Abstract
Background:
All–soft tissue suture anchors provide advantages of decreased removal of bone and decreased glenoid volume occupied compared with traditional tap or screw-in suture anchors. Previous published data have led to biomechanical concerns with the use of first-generation all-soft suture anchors.
Purpose/Hypothesis:
The purpose of this study was to evaluate the load to 2-mm displacement and ultimate load to failure of a second-generation all-soft suture anchor, compared with a first-generation anchor and a traditional PEEK (polyether ether ketone) anchor. The null hypothesis was that the newer second-generation anchor will demonstrate no difference in loads to 2-mm displacement after cycling compared with first-generation all-soft suture anchors.
Study Design:
Controlled laboratory study.
Methods:
Twenty human cadaveric glenoids were utilized to create 97 total suture anchor sites, and 1 of 3 anchors were randomized and placed into each site: (1) first-generation all-soft suture anchor (Juggerknot; Biomet), (2) second-generation all-soft suture anchor (Suturefix; Smith & Nephew), and (3) a control PEEK anchor (Bioraptor; Smith & Nephew). After initial cyclic loading, load to 2 mm of displacement and ultimate load to failure were measured for each anchor.
Results:
After cyclic loading, the load to 2-mm displacement was significantly less in first-generation anchors compared with controls (P < .01). However, the load to 2-mm displacement was significantly greater in second-generation anchors compared with controls (P < .01). There was no difference in ultimate load to failure between the first- and second-generation all-soft suture anchors (P > .05).
Conclusion:
The newer generation all-soft suture anchors with a theoretically more rigid construct and deployment configuration demonstrate biomechanical characteristics (specifically, with load to 2-mm displacement after cyclic loading) that are improved over first-generation all-soft suture anchors and similar to a traditional solid tap-in anchor. The configuration of these newer generation all-soft suture anchors appears to mitigate the biomechanical concerns of decreased load to failure with first-generation all–soft tissue suture anchors.
Clinical Relevance:
The theoretical advantages of all-soft anchors may be particularly valuable in revision surgery or in cases where multiple anchors are being placed into a small anatomic area.
Keywords: glenoid, all-suture, all-soft, anchor, labrum
The advancement of arthroscopic techniques and tissue anchors has been an integral part of the improved outcomes that have allowed the rise in popularity of arthroscopic glenohumeral stabilization.2,21,28,29 The gold standard for fixation of the glenoid labrum to bone has been a solid suture anchor.8,22,23 Metal, bioabsorbable/biocomposite, and nonresorbable polymer anchors are well studied and have all demonstrated acceptable load-to-failure properties.5,22,31 Concerns utilizing these anchors include fatigue fracture, anchor loosening, chondral damage, cystic resorption, incomplete resorption, osteolysis, revision drilling, and difficulties obtaining subsequent magnetic resonance imaging.4,12–16,18,24,25,30
Novel all-soft suture anchors were developed to help mitigate some of these challenges; features include the removal of lower volume of glenoid bone stock during placement of this anchor and less volume of bone occupied by the anchor.12,20 This may be particularly helpful in revision situations or when a large number of anchors need to be placed, such as in panlabral repairs.1,9 The first generation of these suture anchors, such as the Biomet Juggerknot, the Arthrex FiberTak, the Linvatec Y-knot, and the Stryker Iconix, all obtain fixation via a simple insertion device that requires the sutures to be pulled back to the cortical bone for deployment to increase their surface area and increase the required force for pullout. Recent data suggest that some first-generation all-soft suture anchors, namely the Biomet Juggerknot, may have inferior biomechanical properties in terms of submaximal displacement after cyclic loading compared with all-solid anchors,20,26 causing concern about the utilization of this new technology despite the potential advantages.
Second-generation anchors have reconfigured deployment mechanisms that may help mitigate these biomechanical concerns. These anchors, such as the Smith & Nephew Suturefix, the Smith & Nephew Q-fix, and the Cayenne Medical Surelock, use insertion devices that do not require manual tensioning for deployment of the anchor, which theoretically should reduce partial deployments or accidental anchor pullout from overtensioning. There is tactile feedback in the form of a “click” so the user is sure that the anchor has deployed, and the deployment mechanism utilizes the steel inserter, not the bone itself, to form the appropriate anchor conformation in this second-generation model. It may decrease micromotion from increased cavity size created by setting the first-generation anchors.26
Our purpose in this study was to evaluate the biomechanics of a first-generation all-soft suture anchor (Biomet Juggerknot) along with a newer second-generation model (Smith & Nephew Suturefix) compared with a traditional tap-in solid anchor control (Smith & Nephew Bioraptor) in a human cadaveric model. Our null hypothesis was that the newer second-generation all-soft suture anchor will demonstrate no difference in loads to 2-mm displacement after cyclic loading compared with first-generation all-soft suture anchors.
Methods
Specimens
Cadaveric specimens were purchased through the Surgical Research Laboratory of our institution. Ten matched-pair cadaveric shoulders (20 specimens total) were thawed, and all soft tissue attachments, including capsule and labrum, were carefully removed. Demographic data for the specimens are presented in Table 1. Bone density of the matched-pair humeri was established in a prior study17 by dual-energy x-ray absorptiometry and was used in this study to approximate the bone density of the matched glenoid specimen. The specimens were cut approximately 2.25 inches medial to the glenoid. Two 2-inch drywall screws were inserted into the medial border of the cut scapular specimen. The specimens were then potted in bone cement. After potting, the specimens were re-stored at −20°C. Prior to anchor insertion and testing, the specimens were thawed overnight at room temperature.
TABLE 1.
Demographic Data
| Specimen Pair Number | Age, y | Sex | Side (Right/Left) | Bone Mineral Density, g/cm3 |
|---|---|---|---|---|
| 1 | 93 | Female | Right | 0.435 |
| Left | 0.485 | |||
| 2 | 64 | Male | Right | 0.573 |
| Left | 0.514 | |||
| 3 | 76 | Female | Right | 0.644 |
| Left | 0.619 | |||
| 4 | 70 | Male | Right | 0.561 |
| Left | 0.520 | |||
| 5 | 85 | Female | Right | 0.430 |
| Left | 0.407 | |||
| 6 | 42 | Female | Right | 0.607 |
| Left | 0.571 | |||
| 7 | 81 | Male | Right | 0.614 |
| Left | 0.590 | |||
| 8 | 74 | Male | Right | 0.794 |
| Left | 0.799 | |||
| 9 | 89 | Male | Right | 0.674 |
| Left | 0.645 | |||
| 10 | 70 | Female | Right | 0.668 |
| Left | 0.661 |
Anchor Application
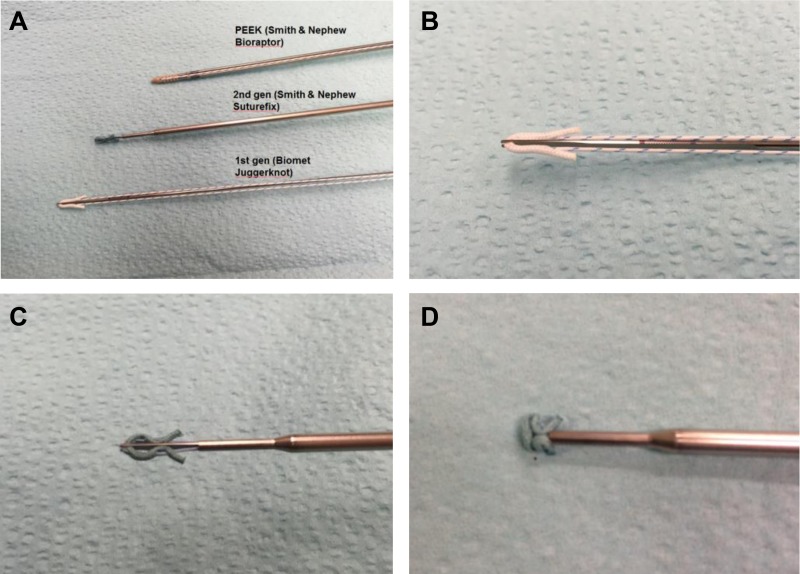
The anchors tested were the Biomet Juggerknot 1.4 mm as a first-generation all-soft suture anchor, the Smith & Nephew Suturefix Ultra S 1.7 mm as a second-generation all-soft suture anchor, and the Smith & Nephew Bioraptor 2.3 PK for an all-solid control polyether ether ketone (PEEK) anchor (Figure 1). These are all anchors designed for use in the glenoid of the shoulder. The potted specimens were placed in a custom adjustable fixation device that was fixed to an Instron universal testing machine (model 4202). Using a goniometer, anchors were inserted at a 45° angle to the glenoid face as previously described.20 Using the assistance of a biostatistician, a randomized pattern for anchor insertion was created. Approximately 1000 randomized patterns were created and then were assessed to ensure they would provide a normal distribution of anchors across each of the 20 specimens, until 1 randomization pattern was chosen. Anchors were inserted at the 12:00, 2:30, 4:30, 6:00, 8:30, and 10:30 positions in all glenoids. This clock-face pattern was standardized, with 12:00 being the superior-most point on the glenoid rim and 2:30 always being in the direction of the tip of the coracoid, regardless of the side of the individual specimen.
Figure 1.
(A) Anchor types; (B) Biomet Juggerknot, (C) Smith & Nephew Suturefix—predeployment, and (D) Smith & Nephew Suturefix—deployed.
Out of a total of 120 possible sites (6 anchors per specimen × 20 specimens), 97 were ultimately included for analysis. A site was excluded if it was already occupied by anchors that were placed for surgical procedures prior to the patient’s death (n = 17), there was a pre-existing glenoid fracture (n = 2), or there was site damage during insertion (n = 4). All anchors were inserted per the manufacturer’s suggested technique.
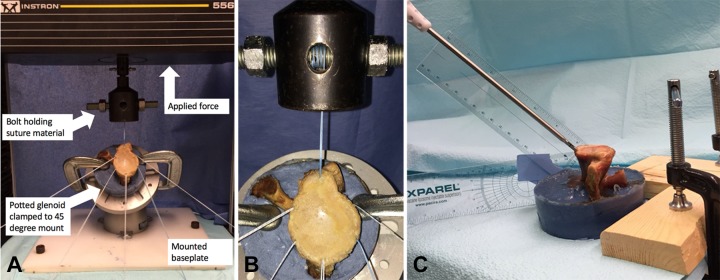
Biomechanical Testing Protocol
Biomechanical testing was performed using the Instron materials testing system, and the testing protocol was similar to that previously used and published.7,13 All anchors were tested with a direct line of pull to simulate the worst-case scenario from prior publications.14 A 10-kN load cell was used. The suture material was passed through a centrally placed hole in a threaded bolt in the Instron testing apparatus. This suture was tied in a square knot and then wrapped around the bolt 4 to 5 times, until exactly 45 mm of distance remained between the glenoid and the Instron testing bolt (Figure 2). A 5-N preload was administered at 1 N/s to eliminate possible slack in the system. Anchor constructs were preloaded to 5 N (in line with the direction of anchor insertion), cycled from 5 to 25 N for 25 cycles, and then pulled to failure at a rate of 15 mm/min. Material creep was minimized by immediately starting the load to failure as soon as cycling was terminated. Load to 2 mm of displacement and load to ultimate failure were calculated during the pull to failure at 15 mm/min. The 5-N preconditioning and cyclic loading was chosen to match previous studies.26 All raw data and measurements were taken directly from the Instron machine via Bluehill software.
Figure 2.
(A) Experimental setup. (B) Experimental setup—suture attachment to Instron testing bolt. (C) Experimental setup—anchor insertion technique.
Statistical Analysis
For our a priori power analysis we assumed a linear model with estimated values obtained from prior studies.4,20,22 We assumed a 10% loss of data from anchor site compromise in our glenoid specimens due to prior anchor placement or glenoid defects. We included in the model the effects of subject sex, subject age, insertion site location, and bone mineral density (BMD), using the true calculated values from our sample population. An a priori sample size calculation demonstrated that 6 specimens were needed to detect their primary outcome of a difference of 40 N at 2 mm of displacement with a pooled SD of 19 N, a type 1 error of 0.05 and a power of 0.8.20 The testing of 20 specimens would allow for 99% power to detect statistical significance (P ≤ .05) with a 40 ± 25 N difference between groups for load to 2-mm displacement.
Analysis of variance (ANOVA) tests were used to compare the first- and second-generation suture anchor groups with each other and also with the solid control group with regard to mean force required for 2-mm displacement and mean force required for ultimate pullout. After ANOVA testing, a linear regression model was employed to investigate the force required for 2 mm of anchor displacement and ultimate load to failure as a function of age, sex, BMD, and insertion site.
Results
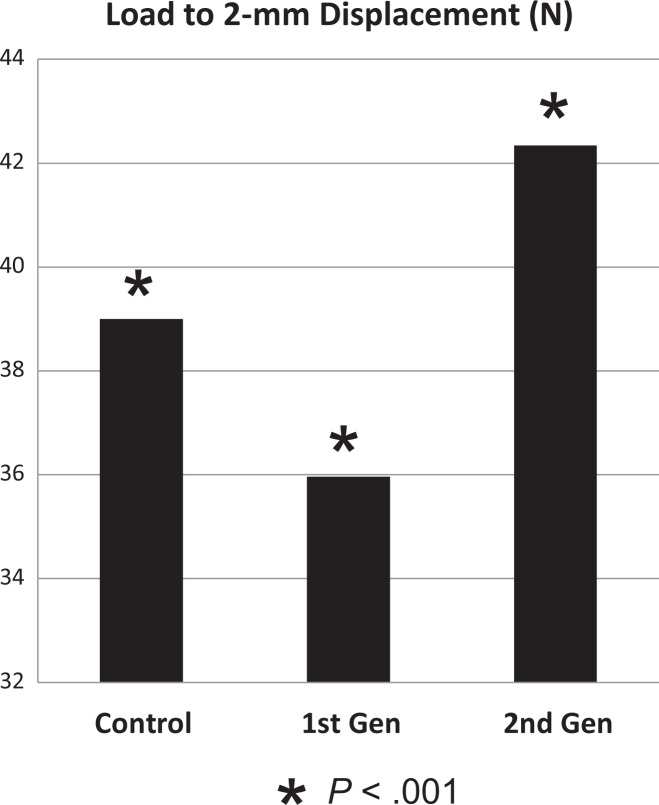
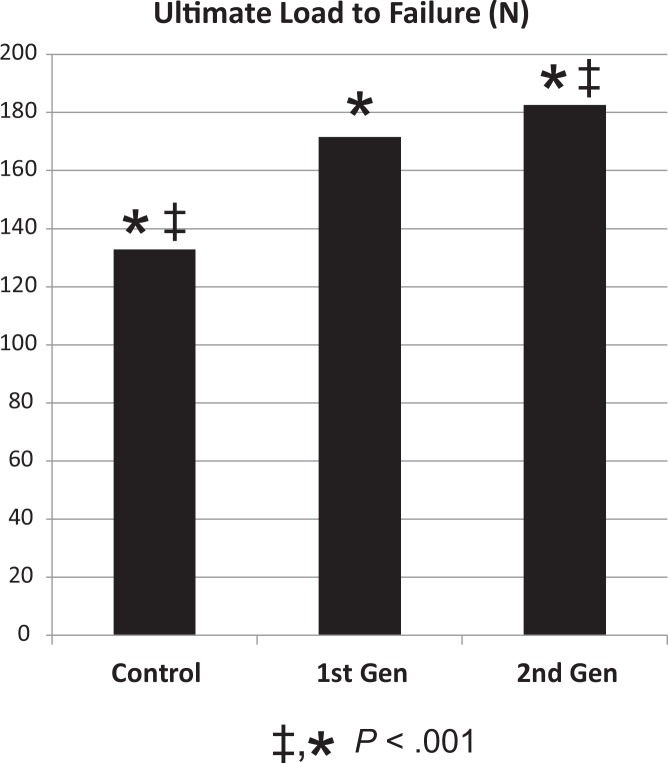
Ten matched-pair cadaveric shoulders (5 male, 5 female) with a mean age 74.4 ± 14.01 years were employed in this study. Mean BMD was 0.61 ± 0.11 g/cm3. Ninety-seven total anchors were tested to completion (load to failure). Two millimeters of pullout occurred during the cycling loading phase of the experiment in 6 anchors (3 Juggerknot, 2 Suturefix, 1 Bioraptor). These anchors were included in the final analysis. The load to 2-mm displacement was 35.96 ± 1.029 N and 42.34 ± 1.013 N for Juggerknot and Suturefix, respectively, and 39.0 ± 1.046 N for the solid anchor Bioraptor (P < .01 for comparisons between all anchors) (Figure 3). The ultimate load-to-failure forces for the all-soft suture anchors were 171.52 ± 14.25 N and 182.51 ± 14.03 N for Juggerknot and Suturefix, respectively, and 132.87 ± 14.25 N for the Bioraptor (Figure 4). No significant difference was seen between the first- and second-generation all-soft suture anchors (P > .05). However, both first- and second-generation soft suture anchors performed significantly better than the solid anchor for load to failure (P < .01). A linear regression model was employed to investigate the force required for 2 mm of anchor displacement and ultimate load to failure as a function of age, sex, BMD, and insertion site (Tables 2 and 3). It compared the effect size, a measure of the strength of a variable’s contribution to a given model, of both all-soft anchors to the all-solid control. When controlling for these variables, age, sex, and BMD did not exhibit a significant effect on the variance of the data (P > .05). The effect size (± standard error) for the Juggerknot was −2.7786 ± 1.1800 (P < .05) for load to 2-mm displacement, and the effect size for load to failure was 35.74 ± 15.76 (P < .01). The effect size for the Suturefix was 3.851 ± 1.345 (P < .01) for load to 2-mm displacement and 52.82 ± 15.84 (P < .01) for load to ultimate failure.
Figure 3.
Load to 2-mm displacement.
Figure 4.
Ultimate load to failure.
TABLE 2.
Linear Regression Model for Load to 2-mm Displacement
| Coefficients | ||||
|---|---|---|---|---|
| Estimate | Standard Error | t Value | Pr(>|t|) | |
| Intercept | 32.320 | 3.538 | 9.135 | 2.88e-14c |
| Age | 3.013 | 1.349 | 2.234 | .02809 |
| Sex, male | 2.732 | 1.218 | 2.242 | .02757a |
| Bone mineral density | 2.619 | 5.682 | 0.461 | .64596 |
| Anchor | ||||
| 1st gen (Juggerknot) | −2.646 | 1.332 | −1.987 | .05018 |
| 2nd gen (Suturefix) | 3.851 | 1.345 | 2.863 | .00528a |
| Insertion sited | ||||
| Site 2 | 3.476 | 1.850 | 1.879 | .06367 |
| Site 3 | 2.077 | 1.986 | 1.045 | .29882 |
| Site 4 | −1.514 | 1.884 | −0.804 | .42388 |
| Site 5 | −1.677 | 1.841 | −0.911 | .36474 |
| Site 6 | 3.192 | 1.988 | 1.605 | .11210 |
a P < .05.
b P < .01.
c P < .001.
dSites 2-6 correspond to the 2:30, 4:30, 6:00, 8:30, and 10:30 clock-face positions for anchor insertion, respectively.
TABLE 3.
Linear Regression Model for Load to Failure
| Coefficients | ||||
|---|---|---|---|---|
| Estimate | Standard Error | t Value | Pr(>|t|) | |
| Intercept | −26.42 | 41.90 | −0.630 | .53007 |
| Age | 17.03 | 16.12 | 1.057 | .29363 |
| Sex, male | 13.71 | 14.52 | 0.944 | .34777 |
| Bone mineral density | 169.43 | 67.93 | 2.494 | .01453a |
| Anchor | ||||
| 1st gen (Juggernaut) | 35.74 | 15.76 | 2.268 | .02583a |
| 2nd gen (Suturefix) | 52.82 | 15.84 | 3.335 | .00126b |
| Insertion sited | ||||
| Site 2 | 103.87 | 21.68 | 4.791 | 6.86e-06c |
| Site 3 | −30.73 | 23.29 | −1.319 | .19056 |
| Site 4 | 2.94 | 22.09 | 0.133 | .89443 |
| Site 5 | 55.35 | 21.60 | 2.563 | .01213a |
| Site 6 | 77.16 | 23.27 | 3.317 | 0.00134b |
a P < .05.
b P < .01.
c P < .001.
dSites 2-6 correspond to the 2:30, 4:30, 6:00, 8:30, and 10:30 clock-face positions for anchor insertion, respectively.
At 2-mm displacement, no particular glenoid testing site showed a statistically significant difference. However, for ultimate load to failure, the model revealed glenoid testing sites 2, 5, and 6 (which correspond to 2:30, 8:30, and 10:30) were associated with a statistically significant (P < .01) increased force requirement for ultimate load to failure, which is in line with previously reported data.3
Discussion
The purpose of this study was to evaluate the biomechanics of a first-generation all-soft suture glenoid anchor (Biomet Juggerknot) and a newer second-generation soft suture glenoid anchor (Smith & Nephew Suturefix) compared with a traditional solid anchor control (Smith & Nephew Bioraptor) in a human cadaveric model. Specifically, we wanted to further clarify if the first-generation all-soft suture anchors have the inferior characteristics in response to cyclic loading and submaximal displacement that have been previously reported. If they did, we sought to determine whether the newer model of second-generation all-soft suture anchors would mitigate some of the possible biomechanical concerns reported in first-generation all-soft suture anchors.20,26 Prior in vitro testing by Mazzoca et al20 has shown that the Biomet Juggerknot anchor possesses comparable ultimate loads to failure when compared with an Arthrex SutureTak biocomposite solid anchor. Our data demonstrated that both the first- and second-generation all-soft suture anchors tested demonstrated ultimate failure loads that were greater than the solid control (P < .001).
There is clinical concern about submaximal displacement of an anchor construct, as this may lead to failure of soft tissue healing to bone despite the construct being “intact.” Displacement of 1 to 3 mm has been suggested by prior publications to correlate with clinical failure of rotator cuff repairs and glenoid labrum repairs.11,27 This submaximal displacement has been postulated to create micromotion and increased synovial fluid access to the repair site, leading to resorption of bone and failure of repair.26 Mazzocca et al20 demonstrated that a solid biocomposite anchor required significantly greater load than the Juggerknot all-suture anchor for 2 mm of labral displacement in a cadaveric labral repair model. These authors postulated that device micromotion could account for the similarity in ultimate load to failure but inferiority in terms of load to 2-mm displacement. Pfeiffer et al26 similarly demonstrated significantly larger anchor displacements in the Juggerknot anchor during cyclic loading and smaller loads to 2-mm displacement after cyclic loading when compared with a solid biocomposite anchor. Their histologic data from canine models showed some cystic change surrounding each anchor. Whether this was the result of the body’s reaction to the suture material or the result of anchor motion and softness is still unclear. Our data parallel the findings of this prior published data, demonstrating that after cyclical loading, the first-generation all-soft suture anchor (Juggerknot) possessed the lowest load to 2-mm displacement (35.96 ± 1.029 N) of the 3 anchors tested. This represented a statistically significant difference when compared with both the control group and the newer generation all-soft suture anchor (Suturefix) (P < .001).
The linear regression model that investigated the force required for 2 mm of anchor displacement and ultimate load to failure as a function of age, sex, BMD, and insertion site revealed that even in the presence of these other variables, the biomechanical differences between suture anchors continued to exhibit a statistically significant effect. The Juggerknot had a negative effect versus control (−2.7786 ± 1.1800, P < .05). However, the Suturefix had a positive effect versus control (3.851 ± 1.345, P < .01) and performed better than control in ANOVA testing (P < .001). These effect sizes show the strength of the contribution of each variable to the linear regression.
Our study demonstrated clear biomechanical differences between the Suturefix model of newer second-generation all-soft suture anchors and the first-generation Juggerknot anchors. We postulate that this is because of the reconfigured locking mechanisms and deployment designs of the second-generation all-soft suture anchors. Further testing will be needed to determine if this difference is fully generalizable to other models of second-generation all-soft suture anchors or against other first-generation anchors. Clinical studies will be needed to determine if the observed biomechanical differences translate into fewer failures in glenoid labral repairs.
Our study has several limitations. Our model does not measure direct labral displacement after labral repair but rather the amount of displacement of the anchor/bone construct. Our force-to-displacement numbers are very similar to those of previous studies evaluating displacement of the construct, including the labrum.8,13 Although highly statistically significant, it is unclear but unlikely the approximately 6 N average difference for force to 2-mm displacement at 25 cycles would represent a meaningful clinical difference. While this difference could possibly be magnified or mitigated in the setting of more testing cycles or in an in vivo setting, that question cannot be answered by this study. The average age of the specimens is clearly significantly older than the typical labral repair population. However, the average BMD was 0.61 + 0.11 g/cm3, which is higher than in previous studies.19,20 Our regression model also demonstrated that age, sex, BMD, and anchor site had no significant impact on strength of effect, which seems to mitigate concerns that these anchors may behave significantly differently in younger bone. As the Juggerknot anchors were sent to us not preloaded onto their inserters, loading onto the inserter was done by us per the technical guide. The biomechanical data from this study are similar to the data from previously published studies, suggesting this did not change the biomechanical characteristics of the anchor. All anchors were inserted per the manufacturer’s instructions. Finally, we chose 25 cycles for our experimental protocol as opposed to 100 or more. Burkhart et al10 showed that up to 5-mm displacement could occur in just 25 cycles in a rotator cuff model. Barber et al6 demonstrated that most anchor displacement happens within the first 100 cycles. For the sake of comparison with Pfeiffer et al,26 it may have been beneficial to opt for the full 100 cycles but, as we had 6 anchors show 2 mm of displacement during the 25 cycles, and as our results were similar to previously published data, 25 cycles were probably sufficient.
Conclusion
A second-generation all-soft suture anchor showed greater loads to 2 mm of displacement than a first-generation all-soft suture anchor. Both all-soft suture anchors had higher load to failure than a solid tap-in anchor. Further research is required to determine if this is generalizable to all first- and second-generation all-soft suture anchors. The configuration and deployment of these newer generation all-soft suture anchors may mitigate the biomechanical concerns of decreased load to failure with first-generation all–soft tissue suture anchors.
Acknowledgment
The authors acknowledge Dr Javier Cabrera, PhD, of the Rutgers Department of Statistics and Biostatistics for his assistance with our randomization pattern and statistical analysis. Without him, the quality of our work would have been significantly diminished.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Smith & Nephew and Biomet donated the anchors used in this study. A.D. was a previous consultant for Smith & Nephew, Biomet, and Arthrex.
Ethical approval was not sought for the present study.
References
- 1. Agrawal V, Pietrzak WS. Triple labrum tears repaired with the Juggerknot soft anchor: technique and results. Int J Shoulder Surg. 2015;9:81–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahmad CS, Stewart AM, Izquierdo R, Bigliani LU. Tendon-Bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med. 2005;33:1667–1671. [DOI] [PubMed] [Google Scholar]
- 3. Anglin C, Tolhurst P, Wyss UP, Pichora DR. Mechanical properties of glenoid cancellous bone. In: Veeger HEJ, Van Der Helm FCT, Rozing PM, eds. Proceedings of the First Conference of the ISG Maastricht, Netherlands: Shaker Publishing; 1997;77:82. [Google Scholar]
- 4. Athwal GS, Shridharani SM, O’Driscoll SW. Osteolysis and arthropathy of the shoulder after use of bioabsorbable knotless suture anchors. a report of four cases. J Bone Joint Surg Am. 2006;88:1840–1845. [DOI] [PubMed] [Google Scholar]
- 5. Barber FA, Coons DA, Ruiz-Suarez M. Cyclic load testing and ultimate failure strength of biodegradable glenoid anchors. Arthroscopy. 2008;24:224–228. [DOI] [PubMed] [Google Scholar]
- 6. Barber FA, Coons DA, Ruiz-Suarez M. Cyclic load testing of biodegradable suture anchors containing 2 high-strength sutures. Arthroscopy. 2007;23:355–360. [DOI] [PubMed] [Google Scholar]
- 7. Barber FA, Herbert MA. Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy. 2013;29:832–844. [DOI] [PubMed] [Google Scholar]
- 8. Barber FA, Herbert MA, Beavis RC, Barrera Oro F. Suture anchor materials, eyelets, and designs: update 2008. Arthroscopy. 2008;24:859–867. [DOI] [PubMed] [Google Scholar]
- 9. Barber FA, Snyder SJ, Abrams JS, Fanelli GC, Savoie FH., 3rd Arthroscopic Bankart reconstruction with a bioabsorbable anchor. J Shoulder Elbow Surg. 2003;12:535–538. [DOI] [PubMed] [Google Scholar]
- 10. Burkhart SS, Johnson TC, Wirth MA, Athanasiou KA. Cyclic loading of transosseous rotator cuff repairs: tension overload as a possible cause of failure. Arthroscopy. 1997;13:172–176. [DOI] [PubMed] [Google Scholar]
- 11. Burkhart SS, Wirth MA, Simonich M, Salem D, Lanctot D, Athanasiou K. Knot security in simple sliding knots and its relationship to rotator cuff repair: how secure must the knot be? Arthroscopy. 2000;16:202–207. [DOI] [PubMed] [Google Scholar]
- 12. Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med. 2012;40:1424–1430. [DOI] [PubMed] [Google Scholar]
- 13. Ekelund A. Cartilage injuries in the shoulder joint caused by migration of suture anchors or mini screw. J Shoulder Elbow Surg. 1998;7:537–539. [DOI] [PubMed] [Google Scholar]
- 14. Fritsch BA, Arciero RA, Taylor DC. Glenoid rim fracture after anchor repair: a report of 4 cases. Am J Sports Med. 2010;38:1682–1686. [DOI] [PubMed] [Google Scholar]
- 15. Gaenslen ES, Satterlee CC, Hinson GW. Magnetic resonance imaging for evaluation of failed repairs of the rotator cuff. Relationship to operative findings. J Bone Joint Surg Am. 1996;78:1391–1396. [DOI] [PubMed] [Google Scholar]
- 16. Glueck D, Wilson TC, Johnson DL. Extensive osteolysis after rotator cuff repair with a bioabsorbable suture anchor: a case report. Am J Sports Med. 2005;33:742–744. [DOI] [PubMed] [Google Scholar]
- 17. Hyatt AQ, Lavery K, Mino C, Dhawan A. Suture anchor biomechanics after rotator cuff footprint decortication. Arthroscopy. 2016;32:544–550. [DOI] [PubMed] [Google Scholar]
- 18. Kaar TK, Schenck RC, Jr, Wirth MA, Rockwood CA., Jr Complications of metallic suture anchors in shoulder surgery: a report of 8 cases. Arthroscopy. 2001;17:31–37. [DOI] [PubMed] [Google Scholar]
- 19. Lehtinen JT, Tingart MJ, Apreleva M, Warner JJP. Total, trabecular, and cortical bone mineral density in different regions of the glenoid. J Shoulder Elbow Surg. 2004;13:344–348. [DOI] [PubMed] [Google Scholar]
- 20. Mazzocca AD, Chowaniec D, Cote MP, et al. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy. 2012;28:642–648. [DOI] [PubMed] [Google Scholar]
- 21. Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36:1824–1828. [DOI] [PubMed] [Google Scholar]
- 22. Mueller MB, Fredrich HH, Steinhauser E, Schreiber U, Arians A, Imhoff AB. Biomechanical evaluation of different suture anchors for the stabilization of anterior labrum lesions. Arthroscopy. 2005;21:611–619. [DOI] [PubMed] [Google Scholar]
- 23. Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25:788–793. [DOI] [PubMed] [Google Scholar]
- 24. Ozbaydar M, Elhassan B, Warner JJ. The use of anchors in shoulder surgery: a shift from metallic to bioabsorbable anchors. Arthroscopy. 2007;23:1124–1126. [DOI] [PubMed] [Google Scholar]
- 25. Park MJ, Hsu JE, Harper C, Sennett BJ, Huffman GR. Poly-l/d-Lactic acid anchors are associated with reoperation and failure of slap repairs. Arthroscopy. 2011;27:1335–1340. [DOI] [PubMed] [Google Scholar]
- 26. Pfeiffer FM, Smith MJ, Cook JL, Kuroki K. The histologic and biomechanical response of two commercially available small glenoid anchors for use in labral repairs. J Shoulder Elbow Surg. 2014;23:1156–1161. [DOI] [PubMed] [Google Scholar]
- 27. Provencher MT, Verma N, Obopilwe E, et al. A biomechanical analysis of capsular plication versus anchor repair of the shoulder: can the labrum be used as a suture anchor? Arthroscopy. 2008;24:210–216. [DOI] [PubMed] [Google Scholar]
- 28. Pulavarti RS, Symes TH, Rangan A. Surgical interventions for anterior shoulder instability in adults. Cochrane Database Syst Rev. 2009;4:CD005077. [DOI] [PubMed] [Google Scholar]
- 29. Richmond JC, Donaldson WR, Fu F, Harner CD. Modification of the Bankart reconstruction with a suture anchor. Report of a new technique. Am J Sports Med. 1991;19:343–346. [DOI] [PubMed] [Google Scholar]
- 30. Silver MD, Daigneault JP. Symptomatic interarticular migration of glenoid suture anchors. Arthroscopy. 2000;16:102–105. [DOI] [PubMed] [Google Scholar]
- 31. Tan CK, Guisasola I, Machani B, et al. Arthroscopic stabilization of the shoulder: a prospective randomized study of absorbable versus nonabsorbable suture anchors. Arthroscopy. 2006;22:716–720. [DOI] [PubMed] [Google Scholar]