Abstract
Background
Bystander cardiopulmonary resuscitation (CPR) is associated with increased survival from cardiac arrest, yet bystander CPR rates are low in many communities. The overall prevalence of CPR training in the United States and associated individual‐level disparities are unknown. We sought to measure the national prevalence of CPR training and hypothesized that older age and lower socioeconomic status would be independently associated with a lower likelihood of CPR training.
Methods and Results
We administered a cross‐sectional telephone survey to a nationally representative adult sample. We assessed the demographics of individuals trained in CPR within 2 years (currently trained) and those who had been trained in CPR at some point in time (ever trained). The association of CPR training and demographic variables were tested using survey weighted logistic regression. Between September 2015 and November 2015, 9022 individuals completed the survey; 18% reported being currently trained in CPR, and 65% reported training at some point previously. For each year of increased age, the likelihood of being currently CPR trained or ever trained decreased (currently trained: odds ratio, 0.98; 95% CI, 0.97–0.99; P<0.01; ever trained: OR, 0.99; 95% CI, 0.98–0.99; P=0.04). Furthermore, there was a greater then 4‐fold difference in odds of being currently CPR trained from the 30–39 to 70–79 year old age groups (95% CI, 0.10–0.23). Factors associated with a lower likelihood of CPR training were lesser educational attainment and lower household income (P<0.01 for each of these variables).
Conclusions
A minority of respondents reported current training in CPR. Older age, lesser education, and lower income were associated with reduced likelihood of CPR training. These findings illustrate important gaps in US CPR education and suggest the need to develop tailored CPR training efforts to address this variability.
Keywords: cardiopulmonary resuscitation, education, education surveillance, educational campaigns, sudden cardiac arrest
Subject Categories: Cardiopulmonary Resuscitation and Emergency Cardiac Care
Clinical Perpective
What is New?
In a cross‐sectional, nationally representative survey completed by 9022 adults, 18% reported being currently trained in CPR, whereas older age was associated with a lower likelihood of CPR training.
Furthermore, higher socioeconomic status was associated with a higher probability of CPR education.
What are the Clinical Implications?
These findings highlight important disparities in CPR education across the United States and suggest the need to develop future targeted bystander CFR training efforts tailored to specific populations.
Introduction
The prompt delivery of bystander cardiopulmonary resuscitation (B‐CPR) increases the probability of survival from sudden cardiac arrest (SCA) by over 2‐fold, yet less than one third of SCA victims receive B‐CPR in the United States.1, 2, 3, 4, 5 Recent work has demonstrated an association between increased public CPR training and B‐CPR delivery.3, 6, 7 Despite growing efforts to promote CPR education of the public, little is known regarding the national prevalence of CPR training or the association of training status with individual‐level demographic characteristics.
A recent investigation sought to quantify national CPR training activity by measuring the distribution of CPR certification cards and found that 2.4% of the adult US population received CPR education within a 1‐year period through certification programs.8 Although this study provided an initial estimate of CPR training incidence, there were important limitations to the investigation, including the lack of individual‐level trainee demographic data and the prevalence of previous training. Understanding demographic associations with training prevalence could aid with targeted CPR training initiatives to maximize CPR education efforts.
We implemented a telephone‐based, prospective, nationally representative survey to determine CPR training prevalence and its relationship with demographic variables and previous training experiences. We hypothesized that increased age and lower socioeconomic status (SES), independently, would be associated with a lower likelihood of CPR training.
Methods
Study Design and Population
This cross‐sectional investigation was designed to estimate the association between individual‐level demographic variation and CPR training status. From September 2015 to November 2015, survey data were collected by random digit dial telephone methodology in collaboration with an established social sciences research organization (SSRS, Media, PA). Participants were queried as part of an ongoing omnibus survey, through both landline and mobile telephone modalities. Results from the omnibus survey have been used in previous peer‐reviewed biomedical investigations.9, 10, 11
Individuals in the United States ages 18 and older were eligible to be survey respondents. After determining eligibility, participants were given a series of questions designed to assess individual‐level demographic characteristics and CPR training status. The study protocol was deemed exempt by the University of Pennsylvania Institutional Review Board (Philadelphia, PA).
Survey Questionnaire Development
Questions were developed and extensively pilot tested among adult laypersons by study personnel (A.L.B., M.L., B.S.A.). The wording was designed to capture an individual's training status (Table S1). Once finalized, the questions were introduced on a regional health survey in southeastern Pennsylvania. Responses from this regional survey were used to establish CPR training content and construct validity. Data from this regional survey in Pennsylvania have been presented elsewhere.12
Demographic data, such as age, race, education, and income, were measured using the survey research company's validated demographic questionnaire.
Survey Methodology
The survey approach was designed to represent the adult US population by a stratified random digit dial sample of landline residential as well as mobile telephone numbers. Telephone numbers were computer generated and loaded into online sample files accessed directly by the computer‐assisted telephone interviewing system by well‐established survey methods.9, 11 Area code‐specific quotas were also set to ensure adequate geographical representation, and interviews were conducted in either English or Spanish to ensure representation of the Spanish‐speaking population. Survey weights, accounting for selection bias and nonresponse bias by household, telephone, and key demographics such as age, race, sex, and education, were used to provide nationally representative estimates of the adult population 18 years of age and older (Data S1).
Variable Definitions
We defined an individual who is CPR trained as anyone who had reported receiving a CPR certification card, or was trained by a noncertification CPR educational program, similar to the methodology of Anderson et al.8 We queried individuals if they reported receiving CPR training within the past 2 years, 3 to 5 years, 6 to 10 years, or greater than 10 years. We defined those who were currently trained as anyone who reported receiving training in the past 2 years (compliant with current CPR certification standards) and defined those who were ever trained as anyone who reported receiving CPR training at any point in time (Table S1).
We captured respondent's age, race/ethnicity, sex, education, and income. Because SES is a multidimensional construct and not well defined by a single unit of measure, we used education and income variables to characterize SES, consistent with previous work.13, 14
Descriptive Comparison of Training and SCA Data
B‐CPR rates are lower in the private residential environment compared with the public setting.1 Spouses (generally of comparable ages) may be the first responders to SCA events in these environments. Age distribution from the CPR training survey was descriptively compared with that of SCA clinical events in a portion of the United States during a similar time period (2011–2015), using data from the Resucitation Outcomes Consortium (ROC). ROC is an NIH‐funded clinical trial network focused on prehospital SCA and severe traumatic injury. Since 2006, ROC has collected data from 10 municipal regions in the United States and Canada. ROC trials have been published previously, including more‐detailed descriptions of data collection elements and data registry infrastructure.1, 15, 16
Statistical Analysis
Data were analyzed using a statistical software package (STATA 14 with the svy suite of commands; StataCorp LP, College Station, TX). The data set was missing 17% of the covariates of interest; we analyzed differences in the covariates by missingness (Table S2) and assessed the final model using complete‐case analysis. As a sensitivity analysis, we used multiple imputation to impute the missing covariates of interest. The estimates from the imputed data sets were similar to the observed data set (data not shown). Given that there may be additional bias among those who are missing income, we compared those with missing income to those with nonmissing income values. These data were similar to those shown in Table S2 (data not shown).
Using survey weights, we estimated the national prevalence of CPR training and associated demographic differences with descriptive statistics. As a continuation of the investigation, using survey‐weighted logistic regression modeling, we analyzed whether there were differences between CPR training prevalence by age, education, and income. We explored this association with CPR training status using the data in a binary (yes/no CPR training) fashion and defined CPR training as currently trained (within previous 2 years) and ever trained (without time boundary). Age was examined continuously (increasing in years) and categorically (by age deciles). Individuals indicated their highest education level achieved and were either categorized as less than high school educated, high school graduate, some college, graduate of college, or graduate school or more. Total household income categories included less than $15 000, $15 000 to $29 999, $30 000 to $49 999, $50 000 to $74 999, $75 000 to $99 999, and $100 000 or more. The association of age, education, income, sex, race, and geographical division with CPR training was assessed in a univariate analysis with admission into the larger model based on a P value of less than 0.15. The final regression model included age, education, income, sex, and race. The geographical variable, division, was modeled and tested as a fixed effect in the final regression equation. We ran the prective margins of age, education, and income.
We examined the age distribution of SCA victims; we calculated the mean age and standard deviation. Further, we modelled the association of age and the likelihood of receiving B‐CPR delivery in a full analysis, and stratified by public and private environments. In the multivariate logistic regression model, we included site, age, race, sex, time of event, witness status, and emergency medical services response time.
Results
CPR Training Prevalence
From September 2015 to November 2015, 9022 individuals completed the survey, with data weighted to represent the adult US population (based on the US Census American Community Survey 2014, reflecting a US adult population [aged 18 years or older] of 245 201 07617); 4497 interviews were completed through mobile telephones and 4525 were completed by landlines. Of those eligible, 17% declined to conduct the survey, 29% halted participation partially through the interview process, and 44% of the phone calls went to voicemail or an answering machine, whereas 10% completed the entire interview (n=9022). Of those surveyed and weighted to represent the entire US adult population, 18% of respondants were currently trained in CPR, 65% were trained at some point previously (ever trained), and 35% had never been trained. Population characteristics are detailed in Table 1. The mean age of all the surveyed population was 48 (95% CI, 47–49) years, and 51% of the population were female. Of all participants, 65% were white, 12% were black, and 15% were Hispanic/Latino; 30% were high school graduates, and 15% had a household income of less then $15 000 a year.
Table 1.
Demographics of 9022 Participants Surveyed Weighted to be Representative of the US National Population 2015
| All Participants | Currently Trained | Ever Trained | Never Trained | |
|---|---|---|---|---|
| Mean age (95% CI), y | 48 (95% CI: 47–49) | 42 (95% CI: 41–43) | 48 (95% CI: 47–49) | 48 (95% CI: 46–51) |
| Race, % | ||||
| White | 65 | 65 | 71 | 55 |
| Black | 12 | 13 | 11 | 12 |
| Hispanic/Latino | 15 | 13 | 11 | 24 |
| Other | 8 | 9 | 7 | 9 |
| Sex, % | ||||
| Female | 51 | 56 | 52 | 50 |
| Male | 49 | 44 | 48 | 50 |
| Highest education, % | ||||
| Less than high school | 11 | 4 | 7 | 20 |
| High school graduate | 30 | 22 | 26 | 38 |
| Some college | 27 | 32 | 30 | 22 |
| Graduated college | 20 | 26 | 23 | 13 |
| Graduate school or more | 12 | 16 | 14 | 7 |
| Household income, % | ||||
| Less than $15 000 | 15 | 10 | 11 | 24 |
| $15 000 to $29 999 | 20 | 14 | 17 | 27 |
| $30 000 to $49 999 | 19 | 19 | 19 | 18 |
| $50 000 to $74 999 | 16 | 19 | 18 | 13 |
| $75 000 to $99 999 | 12 | 14 | 14 | 8 |
| $100 000 or more | 18 | 24 | 21 | 10 |
Survey sample n=9022, but weighted to estimate the US population. Missing variable: age‐447, race‐186, education‐53, income‐1625.
Demographic Characteristics Associated With Training
Of those who were currently trained, increased age was associated with a lower likelihood of being currently CPR trained (odds ratio for each year of increased age, 0.98; 95% CI, 0.97–0.99; P<0.01; Table 2). When age was examined categorically by increased decades (global P value, 0.04), those who were aged 70 to 79 years were 0.15 (95% CI, 0.10–0.23) times less likely to be being currently trained (P<0.01) and those aged 60 to 69 years old were 0.29 (95% CI, 0.20–0.42) times less likely to be currently trained compared with 18 to 29 year olds (P<0.01; Table 2; Figure 1). There were differences in education‐level and likelihood of current CPR training (P<0.02). Specifically, those who were graduate school educated or more had a 3.36 (95% CI, 1.60–7.09) increased likelihood of being currently CPR trained compared with those who had less than a high school education (P<0.01). Furthermore, there were differences in income level and likelihood of current CPR training (P=0.03; Figure 2). There was a significant difference in the global distribution of race and current CPR training (P=0.03), but the individual differences from whites, the reference group, were not significant. Sex was not associated with likelihood of current CPR training (P=nonsignificant; Table 2).
Table 2.
ORs (95% CI) of the Likelihood of Individuals Being Currently CPR Trained or Ever Trained by Individual Demographics n=6854
| Currently Trained | Global P Value | P Value | Ever Trained | Global P Value | P Value | |
|---|---|---|---|---|---|---|
| Age (95% CI), y | 0.04 | 0.04 | ||||
| 18 to 29 (reference) | ··· | ··· | ||||
| 30 to 39 | 0.75 (95% CI: 0.61–0.93) | 0.02 | 1.15 (95% CI: 1:01–1.30) | 0.04 | ||
| 40 to 49 | 0.63 (95% CI: 0.52–0.75) | <0.01 | 1.37 (95% CI: 1.10–1:70) | 0.01 | ||
| 50 to 59 | 0.56 (95% CI: 0.43–0.73) | <0.01 | 1.27 (95% CI: 1.05–1.54) | 0.02 | ||
| 60 to 69 | 0.29 (95% CI: 0.20–0.42) | <0.01 | 0.86 (95% CI: 0.71–1.05) | 0.12 | ||
| 70 to 79 | 0.15 (95% CI: 0.10–0.23) | <0.01 | 0.58 (95% CI: 0.43–0.77) | <0.01 | ||
| 80 and older | 0.05 (95% CI: 0.01–0.20) | <0.01 | 0.34 (95% CI: 0.22–0.52) | <0.01 | ||
| Race, OR (95% CI) | 0.03 | <0.01 | ||||
| White (reference) | ··· | ··· | ||||
| Black | 1.33 (95% CI: 0.84–2.10) | 0.19 | 0.92 (95% CI: 0.78–1.08) | 0.25 | ||
| Hispanic/Latino | 0.88 (95% CI: 0.67–1.14) | 0.29 | 0.44 (95% CI: 0.37–0.52) | <0.01 | ||
| Other | 1.16 (95% CI: 0.88–1.53) | 0.25 | 0.71 (95% CI: 0.52–0.95) | 0.03 | ||
| Female, OR (95% CI) | 1.34 (95% CI: 0.98–1.83) | 0.06 | 1.16 (95% CI: 0.93–1.43) | 0.16 | ||
| Highest education, % | 0.02 | <0.01 | ||||
| Less than high school (reference) | ··· | ··· | ||||
| High school graduate | 1.85 (95% CI: 1.35–2.54) | <0.01 | 1.63 (95% CI: 1.33–1.99) | <0.01 | ||
| Some college | 3.11 (95% CI: 1.89–5.10) | <0.01 | 2.72 (95% CI: 2.20–3.37) | <0.01 | ||
| Graduated college | 3.24 (95% CI: 1.96–5.36) | <0.01 | 2.98 (95% CI: 2.40–3.70) | <0.01 | ||
| Graduate school or more | 3.36 (95% CI: 1.60–7.09) | <0.01 | 3.29 (95% CI: 2.54–4.27) | <0.01 | ||
| Household income, % | 0.03 | <0.01 | ||||
| Less than $15 000 (reference) | ··· | ··· | ||||
| $15 000 to $29 999 | 0.94 (95% CI: 0.64–1.39) | 0.73 | 1.25 (95% CI: 0.99–1.57) | 0.06 | ||
| $30 000 to $49 999 | 1.36 (95% CI: 1.06–1.75) | 0.02 | 1.62 (95% CI: 1.34–1.95) | <0.01 | ||
| $50 000 to $74 999 | 1.55 (95% CI: 1.19–2.02) | 0.01 | 2.02 (95% CI: 1.62–2.53) | <0.01 | ||
| $75 000 to $99 999 | 1.72 (95% CI: 1.38–2.16) | <0.01 | 2.32 (95% CI: 1.49–3.59) | <0.01 | ||
| $100 000 or more | 1.88 (95% CI: 1.26–2.81) | <0.01 | 2.55 (95% CI: 1.67–3.88) | <0.01 |
Missing variables shown in Table 1. CPR indicates cardiopulmonary resuscitation; OR, odds ratios.
Figure 1.
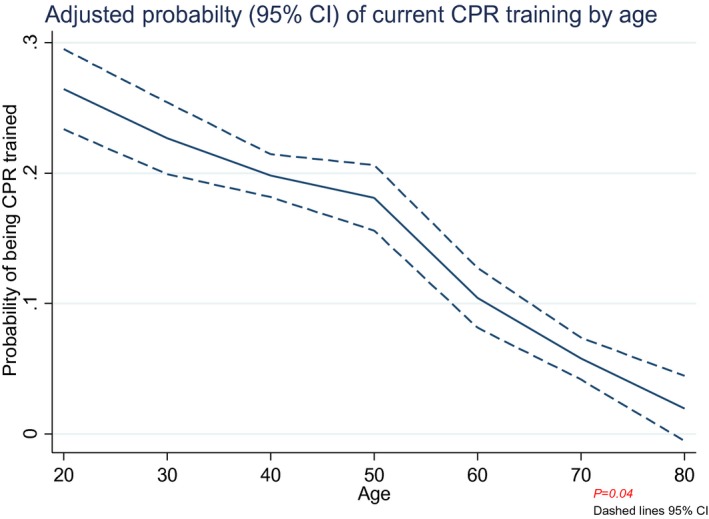
Adjusted probability of current CPR training by age with 95% CIs. CPR indicates cardiopulmonary resuscitation.
Figure 2.
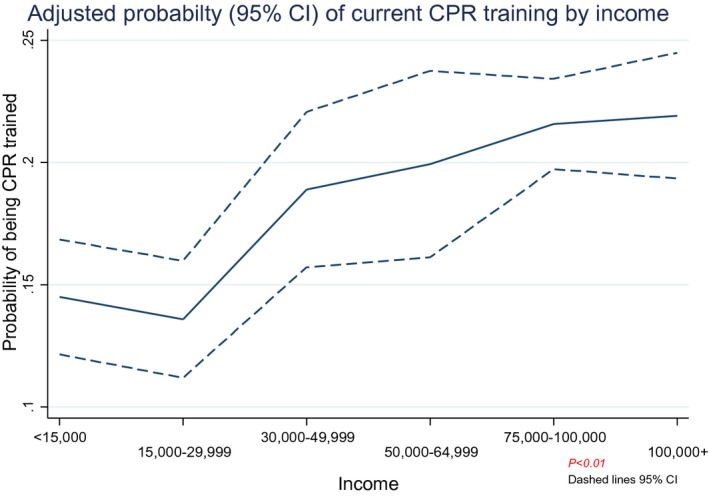
Adjusted probability of current CPR training by income with 95% CIs. CPR indicates cardiopulmonary resuscitation.
Similar demographic associations were noted between those who had ever received training compared to those who never received CPR training. Of those who were ever trained, increased age was associated with CPR training (OR for each year of increased age, 0.99; 95% CI, 0.98–0.99; P=0.04). When age was examined categorically (global P value, 0.04), those who were aged 80 years or older were 0.34 (95% CI, 0.22–0.52) times less likely to be ever CPR trained compared with those who were 18 to 29 years old (P<0.01); those who were aged 70 to 79 years were 0.58 (95% CI, 0.43–0.77) times less likely to be ever trained (P<0.01) and those aged 60 to 69 years were 0.86 (95% CI, 0.71–1.05) times less likely to be ever trained compared with 18 to 30 year olds (P=nonsignificant; Table 2).
Descriptive Comparision of Age of Training and B‐CPR Delivery
Among those who were currently trained, the mean age was 42 (95% CI, 41–43), whereas the mean age of those ever trained was 46 (95% CI, 47–49), compared with 48 (95% CI, 6–51) of those never trained. In contrast, the mean age of SCA victims in the US population within the ROC cohort was 63.8±19.8 (Figure 3). Furthermore, we examined the association of B‐CPR delivery during SCA events by victim age and found a statistically significant association of decreased B‐CPR delivery with increased age with events that occurred in the home environment (Figure 4), in a fashion that mirrored the age‐dependant nature of CPR training demonstrated in our survey work. This association of decreased B‐CPR with victim age was not found among SCA events in the public setting.
Figure 3.
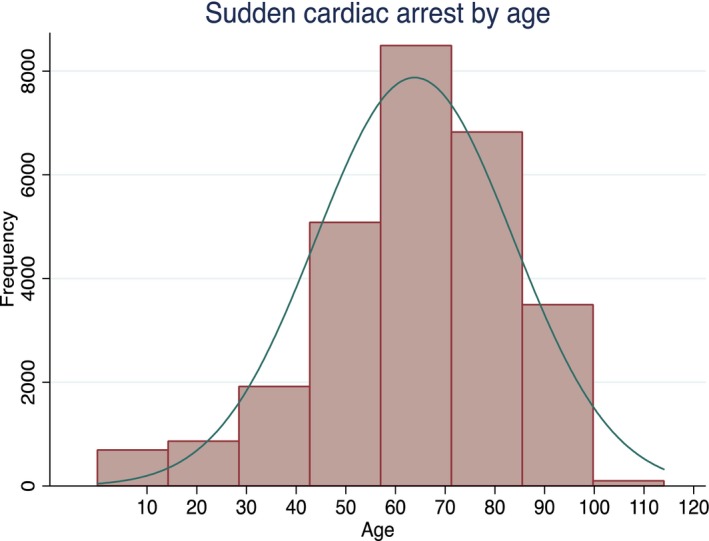
Histogram displaying the frequency of SCA events by victim age using data from the US Resuscitation Outcomes Consortium Epistry data registry (2011–2015).
Figure 4.
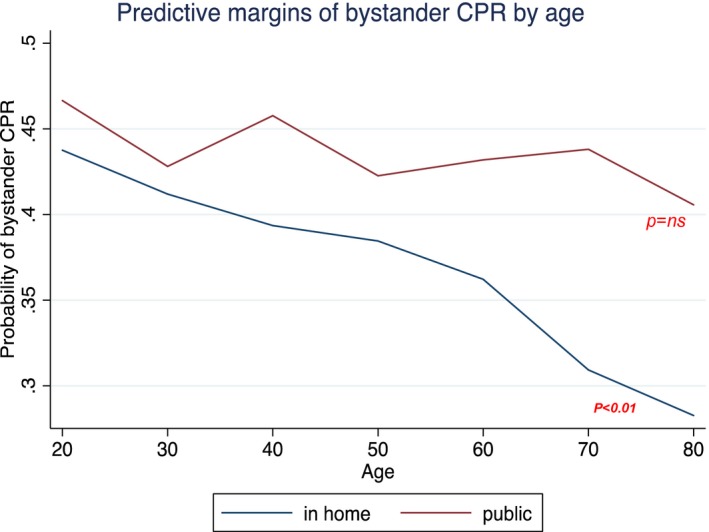
Adjusted probability of SCA victims receiving B‐CPR by age stratified by events in the home and public environment. B‐CPR indicates bystander cardiopulmonary resuscitation; CPR, cardiopulmonary resuscitation.
Discussion
In a nationally representative telephone survey, we found that the overall prevalence of current CPR training was 18%, whereas 65% of the population identified being trained at some point in their lifetime. We identified an independent association between both older age and lower SES with a decreased likelihood of CPR training. To our knowledge, this is the first study to estimate the national CPR training prevalence within the US population.
Age and CPR Training Status
Our work found a striking association with older age and decreased likelihood of CPR training. This is especially important given that the mean age of SCA victims in the United States is ≈64 years of age. Previous studies have demonstrated that B‐CPR rates are lower in the private residential environment compared with the public setting.1, 18 It is possible that spouses (generally of comparable ages) may be the first responders to SCA events in these environments. Whereas our findings suggest that many older individuals have been trained at some point, the prevalence of current training in the highest‐risk population is very low. Furthermore, our findings suggest that a victims chance of receiving B‐CPR in the home environment decreases by age, further affirming the need to consider targeted training in the older population. It may be the spouses or close loved ones of older individuals who are most likely to need to act during SCA events in the home environment. Future initiatives should consider targeted methods to train this population, which may be at higher risk of witnessing SCA events, especially in the home setting where few others may be available to provide prompt care.
SES and CPR Training Status
Previous studies have suggested an association with SES and B‐CPR delivery.19, 20, 21, 22 Specifically, a recent study found that individuals living in low‐income black neighborhoods were much less likely to receive B‐CPR compared with the national population (odds ratio, 0.49; 95% CI, 0.41–0.58).23 Additionally, the work of Anderson et al demonstrated aggregate geographical, racial, and SES disparities with B‐CPR training.8 The current work has confirmed and extended these findings, allowing for individual‐level linkage of CPR training status with self‐reported SES demographic data. We found an association with lower educational attainment and household income and decreased liklihoood of CPR training. Future training initiatives should address barriers that may prevent lower SES individuals from receiving CPR training.
Dispatch CPR as an Alternate to Broad CPR Training
Recent studies have highlighted the importance of dispatch‐assisted CPR (D‐CPR, also known as telephone CPR or telecommunicator CPR) as another method to increase B‐CPR delivery.24, 25, 26 However, the relationship between D‐CPR and CPR training is unknown; it is possible that CPR training improves the bystander response to D‐CPR instructions, and that lack of CPR training may limit willingness to accept instructions from the dispatchers. In a recent investigation, even when D‐CPR instructions were optimized, the change in the B‐CPR rate was modest (61.8% before D‐CPR and 66.8% after D‐CPR bundled intervention; P=0.006),27 suggesting the role of additional factors that affect the actual provision of CPR following dispatch instructions. Further studies will be required to assess the interplay between D‐CPR, layperson CPR training, and actual delivery.
Importance of Targeted CPR Training
Organizations such as the American Heart Association and American Red Cross have expended broad efforts to increase public CPR training, yet little is known as to which individuals should be targeted for training to maximize the public health benefit. The National Academy of Medicine (formerly the Institute of Medicine) has selected SCA, CPR delivery, and resuscitation outcomes as foci of a national report (“Strategies to Improve Cardiac Arrest Survival: A Time to Act”), underscoring the public health importance of this topic.28 Specifically, the National Academy of Medicine report called for educating and engaging the public stating that “all can play a role in the effort to promote and facilitate CPR training.”28 Furthermore, scientific advisories and consensus statements from the American Heart Association have emphasized the importance of addressing barriers to CPR education.29, 30, 31, 32 Understanding individual‐level disparities in CPR training status could help inform future targeted educational initiatives and increase rates of B‐CPR delivery. Developing effective interventions based on our understanding of these relationships has the potential to greatly influence CPR education programs and inform future public health initiatives, to maximize the lay public response to SCA and improve survival.
The current work has limitations inherent in telephone survey methodology. Although our survey has a low response rate, it is similar to other nationally representative telephone surveys.11, 33 Investigations have demonstrated that lower response rates are not necessarily associated with increased nonresponse bias in public health surveys.33, 34 For example, Keeter et al compared the results of a 5‐day survey fielding period (response rate of 36%) to the results from fielding the same survey for 8 weeks (response rate of 61%) and found no significant differences in the outcomes of interest between the 2 surveys.34, 35, 36 Although this is a limitation of the methodology, the random digit dial approach is more cost‐effective than mail or door‐to‐door surveys. Furthermore, we acknowledge that survey methodology is subject to both recall and social desirability bias. We are encouraged that our findings regarding CPR training prevalence are similar to that from our Health Household Survey implemented in southeastern Pennsylvania, which found an 18% prevalence of current CPR training and 61% prevalence of training overall.12
In conclusion, the national prevalence of those currently trained in CPR was low. Our data suggest that many individuals obtain CPR training at some point in time, but few maintain current training. Furthermore, older individuals are less likely to be CPR trained, and lower SES is also associated with a decreased likelihood of CPR training. These findings suggest the need for focused CPR training efforts to address these disparities and maximize public health benefit.
Sources of Funding
This work was supported by a Mentored Clinical and Population Award from the American Heart Association (15MCPRP25090161) and a Patient Centered Outcomes Research Institute Communication and Dissemination Contract (CDR‐1409‐23100).
Disclosures
Ms Blewer has research funding through the American Heart Association. Ms Leary has research funding through the American Heart Association and Medtronic Foundation. Ms Leary has received in‐kind support from Laerdal and Physio‐Control. Dr Morrison is the Robert and Dorothy Pitts Chair in Acute Care and Emergency Medicine at Li Ka Shing Knowledge Institute at St. Michael's Hospital. She volunteers for the American Heart Association and the International Liason Committee on Resuscitation. Dr Aufderheide, Dr Daya, Dr Callaway, and Kudenchuk receives research funding from the National Institutes of Health. Dr Idris receives research funding from the National Institutes of Health and Physio‐Control (HeartSine), as well as in‐kind support. He serves as a volunteer for the American Heart Association. Dr Abella has received research funding from the NIH, PCORI, the Medtronic Foundation, the American Heart Association, and CR Bard. He has received honoraria from Philips Healthcare and CR Bard, as well as in‐kind research support from Laerdal Medical Corporation. Dr Ibrahim is supported in part by a K24 Mid‐Career Development Award from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (K24AR055259). The views expressed in this manuscript are those of the author and do not represent those of the Department of Veterans Affairs, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, or the National Institutes of Health.
Supporting information
Data S1. Additional Survey Weighting Information.
Table S1. National CPR Survey
Table S2. Missing Data by Demographic Variable
Acknowledgments
We thank Shaun McGovern and Andrew Murray for their assistance with manuscript preparation and Daniel Ikeda for his assistance piloting the survey questions.
(J Am Heart Assoc. 2017;6:e006124 DOI: 10.1161/JAHA.117.006124.)28515114
References
- 1. Weisfeldt ML, Everson‐Stewart S, Sitlani C, Rea T, Aufderheide TP, Atkins DL, Bigham B, Brooks SC, Foerster C, Gray R, Ornato JP, Powell J, Kudenchuk PJ, Morrison LJ. Ventricular tachyarrhythmias after cardiac arrest in public versus at home. N Engl J Med. 2011;364:313–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chan PS, McNally B, Tang F, Kellermann A. Recent trends in survival from out‐of‐hospital cardiac arrest in the United States. Circulation. 2014;130:1876–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hasselqvist‐Ax I, Riva G, Herlitz J, Rosenqvist M, Hollenberg J, Nordberg P, Ringh M, Jonsson M, Axelsson C, Lindqvist J, Karlsson T, Svensson L. Early cardiopulmonary resuscitation in out‐of‐hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. [DOI] [PubMed] [Google Scholar]
- 4. Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H. Effectiveness of bystander‐initiated cardiac‐only resuscitation for patients with out‐of‐hospital cardiac arrest. Circulation. 2007;116:2900–2907. [DOI] [PubMed] [Google Scholar]
- 5. Malta Hansen C, Kragholm K, Pearson DA, Tyson C, Monk L, Myers B, Nelson D, Dupre ME, Fosbol EL, Jollis JG, Strauss B, Anderson ML, McNally B, Granger CB. Association of bystander and first‐responder intervention with survival after out‐of‐hospital cardiac arrest in North Carolina, 2010–2013. JAMA. 2015;314:255–264. [DOI] [PubMed] [Google Scholar]
- 6. Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang‐Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp‐Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out‐of‐hospital cardiac arrest. JAMA. 2013;310:1377–1384. [DOI] [PubMed] [Google Scholar]
- 7. Moller Nielsen A, Lou Isbye D, Knudsen Lippert F, Rasmussen LS. Engaging a whole community in resuscitation. Resuscitation. 2012;83:1067–1071. [DOI] [PubMed] [Google Scholar]
- 8. Anderson ML, Cox M, Al‐Khatib SM, Nichol G, Thomas KL, Chan PS, Saha‐Chaudhuri P, Fosbol EL, Eigel B, Clendenen B, Peterson ED. Rates of cardiopulmonary resuscitation training in the United States. JAMA Intern Med. 2014;174:194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blendon RJ, Benson JM, Brule A. Implications of the 2012 election for health care—the voters’ perspective. N Engl J Med. 2012;367:2443–2447. [DOI] [PubMed] [Google Scholar]
- 10. Blendon RJ, Benson JM, Hero JO. Public trust in physicians—U.S. medicine in international perspective. N Engl J Med. 2014;371:1570–1572. [DOI] [PubMed] [Google Scholar]
- 11. Lang K, Alexander IM, Simon J, Sussman M, Lin I, Menzin J, Friedman M, Dutwin D, Bushmakin AG, Thrift‐Perry M, Altomare C, Hsu MA. The impact of multimorbidity on quality of life among midlife women: findings from a U.S. nationally representative survey. J Womens Health (Larchmt). 2015;24:374–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blewer AL, Leary M, Ikeda D, Becker LB, Abella BS. The majority of laypersons trained in CPR do not maintain current certification or training. Circulation. 2015;132:A16326. [Google Scholar]
- 13. Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. [DOI] [PubMed] [Google Scholar]
- 14. Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–784. [DOI] [PubMed] [Google Scholar]
- 15. Idris AH, Guffey D, Aufderheide TP, Brown S, Morrison LJ, Nichols P, Powell J, Daya M, Bigham BL, Atkns DL, Berg R, Davis D, Stiell I, Sopko G, Nichol G; Resuscitation Outcomes Consorium (ROC) Investigators . Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125:3004–3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, Leroux B, Vaillancourt C, Wittwer L, Callaway CW, Christenson J, Egan D, Ornato JP, Weisfeldt ML, Stiell IG, Idris AH, Aufderheide TP, Dunford JV, Colella MR, Vilke GM, Brienza AM, Desvigne‐Nickens P, Gray PC, Gray R, Seals N, Straight R, Dorian P; Resuscitation Outcomes Consortium Investigators . Amiodarone, lidocaine, or placebo in out‐of‐hospital cardiac arrest. N Engl J Med. 2016;374:1711–1722. [DOI] [PubMed] [Google Scholar]
- 17. U.S. Census Bureau; American Community Survey, 2014. 2015. Available at: https://www.census.gov/programs-surveys/acs/news/data-releases.html. Accessed October 15, 2016.
- 18. Nichol G, Aufderheide TP, Eigel B, Neumar RW, Lurie KG, Bufalino VJ, Callaway CW, Menon V, Bass RR, Abella BS, Sayre M, Dougherty CM, Racht EM, Kleinman ME, O'Connor RE, Reilly JP, Ossmann EW, Peterson E. Regional systems of care for out‐of‐hospital cardiac arrest: a policy statement from the American Heart Association. Circulation. 2010;121:709–729. [DOI] [PubMed] [Google Scholar]
- 19. Fosbol EL, Dupre ME, Strauss B, Swanson DR, Myers B, McNally BF, Anderson ML, Bagai A, Monk L, Garvey JL, Bitner M, Jollis JG, Granger CB. Association of neighborhood characteristics with incidence of out‐of‐hospital cardiac arrest and rates of bystander‐initiated CPR: implications for community‐based education intervention. Resuscitation. 2014;85:1512–1517. [DOI] [PubMed] [Google Scholar]
- 20. Root ED, Gonzales L, Persse DE, Hinchey PR, McNally B, Sasson C. A tale of two cities: the role of neighborhood socioeconomic status in spatial clustering of bystander CPR in Austin and Houston. Resuscitation. 2013;84:752–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sasson C, Keirns CC, Smith DM, Sayre MR, Macy ML, Meurer WJ, McNally BF, Kellermann AL, Iwashyna TJ. Examining the contextual effects of neighborhood on out‐of‐hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Becker LB, Han BH, Meyer PM, Wright FA, Rhoades KV, Smith DW, Barrett J. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329:600–606. [DOI] [PubMed] [Google Scholar]
- 23. Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, Haukoos JS; Group CS . Association of neighborhood characteristics with bystander‐initiated CPR. N Engl J Med. 2012;367:1607–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher‐assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–2516. [DOI] [PubMed] [Google Scholar]
- 25. Bobrow B, Spaite D, Vadeboncoeur T, Chengcheng H, Mullins T, Tormala W, Dameff C, Gallagher J, Smith G, Panczyk M. Implementation of a regional telephone cardiopulmonary resuscitation program and outcomes after out‐of‐hospital cardiac arrest. JAMA Cardiol. 2016;1:295–302. [DOI] [PubMed] [Google Scholar]
- 26. Lewis M, Stubbs BA, Eisenberg MS. Dispatcher‐assisted cardiopulmonary resuscitation: time to identify cardiac arrest and deliver chest compression instructions. Circulation. 2013;128:1522–1530. [DOI] [PubMed] [Google Scholar]
- 27. White L, Rogers J, Bloomingdale M, Fahrenbruch C, Culley L, Subido C, Eisenberg M, Rea T. Dispatcher‐assisted cardiopulmonary resuscitation: risks for patients not in cardiac arrest. Circulation. 2010;121:91–97. [DOI] [PubMed] [Google Scholar]
- 28. Committee on the Treatment of Cardiac Arrest: Current S, Future D, Board on Health Sciences P and Institute of M . The National Academies Collection: reports funded by National Institutes of Health In: Graham R, McCoy MA, Schultz AM, eds. Strategies to Improve Cardiac Arrest Survival: A Time to Act. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 29. Abella BS, Aufderheide TP, Eigel B, Hickey RW, Longstreth WT Jr, Nadkarni V, Nichol G, Sayre MR, Sommargren CE, Hazinski MF. Reducing barriers for implementation of bystander‐initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–709. [DOI] [PubMed] [Google Scholar]
- 30. Sayre MR, Berg RA, Cave DM, Page RL, Potts J, White RD. Hands‐only (compression‐only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out‐of‐hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation. 2008;117:2162–2167. [DOI] [PubMed] [Google Scholar]
- 31. Sasson C, Meischke H, Abella BS, Berg RA, Bobrow BJ, Chan PS, Root ED, Heisler M, Levy JH, Link M, Masoudi F, Ong M, Sayre MR, Rumsfeld JS, Rea TD. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–1350. [DOI] [PubMed] [Google Scholar]
- 32. Morley PT, Lang E, Aickin R, Billi JE, Eigel B, Ferrer JM, Finn JC, Gent LM, Griffin RE, Hazinski MF, Maconochie IK, Montgomery WH, Morrison LJ, Nadkarni VM, Nikolaou NI, Nolan JP, Perkins GD, Sayre MR, Travers AH, Wyllie J, Zideman DA. Part 2: evidence evaluation and management of conflicts of interest: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015;132:S40–S50. [DOI] [PubMed] [Google Scholar]
- 33. Keeter S, Kennedy C, Dimock M, Best J, Craighill P. Gauging the impact of growing nonresponse on estimates from a national RDD telephone survey. Public Opin Q. 2006;70:759–779. [Google Scholar]
- 34. Keeter S, Miller C, Kohut A, Groves RM, Presser S. Consequences of reducing nonresponse in a national telephone survey. Public Opin Q. 2000;64:125–148. [DOI] [PubMed] [Google Scholar]
- 35. Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70:646–675. [Google Scholar]
- 36. Groves RM, Peytcheva E. The impact of nonresponse rates on nonresponse bias—a meta‐analysis. Public Opin Q. 2008;72:167–189. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Additional Survey Weighting Information.
Table S1. National CPR Survey
Table S2. Missing Data by Demographic Variable


