Abstract
Background
Preceding release of the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) cholesterol guidelines, prescribers aimed for specific low‐density lipoprotein cholesterol (LDL‐C) goals in patients with atherosclerotic cardiovascular disease (ASCVD). The 2013 guidelines changed this focus to treating patients with appropriate statin intensity given their ASCVD risk. We examined statin use and LDL‐C levels before and after the 2013 ACC/AHA guidelines in patients with clinical ASCVD as defined in the guidelines.
Methods and Results
We conducted a retrospective cohort study of adult commercial and Medicare Advantage health plan enrollees in the Optum Research Database. Patients had ≥1 claim with a diagnosis of clinical ASCVD between November 1, 2012 and December 31, 2014 and were continuously enrolled 6 months before (baseline) and 7 months after (follow‐up) the first ASCVD visit. Patients were assigned to monthly cohorts based on ASCVD event month. Statin use and intensity were measured at baseline and first month of follow‐up. LDL‐C changes were assessed using ordinary least squares regression. For 90 287 patients, mean (SD) age was 68 (12) years; 50% were female; and 30% had commercial insurance. Statin use remained consistent before and after guidelines (32% and 31%, respectively). Of patients receiving statins, high‐intensity use increased by 4 percentage points 1 year after guidelines (P<0.001). Mean LDL‐C levels were 2.4 mmol/L (94 mg/dL) both pre‐ and postguidelines.
Conclusions
Statin use and mean monthly LDL‐C before and after the guidelines remained largely unchanged; statin intensity increased modestly. More effort may be needed to increase guideline understanding and adherence to improve treatment of high‐risk patients.
Keywords: guideline, lipid‐lowering therapy, low‐density lipoprotein cholesterol, statin therapy
Subject Categories: Lipids and Cholesterol, Cardiovascular Disease
Introduction
High levels of low‐density lipoprotein cholesterol (LDL‐C) are associated with greater risk of atherosclerotic cardiovascular disease (ASCVD).1 Approximately 85.6 million people in the United States have at least 1 type of cardiovascular disease (CVD).2 An additional 45 million people in the United States have either a ≥7.5% 10‐year risk of a cardiovascular event (33 million) or a >5% to 7.4% 10‐year risk of a cardiovascular event (12.8 million).2 For patients at high risk for cardiovascular events or with ASCVD, statins are considered standard first‐line therapy to lower LDL‐C. The appropriate statin dose is important to effectively lower LDL‐C and therefore reduce the risk of ASCVD and cardiovascular events; however, not all patients are able to sufficiently lower their LDL‐C levels, even at the maximally tolerated statin dose.1 Approximately 40% of patients are unable to adequately lower their LDL‐C levels despite high‐intensity statin therapy.3 For these patients, treatment regimens may be modified to include a higher statin dose, a switch to a different statin, or combination therapy with other lipid‐lowering agents such as ezetimibe, bile acid sequestrants, niacin, or, when appropriate, an inhibitor of proprotein convertase subtilisin/kexin type 9 (PCSK9).
Preceding the release of the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) blood cholesterol guidelines (hereafter referred to as the “2013 guidelines” or simply “guidelines”), LDL‐C goals were <4.1 mmol/L (160 mg/dL) for patients with a single CVD risk factor, <3.4 mmol/L (130 mg/dL) for patients with 2 or more risk factors, and <2.6 mmol/L (100 mg/dL) for patients with known CVD or risk factor equivalent.4 The guidelines were revised in 2013 to recommend moving away from a “treating to goal” approach with respect to LDL‐C1 and instead focus on treating with the most appropriate statin intensity based on the patient's risk. The 4 statin benefit groups described in the guidelines are (1) patients with clinical ASCVD, (2) adult patients with LDL‐C ≥4.9 mmol/L (190 mg/dL), (3) patients aged 40 to 75 years with diabetes mellitus and LDL‐C levels 1.8 to 4.9 mmol/L (70–189 mg/dL), and (4) patients with an estimated 10‐year ASCVD risk ≥7.5% and LDL‐C levels 1.8 to less than 4.9 mmol/L (70–189 mg/dL; primary prevention).1 With some exceptions for age and risk, in general, high‐intensity statin therapy is recommended for those in statin benefit groups 1 and 2, whereas moderate‐ or high‐intensity statin therapy is recommended for most patients in statin benefit group 3. For statin benefit group 4, the recommendation is to estimate 10‐year ASCVD risk and engage in patient‐clinician discussions to determine an appropriate course of action.5 In addition, the 2013 guidelines no longer recommend monitoring LDL‐C to assess achievement of a particular LDL‐C goal, but instead recommend monitoring LDL‐C to determine adherence and anticipated therapeutic response.
Few studies have evaluated real‐world data to examine the degree to which statin prescribing patterns and LDL‐C levels changed following the release of the new guidelines. The current study is a retrospective analysis of administrative claims and laboratory data with the objectives of describing (1) statin use (including intensity) and (2) LDL‐C levels 1 year before to 1 year after the introduction of the 2013 guidelines in the patient group with highest cardiovascular risk—those with ASCVD. This analysis provides insight into whether the updated guidelines have resulted in meaningful changes in statin use or intensity and corresponding changes in levels of LDL‐C. Additionally, evaluation of the number of LDL‐C orders before and after the 2013 ACC/AHA guidelines were released may provide insight into whether the guideline changes have impacted monitoring of LDL‐C by clinicians.
Methods
Data Source
This was a retrospective analysis of administrative claims data from May 1, 2012 through July 31, 2015 in the Optum Research Database. The database includes medical and pharmacy claims data linked to enrollment information and laboratory data from a large United States health insurer offering both commercial and Medicare Advantage health plans. The individuals covered by these health plans, ≈13 million per year, are geographically diverse across the United States, with the greatest proportion in the Midwest and South Census regions. The insurer provides coverage for physician, hospital, and prescription drug services. All administrative claims data were de‐identified and compliant with the provisions of the Health Insurance Portability and Accountability Act of 1996.
Study Design
The index event was the first ASCVD outpatient visit (physician office, outpatient hospital, or emergency department) or inpatient hospitalization during the identification period of November 1, 2012 through December 31, 2014.
The baseline period was the 180 days immediately preceding the index event. Study follow‐up started on the index date (the day after the index event) and continued for 210 days. Patients were assigned to a monthly cohort based on the month of the index event (ie, index month). Cohort labels corresponded to each month before and after the November 1, 2013 guideline date. November 2012 was month −12, October 2013 was month −1, November 2013 was month 0 (guidelines implementation), December 2013 was month 1, and December 2014 was month 13 (Figure 1). Patients were included in mutually exclusive subgroups based on baseline and follow‐up statin use (new use vs pre‐existing use vs no use) and statin intensity (high, moderate, or low).
Figure 1.
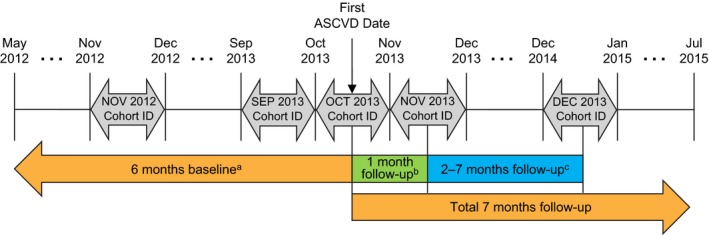
Study design. A total of 26 monthly cohorts were defined based on the month of the first qualifying clinical ASCVD visit. aOutcomes collected included past statin use and comorbidities. bOutcomes collected included overall statin use and high‐intensity statin use. cOutcomes collected included low‐density lipoprotein cholesterol (LDL‐C) levels and patients achieving LDL‐C goal. ASCVD indicates atherosclerotic cardiovascular disease; ID, identification.
Patient Selection
Patients were adults with clinical ASCVD and ≥1 LDL‐C test result. Specifically, patients were required to have ≥1 nondiagnostic medical claim with a code in the primary position for a clinical ASCVD condition or procedure during the identification period. ASCVD conditions and procedures included acute coronary syndrome, history of myocardial infarction, stable or unstable angina, coronary or peripheral artery revascularization, peripheral artery disease, ischemic stroke, and transient ischemic attack. Patients had to be ≥21 years of age as of the index date and continuously enrolled in their health plan with medical and pharmacy benefits from the start of the 180‐day baseline through the end of the 210‐day follow‐up, with ≥1 valid LDL‐C test result in the laboratory database between days 30 and 210 after the index date. Patients who died during an inpatient stay before the index date, were pregnant, had actively treated cancer, or were undergoing lipoprotein apheresis were excluded from the study. In addition, all patients were required to have complete enrollment and demographic data.
Study Measures
Study outcomes included statin use and intensity of statin before and after the 2013 guidelines release, and LDL‐C levels. Statin use during the baseline period and the first month of follow‐up was identified by a pharmacy claim for a statin and further categorized by statin intensity using the classifications described in the revised guidelines (Table 1).1 The count of LDL‐C results per patient (representing LDL‐C orders) and laboratory results during months 2 to 7 of follow‐up were assessed. Other clinical characteristics assessed included clinical ASCVD conditions or procedures on the index date. Demographic characteristics assessed included index month/year, age, sex, insurance type, and geographical region.
Table 1.
Classification of Statin Intensitya
| Intensity | Drug and Dosage |
|---|---|
| High‐intensity statin | Atorvastatin 40 to 80 mg or |
| Rosuvastatin 20 to 40 mg | |
| Moderate‐intensity statin | Atorvastatin 10 to 20 mg or |
| Rosuvastatin 5 to 10 mg or | |
| Simvastatin 20 to 40 mg or | |
| Pravastatin 40 to 80 mg or | |
| Lovastatin 40 mg or | |
| Fluvastatin 40 to 80 mg or | |
| Pitavastatin 2 to 4 mg | |
| Low‐intensity statin | Simvastatin 10 mg or |
| Pravastatin 10 to 20 mg or | |
| Lovastatin 20 mg or | |
| Fluvastatin 20 to 40 mg or | |
| Pitavastatin 1 mg |
Based on Stone et al 2013 American College of Cardiology/American Heart Association guidelines.1
Statistical Analysis
Study variables were analyzed descriptively. Frequencies and percentages are provided for categorical variables and means, medians, and SDs are provided for continuous variables. Ordinary least squares regression was used to assess the change in mean monthly LDL‐C results during follow‐up. Covariates in the model included baseline demographic characteristics.
Results
Patients
A total of 90 287 patients across 26 monthly cohorts were included in the analysis (Figure 2). Demographic characteristics were similar across each monthly cohort. For the overall sample, mean (SD) age was 68 (12) years, 50% were male, 30% had commercial insurance, and a little more than one half (55%) were located in the South (Table 2). Peripheral artery revascularization was the most common ASCVD procedure met for study inclusion (Table 2).
Figure 2.

Patient attrition. ASCVD indicates atherosclerotic cardiovascular disease; LDL‐C, low‐density lipoprotein cholesterol.
Table 2.
Baseline Demographic and Clinical Characteristics Before, During, and Following Release of Guidelines
| Month −12 to −2 (N=45 179) | Month −1 to 1 (N=8576) | Month 2 to 13 (N=36 532) | Total (N=90 287) | |
|---|---|---|---|---|
| Age, mean y (SD) | 69.2 (11.5) | 67.3 (11.7) | 67.6 (11.7) | 68.4 (11.6) |
| Male, n (%) | 22 857 (50.6) | 4256 (49.6) | 18 014 (49.3) | 45 127 (50.0) |
| Insurance type, n (%) | ||||
| Commercial | 12 863 (28.5) | 2866 (33.4) | 11 754 (32.2) | 27 483 (30.4) |
| Medicare advantage | 32 316 (71.5) | 5710 (66.6) | 24 778 (67.8) | 62 804 (69.6) |
| Geographical region, n (%) | ||||
| Northeast | 12 725 (28.2) | 2210 (25.8) | 8226 (22.5) | 23 161 (25.7) |
| Midwest | 5396 (11.9) | 915 (10.7) | 4240 (11.6) | 10 551 (11.7) |
| South | 23 651 (52.4) | 4734 (55.2) | 21 150 (57.9) | 49 535 (54.9) |
| West | 3407 (7.5) | 717 (8.4) | 2916 (8.0) | 7040 (7.8) |
| Index ASCVD condition, n (%)a | ||||
| Acute coronary syndrome | 2092 (4.6) | 455 (5.3) | 2020 (5.5) | 4567 (5.1) |
| History of MI | 881 (2.0) | 228 (2.7) | 1054 (2.9) | 2163 (2.4) |
| Stable or unstable angina | 5720 (12.7) | 1075 (12.5) | 4727 (12.9) | 11 522 (12.8) |
| History of coronary revascularization | 5445 (12.1) | 1089 (12.7) | 4444 (12.2) | 10 978 (12.2) |
| Peripheral artery revascularization | 26 513 (58.7) | 4785 (55.8) | 19 960 (54.6) | 51 258 (56.8) |
| Peripheral artery disease | 176 (0.4) | 35 (0.4) | 143 (0.4) | 354 (0.4) |
| TIA or stroke | 6598 (14.6) | 1358 (15.8) | 6083 (16.7) | 14 039 (15.6) |
ASCVD indicates atherosclerotic cardiovascular disease; MI, myocardial infarction; TIA, transient ischemic attack.
May add up to >100%, as patients could have had multiple conditions on their index date.
Statin Treatment Patterns
Overall statin use declined from 59% at 12 months before the guidelines release to 47% at 13 months after the guidelines were released. In total, 55% of patients were using statins in the 12 months before the guidelines release and 49% were using statins after the guidelines were implemented (P<0.001; Figure 3). Although statistically different, statin use during the first month after an ASCVD visit remained relatively constant before (32%) and after (31%) the new guidelines were implemented (P<0.001). However, in patients receiving statins, the use of high‐intensity statins increased from 27% before to 31% after the guidelines were implemented (P<0.001).
Figure 3.
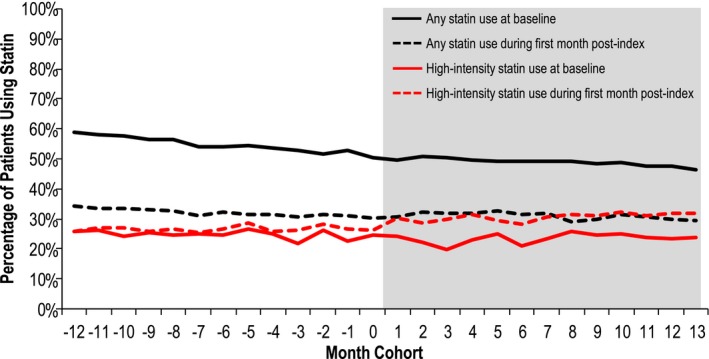
Statin treatment patterns. The percentage (%) of patients using any statin (black lines) or high‐intensity statins (red lines) at baseline (solid lines) and during the first month postindex (dashed lines) are shown. The white area includes month cohorts that occurred before the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline changes, and the gray area includes month cohorts following the changes. Month 0 indicates the release of the ACC/AHA guidelines (November 2013).
LDL‐C Levels
The mean (SD) number of recorded LDL‐C results per patient (representing LDL‐C orders) was 1.2 (0.5) before and 1.2 (0.4) after the guidelines changed. Mean (SD) LDL‐C levels were consistent in the year before and after release of the guidelines: 2.4 (0.9) mmol/L or 93.0 (33.2) mg/dL in the −12 to −2 month group; 2.5 (0.9) mmol/L or 95.7 (34.1) mg/dL in the −1 to 1 month group; and 2.4 (0.9) mmol/L or 94.4 (34.1) mg/dL in the 2 to 13 month group. Similarly, the percentage of patients who achieved an LDL‐C level <2.6 mmol/L (100 mg/dL) or <1.8 mmol/L (70 mg/dL) was similar across all month cohorts (Figure 4). Patients who were not using statins during the study had significantly higher LDL‐C levels (mean, 2.7 mmol/L [105 mg/dL]) compared with patients who were incident statin users (mean, 2.2 mmol/L [85 mg/dL]) or continuing statin users (mean, 2.2 mmol/L [86 mg/dL]; P<0.001). Patients who were not using statins during the study were also significantly less likely than those using statins (both incident and continuing users) to achieve LDL‐C levels <2.6 mmol/L (100 mg/dL) or <1.8 mmol/L (70 mg/dL [both P<0.001]; Table 3). Patients receiving high‐intensity statins had significantly lower LDL‐C levels (mean, 2.0 mmol/L [78 mg/dL]) compared with patients on low‐ or moderate‐intensity statins (mean, 2.2 mmol/L [86 mg/dL]; P<0.001) and were significantly more likely to achieve LDL‐C levels <2.6 mmol/L (100 mg/dL) or <1.8 mmol/L (70 mg/dL; P<0.001; Table 4). Table 5 reports factors that were (month cohort, male sex, and Medicare insurance) and were not (age, geographical region) correlated with percentage change in LDL‐C levels during follow‐up.
Figure 4.
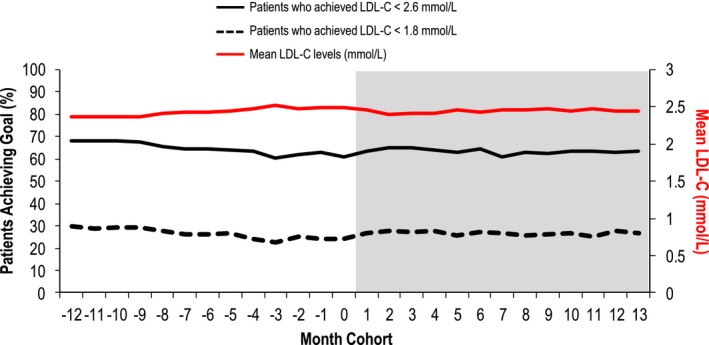
Achievement of LDL‐C goals and mean LDL‐C levels. The percentage (%) of patients who achieved an LDL‐C level <2.6 mmol/L (100 mg/dL; solid black line) or <1.8 mmol/L (70 mg/dL; dashed black line) is shown. Mean LDL‐C levels (red line) across month cohorts are also shown. The white area includes month cohorts that occurred before the 2013 American College of Cardiology (ACC)/American Heart Association (AHA) Guideline changes, and the gray area includes month cohorts following the changes. LDL‐C indicates low‐density lipoprotein cholesterol. Month 0 indicates the release of the ACC/AHA guidelines (November 2013).
Table 3.
LDL‐C Levels and ASCVD Patients Achieving LDL‐C <1.8 mmol/L or <2.6 mmol/L by Statin Use Category (Months 2–7 of Follow‐up)
| Incident Statin Users (n=5518) | Continuing Statin Users (n=47 446) | No Statin Use (n=37 405) | P Value | |
|---|---|---|---|---|
| LDL‐C, mean mmol/L (SD) | 2.2 (0.8) | 2.2 (0.8) | 2.7 (0.9) | <0.001 |
| LDL‐C <1.8 mmol/L, n (%) | 2163 (39.2) | 15 866 (33.4) | 6265 (16.7) | <0.001 |
| LDL‐C <2.6 mmol/L, n (%) | 4124 (74.7) | 35 863 (75.6) | 18 260 (48.8) | <0.001 |
To convert mmol/L to mg/dL, multiply by 38.61. ASCVD indicates atherosclerotic cardiovascular disease; LDL‐C, low‐density lipoprotein cholesterol.
Table 4.
LDL‐C Levels and Patients Achieving LDL‐C <1.8 mmol/L or <2.6 mmol/L by Statin Intensity
| High‐Intensity Statin (n=8087) | Low/Moderate‐Intensity Statin (n=20 532) | P Value | |
|---|---|---|---|
| LDL‐C, mean mg/dL (SD) | 2.0 (0.8) | 2.2 (0.7) | <0.001 |
| LDL‐C <1.8 mmol/L, n (%) | 3706 (45.8) | 6770 (33.0) | <0.001 |
| LDL‐C <2.6 mmol/L, n (%) | 6759 (83.6) | 15 499 (75.5) | <0.001 |
To convert mmol/L to mg/dL, multiply by 38.61. ASCVD indicates atherosclerotic cardiovascular disease; LDL‐C, low‐density lipoprotein cholesterol.
Table 5.
Ordinary Least Squares Regression of Percentage Change in LDL‐C Levels During Follow‐up
| Independent Variables | Coefficient (95% CI) | P Value |
|---|---|---|
| Month cohort (vs −1 to 1) | ||
| −12 to −2 | 1.3 (0.4, 2.3) | 0.005 |
| 2 to 13 | −1.7 (−2.6, −0.7) | <0.001 |
| Male sex (vs female) | −0.7 (−1.3, −0.2) | 0.011 |
| Age (vs 21–44 y) | ||
| 45 to 64 | −0.9 (−2.8, 1.0) | 0.374 |
| 65 to 75 | −0.7 (−2.7, 1.3) | 0.513 |
| ≥76 | 0.5 (−1.6, 2.5) | 0.643 |
| Geographical region (vs Northeast) | ||
| Midwest | −0.2 (−1.2, 0.9) | 0.721 |
| South | 0.5 (−0.2, 1.1) | 0.134 |
| West | −0.6 (−1.8, 0.6) | 0.292 |
| Insurance type (vs commercial) | ||
| Medicare advantage | 1.9 (1.0, 2.8) | <0.001 |
Observations read=90 287, Observations used=43 320. Model F‐test: F=20.317, DF=10, P<0.001. R 2=0.005, adjusted R 2=0.004. LDL‐C indicates low‐density lipoprotein cholesterol.
Discussion
The 2013 ACC/AHA guidelines on managing levels of blood cholesterol were released in 2013;6 since then, with the exception of a few recent studies,7, 8, 9 few studies have examined physician uptake of the 2013 guidelines or how statin use and LDL‐C levels have potentially changed in response. At the time the guidelines were published, projections indicated that they would greatly expand the pool of patients who qualify for statin therapy, thereby increasing the use of statins.8, 10 We examined over 90 000 patients before and after the guidelines release and found that overall statin use decreased following the release of the guidelines. Reasons for this decrease are unclear, but a recent study suggests that there is a gap in physician understanding of the guidelines, with 52% of providers not having read the guidelines or a summary of the guidelines and 39% not using LDL‐C as a target of therapy.9 This gap exists for both specialists and nonspecialists.9
Reports following the publication of the 2013 guidelines also predicted that the new guidelines would lead to a greater number of patients receiving prescriptions for high‐intensity statins. A recent historical cohort analysis of ≈1500 commercially insured patients by Bellows et al reported a 7% postguidelines increase in high‐intensity statin use among patients with ASCVD.7 Similarly, we found a 4 percentage point increase in high‐intensity statin use 1 year after the guidelines among the proportion of ASCVD patients who received statins postguidelines. These relatively modest results are surprising given the widespread publicity of the guidelines, both in the medical and lay press. The reason for this finding is unclear, but a possibility is that physicians are not familiar with the 2013 guidelines classification of statin intensity. Bellows et al found that 71% of practicing providers surveyed do not understand the definitions of low‐, moderate‐, or high‐intensity statin therapy, as given in the 2013 guidelines.7 This gap in provider understanding may be affecting the high‐intensity statin levels that we observed in our study.
Our analysis furthermore demonstrates that LDL‐C levels in patients were similar in the year before and year following the release of the new guidelines. Mean LDL‐C levels were ≈2.4 mmol/L (94 mg/dL) both before and after publication of the 2013 guidelines. Similarly, the percentage of patients who achieved an LDL‐C level <2.6 mmol/L (100 mg/dL) or <1.8 mmol/L (70 mg/dL) was similar across all month cohorts. These data suggest that the revised guidelines had a modest impact on practice and real‐world LDL‐C levels, even in this population of patients with a higher severity of disease who are recommended to be prescribed the most intensive therapy. However, we did observe lower LDL‐C levels in patients who used high‐intensity statins, confirming that following the guidelines results in lower LDL‐C.
Implications for the 2013 ACC/AHA Guidelines
Although the guidelines do not recommend monitoring LDL‐C to assess achievement of a particular LDL‐C goal, they do recommend monitoring LDL‐C to determine adherence and anticipated therapeutic response. There is some evidence that a majority of practitioners are not conducting follow‐up testing of LDL‐C levels.9 We found similar rates between the pre‐ and postguidelines frequency of LDL tests (1.2 LDL‐C orders per patient in the 2–7 months of follow‐up both before and after the guidelines). It is important to note, however, that reasons for ordering LDL‐C tests cannot be determined from claims, and therefore we do not know whether physicians were continuing to order tests to treat to a LDL‐C goal or to follow guideline recommendations. This raises the larger question of how practitioners are determining treatment success and how they are determining criteria for increasing lipid‐lowering therapy.11 It is possible that a lack of treatment goals in the guidelines is leading to confusion and a decreased focus on reducing levels of atherogenic lipids. This study and others surveying physician prescribing practices before and after the guidelines suggests a knowledge gap that may be limiting statin prescribing changes.9 In addition, new lipid‐lowering therapies, such as PCSK9 inhibitors, are currently in use. Cardiovascular outcomes trials of PCSK9 inhibitors are expected to complete in the coming year.12, 13 If these outcome studies are positive, it is possible that the guidelines will be updated. Our data suggest that more intensive and varied educational efforts will likely be needed in order to help clinicians adopt and more closely follow future lipid treatment guidelines. Furthermore, a simplification of the guidelines or even a return to treatment goals may provide clarity and aid the clinician in determining appropriate therapy for patients.
An additional challenge with the 2013 guidelines is in calculating the proposed goal of a 50% reduction in lipid levels. For an individual patient with hyperlipidemia who has been undergoing treatment for a few years, laboratory values may have been recorded by multiple physicians or health systems. On a population level, baseline LDL‐C levels measured before initiation of statin therapy are required, and it may be difficult to determine when statin therapy is initiated in patients who change health plans or physicians. This may have the unintended effect of lowering the emphasis on LDL‐C reduction because of the difficulties of ascertaining which patients are not at ideal LDL‐C levels. Conversely, it is easier to determine at any given point in time which patients are at goal using cross‐sectional data alone, which may facilitate implementing programs for patients not achieving therapeutic goals.
Strengths and Limitations
Our study included LDL‐C levels as a measure, allowing us to explore how these levels differed before and after the release of the 2013 ACC/AHA guidelines in a large (>90 000 patients) managed care population. The health plans included in the analysis were discounted fee‐for‐service plans rather than capitated or gatekeeper models. They did, however, include a wide geographical distribution across the United States and thus provided the ability to generalize results to managed care populations on a national level. Limitations of our study include the lack of information on reasons for laboratory tests and treatment choices. Because of this, we were unable to assess whether patients were statin intolerant or whether they had adverse events or contraindications that may have affected treatment choice. In addition, we did not assess long‐term follow‐up of patients. Only the index event was captured for each patient, and patients could have had other cardiovascular events or evidence of ASCVD before or after the index date. Last, the analysis included only the subset of patients with laboratory results available from outpatient facilities affiliated with the health plan; however, these results were not expected to differ from values collected at nonaffiliated vendors. As a result, the exclusion of patients without an LDL‐C result was not expected to bias the study sample.
Conclusions
This study showed that following the release of the 2013 ACC/AHA guidelines, high‐intensity statin treatment modestly increased, but the number of statin prescriptions overall decreased and mean LDL‐C levels remained largely unchanged. The 2013 guidelines focused on utilizing appropriate statin intensity and percentage reduction of LDL‐C, rather than treatment goals, and were predicted to increase the overall use of statins. Our data suggest that the guidelines did not significantly alter clinician behavior with regard to the treatment of hyperlipidemia. Future updates to clinical treatment guidelines may require more intensive educational efforts centered on practicing clinicians and a simplification of, or change in, recommendations set forth in the guidelines in order to improve physician understanding and use.
Sources of Funding
Amgen Inc. funded this study.
Disclosures
Okerson, Patel, DiMario, and Harrison are employees of Amgen Inc. and own Amgen Inc. stock/stock options. Burton and Seare are employees of Optum Corp.
Acknowledgments
Julia R. Gage, PhD (on behalf of Amgen Inc.), and Annalise M. Nawrocki, PhD (Amgen Inc.), provided medical writing support.
(J Am Heart Assoc. 2017;6:e004909. DOI: 10.1161/JAHA.116.004909.)
References
- 1. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr, Tomaselli GF; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–S45. [DOI] [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB, American Heart Association Statistics Committee, Stroke Statistics Subcommittee . Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. [DOI] [PubMed] [Google Scholar]
- 3. Boekholdt SM, Hovingh GK, Mora S, Arsenault BJ, Amarenco P, Pedersen TR, LaRosa JC, Waters DD, DeMicco DA, Simes RJ, Keech AC, Colquhoun D, Hitman GA, Betteridge DJ, Clearfield MB, Downs JR, Colhoun HM, Gotto AM Jr, Ridker PM, Grundy SM, Kastelein JJ. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta‐analysis of statin trials. J Am Coll Cardiol. 2014;64:485–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC Jr, Stone NJ; National Heart, Lung, and Blood Institute, American College of Cardiology Foundation, American Heart Association . Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227–239. [DOI] [PubMed] [Google Scholar]
- 5. Lambert M. ACC/AHA release updated guideline on the treatment of blood cholesterol to reduce ASCVD risk. Am Fam Physician. 2014;90:260–265. [Google Scholar]
- 6. Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd‐Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889–2934. [DOI] [PubMed] [Google Scholar]
- 7. Bellows BK, Olsen CJ, Voelker J, Wander C. Antihyperlipidemic medication treatment patterns and statin adherence among patients with ASCVD in a managed care plan after release of the 2013 ACC/AHA guideline on the treatment of blood cholesterol. J Manag Care Spec Pharm. 2016;22:892–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tran JN, Kao TC, Caglar T, Stockl KM, Spertus JA, Lew HC, Solow BK, Chan PS. Impact of the 2013 cholesterol guideline on patterns of lipid‐lowering treatment in patients with atherosclerotic cardiovascular disease or diabetes after 1 year. J Manag Care Spec Pharm. 2016;22:901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Virani SS, Pokharel Y, Steinberg L, Chan W, Akeroyd JM, Gowani SA, Kalra A, Polsani V, Miedema MD, Jones PH, Nambi V, Petersen LA, Ballantyne CM. Provider understanding of the 2013 ACC/AHA cholesterol guideline. J Clin Lipidol. 2016;10:497–504.e494. [DOI] [PubMed] [Google Scholar]
- 10. Pencina MJ, Navar‐Boggan AM, D'Agostino RB Sr, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population‐based sample. N Engl J Med. 2014;370:1422–1431. [DOI] [PubMed] [Google Scholar]
- 11. Athyros VG, Sfikas G, Boutari C, Imprialos K, Tziomalos K, Karagiannis A. 2013 American College of Cardiology/American Heart Association Lipid Guidelines after the 2016 American College of Cardiology Expert Panel Consensus Statement: to err is human; to admit it, divine. Hell J Atheroscler. 2016;7:13–26. [Google Scholar]
- 12. Sabatine MS, Giugliano RP, Keech A, Honarpour N, Wang H, Liu T, Wasserman SM, Scott R, Sever PS, Pedersen TR. Rationale and design of the Further cardiovascular OUtcomes Research with PCSK9 Inhibition in subjects with Elevated Risk trial. Am Heart J. 2016;173:94–101. [DOI] [PubMed] [Google Scholar]
- 13. Schwartz GG, Bessac L, Berdan LG, Bhatt DL, Bittner V, Diaz R, Goodman SG, Hanotin C, Harrington RA, Jukema JW, Mahaffey KW, Moryusef A, Pordy R, Roe MT, Rorick T, Sasiela WJ, Shirodaria C, Szarek M, Tamby JF, Tricoci P, White H, Zeiher A, Steg PG. Effect of alirocumab, a monoclonal antibody to PCSK9, on long‐term cardiovascular outcomes following acute coronary syndromes: rationale and design of the ODYSSEY outcomes trial. Am Heart J. 2014;168:682–689. [DOI] [PubMed] [Google Scholar]


