Abstract
Objectives:
To evaluate the effect of a self-controlled vocal exercise in elderly people with glottal closure insufficiency.
Design:
Parallel-arm, individual randomized controlled trial.
Methods:
Patients who visited one of 10 medical centers under the National Hospital Organization group in Japan for the first time, aged 60 years or older, complaining of aspiration or hoarseness, and endoscopically confirmed to have glottal closure insufficiency owing to vocal cord atrophy, were enrolled in this study. They were randomly assigned to an intervention or a control group. The patients of the intervention group were given guidance and a DVD about a self-controlled vocal exercise. The maximum phonation time which is a measure of glottal closure was evaluated, and the number of patients who developed pneumonia during the six months was compared between the two groups.
Results:
Of the 543 patients enrolled in this trial, 259 were allocated into the intervention group and 284 into the control; 60 of the intervention group and 75 of the control were not able to continue the trial. A total of 199 patients (age 73.9 ±7.25 years) in the intervention group and 209 (73.3 ±6.68 years) in the control completed the six-month trial. Intervention of the self-controlled vocal exercise extended the maximum phonation time significantly (p < 0.001). There were two hospitalizations for pneumonia in the intervention group and 18 in the control group, representing a significant difference (p < 0.001).
Conclusion:
The self-controlled vocal exercise allowed patients to achieve vocal cord adduction and improve glottal closure insufficiency, which reduced the rate of hospitalization for pneumonia significantly.
Clinical Trial.gov Identifier-UMIN000015567
Keywords: Aging, glottal closure insufficiency, aspiration pneumonia, self-controlled vocal exercise, randomized controlled trial
Introduction
People with glottal closure insufficiency are at increased risk of aspiration1–4 and developing pneumonia, and this is particularly common in the elderly.5–7 Despite the frequency of occurrence of glottal closure insufficiency, no simple treatment has yet been established.
During the act of swallowing, the larynx normally elevates and the epiglottis is sandwiched between the base of the tongue and the framework of the larynx.8–11 This instantaneous motion prevents aspiration,12,13 however, atrophy of the extrinsic laryngeal muscles with age lowers the position of the larynx,14 and weakening of the muscles makes it difficult to elevate the larynx sufficiently to prevent aspiration while swallowing.15,16
Furthermore, the cough reflex can prevent aspiration even among the elderly.17,18 Increased subglottic pressure with glottal closure is necessary for aspirated inflow to be removed through the cough reflex. Although glottal closure is also important in generating speech with vibration of the vocal cords, its original purpose was to prevent aspiration when swallowing.19 Age-related atrophic changes in the intrinsic laryngeal muscles commonly cause glottal closure insufficiency,20–22 or so-called glottal incompetence. Anatomical and functional problems resulting from glottal closure failure include not only breathy hoarseness or shortening of the maximum phonation time,23,24 but also frequent laryngeal inflow and difficulty in expectoration owing to insufficient subglottic pressure to remove aspirated substances through coughing.25,26 As a result, continued aspiration can lead to the development of pneumonia.6,27
As described, two major defense mechanisms can prevent aspiration: Laryngeal elevation and glottal closure. As a substitute for laryngeal elevation, we recommend that patients draw in the jaw during the act of swallowing. Another solution is preventing glottal incompetence. Currently, the surgical techniques for the treatment of glottal closure insufficiency involve injection or implantation of autologous fat or fascia into atrophied vocal cords.23,28–31 However, the transplanted cells are also aged and the effects sometimes do not last, so the invasive allocations have to be repeated and those take high medical expenses. It was therefore necessary to develop a minimally invasive, low-cost, widely applicable treatment.
The pushing method,32 which is conventionally recommended and effective for unilateral vocal cord paralysis, is sometimes not suitable for the aged larynx because it often causes excessive adduction of the false vocal cords and constriction of the supraglottal structures. To prevent constriction of pharyngeal cavity and supraglottal structures and get proper glottal adduction, we modified the pushing method and developed a self-controlled vocal exercise method as a more cost-effective treatment than the surgery.
To evaluate the effectiveness of the new self-controlled vocal exercise in patients with physiological glottal closure failure owing to aging, the rate of incidence of pneumonia within six months after the start of performing the exercise was compared between the intervention and control groups in a randomized controlled trial.
Methods
Setting
The research was performed in 10 hospitals under the National Hospital Organization (NHO) group in Japan. This research protocol was approved by the NHO Tokyo Medical Center Ethics Committee (the institutional review board of Tokyo Medical Center), and each Ethics Committee of the remaining nine NHO hospitals. Before enrollment, all volunteers signed written informed consent forms. This study was registered as UMIN 000015567.
Recruiting patients
From 2011 to 2014, patients who were 60 years of age or older, visited one of 10 hospitals under the Japanese NHO for the first time for the treatment of dysphonia, and were endoscopically confirmed to have glottal closure insufficiency owing to vocal cord atrophy were assessed for eligibility for this study. Patients who met the selection criteria were enrolled in this study. Selection criteria were: (1) ⩾60 years of age; (2) experiencing hoarseness/dysphonia caused by glottal incompetence; and (3) diagnosis of atrophy of the vocal cords or sulcus vocalis as confirmed in laryngeal endoscopic examination. Exclusion criteria were: (1) patient preference for surgical treatment; (2) inability to perform the self-controlled vocal exercise for any reason; and (3) acute inflammation, polyps, tumors, granulomas, nodules, or paralysis of the vocal cords.
Randomization
Patients who presented with hoarseness/dysphonia underwent laryngeal endoscopy at the initial visit to confirm the diagnosis of glottal closure insufficiency owing to vocal fold atrophy with age. After an explanation of the trial and receiving a signature on the written informed consent form, physicians contacted the independent randomization center and reported they had recruited patients. The people in the center allocated the patients to the intervention or the control group using a random number meter. For example, if an even number came out, the patient was allocated to the intervention group, and an odd number, the control group .Then they replied to the physicians indicating which group their patients were assigned to.
Differentiating the intervention group and the control group
Patients in the intervention group were given a brochure explaining the cause of glottal closure failure owing to aging, how age-related vocal cord atrophy leads to hoarseness and aspiration, recommendations on how to modulate the voice while speaking and singing, and how to prevent aspiration. They were then shown a DVD of how to perform the self-controlled vocal exercise with simultaneous explanation by a physician or a speech therapist. The DVD of the self-controlled vocal exercise with English subtitles can be accessed at http://www.kankakuki.go.jp/video_nhk_eng.html. Although patients in the control group were also given the same brochure, they did not view the DVD and never received any additional instructions of the vocal exercise.
Self-controlled vocal exercise method in the intervention group
Patients in the intervention group were given an explanation of the anatomy and physiology of the glottis and the role of glottal closure. In particular, it was explained that glottal closure is important not only for storing air to increase vocal force, but also to prevent aspiration. Then, they were instructed to perform the self-controlled vocal exercise in the following manner.
Sit on a chair and grip the sides of the seat with both hands.
While saying each number from one to 10 out loud, pull up firmly on both sides of the seat, then relax and inhale naturally before saying the next number.
Repeat this exercise for a total of two sets in both the morning and evening, for a total of four sets per day.
Each set takes about 30 seconds to perform, requiring only two minutes of daily exercise. The point of this exercise is to synchronize vocalization with the motion of pulling upward on the edges of the seat. Moreover, the duration of vocalization while counting should be the same as that of the upward pulling motion. In this method, it takes about 300–500 milliseconds to say each number, and then patients relax until saying the next number. It takes three to five seconds for each movement in the series. It is possible to prevent contraction of the pharyngeal cavity and of supraglottal structures with such a short utterance.
Measurement of the maximum phonation time
At the initial visit, the maximum phonation time, which is one of indicators of glottal closure, was measured. We counted how long the patients kept phonation (the sound; ‘a’) without a breath. By the maximum phonation time levels of the first visit, we divided patients into five groups of A–E. (Group A: less than five seconds; Group B: five to less than 10 seconds; Group C: 10 to less than 15 seconds; Group D: 15 to less than 20 seconds; Group E: 20 seconds and more).
Follow-up
One, three, and six months after enrollment in the randomized controlled trial, the patients in both groups underwent laryngeal fiberscopic examinations and maximum phonation time measurement. As the most frequent side-effect of the pushing method is hyperadduction, meticulous care must be taken in diagnosing this complication. We therefore performed laryngeal fiberscopic examinations one month after the start of training, and if signs of hyperadduction were observed in the intervention group, the correct exercise method was re-guided.
Investigation of hospitalization with pneumonia within six months
One objective of this study was to compare the number of hospitalizations with pneumonia between the intervention group and the control group. Physicians checked whether patients had been suffering from pneumonia and required hospitalization for treatment within six months. Patients or their family reported their hospitalization on the phone, or physicians gave phone calls to ask patients or other physicians who had given diagnosis. The patients were diagnosed with pneumonia by chest X-ray, magnetic resonance imaging, or computed tomography scanning. Each diagnosis of pneumonia was given by the physicians, who were blinded to allocation.
Statistical analysis
Statistical analysis of differences between the intervention and the control groups was carried out with the Statistical Package for Social Science (IBM Corp., released in 2014, IBM SPSS Statistics for Windows version 22.0, Armonk, NY, USA) using two-way factorial analysis of variance for analysis of the maximum phonation time, and the (Mantel–Haenszel method) χ-square test for the analysis of the number of hospitalizations with pneumonia.
Results
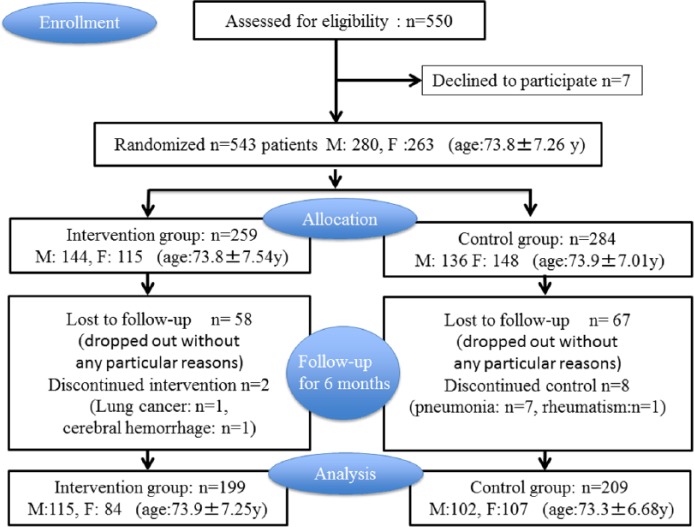
A total of 550 patients were assessed for eligibility for this study. As seven patients declined to participate, 543 patients (men: 280; women: 263), ranging in age from 60 to 91 years (mean 73.8 ±7.26) who met the inclusion criteria were enrolled in this study. Of the 543 patients who participated in this trial, 259 were allocated into the intervention group and 284 into the control group. A total of 60 patients of the intervention group and 75 of the control were not able to continue the trial for six months. A total of 199 patients (men: 115; women: 84; age: 73.9 ±7.25 years) in the intervention and 209 (men: 102; women: 107; age: 73.3 ±6.68 years) in the control group completed the six-month trial (Figure 1).
Figure 1.
Patient enrollment and randomization procedure.
Hyperadduction of the false vocal cords
Only three patients in the intervention group showed hyperadduction of the false vocal cords one month after the start of the exercise. These patients spent one second or longer pulling up on the sides of the seat while vocalizing, which caused the hyperadduction. We explained the reason for this problem in detail and demonstrated the correct performance of the self-controlled vocal exercise method again on the one-month hospital visit. Subsequently, the hyperadduction was resolved in all and was not noted at the three-month examination.
Comparison of maximum phonation time
In all the five groups classified by the maximum phonation time levels of the first visit, there was a tendency that the maximum phonation time had been extended longer in intervention groups than control groups (Table 1). To evaluate the change in the maximum phonation time from the first visit to 6 months in the 2 groups (Table 1; Δ), statistical analysis was conducted using a two-way factorial analysis of variance. The results showed that performance of the self-controlled vocal exercise had a significant effect on the length of the maximum phonation time (p < 0.001) (Figure 2). As there was no interaction between the two factors, i.e. the maximum phonation time at the initial visit and randomization to the intervention or control group, the intervention effect was not affected by the maximum phonation time at the initial visit. In other words, regardless of the length of the maximum phonation time at the initial medical examination, the exercise was effective in prolonging it.
Table 1.
Comparison of maximum phonation time.
| Intervention group |
Control group |
|||||||
|---|---|---|---|---|---|---|---|---|
| n | MPT at first visit | MPT at 6 month | ∆ | n | MPT at first visit | MPT at 6 month | ∆ | |
| Group A less than 5 seconds |
11 | 3.3 ± 0.28 | 16 ± 2.57 | 12.6 ± 8.60 | 7 | 3.7 ± 0.18 | 8.4 ± 1.83 | 4.7 ± 5.26 |
| Group B 5 to less than 10 seconds |
60 | 6.8 ± 0.16 | 15.0 ± 0.76 | 8.2 ± 5.65 | 38 | 7.7 ± 0.18 | 10.1 ± 0.57 | 2.2 ± 3.50 |
| Group C 10 to less than 15 seconds |
70 | 11.9 ± 0.16 | 21.1 ± 0.87 | 9.1 ± 7.23 | 64 | 11.7 ± 0.17 | 13.0 ± 0.52 | 1.2 ± 3.86 |
| Group D 15 to less than 20 seconds |
38 | 16.4 ± 0.23 | 23.6 ± 1.07 | 7.1 ± 6.68 | 43 | 17.0 ± 0.41 | 16.4 ± 0.66 | −0.6 ± 4.02 |
| Group E 20 seconds and more |
20 | 24.1 ± 0.83 | 29.9 ± 1.33 | 5.8 ± 5.73 | 57 | 24.7 ± 0.60 | 21.5 ± 0.87 | −3.2 ± 6.30 |
MPT: maximum phonation time (seconds).
By the maximum phonation time levels of the first visit, we divided patients into five groups of A–E.
In all the five groups, there was a tendency that the maximum phonation time had been extended longer in the intervention groups than the control groups.
Figure 2.
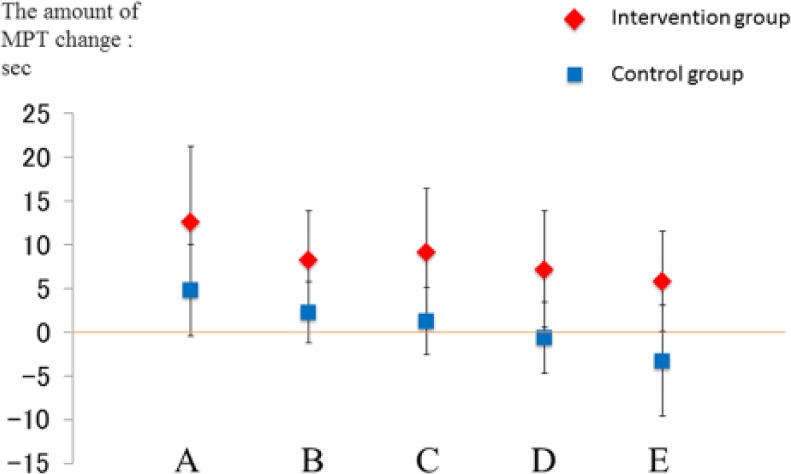
Changes in the maximum phonation time from the first visit to six months.
Assessment of the number of hospitalization with pneumonia
Only two (men) of 199 patients in the intervention group were hospitalized with pneumonia during the six-month trial. Of 216 patients in the control group, including seven who dropped out of the trial because of pneumonia, 18 (nine men and nine women) were hospitalized with pneumonia during the six-month period. The χ-square (Mantel–Haenszel method) test showed that the number of hospitalizations with pneumonia was significantly higher in the control group compared with the intervention group (p < 0.001) (Table 2).
Table 2.
Comparison of hospitalizations with pneumonia in the intervention and control groups.
| Intervention group | Control group | |
|---|---|---|
| Case number | 199 cases | 216 cases (including 7 who dropped out due to pneumonia) |
| Age | 73.9 ± 7.25 years old | 73.3 ±6.66 years old |
| Men | 115 | 106 |
| Women | 84 | 110 |
| Number of hospitalizations for pneumonia within 6 months | 2*
(2 men) |
18**
(9 men, 9 women) |
*, **: p < 0.001.
The number of hospitalizations with pneumonia was significantly higher in the control group compared with the intervention group (p < 0.001).
Discussion
Vocal function in the intervention group improved significantly after six months, and this group had a low rate of hospitalization with pneumonia. It therefore appears that the exercise is an effective, low-cost method for preventing pneumonia.
There were no adverse events in the intervention group during this six-month trial except three cases of hyper adduction. Although three patients exhibited slight hyperadduction one month after the start of the trial, this side-effect was completely resolved in all, after correcting self-controlled vocal exercise performance. Compared with the conventional pushing method, the duration of vocalization in the self-controlled vocal exercise is much shorter, taking as little as 300–500 milliseconds to speak each number. The pushing method was originally recommended for severe glottal closure insufficiency resulting from conditions such as unilateral vocal cord paralysis. It allows the entire structure to center around the glottis and forces glottal closure. However, in cases of closure insufficiency without paralysis, hyperadduction of vocal cords and contraction of the supraglottic structures around the glottis can sometimes occur with the pushing method. For glottal insufficiency owing to aging, the self-controlled vocal exercise allows only the vocal cords to move to the center, and it results in moderate glottal closure.
This study had some limitations. First, patients were simply randomized to the control or intervention group and were not stratified in terms of co-morbidities, medications, etc. Cognition and frailty indices were not measured. Second, the physicians who examined the patients initially at one, three, and six months were not blinded to the randomization, which could have resulted in a degree of reporting bias.
The population experiencing the physiological changes associated with aging, including glottal closure failure, will increase in the future. Although surgical treatments are effective, they are not appropriate as standard therapies owing to their invasiveness and cost. The self-controlled vocal exercise is economical and should be promoted as first-line therapy. In terms of contributing to health and longevity, maintaining the ability to speak will result in the prevention of aspiration and associated pneumonia. This would lead to both improved quality of life for patients and their families, and reduction in healthcare costs.
Clinical message.
The self-controlled vocal exercise allowed patients to achieve vocal cord adduction and improved glottal closure insufficiency.
The self-controlled vocal exercise significantly reduced the rate of hospitalization for pneumonia.
Acknowledgments
The authors thank the patients who participated in this study; the NHO members who cooperated in this trial, in particular Drs Seiji Bito, Kaoru Furuno, Syujiro Minami, Fumiyuki Goto, Tatsuo Matsunaga, Masato Fujii, and Kimitaka Kaga for advice; and Ms Hiromi Tsuruoka and Ms Kazuyo Ishikawa for assistance.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the National Hospital Organization Network Joint Research Fund.
References
- 1. Rajaei A, Barzegar Bafrooei E, Mojiri F, Nilforoush MH. The occurrence of laryngeal penetration and aspiration in patients with glottal closure insufficiency. ISRN Otolaryngol 2014; 2014: 587945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bhattacharyya N, Kotz T, Shapiro J. Dysphagia and aspiration with unilateral vocal cord immobility: Incidence, characterization, and response to surgical treatment. Ann Otolaryngol Rhinol Laryngol 2002; 111(8): 672–679. [DOI] [PubMed] [Google Scholar]
- 3. Ryu JS, Park SR, Choi KH. Prediction of laryngeal aspiration using voice analysis. Am J Phys Med Rehabil 2004; 83(10): 753–757. [DOI] [PubMed] [Google Scholar]
- 4. Giraldez-Rodriguez LA, Johns M., 3rd Glottal insufficiency with aspiration risk in dysphagia. Otolaryngol Clin North Am 2013; 46(6): 1113–1121. [DOI] [PubMed] [Google Scholar]
- 5. Yamaya M, Yanai M, Ohrui T, Arai H, Sasaki H. Interventions to prevent pneumonia among older adults. J Am Geriatrics Soc 2001; 49(1): 85–90. [DOI] [PubMed] [Google Scholar]
- 6. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest 2003; 124(1): 328–336. [DOI] [PubMed] [Google Scholar]
- 7. Kikawada M, Iwamoto T, Takasaki M. Aspiration and infection in the elderly: Epidemiology, diagnosis and management. Drugs Aging 2005; 22(2): 115–130. [DOI] [PubMed] [Google Scholar]
- 8. Shaker R, Dodds WJ, Dantas RO, Hogan WJ, Arndorfer RC. Coordination of deglutitive glottic closure with oropharyngeal swallowing. Gastroenterology 1990; 98(6): 1478–1484. [DOI] [PubMed] [Google Scholar]
- 9. Logemann JA, Kahrilas PJ, Cheng J, et al. Closure mechanisms of laryngeal vestibule during swallow. Am J Physiol 1992; 262(2 Pt 1): G338–344. [DOI] [PubMed] [Google Scholar]
- 10. Ohmae Y, Logemann JA, Kaiser P, Hanson DG, Kahrilas PJ. Timing of glottic closure during normal swallow. Head Neck 1995; 17(5): 394–402. [DOI] [PubMed] [Google Scholar]
- 11. Reidenbach MM. Anatomical considerations of closure of the laryngeal vestibule during swallowing. Eur Arch Oto-rhino-laryngol 1997; 254(9–10): 410–412. [DOI] [PubMed] [Google Scholar]
- 12. Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin North Am 1988; 21(4): 613–623. [PubMed] [Google Scholar]
- 13. Yokoyama M, Mitomi N, Tetsuka K, Tayama N, Niimi S. Role of laryngeal movement and effect of aging on swallowing pressure in the pharynx and upper esophageal sphincter. Laryngoscope 2000; 110(3 Pt 1): 434–439. [DOI] [PubMed] [Google Scholar]
- 14. Feng X, Todd T, Hu Y, et al. Age-related changes of hyoid bone position in healthy older adults with aspiration. Laryngoscope 2014; 124(6): E231–236. [DOI] [PubMed] [Google Scholar]
- 15. Feng X, Todd T, Lintzenich CR, et al. Aging-related geniohyoid muscle atrophy is related to aspiration status in healthy older adults. J Gerontol A Biol Sci Med Sci 2013; 68(7): 853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Curtis DJ, Sepulveda GU. Epiglottic motion: Video recording of muscular dysfunction. Radiology 1983; 148(2): 473–477. [DOI] [PubMed] [Google Scholar]
- 17. Ebihara S, Ebihara T. Cough in the elderly: A novel strategy for preventing aspiration pneumonia. Pulm Pharmacol Ther 2011; 24(3): 318–323. [DOI] [PubMed] [Google Scholar]
- 18. Ebihara S, Ebihara T, Kohzuki M. Effect of aging on cough and swallowing reflexes: Implications for preventing aspiration pneumonia. Lung 2012; 190(1): 29–33. [DOI] [PubMed] [Google Scholar]
- 19. Shaker R, Ren J, Bardan E, et al. Pharyngoglottal closure reflex: Characterization in healthy young, elderly and dysphagic patients with predeglutitive aspiration. Gerontology 2003; 49(1): 12–20. [DOI] [PubMed] [Google Scholar]
- 20. Malmgren LT, Fisher PJ, Bookman LM, Uno T. Age-related changes in muscle fiber types in the human thyroarytenoid muscle: An immunohistochemical and stereological study using confocal laser scanning microscopy. Otolaryngol Head Neck Surg 1999; 121(4): 441–451. [DOI] [PubMed] [Google Scholar]
- 21. Malmgren LT, Jones CE, Bookman LM. Muscle fiber and satellite cell apoptosis in the aging human thyroarytenoid muscle: A stereological study with confocal laser scanning microscopy. Otolaryngol Head Neck Surg 2001; 125(1): 34–39. [DOI] [PubMed] [Google Scholar]
- 22. Martins RH, Benito Pessin AB, Nassib DJ, Branco A, Rodrigues SA, Matheus SM. Aging voice and the laryngeal muscle atrophy. Laryngoscope 2015; 125(11): 2518–2521. [DOI] [PubMed] [Google Scholar]
- 23. Tsunoda K, Baer T, Niimi S. Autologous transplantation of fascia into the vocal fold: Long-term results of a new phonosurgical technique for glottal incompetence. Laryngoscope 2001; 111(3): 453–457. [DOI] [PubMed] [Google Scholar]
- 24. Miller S. Voice therapy for vocal fold paralysis. Otolaryngol Clin North Am 2004; 37(1): 105–119. [DOI] [PubMed] [Google Scholar]
- 25. Britton D, Benditt JO, Merati AL, et al. Associations between laryngeal and cough dysfunction in motor neuron disease with bulbar involvement. Dysphagia 2014; 29(6): 637–646. [DOI] [PubMed] [Google Scholar]
- 26. Pitts T. Airway protective mechanisms. Lung 2014; 192(1): 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lundy DS, Smith C, Colangelo L, et al. Aspiration: Cause and implications. Otolaryngol Head Neck Surg 1999; 120(4): 474–478. [DOI] [PubMed] [Google Scholar]
- 28. Mikaelian DO, Lowry LD, Sataloff RT. Lipoinjection for unilateral vocal cord paralysis. Laryngoscope 1991; 101(5): 465–468. [DOI] [PubMed] [Google Scholar]
- 29. Rihkanen H. Vocal fold augmentation by injection of autologous fascia. Laryngoscope 1998; 108(1 Pt 1): 51–54. [DOI] [PubMed] [Google Scholar]
- 30. Tsunoda K, Takanosawa M, Niimi S. Autologous transplantation of fascia into the vocal fold: A new phonosurgical technique for glottal incompetence. Laryngoscope 1999; 109(3): 504–508. [DOI] [PubMed] [Google Scholar]
- 31. Tsunoda K, Kondou K, Kaga K, et al. Autologous transplantation of fascia into the vocal fold: Long-term result of type-1 transplantation and the future. Laryngoscope 2005; 115(12 Pt 2 Suppl 108): 1–10. [DOI] [PubMed] [Google Scholar]
- 32. Yamaguchi H, Yotsukura Y, Sata H, et al. Pushing exercise program to correct glottal incompetence. J Voice 1993; 7(3): 250–256. [DOI] [PubMed] [Google Scholar]