) general indicators of psychological stress/distress and well‐being, and (IV) parenting stress. Within each area, the review is further organized according to study design and duration of time since the most recent cardiac surgical procedure.
I. Trauma
Five studies reviewed focused on trauma. All of the studies used standardized assessments of trauma symptoms (eg, intrusion, avoidance, arousal and reactivity, and distress/impairment in daily living) that are indicative of a diagnosis of ASD (symptoms <4 weeks after the trauma) or PTSD (symptoms >4 weeks after the trauma). Four of the trauma studies were classified as low risk30, 33, 39, 41 and one was classified as medium risk38 in the bias assessment.
Cross‐sectional studies
In a sample of 132 Australian parents whose children underwent cardiac surgery before the age of 3 months, 35% of mothers and 18% of fathers satisfied criteria for ASD 1 month after their infant was discharged from the hospital. Mothers in this sample reported significantly more symptoms than fathers (P<0.05), with 83% of the parents endorsing at least one trauma symptom at a clinical level.33 Another cross‐sectional study asked 29 parents of children who had undergone the stage I Norwood repair for hypoplastic left heart syndrome to recall their symptoms of trauma at the time they were discharged from the ICU, and 83% of the parents in the sample retrospectively met criteria for either PTSD or ASD.30 These cross‐sectional data were supported by several longitudinal studies of surgery‐related PTSD among Swiss PCCHDs.
Longitudinal studies
Two studies from the same cohort of 233 Swiss parents found that ≈15% of PCCHDs met criteria for ASD upon discharge from the hospital postcardiac surgery,39 25% met criteria for PTSD 1 month postsurgery,41 and 10% to 15% (10% for fathers, 15% for mothers) still met criteria for PTSD 6 months postsurgery.39 Trauma in this cohort of parents was significantly associated with low mental health quality of life in both mothers (adjusted odds ratio, 8.99; 95% CI, 3.57–22.62) and fathers (adjusted odds ratio, 18.15; 95% CI, 4.75–69.39) at hospital discharge, but not 6 months later.41 Similar results were obtained with 61 Swiss PCCHDs assessed 3 weeks postcardiac surgery, with 25% meeting diagnostic criteria for ASD. These acute trauma symptoms were significantly correlated with PTSD symptoms 6 months later (r=0.45, P<0.01).38 In sum, the trauma‐focused literature on PCCHDs reveals levels of PTSD and ASD that are well above national norms58 and consistent with other studies of parents whose children must spend time in an ICU.10, 11, 12
II. Anxiety and depression
Thirteen studies assessed symptoms of depression and/or anxiety using a variety of standardized screening tools at intervals ranging from the inpatient stay associated with the most recent cardiac surgery, to several years postsurgery. Of these studies, eight were classified as low in risk of bias,37, 43, 44, 46, 47, 48, 52, 56 and five were classified as medium.28, 36, 40, 50, 54
Cross‐sectional studies
In a study of 92 Australian mothers who were assessed during their child's hospital stay for cardiac surgery, 25% reported “abnormal” levels of anxiety and 20% reported levels of depression “outside the normal range.”50 Furthermore, the complexity of the surgical repair was significantly associated with depressive symptoms (P<0.05), a finding that was corroborated in a study of 196 Dutch PCCHDs—parents of children who underwent >2 cardiac surgeries reported higher levels of anxiety than parents of children who only had one procedure (P<0.05).56 Evidence for clinical symptoms of depression in the immediate postoperative period was also found in a study of Italian parents (N=38), where there was a significantly higher prevalence among mothers (46%) compared with fathers (20%, P<0.05).28 Similarly, among Australian parents assessed within 4 weeks of their child's cardiac surgery,37, 40 slightly more than half (51%) reported excessive worry and 26% reported symptoms of depression.37 In addition, maternal depression was significantly associated with bonding difficulties (P<0.01) and lower levels of maternal attachment (P<0.0001).40 Finally, two studies found that symptoms of anxiety persisted over time and were significantly (P<0.05) higher than normative reference groups three56 to five36 years posthospitalization. These findings were again among mothers only, and maternal anxiety was also associated with a more than 4‐fold increase in the risk for child behavior problems ≈5 years postcardiac surgery (odds ratio, 4.50; 95% CI, 3.22–5.89).36
Longitudinal studies
The cross‐sectional data were largely supported by several prospective studies monitoring parental anxiety and depression over time. In a study designed to examine the emotional state of 38 American mothers of children with CCHDs who were hospitalized for a cardiac‐related issue, symptoms of anxiety and depression—as measured on a 7–point Likert‐type scale—were high during hospitalization (mean anxiety=5.8; mean depression=4.3), but declined significantly 2 to 4 weeks later (mean anxiety=3.3, mean depression=2.2; P<0.001).54 Similar declines in depressive symptoms were observed among parents with infants undergoing surgical CHD repair who were assessed 1 to 2 days prior to surgery, the day of discharge from the hospital (typically 7 days later), and again 8 weeks postcardiac surgery.44 Compared with a control group of parents of infants attending a well‐baby visit, PCCHDs were not significantly different prior to surgery, but reported significantly more depressive symptoms 7 days postsurgery (P<0.05).44 When the groups were again compared 8 weeks later, the PCCHDs were once again indistinguishable from control parents on symptoms of depression despite continuing to report significant disruption in their home, work, and school environment.44
This variable course of mood symptoms over time was also noted in 2 studies following parents from precardiac surgery to several years postsurgery.43, 52 Among 150 Dutch PCCHDs assessed 5 weeks prior to cardiac surgery and again 18 months later,52 mothers’ symptoms of anxiety and sleeplessness presurgery were higher than both a normative reference group and mothers of children undergoing cardiac catheterization (P<0.05); however, these symptoms decreased significantly over time (P<0.05) and were lower than the normative reference group 18 months postsurgery (P<0.05), but still significantly higher than the mothers of children undergoing cardiac catherterization.52 Fathers of children undergoing cardiac surgery and cardiac catheterization also reported a significant decrease in anxiety over time (P<0.05) and were significantly lower than the normative reference group both precardiac and postcardiac surgery (P<0.05).52 Finally, both mothers and fathers in this sample, while indistinguishable from the normative reference group on symptoms of depression presurgery, reported significantly less severe symptoms than the control group 18 months later. Similar findings were observed with 39 Australian parents who were assessed immediately prior to cardiac surgery and again 1 to 4 years later.43 Mothers reported significantly more symptoms of anxiety than normative reference groups presurgery, irrespective of the severity of the cardiac anomaly, but these levels of anxiety fell significantly and were indistinguishable from the reference group several years later (P<0.0001).
These significant decreases in symptoms of anxiety and depression were not replicated in 3 studies that used data from the MoBa (Norwegian Mother and Child Cohort Study) to assess mothers of children with CCHDs prospectively from pregnancy through 6,46 18,47 and 3648 months postpartum. The first study compared 73 mothers of children with CCHDs with 169 mothers of children with mild or moderate CHDs (ie, generally asymptomatic and without need of invasive surgical repair), and found that while prenatal symptoms of depression were not significantly different between the groups, by 6 months postpartum, 29% of the mothers whose children had severe CHD had scores indicative of clinically significant depression and were ≈2.5 times more likely to be depressed compared with mothers whose children had mild/moderate CHDs (adjusted odds ratio, 2.22; 95% CI, 1.14–4.33 [P<0.05]).46 The other two MoBa studies compared symptoms of anxiety and depression prenatally through 36 months postpartum among similarly grouped mothers of children with mild (n=63–73), moderate (n=31–42), and severe (n=47) CHDs and healthy controls (N=≈44 000).47, 48 The first study of the two found that while, again, there were no significant differences prenatally, by 6 and 18 months postpartum, mothers of children with CCHDs reported significantly (P<0.005) higher symptoms of depression and anxiety compared with controls at 6 months (effect size [d] for anxiety=0.39; d for depression=0.76) and 18 months postpartum (d anxiety=0.36; d for depression=0.73). Mothers of children with severe CHD also had higher depression scores than mothers of infants with mild (P<0.01) or moderate (P<0.01) CHDs.47 These findings persisted at 36 months postpartum, with mothers of children with CCHDs still reporting significantly higher symptoms of depression and anxiety compared with controls (P<0.05) and with mothers of children with mild or moderate CHDs (P<0.05).48 In sum, the data on anxiety and depression indicated that PCCHDs are at significant risk for both; however, the persistence of these symptoms over time is unclear. Some studies reveal that symptoms decrease over time and are even lower than normative reference groups, while others indicate that symptoms can persist for years postsurgery.
III. General indicators of psychological stress, distress, and/or well‐being
Ten studies included global measure of stress, distress, quality of life, or subjective well‐being. There was considerable heterogeneity in how these variables were defined and measured, and at what time point postsurgery assessments occurred. Seven of the studies were classified as low35, 37, 41, 44, 49, 56, 57 in the risk of bias assessment, 2 were classified as medium,28, 50 and 1 was classified as high.34
Cross‐sectional studies
Three studies examined levels of stress or psychosocial functioning of parents while their child was still an inpatient following cardiac surgery.28, 37, 50 The prevalence of distress was high, ranging from 30% to 40% in 2 studies of Australian PCCHDs37, 50 up to 60% to 80% with a small (N=38 couples) sample of Italian parents.28 Again, there were sex differences, with mothers reporting significantly more stress than fathers (P<0.05).28 While there were only two cross‐sectional studies on the long‐term persistence of psychological distress among PCCHDs, both showed that symptoms did not increase over time, but were either equivalent to56 or lower than49 levels of distress in control or normative reference groups.
Longitudinal studies
Four longitudinal studies assessed levels of stress/distress during the hospital stay, and then again 2 to 36 months postcardiac surgery.35, 41, 44, 57 The first,44 mentioned previously, measured overall distress among parents of infants undergoing surgical repair of a CHD (n=20) and parents of infants making visits to a well‐baby clinic (n=8). There were no significant differences between the groups at baseline (assessed 2 days presurgery); however, by 7 days postsurgery, PCCHDs were significantly more distressed compared with the control group (P<0.05), and while mood improved significantly by 2 months postsurgery, overall levels of distress continued to be significantly higher in the CHD group (P<0.05). Similar findings were observed in a study that assessed mental health–related quality of life in a sample of 232 Swiss PCCHDs.41 Mothers reported significantly lower mental health quality of life compared with population norms upon discharge from the hospital postcardiac surgery (P<0.001), while fathers were indistinguishable from population norms. Mental health quality of life scores improved significantly over time with both mothers and fathers scoring significantly higher (P<0.001) than population norms by 6 months postsurgery.41
Extending these findings, 2 studies followed parents 1 to 3 years after cardiac surgery.35, 57 The first compared levels of distress among PCCHDs (n=102) with parents of children undergoing a bone marrow transplant (n=114) and parents of healthy controls (n=122).57 Both bone marrow transplant and CCHD parents exhibited significantly higher levels of distress compared with healthy controls when assessed the day before surgery (P<0.001), with 65% of CCHD mothers and 48% of CCHD fathers reporting clinical levels of distress. Consistent with the other longitudinal studies, there was a significant decrease in symptoms over time (P<0.05), and by 12 months postsurgery there were no significant differences between the 3 groups. Conversely, data from the Norwegian MoBa cohort found that PCCHDs (N=60) had significantly lower scores on a measure of subjective well‐being than controls when assessed at 6 (P<0.01) and 36 (P<0.01) months postpartum.35 In sum, the broad literature on psychological distress indicated that PCCHDs experience significant symptoms in the time immediately before and after cardiac surgery, but that these symptoms often decrease over time and are consistent with or even lower than healthy controls.
IV. Parenting stress
Nine studies measured parenting stress, which is generally defined as the magnitude of stress associated with the parent‐child relationship. All of the studies used a version of the Parenting Stress Index, although domains and number of items measured differed across studies. Only three parenting stress studies were classified as low32, 55, 56 in the risk of bias assessment, with the remainder categorized as medium.29, 31, 42, 45, 51, 53
Cross‐sectional studies
Three cross‐sectional studies assessed parents of children with CCHDs aged 3 months,51 18 months,45 and 6 years,53 and found that PCCHDs reported significantly higher levels of parenting stress compared with healthy controls (P<0.05), with ≈20% of parents reporting symptoms that would be considered in the clinical range on standardized assessments.53 Three studies, however, found no significant differences in parenting stress among PCCHDs, compared with parents of healthy controls, when outcomes were measured more than 3 years after the surgical repair or palliation.29, 31, 56 While these cross‐sectional findings indicate that, similar to the stress/distress studies, parenting stress symptoms may decrease over time, the longitudinal studies were less supportive of this conclusion.
Longitudinal studies
In a study of 326 PCCHDs from the United Kingdom, parenting stress was assessed the day before cardiac surgery and again 2 weeks later.32 Parenting stress was found to be highest the day before surgery and decreased slightly over time until an increase again ≈2 weeks postsurgery. Furthermore, lower socioeconomic status was correlated with greater parenting stress, and parents of infants with CCHDs reported higher levels of stress compared with parents of older children with CCHDs.32 Consistent with these findings, elevated levels of parenting stress persisted up to 5 years postsurgery among a sample of 49 Canadian PCCHDs, with 27% still indicating high levels of stress 5 years later.42 Further, the odds of a parent being stressed 5 years postsurgery were 4.5 times higher (95% CI, 1.05–19.02) among parents of children who were cyanotic prior to surgery, compared with those who were not—again highlighting the relevance of CHD severity in the persistence of parental mental health symptoms over time.42
One study did not find parenting stress to be significantly worse over time among PCCHDs compared with normative samples.55 Among PCCHDs in the United States who were assessed when their children were aged 1 and 4 years, parenting stress was significantly lower (P<0.001) than the normative reference group at both time points and did not increase or decrease significantly over time.55 Furthermore, these parents reported significantly more social support (P<0.0001) and fewer child behavior problems (P<0.0001), compared with a normative reference group, indicating that, as has been noted throughout the review, data are mixed regarding the persistence of parenting stress symptom severity over time, with some parents doing worse and some doing significantly better than reference groups.
Discussion
We conducted a systematic review of the literature on the mental health of parents of children with CCHDs. Using guidelines from the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses, a wide variety of search terms, and 3 electronic databases, the search produced 587 citations, 30 of which were eligible and included in this review. Studies were conducted all over the world, with high variability in measurements used to assess study outcomes, methodological quality, length of time since most recent cardiac surgery when the assessments occurred, and covariates variables included in multivariable analyses.
Overall, the literature revealed that PCCHDs are at an elevated risk for mental health problems, particularly in the immediate weeks and months following cardiac surgery. Consistent with the literature on parents of children who spend time in the ICU, up to 30% of PCCHDs have symptoms consistent with a diagnosis of PTSD, with over 80% presenting with clinically significant symptoms of trauma. Further, 25% to 50% of PCCHDs reported clinically elevated symptoms of depression and/or anxiety, and 30% to 80% of parents reported experiencing psychological distress. For comparison, the prevalence of PTSD in the US general population is 3.5%, with 18% meeting criteria for any anxiety disorder in the last year, 9.5% meeting criteria for any mood disorder, and 10% to 15% meeting criteria for postpartum depression.10, 58
The literature was equivocal on the extent to which these psychological symptoms persist over time, with some studies showing a return to normative values several months postsurgery, others revealing that symptoms can persist at significantly higher levels than normative reference groups many years postsurgery, and still others reporting that PCCHDs have significantly better mental health–related outcomes than “normal” parents. It is unclear to what extent these seemingly contradictory findings can be explained by time at which the assessments occurred, the measurements used, and moderating variables.
While most of the studies reviewed accounted for another variable as either a covariate in multivariable analyses (eg, socioeconomic status) or an effect modifier in stratified analyses (eg, sex), there was inconsistency in which variables were included and how they were factored into hypothesis testing—perhaps due to the exploratory, descriptive nature of most of the studies reviewed. There were 2 variables, however, that were more consistently included than others: sex of the parent and some indicator of heart defect severity (eg, length of hospital stay, ventricular physiology). As noted throughout the review, mothers generally reported significantly more psychological symptoms than fathers, and the severity of mental health symptoms was positively correlated with the severity of the heart defect.
Moving forward, this literature would benefit from the use of a relevant theoretical model (eg, Abdin's model of parenting stress) to guide variable selection, hypothesis generation, data analyses, and interpretation of study findings to further clarify mediators and moderators of the relationship between having a child with a CCHD and parental mental health.
Recommendations for Research and Clinical Practice
Findings from this review indicate that PCCHDs require routine, comprehensive, and standardized mental health screening that would ideally be incorporated into ongoing pediatric cardiac care. This would enable appropriate referral of parents to mental health services that could address their acute psychological needs and enhance their ability to cope with the many ongoing stressors they face. Regular screening within these settings would also allow researchers to better characterize the types of mental health problems experienced most frequently by these parents, their trajectory and severity over time, and key periods of increased risk. These data could inform the development of specialized mental health treatment and referral systems nested within the pediatric cardiology care setting. Indeed, there is already a recognized need for universal screening of depression in pregnant and postpartum women in conjunction with prenatal and postnatal care.59 Based on results of this review, a similar approach to mental health screening and treatment for parents in pediatric cardiac care settings is essential.
Results of this review also indicate the need for further research in 3 important areas. First, the findings suggest that mothers are at greater mental health risk than fathers, but the sources of this risk are not known. It is possible that greater caregiving and parenting demands experienced by mothers contribute to their mental health problems, particularly since mothers are more often at the bedside during long hospitalizations, incurring disproportionate financial, social, and personal costs.60 However, specific contributing factors must continue to be carefully examined. There is also a need to study additional moderating factors that influence parent mental health over time. The lack of consistent findings across studies regarding persistence of mental health problems among parents is likely related to different characteristics of parents, the child's illness, the caregiving environment, and/or access to healthcare support in the samples studied. These moderators must be identifed so that their effects are better understood and specialized mental health services for the most vulnerable parents can be delivered at their greatest times of need.
Finally, findings of the review implicate the importance of an integrated model of care that incorporates empirically supported mental health screening and interventions into pediatric cardiology practice. Given that only 44% of people with serious psychological distress (ie, clinically significant symptoms of a mental disorder) report using mental health services in the past year,61 capturing affected parents in conjunction with their child's medical appointments may be a novel way to connect them to care. The integration of psychological services into medical clinics has been successfully executed in primary care settings over the past 10 to 20 years62 and has proven to be a cost‐effective and efficacious way to treat mental health problems in adult cardiac care settings.63, 64 Research on the implementation of such a model in a pediatric cardiology setting would connect a high‐risk group to treatment and have great potential to improve the physical, cognitive, and psychological outcomes of the pediatric patients themselves.
Limitations
The studies we reviewed were highly variable in terms of sample size, type of measurements used, third variables included, time points assessed, comparison groups used, and sociodemographic composition of the participants. Samples of parents came from all over the world and the extent to which findings from one country and medical care setting can be compared with another is unclear. For example, national policies on paid maternity and paternity leave, socialized medicine, and access to mental health care are likely country‐level moderators of the association between having a child with a CCHD and subsequent development of parental mental health problems. Also, although we focused on CCHDs, rather than all CHDs, there are still subgroups within CCHDs (eg, children with co‐occurring chromosomal abnormalities, parents with preexisting mental health problems) who deserve separate consideration, as the findings we observed here are likely to be more extreme among these groups. Finally, the majority of the reviewed studies did not focus on a mental health diagnosis but instead relied on mental health symptoms and/or general indicators of psychological distress. We thus do not know the full extent of psychological morbidity among these parents based on this review. These limitations highlight the need for more prospective cohort studies that can comprehensively assess mental health disorders with standardized screening instruments, and follow PCCHDs over time, from diagnosis through surgery and ongoing management of the CHD postsurgery.
Conclusions
Parents of children with CCHDs are at elevated risk for mental health problems. There is an urgent need for additional research on the severity, course, persistence, and moderators of these mental health problems over time, and for the development and testing of screening approaches and interventions that can be feasibly delivered in the context of ongoing pediatric cardiac care. Such research would connect PCCHDs to appropriate care, ameliorate psychological symptoms and suffering, and consequently enhance the overall care and well‐being of children with CCHDs.
Sources of Funding
This work was supported by a grant from the Hellman Fellows Fund as part of the Hellman Fellows Program (principal investigator: Woolf‐King) and the following grants from the National Institute of Child and Human Development: NICHD R01 HD084813 (principal investigator: Weiss) and NICHD R01 HD081188 (principal investigator: Weiss).
Disclosures
None.
(J Am Heart Assoc. 2017;6:e004862. DOI: 10.1161/JAHA.116.004862.)
References
- 1. Centers for Disease Control and Prevention (CDC) . Congenital heart defects (CHDs). 2015. Available at: http://www.cdc.gov/ncbddd/heartdefects/data.html. Accessed May 1, 2016.
- 2. Oster ME, Lee KA, Honein MA, Riehle‐Colarusso T, Shin M, Correa A. Temporal trends in survival among infants with critical congenital heart defects. Pediatrics. 2013;131:e1502–e1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Best KE, Rankin J. Long‐term survival of individuals born with congenital heart disease: a systematic review and meta‐analysis. J Am Heart Assoc. 2016;5:e002846 doi: 10.1161/JAHA.115.002846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Connor JA, Kline NE, Mott S, Harris SK, Jenkins KJ. The meaning of cost for families of children with congenital heart disease. J Pediatr Health Care. 2010;24:318–325. [DOI] [PubMed] [Google Scholar]
- 5. Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: a systematic review. J Clin Psychiatry. 2006;67:1285–1298. [DOI] [PubMed] [Google Scholar]
- 6. Hopkins J, Marcus M, Campbell SB. Postpartum depression: a critical review. Psychol Bull. 1984;95:498–515. [PubMed] [Google Scholar]
- 7. Vesga‐Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ward‐Begnoche W. Posttraumatic stress symptoms in the pediatric intensive care unit. Pediatr Nurs. 2007;12:84–92. [DOI] [PubMed] [Google Scholar]
- 9. Murray L, Cooper P, Hipwell A. Mental health of parents caring for infants. Arch Womens Ment Health. 2003;6(suppl 2):S71–S77. [DOI] [PubMed] [Google Scholar]
- 10. Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). J Clin Psychol Med Settings. 2010;17:230–237. [DOI] [PubMed] [Google Scholar]
- 11. Shaw RJ, Deblois T, Ikuta L, Ginzburg K, Fleisher B, Koopman C. Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics. 2006;47:206–212. [DOI] [PubMed] [Google Scholar]
- 12. Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr Crit Care Med. 2012;13:338–347. [DOI] [PubMed] [Google Scholar]
- 13. Lyons‐Ruth K, Wolfe R, Lyubchik A. Depression and the parenting of young children: making the case for early preventive mental health services. Harv Rev Psychiatry. 2000;8:148–153. [PubMed] [Google Scholar]
- 14. McPeak KE, Sandrock D, Spector ND, Pattishall AE. Important determinants of newborn health: postpartum depression, teen parenting, and breast‐feeding. Curr Opin Pediatr. 2015;27:138–144. [DOI] [PubMed] [Google Scholar]
- 15. Mirhosseini H, Moosavipoor SA, Nazari MA, Dehghan A, Mirhosseini S, Bidaki R, Yazdian‐Anari P. Cognitive behavioral development in children following maternal postpartum depression: a review article. Electron Physician. 2015;7:1673–1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tronick E, Reck C. Infants of depressed mothers. Harv Rev Psychiatry. 2009;17:147–156. [DOI] [PubMed] [Google Scholar]
- 17. Abidin RR. Introduction to the special issue: the stresses of parenting. J Clin Child Psychol. 1990;19:298–301. [Google Scholar]
- 18. Miklush L, Connelly CD. Maternal depression and infant development: theory and current evidence. MCN Am J Matern Child Nurs. 2013;38:369–374; quiz 375–366. [DOI] [PubMed] [Google Scholar]
- 19. Jackson AC, Frydenberg E, Liang RP, Higgins RO, Murphy BM. Familial impact and coping with child heart disease: a systematic review. Pediatr Cardiol. 2015;36:695–712. [DOI] [PubMed] [Google Scholar]
- 20. Wei H, Roscigno CI, Hanson CC, Swanson KM. Families of children with congenital heart disease: a literature review. Heart Lung. 2015;44:494–511. [DOI] [PubMed] [Google Scholar]
- 21. Lawoko S. Factors influencing satisfaction and well‐being among parents of congenital heart disease children: development of a conceptual model based on the literature review. Scand J Caring Sci. 2007;21:106–117. [DOI] [PubMed] [Google Scholar]
- 22. Soulvie MA, Desai PP, White CP, Sullivan BN. Psychological distress experienced by parents of young children with congenital heart defects: a comprehensive review of literature. J Soc Serv Res. 2012;38:484–502. [Google Scholar]
- 23. Wiener L, Kazak AE, Noll RB, Patenaude AF, Kupst MJ. Standards for the psychosocial care of children with cancer and their families: an introduction to the special issue. Pediatr Blood Cancer. 2015;62(suppl 5):S419–S424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Allan RE, Scheidt SS. Heart & Mind: The Practice of Cardiac Psychology. Washington, DC: American Psychological Association; 1996. [Google Scholar]
- 25. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Farley LM, DeMaso DR, D'Angelo E, Kinnamon C, Bastardi H, Hill CE, Blume ED, Logan DE. Parenting stress and parental post‐traumatic stress disorder in families after pediatric heart transplantation. J Heart Lung Transplant. 2007;26:120–126. [DOI] [PubMed] [Google Scholar]
- 27. Viswanathan M, Ansari MT, Berkman ND, Chang S, Hartling L, McPheeters M, Santaguida PL, Shamliyan T, Singh K, Tsertsvadze A, Treadwell JR. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions In: Methods Guide for Effectiveness and Comparative Effectiveness Reviews [Internet]. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008. [PubMed] [Google Scholar]
- 28. Bevilacqua F, Palatta S, Mirante N, Cuttini M, Seganti G, Dotta A, Piersigilli F. Birth of a child with congenital heart disease: emotional reactions of mothers and fathers according to time of diagnosis. J Matern Fetal Neonatal Med. 2013;26:1249–1253. [DOI] [PubMed] [Google Scholar]
- 29. Brosig CL, Mussatto KA, Kuhn EM, Tweddell JS. Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatr Cardiol. 2007;28:255–262. [DOI] [PubMed] [Google Scholar]
- 30. Cantwell‐Bartl AM, Tibballs J. Psychosocial experiences of parents of infants with hypoplastic left heart syndrome in the PICU. Pediatr Crit Care Med. 2013;14:869–875. [DOI] [PubMed] [Google Scholar]
- 31. DeMaso DR, Campis LK, Wypij D, Bertram S, Lipshitz M, Freed M. The impact of maternal perceptions and medical severity on the adjustment of children with congenital heart disease. J Pediatr Psychol. 1991;16:137–149. [DOI] [PubMed] [Google Scholar]
- 32. Franck LS, McQuillan A, Wray J, Grocott MP, Goldman A. Parent stress levels during children's hospital recovery after congenital heart surgery. Pediatr Cardiol. 2010;31:961–968. [DOI] [PubMed] [Google Scholar]
- 33. Franich‐Ray C, Bright MA, Anderson V, Northam E, Cochrane A, Menahem S, Jordan B. Trauma reactions in mothers and fathers after their infant's cardiac surgery. J Pediatr Psychol. 2013;38:494–505. [DOI] [PubMed] [Google Scholar]
- 34. Gardner FV, Freeman NH, Black AM, Angelini GD. Disturbed mother‐infant interaction in association with congenital heart disease. Heart. 1996;76:56–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gronning Dale MT, Solberg O, Holmstrom H, Landolt MA, Eskedal LT, Vollrath ME. Well‐being in mothers of children with congenital heart defects: a 3‐year follow‐up. Qual Life Res. 2013;22:2063–2072. [DOI] [PubMed] [Google Scholar]
- 36. Guan G, Liu H, Wang Y, Han B, Jin Y. Behavioural and emotional outcomes in school‐aged children after surgery or transcatheter closure treatment for ventricular septal defect. Cardiol Young. 2014;24:910–917. [DOI] [PubMed] [Google Scholar]
- 37. Hearps SJ, McCarthy MC, Muscara F, Hearps SJ, Burke K, Jones B, Anderson VA. Psychosocial risk in families of infants undergoing surgery for a serious congenital heart disease. Cardiol Young. 2014;24:632–639. [DOI] [PubMed] [Google Scholar]
- 38. Helfricht S, Landolt MA, Moergeli H, Hepp U, Wegener D, Schnyder U. Psychometric evaluation and validation of the german version of the acute stress disorder scale across two distinct trauma populations. J Trauma Stress. 2009;22:476–480. [DOI] [PubMed] [Google Scholar]
- 39. Helfricht S, Latal B, Fischer JE, Tomaske M, Landolt MA. Surgery‐related posttraumatic stress disorder in parents of children undergoing cardiopulmonary bypass surgery: a prospective cohort study. Pediatr Crit Care Med. 2008;9:217–223. [DOI] [PubMed] [Google Scholar]
- 40. Jordan B, Franich‐Ray C, Albert N, Anderson V, Northam E, Cochrane A, Menahem S. Early mother‐infant relationships after cardiac surgery in infancy. Arch Dis Child. 2014;99:641–645. [DOI] [PubMed] [Google Scholar]
- 41. Landolt MA, Buechel EV, Latal B. Predictors of parental quality of life after child open heart surgery: a 6‐month prospective study. J Pediatr. 2011;158:37–43. [DOI] [PubMed] [Google Scholar]
- 42. Majnemer A, Limperopoulos C, Shevell M, Rohlicek C, Rosenblatt B, Tchervenkov C. Health and well‐being of children with congenital cardiac malformations, and their families, following open‐heart surgery. Cardiol Young. 2006;16:157–164. [DOI] [PubMed] [Google Scholar]
- 43. Menahem S, Poulakis Z, Prior M. Children subjected to cardiac surgery for congenital heart disease. Part 2—parental emotional experiences. Interact Cardiovasc Thorac Surg. 2008;7:605–608. [DOI] [PubMed] [Google Scholar]
- 44. Rogers TR, Forehand R, Furey W, Baskin C, Finch AJ Jr, Jordan S. Heart surgery in infants: a preliminary assessment of maternal adaptation. Child Health Care. 1984;13:52–58. [DOI] [PubMed] [Google Scholar]
- 45. Sarajuuri A, Lonnqvist T, Schmitt F, Almqvist F, Jokinen E. Patients with univentricular heart in early childhood: parenting stress and child behaviour. Acta Paediatr. 2012;101:252–257. [DOI] [PubMed] [Google Scholar]
- 46. Solberg O, Dale MT, Holmstrom H, Eskedal LT, Landolt MA, Vollrath ME. Emotional reactivity in infants with congenital heart defects and maternal symptoms of postnatal depression. Arch Womens Ment Health. 2011;14:487–492. [DOI] [PubMed] [Google Scholar]
- 47. Solberg O, Dale MT, Holmstrom H, Eskedal LT, Landolt MA, Vollrath ME. Long‐term symptoms of depression and anxiety in mothers of infants with congenital heart defects. J Pediatr Psychol. 2011;36:179–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Solberg O, Gronning Dale MT, Holmstrom H, Eskedal LT, Landolt MA, Vollrath ME. Trajectories of maternal mental health: a prospective study of mothers of infants with congenital heart defects from pregnancy to 36 months postpartum. J Pediatr Psychol. 2012;37:687–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Spijkerboer AW, Helbing WA, Bogers AJ, Van Domburg RT, Verhulst FC, Utens EM. Long‐term psychological distress, and styles of coping, in parents of children and adolescents who underwent invasive treatment for congenital cardiac disease. Cardiol Young. 2007;17:638–645. [DOI] [PubMed] [Google Scholar]
- 50. Tallon MM, Kendall GE, Snider PD. Development of a measure for maternal confidence in knowledge and understanding and examination of psychosocial influences at the time of a child's heart surgery. J Spec Pediatr Nurs. 2015;20:36–48. [DOI] [PubMed] [Google Scholar]
- 51. Torowicz D, Irving SY, Hanlon AL, Sumpter DF, Medoff‐Cooper B. Infant temperament and parental stress in 3‐month‐old infants after surgery for complex congenital heart disease. J Dev Behav Pediatr. 2010;31:202–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Utens EM, Versluis‐Den Bieman HJ, Witsenburg M, Bogers AJ, Hess J, Verhulst FC. Does age at the time of elective cardiac surgery or catheter intervention in children influence the longitudinal development of psychological distress and styles of coping of parents? Cardiol Young. 2002;12:524–530. [DOI] [PubMed] [Google Scholar]
- 53. Uzark K, Jones K. Parenting stress and children with heart disease. J Pediatr Health Care. 2003;17:163–168. [DOI] [PubMed] [Google Scholar]
- 54. Van Horn M, DeMaso DR, Gonzalez‐Heydrich J, Erickson JD. Illness‐related concerns of mothers of children with congenital heart disease. J Am Acad Child Adolesc Psychiatry. 2001;40:847–854. [DOI] [PubMed] [Google Scholar]
- 55. Visconti KJ, Saudino KJ, Rappaport LA, Newburger JW, Bellinger DC. Influence of parental stress and social support on the behavioral adjustment of children with transposition of the great arteries. J Dev Behav Pediatr. 2002;23:314–321. [DOI] [PubMed] [Google Scholar]
- 56. Vrijmoet‐Wiersma CM, Ottenkamp J, van Roozendaal M, Grootenhuis MA, Koopman HM. A multicentric study of disease‐related stress, and perceived vulnerability, in parents of children with congenital cardiac disease. Cardiol Young. 2009;19:608–614. [DOI] [PubMed] [Google Scholar]
- 57. Wray J, Sensky T. Psychological functioning in parents of children undergoing elective cardiac surgery. Cardiol Young. 2004;14:131–139. [DOI] [PubMed] [Google Scholar]
- 58. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12‐month DSM‐IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Siu AL, Bibbins‐Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, Garcia FA, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, Pignone MP. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2016;315:380–387. [DOI] [PubMed] [Google Scholar]
- 60. Callery P. Paying to participate: financial, social and personal costs to parents of involvement in their children's care in hospital. J Adv Nurs. 1997;25:746–752. [DOI] [PubMed] [Google Scholar]
- 61. Results from the 2007 National Survey on Drug Use and Health: National Findings Substance Abuse and Mental Health Services Administration, National Findings (Office of Applied Studies, NSDUH Series H‐34, DHHS Publication No. SMA 08‐4343). Rockville, MD; 2008. [Google Scholar]
- 62. Robinson PJ, Strosahl KD. Behavioral health consultation and primary care: lessons learned. J Clin Psychol Med Settings. 2009;16:58–71. [DOI] [PubMed] [Google Scholar]
- 63. Huffman JC, Mastromauro CA, Beach SR, Celano CM, DuBois CM, Healy BC, Suarez L, Rollman BL, Januzzi JL. Collaborative care for depression and anxiety disorders in patients with recent cardiac events: the Management of Sadness and Anxiety in Cardiology (MOSAIC) randomized clinical trial. JAMA Intern Med. 2014;174:927–935. [DOI] [PubMed] [Google Scholar]
- 64. Celano CM, Healy B, Suarez L, Levy DE, Mastromauro C, Januzzi JL, Huffman JC. Cost‐effectiveness of a collaborative care depression and anxiety treatment program in patients with acute cardiac illness. Value Health. 2016;19:185–191. [DOI] [PubMed] [Google Scholar]


