Abstract
Background
Heart failure (HF) is a serious complication of acute myocardial infarction (AMI). We explored the excess mortality associated with HF as an early or late complication of AMI and describe changes over time in such excess mortality.
Methods and Results
All patients hospitalized with an incident AMI and without history of prior HF hospitalization were followed up to 1 year after AMI discharge for episodes of HF. New HF episodes were classified as in‐hospital HF if diagnosed during the AMI hospitalization or postdischarge HF if diagnosed within 1 year after discharge from the incident AMI. Logistic and Cox regression models were used to explore the excess mortality associated with HF categories. Changes over time in the excess mortality were assessed by testing the interaction between HF status and study year. In‐hospital HF increased in‐hospital mortality 1.79 times (odds ratio [OR], 1.79; 95% CI: 1.68–1.91). The excess mortality associated with HF increased by 4.3 times from 2001 to 2009 (P interaction<0.001) as a consequence of a greater decline of in‐hospital mortality among AMI patients without (9% per year) compared to those with in‐hospital HF (3% per year). Postdischarge HF increased all‐cause and CVD mortality 5.98 times (hazard ratio, 5.98; 95% CI: 5.39–6.64) and 7.93 times (subhazard ratio, 7.93; 95% CI: 6.84 –9.19), respectively. The relative excess 1‐year mortality associated with HF did not change significantly over time.
Conclusions
Development of HF—either as an early or late complication of AMI—has a negative impact on patients' survival. Changes in the excess mortality associated with HF are driven by modest improvements in survival among AMI patients with HF as compared to those without HF.
Keywords: acute myocardial infarction, CVDNOR, heart failure, mortality, Norway, trends
Subject Categories: Heart Failure, Epidemiology, Cardiovascular Disease
Introduction
Heart failure (HF) is a serious condition affecting 38 million patients worldwide.1 Its prevalence is expected to increase because of aging of the population and improved survival of patients experiencing a cardiovascular event.2
Acute myocardial infarction (AMI) is a frequent cause of HF.3 The development of HF has a negative impact on the prognosis of AMI patients4, 5, 6, 7 and is accordingly regarded as “a warning sign for death” among them.8
The prognostic impact of HF in patients suffering an AMI has mainly been explored in association with short‐term mortality.5, 7, 9, 10, 11 A few analyses have expanded the observation period to include the AMI's postdischarge phase.12, 13 Therefore, the longer‐term prognostic impact of HF is poorly understood. Furthermore, little is known about recent changes over time on the short‐ and long‐term prognostic impact of HF.
Although the overall survival of AMI patients has improved significantly during the last 2 decades,14, 15, 16, 17 no survival analyses stratified by HF status have been published. Thus, it is not known whether the improved survival after an AMI occur both in patients who did, and did not, develop HF.
The objective of our study was to explore the impact of HF on in‐hospital and 1‐year mortality in AMI patients, with particular focus on changes over time in such prognostic impact. To aid our understanding of such changes, we also analyzed trends in mortality (in‐hospital and 1‐year mortality) by HF status using the nationwide cohort of patients hospitalized with an incident AMI in Norway during 2001–2009.
Methods
Data Sources
The Cardiovascular Disease in Norway project
The Cardiovascular Disease in Norway (CVDNOR) project (https://cvdnor.b.uib.no) contains information on CVD and diabetes mellitus–related hospitalizations in Norway during 1994–2009. Data were retrieved from the electronic patient administrative systems and include information on patients' demographics, admission and discharge dates, discharge diagnoses (up to 20), as well as all diagnostic and treatment procedures during each hospital stay.18, 19 Deaths occurring in and outside Norway during the same period were retrieved from the Norwegian Cause of Death Registry and linked to the hospitalization data using the unique and permanent personal identification number assigned to each Norwegian resident.
Study Population, Exposure, and Outcomes
All patients aged 25 to 84 years, hospitalized with an incident (first) AMI20 (ICD–10 codes I21, I22) during 2001–2009 and without prior history of HF (ICD‐9 codes 402, 425.x, 428, 429.1, and 429.3 or ICD‐10 codes I11.0, I13.0, I13.2, I42.x, I43.x, and I.50.x) were included in the analyses.
The occurrence of HF during follow‐up was identified using discharge diagnosis codes (ICD‐10 codes, I50.x). HF was classified as “in‐hospital HF” if diagnosed during the hospital stay for the incident AMI and “postdischarge HF” if developed within 1 year after discharge from the incident AMI.21
The relative excess mortality associated with HF (also referred to here as the “prognostic impact of HF”) was calculated as the ratio between the odds of dying among AMI patients with HF and those without HF. The prognostic impact of in‐hospital HF was explored in connection with in‐hospital mortality. As the in‐hospital mortality may be influenced by the length of AMI hospitalization, we additionally explored the prognostic impact of in‐hospital HF on 30‐day mortality.
The prognostic impact of postdischarge HF was explored in connection with all‐cause and cardiovascular (ICD‐10 codes, I00–I99) mortality within 1 year after discharge from the incident AMI (1‐year mortality). Only patients discharged alive from the incident AMI and without in‐hospital HF were included in the latter analyses.
Comorbidities and AMI Complications
Information on relevant medical conditions such as hypertension (I10–I15), diabetes mellitus (E10–E14), renal failure (N17–N19), chronic obstructive pulmonary disease (J40–J44, J47), valvular heart disease (I05–I09; I34–I35), and atrial fibrillation (I48) was retrieved from any field of discharge diagnosis. Similarly, we identified patients in whom AMI was complicated with pulmonary edema (J81), cardiogenic shock (R57.0), second‐ (I44.1), or third‐ (I44.2) degree atrioventricular block, ventricular fibrillation (I49.0), or mechanical complications (I23).
Data Analyses
Continuous variables are reported as means and SD and categorical data are reported as proportions.
The prognostic impact of in‐hospital HF was explored using logistic regression and results are presented as odds ratio (OR) and 95% CI. The prognostic impact of postdischarge HF on all‐cause mortality was explored using Cox models with HF as a time‐varying covariate and results are expressed as hazard ratio and 95% CI. In the analyses of CVD mortality, death attributable to other causes was treated as a competing risk event and results are expressed as subhazard ratios (SHR) and 95% CI.
Changes over time in the excess mortality associated with HF were explored by testing the interactions between HF status and study year in separate analyses for in‐hospital and postdischarge HF.
Trends in the In‐Hospital, 30‐Day, and 1‐Year Mortality by HF Status
To better understand the factors influencing changes over time in the excess mortality associated with HF, we analyzed time trends in the in‐hospital, 30‐day, and 1‐year mortality by HF status. In these analyses, the year of AMI was the independent variable. The estimated average annual changes in the in‐hospital, 30‐day, and 1‐year mortality were reported as OR, hazard ratio, and SHR, respectively. Analyses were adjusted for sex, age, history of prior coronary heart disease (CHD)–related hospitalization, hypertension, diabetes mellitus, renal failure, obstructive pulmonary disease, valvular heart disease, and atrial fibrillation.
Trends in the Utilization of Myocardial Revascularization During the Incident AMI Hospitalization
We also compared rates of coronary revascularization procedures (percutaneous coronary intervention [PCI] and coronary artery bypass grafting) between patients with and without HF.
Statistical analyses were performed using Stata Statistical Software: Release 14 (Stata Corp LP, College Station, TX). The study protocol was approved by the Regional Committee for Medical and Health Research Ethics, Health Region West (2015/2048).
Results
Baseline Characteristics of the Cohort
A flowchart of patients' enrollment is presented in Figure 1. A total of 69 372 patients, of whom 68.4% were male, were included in the study (Table 1). The mean age (SD) was 66.4 (12.3) years. A total of 11 831 patients (17.1% of the cohort) were discharged from the AMI hospitalization with a diagnosis of HF (in‐hospital HF). Another 2566 patients (5.4% of the population at risk) developed postdischarge HF (Table 1).
Figure 1.
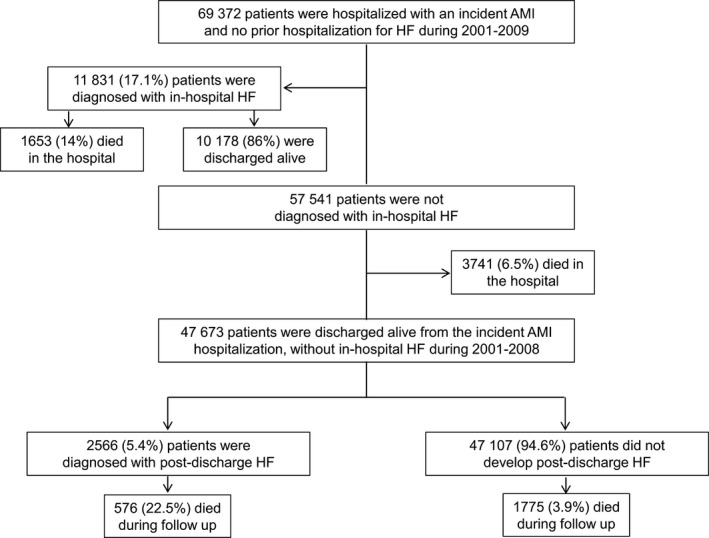
Flowchart of patients' enrollment and timing of development of heart failure in relation to the incident acute myocardial infarction.
Table 1.
Baseline Characteristics of Patients Hospitalized With an Incident AMI in Norway During 2001–2009
| Patients' Characteristics | All Patients (n=69 372) | Patients With Heart Failure (n=14 397) | ||
|---|---|---|---|---|
| In‐Hospital Heart Failure (n=11 831) | Postdischarge Heart Failure (n=2566) | P Valuea | ||
| Sex (male), n (%) | 47 479 (68.4) | 7480 (63.2) | 1608 (62.7) | 0.562 |
| Age (y), mean (SD) | 66.4 (12.3) | 71.0 (11.0) | 72.7 (9.9) | <0.001 |
| Age categories, n (%) | <0.001 | |||
| 25 to 69 years | 37 608 (54.2) | 4365 (36.9) | 747 (29.1) | |
| 70 to 84 years | 31 764 (45.8) | 7466 (63.1) | 1819 (70.9) | |
| Prior CHD, n (%) | 8809 (12.7) | 1682 (14.2) | 544 (21.2) | <0.001 |
| Comorbidities, n (%) | ||||
| Hypertension | 20 276 (29.2) | 3191 (27.0) | 792 (30.9) | <0.001 |
| Diabetes mellitus | 9046 (13.0) | 2152 (18.2) | 493 (19.2) | 0.231 |
| COPD | 5019 (7.2) | 1272 (10.8) | 309 (12.0) | 0.162 |
| Renal failure | 1651 (2.4) | 577 (4.9) | 118 (4.6) | 0.253 |
| Valvular heart disease | 3759 (5.4) | 1524 (12.9) | 252 (9.8) | <0.001 |
| Atrial fibrillation | 7996 (11.5) | 2429 (20.5) | 544 (21.2) | 0.621 |
| AMI complications, n (%) | ||||
| Ventricular fibrillation | 1300 (1.9) | 393 (3.3) | 87 (1.8) | <0.001 |
| Pulmonary edema | 353 (0.5) | 218 (1.8) | 37 (0.7) | <0.001 |
| Cardiogenic shock | 685 (1.0) | 250 (2.1) | 7 (0.3) | <0.001 |
| AV block (2nd/3rd degree) | 933 (1.3) | 231 (1.9) | 42 (1.6) | 0.281 |
| Mechanical complications | 675 (1.0) | 230 (1.9) | 20 (0.8) | <0.001 |
AMI indicates acute myocardial infarction; AV, atrioventricular; CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease.
Age‐adjusted comparisons of patients with in‐hospital and those with postdischarge heart failure.
Compared to patients with postdischarge HF, patients with in‐hospital HF were younger and less often had a prior CHD‐related hospitalization (both P<0.001). Complications including ventricular fibrillation, pulmonary edema, and cardiogenic shock were more common in patients with in‐hospital compared to those with postdischarge HF (P for all comparisons <0.001).
Prevalence of Comorbidities at Different Time Periods in Patients Diagnosed With HF
The prevalence of comorbidities in patients diagnosed with in‐hospital or postdischarge HF is presented for each time period of AMI admission in Figure 2. In patients with in‐hospital HF, the prevalence of comorbidities increased from 2001–2003 to 2007–2009; hypertension from 20.1% to 33.1%, obstructive pulmonary disease from 9.6% to 11.6%, renal failure from 3.4% to 6.6%, valvular heart disease from 11.8% to 13.6%, and atrial fibrillation from 20.0% to 21.1% (all P for trend<0.001). The prevalence of AMI complications also increased over the study periods: ventricular fibrillation from 2.6% to 4.1% (P for trend=0.011), pulmonary edema from 1.1% to 2.4% (P for trend<0.001), and cardiogenic shock from 1.4% to 2.5% (P for trend=0.003). Similarly, in patients with late‐onset HF, we observed increases in the prevalence of hypertension (from 22.4% to 41.4%; P for trend<0.001), diabetes mellitus (from 17.1% to 21.4%; P for trend=0.023), renal failure (from 3.8% to 5.1%; P for trend=0.015), valvular heart disease (from 8.4% to 11.4%; P for trend=0.006), and atrial fibrillation (18.2–28.1%; P for trend<0.001). No significant changes were observed in the prevalence of AMI complications (Figure 2).
Figure 2.
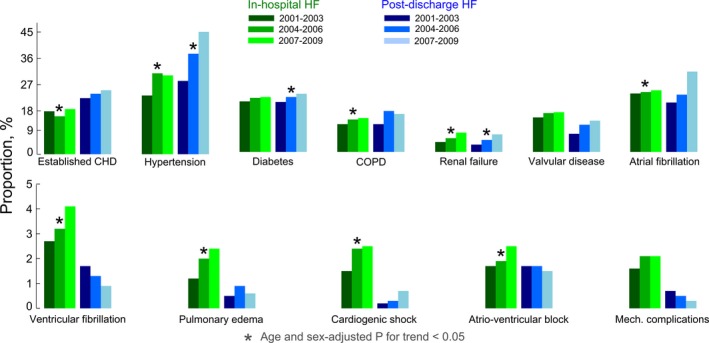
Changes over time in the prevalence of baseline comorbidities in acute myocardial infarction patients developing in‐hospital and postdischarge heart failure. CHD indicates coronary heart disease; COPD, chronic obstructive pulmonary disease; HF, heart failure.
Prognostic Impact of In‐Hospital HF on Early Mortality
In‐hospital mortality
Overall, 5394 AMI patients did not survive the incident AMI hospitalization. The 17.1% of patients who developed in‐hospital HF during 2001–2009 contributed 30.6% of in‐hospital deaths. In 2001, patients with in‐hospital HF accounted for 15.4% of all AMI cases and contributed 22.8% of in‐hospital deaths while in 2009 they accounted for 17.9% of all AMI cases and contributed 38.4% of in‐hospital deaths.
Overall, the adjusted in‐hospital mortality risk in patients with HF was 1.79 times higher than in those without HF (OR=1.79; 95% CI: 1.68–1.91). The excess in‐hospital mortality associated with HF increased 4.3 times over the study period (from 25% in 2001 to 133% in 2009; P for interaction<0.001) (Figure 3 and Table S1). Although in‐hospital mortality rates were reduced in both patients with and without HF, the decline was more pronounced among patients without HF compared to those with HF (9% per year [OR=0.91; 95% CI: 0.89–0.93] versus 3% per year [OR=0.97; 95% CI: 0.95–0.99], respectively) (Table 2 and Figure 4).
Figure 3.
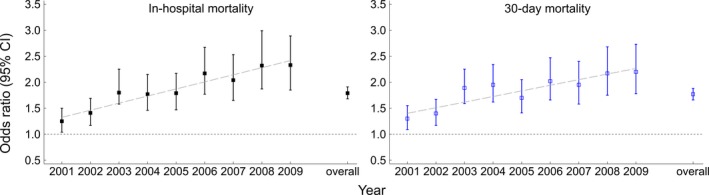
Changes over time in the in‐hospital and 30‐day excess mortality associated with the development of in‐hospital heart failure.
Table 2.
Time Trends in In‐Hospital and 30‐Day Mortality by In‐Hospital Heart Failure Status
| Study Year | No Heart Failure | Heart Failure | ||||
|---|---|---|---|---|---|---|
| AMI, | Deaths, n (%) | Odds Ratioa (95% CI) | AMI, n | Deaths, n (%) | Odds Ratioa (95% CI) | |
| In‐hospital mortality | ||||||
| 2001 | 6756 | 660 (9.8) | 1reference | 1232 | 195 (15.8) | 1reference |
| 2002 | 6675 | 574 (8.6) | 0.91 (0.81–1.03) | 1302 | 202 (15.5) | 0.99 (0.80–1.23) |
| 2003 | 6651 | 496 (7.5) | 0.81 (0.71–0.92) | 1426 | 234 (16.4) | 1.10 (0.89–1.36) |
| 2004 | 6270 | 452 (7.2) | 0.79 (0.70–0.90) | 1235 | 195 (15.8) | 1.07 (0.86–1.34) |
| 2005 | 6106 | 399 (6.5) | 0.76 (0.66–0.86) | 1315 | 186 (14.1) | 1.02 (0.82–1.27) |
| 2006 | 6180 | 332 (5.4) | 0.63 (0.55–0.72) | 1302 | 178 (13.7) | 1.00 (0.80–1.25) |
| 2007 | 6134 | 312 (5.1) | 0.61 (0.53–0.70) | 1296 | 155 (12.0) | 0.89 (0.71–1.12) |
| 2008 | 6395 | 269 (4.2) | 0.51 (0.44–0.59) | 1335 | 154 (11.5) | 0.86 (0.68–1.08) |
| 2009 | 6374 | 247 (3.9) | 0.47 (0.41–0.55) | 1388 | 154 (11.1) | 0.82 (0.65–1.04) |
| Annual change | 0.91 (0.89–0.93) | 0.97 (0.95–0.99) | ||||
| 30‐day mortality | ||||||
| 2001 | 6756 | 708 (10.5) | 1reference | 1232 | 217 (17.6) | 1reference |
| 2002 | 6675 | 623 (9.3) | 0.92 (0.82–1.04) | 1302 | 217 (16.7) | 0.96 (0.78–1.18) |
| 2003 | 6651 | 531 (8.0) | 0.80 (0.71–0.91) | 1426 | 252 (17.7) | 1.07 (0.87–1.31) |
| 2004 | 6270 | 480 (7.7) | 0.78 (0.69–0.88) | 1235 | 219 (17.7) | 1.10 (0.89–1.35) |
| 2005 | 6106 | 442 (7.2) | 0.78 (0.69–0.89) | 1315 | 198 (15.1) | 0.98 (0.79–1.22) |
| 2006 | 6180 | 363 (5.9) | 0.64 (0.56–0.73) | 1302 | 184 (14.1) | 0.93 (0.75–1.16) |
| 2007 | 6134 | 352 (5.7) | 0.64 (0.55–0.73) | 1296 | 167 (12.9) | 0.88 (0.70–1.10) |
| 2008 | 6395 | 301 (4.7) | 0.53 (0.46–0.61) | 1335 | 162 (12.1) | 0.82 (0.65–1.03) |
| 2009 | 6374 | 279 (4.4) | 0.50 (0.43–0.58) | 1388 | 167 (12.0) | 0.82 (0.64–1.02) |
| Annual change | 0.92 (0.91–0.94) | 0.97 (0.94–0.99) | ||||
AMI indicates acute myocardial infarction.
Analyses adjusted for sex, age, previous coronary heart disease, hypertension, diabetes mellitus, renal failure, chronic obstructive pulmonary disease, valvular heart disease, and atrial fibrillation.
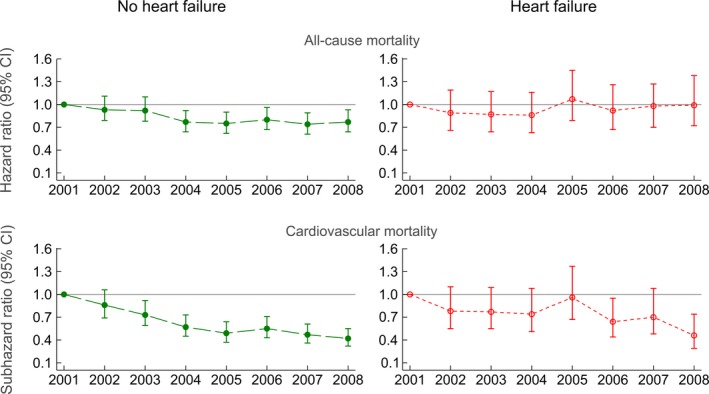
Figure 4.
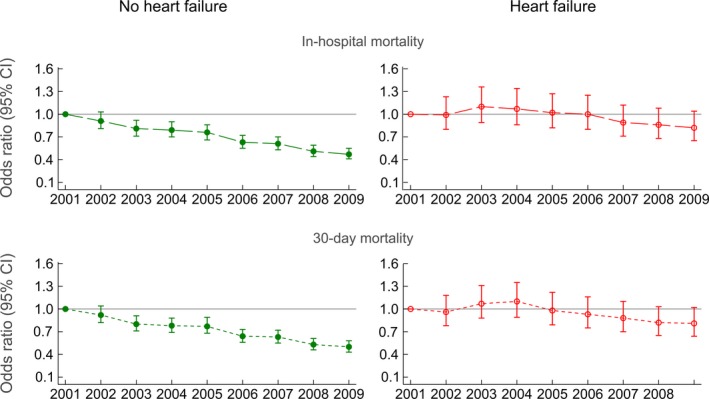
Time trends of in‐hospital and 30‐day mortality by in‐hospital heart failure status.
30‐day mortality
From 2001 to 2009, the length of hospitalization for an incident AMI was reduced significantly (Table S2). However, patients with HF had a longer hospitalization stay than those without HF. To account for the potential effect of differences in the length of AMI hospitalization on prognostic impact of HF, we repeated the analyses using 30‐day mortality as an alternative end point to in‐hospital mortality (used in the main analyses). The adjusted 30‐day mortality risk in patients with HF was 1.77 times higher than in those without HF (OR=1.77; 95% CI: 1.66–1.88). The excess mortality associated with HF increased by 3 times over the study period (from 30% in 2001 to 120% in 2009; P for interaction<0.001) (Figure 3 and Table S1). Patients with and without in‐hospital HF both experienced reductions in 30‐day mortality rates over time, but the decline was steeper among patients without HF compared to those with (8% per year [OR=0.92; 95% CI: 0.91–0.93] versus 3% per year [OR=0.97; 95% CI: 0.95–0.99], respectively) (Table 2 and Figure 4).
Prognostic Impact of Postdischarge HF on 1‐Year Mortality
All‐cause mortality
Overall, 2349 patients died within 1 year after discharge from the incident AMI hospitalization. AMI patients who developed postdischarge HF during follow‐up accounted for 5.4% of AMI cases but contributed 24.5% of all deaths (Table 3). Overall, the adjusted 1‐year mortality risk among patients with HF was 5.98 times higher than in those without HF (hazard ratio=5.98; 95% CI: 5.39–6.64) (Figure 5 and Table S3). The excess mortality associated with HF did not change significantly over the study period (P for interaction=0.67). One‐year all‐cause mortality declined among patients without HF (5% per year [hazard ratio=0.95; 95% CI: 0.93–0.97]) but did not change significantly among those with HF (Table 3 and Figure 6). This was because of increases in the proportion of non‐CVD mortality among patients with HF (data not shown).
Table 3.
Time Trends in 1‐Year Mortality by Postdischarge Heart Failure Status
| Study Year | No Heart Failure | Heart Failure | ||||
|---|---|---|---|---|---|---|
| AMI, n | Deaths, n (%) | Hazard Ratioa, (95% CI) | AMI, n | Deaths, n (%) | Hazard Ratioa (95% CI) | |
| All‐cause mortality | ||||||
| 2001 | 5681 | 272 (4.8) | 1reference | 415 | 99 (23.9) | 1reference |
| 2002 | 5726 | 257 (4.5) | 0.93 (0.79–1.11) | 375 | 77 (20.5) | 0.89 (0.66–1.19) |
| 2003 | 5821 | 258 (4.4) | 0.93 (0.78–1.10) | 334 | 73 (21.9) | 0.87 (0.64–1.17) |
| 2004 | 5502 | 202 (3.7) | 0.77 (0.64–0.92) | 316 | 67 (21.2) | 0.86 (0.63–1.16) |
| 2005 | 5412 | 186 (3.4) | 0.75 (0.62–0.90) | 295 | 75 (25.4) | 1.07 (0.79–1.45) |
| 2006 | 5551 | 202 (3.6) | 0.80 (0.67–0.96) | 297 | 66 (22.2) | 0.92 (0.67–1.26) |
| 2007 | 5563 | 190 (3.4) | 0.74 (0.61–0.89) | 259 | 56 (21.6) | 0.98 (0.70–1.37) |
| 2008 | 5851 | 206 (3.5) | 0.77 (0.64–0.93) | 275 | 63 (22.9) | 0.99 (0.72–1.38) |
| Annual change | 0.95 (0.93–0.97) | 1.01 (0.97–1.05) | ||||
| Cardiovascular mortality | ||||||
| 2001 | 5681 | 179 (3.2) | 1reference | 415 | 77 (18.6) | 1reference |
| 2002 | 5726 | 158 (2.8) | 0.86 (0.69–1.06) | 375 | 53 (14.1) | 0.78 (0.55–1.10) |
| 2003 | 5821 | 136 (2.3) | 0.73 (0.59–0.92) | 334 | 51 (15.3) | 0.77 (0.55–1.09) |
| 2004 | 5502 | 101 (1.8) | 0.57 (0.45–0.73) | 316 | 45 (14.2) | 0.74 (0.51–1.08) |
| 2005 | 5412 | 81 (1.5) | 0.49 (0.37–0.64) | 295 | 53 (18.0) | 0.96 (0.67–1.37) |
| 2006 | 5551 | 95 (1.7) | 0.55 (0.43–0.71) | 297 | 37 (12.5) | 0.64 (0.44–0.95) |
| 2007 | 5563 | 83 (1.5) | 0.47 (0.36–0.61) | 259 | 34 (13.1) | 0.70 (0.48–1.08) |
| 2008 | 5851 | 78 (1.3) | 0.42 (0.32–0.55) | 275 | 24 (8.7) | 0.46 (0.29–0.74) |
| Annual change | 0.88 (0.85–0.91) | 0.93 (0.89–0.98) | ||||
AMI indicates acute myocardial infarction.
Analyses adjusted for sex, age, previous coronary heart disease, hypertension, diabetes mellitus, renal failure, chronic obstructive pulmonary disease, valvular heart disease, and atrial fibrillation.
Figure 5.
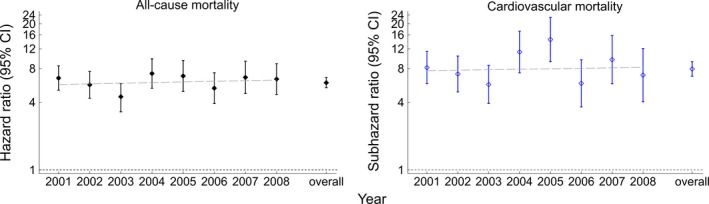
Changes over time in the 1‐year excess mortality associated with the development of postdischarge heart failure.
Figure 6.
Time trends of 1‐year mortality by postdischarge heart failure status.
CVD mortality
Overall, 1285 patients died because of CVD within a year from AMI discharge. AMI patients who developed postdischarge HF during follow‐up accounted for 5.4% of AMI cases but contributed 29.1% of all CVD deaths (Table 3). Overall, the adjusted 1‐year CVD mortality risk among patients with HF was 7.93 times higher (SHR=7.93; 95% CI: 6.84–9.19) compared to those without HF (Figure 5 and Table S3). The excess CVD mortality associated with HF did not change significantly over the study period (P for interaction=0.85). Both patient groups experienced declines in 1‐year CVD mortality (Table 3). The reduction was 12% per year (SHR=0.88; 95% CI: 0.85–0.91) in patients without HF and 7% per year (SHR=0.83; 95% CI: 0.89–0.98) in those with HF.
Myocardial Revascularization During the Incident AMI Hospitalization
In total, 38.6% of the study population received revascularization while hospitalized for the incident AMI. The corresponding proportions among patients with and without in‐hospital HF were 32.4% and 39.9%, respectively (P<0.001).
Overall, the odds of receiving myocardial revascularization in patients with in‐hospital HF were 10% lower (OR, 0.90; 95% CI, 0.86–0.94) than in those without in‐hospital HF (Table S4). These differences narrowed over the study period (P for interaction<0.001) because of the steeper increase in myocardial revascularization rates among patients with versus without HF (26% per year [OR=1.26; 95% CI: 1.23–1.28] versus 17% per year [OR=1.17; 95% CI: 1.16–1.19]).
Discussion
Our study demonstrates that development of HF has a substantial negative impact on survival among AMI patients. Such negative impact is strongly influenced by timing of HF occurrence in relation to AMI. In‐hospital HF nearly doubled the risk of dying at the hospital. Moreover, the excess mortality associated with this HF category increased significantly over the study period, because of more modest improvement in survival among AMI patients with, versus those without HF. Postdischarge HF increased the risk of 1‐year all‐cause and CVD mortality by nearly 6 and 8 times, respectively, and its excess mortality remained stable over the study period.
A few studies have focused on the short‐term prognostic impact of HF among CHD patients. In a register‐based study enrolling 4825 patients with non‐ST‐elevation MI in Canada during 1999–2003, the presence of HF on admission increased the odds of in‐hospital mortality by 1.87 times.6 Similarly, HF on admission increased the odds of in‐hospital mortality by 2.2 times among 13 707 patients enrolled in the Global Registry of Acute Coronary Events (GRACE) registry from 1999 to 2001.11 In a pooled analysis of 7 randomized clinical trials including 46 519 non‐ST‐elevation myocardial infarction patients during 1994–2008, the presence of HF on admission or developing during the AMI hospitalization increased 30‐day mortality by 1.74 and 2.34 times, respectively, compared to patients without HF.22
Lewis et al23 assessed the prognostic impact of postdischarge HF in a cohort of 10 040 stable AMI survivors included in the Valsartan in Acute Myocardial Infarction (VALIANT) study. They reported an 8 times increase in the risk of dying during a median follow‐up of 25 months among patients with HF compared to those without HF. Another study included 25 324 patients with acute coronary syndrome in Canada between 2002 and 2008 and found that postdischarge HF increased 1‐year mortality by 4.6 times.12
Results from our study extend previous knowledge on the negative impact of HF in prognosis of patients suffering an acute coronary event. To the best of our knowledge, it is the first analysis exploring simultaneously the role of HF developing while at the hospital or following AMI discharge on mortality, focusing on changes over time in the prognostic impact of HF.
The observed changes in the prognostic impact of HF should be interpreted in the context of the changes characterizing AMI clinical expression and survival. Although in‐hospital (and 30‐day) mortality following an AMI has improved overall, the proportion of AMI cases discharged with a diagnosis of HF increased by 20% during 2001–2009 (Sulo G et al, Unpublished data). This suggests that a higher proportion of patients are presenting with a more severe form of AMI, supported by the observed increase in the proportion of ventricular fibrillation, pulmonary edema, and cardiogenic shock as well as accompanying comorbidities. We have previously reported a decline of 47% in incident out‐of‐hospital coronary death rates during 2001–2009.20 Taken together, these findings indicate that the increasing proportion of severely ill patients reaching the hospital alive contribute to the increased burden of HF as an early complication of AMI.
Changes in the excess mortality associated with in‐hospital HF are explained by differences in the magnitude of reductions characterizing in‐hospital mortality between patients with and without HF; in‐hospital mortality in patients with HF declined modestly while among those without HF the decline was more pronounced. These different trends are likely to be influenced by differences in the trends of AMI severity between patients with and without HF. Indeed, we observed an increase in the prevalence of ventricular fibrillation, pulmonary edema, and cardiogenic shock (all reliable indicators of AMI severity) among patients with in‐hospital HF, while no changes in the prevalence of these indicators were observed among patients without HF.
Interestingly, the excess mortality associated with in‐hospital HF increased over time while gaps in the utilization of myocardial revascularization procedures between patients with and without HF procedures narrowed. Because of the observational nature of our study and lack of information on whether the myocardial revascularization preceded or came after the development of HF, we could not account for the role of revascularization in the analyses. However, it appears that the excess mortality associated with HF is also influenced by factors other than myocardial revascularization, including differences in the use and efficacy of cardiac drugs between patients with and without HF.24
Although postdischarge HF accounts for only 20% to 25% of AMI‐related HF, the excess mortality it conveys greatly exceeded that of in‐hospital HF. Thus, postdischarge HF is an important source of mortality. The excess mortality associated with postdischarge HF was more evident in relation to CVD than to all‐cause mortality. This is to be expected, as non‐CVD deaths involve other pathophysiological mechanisms, not directly influenced by HF.
Our results suggest that HF may, in the future, slow the rate of reductions characterizing CVD mortality, should the observed trends in the prognostic impact of HF continue. The modest improvements in short‐term survival among patients with HF are offset by increased HF incidence rates. Therefore, reducing the occurrence of HF by addressing coronary risk factors in the general population and shortening the time from onset of symptoms to receiving specialized care becomes of paramount importance in reducing CVD mortality.
Strength and Limitations
Our study is one of few analyses exploring simultaneously the prognostic impact of in‐hospital and postdischarge HF, with additional focus on changes over time characterizing this prognostic impact. The use of a nationwide cohort, without age, sex, or geographical restriction increases the generalizability of our findings. Moreover, troponin measurement was already included in the AMI diagnostic algorithm in Norway by 2001.25 Hence, the inclusion procedures of patients in the cohort were fairly consistent over the study period. We were also able to exclude previous episodes of AMI and HF using a retrospective search of 7 years.26
Our study has some potential limitations. Data were obtained from electronic patient administrative systems and do not include information on lifestyle indicators such as smoking, physical activity, obesity, or alcohol drinking patterns. Furthermore, we were unable to correctly classify all AMIs into ST‐elevation myocardial infarction and non‐ST‐elevation myocardial infarction based on ICD‐10 codes. Therefore, we did not conduct separate analyses for each AMI type. However, previous studies have demonstrated that the magnitude27, 28, 29 and prognostic impact11 of HF as a complication of the 2 AMI types are similar.
The CVDNOR database does not have information on HF severity or left ventricular ejection fraction. Therefore, we were unable to stratify analyses by HF severity. Although HF with preserved ejection fraction is thought to prevail in the community, its prognosis was found to be similar to that of HF with reduced ejection fraction.30
Patients presenting with HF on admission could not be distinguished from those developing HF during the AMI hospitalization; however, it has been reported that both components of early‐onset HF carry a similar risk on 30‐day mortality.22
We also lacked information on prescription of and adherence to medication upon hospital discharge and participation in rehabilitation programs. Hence, we could not assess the additional contribution of secondary prevention in the excess mortality associated with late‐onset HF.
Our results should be interpreted with caution and conclusions drawn considering the abovementioned limitations.
Conclusion
In‐hospital HF was associated with increased early mortality in patients hospitalized with an incident AMI. The in‐hospital and 30‐day survival gap between AMI groups increased over time because of slower declines in mortality rates among patients with, compared to those without in‐hospital HF. Postdischarge HF substantially increased 1‐year mortality following AMI discharge, although the excessive mortality associated with this HF category did not change significantly over the study period.
Sources of Funding
The University of Bergen funded Dr Gerhard Sulo and covered the publishing costs under “Open Access” platform for this work. The CVDNOR project has received funding from “Nasjonalforeningen for folkehelsen”.
Disclosures
None.
Supporting information
Table S1. Changes Over Time in the Excess Mortality Associated With In‐Hospital HF (Heart Failure)
Table S2. Length of Hospitalization for the Incident Acute Myocardial Infarction
Table S3. Changes Over Time in the Excess 1‐Year Mortality Associated With Postdischarge Heart Failure
Table S4. Changes Over Time in the Odds of Receiving Myocardial Revascularization Between Patients With and Without Early‐Onset Heart Failure: A CVDNOR Project
Acknowledgments
The authors thank Tomislav Dimoski at The Norwegian Knowledge Centre for the Health Services, Oslo, Norway for his contribution by developing the software necessary for obtaining data from Norwegian hospitals, conducting the data collection and quality assurance of data in this project.
(J Am Heart Assoc. 2017;6:e005277. DOI: 10.1161/JAHA.116.005277.)
References
- 1. Douglas LM, Felker GM. Heart Failure: A Companion to Braunwald's Heart Disease. 3rd ed Saunders, 2015. [Google Scholar]
- 2. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Pina IL, Trogdon JG. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, Hochadel M, Komajda M, Lassus J, Lopez‐Sendon JL, Ponikowski P, Tavazzi L. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–2736. [DOI] [PubMed] [Google Scholar]
- 4. Shah RV, Holmes D, Anderson M, Wang TY, Kontos MC, Wiviott SD, Scirica BM. Risk of heart failure complication during hospitalization for acute myocardial infarction in a contemporary population: insights from the National Cardiovascular Data ACTION Registry. Circ Heart Fail. 2012;5:693–702. [DOI] [PubMed] [Google Scholar]
- 5. Alsheikh‐Ali AA, Al‐Mallah MH, Al‐Mahmeed W, Albustani N, Al Suwaidi J, Sulaiman K, Zubaid M, Gulf RI. Heart failure in patients hospitalized with acute coronary syndromes: observations from the Gulf Registry of Acute Coronary Events (Gulf RACE). Eur J Heart Fail. 2009;11:1135–1142. [DOI] [PubMed] [Google Scholar]
- 6. Segev A, Strauss BH, Tan M, Mendelsohn AA, Lai K, Ashton T, Fitchett D, Grima E, Langer A, Goodman SG. Prognostic significance of admission heart failure in patients with non‐ST‐elevation acute coronary syndromes (from the Canadian Acute Coronary Syndrome Registries). Am J Cardiol. 2006;98:470–473. [DOI] [PubMed] [Google Scholar]
- 7. Wu AH, Parsons L, Every NR, Bates ER. Hospital outcomes in patients presenting with congestive heart failure complicating acute myocardial infarction: a report from the Second National Registry of Myocardial Infarction (NRMI‐2). J Am Coll Cardiol. 2002;40:1389–1394. [DOI] [PubMed] [Google Scholar]
- 8. Moller JE, Torp‐Pedersen C, Kober LV. Is heart failure the critical warning sign for death following myocardial infarction? Eur Heart J. 2008;29:833–834. [DOI] [PubMed] [Google Scholar]
- 9. Velazquez EJ, Francis GS, Armstrong PW, Aylward PE, Diaz R, O'Connor CM, White HD, Henis M, Rittenhouse LM, Kilaru R, van Gilst W, Ertl G, Maggioni AP, Spac J, Weaver WD, Rouleau JL, McMurray JJ, Pfeffer MA, Califf RM. An international perspective on heart failure and left ventricular systolic dysfunction complicating myocardial infarction: the VALIANT registry. Eur Heart J. 2004;25:1911–1919. [DOI] [PubMed] [Google Scholar]
- 10. Nunez‐Gil IJ, Garcia‐Rubira JC, Luaces M, Vivas D, De Agustin JA, Gonzalez‐Ferrer JJ, Bordes S, Macaya C, Fernandez‐Ortiz A. Mild heart failure is a mortality marker after a non‐ST‐segment acute myocardial infarction. Eur J Intern Med. 2010;21:439–443. [DOI] [PubMed] [Google Scholar]
- 11. Steg PG, Dabbous OH, Feldman LJ, Cohen‐Solal A, Aumont MC, Lopez‐Sendon J, Budaj A, Goldberg RJ, Klein W, Anderson FA Jr. Determinants and prognostic impact of heart failure complicating acute coronary syndromes: observations from the Global Registry of Acute Coronary Events (GRACE). Circulation. 2004;109:494–499. [DOI] [PubMed] [Google Scholar]
- 12. Kaul P, Ezekowitz JA, Armstrong PW, Leung BK, Savu A, Welsh RC, Quan H, Knudtson ML, McAlister FA. Incidence of heart failure and mortality after acute coronary syndromes. Am Heart J. 2013;165:379–385.e2. [DOI] [PubMed] [Google Scholar]
- 13. Torabi A, Cleland JG, Khan NK, Loh PH, Clark AL, Alamgir F, Caplin JL, Rigby AS, Goode K. The timing of development and subsequent clinical course of heart failure after a myocardial infarction. Eur Heart J. 2008;29:859–870. [DOI] [PubMed] [Google Scholar]
- 14. Chen HY, Gore JM, Lapane KL, Yarzebski J, Person SD, Gurwitz JH, Kiefe CI, Goldberg RJ. A 35‐year perspective (1975 to 2009) into the long‐term prognosis and hospital management of patients discharged from the hospital after a first acute myocardial infarction. Am J Cardiol. 2015;116:24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wong CX, Sun MT, Lau DH, Brooks AG, Sullivan T, Worthley MI, Roberts‐Thomson KC, Sanders P. Nationwide trends in the incidence of acute myocardial infarction in Australia, 1993–2010. Am J Cardiol. 2013;112:169–173. [DOI] [PubMed] [Google Scholar]
- 16. Koopman C, Bots ML, van Oeffelen AA, van Dis I, Verschuren WM, Engelfriet PM, Capewell S, Vaartjes I. Population trends and inequalities in incidence and short‐term outcome of acute myocardial infarction between 1998 and 2007. Int J Cardiol. 2013;168:993–998. [DOI] [PubMed] [Google Scholar]
- 17. Sulo E, Vollset SE, Nygard O, Sulo G, Igland J, Egeland GM, Ebbing M, Tell GS. Trends in 28‐day and 1‐year mortality rates in patients hospitalized for a first acute myocardial infarction in Norway during 2001–2009: a “Cardiovascular disease in Norway” (CVDNOR) project. J Intern Med. 2015;277:353–361. [DOI] [PubMed] [Google Scholar]
- 18. Sulo G, Igland J, Vollset SE, Nygård O, Øyen N, Tell GS. Cardiovascular disease and diabetes mellitus in Norway during 1994–2009: CVDNOR—a nationwide research project. Nor Epidemiol. 2013;23:101–107. [Google Scholar]
- 19. Igland J, Tell GS, Ebbing M, Nygård O, Vollset SE, Dimoski T. The CVDNOR project: Cardiovascular Disease in Norway 1994–2009. Description of data and data quality. 2013. Available at: http://cvdnor.b.uib.no/files/2013/08/CVDNOR-Data-and-Quality-Report1.pdf. Accessed October 2016.
- 20. Sulo G, Igland J, Nygard O, Vollset SE, Ebbing M, Tell GS. Favourable trends in incidence of AMI in Norway during 2001–2009 do not include younger adults: a CVDNOR project. Eur J Prev Cardiol. 2014;21:1358–1364. [DOI] [PubMed] [Google Scholar]
- 21. Sulo G, Igland J, Vollset SE, Nygard O, Ebbing M, Sulo E, Egeland GM, Tell GS. Heart failure complicating acute myocardial infarction; burden and timing of occurrence: a nation‐wide analysis including 86 771 patients from the Cardiovascular Disease in Norway (CVDNOR) Project. J Am Heart Assoc. 2016;5:e002667 DOI: 10.1161/JAHA.115.002667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bahit MC, Lopes RD, Clare RM, Newby LK, Pieper KS, Van de Werf F, Armstrong PW, Mahaffey KW, Harrington RA, Diaz R, Ohman EM, White HD, James S, Granger CB. Heart failure complicating non‐ST‐segment elevation acute coronary syndrome: timing, predictors, and clinical outcomes. JACC Heart Fail. 2013;1:223–229. [DOI] [PubMed] [Google Scholar]
- 23. Lewis EF, Velazquez EJ, Solomon SD, Hellkamp AS, McMurray JJ, Mathias J, Rouleau JL, Maggioni AP, Swedberg K, Kober L, White H, Dalby AJ, Francis GS, Zannad F, Califf RM, Pfeffer MA. Predictors of the first heart failure hospitalization in patients who are stable survivors of myocardial infarction complicated by pulmonary congestion and/or left ventricular dysfunction: a VALIANT study. Eur Heart J. 2008;29:748–756. [DOI] [PubMed] [Google Scholar]
- 24. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 25. Langorgen J, Ebbing M, Igland J, Nordrehaug JE, Vollset SE, Kask A, Tell GS, Nygard O. The universal 2012 definition of myocardial infarction compared to the 2007 definition. Scand Cardiovasc J. 2016;50:201–205. [DOI] [PubMed] [Google Scholar]
- 26. Sulo G, Igland J, Vollset SE, Nygard O, Egeland GM, Ebbing M, Sulo E, Tell GS. Effect of the lookback period's length used to identify incident acute myocardial infarction on the observed trends on incidence rates and survival: Cardiovascular Disease in Norway Project. Circ Cardiovasc Qual Outcomes. 2015;8:376–382. [DOI] [PubMed] [Google Scholar]
- 27. Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM. Decline in rates of death and heart failure in acute coronary syndromes, 1999–2006. JAMA. 2007;297:1892–1900. [DOI] [PubMed] [Google Scholar]
- 28. McManus DD, Chinali M, Saczynski JS, Gore JM, Yarzebski J, Spencer FA, Lessard D, Goldberg RJ. 30‐year trends in heart failure in patients hospitalized with acute myocardial infarction. Am J Cardiol. 2011;107:353–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Desta L, Jernberg T, Lofman I, Hofman‐Bang C, Hagerman I, Spaak J, Persson H. Incidence, temporal trends, and prognostic impact of heart failure complicating acute myocardial infarction. The SWEDEHEART Registry (Swedish Web‐System for Enhancement and Development of Evidence‐Based Care in Heart Disease Evaluated According to Recommended Therapies): a study of 199,851 patients admitted with index acute myocardial infarctions, 1996 to 2008. JACC Heart Fail. 2015;3:234–242. [DOI] [PubMed] [Google Scholar]
- 30. Bursi F, Weston SA, Redfield MM, Jacobsen SJ, Pakhomov S, Nkomo VT, Meverden RA, Roger VL. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–2216. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Changes Over Time in the Excess Mortality Associated With In‐Hospital HF (Heart Failure)
Table S2. Length of Hospitalization for the Incident Acute Myocardial Infarction
Table S3. Changes Over Time in the Excess 1‐Year Mortality Associated With Postdischarge Heart Failure
Table S4. Changes Over Time in the Odds of Receiving Myocardial Revascularization Between Patients With and Without Early‐Onset Heart Failure: A CVDNOR Project


