Abstract
Background
Cancer is responsible for 7.6 million deaths worldwide and surgery is the primary modality of a curative outcome. Postoperative care is of considerable importance and it is against this backdrop that a questionnaire based study assessing the attitudes of surgeons to monitoring postoperative systemic inflammation was carried out.
Method
A Web based survey including 10 questions on the “attitudes of surgeons to the use of postoperative markers of the systemic inflammatory response following elective surgery” was distributed via email. Two cohorts were approached to participate in the survey. Cohort 1 consisted of 1092 surgeons on the “Association of Coloproctology of Great Britain and Ireland (ACPGBI)” membership list. Cohort 2 consisted of 270 surgeons who had published in this field in the past as identified by two recent reviews. A reminder email was sent out 21 days after the initial email in both cases and the survey was closed after 42 days in both cases.
Result
In total 29 surgeons (2.7%) from cohort 1 and 40 surgeons (14.8%) from cohort 2 responded to the survey. The majority of responders were from Europe (77%), were colorectal specialists (64%) and were consultants (84%) and worked in teaching hospitals (54%) and used minimally invasive techniques (87%). The majority of responders measured CRP routinely in the post-operative period (85%) and used CRP to guide their decision making (91%) and believed that CRP monitoring should be incorporated into postoperative guidelines (81%).
Conclusion
Although there was a limited response the majority of surgeons surveyed measure the systemic inflammatory response following elective surgery and use CRP measurements together with clinical findings to guide postoperative care. The present results provide a baseline against which future surveys can be compared.
Keywords: Inflammation, C-reactive protein, Elective surgery, Postoperative care, Minimal access surgery, Post-operative complications, Discharge planning
Highlights
-
•
Shows that there is a widespread interest in the use of markers of the systemic inflammatory response in managing patients.
-
•
This is particularly true when managing complications post operatively.
-
•
There would seem to be scope for incorporation of markers of the SIR into formal post operative guidelines.
1. Introduction
Worldwide cancer remains a significant problem with 12.7 million new cases being diagnosed in 2008. Globally cancer remains one of the leading causes of death and is responsible for 7.6 million deaths per year [1], [2]. In the UK each year, there are approximately 331,000 new cases of cancer and over 50,000 deaths each year in the 35–64 age groups. Surgery is the primary modality of cure and therefore post-operative management is important in cancer care [3].
Although, outcomes are predominantly determined by cancer stage in patients with operable disease, post-operative complications are important in the disease progression [4], [5]. In particular, it has been shown that anastomotic leaks have a negative impact on both the short and long-term survival of patients with GI cancer [6], [7]. The basis of this relationship is not clear, however it has been proposed that the magnitude of the post-op systemic inflammatory response [SIRS] is an important determining factor [4]. The magnitude of this SIRS response can be routinely quantified by serial C-reactive protein [CRP] concentration measurement in the post-operative period [8].
Two recent meta-analyses including over 2000 patients have reported the importance of postoperative serum CRP measurement in the early diagnosis of postoperative infective complications and anastomotic leaks in patients undergoing colorectal surgery [9], [10]. Indeed, CRP thresholds have been reported as consistently predicting the development of post-operative infective complications and may be a guide to early discharge [10], [11], [12].
However, this raises the question as to how this information might be used in clinical practice. For example, McDermott and coworkers [2015] have proposed that a CRP <150 mg/L on days 3, 4 and 5, be used to indicate the likelihood of safe discharge postoperatively [11]. In a recent study in the Netherlands the use of serial CRP monitoring has been proposed as a trigger for determining whether or not a post-operative CT should be carried out to investigate the presence of a possible post-operative complication [13]. Also, it has been proposed that serial CRP monitoring may be used to determine the efficacy of ERAS protocols in the post-operative period [8].
It is against this background that the present questionnaire based study was carried out. The aim was to assess the attitudes of surgeons to the use of serial post-operative CRP monitoring and its importance in their clinical decision making. In addition, to investigate the level of awareness of the postoperative CRP thresholds associated with the development of potential complications and to guide clinical decision making in the postoperative period including the decision to instigate a surgical, endoscopic or radiological intervention or in discharge planning. Finally, to assess the attitudes of surgeons to the incorporation of serial CRP monitoring into routine postoperative care protocols and guidelines.
2. Methods
A web based survey that included 10 questions on the “Attitudes of surgeons to the use of postoperative markers of the systemic inflammatory response following elective surgery” was as follows.
2.1. Survey questions
-
1.
What is your surgical specialisation? Colorectal/Oesphagogastric/Hepatobiliary/Urology/Thoracic/Other [please specify]
-
2.
In what country are you based? Open Text
-
3.
What is your grade at present? Consultant/Trainee/Other
-
4.
Which of the following best describes the surgical unit in which you currently practice? University Academic Unit/Teaching Hospital/Non-teaching Hospital/Other [please state]
-
5.
Does your unit currently use an “enhanced recovery” or “fast track” programme following elective surgery? yes/no
-
6.
Do you currently perform any elective procedures using laparoscopic, robotic or other minimally invasive techniques? yes/no
-
7.
Is C-reactive protein measured routinely in your patients during the postoperative period following elective colorectal surgery? yes/no
-
8.
If you answered “Yes” to Q7: Do you currently use C-reactive protein [CRP] to guide decision making in the postoperative period [e.g. to trigger investigation of potential complications or direct discharge]? If you answer “Yes”, please leave specific comments to elaborate. yes/no
-
9.
Are you aware of any existing literature examining the relationship between the magnitude of the postoperative systemic inflammatory response, in particular as measured by C-reactive protein [CRP], and outcomes following surgery? If so, please comment. yes/no
-
10.
Do you think that a measure of the postoperative systemic inflammatory response, such as C-reactive protein [CRP], should be included in postoperative care protocols or guidelines to guide postoperative decision making and/or discharge planning? yes/no
The survey was generated through the SurveyMonkey website [www.surveymonkey.com/, SurveyMonkey, Palo Alto, USA] and the access link emailed to the target cohort. The initial target cohort included surgeons who were part of the Association of Coloproctology of Great Britain and Ireland (ACPGBI) mailing list (n = 1092) however responses from this were few and so a further target cohort was selected from two recent meta-analysis [1], [2] and by performing a literature search for articles using the keywords cancer, inflammation, CRP, postoperative care, minimal access surgery, post-operative complications and discharge planning up to the end of 2015 (n = 270). Once a comprehensive list of articles was obtained, the email addresses of the corresponding authors from each article formed the basis of the mailing list for distribution. These emails were then reviewed to ascertain the specialty of the authors to ensure that they were surgeons.
Once this was completed an email was sent out to the identified surgeons clearly stating that the role of the study was to assess the application of the systemic inflammatory response using CRP in the postoperative care of patients following surgical excisions of resectable cancers and that participation was on a voluntary basis. Software on the website ensured duplication of response from the same individual was not recorded. No incentives were used to promote or encourage participation.
The initial survey to cohort 1 was distributed in November 2015 and remained open for six weeks in total. Following a literature review the survey was sent out again to cohort 2 on 3rd June 2016 with a reminder sent out 21 days later. The survey remained open for 3 weeks and was closed on 15th July. Data were analysed and graphs of results were compiled using Microsoft Excel 2007 [Redmond, WA, USA].
3. Results
In total, 69 people completed the survey. There were 29 from cohort 1 (2.7%) and 40 from cohort 2 (14.8%) giving an overall response rate of 5.9%.
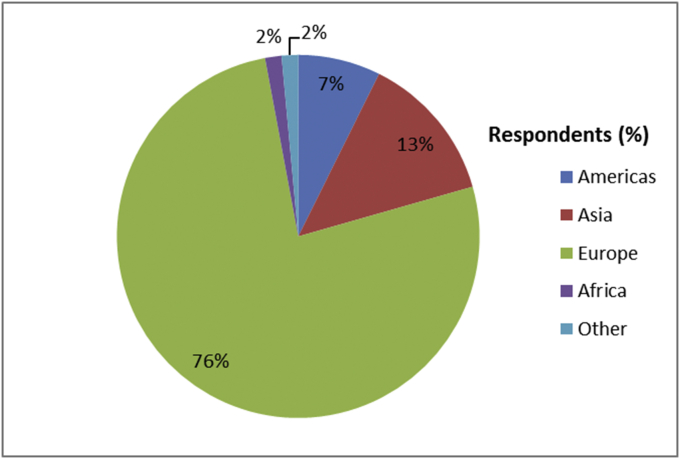
The response to survey question 1 is shown in Fig. 1 and 64% of respondents were colorectal surgeons, 12% were oesophagogastric surgeons and 14%] were hepatobiliary surgeons. The response to question 2 is shown in Fig. 2 and 76% of respondents were from Europe, 13% from Asia and 7% from the Americas. The response to question 3 is shown in Fig. 3 and 84% of respondents were consultants and 12% were trainee surgeons.
Fig. 1.
What is your surgical specialty? [n = 68].
Fig. 2.
In what region are you based? [n = 68].
Fig. 3.
What is your present grade? [n = 68].
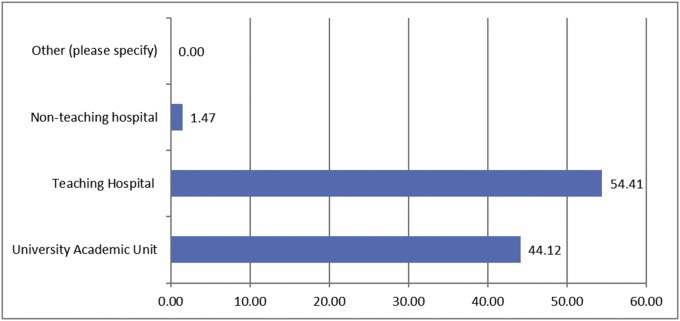
The response to question 4 is shown in Fig. 4 and 95% of respondents worked in either a university academic unit or a teaching hospital. The response to question 5 is shown in Fig. 5 and 90% of respondents used an enhanced recovery/fast track programme following elective surgery. The response to question 6 is shown in Fig. 6 and 87% of respondents carried out elective surgery via laparoscopic, robotic or another minimally invasive techniques.
Fig. 4.
Which of the following best describes the surgical unit in which you currently practice? [n = 68].
Fig. 5.
Does your unit currently use an “enhanced recovery” or “fast track” programme following elective surgery? [n = 68].
Fig. 6.
Do you currently perform any elective procedures using laparoscopic, robotic or other minimally-invasive techniques? [n = 63].
The response to question 7 is shown in Fig. 7 and 85% of respondents routinely used CRP in the monitoring of patients in the post-operative period and of these 91% of respondents used CRP to guide decision making in the post-operative period (Question 8, Fig. 8). The response to question 9 is shown in Fig. 9 and 78% of respondents were aware of existing literature examining the relationship between the magnitude of the postoperative systemic inflammatory response including CRP and outcomes following surgery.
Fig. 7.
Is C-reactive protein [CRP] measured routinely in your patients during the postoperative period following elective surgery? [n = 67].
Fig. 8.
If you answered “yes” to Q7: Do you currently use C-reactive protein [CRP] to guide decision making in the postoperative period [e.g. to trigger investigation of potential complications or direct discharge]? [n = 56].
Fig. 9.
Are you aware of any existing literature examining the relationship between the magnitude of the postoperative systemic inflammatory response, in particular as measured by C-reactive protein [CRP], and outcomes following surgery? [n = 67].
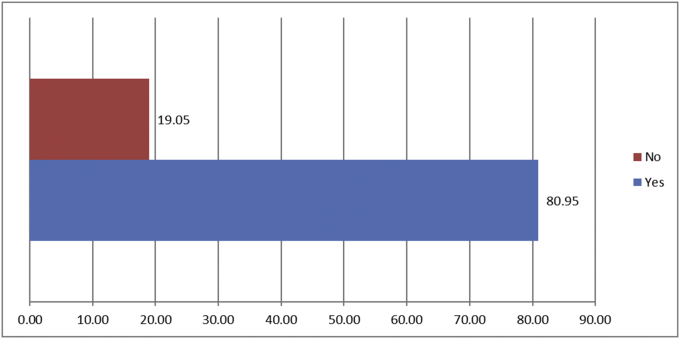
Finally, the response to question 10 is shown in Fig. 10 and 81% of respondents considered that measures of the postoperative systemic inflammatory response, such as CRP, should be included in postoperative care protocols or guidelines to guide postoperative decision making and/or discharge planning.
Fig. 10.
Do you think that a measure of the postoperative systemic inflammatory response, such as C-reactive protein [CRP], should be included in postoperative care protocols or guidelines to guide postoperative decision making and/or discharge planning? [n = 63].
4. Discussion
The results of the present study showed that most respondents were colorectal specialists, European, of consultant grade and worked in Academic Units/Teaching Hospitals. The majority practiced enhanced recovery protocols and used markers of the systemic inflammatory response (i.e. CRP) in the postoperative period to monitor patients and guide discharge. Therefore, of those surgeons with an expressed interest in post-operative management of elective surgery the majority reported that they monitored CRP and considered that a measure of the post-operative systemic inflammatory response should be incorporated into clinical guidelines.
C-reactive protein is the prototypical marker of the systemic inflammatory response reflecting the magnitude of injury [14]. In the context of cancer there is concern that CRP may also be raised in the post-operative period as part of an immune response to the release of tumour antigens. However, the peak operative CRP concentrations are similar following surgery for benign or malignant disease irrespective of open or laparoscopic surgery [15].
Although the majority of survey respondents were at consultant grade it is remarkable, given that the initial reports of the clinical utility of post-operative CRP concentrations were reported less than a decade ago, that this group of surgeons have adopted this measure into their routine clinical practice. This is in part due to the simplicity of the approach and the explosion of interest in the post-operative systemic inflammatory response. Given the survey responses in the present study, it may be problematical, perhaps unethical, to carry out an RCT to prove the efficacy of monitoring the systemic inflammatory response using CRP in the post-operative period. Indeed, this approach is already part of an ERAS protocol following elective resections in some countries [16], [17].
There are a number of implications of the rapid adoption of a CRP first approach to monitoring post-operative complications in patients undergoing elective surgery. Firstly, there may be an increasing requirement for CT resources to be used earlier in the postoperative period. For example, a recent study in the Netherlands, of 399 patients undergoing major abdominal surgery, showed that CT imaging initiated by a combination of a deteriorating clinical picture and an increased CRP had a sensitivity of 91.7% and a specificity of 100% in diagnosing major complications [18]. This study formed the basis of the PREcious trial that will examine continuous monitoring of the postoperative inflammatory response of days 3, 4 and 5 with the addition of a CT-scan should the threshold of CRP > 140 mg/L be exceeded [19].
Secondly, the agreed importance of the postoperative systemic inflammatory response opens up possible treatment options to reduce this response and potentially postoperative complications. For example, increased use of minimally invasive procedures such as laparoscopic/robotic surgery has led to fewer complications [20]. Indeed, most centralised teaching centres are now carrying out their resectional surgery using an enhanced recovery protocol with laparoscopic/robotic techniques. There is good evidence that minimally invasive techniques also produce less surgical stress with a reduced postoperative systemic inflammatory response [15]. The present survey confirms that this is the direction of travel to improve the early but safe discharge from hospital.
Also, pre-operative corticosteroids, given their proven postoperative effect in reducing nausea and vomiting and analgesic requirement, are frequently used in abdominal surgery [21], [22], [23]. Indeed, in two recent meta-analyses the administration of preoperative corticosteroids was reported to significantly reduce postoperative complications and length of stay following abdominal surgery [21], [24]. Other pharmacological methods can also be used to reduce the postoperative systemic inflammatory response and thus improve outcomes. These include the use of NSAIDS, statins and H2 receptor antagonists that can reduce both the local and systemic inflammatory responses [25].
The present study has a number of limitations. The overall response rate was small (6%) and less than the typical response rate of between 20 and 30% for surveys of this type. Actions known to improve survey response rate include reduced complexity of questions, reduced survey length, incentives, and the sending of reminder emails [26]. In the present study the questions were intentionally made as simple as possible and their number limited to ten to encourage a response. A reminder email was sent several weeks after the initial survey was sent out to encourage respondents. However, no incentive for completing the survey was offered. In the present study there were two different cohorts. Surgeons affiliated to the ACPGBI were selected initially as a convenience cohort as their members are often surveyed on aspects of surgical care. However, the response rate was poor and a second cohort with a known interest in the field was surveyed. The response rate in this second cohort was higher although disappointingly low. Therefore, both cohorts may have selection bias. The former primarily due to the low response rate and the latter primarily due to the individuals surveyed. For example, in the first cohort interpretation of the data is difficult due to the small number of observations. Also, in the second cohort surgeons mainly employed minimal access techniques. Therefore, it may be difficult to extrapolate the results obtained to the open technique. A large majority of respondents were from large urban teaching centres and were individuals who have expressed an interest in this field. While it is true that oesophagogastric and hepatobiliary resections are now being centralised, many colonic resections are still carried out on a regional basis. Therefore, the survey results may not reflect practice in a general hospital setting. Although the present survey has a number of limitations it is useful as a first approximation of the clinical use of CRP as a post-operative tool. The present results provide a baseline against which future surveys can be compared.
In the present survey the questions were asked in the context of colorectal cancer since almost all work has been carried out in this cancer. However, recent such work and the present results may also have implications for colorectal resections in benign disease. Further investigation is warranted in benign disease.
In summary, the present study has shown that, at least in specialist surgical units, the majority of consultants measure the systemic inflammatory response, using CRP, in patients following resectional surgery. The majority use this information together with clinical findings to instigate post-operative investigations, guide management, and to guide discharge. It remains for this approach to be incorporated into postoperative care guidelines/protocols.
Ethical approval
None needed this was a questionnaire study.
Sources of funding
None.
Author contribution
Mr Dolan and McSorley designed the questionnaire and distributed it to the cohort of consultants and senior registrars. They conducted the analysis of data and wrote the final report. Prof McMillan and Horgan provided overall supervision and support throughout the entire process.
Conflicts of interest
None.
Guarantor
Mr Ross Dolan.
Research registration unique identifying number (UIN)
N/A.
Acknowledgment
We would like to acknowledge the time and effort taken by all participants in this study.
References
- 1.McMillan D.C. The systemic inflammation-based glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat. Rev. 2013 Aug;39(5):534–540. doi: 10.1016/j.ctrv.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Guthrie G.J., Charles K.A., Roxburgh C.S., Horgan P.G., McMillan D.C., Clarke S.J. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit. Rev. Oncol. Hematol. 2013 Oct;88(1):218–230. doi: 10.1016/j.critrevonc.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Cancer Stats, Cancer Research UK. http://www.cancerresearchuk.org/cancer-info/cancerstats/incidence/commoncancers/. 1-8-2014. 8-9-2015. Ref Type: Online Source.
- 4.Platt J.J., Ramanathan M.L., Crosbie R.A., Anderson J.H., McKee R.F., Horgan P.G. C-reactive protein as a predictor of postoperative infective complications after curative resection in patients with colorectal cancer. Ann. Surg. Oncol. 2012 Dec;19(13):4168–4177. doi: 10.1245/s10434-012-2498-9. [DOI] [PubMed] [Google Scholar]
- 5.Park J.H., Watt D.G., Roxburgh C.S., Horgan P.G., McMillan D.C. Colorectal cancer, systemic inflammation, and outcome: staging the tumor and staging the host. Ann. Surg. 2016 Feb;263(2):326–336. doi: 10.1097/SLA.0000000000001122. [DOI] [PubMed] [Google Scholar]
- 6.Mirnezami A., Mirnezami R., Chandrakumaran K., Sasapu K., Sagar P., Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann. Surg. 2011 May;253(5):890–899. doi: 10.1097/SLA.0b013e3182128929. [DOI] [PubMed] [Google Scholar]
- 7.Woeste G., Muller C., Bechstein W.O., Wullstein C. Increased serum levels of C-reactive protein precede anastomotic leakage in colorectal surgery. World J. Surg. 2010 Jan;34(1):140–146. doi: 10.1007/s00268-009-0304-z. [DOI] [PubMed] [Google Scholar]
- 8.Watt D.G., McSorley S.T., Horgan P.G., McMillan D.C. Enhanced recovery after surgery: which components, if any, impact on the systemic inflammatory response following colorectal surgery?: a systematic review. Med. Baltim. 2015 Sep;94(36):e1286. doi: 10.1097/MD.0000000000001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warschkow R., Beutner U., Steffen T., Muller S.A., Schmied B.M., Guller U. Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann. Surg. 2012 Aug;256(2):245–250. doi: 10.1097/SLA.0b013e31825b60f0. [DOI] [PubMed] [Google Scholar]
- 10.Singh P.P., Zeng I.S., Srinivasa S., Lemanu D.P., Connolly A.B., Hill A.G. Systematic review and meta-analysis of use of serum C-reactive protein levels to predict anastomotic leak after colorectal surgery. Br. J. Surg. 2014 Mar;101(4):339–346. doi: 10.1002/bjs.9354. [DOI] [PubMed] [Google Scholar]
- 11.McDermott F.D., Heeney A., Kelly M.E., Steele R.J., Carlson G.L., Winter D.C. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br. J. Surg. 2015 Apr;102(5):462–479. doi: 10.1002/bjs.9697. [DOI] [PubMed] [Google Scholar]
- 12.Facy O., Paquette B., Orry D., Binquet C., Masson D., Bouvier A. Diagnostic accuracy of inflammatory markers as early predictors of infection after elective colorectal surgery: results from the IMACORS study. Ann. Surg. 2016 May;263(5):961–966. doi: 10.1097/SLA.0000000000001303. [DOI] [PubMed] [Google Scholar]
- 13.Straatman J., Cuesta M.A., Gisbertz S.S., van der Peet D.L. Value of a step-up diagnosis plan: CRP and CT-scan to diagnose and manage postoperative complications after major abdominal surgery. Rev. Esp. Enferm. Dig. 2014 Dec;106(8):515–521. [PubMed] [Google Scholar]
- 14.Gabay C., Kushner I. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 1999 Feb 11;340(6):448–454. doi: 10.1056/NEJM199902113400607. [DOI] [PubMed] [Google Scholar]
- 15.Watt D.G., Horgan P.G., McMillan D.C. Routine clinical markers of the magnitude of the systemic inflammatory response after elective operation: a systematic review. Surgery. 2015 Feb;157(2):362–380. doi: 10.1016/j.surg.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 16.Facy O., Paquette B., Orry D., Binquet C., Masson D., Bouvier A. Diagnostic accuracy of inflammatory markers as early predictors of infection after elective colorectal surgery: results from the IMACORS study. Ann. Surg. 2016 May;263(5):961–966. doi: 10.1097/SLA.0000000000001303. [DOI] [PubMed] [Google Scholar]
- 17.Ortega-Deballon P., Radais F., Facy O., d'Athis P., Masson D., Charles P.E. C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J. Surg. 2010 Apr;34(4):808–814. doi: 10.1007/s00268-009-0367-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Straatman J., Cuesta M.A., Gisbertz S.S., van der Peet D.L. Value of a step-up diagnosis plan: CRP and CT-scan to diagnose and manage postoperative complications after major abdominal surgery. Rev. Esp. Enferm. Dig. 2014 Dec;106(8):515–521. [PubMed] [Google Scholar]
- 19.Straatman J., Cuesta M.A., Schreurs W.H., Dwars B.J., Cense H.A., Rijna H. The PRECious trial PREdiction of Complications, a step-up approach, CRP first followed by CT-scan imaging to ensure quality control after major abdominal surgery: study protocol for a stepped-wedge trial. Trials. 2015;16:382. doi: 10.1186/s13063-015-0903-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Currie A.C., Malietzis G., Jenkins J.T., Yamada T., Ashrafian H., Athanasiou T. Network meta-analysis of protocol-driven care and laparoscopic surgery for colorectal cancer. Br. J. Surg. 2016 Dec;103(13):1783–1794. doi: 10.1002/bjs.10306. [DOI] [PubMed] [Google Scholar]
- 21.McSorley S.T., Horgan P.G., McMillan D.C. The impact of the type and severity of postoperative complications on long-term outcomes following surgery for colorectal cancer: a systematic review and meta-analysis. Crit. Rev. Oncol. Hematol. 2016 Jan;97:168–177. doi: 10.1016/j.critrevonc.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 22.Karanicolas P.J., Smith S.E., Kanbur B., Davies E., Guyatt G.H. The impact of prophylactic dexamethasone on nausea and vomiting after laparoscopic cholecystectomy: a systematic review and meta-analysis. Ann. Surg. 2008 Nov;248(5):751–762. doi: 10.1097/SLA.0b013e3181856024. [DOI] [PubMed] [Google Scholar]
- 23.Waldron N.H., Jones C.A., Gan T.J., Allen T.K., Habib A.S. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br. J. Anaesth. 2013 Feb;110(2):191–200. doi: 10.1093/bja/aes431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Srinivasa S., Kahokehr A.A., Yu T.C., Hill A.G. Preoperative glucocorticoid use in major abdominal surgery: systematic review and meta-analysis of randomized trials. Ann. Surg. 2011 Aug;254(2):183–191. doi: 10.1097/SLA.0b013e3182261118. [DOI] [PubMed] [Google Scholar]
- 25.Park J.H., McMillan D.C., Horgan P.G., Roxburgh C.S. The impact of anti-inflammatory agents on the outcome of patients with colorectal cancer. Cancer Treat. Rev. 2014 Feb;40(1):68–77. doi: 10.1016/j.ctrv.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 26.SurveyMonkey, “Tips and Tricks to Improve Survey Response Rate”. SurveyMonkey. 21-4-2014. Ref Type: Online Source.