Abstract
Background
School cardiopulmonary resuscitation (CPR) training has become mandatory in many countries, but whether legislation has translated into implementation of CPR training is largely unknown. We assessed CPR training of students following 8 years of legislative mandates in Denmark.
Methods and Results
A nationwide cross‐sectional survey of Danish school leadership (n=1240) and ninth‐grade homeroom teachers (n=1381) was carried out for school year 2013‐2014. Qualitative interviews and the Theory of Planned Behavior were used to construct the survey. Logistic regression models were employed to identify factors associated with completed CPR training. Information from 63.1% of eligible schools was collected: 49.3% (n=611) of leadership and 48.2% (n=665) of teachers responded. According to teachers, 28.4% (95% CI 25.0% to 32.0%) and 10.3% (95% CI 8.1% to 12.8%) of eligible classes had completed CPR and automated external defibrillator training, respectively. Among leadership, 60.2% (95% CI 56.2% to 64.1%) reported CPR training had occurred during the 3 years prior to the survey. Factors associated with completed CPR training included believing other schools were conducting training (odds ratio [OR] 9.68 [95% CI 4.65‐20.1]), awareness of mandating legislation (OR 4.19 [95% CI 2.65‐6.62]), presence of a school CPR training coordinator (OR 3.01 [95% CI 1.84‐4.92]), teacher feeling competent to conduct training (OR 2.78 [95% CI 1.74‐4.45]), and having easy access to training material (OR 2.08 [95% CI 1.57‐2.76]).
Conclusions
Despite mandating legislation, school CPR training has not been successfully implemented. Completed CPR training was associated with believing other schools were conducting training, awareness of mandating legislation, presence of a school CPR training coordinator, teachers teacher feeling competent to conduct training, and having easy access to training material. Facilitating these factors may increase rates of school CPR training.
Keywords: automated external defibrillator, cardiopulmonary resuscitation, defibrillation, resuscitation, school
Subject Categories: Cardiopulmonary Arrest, Cardiopulmonary Resuscitation and Emergency Cardiac Care
Introduction
Out‐of‐hospital cardiac arrest is a substantial public health problem, affecting ~700 000 people in the United States and Europe yearly.1, 2, 3 Survival rates are generally less than 10%, but bystander cardiopulmonary resuscitation (CPR) and early defibrillation have been associated with survival rates exceeding 50%.4, 5, 6 According to the American Heart Association, the Institute of Medicine, and other leading organizations, CPR training in schools is one of the key initiatives to increase long‐term bystander intervention.2, 7, 8, 9, 10, 11
Prior to mandating legislation, low rates of and barriers to implementation of CPR training in schools were reported (eg, lack of time and funds, instructor scheduling difficulties, training not mandatory).12, 13, 14 Recently, legislation mandating CPR training in schools was approved in many American states, Canada, and several European countries.7, 15, 16, 17, 18 In Denmark in 2005, CPR training became mandatory by the time of student graduation from middle school; bystander CPR increased following several national initiatives to improve resuscitative efforts from bystanders, including the distribution of 35 000 CPR training kits to school children.18, 19, 20, 21 However, as in many American states, Danish legislation does not provide a framework for how CPR training should be implemented: who should conduct training (teachers vs external instructors), requirements for proficiency level of instructors, training material, length of training session, part of the school curriculum in which CPR training should be integrated, or the source of funding.15, 22 This lack of framework was underscored in a scientific statement by the American Heart Association in 2011.7 Little is known about how mandating legislation has translated into implementation of CPR training in schools, including rates, barriers, and facilitators. This substantial knowledge gap was recently underscored in the Institue of Medicine report: “Strategies to Improve Cardiac Arrest Survival: A Time to Act” as well as recent resuscitation guidelines.2 A study from Toronto and a recent American study suggested that mandating legislation may not be sufficient to establish high rates of CPR or automated external defibrillator (AED) training, and this finding is supported by a recent Danish qualitative study.16, 23, 24
We hypothesized that despite 8 years of legislation mandating CPR training of students prior to middle school graduation, a minority of students would have completed CPR training by the end of the school year 2013‐2014 and that CPR training had not been systematically implemented on a school level. We aimed to assess contemporary rates, barriers, and facilitators of student CPR training in middle schools through a nationwide survey of ninth‐grade homeroom teachers and school leadership.
Methods
Study Population and Design
A cross‐sectional electronic survey of ninth‐grade homeroom teachers and school leadership was conducted from August 28, 2013, to November 29, 2013, in Denmark (5.6 million inhabitants). Schools (private or public) were defined as eligible to participate if they had at least 1 ninth‐grade class during the school year 2013‐2014 because the law in Denmark states that students from public schools are required to receive CPR training before graduating from middle school (students graduate after ninth grade, 14‐15 years old).22 Private schools are not required to train students but are expected to follow legislation for public schools. Schools only enrolling students with special needs (autism or otherwise developmentally challenged students) were not eligible.
Homeroom teachers' responses were chosen as the primary source of data for outcomes and factors associated with CPR training for several reasons. Danish legislation did not specify who should conduct CPR training or who was responsible for ensuring that students were trained but stated that school leadership should decide in which subject CPR training should be included and that it was reasonable for homeroom teachers to be responsible for ensuring CPR training. Further, it is common for a class to have the same homeroom teacher throughout middle school. Also, qualitative interviews with teachers and principals (in detail below) revealed that leadership was not always aware of whether all eligible classes had received CPR training.23 To capture possible discrepancies between school leadership and teachers as well as to explore whether CPR training was systematically implemented (for instance, whether all eligible classes in a given school had completed training), the study was further designed to survey schools at the leadership level, represented by the schools' principals or designated coordinators.
Samples
We obtained the following information through the Danish National Board of Education, which holds information on all schools in Denmark: name, email address of school, number of students in the ninth grade during the school year 2013‐2014, name of principal, and mailing address (http://statweb.uni-c.dk/InstRegUdtraek/).25 The number of students in the ninth grade during the school year 2013‐2014 was obtained directly by request to the Ministry of Children and Education. The exact number of classes in the ninth grade in each school during the school year 2013‐2014 was obtained through the school's website or, if not listed on the website, through a telephone call. Based on this information, a total of 1254 schools were identified. To identify a representative sample of teachers, 600 schools were randomly selected (49.0% of all eligible schools). Of those, 15 schools were excluded because they either had been merged with another school or had no ninth‐grade classes during that specific school year. The final school sample for the teacher survey included 584 schools with 1382 ninth‐grade classes and 1382 homeroom teachers. Sample size calculations are included in Supplemental Material.
The Theory of Planned Behavior
Because of the scarce data on which factors might influence the implementation of CPR training in schools, the Theory of Planned Behavior (TPB) was selected as an approach to identify and understand such factors and thus as guidance to which questions should be included in the questionnaire. The TPB is a well‐established theory that proposes a model about how human action is guided and can be used to investigate implementation processes and identify barriers and facilitators to implementation.26, 27 In summary, the theory assumes that intention is the most important predictor of behavior and that intention is closely related to 3 variables: (1) attitudes toward the behavior, ie, whether teachers are in favor of CPR training of students, (2) subjective norms about the behavior, ie, how much teachers feel pressure to ensure students receive CPR training; and (3) perceived behavioral control, ie, whether teachers feel able to ensure CPR training of students.
Instrument Development
A questionnaire was developed to investigate rates of CPR training as well as to identify barriers and facilitators to CPR training in middle schools. The development was based on a systematic review of the literature and themes emerging from semistructured qualitative interviews and focus groups with teachers and principals (also based on the constructs of the TPB) with a strategic sample of 16 teachers and 9 principals.23, 28 Responses to direct and indirect measurements of attitudes, subjective norms, and perceived behavioral control were given on a 5‐point Likert scale from 1 to 5.29 To pursue content validity, the survey instrument was pilot‐tested on 3 levels: (1) by 5 researchers with expertise in survey construction (M.T.D., T.H., S.A., M.E., A.I.C.), (2) by 3 physicians (2 cardiologists [F.F., C.T.‐P.] and 1 cardiology resident [C.M.H.]) to ensure appropriate content for the purpose of the study, and (3) by a sample of representatives of the target audience (4 teachers and 4 principals from 5 different schools) to pursue correct understanding of the language and relevant content. Cognitive interviewing, which is a widely accepted tool to evaluate sources of response error in survey questionnaires, was used to pilot test teachers and principals.30
The final leadership and teacher surveys included 64 and 72 items, respectively. They were designed to measure how many of eligible ninth‐grade classes had completed CPR training (outcome variable) and factors associated with CPR training: (1) knowledge of mandatory CPR training, (2) attitudes toward training students in CPR (direct and indirect measures), (3) subjective norms (perceived pressure to train or ensure training of students in CPR [direct and indirect measures]), (4) perceived behavioral control to train or help establish CPR training of students (only indirect measures), (5) school and personal characteristics (eg, age, sex, school size, presence of an AED at the school, presence of a CPR training coordinator/employee who is passionate about CPR training), and (6) intention to establish CPR training of students.
Data Collection
We conducted 4 waves of contact (L.Z.). Each school received 1 unique email with a link addressed to school leadership. Schools selected for the survey of teachers received an email containing 1 unique link for each ninth‐grade class in the school addressed to the homeroom teacher. Thus, a school with five ninth‐grade classes received 5 emails with different links and 1 email to school leadership. If no response was received within 2 weeks, 1 email was sent as a reminder, and then again 1 week later. If no response was received, the school was contacted by telephone (n=870). Of those, it was not possible to reach 168 schools.
Definitions
A class was defined as having completed CPR training if the teacher reported the class had completed CPR training sometime during the sixth to ninth grade prior to the date of the survey. A class was defined as having planned CPR training if the teacher reported CPR training had been planned to be completed by the end of the ninth grade during the school year 2013‐2014 but had not completed training prior to the survey. The response rate was calculated based on the proportion of leadership and teachers who responded to the main outcome measure. For this study students are defined as sixth‐ to ninth‐grade students unless otherwise indicated.
Outcome Measures
The primary outcome measure was completed CPR training by the date of the survey. In the teacher survey the specific question inquired whether the teacher's homeroom class had received CPR training prior to the survey. The second outcome measure was whether CPR training was planned to be completed during the school year 2013‐2014 among those who had not yet completed CPR training. The main outcome measure in the leadership survey was whether any sixth‐ to ninth‐grade classes in the school had completed CPR training by the date of the survey during the last 3 school years prior to the survey.
Sample Size Calculation
The sample size calculation for how many ninth‐grade homeroom teachers should be included was based on achieving the target confidence interval of 6% for the main measure of the study, “Has your current ninth‐grade class received CPR training during sixth to ninth grade?” The following calculation was employed: we hypothesized the lowest proportion of positive answers would be 10.0%, and the lowest expected response rate would be 30.0%. Based on the assumption that most schools have 2 classes with ninth‐grade students, 600 schools would yield 1200 ninth‐grade classes. A random selection of 600 schools (100 private and 500 public schools) yielded 1382 ninth‐grade classes, which were estimated to be a representative sample of all eligible ninth‐grade classes.
Data Analysis
Results were summarized by reporting responses on selected survey items. Continuous variables are presented as medians with interquartile ranges, and categorical variables are reported as percentages. The association between personal and school characteristics and completed CPR training (yes, no) by respondents (teachers and leadership) was evaluated using nonparametric 1‐way analysis for continuous variables and a chi‐squared test or Fisher exact test, as appropriate for categorical variables.
Identifying Factors Associated With CPR Training
Factors associated with completed CPR training according to teachers were evaluated using univariable logistic regression analysis with completed CPR training (yes, no) as the outcome measure. A 2‐level hierarchical data structure was implemented with teachers nested within schools by including school as a random effect in the model using generalized estimating equations. Teachers who responded “do not know” (n=114, 17.1%) were coded as “no.” Results are reported as odds ratios (OR) with 95% CIs. A list of all factors included in the analysis is shown in Table S1. For the 3 TPB constructs (attitudes, subjective norms, and perceived behavioral control) using the 5‐item Likert scale, responses were dichotomized (2 lowest responses vs 3 highest).29 Items with negatively worded endpoints on the right were recoded so high scores (ie, 5) reflected the most positive response. For these analyses, only teachers' responses were included. To assess how leadership might influence teachers in their school, we performed a separate analysis for those teachers whose leadership had answered “yes” to the following two questions: “Is CPR training mandatory?” and “Should CPR training be mandatory?” All analyses were performed using SAS (Version 9.3, Cary, NC).
Construction of Latent Variables
Based on TPB, latent variables were constructed for each of the 3 predictor variables (attitudes, subjective norms, and perceived behavioral control) by multiplying the items of indirect measures by the evaluation of such predictors (Table S2). A definition of each latent variable is shown in Table S3, and a descriptive analysis of latent variables is shown in Table S4.
Scale Validation of Latent Variables
Our survey instrument was based on a previously validated instrument.29 Because its applicability has not been assessed for examining CPR training in schools, we performed a scale validation of latent variables (attitudes, subjective norms, and perceived control). Internal consistency (Cronbach α≥0.8) was used as guidance to select latent variables for the final model.31 Construct validity was assessed through confirmatory factor analysis (Figure S1). The adequacy of fit for the model was evaluated using a chi‐squared test, root mean square error of approximation, the comparative fit index, and the normed fit index.32 Differential item functioning evaluated whether male and female teachers responded differently.33
Ethics
This study was approved by the Danish Data Protection Agency J.nr. 2012‐54‐0217. This type of study does not require formal ethical approval in Denmark.
Results
The selection process for inclusion of schools and teachers is depicted in Figure. Thus, the final number of eligible schools was 1240, yielding 1240 school leadership members and 1381 homeroom teachers. Of those, 49.3% (n=611) of the leadership members and 48.2% (n=665) of the teachers responded to the survey, respectively. Taken together, the surveys from leadership and teachers report results from 63.1% (n=783) of eligible schools. Characteristics of the respondents are shown in Table 1.
Figure 1.
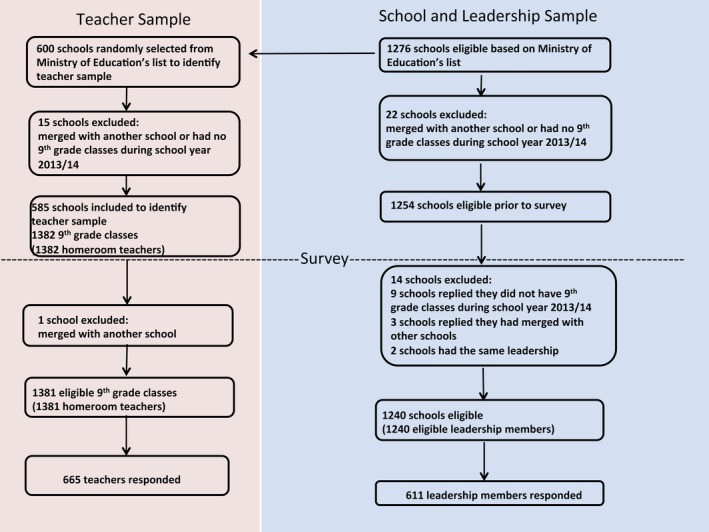
Selection of schools, leadership, and teachers for the study sample.
Table 1.
Characteristics of the Respondents
| Characteristic | School Leadership | Teachers | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n=611) | CPR Training Completed (n=368, 60.2%) | No CPR Training Completed (n=243, 39.8%) | P Value | Missinga, % (n) | Total (n=665) | CPR Training Completed (n=189, 28.4%) | No CPR Training Completed (n=476, 71.6%) | P Value | Missinga, % (n) | |
| Respondents | ||||||||||
| Female sex, % (n) | 43.9 (214) | 43.0 (126) | 45.1 (88) | 0.64 | 20.1 (123) | 72.6 (444) | 79.8 (138) | 69.7 (306) | 0.012 | 8.0 (53) |
| Median age, y (IQR) | 53.5 (47‐58) | 54.0 (47‐59) | 53.0 (45‐58) | 0.10 | 18.2 (111) | 43.0 (36‐54) | 43.0 (36‐55) | 43.0 (36‐64) | 0.83 | 7.7 (51) |
| Years working in a school, y (IQR) | 25.0 (15‐33) | 27.0 (16‐34) | 23 (13‐32) | 0.008 | 17.3 (106) | 12.0 (8‐24) | 13.0 (8‐24) | 12.0 (8‐24) | 0.83 | 8.6 (57) |
| Years in leadership position in a school, y (IQR) | 12.0 (6‐17) | 12.5 (7‐18) | 10 (5‐16) | 0.008 | 18.2 (111) | ··· | ··· | ··· | ··· | ··· |
| Family member, friend, or acquaintance with previous cardiac arrest, % (n) | 42.7 (215) | 47.0 (142) | 36.3 (73) | 0.018 | 17.7 (108) | 38.2 (226) | 46.1 (77) | 35.1 (149) | 0.013 | 11.0 (73) |
| Has thought about CPR training of students prior to this survey, % (n) | 89.7 (452) | 93.4 (283) | 84.1 (169) | 0.002 | 17.5 (107) | 75.7 (462) | 88.4 (152) | 70.8 (310) | <0.001 | 8.3 (55) |
| Has provided first‐aid in life‐threatening situation, % (n) | 20.6 (103) | 22.1 (66) | 18.5 (37) | 0.33 | 18.3 (112) | 17.0 (103) | 19.8 (34) | 15.9 (69) | 0.25 | 8.9 (59) |
| Has taken a first‐aid course, % (n) | 92. 3 (469) | 93.4 (284) | 90.7 (185) | 0.26 | 16.9 (103) | 84.1 (517) | 87.9 (152) | 82.6 (365) | 0.11 | 7.5 (50) |
| Has taken a first‐aid course within the last 2 years, % (n) | 34.7 (156) | 39.4 (109) | 26.9 (47) | <0.001 | 26.4 (161) | 30.8 (151) | 32.9 (48) | 29.9 (103) | 0.51 | 26.2 (174) |
| It is mandatory for students to complete CPR training before middle school graduation | 28.7 (147) | 36.8 (113) | 16.5 (34) | <0.001 | 16.0 (98) | 14.1 (87) | 29.9 (52) | 7.9 (35) | <0.001 | 7.2 (48) |
| Schools | ||||||||||
| AED present, % (n) | 43.5 (222) | 45.9 (140) | 40.0 (82) | 0.14 | 16.5 (101) | 46.5 (286) | 53.2 (92) | 43.9 (194) | 0.002 | 7.5 (50) |
| Number of students, median (IQR) | 440.0 (250‐610) | 430.0 (261‐600) | 450 (240‐650) | 0.83 | 17.0 (104) | 600.0 (430‐750) | 600.0 (400‐700) | 600 (450‐750) | 0.09 | 8.1 (54) |
| Distance to nearest hospital, median, km (IQR) | 10.0 (4‐20) | 10.0 (4‐20) | 9.2 (4‐20) | 0.07 | 17.3 (106) | 10.0 (4‐20) | 10.0 (3‐20) | 10 (4‐20) | 0.79 | 8.9 (59) |
| Presence of employee who is passionate about CPR training, % (n) | 46.1 (257) | 53.7 (176) | 35.4 (81) | <0.001 | 8.8 (54) | 25.7 (164) | 36.7 (65) | 21.4 (99) | <0.001 | 3.9 (26) |
| Presence of a local CPR coordinator, % (n) | 26.2 (148) | 37.7 (125) | 9.9 (23) | <0.001 | 7.7 (47) | 13.7 (89) | 26.0 (47) | 9.0 (42) | <0.001 | 2.6 (17) |
Percentages are calculated based on nonmissing responses. AED indicates automated external defibrillators; CPR, cardiopulmonary resuscitation.
Percentages of total number of responses (611 principals and 665 teachers).
Completed or Planned CPR Training
A minority of teachers reported that their class had completed CPR training prior to the survey (28.4% [95% CI 25.0% to 32.0%]). Among those who had not yet completed CPR training, 11.1% (95% CI 8.5% to 14.3%) had planned to complete training within the school year 2013‐2014. A total of 60.2% (95% CI 56.2% to 64.1%) of school leadership reported that CPR training of students had occurred at their school during the 3 school years prior to the survey (the leadership survey did not include questions on how many ninth‐grade classes had completed training).
Knowledge of and Attitudes Toward Mandatory CPR Training
A minority of teachers and school leadership reported it was mandatory for students to complete CPR training before graduating from middle school; teachers 13.1% (95% CI 10.6% to 15.9%); school leadership 28.7% (95% CI 24.8% to 32.8%). The majority of teachers and leadership reported CPR training in middle school should be mandatory: teachers 82.7% (95% CI 79.6% to 85.5%); school leadership 79.0% (95% CI 75.3% to 82.5%).
Teachers' Ability to Conduct CPR Training
A minority of teachers felt competent to train students in CPR (13.3% [95% CI 10.7% to 16.1%]). According to leadership, 13.0% (95% CI 10.3% to 16.1%) of schools had no teachers competent to conduct training, and 47.0% (95% CI 42.8% to 51.3%) of schools had few teachers competent to conduct training. Half of the teachers reported it was easy to acquire good CPR training material 51.3% (95% CI 47.3% to 55.2%).
Factors Associated With Completed CPR Training
Table 2 shows all factors found to be significantly associated with completed CPR training in univariable logistic regression analysis. Estimates are presented with and without taking the random effect of schools into account. Factors associated with completed CPR training included believing other schools were conducting CPR training (OR 9.68 [95% CI 4.65‐20.1]), awareness of mandating legislation (OR 4.19 [95% CI 2.65‐6.62]), the presence of a school CPR coordinator (OR 3.01 [1.84‐4.92]), feeling competent to conduct training (OR 2.78 [95% CI 1.74‐4.45]), and having easy access to CPR training material (OR 2.08 [1.57‐2.76]).
Table 2.
Factors Associated With CPR Training in Middle Schools According to Teachers
| Variable From Questionnaire Survey | OR (95% CI) | P Value | OR (95% CI) Adjusted for the Random Effect of School | P Value |
|---|---|---|---|---|
| Knowledgea | ||||
| CPR training of students is mandatory before graduation from middle schoola | 4.97 (3.09‐7.98) | <0.001 | 4.19 (2.65‐6.62) | <0.001 |
| Background variables | ||||
| Teacher characteristics | ||||
| Female sex | 1.71 (1.12‐2.62) | 0.013 | 1.28 (0.91‐1.81) | 0.15 |
| Family member, friend, or acquaintance with previous cardiac arresta | 1.59 (1.10‐2.28) | 0.013 | 1.56 (1.13‐2.15) | 0.010 |
| Had thought about CPR training of students before this surveya | 3.14 (1.89‐5.22) | <0.001 | 2.34 (1.52‐3.61) | <0.001 |
| School characteristics | ||||
| AED presenta | 1.45 (1.02‐2.07) | 0.038 | 1.41 (0.99‐2.01) | 0.052 |
| Presence of a staff member who is very passionate about CPR traininga | 2.13 (1.46‐3.11) | <0.001 | 2.04 (1.40‐2.97) | <0.001 |
| School leadership has reported CPR training is mandatorya, b | 2.95 (1.91‐4.55) | <0.001 | ··· | ··· |
| School leadership has reported CPR training should be mandatorya, b | 2.71 (1.76‐4.19) | <0.001 | ··· | ··· |
| Direct measure of teachers' attitudes toward CPR training of studentsa | ||||
| CPR training should be mandatory | 3.12 (1.52‐6.42) | 0.002 | 2.38 (1.37‐4.12) | 0.002 |
| Indirect measures of teachers' attitudes toward CPR training of studentsc | ||||
| CPR training empowers students to take action in emergency situations | 1.90 (1.31‐2.74) | <0.001 | 1.70 (1.18‐2.45) | 0.004 |
| CPR training increases students' understanding of being a citizen | 1.70 (1.18‐2.43) | 0.004 | 1.52 (1.11‐2.09) | 0.009 |
| CPR training of students will increase bystander CPR in the long term | 1.79 (1.10‐2.91) | 0.019 | 1.61 (1.04‐2.48) | 0.032 |
| Students do not find CPR training uncomfortable/scary | 2.78 (1.76‐4.38) | <0.001 | 2.27 (1.58‐3.28) | <0.001 |
| Direct measure of pressure teachers feel to train students in CPRc | ||||
| To what degree is it expected from you, as a teacher at your school, that students are trained in CPR? | 2.91 (1.54‐5.52) | 0.001 | 2.04 (1.07‐3.89) | 0.031 |
| Indirect measures of pressure teachers feel to train students in CPRd | ||||
| During the past 3 years, how many of graduating classes (middle school) do you think have completed CPR training? | 17.3 (10.7‐28.0) | <0.001 | 13.5 (8.39‐21.7) | <0.001 |
| How many middle schools do you think have implemented CPR training? | 12.98 (5.58‐30.17) | <0.001 | 9.68 (4.65‐20.1) | <0.001 |
| The following groups think/express that students should be trained in CPRc | ||||
| Students/the student council | 2.04 (1.80‐3.87) | 0.030 | 1.93 (1.11‐3.34) | 0.019 |
| Parents/parents' committee | 2.62 (1.60‐4.30) | <0.001 | 2.21 (1.42‐3.42) | <0.001 |
| Teachers | 2.10 (1.43‐3.08) | <0.001 | 1.84 (1.30‐2.59) | <0.001 |
| The school leadership | 2.02 (1.33‐3.08) | 0.001 | 1.90 (1.28‐2.80) | 0.001 |
| Indirect measure of teachers' perceived ability to train students in CPR | ||||
| Presence of a CPR training coordinator at your schoola | 3.55 (2.24‐5.62) | <0.001 | 3.01 (1.84‐4.92) | <0.001 |
| At the moment, do you feel you have the skills to train students in CPR?c | 3.16 (1.98‐5.04) | <0.001 | 2.78 (1.74‐4.45) | <0.001 |
| The school provides clear guidelines as to who is responsible for CPR training that is conducted at your schoolc | 1.90 (1.25‐2.88) | 0.003 | 1.57 (1.07‐2.29) | 0.020 |
| I think it is easy to acquire good CPR training materialc | 2.47 (1.71‐3.55) | <0.001 | 2.08 (1.57‐2.76) | <0.001 |
AED indicates automated external defibrillators; CPR, cardiopulmonary resuscitation.
Yes vs no.
Subanalysis only including teachers whose leadership also responded to this item (n=344).
Dichotomized from a 5‐point Likert scale, the 2 lowest levels vs the 3 highest levels.
Dichotimized from a 5‐point Likert scale, all and most classes (schools) vs half or less than half of the classes (schools).
Training in AED Use
A minority of teachers and leadership reported having completed AED training during the sixth to ninth grade prior to the survey: teachers 10.3% (95% CI 8.1% to 12.8%); leadership 19.5% (95% CI 16.4% to 22.8%). The majority of teachers and principals reported training in AED use should be mandatory: teachers 78.4% (95% CI 74.9% to 81.5%); school leadership 59.6% (95% CI 55.2% to 63.9%).
School Level of CPR Training
For teachers who reported that their class had completed CPR training, we assessed whether CPR training was implemented on a school level (all eligible classes with a teacher response in a given school). For this analysis, we performed a subgroup analysis assessing the correlation between teachers' responses within the same school. A total of 191 (52.5%) had responses from at least 2 teachers (range 2‐8 teachers). Among those, in 26.7% (95% CI 20.6% to 33.6%) of schools, some but not all teachers reported completed training. In 59.2% (95% CI 51.8% to 66.2%) of schools, all teachers reported no CPR training was completed, and in 14.1% (95% CI 9.5% to 19.9%) of schools, completed CPR training was reported by all teachers.
Domains of TPB and Scale Validation
The domains in the TPB model were generally good predictors of CPR training and showed a positive association between the domains and completed CPR training; OR 3.12 (95% CI 1.52‐6.42) for direct measure and OR 1.02 (95% CI 1.01‐1.04) for indirect measure of teachers attitudes toward CPR training of students; OR 5.24 (95% CI 3.96‐6.95) for indirect measure of pressure teachers feel to train or ensure CPR training of students. Measures of internal and construct validity were high, indicating good internal and construct validity (Table S5 and Figure S1).
Nonrespondents
Table S6 shows characteristics of nonrespondents. Among teachers, the number of ninth‐grade classes or students was similar among respondents and nonrespondents. Teachers from 1 specific region in Denmark and from private schools were more likely to be nonrespondents. Leadership members from private schools were markedly more likely to respond to this survey.
Discussion
This nationwide survey of Danish middle schools evaluated rates, barriers, and facilitators of CPR training in schools 8 years after nationwide implementation of the mandating legislation. Our main findings were these: (1) 60% of ninth‐grade classes had not and would not receive CPR training or AED training before graduating from middle school; (2) the majority of teachers and school leaders were supportive of mandatory CPR and AED training of students but were unaware that CPR training was mandatory; (3) CPR training was not systematically implemented on a school level (in all eligible classes in a given school); (4) factors associated with completed CPR training included believing other schools were conducting training, awareness of mandating legislation, the presence of a CPR training coordinator at the school, feeling competent to train students in CPR, and having easy access to good training material.
Legislation mandating CPR training of students has recently been approved in many American states and countries, but our findings suggest additional efforts are likely necessary to successfully implement CPR training in schools.7, 15, 16, 17 It may be necessary to systematically inform school leadership and teachers of the requirements as well as to monitor implementation. This is supported by 2 recent small studies that found that despite mandating legislation in Washington state and Toronto, only about half of the schools were training students.16, 24 These studies did not provide information on whether schools providing CPR training had implemented programs for systematic training (eg, for all classes). In our study, among schools with responses from more than 1 teacher, only 14% reported training in all eligible classes, and 27% reported training in 1 of several classes, indicating that training was mostly not implemented across the whole school. Further, 60% of leadership reported that CPR training had been conducted in their school during the last 3 years, but fewer than 30% of teachers reported their class had received training, further supporting that CPR training was unlikely to take place in all classes within a given school. These studies also did not provide information on whether respondents were aware of mandating legislation, which we found to be significantly associated with CPR training. In our study the majority of teachers and leadership were not aware of current legislation, although they were generally supportive of mandatory student CPR and AED training, suggesting an overall positive attitude toward CPR and AED training, in accordance with a previous study.13 Complete CPR training was 4‐fold higher among teachers who reported it was mandatory than among those who did not, and training was 3‐fold higher among teachers whose leadership reported that CPR training was mandatory, underscoring the importance of increasing awareness of mandatory CPR training among both teachers and leadership.
Our findings also indicate it is necessary to ensure that those who are responsible for conducting CPR training, for instance teachers, are qualified, feel competent to train students, and have access to good training material. This is supported by previous studies reporting teachers generally do not feel competent to train students.13, 23, 34 A recent qualitative study of Danish teachers found that teachers generally believe extraordinary skills are required to train students in CPR.13, 23 Although Isbye et al found that distributing CPR training kits to schools was associated with completed CPR training, in that study, 91% of teachers who conducted the training felt competent to train the students.21 However, only a minority of teachers completed the survey, and many teachers might not have felt competent to conduct training (and to respond the survey), despite having the CPR training kit. In our study teachers who found it easy to acquire good training material and felt competent to conduct CPR training were 2 and 3 times more likely to report that their class had completed CPR training. However, only 13.3% of teachers felt competent to conduct training, and half the teachers found it easy to acquire good CPR training material. There are several alternatives to train teachers to become CPR instructors. In Norway, teachers are trained to be CPR instructors during college. Teachers can also be trained by medical students or emergency physicians.35, 36, 37, 38 Alternatively, external CPR instructors could conduct training, but this has been identified as a barrier (scheduling difficulties and high cost).12 We found CPR training to be 3 times more likely to be completed if there was a local CPR training coordinator at the school. Establishing a local CPR training coordinator to ensure availability of CPR training material and teacher instructor skills may facilitate implementing a successful school CPR training program.
CPR training should include AED training, but in our study only a third of those who completed CPR training also completed AED training.7 Similar findings were reported in the Canadian study.16 Danish legislation (similar to legislation in many American states) requires students to learn principles of first‐aid including CPR but does not include a specific curriculum or requirements to include psychomotor skills practice or AED training, as recommended by the AHA.7 To ensure that students properly learn CPR (including AED use), legislators should specify core curriculum elements, including AED training.
Taken together, our study indicates several steps that should be taken to overcome barriers to implementation of CPR training in schools. In terms of legislation, communities need to systematically inform school leadership and teachers, enforce legislation, and monitor the implementation process. Legislation regarding CPR training in schools is typically unfunded, and because costs have been identified as a barrier to implementation, clear sources of funding should be included in future legislation. Authorities need to provide a source of information (eg, a website) to schools that provides all relevant information: who may conduct CPR training of students (teacher or instructor), what proficiency level is required, what training material is necessary and where to find it, which grades may be trained, how often training should take place, and which elements should be included in the curriculum. The curriculum should be thoroughly explained and include hands‐on CPR and hands‐on AED training. Schools should have a CPR training coordinator responsible for establishing and monitoring the program.
Strengths and Limitations
Our findings may not be directly generalizable to other communities with different school structures, legislation, or culture, but our methodology can be used as guidance to authorities, communities, and researchers who wish to understand barriers and facilitators to school CPR training. Other countries have reported conditions similar to those in our study such as low rates of CPR and AED training despite mandating legislation, teachers not feeling competent to train students, lack of resources, indicating at least some degree of generalizability.12, 13, 14, 16, 24 Only half of eligible respondents participated in the survey. This response rate is similar to average response rates of surveys conducted in organizations (including schools) and notably higher than a recent American study.24, 39 Nevertheless, the missing information from nonrespondents may have introduced sampling bias of unknown magnitude and direction. Although the complete questionnaire took a maximum of 10 minutes to complete and was only applicable to those who had completed CPR training (thus, the minority of surveyed), a shorter survey might have achieved higher response rates.
Our reported rates of CPR training might be higher than the national average if a greater portion of schools that had not implemented CPR training declined to participate. Conversely, for teachers who responded that they did not know whether their class had completed training (17.1%), we assumed their class had not completed training, which might have underestimated the proportion that had completed training. However, even if all of these classes had completed training, our main findings would remain unchanged: that a minority of schools had implemented training, and much is needed beyond passing legislation to successfully implement CPR training in schools. Nonrespondents were similar to respondents in terms of school size and number of students and were equally distributed across country regions, which is likely to minimize bias due to local factors. Further, our nationwide data collection decreased the chance of selection bias. The survey instrument was based on a well‐established method and a previously validated survey instrument, further strengthened by qualitative interviews and pilot testing with the target audience to ensure content validity and correct understanding of the language.23, 29, 30, 40 Scale validation indicated good construct validity and internal consistency (reliability).
The TPB was used to guide the development of a questionnaire that focuses on an individual's decision‐making process. This was deemed appropriate because legislation states it would be reasonable to expect homeroom teachers to ensure CPR training of students. Our results support the use of TPB because many individual factors as well as constructs from the domains of the TPB were associated with completed CPR training, and scale validation indicated that our questionnaire survey was an appropriate measurement tool for this study. However, schools could also be viewed as organizational units, and using a different approach to construct our survey, for instance, the Organizational Readiness to Change scale, could have identified other factors that may influence CPR training.26 The slight changes in our estimates when we take the random effect of schools into account suggest schools as an organization might be of importance. However, the changes were small and did not alter the main conclusions. This is further supported by our findings that completed CPR training was not primarily the result of systematic implementation at the school level, further supporting the use of a model based on teachers' decision‐making process.
Conclusions
Despite 8 years of mandating legislation, CPR training has not been systematically implemented in Danish schools, even though the majority of teachers and leadership were supportive of it. A minority of students who completed CPR training also completed AED training. Factors associated with completed CPR training included believing that other schools were conducting training, awareness of mandating legislation, presence of a CPR training coordinator at the school, teacher feeling competent to conduct training, and having easy access to training material. Facilitating these factors may increase rates of school CPR training.
Sources of Funding
This study was funded by TrygFonden and Helsefonden. The study sponsors had no role in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Disclosures
Dr Malta Hansen has reported receiving research grants from the Laerdal Foundation, TrygFonden and Helsefonden. Dr Folke has reported receiving research grants from TrygFonden. Dr Torp‐Pedersen reported serving as a consultant for Cardiome, Merck, Sanofi, and Daiichi and receiving grants or grants pending from Bristol‐Myers Squibb. Dr Gislason is supported by an unrestricted clinical research scholarship from the Novo Nordisk Foundation and reports research grants from Pfizer, Bristol‐Myers Squibb, Bayer, AstraZeneca, and Boehringer Ingelheim.
Supporting information
Table S1. All Variables Included in Univariable Analysis of the Association Between Completed CPR Training and Factors Associated With Completed CPR Training
Table S2. Construction of Latent Variables of Teachers' Attitudes Toward CPR Training, Perceived Pressure, and Perceived Behavioral Control to Ensure Student CPR Training
Table S3. Definition of Latent Variables
Table S4. Descriptive Analysis, Univariable Analysis, and Differential Item Functioning for CPR Training and Each Latent Variable
Table S5. Association Between Domains in the Theory of Planned Behavior and Completed CPR Training
Table S6. Characteristics of Nonrespondents
Figure S1. Confirmatory factor analysis.
Acknowledgments
We sincerely extend our appreciation to all teachers, members of school leadership, or other school staff who took the time to help our team develop and complete this survey; Bjarne Laursen for providing sample size calculations; Mogens Trab Damsgaard, Teresa Holmberg, Susan Andersen, Marie Eliasen, and Anne Illemann Christensen for providing expert opinion and guidance in the construction of the questionnaire.
(J Am Heart Assoc. 2017;6:e004128. DOI: 10.1161/JAHA.116.004128.)
Selected results from this work were presented at the American Heart Association Scientific Sessions, November 15–19, 2014 in Chicago, IL.
References
- 1. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 2. Institute of Medicine . Strategies to improve cardiac arrest survival: a time to act. 2015. Available at: http://www.nationalacademies.org/hmd/Reports/2015/Strategies-to-Improve-Cardiac-Arrest-Survival.aspx. Accessed January 29, 2017.
- 3. Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out‐of‐hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–1487. [DOI] [PubMed] [Google Scholar]
- 4. Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out‐of‐hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ringh M, Jonsson M, Nordberg P, Fredman D, Hasselqvist‐Ax I, Hakansson F, Claesson A, Riva G, Hollenberg J. Survival after public access defibrillation in Stockholm, Sweden—a striking success. Resuscitation. 2015;91:1–7. [DOI] [PubMed] [Google Scholar]
- 6. Daya MR, Schmicker RH, Zive DM, Rea TD, Nichol G, Buick JE, Brooks S, Christenson J, MacPhee R, Craig A, Rittenberger JC, Davis DP, May S, Wigginton J, Wang H; Resuscitation Outcomes Consortium I . Out‐of‐hospital cardiac arrest survival improving over time: results from the Resuscitation Outcomes Consortium (ROC). Resuscitation. 2015;91:108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cave DM, Aufderheide TP, Beeson J, Ellison A, Gregory A, Hazinski MF, Hiratzka LF, Lurie KG, Morrison LJ, Mosesso VN Jr, Nadkarni V, Potts J, Samson RA, Sayre MR, Schexnayder SM. Importance and implementation of training in cardiopulmonary resuscitation and automated external defibrillation in schools: a science advisory from the American Heart Association. Circulation. 2011;123:691–706. [DOI] [PubMed] [Google Scholar]
- 8. Bhanji F, Donoghue AJ, Wolff MS, Flores GE, Halamek LP, Berman JM, Sinz EH, Cheng A. Part 14: education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S561–S573. [DOI] [PubMed] [Google Scholar]
- 9. Greif R, Lockey AS, Conaghan P, Lippert A, De Vries W, Monsieurs KG; Education and implementation of resuscitation section Collaborators . European Resuscitation Council Guidelines for Resuscitation 2015: section 10. Education and implementation of resuscitation. Resuscitation. 2015;95:288–301. [DOI] [PubMed] [Google Scholar]
- 10. Perkins GD, Lockey AS, de Belder MA, Moore F, Weissberg P, Gray H; Community Resuscitation Group . National initiatives to improve outcomes from out‐of‐hospital cardiac arrest in England. Emerg Med J. 2016;33:448–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bottiger BW, Bossaert LL, Castren M, Cimpoesu D, Georgiou M, Greif R, Grunfeld M, Lockey A, Lott C, Maconochie I, Melieste R, Monsieurs KG, Nolan JP, Perkins GD, Raffay V, Schlieber J, Semeraro F, Soar J, Truhlar A, Van de Voorde P, Wyllie J, Wingen S; Board of European Resuscitation Council . Kids Save Lives—ERC position statement on school children education in CPR.: “Hands that help ‐ Training children is training for life”. Resuscitation. 2016;105:A1–A3. [DOI] [PubMed] [Google Scholar]
- 12. Reder S, Quan L. Cardiopulmonary resuscitation training in Washington state public high schools. Resuscitation. 2003;56:283–288. [DOI] [PubMed] [Google Scholar]
- 13. Miro O, Jimenez‐Fabrega X, Espigol G, Culla A, Escalada‐Roig X, Diaz N, Salvador J, Abad J, Sanchez M. Teaching basic life support to 12‐16 year olds in Barcelona schools: views of head teachers. Resuscitation. 2006;70:107–116. [DOI] [PubMed] [Google Scholar]
- 14. Lafferty C, Larsen PD, Galletly D. Resuscitation teaching in New Zealand schools. N Z Med J. 2003;116:U582. [PubMed] [Google Scholar]
- 15. Lockey AS, Georgiou M. Children can save lives. Resuscitation. 2013;84:399–400. [DOI] [PubMed] [Google Scholar]
- 16. Hart D, Flores‐Medrano O, Brooks S, Buick JE, Morrison LJ. Cardiopulmonary resuscitation and automatic external defibrillator training in schools: “is anyone learning how to save a life?”. CJEM. 2013;15:270–278. [DOI] [PubMed] [Google Scholar]
- 17. Semeraro F, Wingen S, Schroeder DC, Ecker H, Scapigliati A, Ristagno G, Bottiger BW. KIDS SAVE LIVES implementation in Europe: a survey through the ERC Research NET. Resuscitation. 2016;107:e7–e9. [DOI] [PubMed] [Google Scholar]
- 18. Undervisningsministeriet . Fælles Mål 2009 Færdselslære. Faghæfte 20. Undervisningsministeriets håndbogsserie. In.; 2009.
- 19. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp‐Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA. 2013;310:1377–1384. [DOI] [PubMed] [Google Scholar]
- 20. Hansen CM, Lippert FK, Wissenberg M, Weeke P, Zinckernagel L, Ruwald MH, Karlsson L, Gislason GH, Nielsen SL, Kober L, Torp‐Pedersen C, Folke F. Temporal trends in coverage of historical cardiac arrests using a volunteer‐based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130:1859–1867. [DOI] [PubMed] [Google Scholar]
- 21. Isbye DL, Rasmussen LS, Ringsted C, Lippert FK. Disseminating cardiopulmonary resuscitation training by distributing 35,000 personal manikins among school children. Circulation. 2007;116:1380–1385. [DOI] [PubMed] [Google Scholar]
- 22. Undervisningsministerium . Fælles Mål 2009 Færdselslære. 2009. Available at: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&uact=8&ved=0ahUKEwj60f6U8OjRAhWFWCYKHfUaAW0QFggZMAA&url=https%3A%2F%2Fwww.uvm.dk%2F-%2Fmedia%2FPublikationer%2F2009%2FFolke%2FFaelles-Maal%2FFiler%2FFaghaefter%2F110902_faerdsel_11.ashx&usg=AFQjCNF2A6vFYRa4iQRb_UzfO0dboOcmxw&sig2=xfC8HDkEADW9__K9fD8B-A. Accessed January 29, 2017.
- 23. Zinckernagel L, Malta Hansen C, Rod MH, Folke F, Torp‐Pedersen C, Tjornhoj‐Thomsen T. What are the barriers to implementation of cardiopulmonary resuscitation training in secondary schools? A qualitative study BMJ Open. 2016;6:e010481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Salvatierra GG, Palazzo SJ, Emery A. High school CPR/AED training in Washington state. Public Health Nurs. 2016. Available at: http://onlinelibrary.wiley.com/wol1/doi/10.1111/phn.12293/full. Accessed March 2, 2017. [DOI] [PubMed] [Google Scholar]
- 25. Undervisningsministerium . Institution Registry, Ministry for Children and Education. 2011. Available at: http://statweb.uni-c.dk/InstRegUdtraek/. Accessed January 29, 2017.
- 26. Chaudoir SR, Dugan AG, Barr CH. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci. 2013;8:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 28. Patton MQ. Qualitative Research & Evaluation Methods. 3rd ed Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 29. Francis JJ, Eccles MP, Johnston M, Walker A, Grimshaw J, Foy R, Kaner EFS, Smith L, Bonetti D. Constructing Questionnaires Based on the Theory of Planned Behavior: A Manual for Health Services Researchers. Newcastle Upon Tyne, United Kingdom: Centre for Health Services Research; 2004. Available at: http://openaccess.city.ac.uk/1735/. Accessed February 29, 2016. [Google Scholar]
- 30. Willis GB. Cognitive Interviewing: a tool for improving questionnaire design. 1st Ed. Thousand Oaks, CA: Sage Publications; 2005. [Google Scholar]
- 31. Mohsen Tavakol RD. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 33. Scott NW, Fayers PM, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, Gundy C, Koller M, Petersen MA, Sprangers MA; EORTC Quality of Life Group and the Quality of Life Cross‐Cultural Meta‐Analysis Group . Differential item functioning (DIF) analyses of health‐related quality of life instruments using logistic regression. Health Qual Life Outcomes. 2010;8:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mpotos N, Vekeman E, Monsieurs K, Derese A, Valcke M. Knowledge and willingness to teach cardiopulmonary resuscitation: a survey amongst 4273 teachers. Resuscitation. 2013;84:496–500. [DOI] [PubMed] [Google Scholar]
- 35. Toner P, Connolly M, Laverty L, McGrath P, Connolly D, McCluskey DR. Teaching basic life support to school children using medical students and teachers in a ‘peer‐training’ model—results of the ‘ABC for life’ programme. Resuscitation. 2007;75:169–175. [DOI] [PubMed] [Google Scholar]
- 36. Jimenez‐Fabrega X, Escalada‐Roig X, Miro O, Sanclemente G, Diaz N, Gomez X, Villena O, Rodriguez E, Gaspar A, Molina JE, Salvador J, Sanchez M. Comparison between exclusively school teacher‐based and mixed school teacher and healthcare provider‐based programme on basic cardiopulmonary resuscitation for secondary schools. Emerg Med J. 2009;26:648–652. [DOI] [PubMed] [Google Scholar]
- 37. Bohn A, Van Aken HK, Mollhoff T, Wienzek H, Kimmeyer P, Wild E, Dopker S, Lukas RP, Weber TP. Teaching resuscitation in schools: annual tuition by trained teachers is effective starting at age 10. A four‐year prospective cohort study. Resuscitation. 2012;83:619–625. [DOI] [PubMed] [Google Scholar]
- 38. Lukas RP, Van Aken H, Molhoff T, Weber T, Rammert M, Wild E, Bohn A. Kids save lives: a six‐year longitudinal study of schoolchildren learning cardiopulmonary resuscitation: who should do the teaching and will the effects last? Resuscitation. 2016;101:35–40. [DOI] [PubMed] [Google Scholar]
- 39. Baruch Y. Survey response rate levels and trends in organizational research. Hum Relat. 2008;61:1139–1160. [Google Scholar]
- 40. Ajzen I, Driver BL. Prediction of leisure participation from behavioral, normative, and control beliefs—an application of the theory of planned behavior. Leis Sci. 1991;13:185–204. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. All Variables Included in Univariable Analysis of the Association Between Completed CPR Training and Factors Associated With Completed CPR Training
Table S2. Construction of Latent Variables of Teachers' Attitudes Toward CPR Training, Perceived Pressure, and Perceived Behavioral Control to Ensure Student CPR Training
Table S3. Definition of Latent Variables
Table S4. Descriptive Analysis, Univariable Analysis, and Differential Item Functioning for CPR Training and Each Latent Variable
Table S5. Association Between Domains in the Theory of Planned Behavior and Completed CPR Training
Table S6. Characteristics of Nonrespondents
Figure S1. Confirmatory factor analysis.


