Abstract
Background
Acute myocardial infarction is a major cause of hospitalization and death in patients with chronic obstructive pulmonary disease (COPD); however, temporal trends in the management and clinical outcomes of these patients remain unclear.
Methods and Results
We conducted an observational study by using a representative sample of 1 million beneficiaries from the Taiwan National Health Insurance Research Database. Comorbidities, in‐hospital treatment, and outcomes were compared for patients with acute myocardial infarction with and without COPD between 2004 and 2013. Temporal trends in treatment and outcomes were analyzed. We included 6770 patients admitted to hospitals with acute myocardial infarction diagnoses, of whom 1921 (28.3%) had COPD. Fewer patients with COPD received β‐blockers (adjusted odds ratio 0.66, 95% CI 0.59–0.74), angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers (adjusted odds ratio 0.83, 95% CI 0.73–0.93), statins, anticoagulants, dual antiplatelets, and coronary interventions. These patients had higher mortality (in hospital: adjusted hazard ratio 1.25 [95% CI 1.11–1.41]; 1 year: adjusted hazard ratio 1.20 [95% CI 1.09–1.32]) and respiratory failure risk during admission. Temporal trends showed little improvement in mortality in patients with COPD over 10 years. Multivariable logistic regression indicated that dual antiplatelets, β‐blockers, angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers, statins, coronary angiography, and coronary artery bypass grafting surgery were significantly correlated with improved mortality in patients with COPD.
Conclusions
In Taiwan, a lower proportion of patients with COPD received evidence‐based therapies for acute myocardial infarction than did patients without COPD, and their clinical outcomes were inferior. Limited improvement in mortality was observed over the preceding 10 years and is attributable to the underuse of evidence‐based treatments.
Keywords: acute myocardial infarction, chronic obstructive pulmonary disease, mortality, temporal trends, β‐blockers
Subject Categories: Epidemiology, Myocardial Infarction, Cardiovascular Disease, Mortality/Survival, Treatment
Introduction
Chronic obstructive pulmonary disease (COPD) is a major chronic illness. COPD is projected to become the third leading cause of death worldwide by 2020, and its prevalence, morbidity, and mortality are increasing.1 In patients with COPD, cardiovascular disease is the most common comorbidity and a major cause of hospitalization and mortality.2, 3, 4
The management of cardiovascular disease has progressed considerably in recent years. With the development of evidence‐based pharmacological and interventional treatments, the morbidity and mortality of patients with acute myocardial infarction (AMI) have decreased. Nevertheless, studies have reported that evidence‐based therapies, such as β‐blockers and coronary angiography, are underused in patients with both COPD and AMI.5, 6 Moreover, updated epidemiological data on AMI for patients with COPD are scant, and even less is available for the Asian population in particular. The extent to which patients with COPD have received different AMI therapies compared with those received by patients without COPD and the effect of this difference on clinical outcomes remain unclear.
This observational study investigated differences in clinical characteristics, hospital treatments, and outcomes between patients with AMI with or without COPD in Taiwan by using the nationwide population‐based database.
Materials and Methods
Data Collection and Patient Selection
We conducted a retrospective cohort study by using the Taiwan National Health Insurance Research Database (NHIRD). The NHIRD is a large database provided by Taiwan National Health Insurance (NHI), which is a single‐payer, universal, and compulsory health care program covering >99% of Taiwan residents. The NHIRD contains complete outpatient and inpatient electronic claims records, which include individual diagnoses, procedures performed, and medications prescribed. These data are encrypted and deidentified for research purposes. In this study, we used medical claims and registration data retrieved from ≈1 million people randomly sampled from the 24 million beneficiaries of the Taiwan NHI between 2003 and 2013.
This study was approved by the institutional review board of Chang Gung Medical Foundation, which waived the requirement for informed consent (approval number 104‐7549B).
Study Populations and Associated Covariates
From the NHIRD, we identified patients admitted to all hospitals with the diagnosis of AMI (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM] code 410.x) and included them in the study cohort. We longitudinally followed the study cohort from January 2004 to December 2013. Patients were included if they were aged ≥20 years when they experienced the index AMI attack. For each patient, the day of admission for AMI during the study period was assigned as the index day. For patients with multiple admissions, we included only the first admission during the study period. We excluded patients who survived an AMI event but were hospitalized for <2 days.7 Furthermore, we categorized patients into COPD and non‐COPD groups. Patients were included in the COPD group if they had received a diagnosis of COPD at previous hospital discharge or in outpatient departments within 12 months before the index day and were prescribed associated treatment. The diagnosis of COPD was identified with the ICD‐9‐CM codes 491, 492, and 496.8
We retrieved records for associated comorbidities including hypertension, diabetes mellitus, previous myocardial infarction, ischemic heart disease, heart failure, stroke, dyslipidemia, chronic kidney disease, and atrial fibrillation for all patients from both inpatient and outpatient records since 1 year prior to the index day. In addition, we recorded patient age, sex, hospital length of stay (LOS), and complete in‐hospital medical treatments and procedures received during the AMI event.
Outcome Measurements
The primary outcome was in‐hospital mortality. Secondary outcomes included 90‐day mortality, 1‐year mortality, and development of respiratory failure and shock during hospitalization. Death was defined as a patient's withdrawal from the NHI program.9 The date of withdrawal from the Taiwan NHI program has been recognized as an accurate proxy for mortality date.10, 11 In‐hospital mortality was defined as withdrawal within 7 days of discharge, and 90‐day and 1‐year mortality was defined as dropping out of the NHI program within 90 days or 1 year of the index day, respectively. The follow‐up duration lasted from the index day until a patient's death or the end of 2013. Respiratory failure was defined on the basis of the use of invasive or noninvasive mechanical ventilatory support. A shock episode was defined according to the use of norepinephrine, dopamine, epinephrine, or intra‐aortic balloon pumping during admission.
Sensitivity Analysis
Three sensitivity analyses were performed to examine the robustness of results. First, we matched patients in the COPD and non‐COPD groups by using a propensity score that included age, sex, socioeconomic status, comorbidities, and year of the index AMI event in the model. Second, we recategorized patients with asthma (ICD‐9‐CM code 493) and bronchiectasis (ICD‐9‐CM code 494) into the COPD group and reperformed the analyses. Finally, because AMI and unstable angina present similar clinical symptoms, a separate analysis was performed in patients with acute coronary syndrome (ACS; ICD‐9‐CM codes 410, 411.1, and 411.8). However, this analysis included only patients receiving ACS‐associated treatment, namely, dual antiplatelets, anticoagulants, percutaneous coronary intervention (PCI), fibrinolysis, or coronary artery bypass grafting.
Statistical Analysis
Data are reported as median (interquartile range) for continuous variables and as proportion (percentage) for categorical variables. Continuous variables were analyzed using the Mann–Whitney U test. Categorical variables were analyzed using a chi‐square test. We first compared the difference in in‐hospital treatment and outcomes between the COPD and non‐COPD groups by using the multivariable logistic regression model. Variables such as age, sex, socioeconomic status, year of hospitalization, hospital LOS, and comorbidities (diabetes mellitus, hypertension, previous myocardial infarction, ischemic heart disease, congestive heart failure, stroke, dyslipidemia, chronic kidney disease, and atrial fibrillation) were adjusted in the model. In addition, we used the univariable and multivariable logistic regression models to evaluate the effect of other medications and treatments received during hospitalization on the use of individual cardiovascular medications. The medications and treatments evaluated included inhalation therapy (bronchodilator, steroids, or mucolytics), theophylline, oral β‐agonists, mucolytic agents, cough and cold preparations, antibiotics, diuretics, and antiarrhythmics.
We then used Cox proportional hazard models to compare mortality outcomes (in‐hospital, 90‐day, and 1‐year mortality) between the COPD and non‐COPD groups. The survival time was measured from the index day until the date of death or the end of the study (December 31, 2013), whichever occurred earlier. The proportional hazards assumption was evaluated graphically and found to be appropriate. Variables such as age, sex, socioeconomic status, comorbidities, hospital LOS, and year of hospitalization were adjusted in the survival models. Adjusted survival curves were presented using the corrected group prognosis method.12
We estimated temporal trends in in‐hospital treatments and outcomes by using logistic regression in the COPD and non‐COPD groups. We categorized the year of the AMI index event into 5 categories and used them as explanatory variables. A P value of <0.05 indicated a positive trend toward an increasing or decreasing use of the specific treatment with time. In addition, an interaction between the COPD group indicator and the index year was analyzed separately.
We evaluated the effect of in‐hospital treatment on patients with COPD by using univariable and multivariable logistic regression models in which baseline confounding factors, including age, sex, socioeconomic status, comorbidities, hospital LOS, and year of hospitalization were adjusted. Variables in the univariable analysis with P values of <0.15 were subjected to multivariable analysis. A 2‐tailed P value of <0.05 indicated statistical significance. The relative risk was calculated using a modified Poisson regression model with robust error variance.13
For propensity score matching in the sensitivity analyses, we estimated the propensity of patients with COPD by using the logistic regression model. The following variables were included in the model: age, sex, socioeconomic status, comorbidities, hospital LOS, and year of hospitalization. We performed the 1:1 matching by using the nearest neighbor algorithm without replacement and a caliper width of 0.05. A total of 1800 patients with COPD were matched with 1800 patients without COPD. The matched samples were well balanced, with all absolute standardized differences of <0.1. After matching, the odds ratio was calculated using the general estimating equation, and survival data were calculated using Cox proportional hazards models with a robust variance estimator.14
Analyses were performed using SAS version 9.4 (SAS Institute, Inc.).
Results
Baseline Characteristics
From the sample of 1 million people, we included 6770 patients with AMI (Figure 1). Among them, 1921 (28.3%) patients had received a diagnosis of COPD. The median age of the patients with AMI was 70 years (interquartile range 58–79 years). Compared with the patients without COPD, the patients with COPD were older and had more comorbidities (Table 1).
Figure 1.
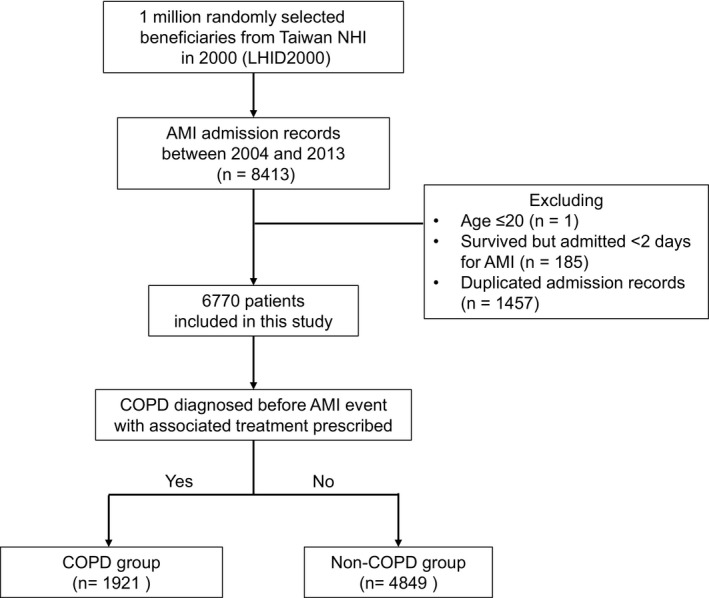
Flow diagram demonstrating patient inclusion and exclusion. AMI indicates acute myocardial infarction; COPD, chronic obstructive pulmonary disease; NHI, National Health Insurance.
Table 1.
Demographic Data of the Study Cohort
| Characteristics | COPD Patients (n=1921) | Non‐COPD Patients (n=4849) | P Value |
|---|---|---|---|
| Patient characteristics | |||
| Age, y, median (IQR) | 77 (68–83) | 67 (55–77) | <0.0001 |
| Male, n (%) | 1306 (68.0) | 3323 (68.5) | 0.6642 |
| Socioeconomic status: monthly income (TWD), n (%) | <0.0001 | ||
| ≥40 000 | 41 (2.1) | 276 (5.7) | |
| 20 000–39 999 | 507 (26.4) | 1453 (30.0) | |
| 1–19 999 | 1158 (60.3) | 2632 (54.3) | |
| Dependent | 215 (11.2) | 488 (10.1) | |
| Medical history, n (%) | |||
| Hypertension | 1375 (71.6) | 2801 (57.8) | <0.0001 |
| Diabetes mellitus | 768 (40.0) | 1727 (35.6) | 0.0008 |
| Previous myocardial infarction | 190 (9.9) | 335 (6.9) | <0.0001 |
| Ischemic heart disease | 822 (42.8) | 1426 (29.4) | <0.0001 |
| Heart failure | 449 (23.4) | 489 (10.1) | <0.0001 |
| Stroke | 432 (22.5) | 645 (13.3) | <0.0001 |
| Dyslipidemia | 495 (25.8) | 1236 (25.5) | 0.8131 |
| Chronic kidney disease | 288 (15.0) | 545 (11.2) | <0.0001 |
| Atrial fibrillation | 160 (8.3) | 152 (3.1) | <0.0001 |
COPD indicates chronic obstructive pulmonary disease; IQR, interquartile range; TWD, Taiwan dollars.
In‐Hospital Treatment and Clinical Outcomes
The median hospital LOS was 6 days (interquartile range 4–12 days). The patients with COPD had longer LOS than did the patients without COPD (median 8 [interquartile range 4–15] versus 6 [interquartile range 4–11] days, P<0.0001). The patients with COPD had a lower likelihood of receiving evidence‐based pharmacological and interventional treatments for AMI, namely, antiplatelets, anticoagulants, β‐blockers, angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers (ACEI/ARB), statins, coronary angiography, PCI, and coronary artery bypass grafting (Table 2). We observed an increasing trend of calcium channel blocker use in the patients with COPD (Table 2). This observation remained consistent after adjusting for age, sex, socioeconomic status, hospital LOS, and comorbidities.
Table 2.
In‐Hospital Treatments and Clinical Outcomes of the Study Cohort
| Outcomes/Therapies | COPD Patients | Non‐COPD Patients | aOR/aHR | 95% CI | P Value | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| In‐hospital treatment | |||||||
| Aspirin | 1579 | 82.2 | 4276 | 88.2 | 0.74 | 0.63–0.86 | 0.0002 |
| Dual antiplatelets | 1375 | 71.6 | 3754 | 77.4 | 0.82 | 0.72–0.94 | 0.0050 |
| Anticoagulantsa | 1458 | 75.9 | 4066 | 83.9 | 0.76 | 0.66–0.88 | 0.0002 |
| β‐Blockers | 885 | 46.1 | 2965 | 61.2 | 0.66 | 0.59–0.74 | <0.0001 |
| Calcium channel blockers | 778 | 40.5 | 1664 | 34.3 | 1.11 | 0.98–1.25 | 0.0866 |
| ACEI/ARB | 1155 | 60.1 | 3286 | 67.8 | 0.83 | 0.73–0.93 | 0.0017 |
| Statins | 754 | 39.3 | 2362 | 48.7 | 0.85 | 0.75–0.96 | 0.0080 |
| Coronary angiography | 1037 | 54.0 | 3296 | 68.0 | 0.76 | 0.67–0.86 | <0.0001 |
| PCI | 780 | 40.6 | 2571 | 53.0 | 0.78 | 0.69–0.88 | <0.0001 |
| CABG | 59 | 3.1 | 256 | 5.3 | 0.57 | 0.41–0.77 | 0.0003 |
| Outcomes | |||||||
| In‐hospital mortality | 489 | 25.5 | 751 | 15.5 | 1.25b | 1.11–1.41 | 0.0003 |
| 90‐day mortality | 577 | 30.0 | 924 | 19.1 | 1.18b | 1.06–1.32 | 0.0028 |
| 1‐year mortality | 769 | 40.0 | 1217 | 25.1 | 1.20b | 1.09–1.32 | 0.0002 |
| Respiratory failure | 573 | 29.8 | 1069 | 22.1 | 1.16 | 1.01–1.32 | 0.0324 |
| Shock episodes | 840 | 43.7 | 1889 | 39.0 | 0.97 | 0.86–1.09 | 0.5783 |
All models were adjusted for age, sex, socioeconomic status, year of hospitalization, hospital length of stay, and comorbidities (diabetes mellitus, hypertension, previous myocardial infarction, ischemic heart disease, congestive heart failure, stroke, dyslipidemia, chronic renal disease, and atrial fibrillation). ACEI/ARB indicates angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers; aHR, adjusted hazard ratio; aOR, adjusted odds ratio; CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; PCI, percutaneous coronary intervention.
Only 189 (2.7%) patients received fibrinolysis. These patients were combined into the anticoagulant group.
Adjusted hazard ratio.
The use of some cardiovascular medications appeared to be affected by other medications and treatments received during hospitalization. The patients receiving theophylline or antibiotics were less often prescribed dual antiplatelets, anticoagulants, β‐blockers, and ACEI/ARB. The patients receiving oral β‐agonists less often received statins and β‐blockers. In contrast, the patients receiving cough and cold preparations or diuretics more often received cardiovascular medications (Table S1). Importantly, COPD remains an independent factor that is correlated with the underuse of several cardiovascular prescriptions.
Regarding clinical outcomes, the patients with COPD had higher risks of in‐hospital, 90‐day, and 1‐year mortality and respiratory failure during hospitalization. The risk of shock episodes, however, did not significantly differ between the 2 groups (Table 2). Moreover, survival curves significantly differed between these 2 groups (Figure 2).
Figure 2.
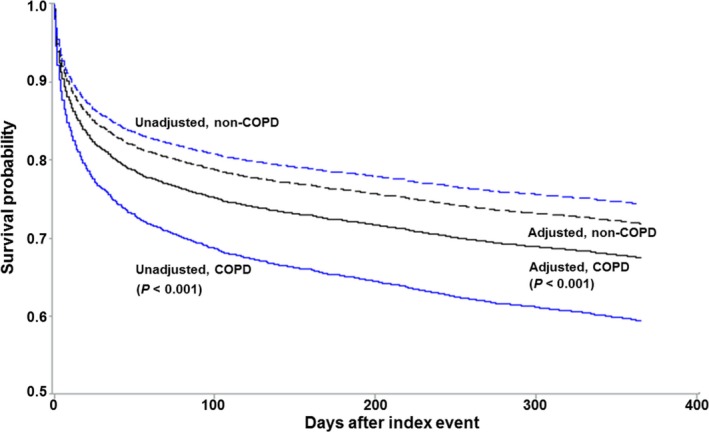
Survival curves of patients with acute myocardial infarction with and without chronic obstructive pulmonary disease (COPD). The adjusted survival curves were adjusted for age, sex, socioeconomic status, year of hospitalization, hospital length of stay, and comorbidities (diabetes mellitus, hypertension, previous myocardial infarction, ischemic heart disease, congestive heart failure, stroke, dyslipidemia, chronic kidney disease, and atrial fibrillation).
Temporal Trends in Treatment and Outcomes
With respect to treatment trends between 2004 and 2013, we observed an increasing use of dual antiplatelets, anticoagulants, and statins in all patients with AMI (Figure 3). Coronary angiography and PCI were also more frequently performed in the patients with AMI (Figure 3). More patients with COPD received β‐blockers with time; however, their percentage remained lower than that of the patients without COPD (Figure 3). The trends of ACEI/ARB use showed no significant change in either group (Figure 3; Table S2).
Figure 3.
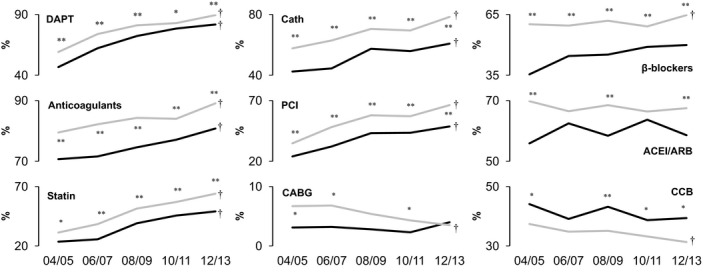
Temporal trends in in‐hospital treatment of acute myocardial infarction between 2004 and 2013. Black lines represent patients with chronic obstructive pulmonary disease (COPD); gray lines represent patients without COPD. *P<0.05, **P<0.01 between patients with and without COPD; † P<0.01 for trend. ACEI/ARB indicates angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers; CABG, coronary artery bypass grafting; Cath, coronary angiography; CCB, calcium channel blockers; DAPT, dual antiplatelet therapy; PCI, percutaneous coronary intervention.
Regarding clinical outcomes over the 10‐year period, in‐hospital, 90‐day, and 1‐year mortality and the occurrence of respiratory failure and shock episodes decreased in the patients without COPD (Figure 4). In the COPD group, although only 1‐year mortality and the occurrence of respiratory failure decreased, a decreasing trend of in‐hospital mortality was observed (Figure 4; Table S3).
Figure 4.
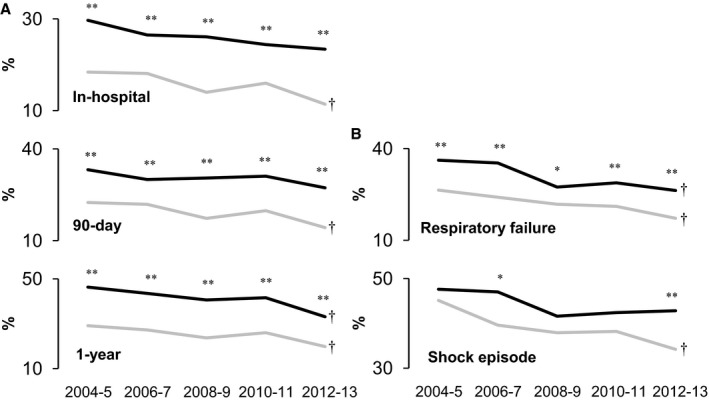
Temporal trends in (A) mortality and (B) morbidities of acute myocardial infarction between 2004 and 2013. Black lines represent patients with chronic obstructive pulmonary disease (COPD); gray lines represent patients without COPD. *P<0.05, **P<0.01 between patients with and without COPD; † P<0.01 for trend.
Influence of Possible In‐Hospital Treatment on In‐Hospital Mortality and Sensitivity Analysis
We investigated the effect of in‐hospital treatment on the in‐hospital mortality of the patients with COPD. After adjusting for baseline covariates, we observed that several treatment modalities were associated with a decreased risk of in‐hospital mortality, namely, dual antiplatelets, β‐blockers, ACEI/ARB, statins, coronary angiography, and coronary artery bypass grafting (Table 3). The β‐blockers and ACEI/ARB were associated with a substantially lower relative risk of in‐hospital mortality (the risk differences were 16% and 43%, respectively). Compared with patients without COPD, the patients with COPD still had a higher risk of in‐hospital mortality after adjustment for dual antiplatelets, anticoagulants, and coronary angiography; however, further adjustment for ACEI/ARB or β‐blockers rendered the difference nonsignificant (Figure 5). Moreover, in‐hospital, 90‐day, and 1‐year mortality did not differ between the patients with COPD who received dual antiplatelets, β‐blockers, statins, ACEI/ARB, and coronary revascularization and the patients without COPD (Table S4). In contrast, the patients with COPD who did not receive cardiac catheterization had higher in‐hospital mortality and an increasing trend of 90‐day and 1‐year mortality than did the patients without COPD (Table S4).
Table 3.
Univariable and Multivariable Models of Acute Treatment on In‐Hospital Mortality of Patients With Both COPD and AMI
| Outcomes: In‐Hospital Mortality | Univariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| Acute Treatment | RR | 95% CI | P Value | RR | 95% CI | P Value |
| Dual antiplatelets | 0.41 | 0.35–0.48 | <0.0001 | 0.85 | 0.72–0.99 | 0.0423 |
| Anticoagulants | 0.53 | 0.46–0.62 | <0.0001 | 0.92 | 0.79–1.06 | 0.2346 |
| β‐Blockers | 0.46 | 0.39–0.56 | <0.0001 | 0.84 | 0.71–1.00 | 0.0476 |
| Calcium channel blockers | 0.82 | 0.70–0.95 | 0.0107 | 1.04 | 0.91–1.19 | 0.5421 |
| ACEI/ARB | 0.33 | 0.27–0.39 | <0.0001 | 0.57 | 0.48–0.68 | <0.0001 |
| Statins | 0.40 | 0.32–0.50 | <0.0001 | 0.69 | 0.56–0.85 | 0.0005 |
| Dobutamine | 1.33 | 1.14–1.56 | 0.0004 | 1.18 | 1.04–1.35 | 0.0137 |
| Dopamine/norepinephrine | 5.13 | 4.22–6.23 | <0.0001 | 4.33 | 3.57–5.25 | <0.0001 |
| Coronary angiography | 0.38 | 0.31–0.46 | <0.0001 | 0.59 | 0.44–0.80 | 0.0005 |
| PCI | 0.45 | 0.37–0.56 | <0.0001 | 1.05 | 0.76–1.45 | 0.7620 |
| CABG | 0.37 | 0.16–0.86 | 0.0211 | 0.35 | 0.15–0.84 | 0.0193 |
All models were adjusted for age, sex, socioeconomic status, year of hospitalization, hospital length of stay, and comorbidities (diabetes mellitus, hypertension, previous myocardial infarction, ischemic heart disease, congestive heart failure, stroke, dyslipidemia, chronic kidney disease, and atrial fibrillation). ACEI/ARB indicates angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers; AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; PCI, percutaneous coronary intervention; RR, relative risk.
Figure 5.
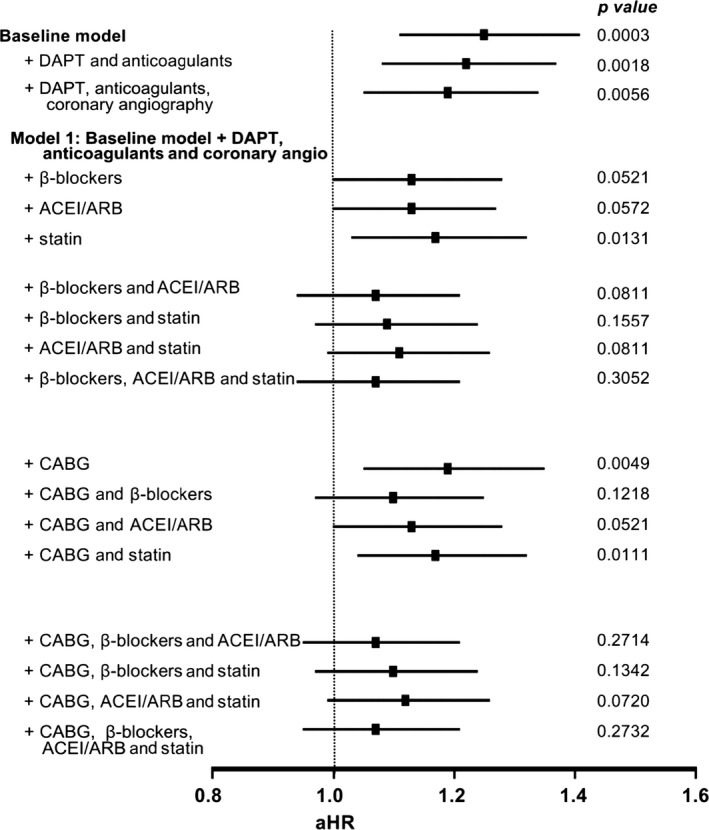
In‐hospital mortality risk of acute myocardial infarction between patients with and without chronic obstructive pulmonary disease. The baseline model was adjusted for age, sex, socioeconomic status, hospital length of stay, year of hospitalization, and comorbidities (diabetes mellitus, hypertension, ischemic heart disease, dyslipidemia, congestive heart failure, stroke, chronic renal disease, and atrial fibrillation); Model 1 was further adjusted for dual antiplatelets, anticoagulants, and coronary angiography. ACEI/ARB indicates angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers; aHR, adjusted hazard ratio; CABG, coronary artery bypass grafting; DAPT, dual antiplatelet therapy.
In the sensitivity analysis, in‐hospital, 90‐day, and 1‐year mortality were consistently higher in the COPD group. In addition, all 3 analyses consistently demonstrated that the COPD group had a lower likelihood of receiving evidence‐based treatments for AMI during hospitalization (Table S5).
Discussion
The results of our population‐based observational study of the patients with AMI in Taiwan between 2004 and 2013 revealed significant differences in in‐hospital treatment and clinical outcomes between the patients with and without COPD. Over these 10 years, a higher proportion of the patients with AMI received improved cardiac therapies and coronary angiography, bringing about a decrease in both short‐ and long‐term mortality in the patients without COPD. The patients with COPD, however, had a lower likelihood of receiving evidence‐based pharmacological or interventional treatments. These patients also exhibited higher short‐ and long‐term mortality, with only limited improvement over the past 10 years. Our findings are consistent with those of a previous study conducted in the United States.6 The Worcester Heart Attack Study reported that patients with COPD in their cohort were less likely to receive anticoagulants, β‐blockers, statins or lipid‐lowering agents, or cardiac invasive treatment between 1997 and 2007. Calcium channel blockers were used more often in patients with COPD; however, the use of dual antiplatelets and ACEI/ARB did not decrease.6
Regarding clinical outcomes, in our study, the patients with COPD had higher in‐hospital, 90‐day, and 1‐year mortality than did the patients without COPD. In previous studies, however, higher in‐hospital mortality was not observed consistently.5, 6, 15, 16 The overall mortality in our study was higher than that in the Worcester study. This might be attributable to the difference in ethnicity17 or possibly to the underuse of evidence‐based AMI treatment.18 The underuse of medications such as β‐blockers and ACEI/ARB is not infrequent in Asian countries (Table 4).5, 17, 19, 20, 21 In the 2005–2007 Worcester study cohort, >90% of patients received β‐blockers; however, in our cohort, only 57% of the patients received β‐blockers. If we assume that the patients in our cohort who did not receive β‐blockers (n=2920) had 20% mortality, then the mortality difference between the 2 studies can be accounted for. With respect to other treatments, the proportions of patients who received ACEI/ARB, anticoagulants, PCI, or coronary artery bypass grafting were similar in the 2 studies.
Table 4.
Medications Prescribed Proportions in Different Countries
| Studies | Country or Region | β‐Blockers | ACEI/ARB | Lipid‐Lowering Agents/Statins | Year |
|---|---|---|---|---|---|
| Qian et al17 | USA | 98.5 | 93.6 | 94.5 | 2008 |
| Daida et al19 | Japan | 49.5 | 78.5 | 77.8 | 2008–2009 |
| Lee et al21 | Korea | 72.7 | 81.5 | 77.2 | 2005–2008 |
| Zubaid et al5, 20 | Middle East | 67.1 | 63.2 | 81.0 | 2006–2007 |
| Our study | Taiwan | 64.5 | 67.5 | 64.0 | 2012–2013 |
ACEI/ARB indicates angiotensin‐converting enzyme inhibitors/angiotensin II receptor blockers.
Mortality in our cohort was higher than that in the Taiwan ACS Full Spectrum Registry, which recruited 3183 patients between October 2008 and January 2010.22 In‐hospital mortality was only 1.6% and 1‐year mortality was only 7.5%. The difference in mortality between the registry and our patient cohort may be attributable to differences in the treatment received and the sampling method. The Taiwan ACS Registry recruited patients from 39 hospitals, of which 19 were tertiary medical centers. PCI was performed in 84.4% of patients, which almost doubled our proportion. Thus, this cohort represents those patients who received aggressive treatment for ACS in Taiwan. In contrast, in 2004 and 2005, only 57.7% and 34.7% of our patients without COPD underwent coronary angiography and PCI, respectively. Moreover, in 2008 and 2009, only 57.9% of our patients without COPD received PCI. This finding suggests that our patient cohort encompasses a broader range of hospital levels and patient characteristics. Moreover, the registry required informed consent, and 10% of patients were lost to follow‐up in the following year, thus mortality may have been underestimated. In contrast, we considered dropping out from the NHI as an indicator of death. This may have resulted in the overestimation of mortality.
We hypothesized that the higher mortality of patients with COPD was due to the underuse of evidence‐based treatment modalities7, 18, 23, 24; therefore, we examined the individual effect of in‐hospital treatment on clinical outcomes. Our data indicate that dual antiplatelets, β‐blockers, ACEI/ARB, statins, coronary angiography, and coronary artery bypass grafting independently reduced in‐hospital mortality in patients with COPD. The β‐blockers and ACEI/ARB were associated with a substantially lower relative risk of in‐hospital mortality. The risk of in‐hospital mortality persisted in the patients with COPD after adjusting for dual antiplatelets, anticoagulants, and coronary angiography; however, after further adjusting for β‐blockers or ACEI/ARB, the risk became nonsignificant. Mortality did not differ between the patients with COPD who received a combination of dual antiplatelets, β‐blockers, statins, ACEI/ARB, and coronary revascularization and the patients without COPD. These data indicate that the risk of mortality was lower in patients with COPD who received evidence‐based treatment modalities. Consequently, we suggest that all evidence‐based pharmacological and interventional treatments should be aggressively used in all patients with AMI, particularly in those with COPD. The underuse of β‐blockers in patients with both COPD and AMI has been reported.5, 25, 26, 27, 28 Past research has indicated that the main concern is bronchospasm; however, recent studies have reported that cardioselective β‐blockers generally do not cause bronchospasm, and the use of β‐blockers may even reduce the risk of exacerbations in patients with COPD.29, 30, 31, 32 We believe that β‐blockers exert beneficial effects on patients with both COPD and AMI, lowering their mortality.
In this study, we could not evaluate whether a patient was indicated or contraindicated for a specific treatment modality. The patients with COPD who did not receive coronary angiography had a higher risk of in‐hospital mortality than those without COPD. This may have occurred because the patients could not tolerate the procedure or their physicians withheld the treatment owing to concerns about risk. Nevertheless, the exact reason could not be established. Considering the nature of the claims database, we could not differentiate between the 2 scenarios. Likewise, the reason for the nonadministration of β‐blockers or ACEI/ARB to the patients with COPD could not be evaluated. Because of our data limitations, we could not investigate whether this nonadministration was because of the concern regarding bronchospasm or owing to the patient having already developed hypotension, preventing their use. This situation possibly generated confounding results, that is, more severely ill patients who were unable to receive β‐blockers or ACEI/ARB might have contributed to the increased mortality of patients not receiving medications. Nevertheless, considering that β‐blockers and ACEI/ARB remain the standard adjunct therapy in AMI, we continue to advocate for their use in patients with COPD. These treatments should be administrated to those patients who have no contraindications for a specific AMI treatment.
Our study has several limitations. First, we used data extracted from the NHIRD, which is a claims database and does not provide additional information, such as cigarette smoking, body mass index, or the lifestyle of the beneficiary. Clinically relevant data including disease manifestation, laboratory data, and examination results (eg, the lung function test) are also not provided; therefore, unspecified potential confounders may have been overlooked. Second, the diagnosis of AMI and COPD relied solely on the presence of diagnostic codes in a beneficiary's record. Miscoding could have happened but was difficult to identify. Moreover, we could not validate the diagnosis of COPD with respect to the standard diagnostic criteria (ie, the ratio between the forced expiratory volume in 1 second and the forced vital capacity). A study conducted in Michigan identified patients with COPD having postbronchodilator spirometry results and reported that the ICD‐9‐CM codes (491, 492, 496, and 493.2) had only 76% and 67% sensitivity and specificity, respectively.33 To the best of our knowledge, no study has validated the accuracy of the NHIRD diagnostic codes for COPD. Moreover, because the NHIRD does not contain laboratory or examination results, we could not assess the sensitivity and specificity of the NHIRD diagnostic codes for the classification of COPD. It is possible that less symptomatic patients often do not receive a diagnosis of COPD or that our patients with COPD were more symptomatic than is usual. These circumstances may have accentuated the difference in clinical outcomes. Regarding the diagnosis of AMI, a study validated the NHIRD diagnosis coding,34 and our sensitivity analysis of the patients receiving ACS‐specific treatment demonstrated consistent results. Third, owing to the inherent limitations of observational studies, we could not address the unmeasurable and unrecorded confounding factors; therefore, bias (eg, confounding by indications) may exist.
Conclusion
In our study, patients with COPD were less likely than those without COPD to receive evidence‐based pharmacological and interventional treatments during hospitalization for AMI. They also had inferior clinical outcomes compared with those of the patients without COPD. Limited improvement of clinical outcomes was observed during the 10‐year study period. Several evidence‐based treatments, especially β‐blockers and ACEI/ARB, were significantly correlated with survival.
Disclosures
None.
Supporting information
Table S1. Effects of In‐Hospital Medications and Cardiovascular Prescriptions in the Study Cohort
Table S2. Temporal Trends of In‐Hospital Treatment in Acute Myocardial Infarction Patients With or Without Chronic Obstructive Pulmonary Disease Between 2004 and 2013
Table S3. Temporal Trends in Clinical Outcomes in Acute Myocardial Infarction Patients With and Without Chronic Obstructive Pulmonary Disease Between 2004 and 2013
Table S4. The Mortality of Acute Myocardial Infarction Between Patients With and Without Chronic Obstructive Pulmonary Disease Who Received Specific Treatment
Table S5. Results of Sensitivity Analyses: Hazard Ratio for Mortality Outcomes and Odds Ratio for Receiving Specific Treatment and Motility of Different Groups of Patients
(J Am Heart Assoc. 2017;6:e004525. DOI: 10.1161/JAHA.116.004525.)
References
- 1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. [DOI] [PubMed] [Google Scholar]
- 2. de Miguel Diez J, Chancafe Morgan J, Jimenez Garcia R. The association between COPD and heart failure risk: a review. Int J Chron Obstruct Pulmon Dis. 2013;8:305–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bellocchia M, Masoero M, Ciuffreda A, Croce S, Vaudano A, Torchio R, Boita M, Bucca C. Predictors of cardiovascular disease in asthma and chronic obstructive pulmonary disease. Multidiscip Respir Med. 2013;8:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cheng SL, Chan MC, Wang CC, Lin CH, Wang HC, Hsu JY, Hang LW, Chang CJ, Perng DW, Yu CJ. COPD in Taiwan: a national epidemiology survey. Int J Chron Obstruct Pulmon Dis. 2015;10:2459–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hadi HA, Zubaid M, Al Mahmeed W, El‐Menyar AA, Ridha M, Alsheikh‐Ali AA, Singh R, Assad N, Al Habib K, Al Suwaidi J. Prevalence and prognosis of chronic obstructive pulmonary disease among 8167 Middle Eastern patients with acute coronary syndrome. Clin Cardiol. 2010;33:228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stefan MS, Bannuru RR, Lessard D, Gore JM, Lindenauer PK, Goldberg RJ. The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction: a 10‐year retrospective observational study. Chest. 2012;141:1441–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee CH, Cheng CL, Yang YH, Chao TH, Chen JY, Liu PY, Lin CC, Chan SH, Tsai LM, Chen JH, Lin LJ, Li YH. Trends in the incidence and management of acute myocardial infarction from 1999 to 2008: Get With the Guidelines Performance Measures in Taiwan. J Am Heart Assoc. 2014;3:e001066 DOI: 10.1161/JAHA.114.001066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang MT, Lo YW, Tsai CL, Chang LC, Malone DC, Chu CL, Liou JT. Statin use and risk of COPD exacerbation requiring hospitalization. Am J Med. 2013;126:598–606.e592. [DOI] [PubMed] [Google Scholar]
- 9. Wu CY, Chen YJ, Ho HJ, Hsu YC, Kuo KN, Wu MS, Lin JT. Association between nucleoside analogues and risk of hepatitis B virus‐related hepatocellular carcinoma recurrence following liver resection. JAMA. 2012;308:1906–1914. [DOI] [PubMed] [Google Scholar]
- 10. Lien HM, Chou SY, Liu JT. Hospital ownership and performance: evidence from stroke and cardiac treatment in Taiwan. J Health Econ. 2008;27:1208–1223. [DOI] [PubMed] [Google Scholar]
- 11. Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH. Validity of in‐hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int J Cardiol. 2015;201:96–101. [DOI] [PubMed] [Google Scholar]
- 12. Ghali WA, Quan H, Brant R, van Melle G, Norris CM, Faris PD, Gallbraith PD, Knudtson ML; APPROACH (Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease) Investigators . Comparison of 2 methods for calculating adjusted survival curves from proportional hazards models. JAMA. 2001;286:1494–1497. [DOI] [PubMed] [Google Scholar]
- 13. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 14. Austin PC. The use of propensity score methods with survival or time‐to‐event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33:1242–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hawkins NM, Huang Z, Pieper KS, Solomon SD, Kober L, Velazquez EJ, Swedberg K, Pfeffer MA, McMurray JJ, Maggioni AP; Valsartan in Acute Myocardial Infarction Trial Investigators . Chronic obstructive pulmonary disease is an independent predictor of death but not atherosclerotic events in patients with myocardial infarction: analysis of the Valsartan in Acute Myocardial Infarction Trial (VALIANT). Eur J Heart Fail. 2009;11:292–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Salisbury AC, Reid KJ, Spertus JA. Impact of chronic obstructive pulmonary disease on post‐myocardial infarction outcomes. Am J Cardiol. 2007;99:636–641. [DOI] [PubMed] [Google Scholar]
- 17. Qian F, Ling FS, Deedwania P, Hernandez AF, Fonarow GC, Cannon CP, Peterson ED, Peacock WF, Kaltenbach LA, Laskey WK, Schwamm LH, Bhatt DL; Get With The Guidelines Steering Committee and Investigators . Care and outcomes of Asian‐American acute myocardial infarction patients: findings from the American Heart Association Get With the Guidelines‐Coronary Artery Disease program. Circ Cardiovasc Qual Outcomes. 2012;5:126–133. [DOI] [PubMed] [Google Scholar]
- 18. Chung SC, Gedeborg R, Nicholas O, James S, Jeppsson A, Wolfe C, Heuschmann P, Wallentin L, Deanfield J, Timmis A, Jernberg T, Hemingway H. Acute myocardial infarction: a comparison of short‐term survival in national outcome registries in Sweden and the UK. Lancet. 2014;383:1305–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, Kimura T, Matsubara T, Ikari Y, Kimura K, Tsukahara K, Origasa H, Morino Y, Tsutsui H, Kobayashi M, Isshiki T; PACIFIC investigators . Management and two‐year long‐term clinical outcome of acute coronary syndrome in Japan: prevention of atherothrombotic incidents following ischemic coronary attack (PACIFIC) registry. Circ J. 2013;77:934–943. [DOI] [PubMed] [Google Scholar]
- 20. Zubaid M, Rashed WA, Almahmeed W, Al‐Lawati J, Sulaiman K, Al‐Motarreb A, Amin H, Al Suwaidi J, Alhabib K. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE). Acta Cardiol. 2009;64:439–446. [DOI] [PubMed] [Google Scholar]
- 21. Lee JH, Yang DH, Park HS, Cho Y, Jeong MH, Kim YJ, Kim KS, Hur SH, Seong IW, Hong TJ, Cho MC, Kim CJ, Jun JE, Park WH, Chae SC; Korea Acute Myocardial Infarction Registory Investigators . Suboptimal use of evidence‐based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J. 2010;159:1012–1019. [DOI] [PubMed] [Google Scholar]
- 22. Chiang FT, Shyu KG, Wu CJ, Mar GY, Hou CJ, Li AH, Wen MS, Lai WT, Lin SJ, Kuo CT, Kuo C, Li YH, Huang JJ; ACS Full Spectrum Registry Investigators . Predictors of 1‐year outcomes in the Taiwan Acute Coronary Syndrome Full Spectrum Registry. J Formos Med Assoc. 2014;113:794–802. [DOI] [PubMed] [Google Scholar]
- 23. McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL. Reduction in acute myocardial infarction mortality in the United States: risk‐standardized mortality rates from 1995‐2006. JAMA. 2009;302:767–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Albouaini K, Andron M, Alahmar A, Egred M. Beta‐blockers use in patients with chronic obstructive pulmonary disease and concomitant cardiovascular conditions. Int J Chron Obstruct Pulmon Dis. 2007;2:535–540. [PMC free article] [PubMed] [Google Scholar]
- 26. Chen J, Radford MJ, Wang Y, Marciniak TA, Krumholz HM. Effectiveness of beta‐blocker therapy after acute myocardial infarction in elderly patients with chronic obstructive pulmonary disease or asthma. J Am Coll Cardiol. 2001;37:1950–1956. [DOI] [PubMed] [Google Scholar]
- 27. Andell P, Erlinge D, Smith JG, Sundstrom J, Lindahl B, James S, Koul S. β‐blocker use and mortality in COPD patients after myocardial infarction: a Swedish nationwide observational study. J Am Heart Assoc. 2015;4:e001611 DOI: 10.1161/JAHA.114.001611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Egred M, Shaw S, Mohammad B, Waitt P, Rodrigues E. Under‐use of beta‐blockers in patients with ischaemic heart disease and concomitant chronic obstructive pulmonary disease. QJM. 2005;98:493–497. [DOI] [PubMed] [Google Scholar]
- 29. Rutten FH, Zuithoff NP, Hak E, Grobbee DE, Hoes AW. β‐blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:880–887. [DOI] [PubMed] [Google Scholar]
- 30. Ni Y, Shi G, Wan H. Use of cardioselective β‐blockers in patients with chronic obstructive pulmonary disease: a meta‐analysis of randomized, placebo‐controlled, blinded trials. J Int Med Res. 2012;40:2051–2065. [DOI] [PubMed] [Google Scholar]
- 31. Salpeter S, Ormiston T, Salpeter E. Cardioselective beta‐blockers for reversible airway disease. Cochrane Database Syst Rev. 2002;(4):CD002992. [DOI] [PubMed] [Google Scholar]
- 32. Salpeter S, Ormiston T, Salpeter E. Cardioselective beta‐blockers for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;(4):CD003566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cooke CR, Joo MJ, Anderson SM, Lee TA, Udris EM, Johnson E, Au DH. The validity of using ICD‐9 codes and pharmacy records to identify patients with chronic obstructive pulmonary disease. BMC Health Serv Res. 2011;11:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH. Validation of acute myocardial infarction cases in the National Health Insurance Research Database in Taiwan. J Epidemiol. 2014;24:500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Effects of In‐Hospital Medications and Cardiovascular Prescriptions in the Study Cohort
Table S2. Temporal Trends of In‐Hospital Treatment in Acute Myocardial Infarction Patients With or Without Chronic Obstructive Pulmonary Disease Between 2004 and 2013
Table S3. Temporal Trends in Clinical Outcomes in Acute Myocardial Infarction Patients With and Without Chronic Obstructive Pulmonary Disease Between 2004 and 2013
Table S4. The Mortality of Acute Myocardial Infarction Between Patients With and Without Chronic Obstructive Pulmonary Disease Who Received Specific Treatment
Table S5. Results of Sensitivity Analyses: Hazard Ratio for Mortality Outcomes and Odds Ratio for Receiving Specific Treatment and Motility of Different Groups of Patients


