Introduction
There are many conditions associated with the formation of numerous cutaneous squamous cell carcinomas (cSCCs), including, among others, xeroderma pigmentosum, epidermolysis bullosa, epidermodysplasia verruciformis, Ferguson-Smith syndrome, Grzybowski syndrome, and Bloom syndrome. We report the first case of multiple cSCCs developing in the setting of functional natural killer cell deficiency (FNKD). This case reveals a potential underlying relationship between natural killer (NK) cells and cSCC development.
Case
A 56-year-old woman with a history of Crohn disease presented to Mayo Clinic Arizona Department of Dermatology in 2011 with a 4-year history of multiple cSCCs. At her initial consult, she was found to have minimal dermatoheliosis and an additional 4 cSCCs. Given concern that immunosuppression could be driving disease progression, treatment with 6-mercaptopurine was discontinued. Despite this change, she developed 24 additional cutaneous cSCCs over the next 2 years.
In 2013, the patient was hospitalized and diagnosed with systemic cytomegalovirus infection along with a urinary tract infection. Following discharge, the patient was closely monitored for persistent and recurrent infections along with continued cSCC development. Her cutaneous lesions presented as pink keratotic papules that were tender on palpation (Fig 1). All cSCCs biopsies were histologically well-differentiated (Figs 2 and 3). A large variety of medical and physical treatments were attempted, including wide local excision, Mohs surgery, electrodessication and curettage, topical 5-fluoruracil, intralesional 5-fluorouracil, imiquimod, cryotherapy, acitretin, photodynamic therapy, intralesional methotrexate, and electron beam radiation therapy. Although she was treated with multiple and combinational therapies over long courses, none were found to be beneficial or were discontinued because of the side effects (eg, acitretin caused extreme dryness of the lips and skin, fatigue, headaches, and worsening of Crohn disease symptoms).
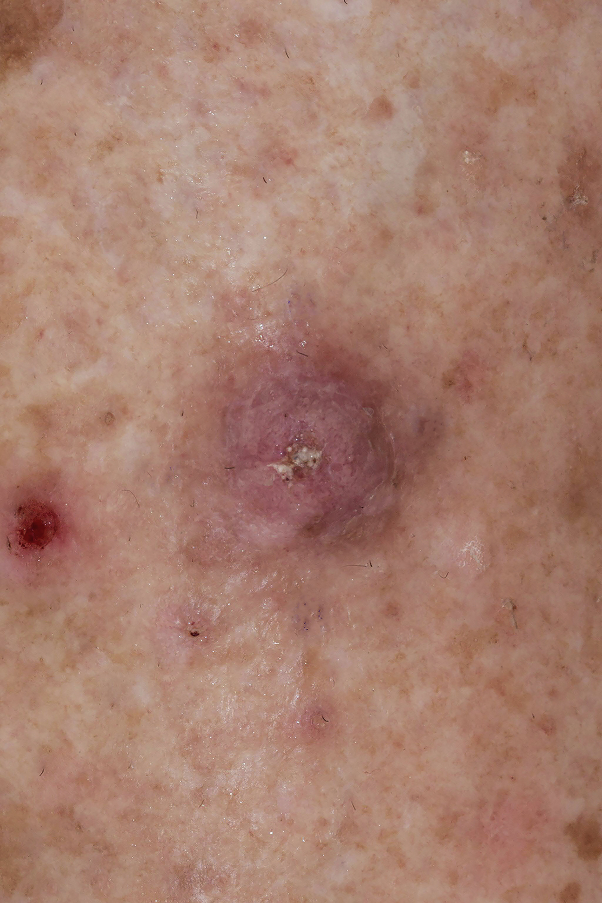
Fig 1.
Tender keratotic papule that was biopsied and found to be a well-differentiated cutaneous squamous cell carcinoma.
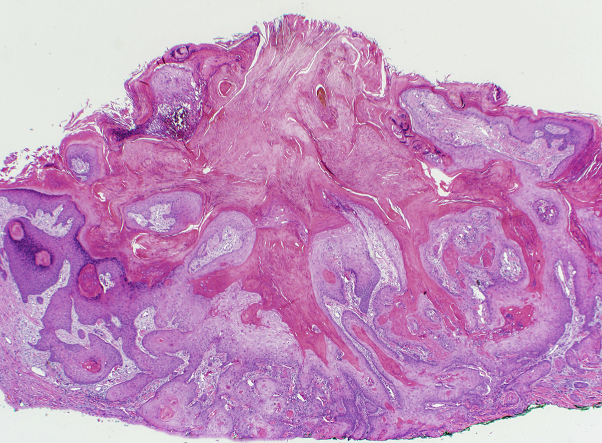
Fig 2.
Well-differentiated cutaneous squamous cell carcinoma lesion. (Hematoxylin-eosin stain; original magnification: ×20.)
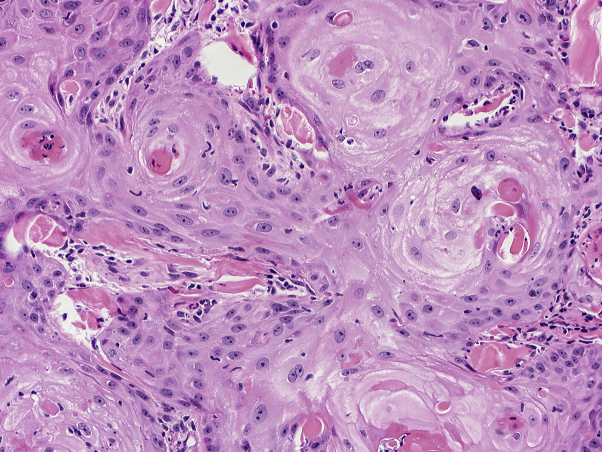
Fig 3.
Well-differentiated cutaneous squamous cell carcinoma lesion. (Hematoxylin-eosin stain; original magnification: ×200.)
Due to her history, the patient was referred to the Department of Clinical Immunology. A complete blood count and lymphocyte panel, including NK cells, B cells, CD4+ T cells, and CD8+ T cells, were performed, and all cell populations were within normal ranges. Because of clinical suspicion, NK cytotoxicity was tested using a 51Chromium-release assay with K562 cells lacking major histocompatibility complex (MHC) class I. Following 3 NK cytotoxicity assays performed at 1-month intervals and after ruling out secondary causes, she was given a diagnosis of FNKD. Afterward, the patient was trialed on cetuximab, which had a measurable effect and reduced tumor frequency in this patient. Yet, this medication had to be discontinued because the patient developed hypomagnesemia. Multiple cSCCs tested for human papillomavirus (HPV) DNA by polymerase chain reaction were negative for the virus. From the date of FNKD diagnosis to September 2016, she had developed an additional 26 biopsy-confirmed cSCCs, for a total of 50 cSCCs over 5 years.
Discussion
FNKD might provide a unique insight into the role of NK cells in cSCC pathogenesis. NK cells are CD16+ CD56+ CD3− lymphocytes of the innate immune system that contribute to antiviral defense and tumor cell surveillance and initiate acquired immunity through cytokine recruitment.1 There are 2 subtypes of NK deficiency: classical NK deficiency, in which the absolute number of NK cells is diminished and FNKD, in which patients have functionally deficient NK cells with normal cell counts. The only known gene defect associated with FNKD is a mutation in FCGR3A, a gene involved in CD16 expression.1 There is an association between FNKD and autoimmune diseases such as type 1 diabetes mellitus, multiple sclerosis, and systemic lupus erythematosus2; however, an association with Crohn disease has not been previously reported. Patients with FNKD often have severe and recurrent herpesvirus infections,3 as evidenced in our patient.
A relationship between FNKD patients and HPV infection has been established.4 In addition, elevated NK cell levels within HPV-induced oropharyngeal SCCs are associated with improved patient outcomes.5 Our patient had multiple cSCCs that were negative for HPV by polymerase chain reaction. This suggests that NK cells play a vital role in inhibiting cSCC development independent of viral defense. For NK cells to exert a cytotoxic effect on tumor cells, the killer cell immunoglobulin-like receptor (KIR) requires an absence of self-antigen on the tumor cell MHC-1 receptor and binding of costimulatory receptors. Research is ongoing on the potential use of NK cells as antitumor therapy using either isolated donor NK cells or KIR-specific monoclonal antibodies.6, 7 This humanized antibody can block the KIR, effectively signaling to the NK cell that it is binding to a nonself MHC-1, activating cytotoxicity. This case of FNKD suggests that the increase in NK cell activity using KIR monoclonal antibodies might be beneficial for cSCC management in healthy patients. Furthermore, therapeutic antibodies including cetuximab cause increases in NK cell cytotoxicity against autologous tumor cells, further suggesting the important role NK cells play in tumor immunity.8
We describe herein the first case, to our knowledge, of a patient with FNKD who developed 50 cSCCs over a 5-year period that were resistant to standard chemoprevention. This patient has not undergone genetic testing, but this might be an appropriate next step. Further studies are warranted to characterize the relationship between NK cells and cSCC. Such investigations might lead to potential insight in the development of eruptive keratoacanthomas, multiple lower-extremity cSCCs, iatrogenic cSCCs in transplant recipients, and additional treatment modalities for cSCC.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Orange J.S. Natural killer cell deficiency. J Allergy Clin Immunol. 2013;132:515–525. doi: 10.1016/j.jaci.2013.07.020. quiz 526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baxter A.G., Smyth M.J. The role of NK cells in autoimmune disease. Autoimmunity. 2002;35:1–14. doi: 10.1080/08916930290005864. [DOI] [PubMed] [Google Scholar]
- 3.Ornstein B.W., Hill E.B., Geurs T.L., French A.R. Natural killer cell functional defects in pediatric patients with severe and recurrent herpesvirus infections. J Infect Dis. 2013;207:458–468. doi: 10.1093/infdis/jis701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cac N.N., Ballas Z.K. Recalcitrant warts, associated with natural killer cell dysfunction, treated with systemic IFN-alpha. J Allergy Clin Immunol. 2006;118:526–528. doi: 10.1016/j.jaci.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 5.Wagner S., Wittekindt C., Reuschenbach M. CD56-positive lymphocyte infiltration in relation to human papillomavirus association and prognostic significance in oropharyngeal squamous cell carcinoma. Int J Cancer. 2016;138:2263–2273. doi: 10.1002/ijc.29962. [DOI] [PubMed] [Google Scholar]
- 6.Vivier E., Ugolini S., Blaise D., Chabannon C., Brossay L. Targeting natural killer cells and natural killer T cells in cancer. Nat Rev Immunol. 2012;12:239–252. doi: 10.1038/nri3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kohrt H.E., Thielens A., Marabelle A. Anti-KIR antibody enhancement of anti-lymphoma activity of natural killer cells as monotherapy and in combination with anti-CD20 antibodies. Blood. 2014;123:678–686. doi: 10.1182/blood-2013-08-519199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pahl J.H., Ruslan S.E., Buddingh E.P. Anti-EGFR antibody cetuximab enhances the cytolytic activity of natural killer cells toward osteosarcoma. Clin Cancer Res. 2012;18:432–441. doi: 10.1158/1078-0432.CCR-11-2277. [DOI] [PubMed] [Google Scholar]