Abstract
Invasive aspergillosis caused by A. Fumigatus, almost occurs in immunocompromised hosts and has a poor prognosis. We report a case of invasive Aspergillosis in a 15-year-old boy with ESRD. He was initially diagnosed as lobar pneumonia and peritonitis. When he complained for lower extremity weakness and had convulsions, a solid mass originated from right lung compresses the spinal cord and intracranial hemorrhagic abscesses were found on MRI. The biopsy specimen showed hypae of aspergillus-spp and he died on 12th day.
Abbreviations: CAPD, continuous ambulatory peritoneal dialysis; CNS, central nervous system; ESRD, end stage renal disease; IA, invasive aspergillosis; MRI, magnetic resonance imaging
Keywords: Aspergillosis, End stage renal disease, Peritoneal dialysis
1. Introduction
The aspergilli are ubiquitous fungi whose normal ecological niche is that of a soil saproyphyte and may cause an invasive disease in immunocompromised patients. Aspergillus fumigatus is the most common isolate obtained in 70–90% of cases of invasive aspergillosis (IA) in immunocompromised patients. Aspergillus spp are primarily respiratory pathogens, and the lungs constitute the main portal of entry before dissemination [1].
Invasive aspergillosis predominantly occurs in immunocompromised hosts, such as those with hematological malignancies, hematopoietic stem cell or solid organ transplants, congenital or acquired immunodeficiency, as well as use of corticosteroids and other immunosuppressive drugs [2]. The central nervous system (CNS) is one of the most frequent involvement of IA besides the lungs and is very rare in immunocompetent patients [3]. The infections mostly occur through hematogenous dissemination from a focus, such as lung infection, or rarely through direct extension from the paranasal sinuses [4], [5]. Invasive aspergillosis in infants and children may exhibit differences from adults, such as less specific findings and greater difficulties in early diagnosis and antifungal treatment [6].
We report a case of IA in a previously healthy immunocompetent boy with end stage renal disease (ESRD), and emphasize that the diagnosis of fungal infections may be missed or delayed due to lack of the particular clinical signs in patients with ESRD.
2. Case
A 15-year-old boy was admitted with a history of abdominal pain and cough of one-week duration. He suffered from ESRD for one year and had undergone a renal biopsy which showed global sclerosis and he was on continuous ambulatory peritoneal dialysis (CAPD) for seven months. There was consanguinity between parents, and in family history, a 16 year old sister died of meningitis, a 10 year old sister of unknown pulmonary problems.
On admission, he was tachypneic with a respiratory rate of 60/min and blood pressure of 120/70 mmHg. The left lung was clear on auscultation but breath sounds were diminished on the upper part of right lung. The chest X-ray showed homogenous consolidation in the same area of the right lung (Fig. 1). The patient was not febrile and Tenchoff catheter was in place with good exit-site, the peritoneal fluid was cloudy and showed 980 white blood cells/mm3 with polymorphs more than 70%. He had no previous history of peritonitis. His blood examination showed a hemoglobin level of 7.2 g/dl, white blood cell (WBC) count of 20700/mm3 and platelet count of 698000/mm3. The results of biochemical parameters were as follows: BUN: 53 mg/dl, creatinine: 6.8 mg/dl, CRP: 309 mg//L, albumin: 1.6 g/dl.
Fig. 1.
Chest radiography.
After samples for blood and peritoneal fluid cultures were obtained, the patient was initially treated with intravenous ceftriaxone for lobar pneumonia, intraperitoneal ceftazidime and cefazolin for peritonitis. The peritoneal fluid was also cultured for fungus and mycobacteria and all cultures were negative. On the 5th day of the therapy, intraperitoneal vancomycin was applied since there was no change in peritoneal fluid cell count and it was continued intravenously for deteriorating findings of pneumonia. On the 7th day of hospital admission, the patient complained for lower extremity weakness, and his neurological examination revealed bilateral lower extremity weakness, hyperactive deep tendon reflexes and bilateral positive Babinski reflex.
Cranial magnetic resonance imaging (MRI) was normal, but the spinal cord was compressed between C7-T5 by a solid mass which was originated from right lung on servical spinal MRI as well as proven on chest CT (Fig. 2).
Fig. 2.
Computed tomography.
On the 8th day, computed tomography-guided transthoracic true-cut biopsy was performed for differential diagnosis of the solid mass in the lung, which was thought to be a primary tumor as an initial diagnosis.
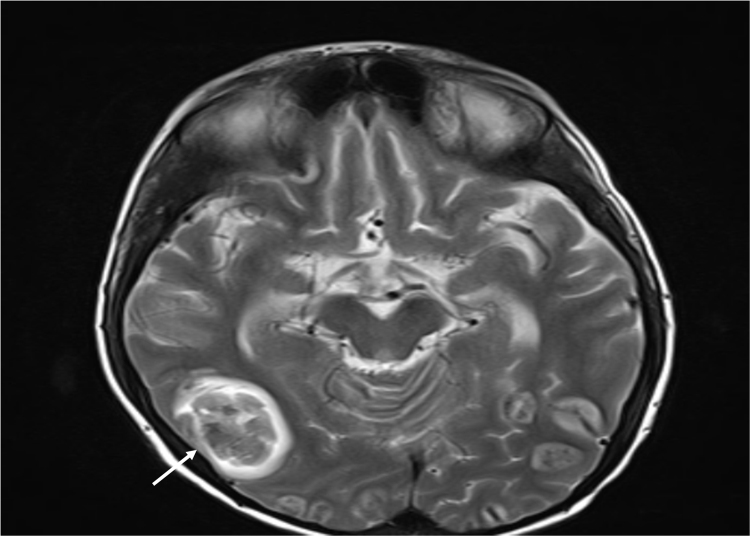
On the 9th day, the patient was unconscious and had convulsions, intraparenchymal multiple hemorrhagic abscesses were found on his second MRI which was performed four days later than the first MRI (Fig. 3). Histological examination of the biopsy specimen showed an aggregate of typical hypae of aspergillus spp with septae and branching at 45 angles (Fig. 4), and at the same time Galactomannan test was positive. These abscesses were evaluated as central nervous system involvement of invasive aspergillosis. Tests performed for immunoglobulin levels and flow cytometry immunophenotyping were normal.
Fig. 3.
Cranial MRI.
Fig. 4.
Branching of hyphae in Grocott's methenamine silver stain.
He was transferred to Pediatric Intensive Care Unit, and amphotericin B and caspofungin was begun. Although we could not be able to isolate Aspergillus spp from the peritoneal dialysis fluid culture, peritoneal aspergillosis was considered very likely in our patient because of the invasive aspergillosis, and the peritoneal catheter was removed and continuous veno venous hemodiafiltration was performed for the patient. Despite administration of amphotericin B and caspofungin, he deteriorated day by day and died of respiratory failure and central nervous system complications ensued on the fourth day of anti fungal therapy.
3. Discussion
The Aspergillus spp are frequently found in environment and commonly affect patients receiving chemotherapy, solid organ transplant and allogeneic stem cell transplant [7], [8]. Aspergillus fumigatus is the most common isolate obtained in 70–90% of cases of IA in immunocompromised patients and this species is also the most frequent cause of CNS aspergillosis [6], [9].
Infections are common in ESRD patients. The mechanisms underlying the defective responses in phagocytic cells, lymphocytes and antigen processing are likely due to either failure to adequately eliminate suppressive compounds by the defective kidneys or to improper metabolic processing of the factors by the damaged renal parenchyma [10], [11].
Fungal infections as peritonitis are common in ESRD patients on peritoneal dialysis, whereas invasive aspergillosis is rarely seen. Invasive pulmonary aspergillosis is rare in ESRD and has previously been reported as a few case reports, it may also rarely occur in immunocompetent individuals [12], [13]. Our patient was a 15 years old boy and had no previous history of the immunodeficiency. Tests performed for immunoglobulin levels and flow cytometry immunophenotyping were normal. End stage renal disease is thought to be the main cause for immunodysregulation leading to invasive disease in our patient.
Aspergillus spp are primarily respiratory pathogens, and the lungs constitute the main entry before dissemination. Central nervous system aspergillosis, being one of the most frequent sites of IA after the lungs, was the result of dissemination from the respiratory tract [14], [15]. Our patient had first pulmonary aspergillosis and CNS aspergillosis developed after dissemination.
As Aspergillus spp is a primarily respiratory pathogen, the most common clinical signs are high fever, cough, and expectoration that are unresponsive to empirical treatment. But on the other hand clinical signs can be non-specific, approximately 25–33% of patients initially have no symptoms attributable to invasive pulmonary aspergillosis [13], [14]. Invasive aspergillosis in infants and children may be underdiagnosed with less specific findings and greater difficulties in early diagnosis. Our patient had only history of cough and abdominal pain for a week. He had no physical findings except diminished breath sounds on the upper part of right lung, and he was not febrile. Therefore, we treated him empirically for lober pneumonia and peritonitis on admission.
The availability of the Platelia Aspergillus, a sandwich ELISA kit that detects circulating galactomannan, has been a major advance for managing patients at risk for invasive aspergillosis because of the early detection of the antigen. In all studies so far the specificity of the galactomannan assay was greater than 85%; however, the sensitivity of the assay varied considerably between 29% and 100% [16]. The definitive diagnosis is made with histological tests. The hyphae appearance with branches of 45° is a typical and specific finding for aspergillus infection [14]. In our patient, galactomannan test was positive and tru-cut biopsy revealed a typical hyphae of Aspergillus fumigatus.
New antifungal therapies as voriconazole are effective in the treatment of cerebral aspergillosis because of their good penetration to brain. Herbrecht et al. studied invasive aspergillosis and reported that the survival rate in the voriconazole treated group (70.8%) was higher than that in the amphotericin B treated group (57.9%) at 12 weeks [17]. In our patient, we used a combined therapy with amphotericin B and caspofungin since voriconazole couldn’t be a choice in ESRD. The intravenous preparation of voriconazole is solubilized in sulfobutylether-ß-cyclodextrin (SBECD) and it is cleared by kidney. There is very limited data regarding safety of accumulation of SBECD in patients with renal insufficiency or in patients receiving any form of dialysis [18], [19]. Hence the peritonitis was thought to be related to aspergillus, the peritoneal catheter was removed and continuous veno venous hemodiafiltration was performed for the patient.
In CNS involvement, the brain lesions ranges from subtle abscesses, extensive hemorrhage, focal purulent meningitis and infarctions to massive hemorrhagic necrosis causing herniation and death. Single or multiple brain abscesses throughout the cerebrum, cerebellum, basal ganglia and brainstem are reported to be the most common sites of CNS aspergillosis (69.2%) [3]. In our patient, intraparenchymal multiple hemorrhagic abscesses were found on his second MRI and were evaluated as central nervous system involvement of invasive aspergillosis.
The prognosis of CNS aspergillosis is discouragingly poor in adults and more favorable in children. The overall mortality rate of published pediatric cases of CNS aspergillosis decreased from 82.8% to 39.5% after 1990. This dramatic decrease in infants and children may have been due to the introduction of amphotericin B lipid formulations and Aspergillus-active azoles as well as most importantly to the developments for earlier diagnosis of CNS aspergillosis [3]. Despite advances in early diagnosis and initiation of treatment and newer antifungal agents, CNS aspergillosis remains a devastating opportunistic infection.
In conclusion, invasive aspergillosis rarely occurs in immunocompetent patients and diagnosis may be missed or delayed due to lack of the particular clinical signs. Invasive aspergillosis should be thought in the differential diagnosis of pneumonia poorly responding to broad spectrum antibiotics in children with ESRD since early treatment before the dissemination of aspergillosis to adjacent tissues and/or organs offers a higher survival chance for the patients.
Conflict of interest
None.
Ethical form
This study received no funding, and there are no potential conflicts of interest to declare. We obtained written and signed consent to publish the case report from the patient.
Acknowledgements
None.
References
- 1.Rog E.L., Steinbach W.J., Aspergillus. Kliegman R.M., Stanton B.F., St. Geme J.W., Schor N.F., Behrman R.E., editors. Nelson Textbook of Pediatrics. 19th ed. Elsevier Saunders; Philadelphia: 2011. pp. 1058–1062. [Google Scholar]
- 2.Kontoyiannis D.P., Bodey G.P. Invasive aspergillosis in 2002: an update. Eur. J. Clin. Microbiol. Infect. Dis. 2002;21:161–172. doi: 10.1007/s10096-002-0699-z. [DOI] [PubMed] [Google Scholar]
- 3.Denning D.W. Invasive aspergillosis. Clin. Infect. Dis. 1998;26:781–803. doi: 10.1086/513943. [DOI] [PubMed] [Google Scholar]
- 4.Green M., Wald E.R., Tzakis A., Todo S., Starzl T.E. Aspergillosis of the CNS in a pediatric liver transplant recipient: case report and review. Rev. Infect. Dis. 1991;13:653–657. doi: 10.1093/clinids/13.4.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robinson M.R., Fine H.F., Ross M.L., Mont E.K., Bryant-Greenwood P.K., Hertle R.W., Tisdale J.F., Young N.S., Zeichner S.L., Van Waes C., Whitcup S.M., Walsh T.J. Sino-orbital-cerebral aspergillosis in immunocompromised pediatric patients. Pediatr. Infect. Dis. J. 2000;19:1197–1203. doi: 10.1097/00006454-200012000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Steinbach W.J. Pediatric aspergillosis: disease and treatment differences in children. Pediatr. Infect. Dis. J. 2005;24:358–364. doi: 10.1097/01.inf.0000157218.37603.84. [DOI] [PubMed] [Google Scholar]
- 7.Kang J.M., Woo J.H., Ryu J.S. Invasive aspergillosis and the clinical management. Korean J. Med. Mycol. 2002;7:14–21. [Google Scholar]
- 8.Ng T.T., Robson G.D., Denning D.W. Hydrocortisone-enhanced growth of Aspergillus spp.: implications for pathogenesis. Microbiology. 1994;140:2475–2479. doi: 10.1099/13500872-140-9-2475. [DOI] [PubMed] [Google Scholar]
- 9.Kleinschmidt-DeMasters B.K. Central nervous system aspergillosis: a 20-year retrospective series. Hum. Pathol. 2002;33:116–124. doi: 10.1053/hupa.2002.30186. [DOI] [PubMed] [Google Scholar]
- 10.Pesanti E.L. Immunologic defects and vaccination in patients with chronic renal failure. Infect. Dis. Clin. N. Am. 2001;15:813–832. doi: 10.1016/s0891-5520(05)70174-4. [DOI] [PubMed] [Google Scholar]
- 11.Sahlen A.O., Suvarna S.K., Wilkie M.E. A case of invasive pulmonary aspergillosis in renal failure. Nephrol. Dial. Transplant. 2004;19:2687. doi: 10.1093/ndt/gfh418. [DOI] [PubMed] [Google Scholar]
- 12.Kose S., Cavdar G., Senger S.S., Akkoclu G. Central nervous system aspergillosis in an immunocompetent patient. J. Infect. Dev. Ctries. 2011;5:313–315. doi: 10.3855/jidc.1461. [DOI] [PubMed] [Google Scholar]
- 13.Xu X.M., Sun H.M., Zhao B.L., Shi Y. Diagnosis of airway-invasive pulmonary aspergillosis by tree-in-bud sign in an immunocompetent patient: case report and literature review. J. Mycol. Méd. 2013;23:64–69. doi: 10.1016/j.mycmed.2012.12.050. [DOI] [PubMed] [Google Scholar]
- 14.Denning D.W. Invasive Aspergillosis. Clin. Infect. Dis. 1996;26:781–803. doi: 10.1086/513943. [DOI] [PubMed] [Google Scholar]
- 15.Dotis J., Iosifidis E., Roilides E. Central nervous system aspergillosis in children: a systematic review of reported cases. Int. J. Infect. Dis. 2007;11:381–393. doi: 10.1016/j.ijid.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 16.Mennink-Kersten M.A., Donnelly J.P., Verweij P.E. Detection of circulating galactomannan for the diagnosis and management of invasive Aspergillosis. Lancet Infect. Dis. 2004;4:349–357. doi: 10.1016/S1473-3099(04)01045-X. [DOI] [PubMed] [Google Scholar]
- 17.Herbrecht R., Denning D.W., Patterson T.F., Bennett J.E., Greene R.E., Oestmann J.W., Kern W.V., Marr K.A., Ribaud P., Lortholary O., Sylvester R., Rubin R.H., Wingard J.R., Stark P., Durand C., Caillot D., Thiel E., Chandrasekar P.H., Hodges M.R., Schlamm H.T., Troke P.F., de Pauw B. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N. Engl. J. Med. 2002;347:408–415. doi: 10.1056/NEJMoa020191. [DOI] [PubMed] [Google Scholar]
- 18.Luke D.R., Tomaszewski K., Damle B., Schlamm H.T. Review of the basic and clinical pharmacology of sulfobutylether-beta-cyclodextrin (SBECD) J. Pharm. Sci. 2010;99:3291–3301. doi: 10.1002/jps.22109. [DOI] [PubMed] [Google Scholar]
- 19.Maertens J. Caspofungin: an advanced treatment approach for suspected or confirmed invasive aspergillosis. Int. J. Antimicrob. Agents. 2006;27:457–467. doi: 10.1016/j.ijantimicag.2006.03.019. [DOI] [PubMed] [Google Scholar]