Abstract
Studies have demonstrated disparate exposures to carcinogenic hazardous air pollutants (HAPs) in neighborhoods with high densities of Black and Hispanic residents in the US. Asians are the fastest growing racial/ethnic group in the US, yet they have been underemphasized in previous studies of environmental health and injustice. This cross-sectional study investigated possible disparities in residential exposure to carcinogenic HAPs among Asian Americans, including Asian American subgroups in the US (including all 50 states and the District of Columbia, n = 71,208 US census tracts) using National Air Toxics Assessment and US Census data. In an unadjusted analysis, Chinese and Korean Americans experience the highest mean cancer risks from HAPs, followed by Blacks. The aggregated Asian category ranks just below Blacks and above Hispanics, in terms of carcinogenic HAP risk. Multivariate models adjusting for socioeconomic status, population density, urban location, and geographic clustering show that an increase in proportion of Asian residents in census tracts is associated with significantly greater cancer risk from HAPs. Neighborhoods with higher proportions (as opposed to lower proportions) of Chinese, Korean, and South Asian residents have significantly greater cancer risk burdens relative to Whites. Tracts with higher concentrations of Asians speaking a non-English language and Asians that are US-born have significantly greater cancer risk burdens. Asian Americans experience substantial residential exposure to carcinogenic HAPs in US census tracts and in the US more generally.
Keywords: environmental injustice, Asian Americans, Hazardous Air Pollutants
Introduction
Air pollution is a significant international public health threat, causing more than seven million deaths per year. Outdoor air pollution exposure is linked with heart disease, stroke, respiratory diseases and cancer (World Health Organization, 2014). In cities and countries worldwide, the burden of outdoor environmental exposures is more often borne by low-income and minority people (Crouse, Ross, & Goldberg, 2009; Jephcote & Chen, 2013; Pearce, Richardson, Mitchell, & Shortt, 2011). In the United States, Black and Latino/a populations experience greater exposure to environmental toxics than do Whites (Bell & Ebisu, 2012; Clark, Millet, & Marshall, 2014; Jones et al., 2014; Mohai, Pellow, & Roberts, 2009). This uneven exposure is termed ‘environmental injustice’ and is a contributing factor to disparities in health (Coker et al., 2016; Payne-Sturges & Gee, 2006; Pearce et al., 2011). Asians are the fastest growing racial/ethnic group in the US (Pew Research Center, 2016), yet they have been underemphasized in previous studies of environmental health and injustice. Currently, there are over 18 million Asian Americans in the US. They comprise 6% of the total population and three-quarters of Asian adults are foreign-born (Pew Research Center, 2016).
The lack of attention paid to the environmental health of the nation’s fastest growing racial/ethnic group likely relates to the model minority label, which has been applied to Asian Americans, since they have the highest incomes and levels of education of all racial groups in the US. Specifically, half of Asian American adults have a college degree compared to one-quarter of all Americans, and their median annual household income is $66,000 compared to the national average of $49,800 (Pew Research Center, 2016). The model minority label was originally constructed in a context of Black-White race relations in the 1960s and used to undermine arguments for race-specific policies to promote the status of disadvantaged minorities (Yi, Kwon, Sacks, & Trinh-Shevrin, 2016). The claims underpinning the label are that the failures of non-Asian minorities are attributable to personal shortcomings, such as laziness, rather than socially-structured disadvantages, and that Asian minorities are hard-working individuals whose success reflects the unfettered opportunities available to everyone in the US.
The model minority label has diverted attention away from health disparities experienced by the Asian American population. For example, cancer is the leading cause of death for Asian Americans (CDC, 2010; Chen, 2005), yet physicians recommend preventative cancer screenings to Asian patients at a lower rate than other groups, in part because of the model minority stereotype (Ibaraki, Hall, & Sabin, 2014). The neglect of health disparities experienced by Asian Americans has only recently been highlighted in the political arena. In 2009, President Obama signed an Executive Order on the Asian community, which included calling for strategies to improve the health of Asian Americans and to redress health disparities impacting them (Obama, 2009).
It is likely that the model minority label has informed conventional wisdom within the research community regarding who in the US is likely to experience environmental health disparities. Asians are included less often than Blacks and Latinos/as in studies of environmental health disparities and injustice, based on the conventional presumption that they would have similar risk profiles to Whites. Sometimes, their population size in a given study area is too small for them to be considered. When Asians are examined, results indicate that they face higher risk from environmental health hazards than Whites (Clark et al., 2014; Cushing et al., 2015; Liam Downey, DuBois, Hawkins, & Walker, 2008; Houston, Li, & Wu, 2014; Lievanos, 2015; McKelvey et al., 2007; Morello-Frosch & Jesdale, 2006; Payne-Sturges & Gee, 2006) [see Jones et al. (2014) for an exception]. However, results indicative of disproportionate risk for Asian Americans have been de-emphasized in many studies.
The model minority label has obfuscated understanding of environmental health disparities experienced by Asian Americans in varied ways. First, the population-level statistics documenting high levels of education and income among Asian Americans conceal the systemic racism that Asians have experienced in the US over the past 150 years (Chou & Feagin, 2015). Greater recognition of this racism would lead to more research on its effects, including those related to environmental health.
Second, internalization of the model minority label by many Asian Americans has produced individuated understandings and experiences of racial oppression. As compared to Black Americans, Asian Americans more often suffer alone and in silence after being victims of discriminatory incidents, which disables them from collectively mobilizing based on their shared experiences of oppression (Chou & Feagin, 2015). In Black communities, there is a stronger collective memory of racism and resistance culture. This contributes to lower levels of social movement organizing by Asians as compared to Blacks (Chou & Feagin, 2015).
Third, the label was strategically created and circulated in the Civil Rights era in order to drive a wedge between other minorities and Asians, as dominant Whites upheld Asians as an example of minority success and evidence for the existence of equal opportunity (Yi et al., 2016). The logical extension of accepting this discourse as fact is that the prevalence of environmental health disparities among Asians in the US appears highly improbable (and, in any case, inexplicable), since it is taken for granted that Asian Americans share high status with Whites. Relatedly, it should be recognized that the environmental justice (EJ) movement itself—and the attendant research on environmental health disparities that the EJ movement spawned—is a political-racial project connecting Civil Rights concerns about racial equality to environmental conditions (Pulido, 1996). It should thus come as no surprise that the dominant framing of EJ in the US has been one of low-income Blacks, and more recently Latino/as, facing environmental injustices in their neighborhoods, with Whites being environmentally privileged. As a result, Asian EJ organizing has been poorly documented in the academic literature and rarely recognized by the wider EJ community, which Sze (2004) terms “the problem of Asian invisibility” (p. 155). In cities across the US, Asian communities have mobilized against hazards in their communities, winning a multilingual warning system and halting an expansion at a Chevron Refinery in Richmond, CA (Asian Pacific Environmental Network, 2012); saving Boston’s Chinatown from demise (Leong, 1995/1996); and providing emergency relief to Vietnamese Americans following Hurricane Katrina (Community-Wealth, 2017). While there is some evidence of Asian EJ activism, the lack of coverage of their organizing feeds back into a lack of focus on Asians in environmental health disparities research.
The discourse of Asians as a model minority group also masks substantial diversity that exists within the US Asian population, and may conceal disparate environmental health risks experienced by particular Asian subgroups. The importance of disaggregating the US Hispanic/Latino population in studies of environmental health disparities has been recognized, and significant differences in exposure to toxics have been uncovered between Latino/a subgroups (Chakraborty, Grineski, & Collins, 2017; Collins, Grineski, Chakraborty, & McDonald, 2011; Grineski, Collins, Chakraborty, & Montgomery, 2016; Grineski, Collins, & Chakraborty, 2013). In one of the only studies of its kind, Korean and Japanese women in California were found to face substantial exposure to mammary gland carcinogens in their neighborhoods, even though the risks for White women as compared to Asian women aggregated into one category were similar overall (Quach et al., 2014). Another study found that over 40% of the Japanese population and 30% of the Filipino population in the US lived in counties that exceed PM2.5 air quality standards; when aggregated together, they found that 20% of the US Asian population lived in exceedance counties (Gordon, Payne-Sturges, & Gee, 2010). Weaknesses in both of these studies include their bivariate study designs that did not adjust for other known factors influencing environmental exposures, e.g., population density and socioeconomic status, and their reliance on data from 2000.
This is the first study to focus on environmental health disparities among Asian Americans and Asian American subgroups in terms of cancer risks from HAPs. We conduct a national-level study at the census tract level using the recently released 2011 National Air Toxics Assessment. We assess the disproportionate risk of Asian Americans to carcinogenic HAPs before disaggregating the Asian category into ancestry, language and nativity subgroups in order to examine risk disparities exhibited within this heterogeneous population.
Materials and Methods
Study Population
We conducted our investigation across all 50 states and the District of Columbia using a set of socio-demographic variables derived from the 2010 Decennial Census and the 2008–2012 American Community Survey (ACS) estimates at the census tract level. To ensure stable proportions for all our variables, we use the 71,208 census tracts with at least 500 people, 200 households, and complete data for all analysis and clustering variables.
Assessment of Exposure to Carcinogenic HAPs
We used the US EPA’s 2011 National Air Toxics Assessment (NATA), which was released in 2015 (Environmental Protection Agency, 2016) to measure tract-level cancer risk exposure estimates in the US. The NATA includes 187 specific substances identified in the Clean Air Act Amendments of 1990 that are known or suspected causes of cancer and other serious health problems. Inputs on HAP emissions in the NATA come from the 2011 National Emissions Inventory and a multi-step methodology is used to generate estimates of cancer risk (Environmental Protection Agency, 2016). The 2011 NATA estimates potential cumulative risks to public health from HAP exposure following the EPA’s risk characterization guidelines that assume a lifelong exposure to 2011 levels of emissions. Cancer risks in the 2011 NATA, which we use here, are derived using unit risk estimates (URE), an upper bound estimate of an individual’s probability of contracting cancer over a lifetime of exposure to a concentration of one microgram of the pollutant per cubic meter of air. For each census tract, the individual lifetime cancer risk associated with each HAP is calculated by combining exposure concentration estimates with available UREs and inhalation reference concentrations. Although the type of cancer and available evidence varies by pollutant, the cancer risks of different HAPs are assumed to be additive and are summed to estimate an aggregate lifetime cancer risk for each census tract, measured in persons per million. These risk estimates are considered to be upper-bound estimates of the probability that an individual will contract cancer over a 70-year lifetime as a result of exposure to HAPs. A lifetime cancer risk of one in a million, for example, implies that one out of a million equally exposed people would contract cancer if exposed continuously to that specific concentration over 70 years. This would be an excess cancer risk in addition to other cancer risks borne by a person not exposed to these HAPs.
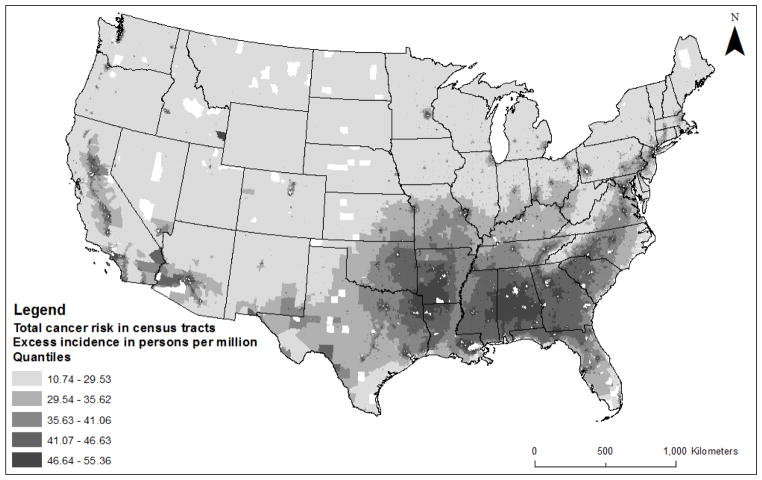
The 2011 NATA risk estimates for this study were obtained directly from the EPA for all census tracts (based on 2010 boundaries). Estimates of cumulative lifetime cancer risk (persons per million) include risks associated with inhalation exposure to HAPs released by major stationary sources (e.g., factories), smaller stationary sources (e.g., small manufacturers), on-road mobile sources (e.g., trucks), non-road mobile sources (e.g., trains, construction vehicles), and background concentrations (i.e., contributions from distant or natural sources). The NATA risk estimates do not consider residents’ length of residence in census tracts, nor do they consider the space-time patterning of residents’ movements across a range of outdoor and indoor environmental contexts within and beyond their census tracts of residence. Thus, while NATA risk estimates are quantified in terms of cumulative lifetime exposure to HAPs, for the purposes of this analysis, they provide estimates of relative cancer risk attributable to outdoor residential HAP exposures. Figure 1 is a map of the cancer risk dependent variable used in the multivariate analyses.
Figure 1.
Total estimated cancer risk for census tracts in the US, 2011
Note: The calculation of the quantiles includes analysis tracts in Alaska and Hawaii, which are not depicted in the map (see supplemental material). Tracts that were excluded due to missing data and small counts are not mapped.
Assessment of Tract-level Sociodemographics
To assess tract-level sociodemographic characteristics, we used the 2010 US Decennial Census to construct analysis variables whenever possible, since the Decennial Census includes the total population and is not a sample. To construct analysis variables that lacked corresponding data in the Decennial Census, we used 2012 American Community Survey (ACS) 5-year estimates, which center on 2010. These data are collected by the US Census Bureau, and are based on a sample of the population.
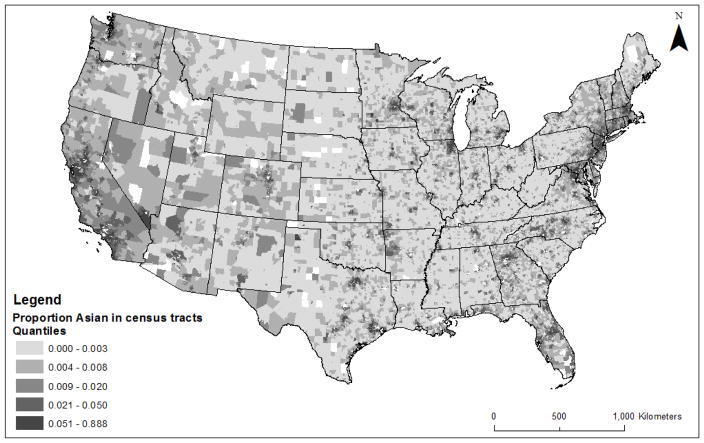
In terms of race/ethnicity, we analyzed seven indicators derived from Decennial Census data, including the proportions of census tract residents identified as being Hispanic or Latino (any race), White non-Hispanic, Black non-Hispanic, American Indian non-Hispanic, Pacific Islander/Native Hawaiian non-Hispanic, Multi-racial/Other non-Hispanic and Asian non-Hispanic (see Figure 2). Henceforth, we do not add “non-Hispanic” after every mention of the non-Hispanic racial/ethnic groups (e.g., we use the term “White”, instead of “White non-Hispanic”).
Figure 2.
Proportion non-Hispanic Asian residents in census tracts in the US, 2010
Note: The calculation of the quantiles includes analysis tracts in Alaska and Hawaii, which are not depicted in the map (see supplemental material). Tracts that were excluded due to missing data and small counts are not mapped.
We also examined several variables related to Asian ethnic heterogeneity, constructed from ACS data, including indicators of ancestry, language, and nativity. For ancestry, we used the coded open-ended responses to the ACS question “What is your ancestry or ethnic origin?”. The ACS codes responses into 18 categories for Asians. Based on small counts and regional similarities, we created seven ancestry categories: Chinese, South Asian (i.e., Indian, Pakistani, Bangladeshi, and Sri Lankan), Filipino, Southeast Asian (i.e., Cambodian, Laotian, Hmong, and Vietnamese), Korean, Japanese, and Other Asians (including Thai, Malaysian, Indonesian, and Taiwanese). Using census tract population counts for those Asian ancestry categories as numerators and the total tract population as the denominator, we constructed seven proportion variables. Note that these variables gauge ethnic identity and heritage rather than place of birth. For language, we used the proportion of the Asian alone population over age five that speaks another (not English) language. For nativity, we used the proportion of the Asian alone population in the tract that is foreign-born. These variables enable us to examine possible disparities in cancer risk from HAPs within the Asian population, based on ancestry, language, and immigrant vs. US-born status.
We also adjusted for the effects of other variables commonly included in quantitative EJ studies. For socioeconomic status (SES), we included median household income from the ACS and the proportion of renter-occupied housing units from the Decennial Census. We included median income, which maps to wealth, power and political clout (Mohai & Saha, 2006); we also included median income squared in the model because the relationship between income and hazard exposure may be curvilinear. This is because low income neighborhoods tend to have fewer economic activities and hence fewer sources of pollution, while high income neighborhoods typically have the political power to resist pollution sources; thus, more air pollution risks are expected in middle income neighborhoods (Pastor, Morello-Frosch, & Sadd, 2005). While education is an important component of SES, an education variable (e.g., percent with a high school diploma or less) was not included as a separate indicator in this study due to collinearity with income. Instead, we conducted a sensitivity analysis using a SES factor combining income and education. Housing tenure was included because renter occupancy indicates greater housing instability, political disengagement, and reduced household resources compared to owner occupancy (Chakraborty, Collins, Montgomery, Grineski, & Hernandez, 2014; Pastor et al., 2005).
We adjusted for crude population density, which was calculated by dividing the total census tract population for 2010 by the area of the tract in square kilometers, because densely populated areas are more likely to contain emission-generating activities that increase estimates of cancer risk from HAPs (Chakraborty et al., 2014). Finally, we included a dichotomous urban location variable given that pollution risks tend to be higher in urban areas. After creating a percent urban housing units variable using Decennial Census data, we employed k-means cluster analysis to naturally break census tracts between urban vs. rural categories. Descriptive statistics of all analysis variables are included in Table 1.
Table 1.
Descriptive statistics for census tracts in the United States (n=71,208)
| Variables | N | Min. | Max. | Mean | Std. Deviation |
|---|---|---|---|---|---|
| DEPENDENT VARIABLE | |||||
| Total Cancer Risk (excess incidence due to HAPs per million) | 71208 | 10.742 | 826.309 | 40.118 | 12.545 |
| INDEPENDENT VARIABLES | |||||
| Median Household Income | 71208 | 4092 | 247064 | 56342 | 27463 |
| Proportion of occupied housing units that are rented | 71208 | 0.005 | 1.000 | 0.356 | 0.222 |
| Proportion of population that is White | 71208 | 0.000 | 0.997 | 0.640 | 0.302 |
| Proportion of population that is Hispanic | 71208 | 0.000 | 0.994 | 0.153 | 0.209 |
| Proportion of population that is Black | 71208 | 0.000 | 0.992 | 0.134 | 0.220 |
| Proportion of population that is American Indian | 71208 | 0.000 | 0.982 | 0.008 | 0.045 |
| Proportion of population that is Asian | 71208 | 0.000 | 0.898 | 0.043 | 0.083 |
| Proportion of population that is Pacific Islander or Hawaiian Native | 71208 | 0.000 | 0.716 | 0.001 | 0.009 |
| Proportion of population that is multi-racial or other race | 71208 | 0.000 | 0.248 | 0.003 | 0.010 |
| Population Density (people per km2) | 71208 | 0.012 | 196419 | 2021 | 4555 |
| Urban Location | 71208 | 0 | 1 | 0.797 | 0.403 |
| Asian Ancestry Groups | |||||
| Proportion of population that is Chinese | 71208 | 0.000 | 1.000 | 0.010 | 0.038 |
| Proportion of population that is South Asian | 71208 | 0.000 | 0.702 | 0.010 | 0.029 |
| Proportion of population that is Filipino | 71208 | 0.000 | 0.893 | 0.007 | 0.025 |
| Proportion of population that is Southeast Asian | 71208 | 0.000 | 0.639 | 0.007 | 0.024 |
| Proportion of population that is Korean | 71208 | 0.000 | 0.582 | 0.004 | 0.017 |
| Proportion of population that is Japanese | 71208 | 0.000 | 0.521 | 0.002 | 0.014 |
| Proportion of population that is Other Asian | 71208 | 0.000 | 0.248 | 0.003 | 0.010 |
| Asian Language and Nativity Variables | |||||
| Proportion of Asians over 5 that speak a non-English language | 71208 | 0.000 | 1.000 | 0.527 | 0.402 |
| Proportion of Asians that are foreign-born | 71208 | 0.000 | 1.000 | 0.538 | 0.375 |
Statistical Analysis
We began by calculating national population-weighted mean cancer risks for race/ethnicity and ancestry groups by multiplying the number of people in each race/ethnicity and ancestry group by the cancer risk value in each tract, and then summing those values and dividing by the total US population in that group (Clark et al., 2014). Then, we specified four generalized estimating equations (GEEs). GEEs expand the generalized liner model to accommodate clustered data (Liang & Zeger, 1986; Nelder & Wedderburn, 1972; Zeger & Liang, 1986). We defined clusters of census tracts based on median year of housing construction (“2000 or later”, “1990 to 1999”, “1980 to 1989”, “1970 to 1979”, “1960 to 1969”, “1950 to 1959”, “1940 to 1949”, and “1939 or earlier”) by county (n=3,101), which yielded 10,455 clusters. This cluster definition method was selected because it corresponds with temporal dimensions of the built-environment across urban space that are associated with the historical-geographical formation of environmental injustice (Bolin, Grineski, & Collins, 2005; Pulido, 2000) and a similar approach has been used previously in similar studies (Collins, Grineski, & Chakraborty, 2015; Collins, Grineski, Chakraborty, Hernandez, & Montgomery, 2015).
GEEs also require the specification of an intracluster dependency correlation matrix (Liang & Zeger, 1986; Zeger & Liang, 1986). Three correlation structure specifications were substantive candidates (Garson, 2012): (1) independent, which assumes the nonexistence of dependency, so that all off-diagonal elements of the working correlation matrix are zero; and (2) exchangeable, which assumes constant intracluster dependency, so that all the off-diagonal elements of the correlation matrix are equal and (3) unstructured, which assumes a completely general correlation matrix, which is estimated without constraints. We modeled all GEEs (outlined below) with the three matrices, using goodness-of-fit coefficients to determine the best specification (Garson, 2012). The exchangeable specification performed better than the independent and unstructured, and so all reported results use that specification.
Model 1 is a traditional EJ model that includes the proportion of tract residents in each racial/ethnic minority group, socioeconomic status, population density, and urban location. The race/ethnicity covariates can be interpreted relative to proportional changes in the White population. In Model 2, we added the seven Asian ancestry proportion variables in place of proportion Asian and those coefficients are interpretable relative to proportional changes in the White population. Model 3 includes the language variable, and so proportion White is added and proportion Asian is removed to make the race/ethnicity covariates and language variable interpretable relative to the proportion of Asians that speak a non-English language. Model 4 includes the proportion of Asians that are foreign-born, in place of the language variable, and the covariates can be interpreted in the same way as in Model 3.
To select the best fitting models, we estimated a series of GEEs by varying the model specifications. We tested normal, gamma and inverse Gaussian distributions with logarithmic and identity link functions. Visual inspection of a histogram of our dependent variable suggested that these were the most appropriate options, given that the dependent variable was not normally distributed. For these four models, the inverse Gaussian distribution with an identity link function was the best fitting. Finally, we examined possible multicollinearity among the analysis variables; based on variance inflation factor, tolerance, and condition index criteria, inferences from the GEEs are not affected by multicollinearity. All independent variables were standardized before inclusion in the GEEs in order to make coefficients directly comparable. We define statistical significance as p<.001, due to the large sample.
Results
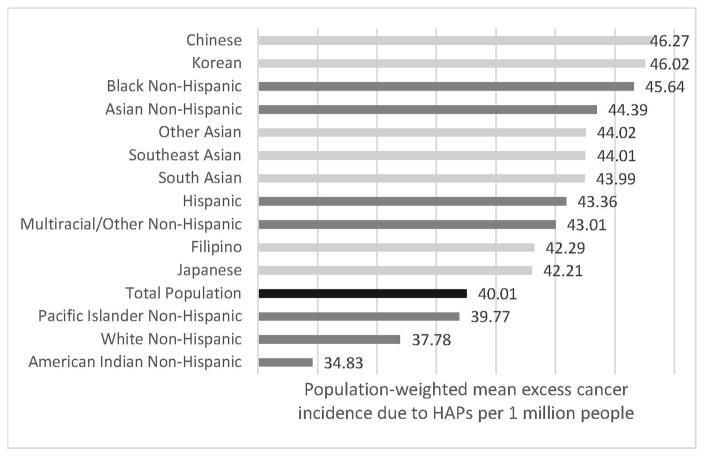
Figure 3 reports population-weighted mean cancer risk from HAPs by racial/ethnic and Asian ancestry group. The mean excess cancer incidence attributable to ambient HAP exposures in the census tract of residence for Asian people in the United States is 44.4 per 1 million, which ranks them second of the seven racial/ethnic groupings (see the dark gray bars in Figure 3) and above the US mean (see black bar in Figure 3). Blacks face the highest risk in the United States and Hispanics the third highest. When considering the Asian ancestry groups (see the light gray bars in Figure 3), both Chinese and Korean populations face greater risks than Blacks in the US. After Blacks, ‘other’ Asians, Southeast Asians and South Asians face the next highest risks, ranking above Hispanics. All Asian ancestry subgroups are above the US mean.
Figure 3.
Population-weighted estimated mean excess cancer incidence due to HAPs by racial/ethnic and Asian ancestry group in the US, 2011
Note: The black bar represents the national average. Dark gray bars represent broad racial/ethnic classifications and light gray bars represent Asian ancestry groups.
Table 2 reports the GEE results for Models 1 and 2. In Model 1, as the proportion of Asian, Black and Hispanic residents in a neighborhood increases relative to the proportion White, cancer risk from HAPs increase significantly. Specifically, a one standard deviation increase (i.e., ~8%) in proportion Asian is associated with HAP cancer incidence risks that are 0.95 (95% CI: 0.76,1.14) persons per million greater than other census tracts, adjusting for the other variables and clustering. As the proportion of American Indian individuals and the proportion of Pacific Islanders/Native Hawaiians increases in a neighborhood, risk decreases significantly. The coefficient for Multiracial/other is also negative but not statistically significant. In terms of the control variables, income is negative and not significantly associated with risk, although the quadratic term suggests a non-linear association. The proportion of renter-occupants is positively and significantly associated with risk, as is residence in a predominately urban (vs. rural) tract. Population density is the strongest predictor, with more densely populated tracts facing greater risk. Urban, Black, Rented, and Asian are the next four strongest predictors of cancer risk. In terms of ancestry (Model 2), increases in the proportions of Chinese, South Asian, and Korean residents (relative to the proportion White) are significantly associated with greater cancer risk from HAPs, while relationships for the other groups are not statistically significant.
Table 2.
GEE results for Models 1 and 2: Traditional environmental justice model (1) and Asian ancestry model (2) for census tracts in the United States (n=71,208)
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| B (95% Confidence Interval) | SE | Sig. | B (95% Confidence Interval) | SE | Sig. | |
| Intercept | 35.471 (35.097, 35.846) | 0.191 | ** | 35.383 (35.007, 35.759) | 0.192 | ** |
| Income | −0.351 (−0.695, 0.065) | 0.194 | −0.293 (−0.673, 0.086) | 0.194 | ||
| Income Squared | 0.672 (0.381, 0.963) | 0.149 | ** | 0.632 (0.340, 0.923) | 0.149 | ** |
| Prop. Rented | 1.376 (1.185, 1.567) | 0.097 | ** | 1.356 (1.164, 1.549) | 0.098 | ** |
| Prop. Hispanic | 0.735 (0.545, 0.926) | 0.097 | ** | 0.750 (0.561, 0.939) | 0.097 | ** |
| Prop. Black | 1.801 (1.554, 2.047) | 0.126 | ** | 1.787 (1.539, 2.035) | 0.127 | ** |
| Prop. American Indian | −0.362 (−0.428, −0.296) | 0.034 | ** | −0.364 (−0.430, −0.298) | 0.034 | ** |
| Prop. Pacific Islander/Nat Hawaiian | −0.103 (−0.165, −0.041) | 0.032 | ** | −0.078 (−0.144, −0.012) | 0.034 | |
| Prop. Multiracial/Other | −0.081 (−0.171, 0.010) | 0.046 | −0.076 (−0.167, 0.015) | 0.046 | ||
| Prop. Asian | 0.952 (0.761, 1.143) | 0.097 | ** | NA | NA | NA |
| Pop Density | 5.508 (4.665, 6.351) | 0.431 | ** | 5.533 (4.684, 6.383) | 0.434 | ** |
| Urban Location | 4.776 (4.554, 4.998) | 0.113 | ** | 4.826 (4.604, 5.048) | 0.113 | ** |
| Prop. Chinese | 0.394 (0.244, 0.545) | 0.077 | ** | |||
| Prop. South Asian | 0.332 (0.240 0.424) | 0.047 | ** | |||
| Prop. Filipino | 0.094 (0.003, 0.184) | 0.046 | ||||
| Prop. Southeast Asian | 0.052 (−0.026, 0.130) | 0.040 | ||||
| Prop. Japanese | 0.004 (−0.127, 0.134) | 0.067 | ||||
| Prop. Korean | 0.413 (0.299 0.527) | 0.058 | ** | |||
| Prop. Other Asian | 0.053 (−0.009, 0.115) | 0.032 | ||||
Note:
p<.001; Models use an inverse Gaussian distribution with identity link and exchangeable correlation matrix. All independent variables are standardized, except Urban Location.
Table 3 presents results for Models 3 and 4. An increase in the proportion of Asians who speak a non-English language relative to those who do not (Model 3) and a decrease in the proportion of Asians who are foreign-born relative to US-born (Model 4) were significantly associated with increased cancer risk from HAPs.
Table 3.
GEE Results for Models 3 and 4: Asian-specific models for language (3) and nativity (4) for census tracts in the United States (n=71,208)
| Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|
| B (95% Confidence Interval) | SE | Sig. | B (95% Confidence Interval) | SE | Sig. | |
| Intercept | 35.562 (35.189, 35.936) | 0.191 | ** | 35.527 (35.152, 35.902) | 0.191 | ** |
| Income | −0.378 (−0.759, 0.002) | 0.194 | −0.288 (−0.667, 0.090) | 0.193 | ||
| Income Squared | 0.714 (0.423, 1.006) | 0.149 | ** | 0.657 (0.367, 0.947) | 0.148 | ** |
| Prop. Rented | 1.324 (1.131,1.517) | 0.099 | ** | 1.350 (1.157,1.542) | 0.098 | ** |
| Prop. Hispanic | −1.673 (−2.174,−1.173) | 0.255 | ** | −1.776 (−2.281,−1.272) | 0.258 | ** |
| Prop. Black | −0.760 (−1.303, −0.216 | 0.277 | −.0888 (−1.434, −0.342 | 0.279 | ** | |
| Prop. American Indian | −0.911 (−1.032, −0.790) | 0.062 | ** | −0.932 (−1.054, −0.811) | 0.062 | ** |
| Prop. Pacific Islander/Nat Hawaiian | −0.265 (−0.345, −0.184) | 0.041 | ** | −.0270 (−0.352, −0.188) | 0.042 | ** |
| Prop. Multiracial/Other | −0.178 (−0.268, −0.088) | 0.046 | ** | −0.177 (−0.269, −0.084) | 0.047 | ** |
| Pop Density | 5.509 (4.669, 6.348) | 0.428 | ** | 5.530 (4.691, 6.369) | 0.428 | ** |
| Urban | 4.702 (4.482, 4.923) | 0.113 | ** | 4.758 (4.536, 4.979) | 0.113 | ** |
| Prop. White | −3.532 (−4.201, −2.862) | 0.341 | ** | −3.698 (−4.372, −3.042) | 0.344 | ** |
| Asian: Non-English language | 0.105 (0.045, 0.165) | 0.031 | ** | NA | NA | NA |
| Asian: Foreign-born | NA | NA | NA | −0.110 (−0.169, −0.050) | 0.030 | ** |
Note:
p<.001; Models use an inverse Gaussian distribution with identity link and exchangeable correlation matrix. All independent variables are standardized, except Urban Location.
As a sensitivity analysis, we ran the models without the clustering variables and found that the findings were generally consistent but more statistically significant, indicating that controlling for clustering produced more conservative estimates of relationships with HAP cancer risk. We also ran the models using the factor combining income and education. Results were nearly identical in terms of significance, suggesting that the findings are not sensitive to how SES is measured. There were three minor differences: in Model 1, Pacific Islander drops from p<0.001 to p=0.003; in Model 3, black becomes significant at p<0.001 instead of p=0.002; and in Model 4, foreign-born reduces in significance to p<0.01 from p<0.001.
Discussion
This is the first focused examination of Asian Americans and distributive EJ in the US. The unadjusted and multivariate analyses reveal that Asians experience significant environmental health injustices nationwide, in terms of facing disparate residential exposures to carcinogenic HAPs. It is not simply the case that Asians face greater exposure to cancer-causing chemicals than Whites; they also face greater risks than Hispanics and have similar but slightly lower risks than Blacks. Nonetheless, they have been largely overlooked within the EJ movement and within the EJ research community (Sze, 2004). The lack of research on Asian Americans’ environmental health makes us unable to determine if this pattern of disparate risk would be found nationwide for other environmental health hazards, such as respiratory toxics and diesel particulate matter, or for occupational exposures, which are beyond the scope of this study.
There are likely health consequences of unequal exposures to environmental health hazards for Asian Americans (Gordon et al., 2010). While heart disease is the leading cause of death in the US, cancer is the leading cause of death for Asian Americans (CDC, 2010). While some cancers known to impact Asians are less linked to air pollution (e.g., liver, stomach), lung cancer and breast cancer, which are among the leading causes of cancer death for Asians (Torre et al., 2016), have been linked to environmental conditions (Crouse, Goldberg, Ross, Chen, & Labrèche, 2010; Fajersztajn, Veras, Barrozo, & Saldiva, 2013). Many Asian Americans also face unhealthy levels of stress in their daily lives due to being the “model minority” as well as frequent victims of discriminatory acts (Chou & Feagin, 2015; Gee, Spencer, Chen, Yip, & Takeuchi, 2007). Stress can synergize with environmental exposures to worsen health (Gee & Payne-Sturges, 2004).
The Importance of Asian Ancestry
While Asian Americans as a group are burdened by cancer-causing HAPs independent of their ancestry, specific ancestry groups face heightened risks. Chinese, Korean, and South Asian Americans are associated with disproportionate risk across both analyses (Figure 3, Table 2). Southeast Asians have high risk, i.e., they were just behind Chinese and Koreans in the unadjusted analyses (Figure 3), but their coefficient is not significant in the multivariate analysis (Table 2). The differences between the two sets of results relate to the unit of analysis (individuals vs. census tracts) and the addition of control variables in the multivariate model. While findings indicate that these groups experience disparate risks, possible explanations for the processes contributing to those disparate risks differ between ancestry groups.
The Chinese have the highest risk from carcinogenic HAPs of all groups included in the unadjusted analysis and they also have the second strongest association with HAP risk (i.e., second largest “B”) as compared to the other Asian ancestry groups in the multivariate model (Table 2). These findings are particularly troubling because the Chinese are the largest Asian ancestry group in the US. It is possible that their actual exposure is less than estimated, since emerging evidence from Los Angeles and Chicago shows that older Chinese adults spend less time outside than Black, White and Hispanic adults (Spalt et al., 2016). However, when examining blood concentrations of heavy metals, Chinese adults had higher levels compared to other racial/ethnic groups (McKelvey et al., 2007) and Chinese women face notably high rates of lung cancer, given their low rates of smoking (Torre et al., 2016). The risk for Chinese people uncovered in this study likely relates to their longstanding urban settlement in the US, racism and discrimination, and their continued desire to live near co-ethnics. Analyses of Chinese settlement in California have shown that even Chinese immigrants who are financially able to residentially integrate into other neighborhoods often choose to live among others of the same ethnicity. This means that Chinese immigrants’ first neighborhood of residence is often their final, desired destination (Walton, 2015) and Chinese immigrants usually settle in urban contexts (Zhou, Tseng, & Kim, 2008). Although some highly educated new Chinese immigrants bypass inner cities to settle in the suburbs, traditional Chinatowns continue to receive newcomers and have expanded in recent years (Lin, 1998; Zhou et al., 2008). The long history of Chinese settlement in the US, combined with historical discrimination against Chinese people (Tsai, 1986), means that ‘Chinatowns’ are often in polluted central city districts.
Korean Americans have the second highest risk from carcinogenic HAPs of all groups (Figure 3) and the strongest association with HAP risk (i.e., largest “B”) as compared to the other Asian ancestry groups (Table 2). There are distinctive reasons for the high risk experienced by Koreans, which were also noted in a California study (Quach et al., 2014). Koreans have tended to settle in poor, commercially underserved, central city neighborhoods, where they operate small businesses (Lee, 2000). Entrepreneurship has contributed to their upward social mobility (Lee, 2000), but their high risk suggests that it has come with an environmental health consequence of heightened residential exposure to carcinogenic HAPs.
Risks for South Asians (Figure 3 and Table 2) likely stem from their immigrant status and engagement in the science and engineering sectors. For example, 87% of South Indian adults are foreign-born and one-third are employed in science and engineering fields (Pew Research Center, 2016). Given that South Asians make up a sizable segment of the science and engineering workforce in the US and are continually migrating to the US to work, it stands to reason that they may be exposed to HAPs due to their desire to live near industrial and tech facilities where they may be employed.
Amplified cancer risks from HAPs among Southeast Asians (Figure 3) derive in part from their status as refugees upon entry to the US (Rumbaut, 2000). Refugees tend to settle in more socially disadvantaged neighborhoods than voluntary migrants (Phillip, 2010). Compared to other Asian Americans, Southeast Asians are more likely to be supported by government assistance programs, have minimum wage jobs, and work in the informal economy (Rumbaut, 2000). Their socioeconomic marginality and reliance on government assistance may lead them to highly polluted, central-city neighborhoods.
Japanese Americans appear to be relatively protected against cancer risks as compared to the other groups, although their unadjusted risk is higher than Whites (Figure 3). Their relative safety may be an outcome of the displacement and forced internment of Japanese Americans during World War II. After the War, the Japanese were dispersed throughout the US (Cho, Gimpel, & Dyck, 2006; Daniels, 2011). Filipinos have similar overall risks to the Japanese, which puts them on the low end of risk among Asians but still higher than Whites.
The Importance of Language and US Nativity
Higher proportions of Asians speaking a language other than English and lower proportions of Asians who were foreign-born are important dimensions of social difference linked to greater cancer risk from air pollution. Speaking a language other than English was also a risk factor for exposure to air toxics in Hispanic populations in the immigrant gateways of El Paso, Texas (Collins et al., 2011) and Miami, Florida (Chakraborty et al., 2017). Speaking a non-English language may make it difficult for people to participate in environmental decision-making processes, which are traditionally English-only. In the case of nativity, researchers found that foreign-born Hispanics were at disproportionate risk (Chakraborty et al., 2017; Collins et al., 2011; Grineski et al., 2016), which is opposite of what we find here for Asians. While this pattern would likely vary based on ancestry group (e.g., between elite Cubans and poor Vietnamese refugees), the nativity divergence may more generally relate to the socially marginal status of Hispanic immigrants and the relatively elite status of well-educated Asian immigrants. The risk disparities based on nativity suggest that intergenerational adjustment to life in the US is actually associated with heightened risk for Asian Americans. This indicates that upward social mobility associated with longer term residence in the US may not protect Asian Americans from exposure to cancer-causing HAPs, as it may for Latino/as. These two findings for Asians taken together suggest that multigenerational Asian Americans may experience relatively high cancer risk to HAPs by remaining in the same (centrally located, ethnic enclave) neighborhoods as their immigrant parents and grandparents, while remaining linguistically connected with their ancestral roots.
Limitations and Future Directions
This study is limited by the modifiable areal unit problem, which arises when the boundaries of the unit of analysis are modifiable and to some degree arbitrary (Fotheringham & Wong, 1991), e.g., census tracts. Sensitivity analyses show that changing the way data are aggregated can affect findings (Downey, 2006). We assumed, as is the convention in air pollution epidemiology, that residential outdoor HAPs are good proxies for individual exposure, even though most people spend the majority of their time indoors and how pollution infiltrates homes varies by location and season (Spalt et al., 2016). Future studies should use individual-level data and incorporate understanding of people’s time-location patterns. Another limitation is our focus only on cancer-causing HAPs, even though HAPs can harm neurological, reproductive and respiratory systems. Related to the respiratory system, Asian Americans have rates of asthma that are similar to Whites, but Asians of Japanese and Filipino descent have significantly higher rates of asthma (Gordon et al., 2010), as do US-born Asians (Brugge, Lee, Woodin, & Rioux, 2007). The component of these elevated rates attributable to environmental exposures has not yet been investigated, but should be in future studies. Finally, future studies of factors that might reduce the cancer burden for Asian Americans should examine unequal exposure to HAPs, since smoking cessation, improved diets, more exercise, and reduced barriers to screening are more often the focus of those efforts (Chen, 2005).
Conclusions
Nationally, Chinese and Korean populations experience the greatest mean cancer risks due to HAPs, followed by the Black population. Multivariate results reveal an association between higher proportions of Asian Americans in neighborhoods and greater exposure to carcinogenic HAPs. Neighborhoods with greater proportions Chinese, Korean, and South Asian Americans are also at increased risk, as are neighborhoods with greater proportions of Asians speaking a non-English language and US-born Asians. It seems that the model minority myth has exerted power over inquiry within the environmental health and EJ research communities, as analytical attention has long been diverted away from Asian Americans. These findings highlight the significant environmental health disparities experienced by Asian Americans, which have been previously overlooked, and speak to the urgent need to address them.
Supplementary Material
Research Highlights.
Asians have been underemphasized in previous studies of environmental injustice
Chinese and Korean Americans face notably high air pollution risks
Higher % Asian in census tracts is associated with greater air pollution risks
Tracts with higher % of US-born Asians have greater air pollution risks
Tracts with higher % Asians not speaking only English have greater pollution risks
Acknowledgments
Research reported in this paper was supported by the National Institute of General Medical Sciences of the National Institutes of Health under linked Award Numbers RL5GM118969, TL4GM118971, and UL1GM118970. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sara E. Grineski, Professor of Sociology, Department of Sociology and Anthropology & BUILDing SCHOLARS, University of Texas at El Paso, 500 W. University Ave., El Paso, TX, USA
Timothy W. Collins, Professor of Geography, Department of Sociology and Anthropology & BUILDing SCHOLARS, University of Texas at El Paso, 500 W. University Ave., El Paso, TX, USA
Danielle X. Morales, Postdoctoral Fellow, Department of Sociology and Anthropology & BUILDing SCHOLARS, University of Texas at El Paso, 500 W. University Ave., El Paso, TX, USA
References
- Asian Pacific Environmental Network. Richmond. 2012 Retrieved from http://apen4ej.org/what-we-do/organizing/Richmond/
- Bell ML, Ebisu K. Environmental Inequality in Exposures to Airborne Particulate Matter Components in the United States. Environmental Health Perspectives. 2012;120(12):1699–1704. doi: 10.1289/ehp.1205201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolin B, Grineski S, Collins T. Geography of Despair: Environmental Racism and the Making of South Phoenix, Arizona, USA. Human Ecology Review. 2005;12(2):155–167. [Google Scholar]
- Brugge D, Lee AC, Woodin M, Rioux C. Native and foreign born as predictors of pediatric asthma in an Asian immigrant population: a cross sectional survey. Environmental Health. 2007;6(13) doi: 10.1186/1476-1069X-1186-1113.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Leading Causes of Death by Age Group, Race/Ethnicity Males, United States, 2010. 2010 Retrieved from https://www.cdc.gov/men/lcod/2010/lcodrace_ethnicitymen2010.pdf.
- Chakraborty J, Collins TW, Montgomery MC, Grineski SE, Hernandez M. Comparing Disproportionate Exposure to Acute and Chronic Pollution Risks: A Case Study in Houston, Texas. Risk Analysis. 2014;34(11):2005–2020. doi: 10.1111/risa.12224. [DOI] [PubMed] [Google Scholar]
- Chakraborty J, Grineski SE, Collins TW. Cancer risks from exposure to vehicular air pollution: a household level analysis of intra-ethnic heterogeneity in Miami, Florida. Urban Geography. 2017;38(1):112–136. [Google Scholar]
- Chen MS. Cancer Health Disparities among Asian Americans. Cancer. 2005;104(12):2895–2903. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- Cho WKT, Gimpel JG, Dyck JJ. Residential Concentration, Political Socialization, and Voter Turnout. The Journal of Politics. 2006;68(1):156–167. [Google Scholar]
- Chou RS, Feagin JR. Myth of the model minority: Asian Americans facing racism. Boulder, CO: Paradigm Publishers; 2015. [Google Scholar]
- Clark LP, Millet DB, Marshall JD. National Patterns in Environmental Injustice and Inequality: Outdoor NO2 Air Pollution in the United States. Plos One. 2014;9(4) doi: 10.1371/journal.pone.0094431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker E, Liverani S, Ghosh JK, Jerrett M, Beckerman B, Li A, … Molitor J. Multi-pollutant exposure profiles associated with term low birth weight in Los Angeles County. Environment International. 2016;91:1–13. doi: 10.1016/j.envint.2016.02.011. [DOI] [PubMed] [Google Scholar]
- Collins T, Grineski S, Chakraborty J, McDonald Y. Understanding environmental health inequalities through comparative intracategorical analysis: Racial/ethnic disparities in cancer risks from air toxics in El Paso County, Texas. Health and Place. 2011;17:335–344. doi: 10.1016/j.healthplace.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Collins TW, Grineski SE, Chakraborty J. Household-level disparities in cancer risks from vehicular air pollution in Miami. Environmental Research Letters. 2015;10:095008. [Google Scholar]
- Collins TW, Grineski SE, Chakraborty J, Hernandez M, Montgomery MC. Downscaling environmental justice analysis: Determinants of household-level hazardous air pollutant exposure in Greater Houston. Annals of the Association of American Geographers. 2015;105(4):684–703. [Google Scholar]
- Community-Wealth. Mary Queen of Vietnam Community Development Corporation. 2017 Retrieved from http://community-wealth.org/content/mary-queen-vietnam-cdc.
- Crouse DL, Goldberg MS, Ross NA, Chen H, Labrèche F. Postmenopausal breast cancer is associated with exposure to traffic-related air pollution in Montreal, Canada: a case-control study. Environmental Health Perspectives. 2010;118(11):1578. doi: 10.1289/ehp.1002221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Ross NA, Goldberg MS. Double burden of deprivation and high concentrations of ambient air pollution at the neighbourhood scale in Montreal, Canada. Social Science & Medicine. 2009;69(6):971–981. doi: 10.1016/j.socscimed.2009.07.010. [DOI] [PubMed] [Google Scholar]
- Cushing L, Faust J, August LM, Cendak R, Wieland W, Alexeeff G. Racial/Ethnic Disparities in Cumulative Environmental Health Impacts in California: Evidence From a Statewide Environmental Justice Screening Tool (CalEnviroScreen 1.1) American Journal of Public Health. 2015;105(11):2341–2348. doi: 10.2105/AJPH.2015.302643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniels R. Asian America: Chinese and Japanese in the United States Since 1850. Seattle: University of Washington Press; 2011. [Google Scholar]
- Downey L. Using geographic information systems to reconceptualize spatial relationships and ecological context. American Journal of Sociology. 2006;112(2):567–612. doi: 10.1086/506418?origin=JSTOR-pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey L, DuBois S, Hawkins B, Walker M. Environmental Inequality in Metropolitan America. Organization & Environment. 2008;21(3) doi: 10.1177/1086026608321327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Environmental Protection Agency. 2011 NATA: Assessment Results. 2016 Retrieved from https://www.epa.gov/national-air-toxics-assessment/2011-nata-assessment-results.
- Fajersztajn L, Veras M, Barrozo LV, Saldiva P. Air pollution: a potentially modifiable risk factor for lung cancer. Nature Reviews Cancer. 2013;13(9):674–678. doi: 10.1038/nrc3572. [DOI] [PubMed] [Google Scholar]
- Fotheringham AS, Wong DWS. The modifiable areal unit problem in multivariate statistical analysis. Environment and Planning A. 1991;7(23):1025–1044. [Google Scholar]
- Garson G. Generalized linear models and generalized estimating equations. Asheboro, NC: Statistical Associates Publishing; 2012. [Google Scholar]
- Gee GC, Payne-Sturges D. Environmental Health Disparities: A Framework Integrating Psychosocial and Environmental Concepts. Environmental Health Perspectives. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. The association between self-reported racial discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Social Science & Medicine. 2007;64(10):1984–1996. doi: 10.1016/j.socscimed.2007.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon L, Payne-Sturges D, Gee G. Environmental Health Disparities: Select Care Studies Related to Asian and Pacific Islander Americans. Environmental Justice. 2010;3(1):21–27. [Google Scholar]
- Grineski SE, Collins T, Chakraborty J, Montgomery MC. Hazard Characteristics and Patterns of Environmental Injustice: Household-level Determinants of Environmental Risk in Miami, Florida. Risk Analysis. 2016 doi: 10.1111/risa.12706. [DOI] [PubMed] [Google Scholar]
- Grineski SE, Collins TW, Chakraborty J. Hispanic heterogeneity and environmental injustice: Intra-ethnic patterns of exposure to cancer risks from vehicular air pollution in Miami. Population and Environment. 2013;35(1):26–44. doi: 10.1007/s11111-012-0184-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston D, Li W, Wu J. Disparities in Exposure to Automobile and Truck Traffic and Vehicle Emissions Near the Los Angeles-Long Beach Port Complex. American Journal of Public Health. 2014;104(1):156–164. doi: 10.2105/AJPH.2012.301120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibaraki AY, Hall GCN, Sabin JA. Asian American Cancer Disparities: The Potential Effects of Model Minority Health Stereotypes. Asian American Journal of Psychology. 2014;5(1):75–81. [Google Scholar]
- Jephcote C, Chen HB. Geospatial analysis of naturally occurring boundaries in road-transport emissions and children's respiratory health across a demographically diverse cityscape. Social Science & Medicine. 2013;82:87–99. doi: 10.1016/j.socscimed.2013.01.030. [DOI] [PubMed] [Google Scholar]
- Jones MR, Diez-Roux AV, Hajat A, Kershaw KN, O'Neill MS, Guallar E, … Navas-Acien A. Race/Ethnicity, Residential Segregation, and Exposure to Ambient Air Pollution: The Multi-Ethnic Study of Atherosclerosis (MESA) American Journal of Public Health. 2014;104(11):2130–2137. doi: 10.2105/AJPH.2014.302135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J. Striving for the American Dream: Struggle, Success, and Intergroup Conflict among Korean Immigrant Entrepreneurs. In: Zhou M, Gatewood JV, editors. Contemporary Asian America. New York: New York University Press; 2000. pp. 278–294. [Google Scholar]
- Leong A. The struggle over parcel C: How Boston’s Chinatown won a victory in the fight against institutional expansionism and environmental racism. Amerasia Journal. 1995/1996;21(3):99–119. [Google Scholar]
- Liang K, Zeger S. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lievanos RS. Race, deprivation, and immigrant isolation: The spatial demography of air-toxic clusters in the continental United States. Social Science Research. 2015;54:50–67. doi: 10.1016/j.ssresearch.2015.06.014. [DOI] [PubMed] [Google Scholar]
- Lin J. Reconstructing Chinatown: Ethnic Enclaves and Global Change. Vol. 2. Minneapolis, MN: University of Minnesota Press; 1998. [Google Scholar]
- McKelvey WR, Gwynn C, Jeffery N, Kass D, Thorpe LE, Garg RK, … Parsons PJ. A biomonitoring study of lead, cadmium, and mercury in the blood of New York city adults. Environmental Health Perspectives. 2007;115(10):1435–1441. doi: 10.1289/ehp.10056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohai P, Pellow DN, Roberts JT. Environmental Justice. Annual Review of Environment and Resources. 2009;34:405–430. [Google Scholar]
- Mohai P, Saha R. Reassessing racial and socioeconomic disparities in environmental justice research. Demography. 2006;43(2):383–399. doi: 10.1353/dem.2006.0017. [DOI] [PubMed] [Google Scholar]
- Morello-Frosch R, Jesdale BM. Separate and unequal: Residential segregation and estimated cancer risks associated with ambient air toxics in US metropolitan areas. Environmental Health Perspectives. 2006;114(3):386–393. doi: 10.1289/ehp.8500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelder J, Wedderburn R. Generalized linear models. Journal of the Royal Statistical Society, Series A. 1972;135:370–384. [Google Scholar]
- Obama B. Executive Order: Increasing Participation of Asian Americans. 2009 Oct 14; Retrieved from http://www.whitehouse.gov/the-press-office/executive-order-asian-american-and-pacific-islander-community.
- Pastor M, Morello-Frosch R, Sadd JL. The air is always cleaner on the other side: Race, space, and ambient air toxics exposures in California. Journal of Urban Affairs. 2005;27(2):127–148. [Google Scholar]
- Payne-Sturges D, Gee GC. National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environmental Research. 2006;102(2):154–171. doi: 10.1016/j.envres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Pearce JR, Richardson EA, Mitchell RJ, Shortt NK. Environmental justice and health: A study of multiple environmental deprivation and geographical inequalities in health in New Zealand. Social Science & Medicine. 2011;73(3):410–420. doi: 10.1016/j.socscimed.2011.05.039. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. The Rise of Asian Americans. Social and Demographic Trends. 2016 Retrieved from http://www.pewsocialtrends.org/asianamericans-graphics/
- Phillip C. Explaining the Refugee Gap: Economic Outcomes of Refugees versus Other Immigrants. Journal of Refugee Studies. 2010;3:377–397. [Google Scholar]
- Pulido L. A Critical Review of the Methodology of Environmental Racism Research. Antipode. 1996;28(2):142–159. [Google Scholar]
- Pulido L. Rethinking Environmental Racism: White Privilege and Urban Development in Southern California. Annals of the Association of American Geographers. 2000;90(1):12–40. [Google Scholar]
- Quach T, Liu RL, Nelson DO, Hurley S, Von Behren J, Hertz A, Reynolds P. Disaggregating Data on Asian American and Pacific Islander Women to Provide New Insights on Potential Exposures to Hazardous Air Pollutants in California. Cancer Epidemiology Biomarkers & Prevention. 2014;23(11):2218–2228. doi: 10.1158/1055-9965.EPI-14-0468. [DOI] [PubMed] [Google Scholar]
- Rumbaut R. Vietnamese, Laotian, and Cambodian Americans. In: Zhou M, Gatewood JV, editors. Contemporary Asian America. New York: New York University Press; 2000. pp. 175–206. [Google Scholar]
- Spalt EW, Curl CL, Allen RW, Cohen M, Adar SD, Stukovsky KH, … Kaufman JD. Time–location patterns of a diverse population of older adults: the Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air) Journal of Exposure Science and Environmental Epidemiology. 2016;26:349–355. doi: 10.1038/jes.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sze J. Asian American Activism for Environmental Justice. Peace Review. 2004;16(2):149–156. [Google Scholar]
- Torre LA, Sauer AMG, Chen MS, Kagawa-Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA: A cancer journal for clinicians. 2016;66(3):182–202. doi: 10.3322/caac.21335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai S-SH. The Chinese Experience in America. Bloomington, IN: Indiana University Press; 1986. [Google Scholar]
- Walton E. Making Sense of Asian American Ethnic Neighborhoods: A Typology and Application to Health. Sociological Perspectives. 2015;58:490–515. [Google Scholar]
- World Health Organization. 7 million premature deaths annually linked to air pollution. News Release. 2014 Retrieved from http://www.who.int/mediacentre/news/releases/2014/air-pollution/en/
- Yi SS, Kwon SC, Sacks R, Trinh-Shevrin C. Commentary: Persistence and Health-related Consequences of the Model Minority Stereotype of Asian Americans. Ethnicity & Disease. 2016;26(1):133–138. doi: 10.18865/ed.26.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- Zhou M, Tseng YF, Kim RY. Rethinking Residential Assimilation: The Case of a Chinese Ethnoburb in the San Gabriel Valley, California. Amerasia Journal. 2008;34:55–83. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.