Abstract
OBJECTIVE
To assess reproductive choices of US reproductive age women and factors that influence consideration of elective egg freezing (EF).
DESIGN
Cross-sectional Internet based survey of 1000 women
METHODS
An anonymous 63-item self-administered questionnaire was distributed to a representative cross section of reproductive age women age 21–45, stratified by age</=35. Half of the sample had at least 1 child, while the remaining expressed desire to have children. Ordinal logistic regression was performed to characterize the association of population characteristics and reproductive knowledge with likelihood to consider EF. Willingness to pay was assessed using a linear prediction model which calculated dollar amounts at varying success rates.
RESULTS
Overall, 87.2% of the sample reported awareness of EF for fertility preservation, 25% would consider this option, yet only 29.8% knew what the EF process entails. Once informed of the process, 30% of women changed their level of consideration. In a multivariable model, Asian race(OR1.71, CI1.36–2.98), single status(OR1.38, CI1.27–1.53), and infertility(OR2.00, CI1.55–2.43) increased the likelihood of considering EF. Women likely to consider egg freezing would be willing to pay $3,811.55 (95% CI $2,862.66 – $4,760.44). If the total cost were $10,000, 91% of the cohort would accept at minimum 50% chance of successful delivery.
CONCLUSION
This study is one of the largest cohorts of reproductive age women in the US addressing reproductive choices and factors associated with the importance of having a biologically-related child and the likelihood of considering EF to preserve fertility. This study provides important insight into the willingness to pay for this elective endeavor.
Keywords: oocyte cryopreservation, fertility preservation, elective egg freezing, willingness to pay
INTRODUCTION
Over the past 60 years, several advances in assisted reproductive technologies have led to an increased number of reproductive choices for women. Substantial improvements in laboratory techniques for oocyte cryopreservation have led to higher pregnancy rates. Indeed, several studies suggest that pregnancy rates with IVF using previously frozen eggs are similar to rates using fresh oocytes1,2. Since the American Society of Reproductive Medicine (ASRM) removed the experimental label on oocyte cryopreservation3 in 2012, oocyte cryopreservation has become a routine service offered to women in most IVF centers in the United States. In particular, there has been increased awareness and interest in using this technology for preserving fertility in the face of the natural age-related fertility decline, i.e. ‘elective’ oocyte cryopreservation. However, elective egg freezing remains controversial because there are no clear evidence based guidelines regarding the safety, efficacy and cost effectiveness. The ASRM has raised the concern that widespread use of this technology could ‘give women false hope and encourage women to delay childbearing.3
Currently, there is very little data from the general population in the United States about knowledge and attitudes regarding oocyte cryopreservation, and under what circumstances such technology might be sought. In particular, there is no information about whether women in the general population are aware of the costs, or which patients are most interested in seeking this technology. Moreover, little is known regarding the value women place on these services from a societal perspective or how much women would be ‘willing to pay’ for the potential to preserve future fertility.
The objectives of this study were to assess the views of women in the general population on their likelihood of considering elective egg freezing to preserve the possibility of having a biologically-related child and biological and non-biological parenting. In particular we sought to assess knowledge on reproductive aging and reproductive technologies and compare reproductive choices and acceptance of options based on the level of knowledge observed. Additionally, we explored the value women placed on this technology in terms of a willingness to pay for this procedure. We hypothesized that women who had not yet completed having children, were over the age of 35, and underestimated reproductive potential with age would be most likely to consider elective oocyte cryopreservation and ART methods.
MATERIALS AND METHODS
Study Design
We conducted a cross-sectional Internet-based study, using survey methodology. This method of survey administration was chosen specifically to reach a large cross-section of the general population of reproductive age women across the United States. An anonymous 50-item questionnaire with 13 demographic-related questions was distributed to a sample of reproductive age women. The survey was self-administered and completely voluntary. Interested participants selected a link inviting them to participate in an anonymous survey. IRB approval was obtained at the Hospital of the University of Pennsylvania.
Survey Platform
Subjects were recruited through social media websites via the online research platform of Lab42, a market research firm. Lab42 was chosen because of their capacity to program and launch a survey instrument through secure links on several Internet and social media sites. The demographic characteristics of survey users from Lab42 are similar to the demographics reported from US census data.4
Study Cohort
Women living in the United States between the ages of 21 and 45 were included. Men or women outside of this age range were excluded. Eligible participants reviewed a standard consent form, and agreed to participate. Recruitment ended once 1000 surveys were fully completed, with responses documented to each question asked. We stratified the sample of the population based on age and whether or not a woman had a child prior to taking the survey. In order to recruit sufficient participants in each age group (<35, ≥35), survey administration was stratified to capture 500 responses from age group 21–34 years and 500 responses from the age group 35–45 years. In addition, within each age group, half the responses were obtained from those who had at least one child and half from those who did not have any children but desired future children.
Survey Instrument
The survey consisted of four parts assessing 1) demographic information; 2) reproduction and fertility awareness, specifically as it relates to age-related changes in fertility and miscarriage rates, as well as knowledge of the procedure, estimated cost, and estimated success of oocyte cryopreservation; 3) reproductive goals and factors that might influence the decision and timing to become a parent; 4) willingness to consider fertility preservation with oocyte cryopreservation, and willingness to pay for use of such technology. Response categories for the majority of survey items, with the exception of demographic data, were measured using a 5-point Likert Scale as appropriate. Specifically reproductive/fertility-related knowledge questions were modeled from previously published data and survey instruments5,6. The survey was piloted among a sample cohort, with feedback from all respondents used to modify and create its final form. Once the survey was programmed and made accessible to the general public, responses were obtained from 10% of the sample size and used to confirm the survey’s usability in its final format.
Statistical Analysis
Demographics
Respondents’ demographic and personal reproductive histories were tabulated, and comparisons made using chi square test, independent student t-test or non-parametric equivalents as appropriate.
Measurement of Outcomes
Responses to the survey to understand the importance of factors that influence the decision to have children, the likelihood of accepting various methods to help to become a parent, including the potential willingness to consider egg freezing for fertility preservation were measured using a Likert scale. The main outcome of interest was an individual’s willingness to consider egg freezing as a method to preserve fertility potential.
Unadjusted Analysis of 2-level Outcome
First, We divided the responses to the 5-point Likert scale into a dichotomous outcome: those who might choose to freeze eggs, “potential egg freezers,” were defined as those who were ‘extremely likely’ or ‘likely’ to consider egg freezing, while the ‘non-freezers’ were those who were ‘extremely unlikely,’ ‘unlikely,’ or ‘neutral’. Associations between each demographic factor and this dichotomous outcome were assessed using chi-square, fisher-exact, or nonparametric equivalents.
Unadjusted and Adjusted Multivariable Analysis
Ordinal logistic regression was then performed using the 5-point Likert scale responses to identify the characteristics that were associated with willingness to consider elective egg freezing in this sample of women. A 5-level outcome was used to account for any subgroup differences. A multivariable logistic regression model was created including the factors that were independently associated with the likelihood of considering egg freezing. A backwards step-wise elimination approach was then used to select the covariates for the final model. In addition, reproductive knowledge and knowledge regarding egg freezing was categorized as either accurate or inaccurate, and in some cases categorized as an underestimate, accurate and overestimate of the correct response. A composite score was generated to compare those who answered the majority of the fertility knowledge-related questions (4/6), egg freezing knowledge-related questions (2/2), and egg freezing cost (2/2), and the combination of all knowledge-related questions (5/8) questions correctly to those who answered fewer correctly and logistic regression was used to compare willingness to consider egg freezing in the more versus less knowledgeable groups.
Finally, willingness to pay was assessed using a linear prediction model comparing the reported maximum amount a subject is willing to pay to have a child using frozen eggs, and varying percent chances of success of having a child in this manner. Using the linear regression equation, dollar amounts at varying levels of percent chance of success were calculated.
Sample Size Calculation
European studies have reported a 30% prevalence of willingness to pursue oocyte cryopreservation.6 For this calculation, we chose age as a primary predictor variable and estimated that if the baseline prevalence is 30% to measure a difference in prevalence of 10% in the age group <35 years, we needed 376 participants in each age group to be able to reject the null hypothesis that the prevalence between the two groups are equal with a power of 80%, and a type I alpha error of 5%.
RESULTS
Demographics
The demographic characteristics of the 1000 women in the study cohort with complete survey responses are shown in Table 1 (Additional detailed demographics in Appendix 1). The median age of the entire cohort was 34.5 (Inter Quartile Range 28–38) years old. Fifty-five percent were currently married. The majority, 82.6% were Caucasian, 46.1% identified with Christianity (non-Catholic), 35.8% reported having a college degree, and 45.2% employed full-time, more than half reported an annual income of $25–49,999 (26%), or $50–74,999 (26%). There were approximately 20% more Caucasian respondents than are representative of the US population, however only 6% more than average with a college degree. Annual household income overall was similar with the median US income of approximately $50,000, as well as a similar proportion of non-Catholic Christians.4,7 The surveyed population was stratified, 50% having at least one child at the time of the survey, with a median number of 2 children, and 50% with no child. In addition, In keeping with national averages8, 9.5% reported taking more than 12 months to conceive with their first pregnancy, compared to 47.3% of women who reported their first pregnancy to be unplanned. In addition, when considering important factors in the decision of when to have a child, 80% of the cohort believed being married or being in a stable relationship with a partner who would share the child rearing responsibilities is ‘extremely important,’ while 48% and 43% believed it to be extremely important to have enough money and to not be ‘too old’ respectively. Sixty-nine percent reported that having a biological child was extremely or moderately important. Only 8 women had previously frozen their eggs.
Table 1.
Demographics of women unlikely or neutral to consider egg freezing compared to women likely to consider egg (n=1000)
| Demographic | Whole survey cohort N=1000 | Non-Egg Freezers N=784 | Potential Egg Freezers N=216 | p-value |
|---|---|---|---|---|
|
| ||||
| Age (years): | 0.677 | |||
| Median (IQR) | 34.5 (28–38) | 34 (28–38) | 35 (28–38) | |
|
| ||||
| Parity: | 0.219 | |||
| 0 children | 500 (50.0) | 384 (49.0) | 116 (53.7) | |
| 1 or more children | 500 (50.0) | 400 (51.0) | 100 (46.3) | |
|
| ||||
| Ethnicity: | 0.619 | |||
| Hispanic or Latino | 71 (7.1) | 54 (6.9) | 17 (7.87) | |
|
| ||||
| Race: | 0.060 | |||
| Caucasian or White | 836 (83.6) | 656 (83.7) | 170 (78.7) | |
| African American or Black | 75 (7.5) | 51 (6.51) | 25 (11.6) | |
| Asian° | 61 (6.1) | 49 (6.25) | 16 (2.3) | |
| Other | 28 (2.8) | 28 (3.57) | 5 (2.3) | |
|
| ||||
| Highest Level of Education Completed: | 0.695 | |||
| High school degree or less | 143 (14.3) | 116 (14.8) | 27 (12.5) | |
| College degree or some college | 721 (72.1) | 562 (71.7) | 159 (73.6) | |
| Higher education degree (Masters, Doctoral or Professional) | 136 (13.6) | 106 (13.5) | 30 (13.9) | |
|
| ||||
| Current Employment Status§: | ||||
| Employed | 638 (63.8) | 483 (61.6) | 155 (71.8) | 0.006 |
| Unemployed | 362 (36.2) | 301 (38.4) | 61 (28.2) | |
|
| ||||
| Type of Medical Insurance: | 0.160 | |||
| Private Insurance (Managed care plan (HMO) or other) | 700 (70.0) | 541 (69.0) | 159 (73.6) | |
| Government-subsidized insurance (Medicare, Medicaid etc) | 163 (16.3) | 137 (17.5) | 26 (12.0) | |
| No Insurance or I don’t know | 137 (13.7) | 106 (13.5) | 31 (14.4) | |
|
| ||||
| Annual Household Income (before taxes): | 0.002 | |||
| </= $124,999 | 935 (93.5) | 743 (94.8) | 192 (88.9) | |
| >/= $125,000 | 55 (5.5) | 41( 5.3) | 24 (11.1) | |
|
| ||||
| Relationship Status: | 0.420 | |||
| Single or dating | 230 (23.0) | 175 (22.3) | 55 (25.5) | |
| Living with Significant Other or engaged | 166 (16.6) | 127 (16.2) | 39 (18.1) | |
| Married/Civil Union/Domestic Partnership | 555 (55.5) | 440 (56.1) | 115 (53.2) | |
| Divorced/Separated/Widowed | 49 (4.9) | 42 (5.4) | 7 (3.2) | |
Southeast Asian/Pacific Islander (including Indian subcontinent)
Other= American Indian or Alaska Native, Middle Eastern, other
Employed: full-time/part-time/self-employed; Unemployed: student/homemaker/retired/disabled
Appendix Table 1.
Demographics of surveyed population (n=1000)§
| Demographic | N (percent) |
|---|---|
|
| |
| Age (years): | |
| Median (IQR) | 34.5 (28–38) |
|
| |
| Age Range (years): | |
| 21–24 | 133 (13.3) |
| 25–29 | 170 (17.0) |
| 30–34 | 197 (19.7) |
| 35–40 | 320 (32.0) |
| 40–45 | 180 (18) |
|
| |
| Ethnicity: | |
| Hispanic or Latino | 71 (7.1) |
|
| |
| Race: | |
| Caucasian or White | 836 (83.6) |
| African American or Black | 75 (7.5) |
| Asian° | 61 (6.1) |
| Other* | 28 (2.8) |
|
| |
| Region of Residence**: | |
| Northeast | 188 (18.8) |
| South | 345 (34.5) |
| Midwest | 259 (25.9) |
| West | 208 (20.8) |
|
| |
| Religion: | |
| Christianity (Protestant, Non-Catholic, Greek or Russian Orthodox) | 461 (46.1) |
| Catholicism | 155 (15.5) |
| Hinduism | 15 (1.5) |
| Islam | 11 (1.1) |
| Judaism | 10 (1.0) |
| Buddhism | 9 (0.9) |
| No organized religion, but spiritual | 151 (15.5) |
| No organized religion, and not spiritual | 79 (7.9) |
| Atheism or Agnosticism | 97 (9.7) |
| Other | 12 (1.2) |
|
| |
| Highest Level of Education Completed: | |
| High school degree or less | 143 (14.3) |
| College degree or some college | 721 (72.1) |
| Higher education degree (Masters, Doctoral or Professional) | 136 (13.6) |
|
| |
| Current Employment Status§: | |
| Employed | 638 (63.8) |
| Unemployed | 362 (36.2) |
|
| |
| Type of Medical Insurance: | |
| Private Insurance (Managed care plan (HMO) or other) | 700 (70.0) |
| Government-subsidized insurance (Medicare, Medicaid, etc.) | 163 (16.3) |
| No Insurance or “I don’t know” | 137 (13.7) |
|
| |
| Annual Household Income (before taxes): | |
| Less than $25,000 | 156 (15.6) |
| $25,000–$49,999 | 262 (26.2) |
| $50,000–$74,999 | 260 (26.0) |
| $75,000–$99,999 | 157 (15.7) |
| $100,000–$124,999 | 70 (7.0) |
| $125,000–$149,999 | 32 (3.2) |
| $150,000 or more | 33 (3.3) |
| Prefer not to answer | 30 (3.0) |
|
| |
| Relationship Status: | |
| Single or dating | 230 (23.0) |
| Married/Civil Union/Domestic Partnership | 166 (16.6) |
| Living with Significant Other or engaged | 555 (55.5) |
| Divorced/Separated/Widowed | 49 (4.9) |
|
| |
| Number of Pregnancies: | |
| 0 | 400 (40.0) |
| 1 | 168 (16.8) |
| 2 | 195 (19.5) |
| >2 | 237 (23.7) |
|
| |
| Number of children current: | |
| 0 | 500 (50.0) |
| 1 | 157 (15.7) |
| 2 | 193 (19.3) |
| >2 | 150 (15.0) |
|
| |
| Sexual Orientation: | |
| Heterosexual | 916 (91.6) |
| Homosexual | 20 (2.0) |
| Bisexual | 64 (6.4) |
|
| |
| Raised by: | |
| Guardian(s) genetically-related (genetic parents/grandparents etc) | 935 (93.5) |
| Adopted (guardian not genetically-related) | 16 (1.6) |
| Both (One guardian genetically-related, one not genetically-related) | 46 (4.6) |
| Other | 3 (0.3) |
|
| |
| Age of first pregnancy (n=600) | |
| <18 years old | 63 (10.5) |
| 18–20 years old | 148 (24.7) |
| 21–24 years old | 144 (24.0) |
| 25–29 years old | 165 (27.5) |
| 30–34 years old | 61 (10.2) |
| 35–40 years old | 17 (2.8) |
| 41–45 years old | 2 (0.3) |
|
| |
| Outcomes of pregnancy/pregnancies other than live birth: (n=600, select all that apply) | |
| No other outcome besides live birth | 329 (52.8) |
| Miscarriage | 196 (31.5) |
| Termination | 70 (11.2) |
| Stillbirth/Death of a child | 24 (3.9) |
| Ectopic | 4 (0.6) |
|
| |
| Ideal age to have a first child: | |
| <20 years old | 28 (2.8) |
| 20–24 years old | 249 (24.9) |
| 25–29 years old | 408 (40.8) |
| 30–34 years old | 198 (19.8) |
| 35–39 years old | 85 (8.5) |
| 40–45 years old | 29 (2.9) |
| >45 years old | 3 (0.3) |
|
| |
| Ideal age to have a last child: (n=843, number who desire > one child): | |
| <20 years old | 1 (0.1) |
| 20–24 years old | 18 (2.1) |
| 25–29 years old | 182 (21.6) |
| 30–34 years old | 341 (34.1) |
| 35–39 years old | 228 (27.1) |
| 40–45 years old | 62 (7.4) |
| >45 years old | 11 (1.3) |
The demographic of the population from which the study group was drawn matched the intentions of the survey in that approximately 60% of those with potential access to this survey were within the desired age-range, 54% female, 28% single without children, 18% single with children, 9% married without children, and 46% married with children. Twenty-eight percent of those approached were likely to have obtained a college degree, with the highest percentage of income being the $50–75,000 range and 40% full time employment. In terms of racial distribution, approximately 70% of those who typically use the sites that would link the survey are Caucasian, 7% African American/Black, 7% Hispanic, and 10% Asian.
Southeast Asian/Pacific Islander (including Indian subcontinent)
Other= American Indian or Alaska Native, Middle Eastern, other
Northeast: Maine, Vermont, New Hampshire, Connecticut, Massachusetts, New York, Rhode Island, New Jersey; South: Delaware, Maryland, District of Columbia, Virginia, West Virginia, Tennessee, Kentucky, North Carolina, South Carolina, Georgia, Florida, Alabama, Louisiana, Mississippi, Texas, Oklahoma; Arkansas; Midwest: Ohio, Indiana, Illinois, Michigan, Kansas, Nebraska, South Dakota, North Dakota, Minnesota, Iowa, Missouri, Wisconsin; West: Washington, Oregon, California, Nevada, New Mexico, Arizona, Colorado, Wyoming, Utah, Montana, Idaho, Alaska, Hawaii
Employed: full-time/part-time/self-employed; Unemployed: student/homemaker/retired/disabled
Egg Freezing
Likelihood of freezing eggs
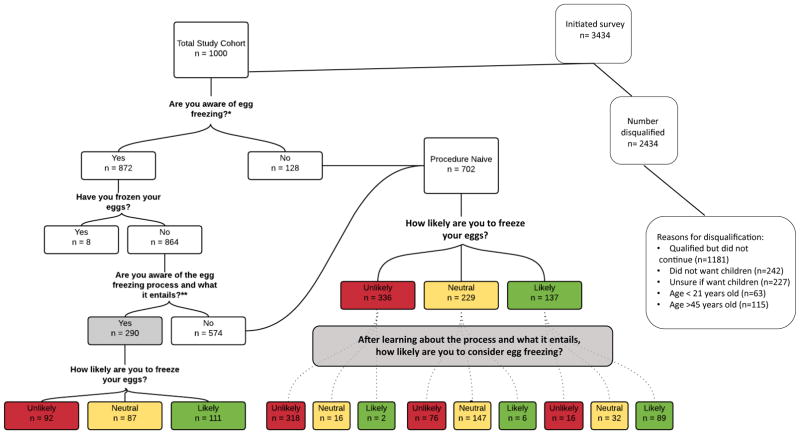
Figure 1 depicts the likelihood of considering egg freezing as an option for fertility preservation as it relates to knowledge of what egg freezing involves. Only 29.2% of the group who did not previously freeze eggs (290/992) knew the process of egg freezing (“procedure-knowledgeable”) involves approximately 2 weeks of frequent office visits and injections, as well as a minor surgical procedure to retrieve eggs.
Figure 1.
*= Knowledge that the option of egg freezing is available as a method to potentially preserve a woman’s fertility and that insurance is unlikely to cover the costs involved
**= Knowledge that egg freezing involves approximately two weeks of daily injections and office visits as well as a minor surgical procedure
 = Procedure-knowledgeable or education provided
= Procedure-knowledgeable or education provided
How procedure-related knowledge changed the likelihood of freezing eggs
Once procedure-naïve women read this description of the procedure, 21% of women changed their level of consideration to a different category. Of the procedure-naïve women, (n=702), one-third were initially neutral to the consideration of egg freezing. Once this group was knowledgeable (“procedure-educated”), one-third changed their mind from neutral to unlikely, and 2% from neutral to likely. As might be expected, all but 5% of the women who were unlikely to consider egg freezing before being fully knowledgeable of the procedure continued to be unlikely to do so after reading the explanation. Sixty-five percent of those who were initially likely to consider freezing after knowing what it entailed continued to be likely to consider. The overall prevalence of those likely to consider egg freezing was 21.6%. This group of potential egg-freezers includes the 8 women who previously froze eggs, the 111 women who were procedure-knowledgeable at the onset, and the 97 procedure-educated women who were likely to consider.
Timing of egg freezing
The majority of the cohort (86.7%) accurately assessed that age 20–29 is the best interval to freeze eggs in terms of chance of success of having a baby. All participants were also asked ‘how likely would you be to consider freezing eggs if you were in each of six age groups and had not yet started/completed having children? By age, the highest proportion that would consider this was actually those who imagined if they had not had a family by either between 26 and 29 years (41%) or 30 to 34 years old (41%).
Willingness to freeze eggs
Table 1 compares demographic information between the ‘likely freezers’ and ‘non-freezers’ as a dichotomous outcome. Those who were currently employed, or made at least $125,000 in annual income were more likely to consider elective egg freezing.
In univariate analysis using a 5-level outcome (Table 2), not currently having a child in this cohort (OR1.32, p=0.031), African American (OR=1.70, p=0.016) and Asian (OR=1.57, p=0.047) race, as well as being single and never married compared to married (OR=1.36, p=0.007) were each independently associated with an increased likelihood to consider egg freezing. In addition, those who were employed (either in full or part-time capacity) or had an annual household income of more than or equal to $125,000 were more likely to be willing to freeze eggs than those who were not employed or made less money. No other variables were significantly associated with this outcome. With regard to personal reproductive history, having a history of impaired fertility (OR 1.81, p<0.001), and history of being treated for infertility (OR=2.89, p=<0.001) were both positively associated with an increased likelihood to consider egg freezing. This was consistent with women who reported more than 12 months time to first pregnancy having an increased likelihood to consider egg freezing (OR 2.06, p=0.004). In addition, women who believed it would be ideal to have one’s first child at the age of 35 or older were 1.41 times more likely to consider freezing eggs compared to those who thought the ideal age to have a first child is under 35 years old. As might be expected, of those women who would ideally desire more than one child, those few who thought it ideal to have their last child after the age of 45 were 4 times more likely to consider egg freezing (OR 4.36, p=0.042). However, age of the participant less than or equal to 35 compared to greater than 35 years old was not significantly associated with the likelihood of considering egg freezing (OR 1.19, p=0.130), even when restricted to those women who had not yet had a child but desire to have one.
Table 2.
Association of demographics and potential to consider freezing eggs
| Unadjusted analysis | Adjusted analysis | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Demographic | OR | p value | 95% CI | OR | p value | 95% CI |
|
| ||||||
| Not currently have a biological child | 1.32 | 0.031 | 1.02–1.37 | --- | --- | --- |
|
| ||||||
| Race: | ||||||
| African American or Black | 1.70 | 0.016 | 1.11–2.61 | 1.56 | 0.046 | 1.01–2.44 |
| Asian | 1.57 | 0.047 | 1.01–2.44 | 1.76 | 0.015 | 1.12–2.77 |
|
| ||||||
| Current Employment Status: | ||||||
| Employed (full-time, part-time or self-) | 1.31 | 0.001 | 1.14–1.46 | 1.32 | 0.044 | 1.01–1.39 |
|
| ||||||
| Annual Household Income (before taxes): | ||||||
| >/= $125,000 | 1.87 | 0.011 | 1.16–3.03 | 1.75 | 0.025 | 1.07–2.86 |
|
| ||||||
| Relationship Status: | ||||||
| Reference: Single or dating | --- | --- | ||||
| Married/Civil Union/Domestic Partnership | 0.64 | 0.001 | 0.49–0.84 | 0.67 | 0.006 | 0.51–0.89 |
|
| ||||||
| History of infertility | 1.81 | <0.001 | 1.31–2.52 | 1.93 | <0.001 | 1.38–2.69 |
In the final multivariable logistic regression model (Table 2) specifically Asian race (OR=1.70, p=0.019), identifying oneself as single (OR=1.33, p=0.006), holding current employment (OR=1.22, p=0.044), having a household income greater than or equal to $125,000 (OR=1.75, p=0.025), as well as having a history of infertility (OR1.98, p<0.001) significantly increased the likelihood of considering egg freezing. Not currently having a child compared to having a child was no longer significantly associated.
Reproductive Knowledge and Consideration of Egg Freezing
Participants were asked 6 questions to assess general reproduction and age-related fertility knowledge (Appendix Table 3). Only 27 of the 1000 (2.7%) answered all of these questions correctly, while 13 (1.3%) women got all of the questions wrong. The majority of women, 75.4%, had at least half (3/6) of the fertility-related questions correct. Forty percent had 4 out of 6 questions correct (‘fertility-knowledgeable’). Those who answered either the majority, or half of these questions correctly were no more likely than those who did not answer these correctly to consider egg freezing. We tested if correct answers to individual questions was associated with the likelihood of considering egg freezing, and we found that those who correctly answered that the risk of miscarriage increases with age were 1.35 times more likely to consider egg freezing for fertility preservation than those who answered incorrectly (p=0.03).
Appendix Table 3.
Survey questions to determine knowledge regarding fertility and egg freezing
| Question | Answer choices | |||||
|---|---|---|---|---|---|---|
| N (percent) | ||||||
| At what age does the average woman start experiencing a decline in fertility? | 18–28 years | 29–34 years* | 35–38 years | > 38 years | ||
| 24 (2.4) | 290 (29.0) | 480 (48.0) | 206 (20.6) | |||
| If a 35–40 year old woman and a man regularly (1–2 times per week) have unprotected intercourse over a period of a year, what is the chance she will become pregnant? | 0–49% | 50–59%* | 60–69% | 70–100% | ||
| 361 (36.1) | 378 (37.8) | 165 (16.5) | 96 (9.6) | |||
| Does a woman’s chance of having a pregnancy that ends in miscarriage (pregnancy loss) increase as the woman gets older? | Yes* | No | I don’t know | |||
| 840(84.0) | 45(4.5) | 115(11.5) | ||||
| The chance for a pregnancy to end in miscarriage when the mother is 40 years old is? | <1% | 1–10% | 11–20% | 21–30%* | >30% | |
| 5 (0.5) | 105 (10.5) | 259 (25.9) | 298 (29.8) | 333 (33.3) | ||
| Does a woman’s risk of having a baby with a genetic abnormality such as Down syndrome increase with age? | Yes* | No | I don’t know | |||
| 837 (83.7) | 49 (4.9) | 114 (11.4) | ||||
| The chance of having a baby using In Vitro Fertilization (IVF) treatment when a woman is at an age between 41 and 43 years old is less than 20%. | True* | False | ||||
| 592(59.2) | 408(40.8) | |||||
| At what age do you think it is best to freeze a woman’s eggs to get the healthiest eggs that would give the highest chance of success of having a baby? | 20–29 years* | 30–35 years | 36–40 years | >40 years | ||
| 867 (86.7) | 107 (10.7) | 20 (2.0) | 6 (0.6) | |||
| In general, if a woman does not have infertility and freezes her eggs before the age of 35, what do you think the chance of having a baby using frozen eggs in the future? (Typically a woman under 35 may be able to freeze between 10–20 eggs.)? | 1% per frozen egg | 5% per frozen egg* | 15% per frozen egg | 30% per frozen egg | 50% per frozen egg | 60% per frozen egg |
| 29 (2.9) | 126 (12.6) | 267 (26.7) | 303 (30.3) | 203 (20.3) | 72 (7.2) | |
| On average, what do you think the cost is to undergo one cycle of IVF to obtain and freeze eggs (including medication)? | < $1,000 | $1,000–$4,999 | $5,000–$7,999 | $8,000–$10,999* | $11,000–$15,000 | |
| 9(0.9) | 116(11.6) | 243(24.3) | 288(28.8) | 344(34.4) | ||
| On average, how much do you think it costs to store frozen eggs for one year? | < $100 | $100–$299 | $300–$800* | > $800 | ||
| 17(1.7) | 148(14.8) | 393(39.3) | 442(44.2) | |||
indicates the correct answer choice according to published data.
Participants were asked 4 questions related specifically to knowledge regarding egg freezing and its estimated success in conception and cost (Appendix Table 4). Those who knew the optimal age range for successful egg freezing (20–29 years old) were more likely to consider freezing eggs compared to those who answered incorrectly, or overestimated success at a later age (OR=1.51, p<0.001). Women who underestimated the chance of conceiving with using a frozen-thawed egg were less likely to consider egg freezing as those who answered an accurate estimation (OR=0.44, p=0.042), and those who overestimated the chance of success were more likely to consider fertility preservation (OR=1.69, p=0.002). Those who underestimated the cost of egg freezing were more likely to consider egg freezing than those who correctly identified or overestimated this cost (OR=1.23, p=<0.001). Similarly, women who overestimated the cost to store frozen eggs were 25% less likely to consider egg freezing (OR=0.75, p=<0.001).
Twelve percent of the entire cohort answered both egg freezing-related knowledge questions correctly. These women were actually significantly less likely to consider egg freezing than the remainder of the group (OR=0.43, p=0.001). Combining questions with regard to knowledge and cost, 16.2% of the cohort correctly answered the majority (3/4) of questions, however, these women were no more or less likely to consider egg freezing than the less-knowledgeable group. Finally, an overall composite score of level of reproduction-related and egg freezing-related knowledge was used to assess its association with egg freezing. The ‘knowledgeable group’ answered at least 5 of 8 questions correctly, while the ‘naïve group’ answered no more than 4 of the 8 questions correctly. The 422 (42.2%) knowledgeable women were less likely to consider egg freezing compared to those who answered fewer correctly (OR=0.78, p=0.026).
Willingness to pursue options to become a parent
Survey participants were asked to consider if they were unable to become pregnant on their own, what options would women be likely to select. Appendix Table 2 describes these theoretical reproductive choices of the entire cohort. In addition, it demonstrates that each option that involves either using assisted reproductive technology to conceive a child who is genetically-related, or using donor gametes were more likely to be selected by the potential egg freezers compared to the group of non-freezers (p<0.001) and less likely to choose not to have children (p<0.001). There was no difference in the two groups when evaluating adoption as an option to become a parent.
Appendix Table 2.
| What would you do or consider doing if you could not become pregnant on your own? | Overall Cohort | Non-Egg Freezers (N=784) | Potential Egg Freezers (N=216) | P value |
|---|---|---|---|---|
|
| ||||
| Seek help from a specialist: | <0.001 | |||
| Likely | 820 (82.0) | 620 (79.1) | 200(92.6) | |
| Unlikely/neutral | 180 (18.0) | 164 (20.9) | 16 (7.4) | |
|
| ||||
| Undergo IVF: | <0.001 | |||
| Likely | 518 (51.8) | 353(45.0) | 165(76.4) | |
| Unlikely/neutral | 482 (48.2) | 431(55.0) | 51(23.6) | |
|
| ||||
| If poor sperm were an issue, would use donor sperm and subject’s own eggs: | <0.001 | |||
| Likely | 254 (25.4) | 195(24.9) | 100(46.3) | |
| Unlikely/neutral | 746 (74.6) | 426(54.3) | 116(53.6) | |
|
| ||||
| If poor eggs were an issue, would use donor eggs and partner’s sperm (or donor sperm if no male partner) and carry the pregnancy: | <0.001 | |||
| Likely | 243 (24.3) | 152(19.4) | 91(42.1) | |
| Unlikely/neutral | 757 (75.7) | 632(80.6) | 125(57.9) | |
|
| ||||
| If could not carry a pregnancy, would use subject’s eggs and partner’s sperm (or donor sperm if no male partner) and a gestational carrier: | <0.001 | |||
| Likely | 353 (35.3) | 227(28.9) | 126(58.3) | |
| Unlikely/neutral | 647 (64.7) | 557(71.1) | 98(41.7) | |
|
| ||||
| If subject did not have a male partner, would use donor sperm: | <0.001 | |||
| Likely | 295 (29.5) | 195(24.9) | 100(46.3) | |
| Unlikely/neutral | 705 (70.5) | 589(75.1) | 116(53.7) | |
|
| ||||
| Choose adoption: | 0.89 | |||
| Likely | 278 (27.8) | 570(72.7) | 152(70.4) | |
| Unlikely/neutral | 722 (72.2) | 214(27.3) | 64(29.6) | |
|
| ||||
| Choose not to have children: | <0.001 | |||
| Likely | 210 (21.0) | 181(23.1) | 29(13.4) | |
| Unlikely/neutral | 790 (79.0) | 603(76.9) | 187(86.6) | |
Utilization of ART services in women who plan to conceive at age 40
We presented the participants with a clinical scenario of deferring child-bearing until age 40 and provided pertinent statistics regarding the chance of successfully conceiving and cost. The subjects were then asked if they were a women age 35 who anticipated waiting until age 40 to conceive, would they 1) consider freezing their eggs at age 35 and using these frozen eggs if unable to conceive without assistance at age 40 or wait until age 40 to attempt conception and if not successful, 2) consider adoption or not having children, 3) consider IVF using her own eggs, or 4) consider IVF using donor eggs. The participants ranked the order in which they would select the above options.
One-Hundred and forty-eight women (14.8%) said they would not consider any of the 4 options. Only 3.4% would consider and rank all four options and 85.2% of the cohort ranked 1 or more of the options presented as something they would consider doing, however, a total of 600 participants selected only one option: of these, 30.0% would choose only to freeze their eggs at 35, attempt to conceive on their own at age 40, and, if unsuccessful, would use their frozen eggs. Of the participants who selected more than one option, the majority (58.7%) of this group selected freezing eggs at age 35 as the first option they would choose. In addition, using a weighted ranking calculated based on the number of responses for each choice and the order of choices selected, freezing eggs at age 35 was ordered as the first preferred option, followed by considering adoption or not having children, then IVF using own eggs and finally using donor eggs.
Willingness to Pay for Egg Freezing
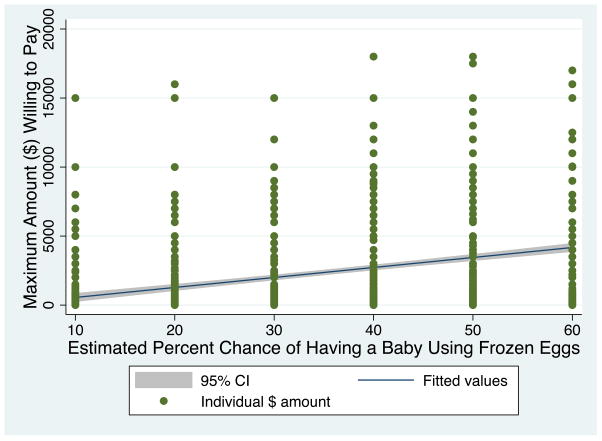
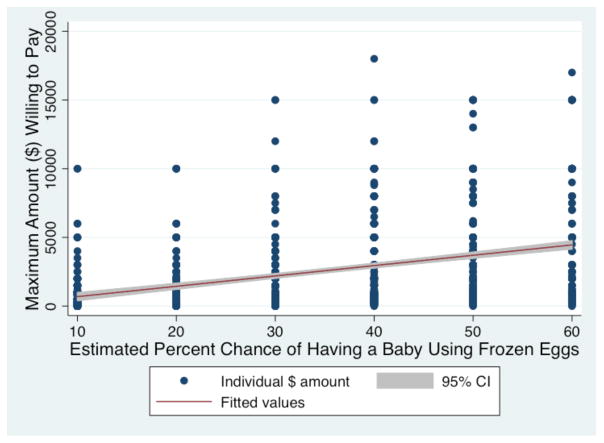
In this sample, the majority of women estimated the cost of egg freezing and medication to be $8,000 or above (n=632, 63.2%), and the majority of women estimated the cost of storing frozen eggs to be at least $300 per year (n=835, 83.5%). Since there is no guarantee of pregnancy or live birth with any fertility treatment, we assessed the individual’s willingness to pay for use of egg freezing technology by presenting the subjects different percent chance of success of having a successful pregnancy using frozen-thawed eggs, and asked the specific dollar amount she would be willing to pay at each level of success. Interestingly, level of reported income and willingness to pay was not significantly correlated (p=0.0168) Figure 2a depicts a linear prediction of the maximum amount of money ($) participants would be willing to pay to freeze and store eggs by the chance of having a baby using the frozen eggs. In the clinical scenario of 40% live birth rate, the geometric mean maximum amount women in the total cohort would be willing to pay is $2,653.40 ((95% CI $2,271.74–$3,035.13). When restricting to women who indicated they would be likely to consider egg freezing (n=216), the geometric mean of the amount this group would be willing to pay for this service increased to $3,811.55 (95% CI $2,862.66 – $4,760.44) (Figure 2b). This suggests that compared to the actual cost of oocyte cryopreservation at this time, most women believe it is overpriced and perhaps demonstrates a more accurate monetary value that these subjects have placed on elective oocyte cryopreservation.
Figure 2.
Figure 2a. Maximum Estimated Amount ($) Willing to Pay By Entire Study Population to Have a Baby Using Frozen Eggs
Figure 2b. Maximum Estimated Amount ($) Willing to Pay to Have a Baby Using Frozen Eggs By Subjects Who Are Willing to Consider Egg Freezing
We then asked the cohort what the minimum rate of success of achieving pregnancy would be if it cost $10,000 for the IVF stimulation, procedure and medications. Ninety-one percent of the cohort would accept a minimum of 50% chance of success, with 53.3% of the cohort accepting a minimum of 80% success. A minimum success rate of 49% is more likely to be acceptable to those likely to freeze eggs (15%) compared to those unlikely to freeze (7.2%). As expected, those who are more likely to freeze their eggs are accepting of a lower minimum success rate compared to those unlikely to freeze(p=0.004).
Discussion
This is one of the first and largest studies in the U.S. to evaluate the reproductive choices of American women in the era of Assisted Reproductive Technologies. Our findings help to define reproductive age women who would be likely to consider egg freezing as an option for fertility preservation. We explored factors including race, relationship and employment status, annual household income, history of impaired fertility, as well as how much one would be likely to pay for such a service. Within the last year, the results of a large internet-based survey was published which addressed the overall acceptability of egg freezing in the U.S. However, this study was not limited to women of childbearing age who are interested in having children, rather, it included men (44.6% of entire cohort), and the majority of subjects were at least 45 years old.9 Up until now, the only published data on this topic in the US involving women of childbearing age is limited to a group of women who had already chosen to electively freeze eggs. However, this cohort is limited by a smaller sample size in a single city.10 In that cohort (n=183), most women were Caucasian, never married or divorced, had no partner, and were >35 years old at the time of freezing eggs. Most of these women (79%), however, wished they underwent egg freezing at an earlier age. Compared to our population based cohort, surprisingly, age was not associated with an increased likelihood to consider egg freezing, even when restricted to the group of women who had not yet had a child by age 35. However, women who believed the ideal age to have a first child was over 35 years old were more likely to consider egg freezing.
Another published survey similar to ours was conducted in Belgium in 2010.6 Overall, the number of ‘potential egg freezers’ was reported as 31.5%, compared to the 21.6% in our cohort. Interestingly one may have expected a lower percentage in the Belgian cohort since they included all women and did not restrict the population to only women who desire future children. One possible explanation for the difference is that the Belgian group found that potential freezers were more likely to be a part of the youngest age category of 21–29, and the mean age of their cohort was younger than ours. Of note, a similar proportion of women in both the Belgian and our cohort reported that they were most likely to freeze eggs, 3% and 4% respectively. In addition, the association of employment status, relationship status and history of infertility was consistent across both populations. Race was not compared between groups in the Belgian cohort, as 97% were Caucasian. A more recent Canadian study evaluated factors that may inform a woman’s decision to pursue oocyte freezing either electively or in the setting of a cancer diagnosis showed similar results with respect to knowledge gaps but was in an overall younger population and did not address a woman’s willingness to pay11.
We chose our study design and population to limit selection bias, and feel that we achieved a study sample that was closely representative of the general US population. However, it should be noted that 78% of those who were disqualified or did not complete the survey were in the 35 to 45 year old age group, and this could have potentially introduced a degree of selection bias. However, since the vast majority of those excluded in this age group were excluded because they were unsure if they wanted children in the future or were certain they did not want children in the future, they would not fit the desired demographic to optimally evaluate one’s potential desire to preserve future fertility.
One of the clinical challenges in offering elective egg freezing is related to the significant decline in fertility as women age12,13, which affects egg freezing success rates. In fact, 100% of surveyed US clinics found it acceptable to offer elective egg freezing to women under the age of 35, but only 26% felt it acceptable to offer to women greater than 40 years old.14 In addition to the decline of egg number, egg quality significantly declines over the reproductive life span, as does the egg’s capacity to contribute a normal genetic complement.15,16. Consistent with several studies, we found that the majority of women are aware that fertility declines with age and that miscarriage rates and risk of genetic abnormalities increase with age. However in contrast to other studies that suggest that women may overestimate pregnancy success as a woman ages, we observed that women accurately estimated the chance of pregnancy at advanced maternal age.17–19 In our study, women who correctly identified that rates of miscarriage increase with age were more likely to consider egg freezing. In addition, as might be expected, women who overestimated the success of egg freezing, and underestimated the cost were more likely to consider freezing eggs. While this suggests that women who are well educated regarding the diminishing chance of pregnancy and live birth with increasing age may be better equipped to make the decision to freeze eggs, we found that accurately estimating a woman’s chance to become pregnant was not associated with being more likely to consider fertility preservation. Nonetheless, providing education regarding fertility preservation techniques may be of value, as it altered decision-making in a substantial proportion of women in our study population (Figure 1). Thus it is possible that educating women with regard to age-related fertility decline and the concurrent increasing risk of miscarriage as well as options for assisted reproduction could influence the number of women who would choose to electively freeze eggs.
As with most procedures that are considered ‘elective,’ the involved costs are generally paid for by the individual desiring the service. Therefore, the cost of undergoing oocyte cryopreservation becomes an important factor to the individual who may elect to use this technology, and an important factor for society and other potential payers to consider. When considering cost-effectiveness, one must consider not only the financial cost of services but also the utility of those services from a patient or societal perspective. This study provides important data regarding not only the factors that influence decision-making but also the perceived value of these services for the purpose of conceiving a biologically-related child. Interestingly, the costs that are predicted using egg freezing to achieve a live birth in prior cost effective analyses substantially surpasses the cost that we found women are willing to pay for these services. A study performed in the Netherlands evaluated whether egg freezing at age 35 (over 3 cycles of ovarian hyperstimulation) followed by the use of frozen eggs at age 40 is cost-effective when compared to doing IVF at age 40 outright, or having an unassisted conception at age 40. This analysis considered the cost of each of these procedures, live birth rates at the different ages, as well as miscarriage rates.20 This study suggested that egg freezing was cost –effective if a minimum of 61% of women use their previously frozen eggs and if one is willing to pay approximately $24,600 per additional live birth achieved, providing more value for the money than delaying conception and then utilizing IVF to conceive. Another study in the US used cost-effectiveness modeling to evaluate women who wished to conceive at the age of 40 who 1) froze eggs at age 25, 2) froze ovarian tissue at age 25, or 3) attempted conception at age 40 and then sought assisted reproductive technologies if unsuccessful at that time.21 This particular study determined that it is most cost-effective to undergo no treatment at age 25 and that the cost of utilizing ART would need to exceed $22,000 for desired efficacy with egg freezing. The differences in conclusions in these two studies could be related to the differences in ages at which fertility preservation was undertaken, differences in sequences of treatment, and differences in estimations of costs for all procedures and presumed success rates. Neither of these studies assigned a value or utility of having a genetically-related child.
Most recently, promising cost-effective data has been published to support the decision to freeze eggs under certain circumstances. In a study using a hypothetical decision tree mathematical model, women who freeze eggs under the age of 35, and have at least 16 mature oocytes frozen, and then defer child-bearing attempts until the age of 40 have a significantly higher chance of live birth (62% versus 42%), and decreased cost per live birth ($39,946 versus $55,060) compared to women who wait until age 40 and attempt pregnancy spontaneously for 6 months, and if unsuccessful, undergo 2 cycles of fresh IVF. 22 Through our study, we know that women, when presented with the chances of live birth in each scenario, and the costs involved, the option that is most popular is to consider freezing eggs at age 35, for use at age 40 if unable to conceive without assistance at that time.
Egg freezing for fertility preservation is generally paid for out-of-pocket by the patient. While many costs are fixed, and others are driven by the market of our capitalist economy,23 little was previously known with regard to what women might be willing to pay to potentially preserve their fertility. Even when restricted to those who would be likely to consider egg freezing, the amount of money these women are willing to pay to undergo the procedure and store eggs is remarkably less than the average amounts charged in the U.S. It appears that there may be a discrepancy in willingness to pay and the estimation of cost when attempting to compare the geometric mean of willingness to pay for a live birth rate of 40%, and where the subjects were told it costs $10,000 for a live birth rate of 50%. Subjects expected a certain threshold of success to be willing to pay what egg freezing may actually cost. Therefore, for egg freezing to become more acceptable and accessible to women who may consider such an option to preserve fertility, the pregnancy success rates need to improve and cost would need to be reduced.
Conclusion
While there are studies that examine acceptability of oocyte cryopreservation, this study assessed for the first time in the US, demographic characteristics and reproductive choices as it relates to the likelihood of freezing eggs for fertility preservation and the willingness to pay for these services amongst the population of women who would actually utilize this service. This information is important in understanding the value placed by the general population on having a genetically-related child, and the extent to which women in the US would be likely to go to pursue fertility preservation procedures to maintain this possibility.
Acknowledgments
Funding Support: NIH 5K12HD001265, SS, MDS
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cobo A, Meseguer M, Remohi J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Human reproduction. 2010;25:2239–46. doi: 10.1093/humrep/deq146. [DOI] [PubMed] [Google Scholar]
- 2.Cobo ADC. Clinical application of oocyte vitrification: a systematic review and meta-analysis of randomized controlled trials. Fertil Steril. 2011;96:277–85. doi: 10.1016/j.fertnstert.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 3.Practice Committee of American Society for Reproductive M, Technology SfAR. Mature oocyte cryopreservation: a guideline. Fertil Steril. 2013;99:37–43. doi: 10.1016/j.fertnstert.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 4.http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml.
- 5.Skoog Svanberg ALC, Karlstrom P, Tyden T. Attitudes toward parenthood and awareness of fertility among postgraduate students in Sweden. Gender Medicine. 2006;3:187–95. doi: 10.1016/s1550-8579(06)80207-x. [DOI] [PubMed] [Google Scholar]
- 6.Stoop DNJ, Devroey P. A survey on the intentions and attitudes towards oocyte cryopreservation for non-medical reasons among women of reproductive age. Human Repro. 2010;26:655–61. doi: 10.1093/humrep/deq367. [DOI] [PubMed] [Google Scholar]
- 7.http://www.pewforum.org/2015/05/12/americas-changing-religious-landscape/.
- 8.Chandra ACC, Stephen EH National Center for Health Statistics. National health statistics reports. National Center for Health Statistics; 2013. Infertility and impaired fecundity in the United States, 1982–2010: Data from the National Survey of Family Growth. [PubMed] [Google Scholar]
- 9.Lewis EI, Missmer SA, Farland LV, Ginsburg ES. Public support in the United States for elective oocyte cryopreservation. Fertil Steril. 2016;106:1183–9. doi: 10.1016/j.fertnstert.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Hodes-Wertz B, Druckenmiller S, Smith M, Noyes N. What do reproductive-age women who undergo oocyte cryopreservation think about the process as a means to preserve fertility? Fertil Steril. 2013;100:1343–9. doi: 10.1016/j.fertnstert.2013.07.201. [DOI] [PubMed] [Google Scholar]
- 11.Daniluk JC, Koert E. Childless women’s beliefs and knowledge about oocyte freezing for social and medical reasons. Human reproduction. 2016;31:2313–20. doi: 10.1093/humrep/dew189. [DOI] [PubMed] [Google Scholar]
- 12.Block E. Quantitative morphological investigations of the follicular system in women; variations at different ages. Acta anatomica. 1952;14:108–23. doi: 10.1159/000140595. [DOI] [PubMed] [Google Scholar]
- 13.Faddy MJ, Gosden RG, Gougeon A, Richardson SJ, Nelson JF. Accelerated disappearance of ovarian follicles in mid-life: implications for forecasting menopause. Human reproduction. 1992;7:1342–6. doi: 10.1093/oxfordjournals.humrep.a137570. [DOI] [PubMed] [Google Scholar]
- 14.Rudick B, Opper N, Paulson R, Bendikson K, Chung K. The status of oocyte cryopreservation in the United States. Fertil Steril. 2010;94:2642–6. doi: 10.1016/j.fertnstert.2010.04.079. [DOI] [PubMed] [Google Scholar]
- 15.Battaglia DE, Goodwin P, Klein NA, Soules MR. Influence of maternal age on meiotic spindle assembly in oocytes from naturally cycling women. Human reproduction. 1996;11:2217–22. doi: 10.1093/oxfordjournals.humrep.a019080. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz D, Mayaux MJ. Female fecundity as a function of age: results of artificial insemination in 2193 nulliparous women with azoospermic husbands. Federation CECOS. The New England journal of medicine. 1982;306:404–6. doi: 10.1056/NEJM198202183060706. [DOI] [PubMed] [Google Scholar]
- 17.Bretherick KLFN, Avila L, Harbord SHA, Robinson WP. Fertility and aging: do reproductive-aged Canadian women kow what they need to know? Fertil Steril. 2010;93:2162–8. doi: 10.1016/j.fertnstert.2009.01.064. [DOI] [PubMed] [Google Scholar]
- 18.Daniluk JC, Koert E, Cheung A. Childless women’s knowledge of fertility and assisted human reproduction: identifying the gaps. Fertil Steril. 2012;97:420–6. doi: 10.1016/j.fertnstert.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 19.Lundsberg LS, Pal L, Gariepy AM, Xu X, Chu MC, Illuzzi JL. Knowledge, attitudes, and practices regarding conception and fertility: a population-based survey among reproductive-age United States women. Fertil Steril. 2014;101:767–74. doi: 10.1016/j.fertnstert.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 20.van Loendersloot LL, Moolenaar LM, Mol BW, Repping S, van der Veen F, Goddijn M. Expanding reproductive lifespan: a cost-effectiveness study on oocyte freezing. Human reproduction. 2011;26:3054–60. doi: 10.1093/humrep/der284. [DOI] [PubMed] [Google Scholar]
- 21.Hirshfeld-Cytron J, Grobman WA, Milad MP. Fertility preservation for social indications: a cost-based decision analysis. Fertil Steril. 2012;97:665–70. doi: 10.1016/j.fertnstert.2011.12.029. [DOI] [PubMed] [Google Scholar]
- 22.Devine K, Mumford SL, Goldman KN, et al. Baby budgeting: oocyte cryopreservation in women delaying reproduction can reduce cost per live birth. Fertil Steril. 2015;103:1446–53. e2. doi: 10.1016/j.fertnstert.2015.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.http://health.costhelper.com/in-vitro-fertilization.html.