Abstract
Purpose
To estimate lifetime risk of receiving an HIV diagnosis in the United States if existing infection rates continue.
Methods
We used mortality, census, and HIV surveillance data for 2010–2014 to calculate age-specific probabilities of an HIV diagnosis. The probabilities were applied to a hypothetical cohort of 10 million live births to estimate lifetime risk.
Results
Lifetime risk was 1 in 68 for males and 1 in 253 for females. Lifetime risk for men was 1 in 22 for blacks, 1 in 51 for Hispanic/Latinos, and 1 in 140 for whites; and for women was 1 in 54 for blacks, 1 in 256 for Hispanic/Latinas, and 1 in 941 for whites. By risk group, the highest risk was among men who have sex with men (1 in 6) and the lowest was among male heterosexuals (1 in 524). The majority of the states with the highest lifetime risk were in the south.
Conclusions
The estimates highlight different risks across populations and the need for continued improvements in prevention and treatment. They can also be used to communicate the risk of HIV infection and increase public awareness of HIV.
Keywords: HIV, surveillance, risk
INTRODUCTION
Approximately 1.2 million people were living with HIV infection in the United States at the end of 2012, 12.8% of whom were unaware of their infection (1). In addition, disparities continue to persist with men who have sex with men, and blacks/African Americans (hereafter referred to as blacks) and Hispanics/Latinos who make up the majority of persons with HIV diagnosed in 2013 (2). For HIV prevention messages to be effective, it is important to communicate clearly the burden of disease and who is at risk. One useful method to describe the burden of disease is to estimate lifetime risk, which is often expressed in terms of the number of people who would need to be followed throughout their lives to observe one occurrence of the disease. This method may be a useful tool for clinicians, outreach workers, and policy makers when describing the burden of HIV because it can be more readily understood by the general public. Lifetime risk is often used to describe the risk of cancer, and is sometimes used for HIV diagnosis.
Previous estimates of the lifetime risk of receiving an HIV diagnosis were generated using surveillance data for 2004–2005 from 33 states that had implemented confidential, name-based HIV reporting at that time (3). However, these estimates did not include all jurisdictions in the nation, and some trends in HIV have changed since that time, such as a decrease in HIV diagnosis rates among women (2). It is now also possible to determine lifetime risk of HIV diagnosis by risk group based on recently published estimates of the proportion of the United States population who are men who have sex with men (MSM), who comprise the majority of persons with HIV, as well as persons at risk for HIV due to injection-drug use or heterosexual contact (4–6). In addition, data on HIV diagnoses are now available from all 50 states and the District of Columbia. This analysis presents lifetime and age-conditional risk estimates using data from 2009–2013 by race/ethnicity, sex, and risk group as well as state-level lifetime risk estimates.
METHODS
Age-specific HIV diagnosis, mortality, and population data were used to derive lifetime and age-specific risk estimates of receiving a diagnosis of HIV infection. Data on HIV diagnoses were obtained from the Centers for Disease Control and Prevention’s (CDC) National HIV Surveillance System (NHSS). Since the early 1980s, cases of stage 3 (AIDS) HIV infection have been reported to NHSS by all states, the District of Columbia, and U.S. dependent areas. In 1994, CDC implemented a uniform system for national, integrated HIV and AIDS surveillance, and over time as jurisdictions implemented confidential, name-based HIV reporting their data was reported to NHSS. By 2008, all 50 states and the District of Columbia (D.C.) were reporting cases of HIV infection to NHSS. To determine the number of HIV diagnoses, we used data for the most recent 5-years available (2010–2014) from the 50 states and D.C. The year of HIV diagnosis was based on the earliest reported date of diagnosis.
General and HIV-specific mortality data were obtained from information on death certificates reported to CDC’s National Centers for Health Statistics for the 50 states and D.C. The most recent NCHS mortality data available were for the year of 2014. Population data were obtained from the Vintage 2014 postcensal estimates file (for years 2010–2014) from the U.S. Census Bureau (7). Our final data consisted of HIV diagnosis data, general and HIV-specific mortality data, and population data from the 50 states and DC between 2010 and 2014.
The numbers of HIV diagnoses and non-HIV deaths between 2010 and 2014 were determined for each single-year age group. The numbers of HIV diagnoses were adjusted for missing transmission category (8). The HIV diagnosis and non-HIV death rates were derived by dividing the HIV diagnoses and non-HIV death counts at each age by the population denominator for that age. These rates were converted to probabilities of a diagnosis of HIV at a given age, conditional on never having acquired HIV prior to that age using a competing risks method, i.e. dying before acquiring an HIV infection (9, 10). The competing risks were assumed to be independent of the event of interest, i.e., HIV diagnosis. The probabilities were applied to a hypothetical cohort of 10 million live births and estimates were derived for each age in the hypothetical cohort of the number alive and HIV-free at the beginning of the interval; the number of newly diagnosed HIV cases in the interval; the number of non-HIV deaths in the interval among the HIV-free population; and the cumulative probability of receiving a diagnosis of HIV infection from birth. The lifetime risk estimate is the cumulative probability of receiving a diagnosis of HIV from birth. The inverse of lifetime risk renders an estimate for the number of persons who would need to be followed throughout the specified life years to observe one HIV diagnosis (reported as 1 in n). Age-conditional risks of receiving an HIV diagnosis were also computed. Age-conditional risk measures were the probabilities of an individual of a specified age receiving a diagnosis of HIV infection within a certain number of years, such as the risk of a diagnosis of HIV in the next 10 years among those alive and HIV-free at age 30. Compared to lifetime risk estimates, age-conditional risk estimates are less restricted by long-term extrapolation of the current rates, and they provide information for specific ages. Confidence intervals (CI) were estimated using a generalized gamma method originally developed for linear combinations of independent Poisson random variables (9). The lifetime risk estimates and age-conditional risk estimates were calculated for the entire population, as well as each combination of sex, race/ethnicity, and HIV-risk group. The lifetime risk estimates were also calculated for each state. All the calculations were conducted in DevCan 6.7.3 software (10), developed by the National Cancer Institute.
The estimates for risk groups, MSM, people who inject drugs (PWID) and heterosexuals, required further assumptions because this information is not noted in the census or mortality data. We used previously published estimates of the population proportions for these three risk groups, and applied them to the census and mortality data (4–6, 11). For example, an estimated 6.55% of the male population are MSM (6.9% MSM (6) – 0.35% MSM/PWID (11)). This percent was applied to the adult male population in the census data and any-cause mortality data, but we also needed the proportion of deaths among people with HIV attributed to each risk group. We obtained this proportion from the NHSS data (2010–2014) and applied this percent to the deaths with any mention of HIV on the death certificate (HIV deaths) in the mortality data. The number of HIV deaths was then subtracted from the total number of deaths in each risk group to get the number of non-HIV deaths for each age.
For each age:
A = # of all deaths in mortality dataset
P = population proportion for risk group based on published estimates (4–6, 11)
B = # of deaths among persons with HIV in the risk group, NHSS data
C = # of all deaths among persons with HIV, NHSS data
D = # of HIV deaths in mortality dataset
The P was based on the published age-group estimates regardless of race or ethnicity. In addition, lifetime risk by risk group was based on following a cohort of people from age 13 instead of from birth.
RESULTS
In the United States, 207,229 people with HIV were diagnosed during 2010–2014. Overall, the lifetime risk of a diagnosis of HIV was 0.95% (95% CI: 0.94–0.95). This means that to observe one HIV diagnosis, 106 (95% CI: 105–106) infants would need to be followed over a lifetime, assuming that the 2010–2014 HIV diagnosis and death rates remain constant over their lifetime.
The lifetime risk for males and females was 1 in 68 and 1 in 253, respectively (Table 1). Among both males and females, blacks had the highest lifetime risk (males: 1 in 22; females: 1 in 54). The lifetime risk among Hispanic/Latino males was 1 in 51 and, among Hispanic/Latino females, it was 1 in 256. Among males and females, the lowest risk was among Asians (males: 1 in 176; females: 1 in 943).
Table 1.
Lifetime Risk of HIV Diagnosis, by Sex, Race/Ethnicity, and Risk Group, United States.
| Males | Females | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Probability X 100 | 95% CI | “One in n” | 95% CI | No. Cases* | Probability X 100 | 95% CI | “One in n” | 95% CI | No. Cases* | |
| Totala | 1.48 | 1.47–1.49 | 68 | 67–68 | 164,456 | 0.40 | 0.39–0.40 | 253 | 250–255 | 42,773 |
| Race/Ethnicitya | ||||||||||
| American Indian/Alaska Native | 0.77 | 0.71–0.84 | 131 | 120–141 | 663 | 0.25 | 0.22–0.29 | 403 | 342–464 | 206 |
| Asian | 0.57 | 0.55–0.59 | 176 | 169–182 | 3,366 | 0.11 | 0.10–0.12 | 943 | 859–1,021 | 663 |
| Black/African American | 4.58 | 4.54–4.61 | 22 | 22–22 | 66,848 | 1.86 | 1.84–1.88 | 54 | 53–55 | 27,045 |
| Hispanic/Latino | 1.97 | 1.94–1.99 | 51 | 50–51 | 38,910 | 0.39 | 0.38–0.40 | 256 | 249–263 | 6,432 |
| Native Hawaiian/other Pacific Islander | 1.05 | 0.91–1.66 | 95 | 60–110 | 219 | 0.23 | 0.17–0.65 | 432 | 153–600 | 43 |
| White | 0.71 | 0.71–0.72 | 140 | 139–141 | 48,811 | 0.11 | 0.10–0.11 | 941 | 919–963 | 7,027 |
| Risk groupb | ||||||||||
| MSM | 16.7 | 16.6–16.8 | 6 | 6–6 | 131,100 | – | – | – | – | – |
| American Indian/Alaska Native | 8.28 | 7.58–9.16 | 12 | 11–13 | 482 | – | – | – | – | – |
| Asian | 7.21 | 6.96–7.50 | 14 | 13–14 | 2,910 | – | – | – | – | – |
| Black/African American | 41.1 | 40.8–41.3 | 2 | 2–2 | 49,538 | – | – | – | – | – |
| Hispanic/Latino | 21.6 | 21.4–21.9 | 5 | 5–5 | 32,029 | – | – | – | – | – |
| Native Hawaiian/other Pacific Islander | 13.2 | 11.5–20.8 | 8 | 5–9 | 191 | – | – | – | – | – |
| White | 8.94 | 8.86–9.02 | 11 | 11–11 | 41,378 | – | – | – | – | – |
| PWID | 2.37 | 2.31–2.42 | 42 | 41–43 | 8,019 | 3.82 | 3.72–3.92 | 26 | 26–27 | 5,770 |
| American Indian/Alaska Native | 2.06 | 1.54–3.09 | 49 | 32–65 | 58 | 5.28 | 4.05–7.57 | 19 | 13–25 | 61 |
| Asian | 0.51 | 0.41–0.73 | 196 | 138–246 | 94 | 0.46 | 0.33–0.89 | 215 | 112–304 | 42 |
| Black/African American | 8.95 | 8.66–9.25 | 11 | 11–12 | 3,663 | 13.5 | 13.0–14.0 | 7 | 7–8 | 2,703 |
| Hispanic/Latino | 3.91 | 3.72–4.14 | 26 | 24–27 | 2,017 | 3.93 | 3.64–4.29 | 25 | 23–27 | 873 |
| Native Hawaiian/other Pacific Islander | 1.55 | 0.69–18.2 | 65 | 5–146 | 10 | 0.37 | 0.01–25.8 | 269 | 4–10,359 | 2 |
| White | 0.92 | 0.88–0.97 | 108 | 103–114 | 1,954 | 2.02 | 1.93–2.12 | 49 | 47–52 | 1,853 |
| Heterosexual | 0.19 | 0.19–0.19 | 524 | 516–532 | 17,839 | 0.38 | 0.37–0.38 | 266 | 263–269 | 36,235 |
| American Indian/Alaska Native | 0.09 | 0.07–0.12 | 1,175 | 809–1,545 | 63 | 0.19 | 0.16–0.24 | 517 | 424–613 | 142 |
| Asian | 0.05 | 0.05–0.06 | 1,860 | 1,567–2,126 | 254 | 0.10 | 0.10–0.11 | 971 | 879–1,058 | 584 |
| Black/African American | 1.03 | 1.01–1.05 | 97 | 95–99 | 11,566 | 1.84 | 1.82–1.86 | 54 | 54–55 | 23,849 |
| Hispanic/Latino | 0.23 | 0.22–0.24 | 437 | 418–455 | 3,241 | 0.37 | 0.36–0.38 | 272 | 263–280 | 5,482 |
| Native Hawaiian/other Pacific Islander | 0.03 | 0.01–0.80 | 3,310 | 125–14,579 | 5 | 0.24 | 0.17–0.69 | 414 | 146–582 | 38 |
| White | 0.04 | 0.04–0.04 | 2,713 | 2,601–2,830 | 2,259 | 0.09 | 0.08–0.09 | 1,166 | 1,134–1,199 | 5,061 |
CI, confidence interval; MSM, men who have sex with men; PWID, people who inject drugs
HIV cases diagnosed in 2010–2014
lifetime risk from birth;
lifetime risk from age 13 years
The risk group with the highest lifetime risk was MSM (1 in 6) with black MSM (1 in 2) and Hispanic/Latino MSM (1 in 5) having a higher risk than white MSM (1 in 11; Table 1). Female PWID (1 in 26) had a higher lifetime risk than male PWID (1 in 43) as did heterosexual females (1 in 266) compared to heterosexual males (1 in 524). Within each risk group blacks had the highest lifetime risk.
By state, the lifetime risk ranged from 1 in 674 in Montana to 1 in 17 in the District of Columbia. (Table 2). The states with the highest lifetime risks were Maryland (1 in 56), Georgia (1 in 57), Florida (1 in 58), and Louisiana (1 in 58).
Table 2.
Lifetime Risk of HIV Diagnosis, by State, United States.
| Probability X 100 | 95% CI | “One in n” | 95% CI | No. Cases* | |
|---|---|---|---|---|---|
| Alabama | 0.99 | 0.96–1.03 | 101 | 97–104 | 3,355 |
| Alaska | 0.29 | 0.24–0.35 | 347 | 283–410 | 154 |
| Arizona | 0.74 | 0.71–0.76 | 136 | 131–141 | 3,286 |
| Arkansas | 0.64 | 0.60–0.67 | 157 | 149–166 | 1,289 |
| California | 0.93 | 0.92–0.94 | 107 | 106–109 | 25,357 |
| Colorado | 0.51 | 0.48–0.53 | 197 | 188–206 | 1,884 |
| Connecticut | 0.68 | 0.65–0.72 | 146 | 139–154 | 1,660 |
| Delaware | 0.95 | 0.88–1.03 | 105 | 97–114 | 604 |
| District of Columbia | 5.94 | 5.73–6.16 | 17 | 16–17 | 3,010 |
| Florida | 1.74 | 1.72–1.76 | 58 | 57–58 | 22,860 |
| Georgia | 1.76 | 1.73–1.79 | 57 | 56–58 | 12,513 |
| Hawaii | 0.49 | 0.45–0.54 | 203 | 185–223 | 472 |
| Idaho | 0.15 | 0.13–0.18 | 648 | 551–760 | 164 |
| Illinois | 0.91 | 0.89–0.93 | 110 | 108–113 | 8,167 |
| Indiana | 0.53 | 0.51–0.55 | 188 | 181–196 | 2,403 |
| Iowa | 0.28 | 0.25–0.30 | 364 | 335–396 | 565 |
| Kansas | 0.37 | 0.34–0.40 | 272 | 252–293 | 719 |
| Kentucky | 0.57 | 0.54–0.60 | 176 | 168–185 | 1,733 |
| Louisiana | 1.73 | 1.68–1.77 | 58 | 56–59 | 5,734 |
| Maine | 0.27 | 0.24–0.31 | 370 | 325–422 | 242 |
| Maryland | 1.78 | 1.74–1.82 | 56 | 55–58 | 7,410 |
| Massachusetts | 0.74 | 0.72–0.77 | 135 | 131–140 | 3,454 |
| Michigan | 0.58 | 0.56–0.60 | 172 | 167–178 | 3,900 |
| Minnesota | 0.43 | 0.41–0.46 | 231 | 220–243 | 1,588 |
| Mississippi | 1.14 | 1.09–1.18 | 88 | 85–92 | 2,397 |
| Missouri | 0.62 | 0.60–0.65 | 161 | 155–167 | 2,584 |
| Montana | 0.15 | 0.12–0.18 | 674 | 547–831 | 98 |
| Nebraska | 0.36 | 0.33–0.39 | 280 | 255–308 | 449 |
| Nevada | 1.02 | 0.98–1.07 | 98 | 93–102 | 2,004 |
| New Hampshire | 0.24 | 0.21–0.28 | 417 | 362–480 | 216 |
| New Jersey | 1.05 | 1.02–1.07 | 96 | 93–98 | 6,352 |
| New Mexico | 0.48 | 0.45–0.52 | 208 | 192–224 | 684 |
| New York | 1.33 | 1.31–1.35 | 75 | 74–76 | 18,453 |
| North Carolina | 1.00 | 0.98–1.02 | 100 | 98–102 | 6,836 |
| North Dakota | 0.15 | 0.12–0.19 | 655 | 515–833 | 77 |
| Ohio | 0.64 | 0.63–0.66 | 155 | 151–160 | 5,052 |
| Oklahoma | 0.57 | 0.55–0.60 | 174 | 166–183 | 1,536 |
| Oregon | 0.45 | 0.43–0.48 | 221 | 209–234 | 1,215 |
| Pennsylvania | 0.79 | 0.78–0.81 | 126 | 123–129 | 6,917 |
| Rhode Island | 0.68 | 0.62–0.74 | 148 | 135–162 | 485 |
| South Carolina | 1.12 | 1.08–1.15 | 90 | 87–93 | 3,703 |
| South Dakota | 0.26 | 0.21–0.30 | 393 | 331–467 | 140 |
| Tennessee | 0.91 | 0.88–0.94 | 110 | 107–113 | 4,104 |
| Texas | 1.18 | 1.16–1.19 | 85 | 84–86 | 21,867 |
| Utah | 0.27 | 0.24–0.29 | 374 | 341–409 | 527 |
| Vermont | 0.19 | 0.15–0.24 | 534 | 423–676 | 80 |
| Virginia | 0.83 | 0.80–0.85 | 121 | 118–125 | 4,816 |
| Washington | 0.50 | 0.49–0.53 | 198 | 190–206 | 2,446 |
| West Virginia | 0.33 | 0.30–0.36 | 307 | 278–339 | 409 |
| Wisconsin | 0.30 | 0.29–0.32 | 329 | 311–349 | 1,187 |
| Wyoming | 0.18 | 0.14–0.23 | 556 | 430–711 | 72 |
| Total | 0.95 | 0.94–0.95 | 106 | 105–106 | 207,229 |
CI, confidence interval;
HIV cases diagnosed in 2010–2014
Table 3 presents the 10-year age-conditional risks of an HIV diagnosis among HIV-free males and females for select ages. These numbers indicate how many people would need to be followed for the next 10 years to observe one HIV diagnosis among those who are HIV-free at a specific age. Among males, those aged 20 years had the highest risk of an infection in the next 10 years (1 in 192). This was true for black, Hispanic/Latino, and white males (Table 3). Among females, the highest risk was at age 30 (1 in 952). By race/ethnicity, the risk among white and black females was highest at age 30 while the risk among Hispanic/Latino females was highest at age 40. Among MSM, risk was highest at age 20 and risk decreased with age. The opposite pattern was true among male PWID; the risk increased with age with the highest risk at age 50. Female PWID had the lowest 10-year risk at age 40. The highest risk among male heterosexuals was at age 40, and, among female heterosexuals, it was at age 20.
Table 3.
10-year Age-Conditional Risk (1 in n) of HIV Diagnosis among HIV-Free Males and Females, Aged 20–50 Years, United States.
| 20 | 30 | 40 | 50 | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| “One in n” | 95% CI | “One in n” | 95% CI | “One in n” | 95% CI | “One in n” | 95% CI | |
| Males | ||||||||
| Total | 192 | 191–194 | 269 | 266–272 | 319 | 316–322 | 580 | 572–588 |
| MSM | 15 | 14–15 | 22 | 22–23 | 29 | 28–29 | 59 | 58–60 |
| PWID | 220 | 207–234 | 207 | 197–217 | 173 | 167–180 | 167 | 160–174 |
| Heterosexual | 3,318 | 3,197–3,444 | 2,252 | 2,185–2,322 | 1,868 | 1,819–1,920 | 2,527 | 2,450–2,607 |
| Black/African American | 55 | 54–55 | 101 | 99–102 | 116 | 114–118 | 173 | 170–177 |
| MSM | 4 | 4–5 | 9 | 9–10 | 13 | 13–14 | 26 | 25–27 |
| PWID | 77 | 69–85 | 72 | 66–78 | 48 | 46–51 | 33 | 32–35 |
| Heterosexual | 665 | 636–696 | 453 | 436–471 | 345 | 334–357 | 422 | 406–438 |
| Hispanic/Latino | 168 | 165–171 | 189 | 185–192 | 232 | 227–237 | 405 | 391–419 |
| MSM | 13 | 12–13 | 16 | 15–16 | 20 | 20–21 | 40 | 38–42 |
| PWID | 174 | 154–196 | 131 | 121–142 | 106 | 98–114 | 102 | 92–112 |
| Heterosexual | 3,632 | 3,339–3,957 | 1,889 | 1,778–2,008 | 1,745 | 1,636–1,863 | 2,096 | 1,925–2,285 |
| White | 508 | 499–516 | 513 | 504–522 | 534 | 525–543 | 998 | 977–1,020 |
| MSM | 39 | 38–39 | 40 | 39–41 | 42 | 41–42 | 79 | 77–81 |
| PWID | 429 | 382–484 | 457 | 417–502 | 435 | 402–472 | 548 | 501–601 |
| Heterosexual | 19,176 | 17,041–21,643 | 13,501 | 12,253–14,912 | 9,150 | 8,492–9,871 | 12,105 | 11,174–13,135 |
| Females | ||||||||
| Total | 1,092 | 1,071–1,113 | 952 | 934–970 | 1,081 | 1,060–1,102 | 1,613 | 1,576–1,650 |
| PWID | 108 | 102–114 | 113 | 107–119 | 137 | 130–143 | 112 | 106–119 |
| Heterosexual | 1,025 | 1,004–1,047 | 1,035 | 1,015–1,056 | 1,202 | 1,177–1,227 | 1,819 | 1,773–1,865 |
| Black/African American | 247 | 242–254 | 206 | 201–211 | 227 | 221–232 | 310 | 301–319 |
| PWID | 40 | 37–44 | 38 | 35–41 | 37 | 35–40 | 25 | 23–27 |
| Heterosexual | 222 | 217–228 | 214 | 208–219 | 241 | 235–248 | 340 | 329–351 |
| Hispanic/Latino | 1,405 | 1,337–1,477 | 1,176 | 1,123–1,233 | 1,120 | 1,066–1,177 | 1,273 | 1,196–1,355 |
| PWID | 127 | 111–148 | 136 | 119–156 | 142 | 125–161 | 97 | 83–114 |
| Heterosexual | 1,341 | 1,271–1,415 | 1,282 | 1,220–1,348 | 1,240 | 1,175–1,310 | 1,410 | 1,318–1,510 |
| White | 3,715 | 3,544–3,896 | 3,375 | 3,223–3,536 | 3,926 | 3,749–4,114 | 6,565 | 6,213–6,942 |
| PWID | 155 | 141–170 | 178 | 162–195 | 274 | 252–299 | 298 | 268–333 |
| Heterosexual | 4,202 | 3,974–4,446 | 4,442 | 4,207–4,693 | 5,151 | 4,877–5,445 | 8,337 | 7,817–8,901 |
CI, confidence interval; MSM, men who have sex with men; PWID, people who inject drugs.
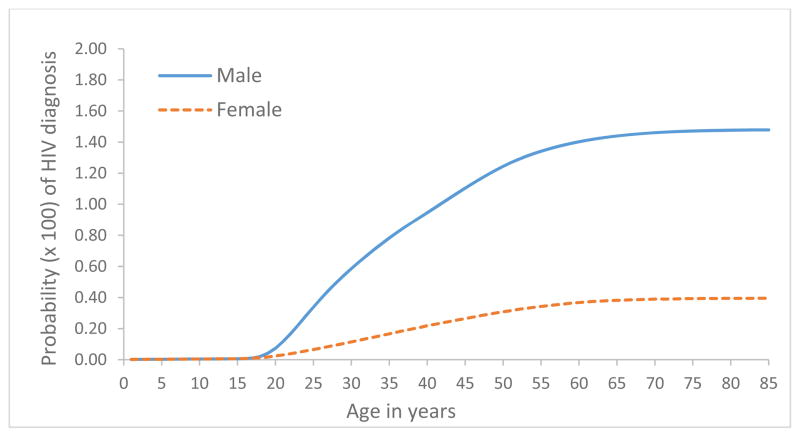
Lifetime risk increases with age (Figure 1), although most of the risk is accumulated before age 50 (risk by age 50, 1.24% for males and 0.31% for females). For males this represents 84% of their lifetime risk and, for females, it is 78% of their risk.
Figure 1.
Lifetime risk of HIV diagnosis, by age and sex, United States.
DISCUSSION
Overall, the lifetime risk of HIV diagnosis was 0.95%, which was a 26% decrease from the previous estimate based on data from 2004–2005 (1.29%) (3). The risk decreased among both males (21%) and females (44%). There was also a decrease in lifetime risk among all race/ethnicities, but severe disparities still persisted. Among males, the lifetime risk among blacks was more than six times the risk among whites and the risk among Hispanics/Latinos was nearly three times the risk of whites. The risk among black females was 17 times the risk of white females, and the risk among Hispanic/Latino females was more than three times the risk for white females. Lifetime risk for MSM and male PWID were 88 and 12 times the risk for male heterosexuals, respectively.
Another shift from previous estimates was the age at highest risk among males. The 2004–2005 estimates showed the highest risk of being diagnosed in the next ten years was among 35 year olds (3). Our estimates now show the highest risk at 20 years old. This could be the result of increases in diagnoses among young MSM and decreases among older MSM (12). Among females, the highest risk of being diagnosed in the next ten years was at age 30 years, which is the same as the previous estimate (3). It should be kept in mind when comparing the current estimates to the previous estimates (2004–2005) that the previous estimates were only based on data from 33 jurisdictions, which accounted for 63% of diagnoses, so the previous estimates may have been an over or underestimate of the actual risk.
This paper also reports lifetime risk by state for the first time, which allows states to communicate about HIV risk at the local level. There was a wide range in estimates of lifetime risk by state. The states with the highest lifetime risk were all in the South, which accounts for the highest morbidity of HIV in the United States (2). The area with the highest risk was the District of Columbia (1 in 17). However, the District of Columbia is a city, so comparisons to states should be made with caution. The majority of persons with HIV diagnosed in a year live in metropolitan statistical areas (2).
Another new element of this paper is the lifetime risk by risk group, which is now possible because of published population size estimates for these groups (4–6). This allows us to better describe the risk among groups such as MSM and PWID. The lifetime risk was very high among MSM, and, in particular, black MSM with a probability of a diagnosis in their lifetime at 41%. This result is lower than a previous analysis in which the estimated HIV prevalence among a cohort of young, black MSM was 61% by age 40 (13). The estimated prevalence among all MSM in an earlier analysis was 41% (14), which is much higher than our estimated probability of a diagnosis (17%). However, both of these previous analyses were based on meta-analyses of several studies including community-based studies and studies conducted at HIV testing sites and STD clinics (13, 14), which may represent a higher risk population. MSM comprise about 78% of men infected with HIV each year (12) and have a very high rate of receiving a diagnosis of HIV infection compared to males in other risk groups: 672 per 100,000 (6) compared to 49 per 100,000 male PWID (4) and 3.6 per 100,000 male heterosexuals (5).
Our analysis is subject to some limitations. First, it is based on diagnosis data, not incidence. Therefore, our estimates are for receiving a diagnosis of HIV, not acquiring a new HIV infection, which can occur years before the diagnosis. While incidence estimates are now available for the United States, they rely on extrapolation from areas with incidence surveillance and incidence estimates are not available for individual states. On the other hand, reliable data on HIV diagnoses are available and estimates are based on data reported by all 50 states and the District of Columbia. In addition, the death certificate data may not have been accurate for all deaths. In particular, HIV may have been omitted from some death certificates of people with diagnosed HIV. Additionally, risk group estimates of lifetime risk are based on estimates of population size. If these estimates are an under or over estimate of the population size, the lifetime risk estimate would also be over or under estimated, respectively. It should also be noted that due to rounding, the 1 in n number can reflect a wide range of probabilities among groups with a high prevalence of infection (e.g., the 1 in 2 lifetime risk among black MSM reflects a probability of 0.41, but it could be reflective of a probability as low as .41 and as high as .66). Lastly, some sub-groups had a small number of HIV diagnoses, such as Native Hawaiian/other Pacific Islander PWID, resulting in wide confidence intervals, so their lifetime risk estimates should be interpreted with caution.
One key caveat of this analysis is that it assumes no change in trend over a person’s lifetime from the 2010–2014 levels, but trends in HIV diagnosis have changed, so these numbers should be updated regularly. It should be noted that these are projections based on rates during 2010–2014 and do not account for cohort effects or changes in diagnosis rates over time. They serve as a method to communicate the level of risk currently being experienced in different communities, and are not a guarantee of what will occur in the future. Lifetime risk has decreased from previous estimates, in part due to prevention efforts such as, prevention of mother-to-child transmission and highly-active antiretroviral therapy. Through continued prevention efforts, including Treatment as Prevention and pre-exposure prophylaxis (PrEP), these rates will hopefully continue to change, resulting in a lower realized lifetime risk. In addition, it is important to monitor disparities to ensure that prevention efforts reduce risk in all groups.
In summary, an estimated 1 in 106 people living in the United States have received or will receive a diagnosis of HIV infection during their lifetime. The risk of an HIV diagnosis among MSM is nearly 88 times the risk among male heterosexuals, and black MSM have 5 times the risk of white MSM. Among females, the risk among blacks was 17 times that among whites, and this disparity was higher (20 times) among heterosexual females. The National HIV/ADS Strategy: Updated to 2020 calls for intensifying HIV prevention efforts in communities where HIV is most heavily concentrated by allocating public funding consistent with the geographic distribution of HIV and focusing on high-risk populations (15). The Strategy also seeks to reduce HIV-related disparities in communities at high risk for HIV infection. These data on lifetime risk can help describe the burden of HIV by state and by population, helping to inform programs and policies that target resources to those at highest risk. In addition, the lifetime risk information can be used in communications to the public, as the Strategy calls for clear, specific, consistent, and scientifically up-to-date messages about HIV risks and prevention strategies be provided to educate all Americans about HIV risks, prevention, and transmission.
While lifetime risk based on data from 2010–2014 has decreased compared to earlier estimates using data from 2004–2005, continued improvements in prevention and care are needed so risk will continue to decline further. CDC’s approach to reducing HIV infections in the United States calls for high-impact prevention through a combination of interventions that are scientifically proven, cost-effective, and scalable (16). These include early diagnosis, prompt linkage to antiretroviral treatment, PrEP, condoms, and services for persons who inject drugs (17). CDC has increased its efforts in groups with the highest diagnosis rates, such as MSM, blacks/African Americans, and the South, with increased funding to health departments and community-based organizations that provide prevention interventions. The availability of lifetime risk estimates to be used by clinicians, outreach workers, and policy makers to more clearly communicate to the general public will hopefully aide efforts in reducing the incidence of HIV and decreasing disparities.
Acknowledgments
Sources of support: All work was supported by the Centers for Disease Control and Prevention.
List of abbreviations and acronyms
- HIV
human immunodeficiency virus
- MSM
men who have sex with men
- CDC
Centers for Disease Control and Prevention
- NHSS
National HIV Surveillance System
- AIDS
acquired immunodeficiency syndrome
- DC
District of Columbia
- CI
confidence interval
- PWID
people who inject drugs
- PrEP
pre-exposure prophylaxis
Footnotes
The authors have no conflicts of interest to report.
Portions of these results were presented at: Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Estimating the lifetime risk of a diagnosis of HIV infection in the United States. Oral presentation at CROI 2016, Boston, MA, February 22–25, 2016.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data - United States and 6 dependent areas - 2013. HIV Surveillance Supplemental Report [Internet] 2015. 2015 Sep 25;20(2) Available from: http://www.cdc.gov/hiv/library/reports/surveillance. [Google Scholar]
- 2.CDC. Diagnosis of HIV infection in the United States and dependent areas, 2013. HIV Surveillance Report [Internet] 2015. 2015 Sep 25;25 Available from: http://cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- 3.Hall HI, An Q, Hutchinson AB, Sansom S. Estimating the lifetime risk of a diagnosis of the HIV infection in 33 states, 2004–2005. Journal of acquired immune deficiency syndromes. 2008;49(3):294–7. doi: 10.1097/QAI.0b013e3181893f17. [DOI] [PubMed] [Google Scholar]
- 4.Lansky A, Finlayson T, Johnson C, Holtzman D, Wejnert C, Mitsch A, et al. Estimating the number of persons who inject drugs in the united states by meta-analysis to calculate national rates of HIV and hepatitis C virus infections. PloS one. 2014;9(5):e97596. doi: 10.1371/journal.pone.0097596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lansky A, Johnson C, Oraka E, Sionean C, Joyce MP, DiNenno E, et al. Estimating the number of heterosexual persons in the United States to calculate national rates of HIV infection. PloS one. 2015;10(7):e0133543. doi: 10.1371/journal.pone.0133543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. The open AIDS journal. 2012;6:98–107. doi: 10.2174/1874613601206010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bureau USC. Population estimates [entire data set] Available from: http://www.census.gov/popest/data/
- 8.Harrison KM, Kajese T, Hall HI, Song R. Risk factor redistribution of the national HIV/AIDS surveillance data: an alternative approach. Public Health Rep. 2008;123(5):618–27. doi: 10.1177/003335490812300512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fay MP, Pfeiffer R, Cronin KA, Le C, Feuer EJ. Age-conditional probabilities of developing cancer. Statistics in medicine. 2003;22(11):1837–48. doi: 10.1002/sim.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DevCan: Probability of developing or dying of cancer software, version 6.7.3. Statistical Research and Applications Branch, National Cancer Institute; Statistical Research and Applications Branch, National Cancer Institute; 2015. Available from: http://srab.cancer.gov/devcan. [Google Scholar]
- 11.Centers for Disease C, Prevention. Estimated percentages and characteristics of men who have sex with men and use injection drugs--United States, 1999–2011. MMWR Morbidity and mortality weekly report. 2013;62(37):757–62. [PMC free article] [PubMed] [Google Scholar]
- 12.CDC. Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report [Internet] 2012. 2015 Sep 29;17(4) Available from: http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. [Google Scholar]
- 13.Matthews DD, Herrick AL, Coulter RW, Friedman MR, Mills TC, Eaton LA, et al. Running Backwards: Consequences of Current HIV Incidence Rates for the Next Generation of Black MSM in the United States. AIDS and behavior. 2016;20(1):7–16. doi: 10.1007/s10461-015-1158-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stall R, Duran L, Wisniewski SR, Friedman MS, Marshal MP, McFarland W, et al. Running in place: implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS and behavior. 2009;13(4):615–29. doi: 10.1007/s10461-008-9509-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 20202015. 2015 Nov 25; Available from: https://www.whitehouse.gov/sites/default/files/docs/national_hiv_aids_strategy_update_2020.pdf.
- 16.CDC. High-impact HIV prevention 2012. 2015 Oct 5; Available from: http://www.cdc.gov/hiv/strategy/dhap/pdf/nhas_booklet.pdf.
- 17.Centers for Disease C, Prevention. Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: summary guidance from CDC and the U.S. Department of Health and Human Services. MMWR Recomm Rep. 2012;61(RR-5):1–40. [PubMed] [Google Scholar]