Abstract
Background
Methamphetamine is considered more dangerous than other stimulants because of its acute complications, long-term neurotoxicity, and potential for drug dependence. Until now, there have been no evidence-based guidelines for the treatment of methamphetamine-related disorders, either in Germany or abroad.
Methods
A systematic literature search was performed on the treatment of methamphetamine-related disorders. Based on this literature review, a multidisciplinary expert panel developed recommendations using the nominal group technique.
Results
The evidence base for the treatment of methamphetamine-related disorders is sparse. The efficacy of psychotherapeutic techniques such as cognitive behavioral therapy and contingency management and the efficacy of complex, disorder-specific treatment programs have been proven in randomized controlled trials, but it remains unclear which method is best. Persons carrying a diagnosis of substance abuse should be offered psychotherapy. Structured exercise programs, whether self-directed or professionally led, can improve addiction-specific endpoints as well as comorbid disorders and should, therefore, be offered as well. Pharmacotherapy has shown little to no effect in relatively low-quality clinical trials with low case numbers and high dropout rates, and therefore only a few weak recommendations were made. These include tranquilizers for the short-term treatment of agitation and atypical antipsychotics if necessary. Attempts to substitute other substances, such as methylphenidate or dexamphetamine, for methamphetamine have not yielded any robust evidence to date. Sertraline should not be administered due to serious adverse events.
Conclusion
Many of the recommendations in the guideline are made with a weak grade of recommendation because of the poor evidence base and the modest size of the reported therapeutic effects. In acute situations, symptom-oriented treatment is recommended. Psychotherapy and exercise should be offered as well.
Physicians and staff working in hospitals, private medical practices, and addiction treatment centers are now increasingly confronted with abuse of methamphetamine (“meth,” “crystal meth”). In Germany, the problem is at its most severe in certain areas of Saxony, Thuringia, and Bavaria that are near the Czech border. Methamphetamine abuse also seems to be prevalent in particular circles, e.g., MSM (men who have sex with men). So-called “chem-sex,” i.e., sexual intercourse under the influence of drugs, is associated with intravenous use of the drug, which carries greater risks than oral use (1). Methamphetamine is more dangerous than other stimulants because of its acute complications, long-term neurotoxicity, and potential for drug dependence. The treatment of methamphetamine-related disorders is challenging for the multidisciplinary drug help facilities as well as for first-aid deliverers and hospital staff. Support is needed, especially because the German and foreign guidelines on treatment for drug abuse do not deal with methamphetamine specifically and are also largely out of date (2).
This S3 guideline was developed by an expert panel between April 2015 and September 2016, according to the criteria established by the Association of Scientific Medical Societies in Germany (Arbeitsgemeinschaft der wissenschaftlichen medizinischen Fachgesellschaften, AWMF), on the initiative of the German Federal Drug Commissioner and on behalf of the German Medical Association, with funding from the Federal Ministry of Health. Methodological assistance was provided by the German Agency for Quality in Medicine (Ärztliche Zentrum für Qualität in der Medizin). The 21 participating experts included physicians from inpatient and outpatient care settings in multiple specialties, psychotherapists, caregivers, social workers, and representatives of patient self-help groups (eTables 1 and 2). Further experts were consulted on specific questions.
eTable 1. Members of the consensus group.
| Participating individuals | Specialty society or organization represented |
|
Dr. med. Wolf-Dietrich Braunwarth Klinikum Nürnberg [Nuremberg] |
Not representing any society or organization |
|
Dr. med. Roland Härtel-Petri Practice of psychotherapy, Bayreuth |
Not representing any society or organization |
|
Dr. med. Heribert Fleischmann Bezirksklinikum Wöllershof |
German Center for Questions of Addiction (Deutsche Hauptstelle für Suchtfragen e. V., DHS) |
|
Prof. Dr. med. Euphrosyne Gouzoulis-Mayfrank Landschaftsverband Rheinland (LVR)-Klinik Köln [Cologne] |
German Society for Psychiatry, Psychotherapy and Neuropsychiatry (Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde, DGPPN) |
|
Dr. med. Willem Hamdorf Allgemeine Hospitalgesellschaft (AHG) Klinik Mecklenburg |
Professional Association for Addiction (Fachverband Sucht, FVS) |
|
Prof. Dr. Ursula Havemann-Reinecke University Medical Center Göttingen |
German Society for Addiction Research and Treatment (Deutsche Gesellschaft für Suchtforschung und Suchttherapie e. V., DG Sucht) |
|
Dipl.-Med. Peter Jeschke Group neurological practice, Halle |
Not representing any society or organization |
|
Dr. med. Josef Mischo Kreiskrankenhaus St. Ingbert |
Working Group on Drugs and Addiction of the German Medical Association (Arbeitsgruppe „Sucht und Drogen“ der Bundesärztekammer, BÄK) |
|
Prof. Dr. med. Bernd Mühlbauer Institute of Clinical Pharmacology, Klinikum Bremen Mitte; Bremen Hospital Group |
Drug Commission of the German Medical Association (Arzneimittelkommission der deutschen Ärzteschaft, AkdÄ) |
|
Prof. Dr. Stephan phil. Mühlig Technische Universität Chemnitz Timo Harfst German Psychotherapists’ Association |
German Psychotherapists’ Association (Bundespsychotherapeutenkammer, BPtK) |
|
PD Dr. med. Ingo Schäfer Centre of Interdisciplinary Addiction Research (ZIS) of the University of Hamburg Sascha Milin Centre of Interdisciplinary Addiction Research (ZIS) of the University of Hamburg |
Center for Interdisciplinary Addiction Research, University of Hamburg (Zentrum für Interdisziplinäre Suchtforschung der Universität Hamburg, ZIS) |
|
Prof. Dr. med. Norbert Scherbaum LVR-Klinikum Essen |
Working Group on Drugs and Addiction of the German Medical Association (Arbeitsgruppe „Sucht und Drogen“ der Bundesärztekammer, BÄK) |
|
Dr. med. Katharina Schoett Ökumenisches Hainich Klinikum |
German Society for Addiction Medicine (Deutsche Gesellschaft für Suchtmedizin, DGS) |
|
Frank Schulte-Derne Landschaftsverband Westfalen-Lippe (LWL) |
German Society for Social Work in Addiction Care (Deutsche Gesellschaft für Soziale Arbeit in der Suchthilfe, DG SAS) |
|
Frank Vilsmeier Psychiatrisches Krankenhaus Rickling Winfried Looser LVR-Klinik Düren |
German Nursing Council Deutscher Pflegerat |
|
Norbert Wittmann Mudra drug counseling Benjamin Löhner Mudra drug counseling |
Mudra – Alternative Youth and Drug Aid Mudra – Alternative Jugend- und Drogenhilfe e. V. |
|
Prof. Dr. med. Norbert Wodarz Klinik und Poliklinik für Psychiatrie und Psychotherapie der Universität am Bezirksklinikum Regensburg |
Bavarian Academy for Questions of Addiction and Health (Bayerische Akademie für Sucht- und Gesundheitsfragen, BAS) |
eTable 2. Further participating experts for specific questions.
| Experts | Chapter |
|
Prof. Dr. med. Michael Christ Klinik für Notfallmedizin und Internistische Intensivmedizin, Klinikum Nürnberg [Nuremberg] |
Acute therapy: the emergency setting |
|
Dr. med. Dr. med. dent. Niklas Rommel, Prof. Dr. med. Dr. med. dent. Marco R. Kesting Klinik und Poliklinik für Mund-, Kiefer- und Gesichtschirurgie am Klinikum rechts der Isar der Technischen Universität München [Munich] |
Comorbidities: dental problems |
|
Jeanine Paulick Institut für Psychologie, Technische Universität Chemnitz |
Pregnant women, young mothers, and prenatal harm; psychotherapeutic interventions |
|
Dr. med. Jan-Peter Siedentopf Ambulanz für Suchterkrankungen und Infektionen in der Schwangerschaft, Klinik für Geburtsmedizin, Campus Virchow-Klinikum, Charité – Universitätsmedizin Berlin |
Pregnant women, young mothers, and prenatal harm |
|
PD Dr. med. Jürgen Dinger Neonatologie und Pädiatrische Intensivmedizin, Klinik und Poliklinik für Kinder- und Jugendmedizin, Universitätsklinikum Dresden |
Pregnant women, young mothers, and prenatal harm |
|
Prof. Dr. rer. nat. Michael Klein, Dipl.-Psych. Janina Dyba Deutsches Institut für Sucht- und Präventionsforschung, Katholische Hochschule Nordrhein-Westfalen, Köln [Cologne} |
Methamphetamine abuse in the family context |
|
Dr. rer. medic. Henrike Dirks Klinik für Abhängiges Verhalten und Suchtmedizin, LVR-Klinikum Essen |
Methamphetamine abuse among men who have sex with men (MSM) |
|
Antje Kettner Drug Scouts, Leipzig |
Harm reduction |
Methods
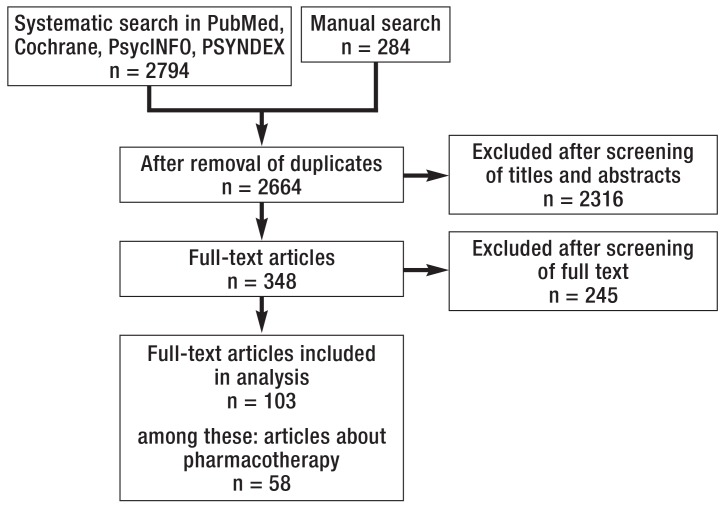
The guideline was developed in accordance with the rules laid down by the AWMF (3). In June 2015, a systematic review of the literature was performed in the Cochrane, Medline, PSYNDEX, and PsycINFO databases and supplemented by a manual search. All studies and systematic reviews on the treatment of methamphetamine-related disorders from 2000 onward were included in the analysis (Figure, eTables 3 and 4, eBox). The evidence was graded according to the scheme of the Oxford Centre for Evidence-Based Medicine (2011), and systematic reviews were assessed as described in AMSTAR (Assessing the Methodological Quality of Systematic Reviews). A systematic search for guidelines was carried out in April 2015. The identified guidelines were assessed with the German Guideline Assessing Instrument (Deutsches Leitlinien-Bewertungsinstrument, DELBI). These searches were not updated, and the experts did not introduce any new publications during the guideline development process.
Figure.
Flowchart: systematic literature search
eTable 3. Literature search: search strategies.
| Database | Search terms | Filters | Hits |
| Cochrane Library Date: 6/4/2015 |
psychostimulant OR methamphetamin* OR “amphetamine-type” OR psychoactive OR ”amphetamine-related disorders” |
Period 2000–2015 | Cochrane Reviews: 14 Clinical Trials: 768 |
| Medline via PubMed Date: 6/9/2015 |
(methamphetamin* OR methylamphetamin* OR “crystal meth” OR “amphetamine type stimulants” OR “amphetamine-type stimulants” OR “amphetamine derivative”) OR Methamphetamine [MeSH Terms] OR (“Amphetamine-Related Disorders/rehabilitation”[Mesh] OR “Amphetamine-Related Disorders/therapy”[Mesh]) |
Period 2000–2015,“ English,” “German,” “human,” “clinical trials,” “case report,” “systematic reviews” |
1533 |
| PsycINFO Date: 6/26/2015 |
methamphetamin* in “Title” treatment in “Abstract” |
Period 2000–2015, “English,” “German,” “human” |
466 |
| PSYNDEX | methamphetamin* in “Textfeld” | Period 2000–2015, English, German, human |
13 |
eTable 4. Literature search: guideline databases searched.
| Database | URL | Hits | Relevant |
| Association of Scientific Medical Societies in Germany (AWMF) (D) | www.awmf.org | 28 | 0 |
| Guidelines International Network (GIN) (international) | www.g-i-n.net | 19 | 0 |
| National Guideline Clearinghouse (NGC) (USA) | www.guidelines.gov | 72 | 0 |
| Canadian Medical Association Guidelines Infobase (CA) | www.cma.ca | 18 | 0 |
| National Institute for Health and Clinical Excellence (NICE) (GB) | www.nice.org.uk | 5 | 1 |
| Evidence Search (GB) | www.evidence.nhs.uk | 33 | 1 |
| Scottish Intercollegiate Guidelines Network (SIGN) (GB) | www.sign.ac.uk | 12 | 0 |
| Institute for Clinical Systems Improvement (ICSI) (USA) | www.icsi.org | 39 | 0 |
| World Health Organization (WHO) (international) | www.who.int | 8 | 1 |
| American Psychiatric Association (APA) (USA) | www.psychiatry.org | 1 | 1 |
| European Psychiatric Association (EPA) (Europe) | www.europsy.net | 16 | 0 |
| European College of Neuropsychopharmacology (ECNP) (Europe) | www.ecnp.eu | 14 | 0 |
| Manual search | 5 | 5 |
CA, Canada; D, Germany; GB, United Kingdom of Great Britain and Northern Ireland; USA, United States of America; URL, uniform resource locator
eBOX. Literature search: inclusion and exclusion criteria for articles.
Inclusion
Appropriate subject matter (treatment of methamphetamine-related disorders)
Appropriate type of publication (systematic review, clinical trial, or case report)
In German or English
Published 2000–2015
Exclusion
Subject other than the treatment of methamphetamine-related disorders
Other type of study (e.g., epidemiological, prognostic, or preclinical)
Other type of publication (e.g., editorial, narrative or unsystematic review, abstract, letter)
Too few patients (<10)
Duplicate or double publication
Inaccessible or withdrawn publication
Recommendations were consented in three consensus conferences using the nominal group technique. A consensus strength of at least 75% was required. The draft guideline underwent public consultation in May and June 2016.
All of the participants’ conflicts of interest were disclosed and discussed as recommended by the AWMF (3). It was not considered necessary to dismiss any of the experts from the panel; the panel agreed on abstention in particular cases.
The methods employed, the evidence tables, comments from public consultation, and the conflicts of interest have all been published in the guideline report (2).
Results
Evidence base
348 full texts were examined and 103 studies were included in the analysis, 58 of which dealt with pharmacotherapy. Although the evidence base included randomized controlled trials (RCTs), most of the publications had marked limitations, including small case numbers and high dropout rates. Abstinence was only rarely studied as the primary endpoint; more common endpoints were the quantity and frequency of drug consumption, retention rate (percentage of patients remaining in treatment), and craving. In sum, the currently available evidence for the efficacy of pharmacotherapy in the acute and postacute phases is both sparse and rather weak. With regard to psychotherapy, it is uncertain whether approaches that have been used in the English-speaking countries, e.g., reward-based contingency management, can be successfully used in Germany as well, because patients’ acceptance of the material reinforcements that were employed may depend strongly on their sociocultural attitudes and socioeconomic modes of living.
Recommendations
Consensus was nevertheless obtained for 135 recommendations on diagnosis, awareness and early intervention, acute and postacute treatment, comorbidities, special groups of persons, relapse prevention, and harm reduction; more than two-thirds of the recommendations were issued by unanimous consensus. Many of these recommendations are weak because of the limited reliability of the evidence and the small effect sizes that were found. Strong recommendations were only issued when there was reliable evidence in support of therapeutic efficacy, when ethical considerations played an important role, or when the item in question was a description of established good clinical practice. In the sections below, particular treatment recommendations will be presented. Recommendations on treatment planning are listed in Table 1.
Table 1. Selected recommendations on treatment planning.
| Recommendation | Strength of recommendation |
| A person actively seeking help from the addiction aid system for the first time ought to be given an appointment for counseling with in 24 hours. – Unanimous expert consensus | ↑ |
| All persons who consume methamphetamine should also be advised about self-help and referred to a local self-help group. – Unanimous expert consensus | ↑↑ |
| Methamphetamine abstinence ought to be the primary goal of treatment for methamphetamine-related disorder. – Unanimous expert consensus | ↑ |
| The patient’s own goals for treatment should be taken into account in treatment planning. – Unanimous expert consensus | ↑↑ |
↑↑, strong recommendation; ↑, recommendation
Acute treatment
Emergency treatment
The literature search on the emergency treatment of methamphetamine intoxication yielded one older, consensus-based guideline of moderate methodological quality (4), and no primary clinical trials. The recommendations are based on this guideline and on the authors’ clinical experience.
A person suffering from methamphetamine intoxication should be treated in an environment that is as quiet as possible and shielded from outside stimuli, and should not be left alone at any time. Such persons have often consumed other drugs as well; therefore, the administration of medications should be avoided whenever possible, unless constant medical monitoring can be provided. If the patient urgently needs treatment for marked agitation, aggressiveness, or psychotic manifestations, benzodiazepines should be used as the agent of first choice. If these alone do not sedate the patient adequately, the adding-on of an antipsychotic drug may be considered, especially if the patient has delusions or hallucinations.
After an episode of intoxication, patients should be recommended a more detailed psychiatric/addiction-medical diagnostic assessment and, where appropriate, treatment. Persons diagnosed as methamphetamine-dependent should be offered a course of qualified withdrawal treatment for a minimum of three weeks.
Qualified withdrawal treatment
Only a small number of the studies that were identified investigated the efficacy of qualified withdrawal treatment. The guideline’s recommendations in this area are based mainly on extrapolations from studies of postacute treatment, and on expert opinion.
A patient with a methamphetamine-related disorder should be offered techniques of psychotherapy such as psychoeducation and motivational interviewing in an inpatient setting as part of qualified multimodal withdrawal treatment. The available data do not enable a reliable comparison of individual psychotherapeutic techniques for use in acute therapy. Over the long term, complex, tightly coordinated packages of multiple interventions seem to be more promising than several distinct interventions performed in sequence (5). Acute and postacute therapy may also be linked together through the use of other psychotherapeutic methods, such as behavioral therapy or contingency management, as early as the qualified withdrawal phase.
As regards pharmacotherapy, the available RCTs have very small case numbers and high dropout rates and reveal effects only for secondary endpoints such as craving or retention rate. Not just for this reason, but also because drugs must generally be used off label to treat methamphetamine-related disorders, the experts recommend caution in pharmacotherapy; depending on the target condition, tranquilizers, drive-increasing antidepressants, or antipsychotic drugs may be considered (symptom-oriented treatment, Table 2). The guideline explicitly recommends against the use of selective serotonin-reuptake inhibitors (SSRI), even in patients with depressive manifestations, because of the danger of serotonin syndrome and the increased rate of side effects that has frequently been described. Weak recommendations are given for dexamphetamine (in case of multiple unsuccessful prior withdrawal attempts, for a limited time only, and in an inpatient setting) and acetylcysteine (for strong craving). Two small RCTs showed no effect of dexamphetamine on methamphetamine consumption, but did show a benefit, compared to placebo treatment, with respect to secondary endpoints (retention rate, 86.3 ± 52.2 days vs. 48.6 ± 45.4 days; p = 0.014). In a study with a very small number of patients, acetylcysteine relieved craving significantly better than placebo (4.57 versus 3.2; p <0.001). The favorable side-effect profile of acetylcysteine was a further important factor leading to a positive recommendation for treatment with the drug.
Table 2. Symptom-oriented pharmacotherapy as a component of acute treatment.
| Symptom | Treatment options | Recommendations |
| Methamphetamine intoxication with acute agitation or markedly fluctuating state with unpredictable responses | – Once psychotherapeutic de-escalating measures have been exhausted, benzodiazepines are the treatment of choice, as soon as adequate provisions for intervention and monitoring are in place | ↑↑ |
| Depressive-anxious symptoms with exhaustion and/or hypersomnia during methamphetamine withdrawal | – Bupropion or a drive-increasing tricyclic antidepressant such as desipramine | ↔ |
| Sleep disturbances and/or agitation during methamphetamine withdrawal | – The drugs of choice, according to expert opinion, are sedating antidepressants or low-potency sedating antipsychotic drugs – Avoid hypnotic agents! | Antidepressants: ↔ Low-potency sedating antipsychotic drugs: ↔ |
| Methamphetamine-induced psychotic manifestations | – Atypical antipsychotic drugs – Benzodiazepines in addition, as needed, for a short time only – R eassess the indication and discontinue within 6 months if possible | Atypical antipsychotic drugs: ↑ Benzodiazepines: ↔ |
| Acute depressive and/or anxious state with endangerment to self or others during methamphetamine withdrawal | – Benzodiazepines as needed, for a short time only | ↔ |
| In case of multiple unsuccessful prior withdrawal attempts | – Dexamphetamine only in individual cases & in an inpatient setting – Taper to off within 2 weeks | ↔ ↔ |
| Marked craving during methamphetamine withdrawal | – Acetylcysteine as needed, 600–1200 mg/day | ↔ |
↑↑, strong recommendation; ↑, recommendation; ↔, open recommendation
Postacute therapy
Based on expert opinion, postacute interventions should be offered after the withdrawal phase as a seamless continuation of treatment so that patients can be stably retained within the addiction aid system.
Psychotherapeutic counseling and treatment
The search identified 26 RCTs on psychotherapeutic interventions for which a reduction in methamphetamine consumption was a primary endpoint. Drug abstinence was not an explicit goal of treatment in any of the trials; abstinence (temporary or permanent) was no more than a secondary endpoint. In consequence, the available data do not permit any conclusive determination of the suitability of the interventions tested for promoting abstinence. Positive effects were found, for example, on the frequency of drug use, the number of negative urine samples, or craving.
Studies were found on the efficacy of the following interventions:
Psychoeducation
Motivational interviewing
Motivation enhancement
Contingency management
Cognitive behavioral therapy
Acceptance and commitment therapy
Matrix and FAST (Family Alternative Treatment Activities, Self-Help and Therapeutic Community)
Stepped-care approaches (a need-based, incremental system of interventions, ranging from low-threshold educative approaches to complex inpatient treatment methods)
Community-based approaches.
All interventions improved addiction-specific endpoints, such as the quantity of methamphetamine consumed, significantly as compared to baseline and to the control group. Comparisons across methods rarely revealed a marked advantage of any particular method over the others. In an RCT with 229 patients, a psychotherapeutic intervention (contingency management) was compared with withdrawal under pharmacotherapy with sertraline (6). Contingency management is an intervention derived from classic behavioral therapy in which the achievement of an agreed-upon behavioral change, such as the reduction of drug consumption, is reinforced by a reward such as a gift certificate. In this trial, the patients treated with sertraline had a significantly lower retention rate and made significantly less use of relapse prevention. Those treated with contingency management had a significantly higher rate of achieving three successive weeks of abstinence (sertraline [25.4%] versus sertraline + contingency management [42.6%] versus contingency management [51.9%] versus placebo [41.8%], p = 0.035). No differences were found with respect to craving, depression, or compliance. Sertraline had significantly more side effects (nausea, sexual dysfunction, undesired gastrointestinal and anticholinergic effects).
The guideline panel concluded that the psychotherapeutic interventions studied are effective, but that the design of the trials does not enable any determination of which particular techniques are most effective. Complex, disorder-specific approaches such as Matrix may be especially effective. The RCT on Matrix (7) may have underestimated its therapeutic effect, because the “treatment as usual” given to the control group was at a higher dosage and intensity.
Thus, any person who abuses methamphetamine, with or without a diagnosis of methamphetamine dependence, should be offered psychotherapeutic counseling or treatment of an appropriate type for his or her individual needs and motivation. In a stepped-care approach, this ought to range from low-threshold information, psychoeducation, and counseling all the way to multimodal consumption-reducing and withdrawal-treatment programs. Methamphetamine abusers meeting the diagnostic criteria for a substance-related disorder ought to be offered behavioral therapy or a complex methamphetamine-specific program for reduction of drug consumption or withdrawal from the drug, depending on their willingness to undergo such treatment and its local availability.
Pharmacotherapy
The literature search yielded 58 studies on pharmacotherapeutic interventions, mostly RCTs, only a few of which were of adequate methodological quality. Many were carried out in combination with cognitive behavioral therapy (8). The drugs studied included acetylcysteine, antidepressants, antiepileptic drugs, atypical neuroleptic drugs, calcium antagonists, muscle relaxants, opioid antagonists, psychostimulants, varenicline, cholinesterase inhibitors, and citicoline. None of the drugs studied is approved in Germany for the treatment of methamphetamine dependence.
After considering the limitations of each study, the observed effects, and the potential complications of the use of each drug, the expert panel gave only a weak recommendation for the drive-increasing antidepressants bupropion and imipramine. Post hoc analysis of a methodologically acceptable RCT with 151 participants revealed a mild advantage of bupropion over placebo with regard to the duration of abstinence in patients whose consumption at baseline was already moderate (i.e., on fewer than 18 days per month). The rate of abstinence for two weeks or longer was 20% versus 7%; for 6 weeks or longer, 14% versus 4%; for 12 weeks, 6% versus 1% (p = 0.0176) (9, 10). These results were not confirmed in another, smaller RCT (94 participants) (11), yet the experts still consider this to be at least a potential supportive treatment for persons whose methamphetamine consumption is low to moderate. In a small RCT (32 participants), a significantly higher retention rate was seen in patients taking 150 mg of imipramine per day than in those taking 10 mg per day (median duration of retention, 33 days versus 10.5 days) (12, 13).
Sertraline should not be given to patients with methamphetamine-related disorders. A methodologically adequate RCT did not show any benefit from sertraline compared to placebo, but it did show a significantly lower retention rate (38% versus 60%, p = 0.036) and a strong trend toward worse results with respect to abstinence, measured as three negative weekly urine tests in a row (34.2% versus 46.8%, p = 0.052) (6).
The substitution of psychostimulants for methamphetamine is a pharmacologically plausible approach, but the experts consider its efficacy to be inadequately documented. Drugs that have been used for this purpose include sustained-release dexamphetamine and sustained-release methylphenidate. The few RCTs on the subject have marked limitations, and the reported effects are inconsistent and mainly related to secondary endpoints. This type of treatment should be provided only in the setting of a high-quality clinical trial, preferably in an inpatient setting. Modafinil ought not to be used either: an RCT involving 210 patients, with a high dropout rate and poor compliance (14), revealed no advantage over placebo while bearing a high risk of serious drug interactions (effect potentiation).
Nor did a further RCT (15) show any efficacy of combined pharmacotherapy with flumazenil, gabapentin, and hydroxyzine, which did, however, cause more frequent serious side effects, such as epileptic seizures. This type of treatment should not be given.
For all other substances tested, the experts considered the evidence to be insufficiently informative to enable any recommendation. They saw an urgent need for further research in this area.
Further treatments
In three methodologically robust RCTs, exercise therapy was found to yield significant improvement in methamphetamine withdrawal symptoms such as craving as well as accompanying symptoms such as anxiety and depression (16– 18). Professionally led, structured exercise programs conduced several times a week, with varying intensity, were studied, as well as an exercise program conducted by the patients themselves. Thus, exercise therapy should be offered and provided as supportive treatment.
Neurofeedback was also found in an RCT to improve addiction-specific endpoints and quality of life, compared to pharmacotherapy alone (19). As neurofeedback is a cumbersome technique, the experts only issued a weak recommendation for it.
There have been no trials investigating the treatment of methamphetamine abusers with ear acupuncture according to the scheme of the National Acupuncture Detoxification Association (NADA), but there have been positive individual case reports. As ear acupuncture is considered to have practically no risk, the experts issued a weak recommendation for it, despite the absence of evidence in its favor.
Comorbid disorders
Persons with methamphetamine-related disorders often have comorbid mental disorders; the associations are complex and bidirectional. Methamphetamine may be abused as a form of self-medication to relieve the symptoms of a depressive disorder, an anxiety disorder, or a post-traumatic disorder (1). On the other hand, methamphetamine abuse can itself give rise to mental symptoms and disorders.
According to expert opinion, methamphetamine-related disorders and comorbid disorders are best treated in integrated fashion, or, if this is not possible, in appropriately coordinated fashion. Patients with a comorbid mental disorder should be offered disorder-specific psychotherapy.
The following sections will deal with a few particulars of the treatment of comorbid mental disorders inpatients with methamphetamine-related disorders, insofar as these can be derived from the available literature.
Depression and bipolar disorder
For patients with comorbid depression, the available studies have not revealed any efficacy of antidepressants. Studies of limited methodological quality have yielded weak evidence for the efficacy of quetiapine (an antipsychotic drug) and very weak evidence for that of the nutritional supplements citicoline and creatine; the latter may be considered as supplementary treatment for patients suffering from depression or bipolar disorder (20– 22). Risperidone may also be offered to patients with bipolar disorder, as there is weak evidence for its efficacy in this situation (20). The recommendation for the nutritional supplements is based mainly on their low risk, rather than on any robust evidence of benefit: in a placebo-controlled RCT involving 60 patients, depressive manifestations as measured on the Inventory of Depressive Symptomatology-Clinician Rating (IDS-C) fell from 38.8 and 37.8 points at baseline in the drug and placebo groups, respectively, to 26.2 and 33.1 points at the end of the study (p = 0.05) (21). Psychoeducation and exercise therapy have been found effective and should be offered (17, 23).
Anxiety disorders
In an RCT of high methodological quality, exercise therapy reduced the manifestations of anxiety. It should, therefore, be offered (17).
Attention-deficit/hyperactivity disorder
The general recommendation to treat persons suffering from attention-deficit/hyperactivity disorder (ADHD) with methylphenidate does not apply to patients with comorbid methamphetamine-related disorders. These patients may have tolerance to methylphenidate because of the similar chemical structures of the two drugs, and treatment with methylphenidate may also carry a potential for abuse. If pharmacotherapy for ADHD is indicated, the first line of treatment ought to be atomoxetine or an antidepressant such as bupropion, venlafaxine, or duloxetine.
Relapse prevention
On the basis of case reports and their own clinical experience, the expert panel recommended that, after postacute therapy, patients ought to be offered at least a full year of further follow-up care to prevent relapse. Ideally, the type of care provided should be tailored to the needs of the patient; it may consist, for example, of individual or group psychotherapy, sociotherapeutic interventions, self-help, or exercise therapy.
Harm reduction
Although abstinence is the recommended primary goal of treatment, many patients do not (yet) want to achieve this goal, or are not (yet) able to do so. For such patients, appropriate means of harm reduction are recommended:
Reducing consumption
Switching to less dangerous forms of consumption—above all, abstaining from intravenous consumption
Avoiding dangerous drug interactions, such as serotonin syndrome
Regular nutrition
Proper attention to dental health and hygiene
Safe sex.
Discussion
A systematic search for publications on the treatment of methamphetamine-related disorders yielded evidence on many types of psychotherapeutic, pharmacotherapeutic, and other interventions. The experts judged most of the available studies to be methodologically inadequate, and many of their recommendations were therefore issued as expert consensus. Although fewer RCTs have been published on psychotherapy than on pharmacotherapy (26 vs. 58), the efficacy of the former in lowering drug consumption is better documented: behavioral therapy, contingency management, and combined programs have all been found effective (although certain approaches used in the English-speaking world may not be as effective in Germany). There is no empirically derived answer to the question whether psychotherapy can effectively promote the goal of abstinence from methamphetamine. For pharmacotherapy, despite the larger number of RCTs, only a few positive effects on the various aspects of methamphetamine-related disorders have been documented. The guideline panel sees an urgent need for more research in this area.
Key Messages.
This S3 guideline is the first one in which the evidence on the pharmacotherapy and psychotherapy of methamphetamine-related disorders is systematically summarized. The available studies suffer from methodological limitations of varying severity.
Psychotherapeutic interventions, such as cognitive behavioral therapy or contingency management, and complex addiction-specific programs are effective and should be offered.
Methamphetamine-dependent persons should also be encouraged to participate in local self-help groups.
Pharmacotherapy in the acute phase of treatment should be symptom-oriented. Giving other psychoactive drugs instead of methamphetamine has not been found to be an effective form of withdrawal treatment.
Exercise programs make the success of treatment more likely and should therefore be offered.
Acknowledgments
Acknowledgement
We thank all of the authors and outside experts involved in the creation of the S3 guideline on methamphetamine-related disorders: Wolf-Dietrich Braunwarth, Michael Christ, Jürgen Dinger, Henrike Dirks, Janina Dyba, Timo Harfst, Heribert Fleischmann, Peter Jeschke, Marco R. Kesting, Antje Kettner, Michael Klein, Benjamin Löhner, Winfried Looser, Sascha Milin, Josef Mischo, Bernd Mühlbauer, Jeanine Paulick, Niklas Rommel, Ingo Schäfer, Norbert Scherbaum, Katharina Schoett, Frank Schulte-Derne, Jan-Peter Siedentopf, Frank Vilsmeier, Norbert Wittmann, and Anne Krampe-Scheidler.
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Prof. Gouzouli-Mayfrank has received honoraria for book projects dealing with the topic of this article from the following publishing companies: Springer, Kohlhammer, Steinkopff, and Thieme.
The remaining authors state that they have no conflicts of interest.
References
- 1.Milin S, Lotzin A, Degkwitz P, et al. Amphetamin und Methamphetamin - Personengruppen mit missbräuchlichem Konsum und Ansatzpunkte für präventive Maßnahmen Sachbericht. 2014. www.methstudie.de/ats-bericht.pdf (last accessed 2 June 2017) [Google Scholar]
- 2.Die Drogenbeauftragte der Bundesregierung, Bundesministerium für Gesundheit (BMG), Bundesärztekammer (BÄK), Deutsche Gesellschaft für Psychiatrie, Psychotherapie und Nervenheilkunde (DGPPN) S3-Leitlinie Methamphetamin-bezogene Störungen. Leitlinienreport. 1st Edition. Version 1. doi.org/10.6101/AZQ/000337 (last accessed on 21 November 2016) [Google Scholar]
- 3.Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF) Zuckschwerdt. München: 2012. Das AWMF-Regelwerk Leitlinien. [Google Scholar]
- 4.Jenner J, Spain D, et al. Guidelines Development Working Party. Australian Government Department of Health and Ageing. Canberra: 2006. Management of patients with psychostimulant toxicity: guidelines for emergency departments. [Google Scholar]
- 5.Lee N, Johns L, et al. Turning Point Alcohol and Drug Centre, No 14: Methamphetamine dependence and treatment. Fitzroy, Victoria: Turning Point Alcohol and Drug Centre. 2007 [Google Scholar]
- 6.Shoptaw S, Huber A, Peck J, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85:12–18. doi: 10.1016/j.drugalcdep.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Rawson RA, Marinelli-Casey P, Anglin MD, et al. A multi-site comparison of psychosocial approaches for the treatment of methamphetamine dependence. Addiction. 2004;99:708–717. doi: 10.1111/j.1360-0443.2004.00707.x. [DOI] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration (SAMHSA) Counselor‘s treatment manual: matrix intensive outpatient treatment for people with stimulant use disorders. Reprinted. 2007 Rockville, MD: SAMHSA 2006. [Google Scholar]
- 9.Elkashef A, Vocci F, Hanson G, White J, Wickes W, Tiihonen J. Pharmacotherapy of methamphetamine addiction: an update. Subst Abus. 2008;29:31–49. doi: 10.1080/08897070802218554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCann DJ, Li SH. A novel, nonbinary evaluation of success and failure reveals bupropion efficacy versus methamphetamine dependence: reanalysis of a multisite trial. CNS Neurosci Ther. 2012;18:414–418. doi: 10.1111/j.1755-5949.2011.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson AL, Li SH, Markova D, et al. Bupropion for the treatment of methamphetamine dependence in non-daily users: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2015;150:170–174. doi: 10.1016/j.drugalcdep.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galloway GP, Newmeyer J, Knapp T, Stalcup SA, Smith D. Imipramine for the treatment of cocaine and methamphetamine dependence. J Addict Dis. 1994;13:201–216. doi: 10.1300/j069v13n04_08. [DOI] [PubMed] [Google Scholar]
- 13.Galloway GP, Newmeyer J, Knapp T, Stalcup SA, Smith D. A controlled trial of imipramine for the treatment of methamphetamine dependence. J Subst Abuse Treat. 1996;13:493–497. doi: 10.1016/s0740-5472(96)00154-7. [DOI] [PubMed] [Google Scholar]
- 14.Anderson AL, Li SH, Biswas K, et al. Modafinil for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2012;120:135–141. doi: 10.1016/j.drugalcdep.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ling W, Shoptaw S, Hillhouse M, et al. Double-blind placebo-controlled evaluation of the PROMETA protocol for methamphetamine dependence. Addiction. 2012;107:361–369. doi: 10.1111/j.1360-0443.2011.03619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang T, Shen B, Shi Y, Xiang P, Yu Z. Chiral separation and determination of R/S-methamphetamine and its metabolite R/S-amphetamine in urine using LC-MS/MS. Forensic Sci Int. 2015;246:72–78. doi: 10.1016/j.forsciint.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 17.Rawson RA, Chudzynski J, Gonzales R, et al. The impact of exercise on depression and anxiety symptoms among abstinent methamphetamine-dependent individuals in a residential treatment setting. J Subst Abuse Treat. 2015;57:36–40. doi: 10.1016/j.jsat.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dolezal BA, Chudzynski J, Storer TW, et al. Eight weeks of exercise training improves fitness measures in methamphetamine-dependent individuals in residential treatment. J Addict Med. 2013;7:122–128. doi: 10.1097/ADM.0b013e318282475e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rostami R, Dehghani-Arani F. Neurofeedback training as a new method in treatment of crystal methamphetamine dependent patients: a preliminary study. Appl Psychophysiol Biofeedback. 2015;40:151–161. doi: 10.1007/s10484-015-9281-1. [DOI] [PubMed] [Google Scholar]
- 20.Nejtek VA, Avila M, Chen LA, et al. Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized double-blind trial. J Clin Psychiatry. 2008;69:1257–1266. doi: 10.4088/jcp.v69n0808. [DOI] [PubMed] [Google Scholar]
- 21.Brown ES, Gabrielson B. A randomized, double-blind, placebo-controlled trial of citicoline for bipolar and unipolar depression and methamphetamine dependence. J Affect Disord. 2012;143:257–260. doi: 10.1016/j.jad.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Hellem TL, Lundberg KJ, Renshaw PF. A review of treatment options for co-occurring methamphetamine use disorders and depression. J Addict Nurs. 2015;26:14–23. doi: 10.1097/JAN.0000000000000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sherman SG, Sutcliffe C, Srirojn B, Latkin CA, Aramratanna A, Celentano DD. Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Soc Sci Med. 2009;68:69–79. doi: 10.1016/j.socscimed.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]