Abstract
Background
Women, on average, have less muscle strength than men. This anthropometric-physiological trait may make them more vulnerable to excessive physical strain, injury, and inability to work. Strength training is used for preventive health maintenance and to lessen musculoskeletal symptoms. In this context, we studied whether the degree of muscle strength has any effect on women’s health in everyday working life, and also the effects of strength training for women on their health in the workplace.
Methods
We systematically searched the PubMed/MEDLINE, Embase, CINAHL, Web of Science, CENTRAL, and SPOLIT databases for pertinent publications, in accordance with the PRISMA criteria for literature searches. We analyzed all of the retrieved randomized controlled trials conducted on women aged 18 to 65 to determine the effects of training on muscle strength, physical performance ability, and health-related parameters including body composition, musculoskeletal pain, and subjective well-being.
Results
We did not find any studies that provided answers to the first question. As for the second question, the selection criteria were met by 12 of the 4969 retrieved studies, which dealt with the effect of strength training on health in the occupational environment and involved a total of 1365 female subjects. These studies were carried out in heterogeneous subject groups, with a variety of overlapping interventions consisting of both strength and endurance training. Significantly increased strength was found in all studies, as was a reduction of pain in all of the studies where this question was asked. Inconsistent results were obtained with respect to body weight, body composition, and subjective well-being.
Conclusion
The interventions that were conducted in these studies succeeded in increasing strength and reducing pain, even when the training was brief and of low intensity. This was true not only for women working in occupations requiring unusual physical strength, but also for those in sedentary occupations. The small number of studies performed on this subject to date is surprising in view of the high prevalence of musculoskeletal symptoms in women.
Continuing technological progress has had an enormous effect on working conditions and general lifestyle in recent decades, leading to a sharp decrease in physical activity (1, 2, e1– e3). This trend has been especially pronounced in the areas of work affected most by digitalization and automation. Nevertheless, many jobs still place high demands on physical performance capacity, particularly on muscle strength (3). Foremost among these occupations are the police, fire service, and armed forces, where the weight of operational equipment and protective clothing may reach 20 or even 40 kg (e4). Metal, wood, and construction workers regularly have to move heavy loads, as do those employed in the mail-order sector. The same is true for the health-related occupations, in which a high proportion of employees—4.0 out of 5.2 million in Germany—are women (e5). Nurses and carers have to turn patients and adopt uncomfortable and unnatural positions, often for extended periods, on a daily basis. These activities result in augmented occurrence of pathological biomechanical stress, injuries, and lost workdays (e6, e7). This is demonstrated, for instance, by the German statistics on occupational diseases: between 2002 and 2009, 59.1% of the recognized cases of occupational intervertebral disc-related disorders of the lumbar spine (code number 2108 in the official catalog of occupational diseases) occurred in women. Eighty-six percent of the affected women were working in the care and health sectors (4, 5).
However, musculoskeletal symptoms are not restricted to occupations with high physical demands but are also found in predominantly sedentary occupations (6). Data from health insurance providers clearly show the consequences of abnormal and excessive biomechanical stress across the whole working population. Almost a quarter of all lost workdays are attributable to disorders of the musculoskeletal system (7).
Women, owing to their anthropometric and physiological characteristics, are at elevated risk of musculoskeletal injuries from working with heavy loads. On average, they are around 10 cm shorter and 15 kg lighter than men (8, e8). Women have higher absolute and relative body fat than men, despite their lower body weight, and possess much less muscle tissue (9): men have about 40% more muscle mass in the upper body and about 33% more in the lower extremities (10– 12). The maximal strength attained by women is therefore only around 50–70% of that for men (13– 16).
Although for hormonal reasons strength training is less effective in women than in men, they may stand to particularly benefit from targeted functional training (14, 17). Employers, health insurance providers, and sports clubs have long offered programs to reduce back problems and improve performance capacity and biomechanical resilience in daily life by strengthening the muscles.
Despite the importance and the topicality of musculoskeletal injuries, we know of no reviews on the role of muscle strength and strength training as a preventive factor for women in the workplace. Our aim in carrying out the systematic literature review described in this article was therefore to answer the following questions:
Does a woman’s muscle strength affect her health in everyday work life?
Does strength training for women have any consequences for health in everyday work life?
Methods
A systematic review of the literature was carried out according to the stipulations of the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement (18). The study was registered in advance in the PROSPERO database (e9) (registration number: CRD42016039103).
Inclusion and exclusion criteria
The inclusion and exclusion criteria (table 1) were defined on the basis of an expanded PICO strategy (e10). No other publication or search restrictions were applied.
Table 1. PICO scheme for study selection expanded to include study design.
| PICO(S) item | Inclusion and exclusion criteria |
| P – Patient collective | The majority of the probands must be women in employment aged 18–65 years. Studies with pregnant women, minors, and tertiary prevention collectives will be excluded. If two or more publications with relevant methods deal with the same population, only the first publication will be considered |
| I – Intervention | The intervention must comprise defined strength training. Body strength must be measured as maximal voluntary isometric contraction or one-repetition maximum (1-RM). 1-RM describes the maximal weight that can be lifted or moved only once. |
| C – Control interven‧tion | Control groups without training intervention or with alternative training methods will be considered. |
| O – Outcome | The outcome must comprise information on muscle strength and the subjective or objective influence of muscle strength or strength training on health. Outcome evaluation must be sex specific. |
| S – Study design | Randomized controlled studies published in English or German before March 2016 will be included. No other study designs will be considered. |
Search strategy
The literature survey was carried out on 1 March 2016 and covered the databases PubMed/MEDLINE, Embase, CINAHL, Web of Science, CENTRAL, and SPOLIT. The detailed search strategy is shown in Table 1. In addition, the reference lists of the publications finally chosen for inclusion were scrutinized.
Study selection and data extraction
Initially, potentially relevant publications were selected by two of the authors of this article independently on the basis of title and abstract. Selection by one of the two searchers was deemed sufficient. Full analysis with verification of inclusion and exclusion criteria was carried out by all of the authors, with consensus being reached by discussion. Study data and study characteristics were recorded and checked according to an expanded PICO strategy.
Each publication’s risk of bias, i.e., the risk of systemic error, was analyzed with the Cochrane risk of bias tool for randomized controlled trials (RCT) (e11, e12). The bias was assessed independently by two authors. If they failed to agree, a third author joined them to achieve consensus by discussion. Owing to the heterogeneity of study design, the studies were summarized quantitatively.
The effect sizes of significant results, if not reported in the source, were calculated from the existing data (mean, standard deviation or standard error, group size) using R (package: compute.es) (e13) and expressed as corrected Hedges g. The small, medium, and large effect sizes according to Cohen are approximately 0.2, 0.5, and 0.8 (e14).
Results
Study selection
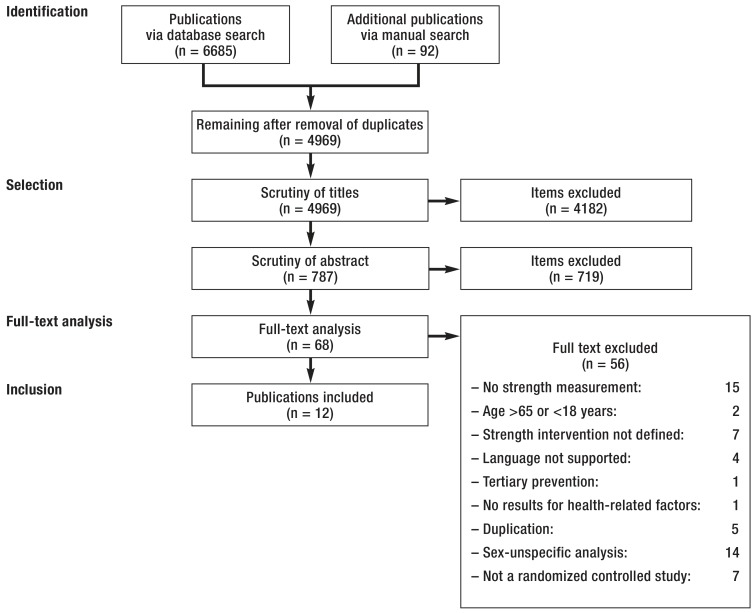
A total of 6685 publications were identified (figure). After elimination of duplicates and scrutiny of study titles and abstracts, 68 articles remained for full-text analysis. Twelve publications fulfilled the selection criteria laid out in Table 1 (19– 30). The commonest reasons for exclusion were the absence of sex-specific analysis and the lack of muscle strength measurement. The 12 selected studies included a total of 1365 female probands. No studies on the health consequences of differences in strength were identified.
Figure.
Flow chart of study selection according to the PRISMA criteria (18)
PRISMA, Preferred Reporting Items for Systematic Review and Meta-analysis
Risk of bias and effect sizes
The domains and the evaluation of the risk of bias in the studies chosen for inclusion can be found in eTable 2. One basic problem in training interventions is blinding of the participants and trainers, which is practically impossible with full prior provision of information. These systematic limitations explain the overall high or unclear risk of bias with regard to blinding of study participants and personnel. Furthermore, only one third of the studies describe how the randomization was performed and how the participants were kept unaware of group assignment (selection bias). In six studies there were no data on blinding with regard to endpoint ascertainment (detection bias), and in one study no blinding was undertaken at this stage (eTable 2, eTable 3) (e10).
eTable 2. Assessment of the risk of bias in the studies reviewed (19– 30) according to the Cochrane recommendations (e11).
| Study (First author. year) |
Domains for risk of bias assessment | ||||||
| Random sequence generation |
Allocation concealment | Blinding of participants | Blinding of personnel | Blinding of outcome assessment |
Incomplete outcome data | Selective reporting | |
| Ahlgren. 2001 (19) | ? | ? | B | ? | ? | ? | + |
| Christensen. 2012 (20) | + | + | – | ? | + | + | + |
| Hagberg. 2000 (21) | + | + | – | – | – | + | + |
| Hendrickson. 2010 (22) | ? | ? | – | ? | ? | ? | + |
| Jakobsen. 2015 (23) | + | + | – | ? | + | + | + |
| Jorgensen. 2011 (24) | + | ? | – | ? | + | + | + |
| Kraemer. 2001 (25) | ? | ? | – | ? | ? | ? | + |
| Lovelady. 2009 (26) | + | ? | – | ? | ? | + | + |
| Rasotto. 2015 (27) | + | + | – | ? | + | + | + |
| Schmitz. 2003 (28) | + | ? | – | ? | ? | + | + |
| Sinaki. 1996 (29) | ? | ? | – | ? | ? | + | – |
| Ylinen. 2003 (30) | + | ? | – | ? | + | + | – |
– High risk of bias; + low risk of bias; ? unclear risk of bias
Because blinding of participants is not feasible in the type of study reviewed here. the domain “Blinding of participants and personnel” was split and the two parts assessed separately
With the exception of one study, no effect sizes were stated. Jakobsen et al. were the only authors to report effect sizes for a portion of their results (23). For three publications effect sizes could not even be calculated retrospectively (25, 28, 30). The effect sizes we calculated are given with the individual results below.
Study characteristics
Table 2 provides an aggregated overview of the most important findings. Details of each study—participants, interventions, outcomes, measurement methods, and principal effects on physical performance capacity, health, and wellbeing—can be found in eTable 4.
Table 2. Aggregated overview of the principal intervention outcomes (19– 30).
| Study (first author. year) |
Main interventions | Physical performance capacity |
Pain | Wellbeing | Body weight/ FFM |
| Ahlgren. 2001 (19) |
Gym machine training. exercise bands with arm ergometry. body perception training | + | + | ø | ø |
| Christensen. 2012 (20) |
Gym machine. barbell. and body weight training. exercise bands |
+ | + | ø | + |
| Hagberg. 2000 (21) |
Dynamic suspension training. static arm-holding exercise |
+ | + | ■ | ø |
| Hendrickson. 2010 (22) |
Gym machine and barbell training. endurance running | + | ø | ø | ■ |
| Jakobsen. 2015 (23) |
Barbell training. exercise bands | + | + | + | ø |
| Jorgensen. 2011 (24) |
Body weight training._cognitive behavioral therapy | + | ø | ø | ø |
| Kraemer. 2001 (25) |
Gym machine. barbell. and body weight train‧ing. aerobic exercises. endurance running | + | ø | ø | ± |
| Lovelady. 2009 (26) |
Training with barbells. exercise balls. and body weight. endurance running | + | ø | ø | ± |
| Rasotto. 2015 (27) |
Barbell training. exercise bands | + | + | + | ø |
| Schmitz. 2003 (28) |
Gym machine and barbell training | + | ø | ø | + |
| Sinaki. 1996 (29) |
Weight lifting and exercise bands | + | ø | ø | ø |
| Ylinen. 2003 (30) |
Training with barbells and body weight. exercise bands | + | + | + | ø |
+ Positive effects found; ± mixed effects found; ¦ no effects found; ø not investigated/reported
Details of study characteristics. interventions. methods. and outcome are given in eTable 4.
FFM. fat-free mass
eTable 4. Study characteristics (19– 30).
| Study (first author. year) | Intervention and probands | Outcome and measurement methods | Physical performance capacity | Health and wellbeing |
| Ahlgren. 2001 (19) |
n = 126 Intervention period: 10 weeks Working women with work-related pain of neck and shoulder muscles Intervention groups: (1) Strength: stationary gym machine training (2) Strength/endurance: exercise bands and arm ergometer (3) Coordination: body perception training 3 × 60 min/week supervised training during working hours (1–3) (R) 1 × 120 min/week session on coping with stress | Pain: visual analog scale Muscle strength (shoulder): dynamometer Muscle endurance/coordination: dynamometer and EMG Endurance: bicycle ergometer. spiroergometer | Significant results (p <0.05): ↑ strength shoulder flexion (all) pre-post comp. ↑ strength shoulder (1) vs. (R) ↑ strength trapezius muscle + infraspinatus muscle [(1), (3)] pre-post comp. ↑ muscle endurance (all) pre-post comp. ↑ muscle endurance (all) vs. (R) ↑ muscle coordination (part) VO2max in [(2), (3)] pre-post comp. Nonsignificant results (p ≥ 0.05): Strength shoulder elevation pre-post comp. VO2max in [(1–3)] vs. (R) | Significant results (p <0.05): ↓ pain (all) pre-post comp. |
| Christensen. 2012 (20) |
n = 98 Intervention period: 52 weeks Female healthcare workers, combined workplace and home intervention Intervention groups: (1) Strength/endurance: gym machine, barbell, and body weight training, exercise bands, endurance sport of choice, cognitive behavioral therapy, and dietetic intervention (frequency and duration of training varied) (R) 12 oral presentations on health-related topics | Anthropometry (body weight, body fat, waist and hip measurement): body analysis scales, measuring tape Blood pressure (syst./diast.): sphygmomano -meter Endurance: bicycle ergometer Muscle strength (hand, shoulder, and trunk): dynamometer Pain: questionnaire | Significant results (p <0.05): ↑ shoulder elevation right (R) + left (all) pre-post comp. ↑ shoulder abduction right + left (all) pre-post comp. ↑ trunk strength extension (1) pre-post comp. ↑ physical fitness (1) pre-post comp. Nonsignificant results (p ≥ 0.05): Shoulder elevation right (1) pre-post comp. Strength hand/trunk flexion, VO2max (all) pre-post comp. Trunk strength extension, physical fitness (R) pre-post comp. | Significant results (p <0.05): ↓ blood pressure syst. (all) + diast. (1) pre-post comp. ↓ weight, body fat, hip measurement (1) pre-post comp. ↓ pain lower back, (R) pre-post comp. ↓ pain shoulder right, (1) pre-post comp. Nonsignificant results (p ≥ 0.05): Weight, body fat, hip measurement (R) pre-post comp. Pain neck(all) shoulder left (all), upper back (all) pre-post comp. Blood pressure diast. (R) pre-post comp. |
| Hagberg. 2000 (21) |
n = 77 Intervention period: 12 weeks Female industrial workers with unspecified neck/shoulder pain Intervention groups: (1) Strength: dynamic suspension training (frequency not reported; 10 × 5 s with 2 min break after each exercise) (2) Strength/endurance: static arm-holding exercise (training 3 ×/week at home or in healthcare facility; 4 × 2 min with 2 min break after each exercise) | Pain: visual analog scale Physical demands of work: Borg scale Coordination: (shoulder): arm motion test Muscle strength (shoulder. hand strength): dynamometer. vigorimeter Muscle endurance (shoulder): Borg scale | Significant results (p <0.05): ↑ shoulder strength (all) pre-post comp. ↑ arm-shoulder movement right (all) pre-post comp. ↑ shoulder endurance (all) pre-post comp. Nonsignificant results (p ≥ 0.05): Strength hand (all) pre-post comp. Arm-shoulder movement left (all) pre-post comp. | Significant results (p <0.05): ↓ current pain shoulder (2) pre-post comp. Nonsignificant results (p ≥ 0.05): Current pain shoulder (1) pre-post comp. Occupational exertion (1) + (2) pre-post comp. |
| Hendrickson. 2010 (22) |
n = 56 Intervention period: 12 weeks, incl. 8 weeks of training Female university employees Intervention groups: (1) Aerobic/endurance: endurance running 3 × 30–50 min/week (2) Strength: gym machine and barbell training 3 × 40–63 min/week (3) Combination: both (1) and (2) (R) Continuation of normal lifestyle | Military-specific performance capacity: endurance, obstacle and load-carrying running, lifting and pulling loads Muscle strength (leg extensors, arm extensors, chest): 1-RM squat, bench press Endurance (VO2max): treadmill ergometer, spiroergometer Anthropometry (body fat and fat-free mass): dual-energy X-ray absorptiometry | Significant results (p <0.05): ↑ strength squat, bench press [(2), (3)] pre-post comp. ↑ strength squat [(2), (3)] vs. (R) ↓ running time [(1), (3)] pre-post comp. ↓ running time with load (2) vs. (R) Nonsignificant results (p ≥ 0.05): Muscle strength bench press [(1), (R)] pre-post comp. High jump, obstacle course (all) pre-post comp. Running times [(2), (R)] pre-post comp. | Nonsignificant results (p ≥ 0.05): Body fat (all) pre-post comp. Fat-free mass (all) pre-post comp. |
| Jakobsen. 2015 (23) |
n = 200 Intervention period: 10 weeks Women employed in healthcare Intervention groups: (1) Strength (work): supervised intervention at the workplace, high intensity with exercise bands and kettlebells, 5 × 10 min training + 5 × 30–45 min/participant motivational coaching (2) Strength (home): intervention during free time at home with exercise bands and written training instructions, 5 × 10 min training | Pain: visual analog scale Muscle strength (lower back musculature): ‧dynamometer Analgesic consumption: questionnaire Life and work quality (wellbeing. work satisfaction. etc.): questionnaire | Significant results (p <0.05): ↑ strength back musculature (all) pre-post comp. ↑ strength back musculature (1) vs. (2) | Significant results (p <0.05): ↓ pain intensity (all) pre-post comp. ↓ pain intensity (1) vs. (2) ↓ analgesic consumption (1) vs. (2) ↓ analgesic consumption (all) pre-post comp. ↑ wellbeing + work satisfaction (1) vs. (2) |
| Jorgensen. 2011 (24) |
n = 294 Intervention period: 12 weeks Female cleaners: supervised training and behavioral therapy in the workplace Intervention groups: (1) Strength/coordination: body weight training without gym machines (3 × 20 min/week) (2) Cognitive behavioral therapy: understanding, experience, and anticipation of motion pain (6 × 120 min sessions) (R) Continuation of normal lifestyle | Muscle strength (trunk. shoulder): dynamometer Balance: measuring platform Kinesiophobia: Tampa Scale of Kinesiophobia questionnaire | Significant results (p <0.05): ↑ strength trunk flexion (1) pre-post comp. ↑ strength trunk flexion (1) vs. [(1). (2)] Nonsignificant results (p ≥ 0.05): Strength trunk extension. shoulder (abduction and elevation) [(1); (2). (R)] pre-post comp. | Significant results (p <0.05): ↓ kinesiophobia (2) vs. [(1). (R)] ↑ positional balance (1) vs. (2) Nonsignificant results (p ≥ 0.05): Postural balance (1) vs. (R) |
| Kraemer. 2001 (25) |
n = 93 Intervention period: 24 weeks Untrained young women (+ 100 untrained men as basic control group without intervention) Intervention groups: (1) Strength: total body/strength (supervised training 3 ×/week, duration ns) (2) Strength: total body/hypertrophy (supervised training 3 ×/week, duration ns) (3) Strength: upper body/strength (supervised training 3 ×/week, duration ns) (4) Strength: upper body/hypertrophy (supervised training 3 ×/week, duration ns) (5) Power (no gym machines): plyometrics, exercises with and without partner (supervised training 3 ×/week, duration ns) (6) Aerobic/endurance: running, bicycle ergometer, and stepper exercises (supervised training 3 ×/week, duration ns) | Muscle strength (leg. back. chest. arms): 1-RM various exercises Power (squat jump. bench throw): Smith machine Strength endurance (squat): max. repetitions Anthropometry (body fat and fat-free mass): calipometry | Significant results (p <0.05): ↑ strength squat [(1),(2),(5)] pre-post comp. ↑ strength bench press [(1–5)] pre-post comp. ↑ strength repetitive deadlift (1) pre-post comp. ↑ power squat jump [(1),(2),(5)] pre-post comp. ↑ power bench throw [(1–5)] pre-post comp. ↑ strength endurance squat [(1–5)] pre-post comp. Nonsignificant results (p ≥ 0.05): Strength squat [(3), (4), (6)] pre-post comp. Strength bench press (6) pre-post comp. Strength repetitive deadlift [(2–6)] pre-post comp. Power bench press (6) pre-post comp. Strength endurance squat (6) pre-post comp | Significant results (p <0.05): ↑ fat-free mass [(1). (5)] pre-post comp. ↑ body weight (1) pre-post comp. Nonsignificant results (p ≥ 0.05): Fat-free mass [(2–6)] pre-post comp. Body weight [(2–6)] pre-post comp. |
| Lovelady. 2009 (26) |
n = 20 Intervention period: 16 weeks Breastfeeding mothers Intervention groups: (1) Strength/endurance: strength training with barbells, exercise balls, and body weight (with out gym machines) 3 × variable duration/week and endurance running 3 × 15–45 min/week; strength and endurance on alternating days (R) Continuation of normal lifestyle | Bone mineral density: dual-energy X-ray absorptiometry Anthropometry (height, weight, body fat, and fat-free mass): stadiometer, beam balance, dual-energy X-ray absorptiometry Muscle strength (various muscle groups): 1-RM for 10 different exercises Endurance: treadmill ergometer | Significant results (p <0.05): ↑ strength all exercises (1) vs. (R) ↑ strength squat. deadlift (1) pre-post comp. ↑ calc. VO2max increase. relative (1) pre-post comp. Nonsignificant results (p ≥ 0.05): Calc. r VO2max increase. absolute (all) | Significant results (p <0.05): ↓ LS bone mineral density (1) vs. (R) ↓ body fat (1) pre-post comp. ↓ body weight (1) pre-post comp. ↓ fat-free mass (1) pre-post comp. Nonsignificant results (p ≥ 0.05): Bone mineral density hip + total body (1) vs. (R) |
| Rasotto. 2015 (27) |
n = 60 Intervention period: 24 weeks Female workers performing repetitive fine manual tasks: supervised training in the workplace Intervention groups: (1) Strength: variable intensity with exercise bands and barbells 2 × 30 min/week (R) Continuation of normal lifestyle | Pain: visual analog scale Physical disability: DASH and NPDS-I questionnaires Muscle strength (hand): dynamometer Flexibility: goniometer | Significant results (p <0.05): ↑ strength hand (1) vs. (R) | Significant results (p <0.05): ↓ pain shoulder (1) vs. (R) ↓ pain shoulder (1) pre-post comp. ↓ physical disability (1) vs. (R) ↑ range of motion (1) vs. (R) ↑ shoulder flexibility (1) vs. (R) ↑ lateral flexion head (1) vs. (R) ↑ CS/head rotation (1) vs. (R) |
| Schmitz. 2003 (28) |
n = 60 Intervention period: 39 weeks, comprising 15 weeks of supervised training + 24 weeks of unsupervised training Female university employees Intervention groups: (1) Strength: gym machine and barbell training 2 × 50 min/week (R) Continuation of normal lifestyle | Anthropometry (body fat and fat-free mass): dual-energy X-ray absorptiometry Physical activity: TWPAS questionnaire Muscle strength (legs. arms. shoulders. trunk): 1-RM | Significant results (p <0.05): ↑ strength (1) vs. (R) ↑ strength (1) pre-post comp. ↑ calc. VO2max increase. relative (all) | Significant results (p <0.05): ↓ body fat (1) vs. (R) ↑ fat-free mass (1) vs. (R) |
| Sinaki. 1996 (29) |
n = 96 Intervention period: 36 months Premenopausal women with no regular sporting activity. 1/3 of TS under supervision Intervention groups: (1) Strength: Weight lifting and exercise bands 3 × 30 min/week (R) Continuation of normal lifestyle | Muscle strength (back. trunk. hand): dynamometer Bone mineral density: dual-energy X-ray absorptiometry Endurance: treadmill ergometer. spiroergometer | Significant results (p <0.05): ↑ strength shoulder, trunk extension, hand (1) pre-post comp. ↑ strength shoulder abduction/extension (1) vs. (R) ↑ endurance (all) pre-post comp. Nonsignificant results (p ≥ 0.05): Strength trunk and hip after 36 months (1) pre-post comp. Strength hip, trunk (1) vs. (R) Endurance (1) vs. (R) | Nonsignificant results (p ≥ 0.05): Bone mineral density (all) |
| Ylinen. 2003 (30) |
n = 180 Intervention period: 12 months Female office workers with chronic nonspecific neck pain, supervised or unsupervised training (free choice; jointly evaluated) Intervention groups: (1) Strength: Barbell training and exercise bands 3–5 x 45 min/week, aerobic exercises 3 × 30 min/week (2) Endurance: Body weight and light barbell training 3–5 × 45 min/week, aerobic exercises 3 × 30 min/week (R) Stretching exercises 3 × 20 min/week and aerobic exercises 3 × 30 min/week | Pain: visual analog scale Physical disability: mNPDS und VNDI Movement (neck): range of motion Muscle strength (neck. hand): dynamometer Endurance: bicycle ergometer. spiroergometer Mood: (short depression inventory score) | Significant results (p <0.05): ↑ strength neck flexion/rotation/extension (1) vs. [(2). (R)] Nonsignificant results (p ≥ 0.05): VO2max (all) | Significant results (p <0.05): ↓ pain neck [(1). (2)] vs. (R) ↓ disability (1). (2) vs. (R) ↑ range of motion (1) vs. (R) ↑ rotation (2) vs. (R) ↑ rotation [(1). (2)] pre-post comp. Nonsignificant results (p ≥ 0.05): Strength hand (all) pre-post comp. |
n, total number of study participants; (R), reference group; (1), (2), etc., intervention group number; [ ], each of the groups in brackets; vs, group to right of vs was tested against group(s) to left; diast., diastolic; EMG, electromyography; CS, cervical spine; calc., calculated; calc. r., calculated relative; LS, lumbar spine; max., maximal; ns, not specified; 1-RM, one-repetition maximum; pre-post comp., before and after comparison; syst., systolic; TS, training session; VO2max, maximal oxygen uptake; DASH, disabilities of the arm, shoulder and hand; NPDS-I: neck pain and disability scale index; mNPDS, modified neck pain and disability scale; TWPAS: typical weekly physical activity survey; VNDI: Vernon neck disability index; ↑ increase; ↓ decrease
With regard to evaluation of the results, it should be noted that the studies varied considerably both in the composition of their collectives and in the interventions used. The intervention periods ranged from 8 weeks to 3 years, and the training sessions differed widely not only in content but also in intensity, scale, duration, and frequency. In almost all studies the intervention comprised elements of strength, endurance, and agility training.
Effects of intervention on strength and physical performance capacity
Despite the pronounced heterogeneity, improvement of physical performance capacity was observed in all studies. The training led not only to increased strength but frequently to enhancement of other motor functions. Muscular endurance, coordination/agility, and endurance increased in dependence on the focus of the intervention (etable 4) (21, 22, 25, 29, 30).
Combinations of strength and endurance elements also brought about significant increases in strength. Ylinen et al. divided female office workers with chronic unspecific neck pain into three different groups (two training groups and a control group). In the control group, with three sessions per week of 20 min stretching exercises and 30 min aerobic exercises, the neck musculature became 7 to 10% stronger. In the endurance training group, featuring three 30-min sessions of aerobics each week plus three to five 45-min periods of light training with and without barbells, the improvement was 16 to 29%. The greatest increases in neck flexion, neck rotation, and neck extension strength—110%, 76%, and 69% respectively—were seen in the strength training group whose weekly schedule comprised three to five 45-min sessions of intensive weight training and work with exercise bands together with three 30-min periods of aerobic training (30). At the end of the 12-month intervention the increase in strength differed significantly among the three groups (p <0.001).
Hendrickson et al. also found considerable enhancement of performance following combined resistance and endurance training. Eight weeks of training in young female amateur athletes achieved improvement of 13.1% in load carriage for 3.2 km (p <0.05, g ˜ -0.91; pre-training: 34.9 ± 5.6 min; post-training: 30.2 ± 4.3 min) and 33.8% in repetitive lift and carry (p <0.05, g ˜ 1.47; pre-training: 30.8 ± 7.6; post-training: 41.2 ± 5.9). The figure of 33.8% was calculated from the mean values, because the source was inconsistent in this respect, stating 45.5% in the abstract and 35.7% in the figure (22).
Kraemer et al. carried out a 6-month program of training in a group of previously untrained young women. The participants were divided into six different intervention groups: a pure endurance group and a rapid strength group were accompanied by four strength groups in which either upper-body or total-body training aimed to increase either maximum strength or explosive exercise capacity. At the end of the training period all groups evinced enhanced performance as measured by repetitive lifting of a box weighing 20.45 kg. Only the endurance group showed no improvement in other strength-dependent tasks (25).
Effects of intervention on health and wellbeing
The interventions also affected the health-related categories of musculoskeletal pain, subjective wellbeing, body weight, body fat, and bone mineral density.
Pain and subjective wellbeing: The effects of the interventions on pain were tested in six studies. In every case, significant decreases in pain were observed over time and in comparison with control groups. Broadly independent of the precise training plan, regular exercise lowered the pain level.
Ahlgren et al. investigated the effects of various training interventions in 102 women with work-related pain in their neck and shoulder muscles. Compared with the control intervention, a weekly session of tuition in coping with stress, all variants of a 10-week exercise program (three 60-min sessions per week) reduced pain levels (p <0.05, pain at present g = 0.43, pain in general g = 0.61). With regard to the decrease in pain at worst, strength training showed a considerable effect (p <0.05, g ˜ 0.83) and was the only intervention (endurance training: p < 0.05, g ˜ 0.57; coordination training: p < 0.05, g ˜ 0.56) to differ from control (p <0.05) (19).
Four studies reported the effects of training on associated subjective factors such as wellbeing, exercise motivation, and work satisfaction. Largely independent of the composition of the collective and the training methods, these factors were enhanced. In their study of 200 female healthcare professionals, Jakobsen et al. found that interventions in the workplace were more likely than interventions at home to result in positive changes with regard to wellbeing, work satisfaction, and the desire to exercise (p <0.0001) (23).
Body composition: Two of the 12 studies reported on weight reduction and obesity prevention. Three further studies additionally measured body weight and fat-free mass (table 2). Schmitz et al. investigated to what extent fat-free mass and weight could be modified in female midlife university staff by a program of two weekly 50-min sessions of training with gym machines and barbells. In the first 15 weeks, during which each session was supervised by a trainer, body fat decreased (-1.7 ± 0.6%, p = 0.005) and fat-free mass increased (+1.0 ± 0.3 kg, p = 0.006) compared with the control group. For the next 6 months the participants continued the same training without supervision. The changes in body composition persisted to the end of the study period (28).
Christensen et al. studied the effects of a combination of strength training (1 h/week), cognitive behavioral training, and dietary modification in overweight female healthcare professionals. After a year, the intervention group had an average weight loss of ˜ 6 kg (p <0.0001, g ˜ 0.36; baseline: 84.2 ± 15.9 kg, 12 months: 78.4 ± 15.8 kg) and average reduction in body fat of ca. 3 percentage points (p <0.0001, g ˜ 0.42; baseline: 41.2 ± 5.7%, 12 months: 38.4 ± 7.3%). The members of the control group attended 12 two-hour oral presentations on health-related topics; they showed no changes in body composition (20).
Two studies investigated the consequences of strength training for bone structure. Sinaki et al. observed no significant effect of a 3-year program of strength training (3 × 30 min/week) on bone mineral density in healthy women between 30 and 40 years of age (29). In breastfeeding women, combined strength and endurance training (3 × 15–45 min/week) failed to prevent a decrease in bone mineral density (26). In comparison with the control group, however, there was a slightly lower reduction in density in the lumbar spine (p <0.01; -4.8%, g ˜ 0.38 versus -7.0%, g ˜ 0.60). No significant differences were seen in total-body values or in the hip.
Discussion
Given that insufficient muscle strength may facilitate biomechanical stress, injuries, and chronic impairment of health and thus cause considerable additional costs both for employers and for the healthcare system, it is astounding that our systematic survey of the medical literature identified only 12 publications. While these studies report the results of training interventions, the data do not indicate whether and to what extent women’s muscle strength influences their health in daily life.
In addition to the small number of publications, a number of other limitations are apparent. The studies selected for inclusion differed, in some cases widely, with regard to the collective investigated and the interventions carried out. The intervention period varied in duration from 8 weeks to 3 years. The training programs also differed substantially in terms of normative standards, i.e., intensity of training stimuli, frequency of sessions, and amount of training. In at least three studies (20, 24, 27) the training schedule did not even meet the minimum standards of the World Health Organization (WHO) for strength-promoting exercise to prevent ill health (two sessions per week adding up to 75 min) (31).
Furthermore, the measurement of the dependent variables varied considerably: four studies used one-repetition maximum (1-RM), while eight employed dynamometric measurement of strength. 1-RM describes the greatest weight that can be lifted or moved only once. Subjective estimates were quantified by various means. Only the visual analog scale for pain was used in all 12 studies.
Moreover, hardly any of the studies report effect sizes or test statistics to permit assessment of the practical relevance of individual findings. Detailed examination of bias (eTable 3) clearly shows variation in study quality, to the extent that the internal validity of some particular findings is questionable. This, together with the heterogeneity of the studies, meant that no efficacy limit for strength training could be established and no realistic funnel plot could be created to evaluate publication bias. At least with regard to the health-related results, the individual primary studies have no reliable generalizability (external validity).
Despite the considerable differences among the studies, it is astonishing that in all of them the strength-promoting interventions led to significant increases in strength, regardless of collective, muscle group, and nature, duration, and intensity of training stimulus. This was observed in pre-/postintervention comparisons and in comparisons with inactive control groups.
The need for effective strength-promoting interventions is plain. Repetitive overloading inevitably causes damage, potentially leading to reduced working capacity and risking acute injury with chronic health consequences. It therefore comes as no surprise that the prevalence of musculoskeletal symptoms among emergency rescue personnel rises from ˜ 22% to ˜ 43% over a 10-year period (from the 5th to the 14th year of service) and continues to grow thereafter (e15).
The potential disparity between the required workload and the individual physical strain is clearly illustrated by the case of manual patient transport. Lifting a 75-kg person involves repetitive peak forces of over 350 N at the grip of the stretcher (3). Maximal grip strength is a crucial performance-limiting factor for this work (32– 34). A study of over 500 healthy women aged 20 to 25 years found that their mean maximal grip strength was 329 ± 57 N (35). Therefore, more than 50% of these women would not be strong enough to transport the patient in the example above. These types of demands on the musculoskeletal system mean that women working in the care and health sectors run an elevated risk of health impairment (4).
Summary
Our systematic analysis of the relevant literature indicates that even slight to moderate amounts of exercise can increase women’s strength significantly in just a few months. Both women challenged by the biomechanical stresses of their professions and those with predominantly sedentary occupations benefit from regular functional strength training. Some of the interventions had other effects on health and wellbeing. Both the positive effects on musculoskeletal pain and the effects on body composition and wellbeing could represent unspecific reactions to regular exercise. Such effects have been reported in a number of review articles (36– 39).
This response to the interventions points up the high potential for health-promoting activities in the workplace. The fact that no studies investigating the influence of muscle strength on women’s health in everyday work life could be found, and only a small number on the health-related consequences of strength training, highlights the urgent need for solid primary data. The existing data do not enable determination of efficacy limits for strength training; only general training recommendations can be made.
THE CLINICAL PERSPECTIVE.
This systematic review of muscle strength and strength training shows that physically inactive women benefit from even small amounts of low-intensity training in two ways: their physical performance capacity increases (performance aspect) and musculoskeletal symptoms decrease (health aspect). These proven benefits can help physicians to motivate women to take an interest in an active, health-enhancing lifestyle.
Moreover, the recently enacted new German law on health promotion and prophylaxis (referred to as the Prevention Act) facilitates promotion of strength, coordination, and agility: since 2017 it has been possible to prescribe certified prevention courses (e18). Courses appropriate to the individual patient’s occupational exposure and symptoms can be offered: Pilates, yoga, and gym machine training are among the many options. An up-to-date catalog of the range of courses available locally and other relevant information helps patients to find a suitable program. This introduction to training often makes it easier for them to join a sports or rehabilitation club, train regularly, and ultimately achieve a long-term transformation of their habitual behavior.
Every patient—particularly those with pre-existing health-related risk factors or illness—should be examined by a specialist in sports medicine before commencement of training (e19).
Key Messages.
The health consequences of strength training for women have been investigated in only 12 studies with heterogeneous study groups and widely differing interventions. No studies at all on the influence of muscle strength on women’s health in everyday work life could be found.
Strength-promoting interventions led to significant increases in strength, regardless of the muscle group and the nature, duration, and intensity of the training stimulus.
In all six of the studies in which the effect of training on pain was investigated, pain decreased significantly.
The effects on health and wellbeing described in some studies cannot (yet) be generalized owing to methodological limitations.
Based on the current state of knowledge, no efficacy limits for strength training can be determined; only general training recommendations can be made.
eTable 1. Complete search strategy.
| Step | Link | Search term(s) |
| 1 | female, woman, women | |
| 2 | AND | adult |
| 3 | NOT | child, children |
| 4 | AND | force, strength |
| 5 | AND | prevention, training, health |
| 6 | AND | job, workplace, desk work, occupation, household, nursing, construction, craftsman, police, military, firefighter |
The search terms separated by commas were OR items. A supplementary search without step 3 identified no further studies that met the selection criteria
Acknowledgments
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Leyk D, Rüther T, Wunderlich M, et al. Sporting activity, prevalence of overweight, and risk factors: cross-sectional study of more than 12 500 participants aged 16 to 25 years. Dtsch Arztebl Int. 2008;105:793–800. doi: 10.3238/arztebl.2008.0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev. 2012;13:659–680. doi: 10.1111/j.1467-789X.2011.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leyk D, Rohde U, Erley OM, et al. Maximal manual stretcher carriage: performance and recovery of male and female ambulance workers. Ergonomics. 2007;50:752–762. doi: 10.1080/00140130701195063. [DOI] [PubMed] [Google Scholar]
- 4.BMAS (ed.) Bundesministerium für Arbeit und Soziales. Bonn: 2006. Merkblatt zu der Berufskrankheit Nr 2108 der Anlage zur Berufskrankheiten-Verordnung (BKV): „Bandscheibenbedingte Erkrankungen der Lendenwirbelsäule durch langjähriges Heben oder Tragen schwerer Lasten oder durch langjährige Tätigkeiten in extremer Rumpfbeugehaltung, die zur Unterlassung aller Tätigkeiten gezwungen haben, die für die Entstehung, die Verschlimmerung oder das Wiederaufleben der Krankheit ursächlich waren oder sein können“. [Google Scholar]
- 5.Thiede M, Liebers F, Seidler A, Gravemeyer S, Latza U. Gender specific analysis of occupational diseases of the low back caused by carrying, lifting or extreme trunk flexion—use of a prevention index to identify occupations with high prevention needs. Am J Ind Med. 2014;57:233–244. doi: 10.1002/ajim.22277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eltayeb S, Staal JB, Hassan A, de Bie RA. Work related risk factors for neck, shoulder and arms complaints: a cohort study among Dutch computer office workers. J Occup Rehabil. 2009;19:315–322. doi: 10.1007/s10926-009-9196-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grobe T, Steinmann S. Techniker Krankenkasse. Hamburg: 2016. Gesundheitsreport 2016 - Veröffentlichungen zum betrieblichen Gesundheitsmanagement der TK Schwerpunkt: Gesundheit zwischen Beruf und Familie. [Google Scholar]
- 8.DeStatis (ed.) Statistsches Bundesamt. Wiesbaden: 2014. Mikrozensus-Fragen zur Gesundheit 2013: Körpermaße der Bevölkerung. [Google Scholar]
- 9.Schmidtke H, editor. Handbuch der Ergonomie. Koblenz: Bundesamt für Wehrtechnik und Beschaffung. 1999 [Google Scholar]
- 10.Janssen I, Heymsfield SB, Wang ZM, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18-88 yr. J Appl Physiol. 2000;89:81–88. doi: 10.1152/jappl.2000.89.1.81. [DOI] [PubMed] [Google Scholar]
- 11.Miller GA, MacDougall JD, Tarnopolsky MA, Sale DG. Gender differences in strength and muscle fiber characteristics. Eur J Appl Physiol. 1993;66:254–262. doi: 10.1007/BF00235103. [DOI] [PubMed] [Google Scholar]
- 12.Fink WJ, Costill DL, Pollock ML. Submaximal and maximal working capacity of elite distance runners Part II muscle fiber composition and enzyme activities. Ann New York Acad Sci. 1977;301:323–327. doi: 10.1111/j.1749-6632.1977.tb38210.x. [DOI] [PubMed] [Google Scholar]
- 13.Leyk D, Rohde U, Mödl A, Harbaum T, Schoeps S, Franke E. Körperliche Leistungsfähigkeit und Belastbarkeit von Soldatinnen: Ein Kraft-Last-Dilemma. Wehrmed Mschr. 2015;59:2–7. [Google Scholar]
- 14.Kenney WL, Wilmore JH. Physiology of sport and exercise. Champaign: Human Kinetics. (6) 2015 [Google Scholar]
- 15.Falkel JE, Sawka MN, Levine L, Pandolf KB. Upper to lower body muscular strength and endurance ratios for womes and men. Ergonomics. 1985;28:1661–1670. doi: 10.1080/00140138508963302. [DOI] [PubMed] [Google Scholar]
- 16.Laubach LL. Comparative muscular strength of men and women: a review of the literature. Aviat Space Environ Med. 1976;47:534–542. [PubMed] [Google Scholar]
- 17.Kraemer WJ, Fleck SJ, Deschenes MR. Lippincott Williams & Wilkins. Baltimore,: Philadelphia; 2012. Exercise physiology Integrating theory and application. [Google Scholar]
- 18.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Sys Rev. 2015;4:1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahlgren C, Waling K, Kadi F, Djupsjöbacka M, Thornell LE, Sundelin G. Effects on physical performance and pain from three dynamic training programs for women with work-related trapezius myalgia. J Rehabil Med. 2001;33:162–169. [PubMed] [Google Scholar]
- 20.Christensen JR, Overgaard K, Carneiro IG, Holtermann A, Sogaard K. Weight loss among female health care workers—a 1-year workplace based randomized controlled trial in the FINALE-health study. BMC Publ Health. 2012;12:1–10. doi: 10.1186/1471-2458-12-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagberg M, Harms-Ringdahl K, Nisell R, Hjelm EW. Rehabilitation of neck-shoulder pain in women industrial workers: a randomized trial comparing isometric shoulder endurance training with isometric shoulder strength training. Arch Phys Med Rehabil. 2000;81:1051–1058. doi: 10.1053/apmr.2000.7582. [DOI] [PubMed] [Google Scholar]
- 22.Hendrickson NR, Sharp MA, Alemany JA, et al. Combined resistance and endurance training improves physical capacity and performance on tactical occupational tasks. Eur J Appl Physiol. 2010;109:1197–1208. doi: 10.1007/s00421-010-1462-2. [DOI] [PubMed] [Google Scholar]
- 23.Jakobsen MD, Sundstrup E, Brandt M, Jay K, Aagaard P, Andersen LL. Effect of workplace—versus home-based physical exercise on musculoskeletal pain among healthcare workers: a cluster randomized controlled trial. Scand J Work Environ Health. 2015;41:153–163. doi: 10.5271/sjweh.3479. [DOI] [PubMed] [Google Scholar]
- 24.Jorgensen MB, Ektor-Andersen J, Sjogaard G, Holtermann A, Sogaard K. A randomised controlled trial among cleaners—effects on strength, balance and kinesiophobia. BMC Publ Health. 2011;11:1–10. doi: 10.1186/1471-2458-11-776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kraemer WJ, Mazzetti SA, Nindl BC, et al. Effect of resistance training on women‘s strength/power and occupational performances. Med Sci Sports Exerc. 2001;33:1011–1025. doi: 10.1097/00005768-200106000-00022. [DOI] [PubMed] [Google Scholar]
- 26.Lovelady CA, Bopp MJ, Colleran HL, Mackie HK, Wideman L. Effect of exercise training on loss of bone mineral density during lactation. Med Sci Sports Exerc. 2009;41:1902–1907. doi: 10.1249/MSS.0b013e3181a5a68b. [DOI] [PubMed] [Google Scholar]
- 27.Rasotto C, Bergamin M, Sieverdes JC, et al. A tailored workplace exercise program for women at risk for neck and upper limb musculoskeletal disorders: a randomized controlled trial. J Occup Environ Med. 2015;57:178–183. doi: 10.1097/JOM.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 28.Schmitz KH, Jensen MD, Kugler KC, Jeffery RW, Leon AS. Strength training for obesity prevention in midlife women. Int J Obes Relat Metab Disord. 2003;27:326–333. doi: 10.1038/sj.ijo.0802198. [DOI] [PubMed] [Google Scholar]
- 29.Sinaki M, Wahner HW, Bergstralh EJ, et al. Three-year controlled, randomized trial of the effect of dose-specified loading and strengthening exercises on bone mineral density of spine and femur in nonathletic, physically active women. Bone. 1996;19:233–244. doi: 10.1016/8756-3282(96)00174-3. [DOI] [PubMed] [Google Scholar]
- 30.Ylinen J, Takala EP, Nykanen M, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA. 2003;289:2509–2516. doi: 10.1001/jama.289.19.2509. [DOI] [PubMed] [Google Scholar]
- 31.World Health Organization (ed.) WHO Press. Geneva: 2010. Global recommendations on physical activity for health. [PubMed] [Google Scholar]
- 32.von Restorff W. Physical fitness of young women: carrying simulated patients. Ergonomics. 2000;43:728–743. doi: 10.1080/001401300404706. [DOI] [PubMed] [Google Scholar]
- 33.Knapik JJ, Harper W, Crowell HP. Physiological factors in stretcher carriage performance. Eur J Appl Physiol. 1999;79:409–413. doi: 10.1007/s004210050530. [DOI] [PubMed] [Google Scholar]
- 34.Steiber N. Strong or weak handgrip? Normative reference values for the German population across the life course stratified by sex, age, and body height. PLoS One. 2016;11 doi: 10.1371/journal.pone.0163917. e0163917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leyk D, Gorges W, Ridder D, et al. Hand-grip strength of young men, women and highly trained female athletes. Eur J Appl Physiol. 2007;99:415–421. doi: 10.1007/s00421-006-0351-1. [DOI] [PubMed] [Google Scholar]
- 36.Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med. 2003;13:106–117. doi: 10.1097/00042752-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 37.Lowe BD, Dick RB. Workplace exercise for control of occupational neck/shoulder disorders: a review of prospective studies. Environ Health Insights. 2014;8:75–95. doi: 10.4137/EHI.S15256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada‘s Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act. 2010;7:1–220. doi: 10.1186/1479-5868-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2008;15:239–246. doi: 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- E1.Hofmeister M. Hippokrates gibt Präventionstipps mit zeitloser Gültigkeit. die BG. 2006;121:84–89. [Google Scholar]
- E2.Cordain L, Gotshall RW, Eaton SB, Eaton SB. III.: Physical activity, energy expenditure and fitness: an evolutionary perspective. Int J Sports Med. 1998;19:328–335. doi: 10.1055/s-2007-971926. [DOI] [PubMed] [Google Scholar]
- E3.Statista. Mediennutzung in Deutschland - Statista Dossier. de.statista.com/statistik/studie/id/3177/dokument/mediennutzung-statista-dossier (last accessed on 13 January 2017) [Google Scholar]
- E4.Eßfeld D. BMVg. Bonn: 2007. Entwicklung einsatznaher Leistungstests und Prüfverfahren (Abschlussbericht zum Verbundprojekt M/SAB1/3/A011) [Google Scholar]
- E5.Destatis (ed.) Statistisches Bundesamt. Wiesbaden: 2016. Gesundheit: Personal 2014. [Google Scholar]
- E6.Liersch A. Arbeitsunfälle und arbeitsbedingte Gesundheitsprobleme Ergebnisse einer Zusatzerhebung im Rahmen des Mikrozensus 2013. In: Statistisches Bundesamt (Destatis) Wirtschaft und Statistik, editor. Destatis. Wiesbaden: 2014. pp. 561–575. [Google Scholar]
- E7.Pompeii LA, Lipscomb HJ, Dement JM. Surveillance of musculoskeletal injuries and disorders in a diverse cohort of workers at a tertiary care medical center. Am J Ind Med. 2008;51:344–356. doi: 10.1002/ajim.20572. [DOI] [PubMed] [Google Scholar]
- E8.Destatis. Körpermaße nach Altersgruppen und Geschlecht. www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Gesundheit/GesundheitszustandRelevantesVerhalten/Tabellen/Koerpermasse.html (last accessed on 13 January 2017) [Google Scholar]
- E9.National Institute for Health Research. PROSPERO - International prospective register of systematic reviews. www.crd.york.ac.uk/PROSPERO (last accessed on 13 January 2017) [Google Scholar]
- E10.Schmucker C, Nothacker M, Rücker G, Muche-Borowski C, Kopp I, Meerpohl JJ. Bewertung des Biasrisikos (Risiko systematischer Fehler) in klinischen Studien: Ein Manual für die Leitlinienerstellung Version 1.0 vom 4. 5. 2016. www.cochrane.de/de/rob-manual (last accessed on 13 January 2017) [Google Scholar]
- E11.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 51.0. www.handbook.cochrane.org (last accessed on 13 January 2017) [Google Scholar]
- E12.AWMF online. Leitlinie Struktur des AWMF-Regelwerks-Ablaufschema. www.awmf.org/leitlinien/awmf-regelwerk/ll-entwicklung.html (last accessed on 13 January 2017) [Google Scholar]
- E13.The R Core Team (ed.) R Foundation for Statistical Computing. Wien: 2016. A language and environment for statistical computing. [Google Scholar]
- E14.Cohen J. Taylor and Francis. Hoboken: 2013. Statistical power analysis for the behavioral sciences 2nd ed. [Google Scholar]
- E15.Gebhardt H, Klussmann A, Massbeck P, Topp S, Steinberg U. Wissenschaftsverlag N. W. Verlag für neue Wissenschaft. Dortmund: 2006. Sicherheit und Gesundheit im Rettungsdienst. [Google Scholar]
- E16.Christensen JR, Faber A, Ekner D, Overgaard K, Holtermann A, Sogaard K. Diet, physical exercise and cognitive behavioral training as a combined workplace based intervention to reduce body weight and increase physical capacity in health care workers—a randomized controlled trial. BMC Public Health. 2011;11 doi: 10.1186/1471-2458-11-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Holtermann A, Jorgensen MB, Gram B, et al. Worksite interventions for preventing physical deterioration among employees in job-groups with high physical work demands: background, design and conceptual model of FINALE. BMC Publ Health. 2010;10:1–12. doi: 10.1186/1471-2458-10-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Beerheide R. Ärzte können ab 2017 Präventionskurse verordnen Deutsch Arztebl 2016. www.aerzteblatt.de/nachrichten/69688/Aerzte-koennen-ab-2017-Praeventionskurseverordnen (last accessed on 29 March 2017) [Google Scholar]
- E19.Deutsche Gesellschaft für Sportmedizin und Prävention. S1- Leitlinie Vorsorgeuntersuchung im Sport. www.dgsp.de/seite/278046/antragsformular.html (last accessed on 29 March 2017) [Google Scholar]