Abstract
Background
Several studies have suggested sex‐related differences in diagnostic and invasive therapeutic coronary procedures.
Methods and Results
Data from consecutive patients who were enrolled in the Coronary Angiography and PCI Registry of the German Society of Cardiology were analyzed. We aimed to compare sex‐related differences in in‐hospital outcomes of patients undergoing percutaneous coronary intervention (PCI) for stable coronary artery disease, non‐ST elevation acute coronary syndromes, ST elevation myocardial infarction, and cardiogenic shock. From 2007 until the end of 2009 data from 185 312 PCIs were prospectively registered: 27.9% of the PCIs were performed in women. Primary PCI success rate was identical between the sexes (94%). There were no sex‐related differences in hospital mortality among patients undergoing PCI for stable coronary artery disease, non‐ST elevation acute coronary syndromes, or cardiogenic shock except among ST elevation myocardial infarction patients. Compared to men, women undergoing primary PCI for ST elevation myocardial infarction have a higher risk of in‐hospital death, age‐adjusted odds ratio (1.19, 95% CI 1.06‐1.33), and risk of ischemic cardiac and cerebrovascular events (death, myocardial infarction, transient ischemic attack/stroke), (age‐adjusted odds ratio 1.19, 95% CI 1.16‐1.29). Furthermore, access‐related complications were twice as high in women, irrespective of the indication.
Conclusions
Despite identical technical success rates of PCI between the 2 sexes, women with PCI for ST elevation myocardial infarction have a 20% higher age‐adjusted risk of death and of ischemic cardiac and cerebrovascular events. Further research is needed to determine the reasons for these differences.
Keywords: acute coronary syndrome, angioplasty and stenting, coronary artery disease, outcome, women
Subject Categories: Cardiovascular Disease, Women, Percutaneous Coronary Intervention, Stent, Treatment
Introduction
Recently, the German Heart Report 2013 described a decrease in total mortality rate of acute myocardial infarction in men since 1980 and in women since 1995. In men, there was a decrease of about 50%, and in women of about 35%.1 This is in line with data from the World Health Organization global mortality database, which describe a decrease in age‐standardized coronary heart disease mortality in the last 25 years of 49% in men and 39% in women.2 There has been speculation about possible explanations for these sex differences, such as delay in seeking medical care for acute coronary syndromes with longer time from symptom onset to balloon in women, sex bias in use of evidence‐based and guideline‐recommended lifesaving medical therapy, differences in use of drug‐eluting stents, thrombolysis, emergency percutaneous coronary intervention (PCI), or timely coronary artery bypass graft (CABG) procedures.1, 2 In addition, it has been reported that only an estimated 33% of annual PCIs were performed in women despite the established benefits of PCI in reducing fatal and nonfatal ischemic complications in patients with acute coronary syndromes.3 It has been found that women were less likely to be revascularized than men, either in the management of stable angina4 or in acute coronary syndromes.5, 6 Recently, we have been able to show that in patients with significant coronary artery disease there was no difference in recommendation for PCI between women and men.7 Nearly all of the studies found a higher crude hospital mortality in women with PCI for acute coronary syndromes. In some of the studies the difference in hospital mortality between the sexes disappeared after adjustment for age and comorbidity,5, 6, 8, 9, 10, 11 whereas in others it persisted.12, 13, 14, 15, 16, 17 Interestingly, despite the pronounced decrease in mortality for men, the long‐term prognosis after an acute myocardial infarction was still less favorable in men than in women in Germany and in all other European countries.1, 2
The purpose of this study was to examine sex differences in procedural features, safety, and efficacy of PCI in a very large coronary angiography and PCI registry in Germany.
Methods
The data presented in this analysis were taken from 218 hospitals that transferred data to the Bundesgeschäftsstelle Qualitätssicherung gGmbH (BQS) or enrolled patients in the German Arbeitsgemeinschaft Leitende Kardiologische Krankenhausärzte (ALKK) registry. The comprehensive collection and analysis of these data was endorsed by the German Cardiac Society. Details of the BQS quality program and the ALKK registry have been described before.7, 18, 19, 20 Since 2002 all hospitals that perform invasive coronary procedures in Germany were legally obligated to record details about these procedures to monitor quality control. Therefore, consent of patients for the processing of their anonymized data was generally obtained. The data contain all consecutive PCIs of the participating hospitals on an intention‐to‐treat basis. Baseline characteristics, course of PCI, and hospital complications were registered prospectively and analyzed centrally at the Karl Ludwig Neuhaus Datenzentrum, Stiftung Institut für Herzinfarktforschung, Ludwigshafen, Germany. All information about success of PCI is based on the evaluation of the treating physician. PCI was rated successful if there was a residual stenosis of <50% after balloon angioplasty without stenting and <20% after PCI with stent application. The present analysis comprises all patients who were treated with PCI for stable coronary artery disease, non‐ST elevation acute coronary syndromes (NSTE‐ACS), and ST elevation myocardial infarction (STEMI). The first PCI performed in each patient during hospital stay was considered for the analysis.
Data Collection
Data on patient characteristics on admission comprised age, sex, concomitant diseases, cardiovascular risk factors, prior PCI or CABG, prior myocardial infarction, or stroke. Following completion of the procedure, lesion characteristics, details of the intervention, and intraprocedural and in‐hospital adverse cardiovascular outcomes were recorded on a standardized form by the treating physician and transmitted to the central data registry center in Ludwigshafen via the Internet by the treating physician.
Definitions
STEMI was defined as ST‐segment elevation of ≥2 mm in ≥2 precordial leads or >1 mm in ≥2 extremity leads; non‐ST elevation myocardial infarction (NSTEMI) was defined as any significant increase in troponin level without ST elevation in the defining ECG. Adverse outcomes (major adverse cardiac or cerebrovascular events), defined as in‐hospital death, myocardial infarction, stroke, or reinfarction, were evaluated. Myocardial infarction was defined as a 2‐fold rise in creatine kinase level above normal. A cerebrovascular event was defined as a stroke or a transitory or reversible cerebral ischemic attack that was confirmed clinically as a permanent neurological deficit or by CT scan. In addition, pulmonary embolism, resuscitation, complications at the puncture site, acute renal failure, requirement for dialysis, septicemia, and urgent CABG procedure were reported as in‐hospital events.
Primary success of PCI was defined as the achievement of <20% final diameter stenosis after stent implantation and <50% after coronary angioplasty without stent implantation in visual assessment associated with Thrombolysis In Myocardial Infarction (TIMI) flow grade ≥2.
Statistical Analysis
Statistical analysis was performed using the SAS software package version 9.3 (SAS Inc, Cary, NC). Binary data are expressed as percentages (numerator/denominator numbers); for continuous variables such as age and hospital stay, median values with 25th and 75th percentiles (interquartile range) are shown. The descriptive statistics are based on the available cases, which are used as denominator of rates. The Pearson χ2 test was used to examine differences between patient groups in categorical variables, and the Mann‐Whitney‐Wilcoxon test for metrically scaled variables. Statistical significance was defined as 2‐sided P≤0.05. Odds ratios (OR) with 95% CIs were calculated for the comparison of binary variables. OR with 95% CIs adjusted for age as a linear term were calculated by logistic regression for sex comparisons.
Results
From 2007 until the end of 2009, data of 185 312 PCIs from a total of 218 German hospitals were prospectively registered. Sex differences in therapeutic recommendation after diagnostic coronary angiography were described before.7
Sex Differences in Baseline and Procedural Characteristics, All Procedures
Of patients undergoing PCI, 27.9% were female. Women were 5 years older than men (72 years vs 67 years, P<0.001). Compared to men, they less often had a history of former coronary angiography (44.6% vs 52.9%, OR 0.72, 95% CI 0.70‐0.73), of PCI (33.2% vs 40.7%, OR 0.72, 95% CI 0.71‐0.74), and of CABG (8.4% vs 13.7%, OR 0.58, 95% CI 0.56‐0.60). Women more often had diabetes mellitus (29.5% vs 23.7%, OR 1.34, 95% CI 1.31‐1.38), and they more often presented with congestive heart failure (8.5% vs 7.8%, OR 1.09, 95% CI 1.05‐1.13). Procedural success was slightly higher in women than in men (94.5% vs 94%, OR 1.09, 95% CI 1.04‐1.14), but procedural complications were higher in women, including death in the catheterization laboratory (0.3% vs 0.2%, OR 1.47, 95% CI 1.21‐1.80) and resuscitation (0.8% vs 0.5%, OR 1.43, 95% CI 1.27‐1.62). The absolute number of TIAs/strokes was 23/51 771 in women and 33/133 530 in men (OR 1.80, 95% CI 1.06‐3.06).
Sex Differences in Baseline and Procedural Characteristics According to the Indication for First PCI
Results are shown in Tables 1 and S1. In elective PCI the primary success rate was higher in women compared to men, the stent rate was higher, as was the number of PCI in ostial stenoses. In contrast, men more often had PCI in more than 1 vessel, more often with complete vessel occlusion, more often in bypass grafts, more often in an unprotected left main stenosis, and more often in the last coronary vessel. There was no difference in acute mortality in the catheterization laboratory between the 2 sexes (see Tables 1 and S1).
Table 1.
Baseline and Procedural Characteristics
| Women | Men | Age‐Adjusted OR (95% CI) | |
|---|---|---|---|
| PCI in elective patients | |||
| n=24 262 (26.9%) | n=65 972 (73.1%) | ||
| Age, y | 72 (65; 78) | 68 (60; 74) | |
| History of PCI | 42.9% (10 316/24 066) | 51.6% (33 711/65 308) | 0.72 (0.69‐0.74) |
| History of CABG surgery | 10.1% (2443/24 178) | 16.5% (10 811/65 684) | 0.50 (0.47‐0.52) |
| LV ejection fraction ≤40% | 8.9% (1946/21 805) | 13.4% (7921/59 019) | 0.59 (0.56‐0.62) |
| Diabetes mellitus | 29.8% (7124/23 879) | 25.0% (16 222/64 800) | 1.20 (1.16‐1.24) |
| Renal insufficiency | 16.5% (3931/23 862) | 16.7% (10 863/64 874) | 0.79 (0.76‐0.82) |
| Diagnostic XA and PCI in 1 session | 84.8% (20 565/24 262) | 83.9% (55 371/65 972) | 1.08 (1.04‐1.13) |
| PCI successfula | 95.2% (23 093/24 262) | 94.1% (62 051/65 972) | 1.25 (1.16‐1.33) |
| Stent implanted | 90.0% (21 829/24 262) | 88.9% (58 651/65 972) | 1.11 (1.06‐1.17) |
| PCI in more than 1 vessel | 8.9% (2169/24 261) | 11.0% (7224/65 972) | 0.78 (0.74‐0.82) |
| PCI in complete vessel occlusion | 7.5% (1808/24 181) | 9.2% (6028/65 733) | 0.87 (0.82‐0.92) |
| PCI in CABG | 2.1% (512/24 181) | 4.6% (3024/65 733) | 0.38 (0.35‐0.42) |
| PCI in unprotected left main | 1.2% (288/24 181) | 1.4% (935/65 733) | 0.76 (0.67‐0.87) |
| PCI in last coronary vessel | 0.3% (67/24 181) | 0.4% (233/65 733) | 0.72 (0.55‐0.95) |
| PCI in NSTE‐ACS patients without cardiogenic shock | |||
| n=14 336 (29.7%) | n=33 879 (70.3%) | ||
| Age, y | 74 (66; 80) | 68 (58; 75) | |
| History of PCI | 30.0% (4227/14 101) | 35.6% (11 872/33 326) | 0.72 (0.69‐0.75) |
| History of CABG surgery | 8.9% (1263/14 234) | 15.0% (5043/33 623) | 0.44 (0.41‐0.47) |
| LV ejection fraction ≤40% | 13.6% (1561/11 437) | 16.8% (4525/26 886) | 0.66 (0.62‐0.70) |
| Diabetes mellitus | 31.6% (4367/13 808) | 25.1% (8205/32 649) | 1.22 (1.17‐1.28) |
| Renal insufficiency | 21.5% (2989/13 888) | 20.7% (6807/32 806) | 0.73 (0.70‐0.77) |
| On hemodialysis | 1.9% (257/13 888) | 2.0% (643/32 806) | 0.83 (0.72‐0.97) |
| Diagnostic XA and PCI in 1 session | 95.3% (13 662/14 336) | 95.1% (32 230/33 879) | 1.14 (1.04‐1.25) |
| PCI successfula | 94.6% (13 556/14 336) | 94.1% (31 893/33 878) | 1.17 (1.07‐1.28) |
| Stent implanted | 90.2% (12 935/14 336) | 89.8% (30 436/33 879) | 1.10 (1.02‐1.17) |
| PCI in more than 1 vessel | 11.9% (1703/14 336) | 11.8% (3987/33 879) | 0.93 (0.88‐0.99) |
| PCI in complete vessel occlusion | 17.4% (2486/14 288) | 20.3% (6836/33 753) | 0.92 (0.88‐0.97) |
| PCI in CABG | 3.0% (429/14 288) | 6.8% (2301/33 753) | 0.33 (0.30‐0.37) |
| PCI in ostial stenosis | 7.0% (1007/14 288) | 5.7% (1910/33 753) | 1.13 (1.04‐1.22) |
| Resuscitation in cath lab | 0.6% (88/14 335) | 0.3% (101/33 877) | 1.78 (1.32‐2.39) |
| PCI in STEMI‐ACS patients without cardiogenic shock | |||
| n=9156 (27.8%) | n=23 830 (72.2%) | ||
| Age, y | 72 (61; 79) | 62 (53; 71) | |
| History of PCI | 12.4% (1103/8875) | 17.6% (4057/23 112) | 0.59 (0.55‐0.64) |
| History of CABG surgery | 2.8% (251/9028) | 4.5% (1065/23 562) | 0.42 (0.37‐0.49) |
| LV ejection fraction ≤40% | 19.7% (1161/5894) | 18.6% (2849/15 304) | 0.92 (0.85‐0.99) |
| Diabetes mellitus | 25.5% (2115/8282) | 17.7% (3811/21 547) | 1.31 (1.23‐1.40) |
| Renal insufficiency | 16.4% (1305/7934) | 12.3% (2550/20 690) | 0.87 (0.81‐0.94) |
| On hemodialysis | 98.1% (8978/9156) | 98.1% (23 372/23 830) | 1.08 (0.90‐1.30) |
| Diagnostic XA and PCI in 1 session | 93.5% (8557/9156) | 94.7% (22 568/23 830) | 0.96 (0.87‐1.07) |
| PCI successfula | 91.1% (8341/9156) | 92.4% (22 028/23 830) | 0.96 (0.87‐1.05) |
| Stent implanted | 1.1% (103/9146) | 2.2% (517/23 818) | 0.33 (0.27‐0.42) |
| PCI in more than 1 vessel | 0.1% (5/9156) | <0.1% (3/23 830) | 4.94 (1.12‐21.72) |
| PCI in complete vessel occlusion | 1.4% (127/9156) | 1.0% (231/23 830) | 1.32 (1.06‐1.66) |
| PCI in CABG | 12.4% (1103/8875) | 17.6% (4057/23 112) | 0.59 (0.55‐0.64) |
| PCI in ostial stenosis | 2.8% (251/9028) | 4.5% (1065/23 562) | 0.42 (0.37‐0.49) |
| Resuscitation in cath lab | 19.7% (1161/5894) | 18.6% (2849/15 304) | 0.92 (0.85‐0.99) |
| PCI in cardiogenic shock | |||
| n=963 (30.3%) | n=2219 (69.7%) | ||
| Age, y | 74 (66; 81) | 67 (57; 75) | |
| History of PCI | 17.8% (154/864) | 25.6% (498/1943) | 0.59 (0.48‐0.72) |
| History of CABG surgery | 7.0% (64/919) | 10.2% (218/2145) | 0.55 (0.41‐0.75) |
| LV ejection fraction ≤40% | 62.4% (406/651) | 66.9% (984/1471) | 0.77 (0.63‐0.94) |
| Diabetes mellitus | 35.4% (274/775) | 31.4% (544/1735) | 1.00 (0.83‐1.20) |
| Renal insufficiency | 37.5% (291/776) | 36.6% (654/1788) | 0.76 (0.63‐0.92) |
| STEMI | 77.6% (747/963) | 73.7% (16 536/2219) | 1.45 (1.21‐1.75) |
| Diagnostic XA and PCI in 1 session | 97.9% (943/963) | 98.0% (2175/2219) | 0.99 (0.57‐1.72) |
| PCI successfula | 86.1% (829/963) | 85.7% (1901/2219) | 1.19 (0.95‐1.49) |
| Stent implanted | 86.1% (829/963) | 85.9% (1907/2219) | 1.13 (0.90‐1.41) |
| PCI in complete vessel occlusion | 65.3% (628/962) | 62.0% (1376/2218) | 1.29 (1.09‐1.51) |
| PCI in CABG | 2.5% (24/962) | 4.7% (105/2218) | 0.41 (0.26‐0.64) |
| PCI in last coronary vessel | 2.8% (27/962) | 4.3% (96/2218) | 0.62 (0.39‐0.96) |
Values are expressed as percentages (number of occurrences/available cases) except for age (median; interquartile range). Only relevant data are shown. The complete tables can be found in Tables S1 through S4. CABG indicates coronary artery bypass graft; LV, left ventricle; NSTE‐ACS, non‐ST elevation acute coronary syndrome; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST elevation myocardial infarction; XA, coronary angiography.
Defined as <20% final diameter stenosis after stent implantation and <50% after coronary angioplasty without stent implantation in visual assessment associated with TIMI flow grade ≥2.
Sex differences in NSTE‐ACS were comparable to that of elective PCI. Primary success rate and stent rate were higher in women. PCI in more than 1 area, PCI in complete vessel occlusion, PCI in CABG, PCI in an unprotected left main, and PCI in last coronary vessel had higher incidence in men than in women, but PCI in ostial stenosis was more frequent in women (see Tables 1 and S2).
In STEMI, sex differences in procedural characteristics were less pronounced. There was no difference in success rate between men and women. Resuscitation in the catheterization laboratory was more often necessary in women, and PCI in bypass grafts was performed more frequently in men than in women (see Tables 1 and S3).
In cardiogenic shock, there was no sex difference in primary success rate between the sexes. PCI in CABG was less often performed in women. Resuscitation in the catheterization laboratory was more often necessary in women than in men (see Tables 1 and S4).
Sex Differences in In‐Hospital Course and Procedure‐Related Complications According to the Indication for First PCI
Results are shown in Table 2, Tables S5 through S8, and Figure 1A and 1B. After adjustment for age, hospital mortality after PCI was higher in women with PCI in STEMI but not in elective PCI, PCI in NSTE‐ACS, or PCI in cardiogenic shock. Hospital major adverse cardiac or cerebrovascular events were higher in women with elective PCI and in PCI for STEMI. Unadjusted access‐related complications were twice as high in women in PCI for all indications.
Table 2.
In‐Hospital Outcomes
| Women | Men | Age‐Adjusted OR (95% CI) | |
|---|---|---|---|
| PCI in elective patients | |||
| n=24 262 (26.9%) | n=65 972 (73.1%) | ||
| Hospital death | 0.3% (82/24 262) | 0.2% (154/65 972) | 1.07 (0.82‐1.41) |
| Hospital MACE | 0.7% (162/24 262) | 0.4% (272/65 972) | 1.37 (1.12‐1.67) |
| Hospital MACCE | 0.8% (184/24 262) | 0.5% (323/65 972) | 1.31 (1.09‐1.57) |
| Nonfatal resuscitation | 0.2% (44/24 262) | 0.1% (90/65 972) | 1.33 (0.92‐1.91) |
| Access‐related complications | 1.8% (447/24 245) | 0.8% (553/65 932) | 2.07 (1.83‐2.36) |
| PCI in NSTE‐ACS patients without cardiogenic shock | |||
| n=14 336 (29.7%) | n=33 879 (70.3%) | ||
| Hospital death | 2.4% (350/14 336) | 1.8% (597/33 879) | 1.02 (0.89‐1.16) |
| Hospital MACE | 2.7% (388/14 336) | 2.0% (670/33 879) | 1.04 (0.91‐1.18) |
| Hospital MACCE | 2.9% (415/14 336) | 2.1% (704/33 879) | 1.06 (0.94‐1.21) |
| Nonfatal resuscitation | 0.3% (47/14 336) | 0.2% (67/33 879) | 1.61 (1.10‐2.37) |
| Access‐related complications | 2.3% (324/14 299) | 1.0% (352/33 844) | 1.99 (1.70‐2.33) |
| PCI in STEMI‐ACS patients without cardiogenic shock | |||
| n=9156 (27.8%) | n=23 830 (72.2%) | ||
| Hospital death | 6.3% (581/9156) | 3.6% (854/23 830) | 1.19 (1.06‐1.33) |
| Hospital MACE | 6.6% (608/9156) | 3.8% (906/23 830) | 1.19 (1.07‐1.34) |
| Hospital MACCE | 6.8% (621/9156) | 3.9% (924/23 830) | 1.20 (1.08‐1.34) |
| Nonfatal resuscitation | 0.7% (65/9156) | 0.6% (154/23 830) | 1.18 (0.87‐1.59) |
| Access‐related complications | 2.2% (201/9142) | 0.8% (201/23 808) | 2.32 (1.89‐2.85) |
| PCI in cardiogenic shock | |||
| n=963 (30.3%) | n=2219 (69.7%) | ||
| Hospital death | 46.5% (448/963) | 40.4% (896/2219) | 1.05 (0.89‐1.23) |
| Hospital MACE | 46.6% (449/963) | 40.6% (902/2219) | 1.04 (0.89‐1.22) |
| Hospital MACCE | 46.6% (449/963) | 40.7% (903/2219) | 1.04 (0.89‐1.22) |
| Nonfatal resuscitation | 2.7% (26/963) | 3.2% (70/2219) | 0.93 (0.59‐1.49) |
| Access‐related complications | 1.1% (11/961) | 0.4% (9/2206) | 2.66 (1.07‐6.63) |
Values are expressed as percentages (number of occurrences/available cases). Only relevant data are shown. The complete tables can be found in Tables S5 through S8. MACCE, major adverse cardiac or cerebrovascular event (death, nonfatal myocardial infarction, hospital transient ischemic attack, and hospital stroke); MACE, major adverse cardiac event (death, nonfatal myocardial infarction); NSTE‐ACS, non‐ST elevation acute coronary syndrome; OR, odds ratio; PCI, percutaneous coronary intervention; STEMI, ST elevation myocardial infarction.
Figure 1.
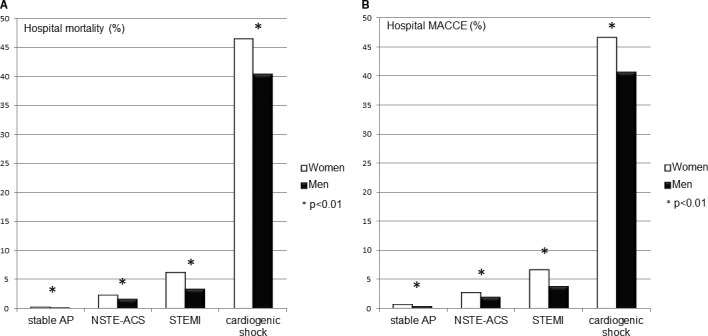
Hospital mortality (A) and hospital MACCE (B) for women and men after elective percutaneous coronary intervention for stable angina pectoris (AP), non‐ST elevation acute coronary syndrome (NSTE‐ACS), ST elevation myocardial infarction (STEMI), and cardiogenic shock in the univariate analysis (MACCE [major adverse cardiac or cerebrovascular event]=death, nonfatal myocardial infarction, hospital transient ischemic attack, and hospital stroke).
Sex Differences in Hospital Mortality in Different Age Groups
Hospital mortality in women <50 years of age with elective PCI or with PCI for STEMI was significantly higher compared to men in the same age group. Differences in the other age groups were not significant (Figure 2A through 2D).
Figure 2.
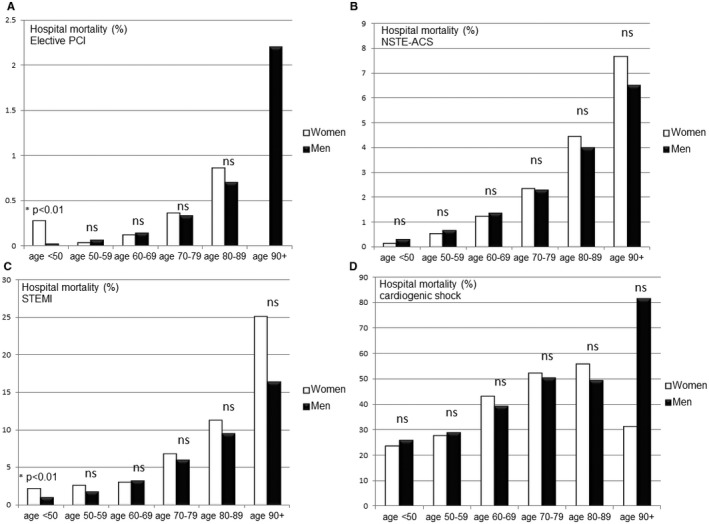
Sex differences in hospital mortality after elective percutaneous coronary intervention (PCI) (A), non‐ST elevation acute coronary syndrome (NSTE‐ACS) (B), ST elevation myocardial infarction (STEMI) (C), and cardiogenic shock (D) in different age groups in a univariate analysis.
Sex Differences in Predictors for Hospital Mortality in STEMI, NSTE‐ACS, and Elective PCI, Multivariate Analysis
In a multivariate analysis for predictors of hospital mortality, we found different predictors that were associated with increased hospital mortality in stable CAD, NSTE‐ACS, STEMI, and cardiogenic shock (see Figure 3).
Figure 3.
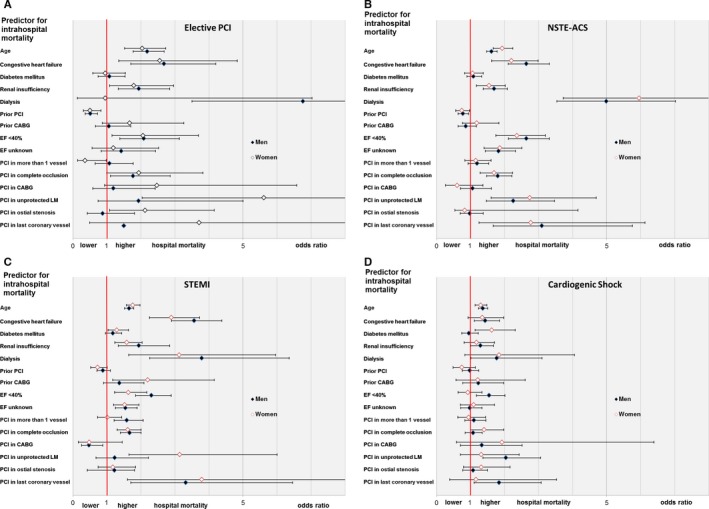
Sex differences in predictors for intrahospital mortality, elective percutaneous coronary intervention (A), non‐ST elevation acute coronary syndrome (NSTE‐ACS) (B), ST elevation myocardial infarction (STEMI) (C), and cardiogenic shock (D). The figure shows odds ratios with 95% confidence intervals. CABG indicates coronary artery bypass graft; EF, ejection fraction; LM, left main coronary artery; PCI, percutaneous coronary intervention.
Discussion
The present analysis gives a representative overview of sex‐associated differences in PCI in Germany from 2007 until 2009. We found that 27.8% of all PCIs were performed in women despite the fact that mortality rates due to coronary heart disease in Germany are almost the same in women and men.1, 2 This rate of PCI is comparable to that in the United States.3 It is not yet completely understood why this difference in use of invasive coronary procedures between men and women exists in spite of the established benefits of PCI in reducing fatal and nonfatal ischemic complications.21
Women with PCI were older than men, and they had more comorbidity. The largest difference of about 10 years was found in STEMI patients, which has been described before.5 We did not find any evidence that primary success rate of PCI was lower in women than in men. In elective PCI and NSTE‐ACS, it was even higher in women than in men, as was the percentage of implanted stents. This finding is in line with former reports in which it was found that the technical success of PCI is similar in women and in men.11
Procedural and postinterventional hospital complications were significantly higher in women compared to men, even after adjustment for age. This has been described before,5, 6, 11, 22, 23 but the reasons for this finding are speculative (smaller vessel size in women, higher comorbidity, differences in endothelial function, variability in correct dosage of adjunctive medical therapy). Although the overall superiority of primary PCI in acute myocardial infarction over fibrinolytic therapy has been clearly demonstrated for women,3, 10 in FRISC II and RITA‐3 an early invasive strategy in NSTE‐ACS did not reduce the risk of future events among women with unstable angina or NSTEMI.24, 25 In other studies women with PCI for acute coronary syndromes showed a lower or at least identical long‐term mortality compared to men.5, 6, 11, 23 Hospital mortality after PCI for STEMI in our population was higher in women compared to men—even after adjustment for age and other covariables. Yet, it has considerably decreased in the last decade in men and women, both in STEMI and NSTE‐ACS.2, 3, 5, 6, 21, 26, 27, 28, 29, 30 In line with former studies we found that younger women with STEMI have higher hospital mortality.2, 5, 31 In comparison to historical data from the MITRA registry (data from 1994 to 1997, hospital mortality in women 20.9%, in men 12.3%), hospital mortality after STEMI has dramatically decreased in both sexes, but there is still a sex difference with a 20% higher mortality in women after adjustment for age. Not unexpectedly, hospital mortality was lowest in elective PCI and highest in cardiogenic shock without differences between the sexes after age‐adjustment.
Interestingly, sex differences in vascular complications after PCI were comparable to that after lone diagnostic coronary angiography, and they were lower compared to former reports, which may reflect the decreasing use of aggressive anticoagulation regimes, the use of weight‐adjusted heparin dosing, and the introduction of smaller sheath sizes and early sheath removal.3
As for subgroup analysis, we did not find any relevant sex differences in specific risk groups. Regarding procedure related differences, we found that PCI in more than 1 coronary vessel (non‐culprit PCI) in STEMI was associated with a higher mortality in men, but not in women, and not in NSTE‐ACS. In patients without acute coronary syndromes, PCI in more than 1 vessel, PCI in CABG, and PCI in unprotected left main coronary artery were associated with higher mortality in women, but not in men. The reasons for these procedure‐associated differences in hospital mortality cannot be explained by the data of this registry and should be further investigated.
Limitations
Our data are taken from a German population and describe the treatment reality in German hospitals. So our data may be not generalizable to other populations in other countries. As we report about an invasive coronary angiography/PCI registry we have no data about patients who were primarily treated noninvasively. The diagnosis of CAD is subjective and not based on objective measurement (such as quantitative coronary angiography). We have no information about the vascular access, but we guess that the rate of radial access in the years 2007‐2009 was less than 10% in Germany. The completeness of revascularization in both sexes cannot be evaluated with our data. The present analysis is not a randomized, controlled study, and all treatment decisions were left to the discretion of the physician. There was no documentation of concomitant medical treatment. The analysis was designed after the data had been collected. Therefore, the results have to be interpreted as descriptive. On the other hand, this investigation is one the largest analyses on a contemporary population and, therefore, is likely to reliably reflect the current clinical practice.
Conclusion
The present analysis gives a representative overview of sex‐associated differences in PCI for different indications in Germany. Hospital mortality after PCI for STEMI was 20% higher in women than in men, but there was no difference in hospital mortality after PCI for NSTE‐ACS, for cardiogenic shock, and after elective PCI. Nonfatal postinterventional major adverse cardiac and cerebrovascular events were higher in women with PCI for STEMI and after elective PCI. Access‐related complications were twice as high in women as in men, irrespective of the indication. The reasons for these differences need to be addressed in future research.
Sources of Funding
This work was supported by the German Society of Cardiology and The Stiftung Institut für Herzinfarktforschung Ludwigshafen. The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Disclosures
None.
Supporting information
Table S1. Baseline and Procedural Characteristics, Elective PCI
Table S2. Baseline and Procedural Characteristics, PCI in NSTE‐ACS, No Cardiogenic Shock
Table S3. Baseline and Procedural Characteristics, PCI in STEMI, No Cardiogenic Shock
Table S4. Baseline and Procedural Characteristics, PCI in Cardiogenic Shock
Table S5. In‐Hospital Course and Procedure‐Related Complications, Elective PCI
Table S6. Hospital Course and Procedure‐Related Complications, PCI in NSTE‐ACS, No Cardiogenic Shock
Table S7. Hospital Course and Procedure‐Related Complications, PCI in STEMI, No Cardiogenic Shock
Table S8. Hospital Course and Procedure‐Related Complications, PCI in Cardiogenic Shock
Acknowledgments
We thank all 218 hospitals that transferred data to the BQS or consecutively enrolled patients in the German ALKK registry from 2004 until 2009. These data were taken to perform the present analysis.
(J Am Heart Assoc. 2017;6:e004972. DOI: 10.1161/JAHA.116.004972.)
References
- 1. Meinertz T, Diegeler A, Stiller B, Fleck E, Heinemann MK, Schmaltz AA, Vestweber M, Bestehorn K, Beckmann A, Hamm C, Cremer J. German heart report 2013. Clin Res Cardiol. 2015;104:112–123. [DOI] [PubMed] [Google Scholar]
- 2. Nichols M, Townsend N, Scarborough P, Rayner M. Trends in age‐specific coronary heart disease mortality in the European Union over three decades: 1980‐2009. Eur Heart J. 2013;34:3017–3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, New G, Grines CL, Pietras CG, Kern MJ, Ferrell M, Leon MB, Mehran R, White C, Mieres JH, Moses JW, Stone GW, Jacobs AK; American College of Cardiology Foundation, American Heart Association . Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005;111:940–953. [DOI] [PubMed] [Google Scholar]
- 4. Daly C, Clemens F, Lopez Sendon JL, Tavazzi L, Boersma E, Danchin N, Delahaye F, Gitt A, Julian D, Mulcahy D, Ruzyllo W, Thygesen K, Verheugt F, Fox KM; Euro Heart Survey Investigators . Gender differences in the management and clinical outcome of stable angina. Circulation. 2006;113:490–498. [DOI] [PubMed] [Google Scholar]
- 5. Heer T, Schiele R, Schneider S, Gitt AK, Wienbergen H, Gottwik M, Gieseler U, Voigtlander T, Hauptmann KE, Wagner S, Senges J. Gender differences in acute myocardial infarction in the era of reperfusion (the MITRA Registry). Am J Cardiol. 2002;89:511–517. [DOI] [PubMed] [Google Scholar]
- 6. Heer T, Gitt AK, Juenger C, Schiele R, Wienbergen H, Towae F, Gottwitz M, Zahn R, Zeymer U, Senges J; Investigators A . Gender differences in acute non‐ST‐segment elevation myocardial infarction. Am J Cardiol. 2006;98:160–166. [DOI] [PubMed] [Google Scholar]
- 7. Heer T, Hochadel M, Schmidt K, Mehilli J, Zahn R, Kuck KH, Hamm C, Bohm M, Ertl G, Andresen D, Massberg S, Senges J, Pilz G, Gitt AK, Zeymer U. Gender differences in therapeutic recommendation after diagnostic coronary angiography: insights from the Coronary Angiography and PCI Registry of the German Society of Cardiology. Clin Res Cardiol. 2015;104:507–517. [DOI] [PubMed] [Google Scholar]
- 8. Alfredsson J, Stenestrand U, Wallentin L, Swahn E. Gender differences in management and outcome in non‐ST‐elevation acute coronary syndrome. Heart. 2007;93:1357–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hasdai D, Porter A, Rosengren A, Behar S, Boyko V, Battler A. Effect of gender on outcomes of acute coronary syndromes. Am J Cardiol. 2003;91:1466–1469. [DOI] [PubMed] [Google Scholar]
- 10. Stone GW, Grines CL, Browne KF, Marco J, Rothbaum D, O'Keefe J, Hartzler GO, Overlie P, Donohue B, Chelliah N, Vlietstra R, Puchrowicz‐Ochocki S, O'Neill WW. Comparison of in‐hospital outcome in men versus women treated by either thrombolytic therapy or primary coronary angioplasty for acute myocardial infarction. Am J Cardiol. 1995;75:987–992. [DOI] [PubMed] [Google Scholar]
- 11. Mehilli J, Kastrati A, Dirschinger J, Bollwein H, Neumann FJ, Schomig A. Differences in prognostic factors and outcomes between women and men undergoing coronary artery stenting. JAMA. 2000;284:1799–1805. [DOI] [PubMed] [Google Scholar]
- 12. Theres H, Maier B, Matteucci Gothe R, Schnippa S, Kallischnigg G, Schuren KP, Thimme W; Berliner Herzinfarktregister e V . Influence of gender on treatment and short‐term mortality of patients with acute myocardial infarction in Berlin. Z Kardiol. 2004;93:954–963. [DOI] [PubMed] [Google Scholar]
- 13. de Boer SP, Roos‐Hesselink JW, van Leeuwen MA, Lenzen MJ, van Geuns RJ, Regar E, van Mieghem NM, van Domburg R, Zijlstra F, Serruys PW, Boersma E. Excess mortality in women compared to men after PCI in STEMI: an analysis of 11,931 patients during 2000‐2009. Int J Cardiol. 2014;176:456–463. [DOI] [PubMed] [Google Scholar]
- 14. Fengler K, Fuernau G, Desch S, Eitel I, Neumann FJ, Olbrich HG, de Waha A, de Waha S, Richardt G, Hennersdorf M, Empen K, Hambrecht R, Fuhrmann J, Bohm M, Poess J, Strasser R, Schneider S, Schuler G, Werdan K, Zeymer U, Thiele H. Gender differences in patients with cardiogenic shock complicating myocardial infarction: a substudy of the IABP‐SHOCK II‐trial. Clin Res Cardiol. 2014;104:71–78. [DOI] [PubMed] [Google Scholar]
- 15. Gevaert SA, De Bacquer D, Evrard P, Convens C, Dubois P, Boland J, Renard M, Beauloye C, Coussement P, De Raedt H, de Meester A, Vandecasteele E, Vranckx P, Sinnaeve PR, Claeys MJ. Gender, TIMI risk score and in‐hospital mortality in STEMI patients undergoing primary PCI: results from the Belgian STEMI registry. EuroIntervention. 2014;9:1095–1101. [DOI] [PubMed] [Google Scholar]
- 16. Glaser R, Selzer F, Jacobs AK, Laskey WK, Kelsey SF, Holper EM, Cohen HA, Abbott JD, Wilensky RL. Effect of gender on prognosis following percutaneous coronary intervention for stable angina pectoris and acute coronary syndromes. Am J Cardiol. 2006;98:1446–1450. [DOI] [PubMed] [Google Scholar]
- 17. Kim C, Redberg RF, Pavlic T, Eagle KA. A systematic review of gender differences in mortality after coronary artery bypass graft surgery and percutaneous coronary interventions. Clin Cardiol. 2007;30:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mohr V, Bauer J, Döbler K, Fischer B, Woldenga C, Höfele F. Qualität sichtbar machen. BQS‐Qualitätsreport. Düsseldorf: BQS Bundesgeschäftsstelle Qualitätssicherung gGmbH; 2002. [Google Scholar]
- 19. Zeymer U, Zahn R, Hochadel M, Bonzel T, Weber M, Gottwik M, Tebbe U, Senges J. Indications and complications of invasive diagnostic procedures and percutaneous coronary interventions in the year 2003. Results of the quality control registry of the Arbeitsgemeinschaft Leitende Kardiologische Krankenhausarzte (ALKK). Z Kardiol. 2005;94:392–398. [DOI] [PubMed] [Google Scholar]
- 20. Zeymer U, Hochadel M, Zahn R, Kuck KH, Brachmann J, Senges J, Ertl G, Hamm C, Böhm M. Indikationen zur Koronarangiographie und perkutanen koronaren Intervention (PCI) in Deutschland von 2004 bis 2009. Der Kardiologe. 2012;6:390–398. [Google Scholar]
- 21. Shaw LJ, Bairey Merz CN, Pepine CJ, Reis SE, Bittner V, Kelsey SF, Olson M, Johnson BD, Mankad S, Sharaf BL, Rogers WJ, Wessel TR, Arant CB, Pohost GM, Lerman A, Quyyumi AA, Sopko G; WISE Investigators . Insights from the NHLBI‐Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study: part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender‐optimized diagnostic strategies. J Am Coll Cardiol. 2006;47:S4–S20. [DOI] [PubMed] [Google Scholar]
- 22. Sharaf BL, Pepine CJ, Kerensky RA, Reis SE, Reichek N, Rogers WJ, Sopko G, Kelsey SF, Holubkov R, Olson M, Miele NJ, Williams DO, Merz CNB. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI‐sponsored Women's Ischemia Syndrome Evaluation [WISE] study angiographic core laboratory). Am J Cardiol. 2001;87:937–941. [DOI] [PubMed] [Google Scholar]
- 23. Kouraki K, Muth K, Zahn R, Bauer T, Koeth O, Junger C, Gitt A, Senges J, Zeymer U; Acute Coronary Syndromes Registry Investigators . Effect of an invasive strategy on in‐hospital outcome and one‐year mortality in women with non‐ST‐elevation myocardial infarction. Int J Cardiol. 2011;153:291–295. [DOI] [PubMed] [Google Scholar]
- 24. Lagerqvist B, Säfström K, Ståhle E, Wallentin L, Swahn E. Is early invasive treatment of unstable coronary artery disease equally effective for both women and men? J Am Coll Cardiol. 2001;38:41–48. [DOI] [PubMed] [Google Scholar]
- 25. Clayton TC, Pocock SJ, Henderson RA, Poole‐Wilson PA, Shaw TR, Knight R, Fox KA. Do men benefit more than women from an interventional strategy in patients with unstable angina or non‐ST‐elevation myocardial infarction? The impact of gender in the RITA 3 trial. Eur Heart J. 2004;25:1641–1650. [DOI] [PubMed] [Google Scholar]
- 26. Hanssen M, Cottin Y, Khalife K, Hammer L, Goldstein P, Puymirat E, Mulak G, Drouet E, Pace B, Schultz E, Bataille V, Ferrieres J, Simon T, Danchin N; Fast‐MI 2010 Investigators . French registry on acute ST‐elevation and non ST‐elevation myocardial infarction 2010. FAST‐MI 2010. Heart. 2012;98:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe: epidemiological update. Eur Heart J. 2013;34:3028–3034. [DOI] [PubMed] [Google Scholar]
- 28. Puymirat E, Simon T, Steg PG, Schiele F, Gueret P, Blanchard D, Khalife K, Goldstein P, Cattan S, Vaur L, Cambou JP, Ferrieres J, Danchin N. Association of changes in clinical characteristics and management with improvement in survival among patients with ST‐elevation myocardial infarction. JAMA. 2012;308:998–1006. [DOI] [PubMed] [Google Scholar]
- 29. Radovanovic D, Erne P, Urban P, Bertel O, Rickli H, Gaspoz JM; AMIS Plus Investigators . Gender differences in management and outcomes in patients with acute coronary syndromes: results on 20,290 patients from the AMIS Plus Registry. Heart. 2007;93:1369–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shaw LJ, Shaw RE, Merz CN, Brindis RG, Klein LW, Nallamothu B, Douglas PS, Krone RJ, McKay CR, Block PC, Hewitt K, Weintraub WS, Peterson ED; American College of Cardiology‐National Cardiovascular Data Registry Investigators . Impact of ethnicity and sex differences on angiographic coronary artery disease prevalence and in‐hospital mortality in the American College of Cardiology‐National Cardiovascular Data Registry. Circulation. 2008;117:1787–1801. [DOI] [PubMed] [Google Scholar]
- 31. Simon T, Mary‐Krause M, Cambou JP, Hanania G, Gueret P, Lablanche JM, Blanchard D, Genes N, Danchin N; USIC Investigators . Impact of age and gender on in‐hospital and late mortality after acute myocardial infarction: increased early risk in younger women: results from the French nation‐wide USIC registries. Eur Heart J. 2006;27:1282–1288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Baseline and Procedural Characteristics, Elective PCI
Table S2. Baseline and Procedural Characteristics, PCI in NSTE‐ACS, No Cardiogenic Shock
Table S3. Baseline and Procedural Characteristics, PCI in STEMI, No Cardiogenic Shock
Table S4. Baseline and Procedural Characteristics, PCI in Cardiogenic Shock
Table S5. In‐Hospital Course and Procedure‐Related Complications, Elective PCI
Table S6. Hospital Course and Procedure‐Related Complications, PCI in NSTE‐ACS, No Cardiogenic Shock
Table S7. Hospital Course and Procedure‐Related Complications, PCI in STEMI, No Cardiogenic Shock
Table S8. Hospital Course and Procedure‐Related Complications, PCI in Cardiogenic Shock


