Abstract
Background
Up to one fifth of readmissions after a heart failure hospitalization occur at a different hospital. This negatively impacts information continuity, but whether site of readmission impacts subsequent outcomes is unclear.
Methods and Results
Retrospective cohort study of all patients discharged with a primary diagnosis of heart failure in Canada between April 2004 and December 2013. We compared patients readmitted within 30 days to the original hospital versus a different hospital. Of the 217 039 heart failure patients (mean age, 76.8 years, 50.1% male), 39 368 (18.1%) were readmitted within 30 days—32 771 (83.2%) to the original hospital and 6597 (16.8%) to a different hospital (increasing over time from 15.6% in 2004 to 18.5% by 2013; P for trend=0.001). Patients readmitted to different hospitals were younger and were more likely to be male, have a rural residence, a more‐recent discharge year, an index hospitalization at a teaching hospital, and to be brought in by ambulance at the time of the readmission. Readmissions to the original hospital were substantially shorter (mean, 10.4 days [95% CI, 10.3–10.6] versus 11.6 days [95% CI, 11.3–12.0]; adjusted means, 11.0 versus 12.0; P<0.0001) and had lower mortality (14.4% versus 15.0%; adjusted odds ratio, 0.89; 95% CI, 0.82–0.96) than readmissions to different hospitals.
Conclusions
Readmissions to a different hospital are becoming more frequent over time and are associated with longer stays and higher mortality rates than readmissions to the original hospital. Our findings provide further evidence that care fragmentation may be deleterious for patients with heart failure.
Keywords: heart failure, outcomes research, readmissions
Subject Categories: Heart Failure, Epidemiology, Health Services
Introduction
Heart Failure (HF) is one of the most common reasons for hospitalization in North America,1 and the risks of hospitalization and readmission are continuing to increase.2, 3 Although most patients are readmitted to the hospital they were originally discharged from, approximately one fifth are readmitted to a different hospital.4, 5, 6, 7, 8 Because most hospitals do not share inpatient data (such as admission and progress notes, diagnostic test results, and in‐hospital therapies or interventions) with one another9 and given the well‐known deficiencies in discharge summary completeness and promptness,10 readmission to a different hospital negatively impacts information continuity.
Whether site of readmission impacts subsequent outcomes is unclear. Whereas 1 study4 suggested that 30‐day readmissions to a different hospital were associated with higher mortality, another5 did not find any difference in mortality rates for those readmitted to the original versus a different hospital. However, both studies evaluated patients discharged after hospitalization for any reason—large proportions of which were surgical hospitalizations—and it is already known that surgical patients demonstrate markedly poorer outcomes when readmitted to a different hospital.7 Thus, the influence of readmission site for patients with HF as the primary diagnosis for their index hospitalization is unknown. Although this is an important policy question with implications for clinicians, patients, ambulance referral practices, and hospital funding models, it has not been addressed in a randomized trial. Thus, we designed a population‐based cohort study to test whether site of hospital readmission influenced subsequent length of stay or in‐patient mortality for patients with a primary diagnosis of HF.
Methods
Setting
Canada has a system of universal health insurance that provides access to medical care at no direct cost to the patient, and all acute care hospitals in Canada submit information to the Discharge Abstract Database held by the Canadian Institute for Health Information.
Study Sample
We used the Discharge Abstract Database in 9 Canadian provinces and 3 territories to examine all acute care hospitalizations with a primary diagnosis of HF using International Classification of Diseases, Tenth Revision code I50.x (93% positive predictive value for HF when validated against chart audit)11 between April 1, 2004 and December 31, 2013. The Discharge Abstract Database includes the admission and discharge dates, acuity (elective versus urgent/emergent), the primary diagnosis assigned by the attending physician, and up to 24 other diagnoses coded by trained nosologists in each hospital using nationally standardized definitions.
Hospitalizations that overlapped within 24 hours were combined into 1 episode of care (which was the unit of analysis), and the index hospital was defined as the last hospital in the episode of care cascade that had HF as the primary diagnosis. Length of stay (LOS) was summed across all hospitals for each episode of care. For patients with multiple HF episodes during the study time period, we selected their first hospitalization as the index.
In the primary analysis, we analyzed a cohort of adult patients discharged alive after a typical hospitalization for HF; thus, we excluded patients who were younger than 20 years old, died during the index hospitalization, were hospitalized for longer than 30 days, or signed themselves out against medical advice. We identified any nonelective readmissions for any cause between 1 and 30 days after discharge (as mentioned previously, we excluded readmissions within 24 hours of discharge to avoid misattributing transfers between hospitals and instead combined these with the initial hospitalization into a single episode of care). For patients with multiple readmissions within 30 days of the index hospitalization, we used the first readmission for analysis.
Covariates
Comorbidities for each patient were identified using International Classification of Diseases, Tenth Revision codes from the Discharge Abstract Database for the index hospitalization and any hospitalizations in the previous 12 months.12 Other covariates included type of hospital (teaching, large community, medium community, and small community), patient residence (rural versus urban), number of hospitalizations in the past 6 months, day of discharge (given that this is known to influence readmission rates),13 and specialty of most responsible physician during the index hospitalization (cardiologist, other internal medicine, family physician, or other).
Outcomes
Our primary outcomes of interest were LOS and in‐hospital mortality for HF patients readmitted for any cause within 30 days to the original versus a different hospital. In a sensitivity analysis, we examined these outcomes in only those patients readmitted for HF to the original versus a different hospital.
Statistical Analyses
Ages and patient comorbidities were compared using t tests or chi‐squared tests between those patients who were/were not readmitted within 30 days and between those who were readmitted to the original versus a different hospital. We identified which factors were associated with different versus original hospital readmission using multivariable logistic regression adjusting for age, sex, Charlson score, number of hospitalizations in past 6 months, acuity of admission, type of most responsible physician during index hospitalization, discharge disposition after index hospitalization, day of discharge from index hospitalization, type of hospital for index hospitalization, rural residence for the patient, day of readmission (weekday versus weekend/holiday), arrival by ambulance to readmission hospital, year of index hospitalization, and 2 random intercepts to account for clustering effects of province and of hospital. A similar logistic regression model including the same covariates was used to obtain an adjusted odds ratio comparing in‐hospital mortality between patients who were readmitted to the original versus a different hospital. To compare the readmission LOS between patients readmitted to the original versus a different hospital, a generalized linear mixed model was used to obtain adjusted length of stay by least squares means and adjusting for age, sex, rural residence, Charlson score, type of hospital, type of most responsible physician during index hospitalization, discharge disposition after index hospitalization, day of readmission, arrival by ambulance to readmission hospital, and 2 random intercepts (thus the mixed model) to account for clustering effects of province and hospital. A model using log‐transformed LOS was also examined, but did not appreciably alter the results. SAS software (version 9.4; SAS Institute Inc, Cary, NC) was used for all statistical analysis. The University of Alberta Health Research Ethics Board approved this study with waiver of informed consent because we were using de‐identified data.
Results
Of the 217 039 patients (mean age, 76.8 years; 50.1% male) discharged alive after an acute care hospitalization for HF (Figure), 39 368 (18.1%) were readmitted within 30 days—32 771 (83.2%) to the original hospital and 6597 (16.8%) to a different hospital. There was a statistically significant increase in the proportion being readmitted to a different hospital over time: from 15.6% in 2004 to 18.5% in 2013 (P for trend=0.001). Patients were more likely to be readmitted to the original hospital if they were older, female, lived in an urban setting, had shorter LOS during the index hospitalization, had lower comorbidity burdens, were treated in a community hospital, and if their attending physician during the index hospitalization had been a primary care physician (Table 1)—however, many of these differences disappeared on multivariate analysis. The factors independently associated with being readmitted to a different hospital (after adjusting for Charlson scores and the other factors in Table 1) were male sex, younger age, rural residence, more‐recent discharge year, long‐term care facility resident, index hospitalization was at a teaching hospital, and being brought in by ambulance for the readmission; patients cared for by family physicians were less likely to be readmitted to a different hospital (Table 2).
Figure 1.
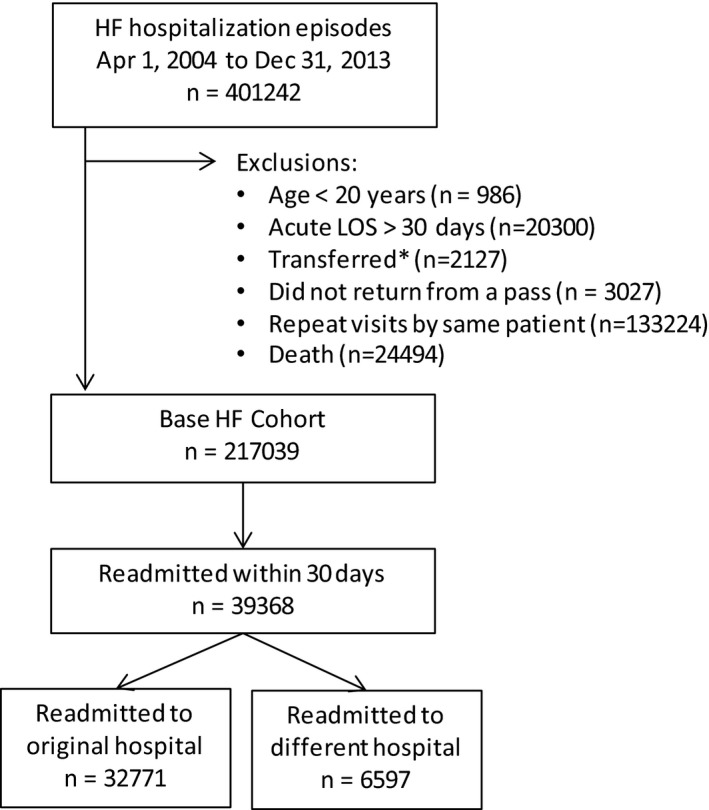
Cohort derivation. *Transferred to inpatient facility as final discharge disposition, but no subsequent hospitalization within 24 hours. HF indicates heart failure; LOS, length of stay.
Table 1.
Patient Characteristics at the Time of the Index Hospitalization With a Primary Diagnosis of HF
| Characteristic | Not Readmitted Within 30 Days n=177 671 | Readmitted Within 30 Days n=39 368 | P Value | Readmitted Within 30 Days to Original Hospital n=32 771 | Readmitted Within 30 Days to Different Hospital n=6597 | P Value |
|---|---|---|---|---|---|---|
| Age at time of index hospitalization | 76.6 (12.3) | 77.6 (11.5) | <0.0001 | 78.1 (11.3) | 75.1 (12.5) | <0.0001 |
| Male | 88 770 (50.0) | 19 954 (50.7) | 0.10 | 16 361 (49.9) | 3593 (54.5) | <0.0001 |
| Rural resident | 37 362 (21.1) | 8680 (22.1) | <0.0001 | 6886 (21.0) | 1794 (27.2) | <0.0001 |
| Admitted on a nonholiday weekdaya | 130 084 (73.2) | 28 450 (72.3) | 0.0001 | 23 630 (72.1) | 4764 (72.2) | 0.86 |
| Arrived by ambulancea | 75 798 (42.7) | 18 079 (45.9) | <0.0001 | 17 338 (52.9) | 3595 (54.5) | 0.02 |
| Resided in long‐term care facility before index hospitalization | 15 672 (8.8) | 3583 (9.1) | 0.08 | 3136 (9.6) | 447 (6.8) | <0.0001 |
| Charlson comorbidity index score | 4.0 (2.1) | 4.5 (2.3) | <0.0001 | 4.5 (2.3) | 4.6 (2.3) | <0.0001 |
| Hospitalizations during previous 6 months | 0.3 (0.7) | 0.5 (0.9) | <0.0001 | 0.5 (0.9) | 0.5 (0.9) | 0.10 |
| Acute length of stay for index hospitalization | 7.7 (5.9) | 8.2 (6.2) | <0.0001 | 8.0 (6.0) | 8.9 (6.8) | <0.0001 |
| LACE score | 11.4 (2.5) | 11.9 (2.5) | <0.0001 | 11.8 (2.5) | 12.0 (2.6) | <0.0001 |
| Discharged on weekend/holiday | 27 633 (15.6) | 6247 (15.9) | 0.12 | 5229 (16.0) | 1018 (15.4) | 0.29 |
| Discharge disposition | <0.0001 | <0.0001 | ||||
| Home | 121 425 (68.3) | 25 587 (65.0) | 21 116 (64.4) | 4471 (67.8) | ||
| Home with homecare | 34 046 (19.2) | 9775 (24.8) | 8352 (25.5) | 1423 (21.6) | ||
| Long‐term care/skilled nursing facility | 22 200 (12.5) | 4006 (10.2) | 3303 (10.1) | 703 (10.7) | ||
| Past history of heart failure in the 1 year before index | 28 744 (16.2) | 9333 (23.7) | <0.0001 | 7853 (24.0) | 1480 (22.4) | 0.008 |
| Hypertension | 73 199 (41.2) | 16 705 (42.4) | <0.0001 | 13 581 (41.4) | 3124 (47.4) | <0.0001 |
| Diabetes mellitus | 63 276 (35.6) | 15 319 (38.9) | <0.0001 | 12 692 (38.7) | 2627 (39.8) | 0.10 |
| Ishemic heart disease, including past MI, CABG, or PCI/stent | 64 634 (36.4) | 16 191 (41.1) | <0.0001 | 13 223 (40.3) | 2968 (45.0) | <0.0001 |
| Peripheral arterial disease | 1203 (0.7) | 357 (0.9) | <0.0001 | 284 (0.9) | 73 (1.1) | 0.06 |
| Cerebrovascular disease (previous stroke/TIA) | 3265 (1.8) | 854 (2.2) | <0.0001 | 689 (2.1) | 165 (2.5) | 0.04 |
| Atrial fibrillation/flutter | 61 682 (34.7) | 14 111 (35.8) | <0.0001 | 11 719 (35.8) | 2392 (36.3) | 0.44 |
| Ventricular arrythmias | 3593 (2.0) | 916 (2.3) | 0.0001 | 726 (2.2) | 190 (2.9) | 0.0011 |
| Chronic kidney disease | 37 805 (21.3) | 11 224 (28.5) | <0.0001 | 9176 (28.0) | 2048 (31.0) | <0.0001 |
| Cancer | 7028 (4.0) | 2267 (5.8) | <0.0001 | 1858 (5.7) | 409 (6.2) | 0.09 |
| COPD or asthma | 35 721 (20.1) | 9421 (23.9) | <0.0001 | 7902 (24.1) | 1519 (23.0) | 0.06 |
| Peptic ulcer disease | 1650 (0.9) | 480 (1.2) | <0.0001 | 376 (1.1) | 104 (1.6) | 0.004 |
| Liver disease | 2145 (1.2) | 639 (1.6) | <0.0001 | 516 (1.6) | 123 (1.9) | 0.09 |
| Dementia | 9621 (5.4) | 2106 (5.3) | 0.60 | 1764 (5.4) | 342 (5.2) | 0.51 |
| Index hospital characteristics | <0.0001 | <0.0001 | ||||
| Teaching hospital | 41 136 (23.3) | 8815 (22.5) | 6675 (20.5) | 2140 (32.7) | ||
| Large community hospital | 78 424 (44.4) | 16 837 (43.0) | 14 278 (43.8) | 2559 (39.0) | ||
| Medium community hospital | 34 604 (19.6) | 7671 (19.6) | 6730 (20.6) | 941 (14.4) | ||
| Small community hospital | 22 618 (12.8) | 5824 (14.9) | 4910 (15.1) | 914 (13.9) | ||
| Most responsible physician during index hospitalization | <0.0001 | <0.0001 | ||||
| Cardiologist | 30 880 (17.4) | 5717 (14.5) | 4252 (13.0) | 1465 (22.2) | ||
| Internal medicine other than cardiology | 50 576 (28.5) | 11 404 (29.0) | 9119 (27.8) | 2285 (34.6) | ||
| Family physician | 85 386 (48.1) | 19 778 (50.2) | 17 393 (53.1) | 2385 (36.2) | ||
| Other | 10 829 (6.1) | 2469 (6.3) | 2007 (6.1) | 462 (7.0) |
Data are presented as means (SD) or n (%). P values calculated using t test (means) or chi‐square test (binary/categorical). Missing values: 337 (0.16%) for rural residence status; 1110 (0.51%) for hospital type. LACE score=index to identify risk for readmission or death, L stands for length of stay, A stands for acuity of admission, C stands for Charlson commorbidity score, and E stands for number of emergency department visits in the past 6 months. CABG indicates coronary artery bypass grafting; COPD, chronic obstructive pulmonary disease; MI, myocardial infarction; PCI, percutaneous coronary intervention; TIA, transient ischemic attack.
Refers to the index hospitalization for the first 2 columns and the readmission hospitalization for the last 2 columns.
Table 2.
Factors Associated With Readmission to a Hospital Different Than the Index Hospital
| Variable | Univariate Odds Ratio (95% CI) | Adjusted Odds Ratio (95% CI) |
|---|---|---|
| Age (per 1 year increase) | 0.98 (0.98, 0.98) | 0.98 (0.98, 0.98) |
| Male | 1.20 (1.14, 1.27) | 1.10 (1.04, 1.16) |
| Rural residence | 2.42 (2.23, 2.63) | 2.43 (2.23, 2.65) |
| Charlson Score (per 1‐unit increase) | 1.01 (1.00, 1.03) | 1.00 (0.99, 1.01) |
| Number of hospitalizations in previous 6 months (per 1‐unit increase) | 1.03 (1.00, 1.07) | 1.02 (0.99, 1.05) |
| Urgent index admission (vs elective) | 0.55 (0.45, 0.68) | 0.61 (0.50, 0.75) |
| Family physician as most responsible during index | 0.55 (0.50, 0.59) | 0.61 (0.55, 0.66) |
| Index discharge on weekend/holiday | 0.97 (0.90, 1.04) | 0.94 (0.87, 1.02) |
| Year of index discharge (per 1‐year increase) | 1.01 (1.00, 1.02) | 1.02 (1.01, 1.03) |
| Discharge disposition | ||
| Home (ref) | 1 (ref) | 1 (ref) |
| Home with homecare | 0.77 (0.71, 0.82) | 0.89 (0.82, 0.95) |
| Long term care/skilled nursing facility | 0.95 (0.87, 1.05) | 1.17 (1.06, 1.28) |
| Index hospital type | ||
| Teaching (ref) | 1 (ref) | 1 (ref) |
| Large community | 0.63 (0.52, 0.77) | 0.74 (0.60, 0.92) |
| Medium community | 0.52 (0.42, 0.65) | 0.58 (0.46, 0.74) |
| Small community | 0.66 (0.54, 0.81) | 0.59 (0.46, 0.75) |
| Readmission on weekend/holiday | 1.02 (0.96, 1.08) | 1.02 (0.96, 1.09) |
| Arrived by ambulance to readmission hospital | 1.07 (1.01, 1.13) | 1.22 (1.15, 1.29) |
Adjusted odds ratios obtained from model including all variables listed in table. Response variable=readmission to NON‐Index hospital (vs readmission to same hospital as index admission). Eg, odds ratio >1 implies positive association with readmission to different hospital (compared to readmission to same hospital).
The top 5 causes for readmission in this cohort of patients were HF (n=14 535; 36.9%), chronic obstructive pulmonary disease (n=1945; 4.9%), acute myocardial infarction (n=1332; 3.4%), pneumonia (n=1133; 2.9%), and atrial fibrillation or flutter (n=940; 2.4%).
Whereas readmitted patients exhibited longer LOS during the readmission than during their index hospitalization (mean, 8.2 days; 95% CI, 8.1–8.2), those readmitted to the original hospital demonstrated substantially shorter LOS for the readmission (mean, 10.4 days; 95% CI, 10.3–10.6; adjusted mean, 11.0; 95% CI, 10.1–12.0) than those readmitted to different hospitals (mean, 11.6 days; 95% CI, 11.3–12.0; adjusted mean, 12.0; 95% CI, 11.1–13.0; P<0.0001). Patients readmitted to the original hospital also demonstrated lower mortality rates during the readmission (14.4% versus 15.0% for those readmitted to a different hospital; adjusted odds ratio, 0.89; 95% CI, 0.82–0.96). Of note, perusal of our exclusion criteria (Figure) reveals that mortality during the index hospitalization was 6.1%.
Our sensitivity analysis restricted to patients readmitted for HF as the primary diagnosis found similar patterns in terms of factors associated with readmission to the original hospital versus a different hospital and worse outcomes for readmissions than index hospitalizations.
Discussion
We found that readmission to a different hospital was common for patients with HF, was becoming more frequent over time, and was associated with longer LOS and higher inpatient mortality rates than readmissions to the original hospital. Although we could not examine resource use in our data set, a recent Medicare study found that patient readmissions to different hospitals generated higher costs because of more diagnostic testing and procedures than readmissions to the original hospital.5 Although it is already known1 that readmissions are associated with longer LOS and poorer outcomes than the original hospitalization, our study adds to the literature base by demonstrating that readmissions to different hospitals have even worse outcomes than readmissions to the original hospital. Our study also helps clarify the conflicting results from 2 previous studies of this phenomenon: 14 demonstrated higher mortality rates with different hospital readmissions whereas the other5 did not. Furthermore, as mentioned in the Introduction, both previous studies evaluated a broad mix of patients discharged after hospitalization for a wide variety of medical or surgical diagnoses, and neither examined LOS during the readmission.
We cannot say definitively why alternate hospital readmissions have poorer outcomes because this is an observational study. However, we theorize that fragmentation of care plays a role. Previous studies14, 15 have shown better outcomes for HF patients cared for by physicians familiar with them after hospital discharges or emergency department visits. Other studies have also demonstrated that continuity of physician care reduces hospitalizations, especially for patients with high comorbidity burdens.16 Thus, it seems reasonable to hypothesize that continuity of inpatient care would be associated with improved outcomes—however, we acknowledge that this is a hypothesis that requires testing in a prospective, controlled study.
Although it is possible that our results are a manifestation of residual confounding, it is worth noting that patients readmitted to a different hospital were not only younger and less likely to have been urgently admitted during the index hospitalization (suggesting that they were perhaps less sick), but they were also more likely to have been treated by a specialist or in an academic teaching hospital during their preceding index event—all factors shown to be associated with better subsequent outcomes.13 This would suggest that any residual confounding may, in fact, have biased toward the null in our study by improving outcomes in the “different hospital readmission” group. Regardless, without information on the factors motivating alternate hospital readmissions, we cannot comment on the potential modifiability of this practice. However, given the poorer prognosis associated with alternate hospital readmission, our data suggest that clinicians should counsel patients on the potential benefits of returning to their original hospital if they deteriorate. In the same vein, we believe that our findings should prompt policy makers to revisit current ambulance policies which focus on shortening wait times in emergency rooms by diverting ambulances to the least busy emergency room regardless of where they had been most recently discharged from. In fact, given that delaying care so that one can be cared for by familiar providers may have harms as well as benefits, we believe a controlled trial comparing sending patients back to the original hospital versus to the closest facility should be conducted. Our findings also have implications for hospital performance measures and funding models based on readmission rates given the substantial proportion of patients readmitted to hospitals other than the one they were discharged from. Finally, our results should motivate attempts to improve the sharing of patient information between hospitals—one of the many hopes for electronic medical records.
Despite reporting outcomes in all adults (ie, not just elderly patients) hospitalized for HF in 9 provinces and 3 territories of Canada (a country with free universal access to acute care hospitals), robust data permitting adjustment for comorbidities as well as health resource use, and a large sample, there are some limitations to our analysis. First, we relied on administrative data to define HF and comorbidities and do not have information on ejection fraction, natriuretic peptide levels, nor clinical findings that would permit delineation of illness severity. Although we acknowledge this weakness, we used validated International Classification of Diseases codes and data definition algorithms11, 12 to build comorbidity profiles and the outcomes we evaluated (all‐cause rehospitalizations, LOS, and in‐hospital mortality) are relevant in HF patients regardless of ejection fraction, etiology, or clinical status. Second, although outpatient visits, particularly with familiar physicians14, 15, 16 or access to specialized clinics17 after discharge, would reduce readmissions, we do not have any data on whether availability of these outpatient resources varied over time or whether outpatient physician visits were or were not with physicians associated with the original hospital. Third, we had no data on distance from patient home to nearest hospital nor socioeconomic factors, such as homelessness or access to motor vehicle, that may have influenced both health outcomes and choice of hospital. Fourth, we had no data on completeness, promptness, or dissemination of discharge summaries after the index hospitalization, although previous studies suggest that these are low within a 30‐day time frame.18 Finally, although we focused on 30‐day readmissions, a study in 1 Canadian province suggested that mortality differences observed at 30 days persisted across a full year of follow‐up.4
In conclusion, our finding that readmissions to hospitals other than the original one are associated with poorer outcomes for patients with HF reinforces concerns that such readmissions may not only result in duplication of tests and procedures5 and lead to exposure to potentially different nosocomial pathogens,4 but also may delay timely diagnoses or treatments. We believe our study provides further support for the importance of continuity in health care and should motive patients, caregivers, and their physicians to ensure follow‐up after discharge occurs with healthcare providers who are familiar with them. Our study should also motivate health system planners to conduct evaluations of “return to original hospital” versus “take to the closest facility” ambulance policies for HF patients who deteriorate post‐discharge.
Sources of Funding
Dr McAlister receives salary support from Alberta Innovates Health Solution (AIHS) and holds the University of Alberta Chair in Cardiovascular Outcomes Research.
Disclosures
All authors declare that they have no financial interests that may be relevant to the submitted work. Dr McAlister is guarantor of this work.
(J Am Heart Assoc. 2017;6:e004892 DOI: 10.1161/JAHA.116.004892.)28490524
References
- 1. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360:1418–1428. [DOI] [PubMed] [Google Scholar]
- 2. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:143–152. [DOI] [PubMed] [Google Scholar]
- 3. Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand SL, Curtis JP, Drye EE, Lichtman JH, Keenan PS, Kosiborod M, Krumholz HM. Trends in length of stay and short‐term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010;303:2141–2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Staples JA, Thiruchelvam D, Redelmeier DA. Site of hospital readmission and mortality: a population‐based retrospective cohort study. CMAJ Open. 2014;2:E77–E85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kind AJM, Bartels C, Mell MW, Mullahy J, Smith M. For‐profit hospital status and rehospitalizations at different hospitals: an analysis of Medicare data. Ann Intern Med. 2010;153:718–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hempstead K, DeLia D, Cantor JC, Nguyen T, Brenner J. The fragmentation of hospital use among a cohort of high utilizers. Implications for emerging care coordination strategies for patients with multiple chronic conditions. Med Care. 2014;52:S67–S74. [DOI] [PubMed] [Google Scholar]
- 7. Tsai TC, Orav EJ, Jha AK. Care fragmentation in the postdischarge period. Surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg. 2015;150:59–64. [DOI] [PubMed] [Google Scholar]
- 8. Bourgeois FC, Olson KL, Mandl KD. Patients treated at multiple acute health care facilities. Quantifying information fragmentation. Arch Intern Med. 2010;170:1989–1995. [DOI] [PubMed] [Google Scholar]
- 9. Adler‐Milstein J, DesRoches CM, Jha AK. Health information exchange among US hospitals. Am J Manag Care. 2011;17:761–768. [PubMed] [Google Scholar]
- 10. Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital‐based and primary care physicians. JAMA. 2007;297:831–841. [DOI] [PubMed] [Google Scholar]
- 11. Quan H, Li B, Saunders LD, Parsons GA, Nilsson CI, Alibhai A, Ghali WA; for the IMECCHI Investigators . Assessing validity of ICD‐9‐CM and ICD‐10 administrative data in recording clinical conditions in a unique dually coded database. Health Serv Res. 2008;43:1424–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lee DS, Donovan L, Austin PC, Gong Y, Liu PP, Rouleau JL, Tu JV. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcomes research. Med Care. 2005;43:182–188. [DOI] [PubMed] [Google Scholar]
- 13. McAlister FA, Au A, Majumdar SR, Youngson E, Padwal RS. Postdischarge outcomes in heart failure are better for teaching hospitals and weekday discharges. Circ Heart Fail. 2013;6:922–929. [DOI] [PubMed] [Google Scholar]
- 14. McAlister FA, Youngson E, Bakal JA, Kaul P, Ezekowitz J, van Walraven C. Impact of physician continuity on death or urgent readmission after discharge among patients with heart failure. CMAJ. 2013;185:e681–e689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sidhu R, Youngson E, McAlister FA. Physician continuity improves outcomes for heart failure patients treated and released from the emergency department. JACC Heart Fail. 2014;2:368–376. [DOI] [PubMed] [Google Scholar]
- 16. Gruneir A, Bronskill SE, Maxwell CJ, Bai YQ, Kone AJ, Thavorn K, Petrosyan Y, Calzavara A, Wodchis WP. The association between multimorbidity and hospitalization is modified by individual demographics and physician continuity of care: a retrospective cohort study. BMC Health Serv Res. 2016;16:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McAlister FA, Stewart S, Ferrua S, McMurray JJV. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44:810–819. [DOI] [PubMed] [Google Scholar]
- 18. van Walraven C, Taljaard M, Bell CM, Etchells E, Stiell IG, Zarnke K, Forster AJ. A prospective cohort study found that provider and information continuity was low after patient discharge from hospital. J Clin Epidemiol. 2010;63:1000–1010. [DOI] [PubMed] [Google Scholar]


