Abstract
Background
Late-onset preeclampsia is the most prevalent phenotype of this syndrome; nevertheless, only a few biomarkers for its early diagnosis have been reported. We sought to correct this deficiency using a high through-put proteomic platform.
Methods
A case-control longitudinal study was conducted, including 90 patients with normal pregnancies and 76 patients with late-onset preeclampsia (diagnosed at ≥34 weeks of gestation). Maternal plasma samples were collected throughout gestation (normal pregnancy: 2–6 samples per patient, median of 2; late-onset preeclampsia: 2–6, median of 5). The abundance of 1,125 proteins was measured using an aptamers-based proteomics technique. Protein abundance in normal pregnancies was modeled using linear mixed-effects models to estimate mean abundance as a function of gestational age. Data was then expressed as multiples of-the-mean (MoM) values in normal pregnancies. Multi-marker prediction models were built using data from one of five gestational age intervals (8–16, 16.1–22, 22.1–28, 28.1–32, 32.1–36 weeks of gestation). The predictive performance of the best combination of proteins was compared to placental growth factor (PIGF) using bootstrap.
Results
1) At 8–16 weeks of gestation, the best prediction model included only one protein, matrix metalloproteinase 7 (MMP-7), that had a sensitivity of 69% at a false positive rate (FPR) of 20% (AUC = 0.76); 2) at 16.1–22 weeks of gestation, MMP-7 was the single best predictor of late-onset preeclampsia with a sensitivity of 70% at a FPR of 20% (AUC = 0.82); 3) after 22 weeks of gestation, PlGF was the best predictor of late-onset preeclampsia, identifying 1/3 to 1/2 of the patients destined to develop this syndrome (FPR = 20%); 4) 36 proteins were associated with late-onset preeclampsia in at least one interval of gestation (after adjustment for covariates); 5) several biological processes, such as positive regulation of vascular endothelial growth factor receptor signaling pathway, were perturbed; and 6) from 22.1 weeks of gestation onward, the set of proteins most predictive of severe preeclampsia was different from the set most predictive of the mild form of this syndrome.
Conclusions
Elevated MMP-7 early in gestation (8–22 weeks) and low PlGF later in gestation (after 22 weeks) are the strongest predictors for the subsequent development of late-onset preeclampsia, suggesting that the optimal identification of patients at risk may involve a two-step diagnostic process.
Introduction
Preeclampsia, a frequent complication of pregnancy that affects 5%-8% of all gestations [1–3], is a leading cause of maternal [2–13] and perinatal morbidity and mortality [4,14–16]. Over the last decade, it has become clear that preeclampsia is not a single disorder but a syndrome with many etiologies [17–21], such as abnormal placentation [19,22–24], utero-placental ischemia [20,25–29], vascular disorders of the placenta [30–32], insulin resistance [33–40], systemic maternal inflammation [41–44], endothelial dysfunction [45–50], and imbalance of angiogenic and anti-angiogenic proteins [26,51–76].
A major advance in the classification of preeclampsia was its subdivision into early- (<34 weeks of gestation) and late-onset variants [77–79]. Although other cut-off values between early- and late-onset diseases have been suggested, such as 32 and 36 weeks of gestation [80–82], the value of 34 weeks remains the most commonly used [83–85], presumably because the rate of neonatal morbidity declines considerably after 34 weeks [86–88].
Late-onset preeclampsia is more common than its early-onset variant [83,89] and accounts for 90% of cases [12] and a substantial fraction of maternal complications [12]. For example, in a study from South Africa [89], late-onset preeclampsia accounted for 30% of severe maternal complications, 13% of eclampsia, and 1.9% of fetal deaths [89].
Early-onset preeclampsia is likely caused by a disorder of deep placentation in which there is a failure of physiologic transformation of the spiral arteries, a small placenta with histologic features of maternal vascular underperfusion [90–94], fetal growth restriction or small for gestational age [95–98], and abnormal Doppler velocimetry of umbilical and uterine arteries [99–104]; it frequently requires preterm delivery for maternal and/or fetal indications [12]. By contrast, late-onset preeclampsia seems to be the manifestation of a mismatch between the metabolic demands of the growing fetus close to term and maternal supply [77–79]: the placenta has fewer lesions of maternal vascular underperfusion [90–93] and abnormalities of umbilical/uterine artery Doppler velocimetry [79]. Consistent with these findings, in most cases of late-onset preeclampsia, neonates are appropriate or large for gestational age [105–108].
Maternal hemodynamic status differs in patients with early- and late-onset preeclampsia [79]. These differences can be identified as early as 24 weeks of gestation. Those who develop late-onset preeclampsia have increased cardiac output and relatively unchanged total vascular resistance [79], whereas patients with early-onset preeclampsia have lower cardiac output and relatively increased vascular resistance.
The angiogenic/anti-angiogenic imbalance is milder in late-onset rather than in early-onset preeclampsia [58,59,72,80,82,83,109–112]: indeed, it has been suggested that angiogenic/anti-angiogenic factors can be used as biomarkers to identify patients destined to develop early preeclampsia. These include placental growth factor (PlGF), soluble vascular endothelial growth factor receptor 1, endoglin, and their ratios [55,58,65,82,109,113–117]. Prediction models have also been developed that combine maternal blood pressure, uterine artery Doppler, PlGF [99,101,118–124], pregnancy-associated plasma protein A, and inhibin-A [125]. One such model has been used to identify nulliparous women at risk for early preeclampsia [121] and to design a randomized clinical trial of aspirin in early pregnancy to prevent early-onset preeclampsia [126]. However, the predictive performance (especially in early pregnancy) of models, including angiogenic/anti-angiogenic factors, for the identification of women destined to develop late-onset preeclampsia was lower than those for early-onset disease [82,114,118,119].
New technology, not based on antigen-antibody reactions, has been developed to increase the number of proteins that can be detected simultaneously with a high degree of sensitivity and dynamic range [127,128]. This aptamer-based method uses single-strand DNA or RNA molecules that bind to proteins, peptides, or other pre-defined molecules with high affinity and specificity. The use of aptamer technology for the discovery of biomarkers for cardiovascular disease [129] and other medical conditions [130–135] has recently been reported, and we have previously reported changes in the maternal plasma proteome as a function of gestational age [128]. Therefore, we used this high through-put proteomic platform to identify proteins that can serve as biomarkers for the identification of patients who subsequently develop late-onset preeclampsia.
Materials and methods
Study design
A retrospective nested case-control study was designed to include 90 patients with normal pregnancies (controls) and 76 patients with late-onset preeclampsia defined as preeclampsia diagnosed at ≥34 weeks of gestation). Patients were enrolled between February 2007 and Dec 2013 as part of a longitudinal cohort study conducted at the Center for Advanced Obstetrical Care and Research of the Perinatology Research Branch, NICHD/NIH/DHHS, the Detroit Medical Center and Wayne State University. Plasma samples were collected at the time of each prenatal visit scheduled at four-week intervals from the first or early second trimester until delivery. Each patient had at least two samples collected during the following gestational age intervals: 8-<16 weeks, 16-<24 weeks, 24-<28 weeks, 28-<32 weeks, 32-<37 weeks and >37 weeks. The median number (range) of samples per patient was 5(2–6) for cases and 2 (2–6) for controls. All patients provided written informed consent, and the use of biological specimens, as well as clinical and ultrasound data for research purposes, were approved by the Wayne State University Human Investigation Committee and the Institutional Review Board of NICHD.
Clinical definitions
Preeclampsia was defined as new-onset hypertension that developed after 20 weeks of gestation (systolic or diastolic blood pressure ≥140 and/or ≥90 mm Hg, respectively, measured on at least two occasions, 4 hours to 1 week apart) and proteinuria (≥300 mg in a 24-hour urine collection, or two random urine specimens obtained 4 hours to 1 week apart containing ≥1+ by dipstick or one dipstick demonstrating ≥2+ protein) [83,136].
Early-onset preeclampsia was defined as preeclampsia diagnosed before 34 weeks [83]. Late-onset preeclampsia was defined as preeclampsia diagnosed at or after 34 weeks of gestation.
Mild preeclampsia was diagnosed as preeclampsia with systolic blood pressure < 160 mmHg, or diastolic blood pressure < 110 mmHg, platelet count ≥ 100,000 per mm3, non-elevated liver enzymes, absence of renal insufficiency, pulmonary edema, cyanosis, new-onset cerebral/visual disturbances, and/or right upper quadrant or epigastric pain [20,85].
Severe preeclampsia was diagnosed as preeclampsia with systolic blood pressure ≥ 160 mmHg, or diastolic blood pressure ≥ 110 mmHg, platelet count < 100,000 per mm3, elevated liver enzymes, renal insufficiency, pulmonary edema or cyanosis, new-onset cerebral/visual disturbances, and/or right upper quadrant or epigastric pain [20,85].
Body mass index (BMI) was calculated as follows: BMI = [weight (in pounds) × 703)/height2 (in inches)]. Obesity was defined as BMI ≥ 30 kg/m2 [137].
Proteomic analysis
Maternal plasma protein abundance was determined using the SOMAmer (Slow Off-rate Modified Aptamers) platform and its reagents that allowed the abundance of 1,125 proteins to be profiled [138–140]. Proteomics profiling services were provided by Somalogic, Inc. (Boulder, CO, USA) in December 2014.
The serum samples were diluted and then incubated with the respective SOMAmer mixes pre-immobilized onto streptavidin-coated beads. The beads were washed in order to remove all non-specifically bound proteins and other matrix constituents. Proteins that remained bound to their cognate SOMAmer reagents were tagged using an NHS-biotin reagent. After the labeling reaction, the beads were exposed to an anionic competitor solution to prevent non-specific interactions from reforming after disruption.
Using this approach, pure cognate-SOMAmer complexes and unbound (free) SOMAmer reagents are released from the streptavidin beads using ultraviolet light that cleaves the photo-cleavable linker used to quantitate proteins. The photo-cleavage eluate, which contains all SOMAmer reagents (some bound to a biotin-labeled protein and some free), was separated from the beads and then incubated with a second streptavidin-coated bead that binds the biotin-labeled proteins and the biotin-labeled protein-SOMAmer complexes. The free SOMAmer reagents were then removed using subsequent washing steps. In the final elution step, protein-bound SOMAmer reagents were released from their cognate proteins using denaturing conditions. These SOMAmer reagents were then quantified by hybridization to custom DNA microarrays. The Cyanine-3 signal from the SOMAmer reagent was detected on microarrays and used for quantification [138–140].
Statistical analysis
Demographics data analysis
Clinical characteristics of the patient population were summarized as median and inter-quartile ranges (IQR) for continuous variables or as percentages for categorical variables. Comparisons of the demographics variables between groups were performed using a Fisher’s exact test (for binary variables) and the Wilcoxon rank-sum test for continuous variables.
Data transformation
The raw protein abundance data consisted of relative fluorescence units obtained from scanning the microarrays with a laser scanner. A sample-by-sample adjustment of the overall signal within a single plate (85 samples processed per plate/run) was performed in three steps: Hybridization Control Normalization, Median Signal Normalization, and Calibration, using the manufacturer’s protocol. Outlier protein abundance values above 2 × the 98th percentile of all samples, were replaced with 2 × the 98th percentile of all samples (data thresholding) (See S1 File for the protein abundance data after the thresholding step). Protein abundance was then log (base 2) transformed to improve normality. Linear mixed-effects models with cubic splines (number of knots = 3) were used to model protein abundance in controls as a function of gestational age using the lme4 package [141] under the R statistical language and environment (www.r-project.org). Data for all samples was then expressed as multiples-of-the-mean (MoM) values for the corresponding gestational age in normal pregnancies.
Development of multi-marker prediction models
The goal of this analysis was to develop parsimonious, accurate prediction models by using protein abundance in each gestational age interval separately (8–16, 16.1–22, 22.1–28, 28.1–32, 32.1–36 weeks of gestation) applying predictive modeling techniques for omics data that we previously reported [142–144]. Log (base 2) MoM values for one protein at a time were used to fit a Linear Discriminant Analysis (LDA) model, and compute, by leave-one-out cross-validation (LOOCV), a classification performance measure for each protein. This performance measure was the partial Area Under the Receiver Operating Characteristic (ROC) curve (pAUC) using a cut-off of 0.5 false positive rate. The use of a partial as opposed to the full area under the ROC curve was chosen to emphasize the need to find proteins that have high sensitivity at low false positive rates. Further, proteins that did not change at least 10% in average abundance between the groups were removed from the analysis. Then, LDA models were fit using increasing sets of up to 5 of the top proteins ranked by the pAUC. To enforce model parsimony, the inclusion of each additional protein was conditioned on the increase of 0.01 units in a pAUC statistic. Classification performance indices [AUC, sensitivity, specificity, positive and negative predictive values, likelihood ratio (+) and (-)] were obtained for the best combinations of markers in each interval by LOOCV. While this accounts for biases due to over-fitting of the data for a given set of selected proteins, it does not account for the fact that those proteins were selected from a large pool of candidate predictors. Therefore, classification performance indices were also obtained using bootstrap. With this approach, after data transformation into MoM, patients (both cases and controls) were selected with replacement. All analysis steps involved in the prediction model development (including selection of predictor proteins) were performed using only data from the selected patients (training set) and prediction performance was calculated by applying the resulting model on the patients left out (test set). Averages of 100 such bootstrap iterations are reported and the discussion of results is based primarily on these performance estimates since they are considered most robust.
Differential abundance analysis
Since the classifier development pipeline described above is focused on finding the most accurate, parsimonious set of proteins that predict late-onset preeclampsia, it will not necessarily retain all proteins showing evidence of differential abundance. Therefore, a complementary analysis was performed to test for differences between mean log (base 2) MoM values between cases and controls at each gestational age interval. Linear models with coefficient significance evaluated via moderated t-tests were implemented using the limma package [145] of Bioconductor repository [146]. With this procedure, standard deviation estimates of log2 MoM values for each protein are shrunk toward a common (pooled) value to improve robustness. Significance was inferred based on the false discovery rate adjusted p-value (q-value) <0.25 and fold-change in abundance >1.1 fold after adjusting for BMI, smoking status, maternal age, and parity.
Gene ontology enrichment analysis
Proteins selected as differentially abundant between late-onset preeclampsia and normal pregnancy in each interval of gestation were mapped to Entrez gene identifiers [147] based on Somalogic, Inc., annotation, and then to gene ontology [148]. Biological processes over-represented among the proteins that changed with late-onset preeclampsia were identified using a Fisher’s exact test. Gene ontology terms with three or more hits and q-values <0.1 were considered significantly enriched.
Results
Clinical characteristics of the study population
Women with late-onset preeclampsia had a lower median gestational age at delivery (p<0.001) and a higher median maternal BMI (p = 0.03) than the controls. Thirty-seven percent (28/76) of cases had severe preeclampsia and 63% (48/76) had mild preeclampsia. Median gestational age at delivery was lower both in patients who had mild preeclampsia and in those who had severe preeclampsia than in the controls (p<0.001), but the median maternal BMI was higher than the controls only in patients who had severe preeclampsia (p = 0.01) (Table 1).
Table 1. Demographic characteristics of the study population.
| Characteristic | Normal (n = 90) | Late PE (n = 76) | Mild Late PE (n = 48) | Severe Late PE (n = 28) |
|---|---|---|---|---|
| Gestational age at delivery (weeks) | 39.4 (39.0–40.4) | 38.7 (37.7–39.4) [p<0.001] | 38.8 (37.7–39.4) [p<0.001] | 38.6 (37.7–39.5) [p<0.001] |
| BMI (kg/m2) | 26.5 (22.8–33.2) | 30.0 (24.8–36.2) [p = 0.03] | 28.4 (24.0–33.0) [p = 0.23] | 32.5 (27.2–38.7) [p = 0.01] |
| Maternal age (years) | 24 (21.0–27.8) | 22 (20.0–29.0) [p = 0.45] | 22.5 (20.0–28.3) [p = 0.57] | 22 (19.0–29.3) [p = 0.5] |
| Smoking | 18 (20%) | 13 (17.1%) [p = 0.7] | 9 (18.8%) [p = 1] | 4 (14.2%) [p = 0.6] |
| Nulliparity | 26 (28.9%) | 32 (42.1%) [p = 0.1] | 22 (45.8%) [p = 0.06] | 10 (35.7%) [p = 0.5] |
Data is presented as median (interquartile range) or as percentage (n); BMI, body mass index. P values are given for the comparison to the normal pregnancy group.
Proteomic prediction models for late-onset preeclampsia prior to diagnosis
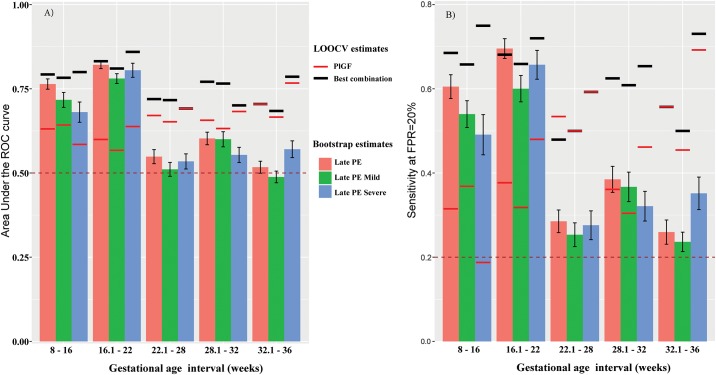
Fig 1 depicts a summary of the LOOCV (black segments for best combination of markers; red segments, PlGF alone) and bootstrap (bars with 95% CI) based performance estimates for the prediction of late preeclampsia. The bootstrap estimates of AUC (Fig 1A) and sensitivity at a 20% false positive rate (FPR) (Fig 1B) achieved by the best combinations of proteins were significantly higher than those of PlGF in the first two gestational age intervals (8–16 and 16.1–22 weeks) (bars higher than red line segments).
Fig 1. Prediction of late-onset preeclampsia using multi-protein markers.
The area under the Receiver Operating Characteristic (ROC) curve (A) and the sensitivity at a 20% false positive rate (FPR) (B) are shown. Estimates obtained by leave-one-out cross-validation (LOOCV) for the best combination of markers (Table 2) is shown as horizontal black segments for late preeclampsia (PE) as well as for mild and severe phenotypes of the disease. The LOOCV performance of PlGF alone is shown with red horizontal segments. The bars in this figure represent average (whiskers are with 95% confidence intervals [CI]) prediction performance obtained from 100 bootstrap iterations. For prediction of severe preeclampsia at 28.1–32 weeks and for overall preeclampsia at 32.1–36 weeks, PlGF was the only predictor selected in the final model.
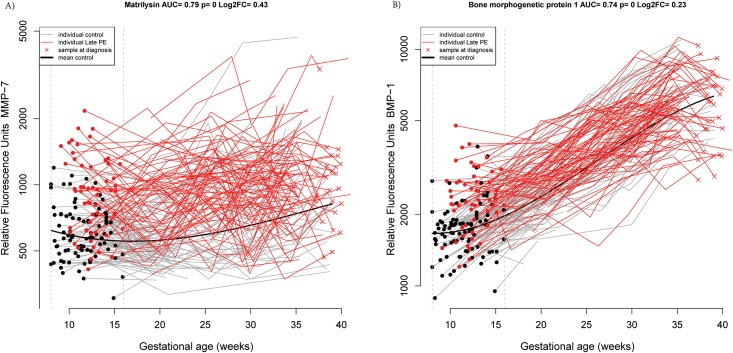
At 8–16 weeks of gestation, the best combination of proteins included only matrix metalloproteinase 7 (MMP-7) that had a sensitivity of 69% at a FPR of 20% (black segment on top of the red bar at 8–16 weeks, Fig 1B) and 57% at a FPR of 10% (AUC = 0.79; see black segment at 8–16 weeks, Fig 1A and Table 2). Individual patient longitudinal MMP-7 profiles are depicted in Fig 2A, highlighting the differences in the samples taken between 8–16 weeks of gestation. When random sets of cases and controls were selected with replacement, and the entire procedure to build the classification model was repeated, MMP-7 was chosen as the best predictor in 88 of the 100 bootstrap trials and the typical (mean) AUC of the prediction model was 0.76 (see Table 3, and red bar at 8–16 weeks Fig 1A). The consistency of bootstrap-based (AUC = 0.76) and final model estimates (AUC = 0.79) of prediction performance suggest minimal to no data over-fitting. The second most frequently selected predictor protein (23/100 iterations) either by itself or in combination with other proteins was BMP-1 (AUC = 0.74) (see Fig 2B).
Table 2. Summary of prediction performance of multi-protein prediction models for late-onset, mild late-onset, and severe late preeclampsia.
| Outcome | Sample GA (weeks) | N (Ctrls. /Cases) | Model Predictors | AUC | Sens. FPR = 20% | Sens. | Spec. | PPV | NPV | LR(+) | LR(-) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Late PE | 8–16 | 89/54 | MMP-7 | 0.79 | 0.69 | 0.57 | 0.90 | 0.78 | 0.78 | 5.7 | 0.47 |
| Late PE | 16.1–22 | 87/69 | MMP-7 | 0.83 | 0.68 | 0.62 | 0.89 | 0.81 | 0.75 | 5.4 | 0.43 |
| Late PE | 22.1–28 | 43/73 | RAN+METAP1 | 0.72 | 0.48 | 0.23 | 0.86 | 0.74 | 0.40 | 1.7 | 0.89 |
| Late PE | 28.1–32 | 40/72 | RAN+CAMK2A+TF | 0.77 | 0.63 | 0.50 | 0.85 | 0.86 | 0.49 | 3.3 | 0.59 |
| Late PE | 32.1–36 | 39/70 | PlGF | 0.70 | 0.56 | 0.26 | 0.87 | 0.78 | 0.40 | 2.0 | 0.85 |
| Mild | 8–16 | 89/38 | MMP-7 + Phosphoglycerate mutase 1 | 0.78 | 0.66 | 0.47 | 0.89 | 0.64 | 0.80 | 4.2 | 0.59 |
| Mild | 16.1–22 | 87/44 | MMP-7 | 0.81 | 0.66 | 0.59 | 0.90 | 0.74 | 0.81 | 5.7 | 0.46 |
| Mild | 22.1–28 | 43/46 | METAP1+RAN | 0.72 | 0.50 | 0.17 | 0.88 | 0.62 | 0.50 | 1.5 | 0.93 |
| Mild | 28.1–32 | 40/46 | TF+RAN+FER | 0.77 | 0.61 | 0.41 | 0.85 | 0.76 | 0.56 | 2.8 | 0.69 |
| Mild | 32.1–36 | 39/44 | TF | 0.68 | 0.50 | 0.43 | 0.90 | 0.83 | 0.58 | 4.2 | 0.63 |
| Severe | 8–16 | 89/16 | MMP-7 | 0.80 | 0.75 | 0.63 | 0.89 | 0.50 | 0.93 | 5.6 | 0.42 |
| Severe | 16.1–22 | 87/25 | MMP-7 | 0.86 | 0.72 | 0.68 | 0.90 | 0.65 | 0.91 | 6.6 | 0.36 |
| Severe | 22.1–28 | 43/27 | PlGF | 0.69 | 0.59 | 0.52 | 0.88 | 0.74 | 0.75 | 4.5 | 0.54 |
| Severe | 28.1–32 | 40/26 | PTP-1B | 0.70 | 0.65 | 0.42 | 0.93 | 0.79 | 0.71 | 5.6 | 0.62 |
| Severe | 32.1–36 | 39/26 | PlGF + Histone H2A.z | 0.79 | 0.73 | 0.50 | 0.82 | 0.65 | 0.71 | 2.8 | 0.61 |
GA: gestational age; AUC: area under the receiver operating characteristic curve; FPR: false-positive rate; Sens. Sensitivity, Spec. Specificity, PPV: Positive Predicted Value, NPV: Negative Predicted Value, LR: Likelihood Ratio (LR).
Fig 2. Longitudinal maternal plasma MMP-7 (A) and BMP−1 (B) abundance in normal pregnancy and late-onset preeclampsia cases, highlighting differences in the 8–16 weeks interval.
Each line corresponds to one patient (grey = normal pregnancy, red = late-onset preeclampsia). Individual dots correspond to samples in the current gestational age interval (see vertical interrupted lines). The thick black line represents the mean value in normal pregnancy estimated by linear mixed-effects models. AUC is the area under the Receiver Operating Characteristic (ROC) curve of the protein using data in the current interval only; p is the nominal significance p-value comparing mean MoM values between groups with a moderated t-test. Log2FC is the log (base 2) of the fold-change between cases and controls, with negative values denoting lower MoM values in cases than in controls.
Table 3. Summary of prediction performance for late-onset preeclampsia evaluated by bootstrap.
| Outcome | Sample GA (weeks) | AUC | Sens. | Spec. | Predictor Symbols (# of inclusions in the best combination) |
|---|---|---|---|---|---|
| Late PE | 8–16 | 0.76 | 0.61 | 0.80 | MMP-7(88); BMP-1(23); CDK8/cyclin C(12) |
| Late PE | 16.1–22 | 0.82 | 0.70 | 0.80 | MMP-7(94); HMG-1(18); gpIIbIIIa(17); Integrin aVb5(10) |
| Late PE | 22.1–28 | 0.55 | 0.29 | 0.80 | PlGF(24); METAP1(16); MMP-7(15); RAN(12) |
| Late PE | 28.1–32 | 0.60 | 0.38 | 0.80 | RAN(44); CAMK2A(23); TF(14); FER(12); CAMK2D(11) |
| Late PE | 32.1–36 | 0.52 | 0.26 | 0.79 | Cathepsin B(21); PlGF(20); BMPER(11) |
| Mild | 8–16 | 0.72 | 0.54 | 0.80 | MMP-7(74); Phosphoglycerate mutase 1(17); BMP-1(12); CDK8/cyclin C(10) |
| Mild | 16.1–22 | 0.78 | 0.60 | 0.80 | MMP-7(84); gpIIbIIIa(27); HMG-1(12) |
| Mild | 22.1–28 | 0.51 | 0.25 | 0.79 | RAN(15); PlGF(13); Cathepsin B(10) |
| Mild | 28.1–32 | 0.60 | 0.37 | 0.80 | RAN(41); TF(30); FER(20) |
| Mild | 32.1–36 | 0.49 | 0.24 | 0.79 | Cathepsin B(16); TF(13) |
| Severe | 8–16 | 0.68 | 0.49 | 0.80 | MMP-7(52); BMP-1(23); PPID(10) |
| Severe | 16.1–22 | 0.81 | 0.66 | 0.80 | MMP-7(79); Integrin aVb5(34); HMG-1(18) |
| Severe | 22.1–28 | 0.53 | 0.28 | 0.79 | PlGF(20) |
| Severe | 28.1–32 | 0.55 | 0.32 | 0.80 | PTP-1B(18) |
| Severe | 32.1–36 | 0.57 | 0.35 | 0.79 | PlGF(24); FCN2(10) |
The number in parentheses following the name of each protein in the column labeled Predictor Symbols represents the number of bootstrap iterations for which the protein was selected in the best predictor combination. Only proteins selected 10 times or more are listed. AUC: Area under the Receiver Operating Characteristic Curve, Sens. Sensitivity, Spec. Specificity.
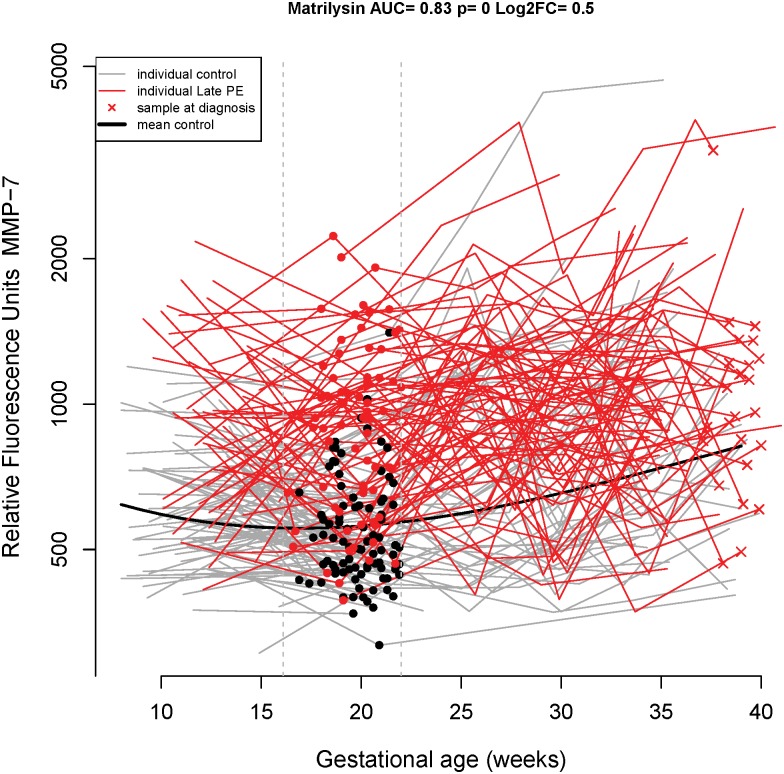
At 16.1–22 weeks of gestation, MMP-7 was again the single best predictor of late-onset preeclampsia with a sensitivity of 68% at a FPR of 20%, and 62% at a FPR of 10% (AUC = 0.83; 0.82 bootstrap estimate) (Tables 2 and 3). Longitudinal MMP-7 profiles emphasizing the differences in the samples taken between 16.1 to 22 weeks of gestation are shown in Fig 3. MMP-7 was selected in the best model of 94 of the 100 bootstrap trials with the next most frequently selected proteins HMG-1 (high-mobility group protein box-1) and gpIIbIIIa (Integrin alpha-IIb: beta-3 complex) being selected only 18 and 17 times, respectively.
Fig 3. Longitudinal maternal plasma MMP-7 abundance in normal pregnancy and late-onset preeclampsia cases, highlighting differences in the 16.1–22 weeks interval.
See the Fig 1 legend for more details.
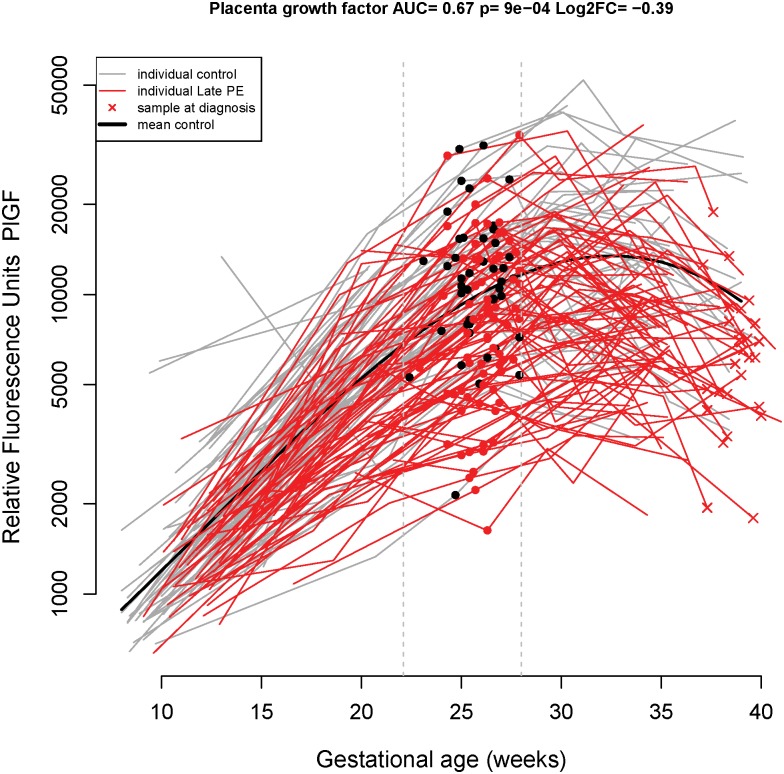
At 22.1–28 weeks of gestation, the proteomics profile predicted late-onset preeclampsia with a sensitivity of 48% at a FPR of 20% and with a sensitivity of 23% at FPR of 10% (AUC = 0.72). The two proteins included in the final model at this gestational age interval were RAN (RAs-related Nuclear protein, also known as GTP-binding nuclear protein Ran) and METAP1 (Methionine aminopeptidase 1). However, the bootstrap-estimated performance of combinations of proteins at this gestational age interval was substantially lower (29% sensitivity at a FPR of 20%, AUC = 0.55): PlGF (Fig 4: longitudinal profiles) was selected most frequently in the best model (24/100 times) followed by METAP1 (16/100), MMP-7(15/100) and RAN (12/100) (Table 3).
Fig 4. Longitudinal maternal plasma PlGF abundance in normal pregnancy and late-onset preeclampsia cases, highlighting differences in the 22.1–28 weeks interval.
See the Fig 1 legend for more details.
Prediction performance for late-onset preeclampsia at the 28.1–32 and 32.1–36 week intervals did not exceed the values obtained at the 8–16 and 16.1–22 week intervals, with proteins such as RAN, Calcium/calmodulin-dependent protein kinase type II alpha chain (CAMK2A), PlGF, tissue factor (TF), and Cathepsin B being among the most frequently (14 to 44 times out of 100) included as predictors in the optimal LDA prediction models for late-onset preeclampsia (Table 3).
Prediction of late-onset preeclampsia according to its severity
When severe and mild late-onset preeclampsia cases were compared separately against the controls, the estimated prediction performance of multi-protein models was very similar to the one for overall late-onset preeclampsia (Fig 1A and 1B and Tables 2 and 3). Although for the 8–16 and 16.1–22 weeks’ intervals when MMP-7 was selected as the best model in a majority of bootstrap trials, there were differences in the top proteins included for prediction of subsequent mild as opposed to severe late-onset preeclampsia (Table 3). PlGF, PTP-1B (Tyrosine-protein phosphatase non-receptor type 1), and FCN2 (Ficolin-2) were the most frequently selected to predict severe preeclampsia (10-24/100 times) while RAN, TF, FER, and Cathepsin B were the most frequently selected in the best combinations of predictors of mild late-onset preeclampsia (Table 3). Since combinations of proteins did not perform any better than PlGF alone, we describe only the prediction performance indices for PlGF in the intervals from 22.1–36 weeks of gestation (see red line segments in Fig 1): at 22.1–28 weeks, the sensitivity of PlGF was 53% (FPR = 20%) for overall late-onset preeclampsia (50% for mild and 59% for severe preeclampsia) (Fig 1B); at 28.1–32 weeks, the sensitivity of PlGF was 36% (FPR = 20%) for overall late-onset preeclampsia (30% for mild and 46% for severe preeclampsia) (Fig 1B). At 32.1–36 weeks, the sensitivity of PlGF was 56% (FPR = 20%) for overall late-onset preeclampsia (45% for mild and 69% for severe preeclampsia) (Fig 1B).
Differential protein abundance summary
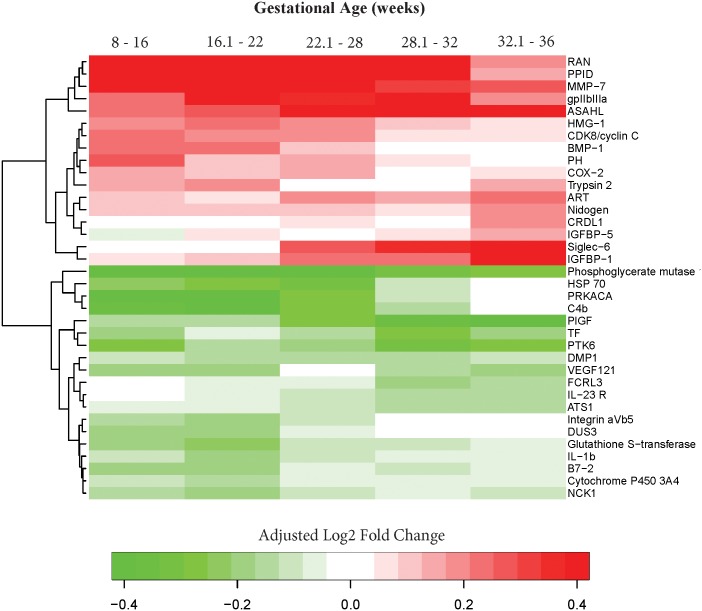
In addition to the few proteins that were included in the parsimonious models predictive of late-onset preeclampsia at different gestational age intervals (Table 2), 36 additional proteins showed evidence for differential abundance after adjusting for BMI, smoking status, maternal age, and parity (q-value<0.25 and fold change >1.1) in at least one interval of gestation. Table 4 shows the linear fold-changes in the MoM values between late-onset preeclampsia and the control groups, as well as the nominal and FDR adjusted p-values (q-values) for each gestational age interval. The heatmap summarizes the differential abundance patterns across all gestational age intervals considered (Fig 5 and Table 4). Notably, the abundance of MMP-7, CDK8/cyclin C (Cyclin-dependent kinase 8:Cyclin-C complex), PPID (Peptidylprolyl isomerase D), and RAN were higher while the abundance of HSP70 (Heat shock 70 kDa protein 1A/1B) was lower in cases compared to the controls in the first three gestational age intervals (8–16, 16.1–22, 22.1–28 weeks).
Table 4. Summary of differential abundance analysis between late-onset preeclampsia and normal pregnancy in five intervals of gestation.
| 8–16 (weeks) | 16.1–22 (weeks) | 22.1–28 (weeks) | 28.1–32 (weeks) | 32.1–36 (weeks) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SYMBOL | FC | Sig. | FC | Sig. | FC | Sig. | FC | Sig. | FC | Sig. |
| PPID | 1.4 | Yes | 1.4 | Yes | 1.6 | Yes | 1.3 | No | 1.1 | No |
| RAN | 1.4 | Yes | 1.4 | Yes | 1.6 | Yes | 1.5 | No | 1.1 | No |
| MMP-7 | 1.4 | Yes | 1.4 | Yes | 1.3 | Yes | 1.2 | No | 1.2 | No |
| CDK8/cyclin C | 1.2 | Yes | 1.1 | Yes | 1.1 | Yes | 1.1 | No | 1.0 | No |
| HSP 70 | -1.2 | Yes | -1.2 | Yes | -1.2 | Yes | -1.1 | No | 1.0 | No |
| BMP-1 | 1.2 | Yes | 1.2 | Yes | 1.1 | No | 1.0 | No | -1.0 | No |
| HMG-1 | 1.1 | Yes | 1.2 | Yes | 1.1 | No | 1.1 | No | 1.0 | No |
| Glutathione S-transferase Pi | -1.1 | Yes | -1.2 | Yes | -1.1 | No | -1.1 | No | -1.0 | No |
| C4b | -1.3 | Yes | -1.3 | Yes | -1.2 | No | -1.1 | No | -1.0 | No |
| PH | 1.2 | Yes | 1.1 | No | 1.1 | No | 1.0 | No | 1.0 | No |
| COX-2 | 1.1 | Yes | 1.1 | No | 1.1 | No | 1.0 | No | 1.0 | No |
| Phosphoglycerate mutase 1 | -1.8 | Yes | -1.4 | No | -1.4 | No | -1.2 | No | -1.2 | No |
| gpIIbIIIa | 1.2 | No | 1.5 | Yes | 1.3 | No | 1.3 | No | 1.1 | No |
| Trypsin 2 | 1.1 | No | 1.1 | Yes | 1.0 | No | -1.0 | No | 1.1 | No |
| Cytochrome P450 3A4 | -1.1 | No | -1.1 | Yes | -1.0 | No | -1.1 | No | -1.0 | No |
| IL-1b | -1.1 | No | -1.1 | Yes | -1.1 | No | -1.0 | No | -1.0 | No |
| DMP1 | -1.1 | No | -1.1 | Yes | -1.1 | No | -1.1 | No | -1.1 | No |
| Integrin aVb5 | -1.1 | No | -1.1 | Yes | -1.1 | No | -1.0 | No | 1.0 | No |
| NCK1 | -1.1 | No | -1.1 | Yes | -1.1 | No | -1.1 | No | -1.1 | No |
| B7-2 | -1.1 | No | -1.1 | Yes | -1.0 | No | -1.1 | No | -1.0 | No |
| VEGF121 | -1.1 | No | -1.1 | Yes | -1.0 | No | -1.1 | No | -1.1 | No |
| DUS3 | -1.1 | No | -1.1 | Yes | -1.0 | No | -1.0 | No | 1.0 | No |
| PRKACA | -1.3 | No | -1.3 | Yes | -1.2 | No | -1.1 | No | -1.0 | No |
| ASAHL | 1.2 | No | 1.2 | No | 1.4 | No | 1.4 | Yes | 1.4 | Yes |
| TF | -1.1 | No | -1.0 | No | -1.1 | No | -1.2 | Yes | -1.1 | No |
| PTK6 | -1.2 | No | -1.1 | No | -1.1 | No | -1.2 | Yes | -1.2 | No |
| Nidogen | 1.1 | No | 1.1 | No | 1.1 | No | 1.1 | No | 1.1 | Yes |
| ART | 1.1 | No | 1.1 | No | 1.1 | No | 1.1 | No | 1.2 | Yes |
| IGFBP-1 | 1.1 | No | 1.1 | No | 1.2 | No | 1.2 | No | 1.3 | Yes |
| Siglec-6 | 1.0 | No | 1.0 | No | 1.2 | No | 1.3 | No | 1.5 | Yes |
| FCRL3 | 1.0 | No | -1.0 | No | -1.0 | No | -1.1 | No | -1.1 | Yes |
| CRDL1 | 1.0 | No | 1.0 | No | 1.0 | No | 1.0 | No | 1.1 | Yes |
| IL-23 R | -1.0 | No | -1.0 | No | -1.1 | No | -1.1 | No | -1.1 | Yes |
| IGFBP-5 | -1.0 | No | 1.0 | No | 1.0 | No | 1.0 | No | 1.1 | Yes |
| ATS1 | -1.0 | No | -1.1 | No | -1.1 | No | -1.1 | No | -1.1 | Yes |
| PlGF | -1.1 | No | -1.1 | No | -1.2 | No | -1.3 | No | -1.3 | Yes |
Thirty-six proteins that were significant (Sig.) (q<0.25 and fold change >1.1) in at least one interval are shown. Adjustment was performed for BMI, maternal age, parity and smoking. FC: linear fold change, with negative values denoting lower while positive values denoting higher level in cases than in controls. See S2 File for full names of proteins, p-values and q-values as well as for which proteins change in abundance during gestation.
Fig 5. A summary of differential protein abundance between late-onset preeclampsia and normal pregnancy throughout gestation.
The value shown using a color scheme represents the log2 fold-change in MoM values between cases and controls (green = lower, red = higher mean MoM in cases than in controls). Absolute fold-changes >1.3 (absolute log2 fold change >0.4) were re-set to 1.3 in order to enhance visualization of the data.
Of the 36 proteins associated with late-onset preeclampsia in at least one gestational age interval, 11 (31%) were among those modulated during gestation in normal pregnancy [149] (OR = 4.3, p<0.001) (Table 4). This supports our prediction that proteins that change with gestation in normal pregnancy could be helpful in understanding obstetrical complications and may serve as biomarkers for the prediction of these disorders.
Biological processes perturbed in late-onset preeclampsia
Gene ontology analysis of the proteins that changed significantly between the cases and controls was performed for each gestational age interval. Despite the inherent limited power of such analysis (due to few significant proteins at each gestational age interval), we have identified biological processes perturbed in late-onset preeclampsia. These gene ontologies included: small molecule metabolic process and positive regulation of apoptotic process at 8–16 weeks, and positive regulation of vascular endothelial growth factor receptor signaling pathway, positive regulation of cell adhesion, and extracellular matrix organization at 16–22 weeks (OR = 3.1–38.1, all q<0.1) (Table 5).
Table 5. Gene ontology (GO) biological processes associated with protein abundance changes with late-onset preeclampsia.
| GA Interval | Name | N | Proteins | OR | p | q |
|---|---|---|---|---|---|---|
| 8–16 | small molecule metabolic process | 5 | BMP-1;Glutathione S-transferase Pi;Phosphoglycerate mutase 1;RAN;COX-2 | 5.8 | 0.007 | 0.01 |
| 8–16 | positive regulation of apoptotic process | 3 | PPID;HMG-1;COX-2 | 8.1 | 0.012 | 0.01 |
| 16–22 | positive regulation of vascular endothelial growth factor receptor signaling pathway | 3 | gpIIbIIIa;IL-1b;VEGF121 | 38.1 | 0.000 | 0.00 |
| 16–22 | positive regulation of cell adhesion | 3 | Integrin aVb5;Trypsin 2;VEGF121 | 14.7 | 0.002 | 0.02 |
| 16–22 | extracellular matrix organization | 6 | MMP-7;gpIIbIIIa;BMP-1;Integrin aVb5;DMP1;Trypsin 2 | 4.5 | 0.006 | 0.04 |
| 16–22 | cell migration | 3 | gpIIbIIIa;Integrin aVb5;NCK1 | 6.5 | 0.017 | 0.07 |
| 16–22 | innate immune response | 7 | HMG-1;C4b;PRKACA;NCK1;B7-2;Trypsin 2;DUS3 | 3.1 | 0.022 | 0.07 |
| 16–22 | positive regulation of transcription from RNA polymerase II promoter | 5 | HMG-1;CDK8/cyclin C;NCK1;IL-1b;VEGF121 | 3.7 | 0.023 | 0.07 |
| 16–22 | positive regulation of protein phosphorylation | 3 | gpIIbIIIa;IL-1b;VEGF121 | 5.4 | 0.027 | 0.07 |
| 16–22 | negative regulation of transcription from RNA polymerase II promoter | 3 | HMG-1;PPID;VEGF121 | 4.8 | 0.035 | 0.08 |
| 16–22 | positive regulation of transcription, DNA-templated | 3 | RAN;IL-1b;B7-2 | 4.2 | 0.047 | 0.09 |
| 16–22 | extracellular matrix disassembly | 3 | MMP-7;BMP-1;Trypsin 2 | 4.1 | 0.053 | 0.09 |
GA: gestational age, N: number of significant proteins belonging to the GO term; OR: enrichment odds ratios; p: p value, q: false discovery rate adjusted p-value. P-values displayed as 0.00 and 0.000 should be considered <0.01 and <0.001 respectively.
Discussion
Principal findings of the study
1) The strongest predictors of late-onset preeclampsia are the elevated abundance of maternal plasma MMP-7 early in gestation (8–22 weeks) and the low maternal plasma abundance of PlGF later in gestation (after 22 weeks); 2) the high abundance of MMP-7, CDK8/cyclin C, PPID, and RAN and the low abundance of HSP70 at 8–28 weeks of gestation were associated with late-onset preeclampsia after adjusting for covariates; 3) biological processes perturbed at 8–16 weeks of gestation in patients destined to develop late-onset preeclampsia included: a) a small-molecule metabolic process and b) a positive regulation of the apoptotic process (at 8–16 weeks), while, at 16–22 weeks, the biological processes included a) the positive regulation of the vascular endothelial growth factor receptor signaling pathway, b) the positive regulation of cell adhesion, and c) the extracellular matrix organization; and 4) from 22.1 weeks of gestation onward, the set of proteins most predictive differed in patients who subsequently developed mild versus severe late-onset preeclampsia.
Early-onset vs. late-onset preeclampsia: Two different disorders
The syndrome of preeclampsia has been classified into two major clinical conditions, according to the gestational age at diagnosis and delivery [77–79]. Early-onset preeclampsia is characterized by a high frequency of placental maternal vascular lesions of underperfusion and a small placenta [90–94], abnormal umbilical artery and uterine arteries Doppler velocimetry [99–104], an abnormal angiogenic/anti-angiogenic profile [58,59,72,80,109,111], fetal growth restriction [95–98], and a relatively high rate of thrombocytopenia, elevated liver enzyme abnormalities, and the HELLP syndrome [150]. By contrast, late-onset preeclampsia is thought to result from a mismatch between the nutrient supply by the mother and the metabolic demands of the fetus at the end of pregnancy [77–79]. Typically, the placenta is of normal weight [92]; it is less likely to have maternal vascular lesions of underperfusion than the placenta in early-onset disease [90–93]; fetuses are frequently of appropriate or large birth weight for gestational age [105–108]; and the uterine arteries and umbilical artery Doppler velocimetries are generally within normal range [79]. Late-onset preeclampsia is more likely to occur in obese patients [151–153]. Cardiac output, total vascular resistance, and the morphology of the left ventricle, as determined by echocardiography, are also different in early- and late-onset preeclampsia by 24 weeks of gestation [79].
Because the etiologies of early- and late-onset preeclampsia are different, biomarkers predicting their development are expected to diverge. For example, the concentrations of PlGF and anti-angiogenic factors (sFlt-1 and sEng) are good predictors of early-onset preeclampsia, but not of late-onset disease. We undertook the discovery of biomarkers focusing exclusively on late-onset disease: we and other investigators previously addressed the prediction of early-onset preeclampsia [99,101,119–123].
MMP-7, a predictor of late-onset preeclampsia
Elevated abundance of MMP-7 in maternal plasma before 22 weeks of gestation was the strongest predictor of late-onset preeclampsia. This matrix metalloproteinase, also called matrilysin, is involved in the degradation of several types of collagen (III, IV, V, IX, X, XI), proteoglycans, fibronectin, elastin, and casein [154]. It is the smallest MMP that circulates in the blood. The main form is pro-MMP-7, which is enzymatically inactive. MMP-7 is involved in innate immune processes, mainly in the lung and gut, due to its proteolytic activity that activates α-defensins (anti-bacterial peptides able to disrupt bacterial membrane) [154]. Indeed, silencing MMP-7 in mice will result in the inability to activate pro-α-defensins in the gut and a higher susceptibility to intestinal bacterial infections [155]. MMP-7 also has an important role in releasing TNF-α from macrophages; and it is involved in the transepithelial migration of neutrophils by cleaving syndecan-1, the main heparan sulphate proteoglycan on the epithelium. Maternal plasma concentration of TNF-α is elevated in preeclampsia [156,157].
Recent evidence suggests that MMP-7 may play a role in atherosclerotic disease, which has many parallels to preeclampsia [158]. Indeed, the SUMMIT Consortium (surrogate markers for micro- and macrovascular hard endpoint for innovative diabetes tools) reported that circulating MMP-7 concentrations were higher in patients with Type 2 diabetes mellitus, correlated with patients’ age, and were independently associated with the prevalence of cardiovascular disease and the burden of atherosclerosis as well as arterial stiffness and plaque inflammation. Baseline MMP-7 concentrations were elevated in patients who had a coronary event during the study period [158]. Circulating concentrations of MMP-7 are significantly higher in patients with histological unstable atherosclerotic carotid lesions compared to patients with stable lesions [159]. In addition, markedly higher mRNA levels of MMP-7 were found within carotid plaques than in arteries without plaques [160]. MMP-7 within the carotid plaques was primarily localized in macrophages [160,161], and in vitro studies showed that combined stimulation of inflammatory mediators (TNF-α), oxidized LDL, and hypoxia markedly increased MMP-7 expression in monocytes [160]. In atherosclerotic plaques, MMP-7 is expressed by lipid-laden macrophages [161], the same cells present in acute atherosis of the spiral arteries, a lesion associated with preeclampsia [162,163]. Thus, MMP-7 may contribute to plaque destabilization in patients with carotid artery stenosis. Abbas et al. [160] reported that MMP-7 concentrations were especially higher if the patients were symptomatic within the prior two months of sampling. Moreover, high plasma concentrations of MMP-7 in these patients were independently associated with total mortality [160].
During pregnancy, MMP-7 is expressed in the decidua and trophoblast. In the first trimester, uterine NK cells and macrophages abundant in the decidua express MMP-7; and matrilysin may have a role in the process of transformation of the spiral arteries, because 50%-75% of leukocytes infiltrating and remodeling the vessels are positive for MMP-7 and MMP-9 [164]. During normal pregnancy there is constant expression of MMP-7 in the intermediate trophoblast and decidual cells throughout gestation [165].
Matrilysin is associated with pregnancy complications: 1) its amniotic fluid concentrations are elevated in women with preterm labor and intact membranes who deliver preterm regardless of the presence of intra-amniotic infection [166]; 2) in the placentas of patients with severe preeclampsia, there is extensive immunostaining of all layers of villous trophoblast for MMP-7 [165]; 3) by contrast, placentas from patients with severe early-onset preeclampsia with fetal growth restriction, the interstitial trophoblast cell expression of MMP-3 and MMP-7 are markedly reduced [167]. The authors attributed this finding to the fact that decidual NK cells aggregated near the spiral arteries secrete leukemia inhibitory factor (LIF) that suppresses the expression of MMPs. This may impede the physiological transformation of the spiral arteries, which has been implicated in the pathophysiology of early-onset preeclampsia [167]. Collectively, these reports suggest that MMP-7 may be involved in two fundamental processes associated with the development of preeclampsia: placentation and inflammation.
A previous study reported that MMP-2 is elevated in maternal urine as early as 12–16 weeks of gestation, and an elevated concentration of MMP-2 at 12 weeks predicted the development of preeclampsia with a sensitivity of 100% and a specificity 62.5%; at 16 weeks of gestation, an elevated MMP-2 in maternal urine predicted the development of preeclampsia with a sensitivity of 87.5% and a specificity of 74.1% [168]. The urine concentration of MMP-7 in patients who subsequently developed preeclampsia did not differ from those with a normal pregnancy, but the study could not differentiate between patients who subsequently developed early- and late-onset preeclampsia [168].
What are the differences in the proteomic profile between patients with mild and severe late-onset preeclampsia?
The severity of preeclampsia has major implications for maternal and neonatal outcomes. Patients with a mild disease need only timely delivery and observation. By contrast, women with severe preeclampsia have a high rate of maternal morbidity, including eclampsia, abruption, elevated liver enzymes, and emergency cesarean delivery [20]. Therefore, early identification of women who will subsequently develop severe preeclampsia is important as they may benefit from a timely delivery prior to the onset of the severe preeclampsia [169].
Until 22 weeks of gestation, MMP-7 was the most predictive protein for the development of late-onset preeclampsia, either in mild or severe form. After 22 weeks, we observed differences in the set of proteins most predictive of mild or severe preeclampsia. PlGF optimally identified patients destined to develop severe preeclampsia at 22.1–28 and 32.1–36 weeks of gestation, whereas patients destined to develop mild preeclampsia were better predicted by a different set of proteins at each gestational age. These proteins are involved in angiogenesis (e.g., PlGF), coagulation (e.g., tissue factor), cell division (e.g., RAs-related Nuclear protein), and cell-to-cell interaction (e.g., tyrosine-protein kinase Fer). The finding that, after 22 weeks of gestation, PlGF is the best predictor of late-onset preeclampsia, especially in its more severe form, is consistent with previous reports [61,115,170–173]. We and others [55,70,174] presented the use of this angiogenic factor as a tool for the assessment of the impending risk for preeclampsia, demonstrating lower concentrations of PlGF in cases when compared to controls as early as at least six weeks prior to the onset of the disease [61]. Moreover, the determination of this angiogenic factor has prognostic value in patients presenting to the obstetrical triage area with suspected preeclampsia for the identification of those requiring delivery due to impending preeclampsia[171, 172].
Identification of patients who subsequently developed late-onset preeclampsia may warrant a two-stage assessment approach
The comparison of the proteomic prediction models built to predict subsets of cases based on the severity of this syndrome suggests that we may need a two-step approach for the prediction of late-onset preeclampsia. Similar to the current paradigm for the identification of patients at risk of aneuploidy, for which a two-step model has been used (the first at 11–13 weeks of gestation includes nuchal translucency and biochemical markers such as hCG and PAPP-A; and the second at 17 weeks includes alpha feto-protein, hCG, and E3, as well as inhibin in cases of quad test) to generate an integrated risk that serves as the basis for further diagnostic tests, e.g., amniocentesis to diagnose aneuploidy [175–178]. Unlike the detection of patients at risk for early-onset preeclampsia, in which maternal background characteristics, PlGF concentration, and maternal blood pressure at the time of sample collection can identify the majority of patients at risk for the development of this syndrome [82,114,118,119], our study indicates that optimal prediction of late-onset preeclampsia may involve two diagnostic steps: the first assessment during early gestation (8–22.1 weeks), using MMP-7, and the second one later during the third trimester (28.1–32 weeks). Until 22.1 weeks, MMP-7 has the highest predictive performance for the identification of patients at risk to develop late-onset preeclampsia regrades to severity, whereas, after 22 weeks, the set of optimal proteomic predictors differs according to the severity of late-onset preeclampsia. This has implications on clinical management, since those who are at risk for the development of severe late-onset preeclampsia may benefit from timely delivery near 37 weeks of gestation, while those who are destined to have a mild disease may continue pregnancy to term under close surveillance.
Strengths and limitations
The major strengths of this study are the large number of proteins tested, as well as its longitudinal design and the number of samples included in the analysis, especially during early stages of pregnancy. This is the first study to demonstrate that proteomic profiles identify patients destined to develop severe or mild late-onset preeclampsia as early as 16 weeks with a sensitivity that surpasses that of PlGF. Our study includes mainly African American women; this may limit the generalizability of our results to this ethnic group, which is at much higher risk to develop preeclampsia than other ethnic groups.
It is common in the field of high-dimensional biology to combine predictors (e.g., mRNAs, proteins, metabolites, etc.) in a logistic regression (or other type of prediction model) and report one set of predictive performance indices on the full set of patients used to select the predictors and fit models for this purpose. However, such approaches would lead to optimistically biased performance indices due to at least two sources of bias. The most important is the feature selection bias, since, when selecting from a large pool of candidate biomarkers, it is generally possible to find a few “biomarkers” that appear to predict the outcome better than expected by chance (e.g., AUC>0.5). The second source of bias comes from tuning (estimating) the weights (co-efficients) of a predefined set of predictors to fit the available data. We avoided these common pitfalls by relying on bootstrap-estimated performance indices. With this procedure, predictor/feature selection and model fitting are repeated 100 times on data from a training set of patients while the model is tested on data from patients left out at each iteration. As shown in Fig 1, the LOOCV AUC and sensitivity estimates of the best combination of markers are in the worst case as low as the one of PlGF, yet we only claim better prediction compared to PlGF alone in the first two intervals when the bootstrap-based estimates of multi-marker models are significantly higher than those of PlGF.
Also, we and others [143] have addressed the problem that indicates when high-dimensional data are used to build prediction models, the same prediction performance can be achieved with widely different sets of predictors, due, among other reasons, to the correlation that may exist among them. Therefore, instead of emphasizing the sets of proteins identified in the final models (Table 2), we focused our inferences on the proteins that appear to be selected as the best predictors more often during the 100 different bootstrap iterations. For instance, while PlGF was the most reliable predictor of late-onset preeclampsia in the interval 22.1–28 weeks, being included in the best combination 24/100 times, when all data was used to fit the final model, RAN and METAP1 appeared to be the best choices even though they were selected 12 and 16 times in the best combination out of 100 bootstrap trials.
Conclusion
We present herein new biomarkers to identify patients who will develop late-onset preeclampsia based on a high through-put proteomics method. We report that elevated MMP-7 early in gestation (8–22 weeks) and low PlGF later in gestation (after 22 weeks) are the strongest predictors for the subsequent development of late-onset preeclampsia, hence suggesting that the optimal identification of patients at risk may involve a two-step diagnostic approach. In addition, abnormal proteomic profiles before 22 weeks of gestation are associated with perturbation of several biological processes including the positive regulation of vascular endothelial growth factor receptor signaling pathway.
Supporting information
Protein abundance data for each sample (rows) and each of the 1125 proteins is given in this table. ID: anonymized identifier indicator of the patient, GA: gestational age at sample, LatePE: is 1 for late preeclampsia and 0 for normal pregnancy. Protein symbol and names provide by Somalogic, Inc, are included above the protein accession numbers.
(CSV)
Thirty-six proteins that were significant (Sig.) (q<0.25 and fold change >1.1) in at least one interval are shown. Adjustment was performed for BMI, maternal age, parity and smoking. FC: linear fold change, with negative values denoting lower while positive values denoting higher level in cases than in controls, p: p-value, q: adjusted p-value, GA: gestational age. The column labeled as “Changes with GA” indicates whether the protein abundance changes with gestational age [128].
(XLS)
Data Availability
All relevant data are included within the paper and its Supporting Information files.
Funding Statement
This research was supported, in part, by the Perinatology Research Branch, Program for Perinatal Research and Obstetrics, Division of Intramural Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, U.S. Department of Health and Human Services (NICHD/NIH/DHHS); and, in part, with Federal funds from NICHD/NIH/DHHS under Contract No. HHSN275201300006C. ALT was also supported by the Perinatal Initiative of the Wayne State University School of Medicine.
References
- 1.Wallis AB, Saftlas AF, Hsia J, Atrash HK (2008) Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens 21: 521–526. doi: 10.1038/ajh.2008.20 [DOI] [PubMed] [Google Scholar]
- 2.Kuklina EV, Ayala C, Callaghan WM (2009) Hypertensive disorders and severe obstetric morbidity in the United States. Obstet Gynecol 113: 1299–1306. doi: 10.1097/AOG.0b013e3181a45b25 [DOI] [PubMed] [Google Scholar]
- 3.Hutcheon JA, Lisonkova S, Joseph KS (2011) Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 25: 391–403. doi: 10.1016/j.bpobgyn.2011.01.006 [DOI] [PubMed] [Google Scholar]
- 4.Paruk F, Moodley J (2000) Maternal and neonatal outcome in early- and late-onset pre-eclampsia. Semin Neonatol 5: 197–207. doi: 10.1053/siny.2000.0023 [DOI] [PubMed] [Google Scholar]
- 5.MacKay AP, Berg CJ, Atrash HK (2001) Pregnancy-related mortality from preeclampsia and eclampsia. Obstet Gynecol 97: 533–538. [DOI] [PubMed] [Google Scholar]
- 6.Smith GC, Pell JP, Walsh D (2001) Pregnancy complications and maternal risk of ischaemic heart disease: a retrospective cohort study of 129,290 births. Lancet 357: 2002–2006. doi: 10.1016/S0140-6736(00)05112-6 [DOI] [PubMed] [Google Scholar]
- 7.Bellamy L, Casas JP, Hingorani AD, Williams DJ (2007) Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. Bmj 335: 974 doi: 10.1136/bmj.39335.385301.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berg CJ, Mackay AP, Qin C, Callaghan WM (2009) Overview of maternal morbidity during hospitalization for labor and delivery in the United States: 1993–1997 and 2001–2005. Obstet Gynecol 113: 1075–1081. doi: 10.1097/AOG.0b013e3181a09fc0 [DOI] [PubMed] [Google Scholar]
- 9.Stekkinger E, Zandstra M, Peeters LL, Spaanderman ME (2009) Early-onset preeclampsia and the prevalence of postpartum metabolic syndrome. Obstet Gynecol 114: 1076–1084. doi: 10.1097/AOG.0b013e3181b7b242 [DOI] [PubMed] [Google Scholar]
- 10.Schutte JM, Steegers EA, Schuitemaker NW, Santema JG, de Boer K, Pel M, et al. (2010) Rise in maternal mortality in the Netherlands. Bjog 117: 399–406. doi: 10.1111/j.1471-0528.2009.02382.x [DOI] [PubMed] [Google Scholar]
- 11.Adams T, Yeh C, Bennett-Kunzier N, Kinzler WL (2014) Long-term maternal morbidity and mortality associated with ischemic placental disease. Semin Perinatol 38: 146–150. doi: 10.1053/j.semperi.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 12.Lisonkova S, Sabr Y, Mayer C, Young C, Skoll A, Joseph KS (2014) Maternal morbidity associated with early-onset and late-onset preeclampsia. Obstet Gynecol 124: 771–781. doi: 10.1097/AOG.0000000000000472 [DOI] [PubMed] [Google Scholar]
- 13.Ozimek JA, Eddins RM, Greene N, Karagyozyan D, Pak S, Wong M, et al. (2016) Opportunities for improvement in care among women with severe maternal morbidity. Am J Obstet Gynecol 215: 509.e501–506. [DOI] [PubMed] [Google Scholar]
- 14.Hnat MD, Sibai BM, Caritis S, Hauth J, Lindheimer MD, MacPherson C, et al. (2002) Perinatal outcome in women with recurrent preeclampsia compared with women who develop preeclampsia as nulliparas. Am J Obstet Gynecol 186: 422–426. [DOI] [PubMed] [Google Scholar]
- 15.Madazli R, Yuksel MA, Imamoglu M, Tuten A, Oncul M, Aydin B, et al. (2014) Comparison of clinical and perinatal outcomes in early- and late-onset preeclampsia. Arch Gynecol Obstet 290: 53–57. doi: 10.1007/s00404-014-3176-x [DOI] [PubMed] [Google Scholar]
- 16.Sarno L, Maruotti GM, Saccone G, Sirico A, Mazzarelli LL, Martinelli P (2015) Pregnancy outcome in proteinuria-onset and hypertension-onset preeclampsia. Hypertens Pregnancy 34: 284–290. doi: 10.3109/10641955.2015.1015731 [DOI] [PubMed] [Google Scholar]
- 17.Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365: 785–799. doi: 10.1016/S0140-6736(05)17987-2 [DOI] [PubMed] [Google Scholar]
- 18.Di Renzo GC (2009) The great obstetrical syndromes. J Matern Fetal Neonatal Med 22: 633–635. doi: 10.1080/14767050902866804 [DOI] [PubMed] [Google Scholar]
- 19.Brosens I, Pijnenborg R, Vercruysse L, Romero R (2011) The "Great Obstetrical Syndromes" are associated with disorders of deep placentation. Am J Obstet Gynecol 204: 193–201. doi: 10.1016/j.ajog.2010.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R (2014) Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol 10: 466–480. doi: 10.1038/nrneph.2014.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myatt L, Roberts JM (2015) Preeclampsia: Syndrome or Disease? Curr Hypertens Rep 17: 83 doi: 10.1007/s11906-015-0595-4 [DOI] [PubMed] [Google Scholar]
- 22.Robertson WB, Brosens I, Dixon G (1976) Maternal uterine vascular lesions in the hypertensive complications of pregnancy. Perspect Nephrol Hypertens 5: 115–127. [PubMed] [Google Scholar]
- 23.Pijnenborg R, Anthony J, Davey DA, Rees A, Tiltman A, Vercruysse L, et al. (1991) Placental bed spiral arteries in the hypertensive disorders of pregnancy. Br J Obstet Gynaecol 98: 648–655. [DOI] [PubMed] [Google Scholar]
- 24.Silasi M, Cohen B, Karumanchi SA, Rana S (2010) Abnormal placentation, angiogenic factors, and the pathogenesis of preeclampsia. Obstet Gynecol Clin North Am 37: 239–253. doi: 10.1016/j.ogc.2010.02.013 [DOI] [PubMed] [Google Scholar]
- 25.Granger JP, Alexander BT, Llinas MT, Bennett WA, Khalil RA (2002) Pathophysiology of preeclampsia: linking placental ischemia/hypoxia with microvascular dysfunction. Microcirculation 9: 147–160. doi: 10.1038/sj.mn.7800137 [DOI] [PubMed] [Google Scholar]
- 26.Makris A, Thornton C, Thompson J, Thomson S, Martin R, Ogle R, et al. (2007) Uteroplacental ischemia results in proteinuric hypertension and elevated sFLT-1. Kidney Int 71: 977–984. doi: 10.1038/sj.ki.5002175 [DOI] [PubMed] [Google Scholar]
- 27.Gilbert JS, Ryan MJ, LaMarca BB, Sedeek M, Murphy SR, Granger JP (2008) Pathophysiology of hypertension during preeclampsia: linking placental ischemia with endothelial dysfunction. Am J Physiol Heart Circ Physiol 294: H541–550. doi: 10.1152/ajpheart.01113.2007 [DOI] [PubMed] [Google Scholar]
- 28.Gilbert JS, Gilbert SA, Arany M, Granger JP (2009) Hypertension produced by placental ischemia in pregnant rats is associated with increased soluble endoglin expression. Hypertension 53: 399–403. doi: 10.1161/HYPERTENSIONAHA.108.123513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Makris A, Yeung KR, Lim SM, Sunderland N, Heffernan S, Thompson JF, et al. (2016) Placental Growth Factor Reduces Blood Pressure in a Uteroplacental Ischemia Model of Preeclampsia in Nonhuman Primates. Hypertension 67: 1263–1272. doi: 10.1161/HYPERTENSIONAHA.116.07286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salafia CM, Pezzullo JC, Lopez-Zeno JA, Simmens S, Minior VK, Vintzileos AM (1995) Placental pathologic features of preterm preeclampsia. Am J Obstet Gynecol 173: 1097–1105. [DOI] [PubMed] [Google Scholar]
- 31.Aardema MW, Oosterhof H, Timmer A, van Rooy I, Aarnoudse JG (2001) Uterine artery Doppler flow and uteroplacental vascular pathology in normal pregnancies and pregnancies complicated by pre-eclampsia and small for gestational age fetuses. Placenta 22: 405–411. doi: 10.1053/plac.2001.0676 [DOI] [PubMed] [Google Scholar]
- 32.Egbor M, Ansari T, Morris N, Green CJ, Sibbons PD (2006) Morphometric placental villous and vascular abnormalities in early- and late-onset pre-eclampsia with and without fetal growth restriction. BJOG 113: 580–589. doi: 10.1111/j.1471-0528.2006.00882.x [DOI] [PubMed] [Google Scholar]
- 33.Wolf M, Sandler L, Munoz K, Hsu K, Ecker JL, Thadhani R (2002) First trimester insulin resistance and subsequent preeclampsia: a prospective study. J Clin Endocrinol Metab 87: 1563–1568. doi: 10.1210/jcem.87.4.8405 [DOI] [PubMed] [Google Scholar]
- 34.Erez-Weiss I, Erez O, Shoham-Vardi I, Holcberg G, Mazor M (2005) The association between maternal obesity, glucose intolerance and hypertensive disorders of pregnancy in nondiabetic pregnant women. Hypertens Pregnancy 24: 125–136. doi: 10.1081/PRG-200059853 [DOI] [PubMed] [Google Scholar]
- 35.Parretti E, Lapolla A, Dalfra M, Pacini G, Mari A, Cioni R, et al. (2006) Preeclampsia in lean normotensive normotolerant pregnant women can be predicted by simple insulin sensitivity indexes. Hypertension 47: 449–453. doi: 10.1161/01.HYP.0000205122.47333.7f [DOI] [PubMed] [Google Scholar]
- 36.von Versen-Hoeynck FM, Powers RW (2007) Maternal-fetal metabolism in normal pregnancy and preeclampsia. Front Biosci 12: 2457–2470. [DOI] [PubMed] [Google Scholar]
- 37.Mastrogiannis DS, Spiliopoulos M, Mulla W, Homko CJ (2009) Insulin resistance: the possible link between gestational diabetes mellitus and hypertensive disorders of pregnancy. Curr Diab Rep 9: 296–302. [DOI] [PubMed] [Google Scholar]
- 38.Scioscia M, Gumaa K, Rademacher TW (2009) The link between insulin resistance and preeclampsia: new perspectives. J Reprod Immunol 82: 100–105. doi: 10.1016/j.jri.2009.04.009 [DOI] [PubMed] [Google Scholar]
- 39.Catalano PM (2010) Obesity, insulin resistance, and pregnancy outcome. Reproduction 140: 365–371. doi: 10.1530/REP-10-0088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jeyabalan A, Hubel CA, Roberts JM (2014) Metabolic syndrome and preeclampsia In: Taylor RN, Roberts JM, Cunningham FG, Lindheimer MD, editors. Chesley's hypertensive disorders in pregnancy: Elsevier; pp. 133–160. [Google Scholar]
- 41.Sacks GP, Studena K, Sargent K, Redman CW (1998) Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. Am J Obstet Gynecol 179: 80–86. [DOI] [PubMed] [Google Scholar]
- 42.Redman CW, Sacks GP, Sargent IL (1999) Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol 180: 499–506. [DOI] [PubMed] [Google Scholar]
- 43.Gervasi MT, Chaiworapongsa T, Pacora P, Naccasha N, Yoon BH, Maymon E, et al. (2001) Phenotypic and metabolic characteristics of monocytes and granulocytes in preeclampsia. Am J Obstet Gynecol 185: 792–797. doi: 10.1067/mob.2001.117311 [DOI] [PubMed] [Google Scholar]
- 44.Redman CW, Sargent IL (2010) Immunology of pre-eclampsia. Am J Reprod Immunol 63: 534–543. doi: 10.1111/j.1600-0897.2010.00831.x [DOI] [PubMed] [Google Scholar]
- 45.Roberts JM, Taylor RN, Musci TJ, Rodgers GM, Hubel CA, McLaughlin MK (1989) Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol 161: 1200–1204. [DOI] [PubMed] [Google Scholar]
- 46.Roberts JM, Taylor RN, Goldfien A (1991) Endothelial cell activation as a pathogenetic factor in preeclampsia. Semin Perinatol 15: 86–93. [PubMed] [Google Scholar]
- 47.Roberts JM, Taylor RN, Goldfien A (1991) Clinical and biochemical evidence of endothelial cell dysfunction in the pregnancy syndrome preeclampsia. Am J Hypertens 4: 700–708. [DOI] [PubMed] [Google Scholar]
- 48.Dekker GA, van Geijn HP (1996) Endothelial dysfunction in preeclampsia. Part I: Primary prevention. Therapeutic perspectives. J Perinat Med 24: 99–117. [DOI] [PubMed] [Google Scholar]
- 49.Roberts JM (1998) Endothelial dysfunction in preeclampsia. Semin Reprod Endocrinol 16: 5–15. doi: 10.1055/s-2007-1016248 [DOI] [PubMed] [Google Scholar]
- 50.Lamarca B (2010) The role of immune activation in contributing to vascular dysfunction and the pathophysiology of hypertension during preeclampsia. Minerva Ginecol 62: 105–120. [PMC free article] [PubMed] [Google Scholar]
- 51.Torry DS, Wang HS, Wang TH, Caudle MR, Torry RJ (1998) Preeclampsia is associated with reduced serum levels of placenta growth factor. Am J Obstet Gynecol 179: 1539–1544. [DOI] [PubMed] [Google Scholar]
- 52.Reuvekamp A, Velsing-Aarts FV, Poulina IE, Capello JJ, Duits AJ (1999) Selective deficit of angiogenic growth factors characterises pregnancies complicated by pre-eclampsia. Br J Obstet Gynaecol 106: 1019–1022. [DOI] [PubMed] [Google Scholar]
- 53.Tidwell SC, Ho HN, Chiu WH, Torry RJ, Torry DS (2001) Low maternal serum levels of placenta growth factor as an antecedent of clinical preeclampsia. Am J Obstet Gynecol 184: 1267–1272. doi: 10.1067/mob.2001.113129 [DOI] [PubMed] [Google Scholar]
- 54.Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, et al. (2003) Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 111: 649–658. doi: 10.1172/JCI17189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, et al. (2004) Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med 350: 672–683. doi: 10.1056/NEJMoa031884 [DOI] [PubMed] [Google Scholar]
- 56.Rajakumar A, Michael HM, Rajakumar PA, Shibata E, Hubel CA, Karumanchi SA, et al. (2005) Extra-placental expression of vascular endothelial growth factor receptor-1, (Flt-1) and soluble Flt-1 (sFlt-1), by peripheral blood mononuclear cells (PBMCs) in normotensive and preeclamptic pregnant women. Placenta 26: 563–573. doi: 10.1016/j.placenta.2004.09.001 [DOI] [PubMed] [Google Scholar]
- 57.Lindheimer MD, Romero R (2007) Emerging roles of antiangiogenic and angiogenic proteins in pathogenesis and prediction of preeclampsia. Hypertension 50: 35–36. doi: 10.1161/HYPERTENSIONAHA.107.089045 [DOI] [PubMed] [Google Scholar]
- 58.Chaiworapongsa T, Romero R, Espinoza J, Bujold E, Mee Kim Y, Goncalves LF, et al. (2004) Evidence supporting a role for blockade of the vascular endothelial growth factor system in the pathophysiology of preeclampsia. Young Investigator Award. Am J Obstet Gynecol 190: 1541–1547; discussion 1547–1550. doi: 10.1016/j.ajog.2004.03.043 [DOI] [PubMed] [Google Scholar]
- 59.Chaiworapongsa T, Romero R, Kim YM, Kim GJ, Kim MR, Espinoza J, et al. (2005) Plasma soluble vascular endothelial growth factor receptor-1 concentration is elevated prior to the clinical diagnosis of pre-eclampsia. J Matern Fetal Neonatal Med 17: 3–18. doi: 10.1080/14767050400028816 [DOI] [PubMed] [Google Scholar]
- 60.Widmer M, Villar J, Benigni A, Conde-Agudelo A, Karumanchi SA, Lindheimer M (2007) Mapping the theories of preeclampsia and the role of angiogenic factors: a systematic review. Obstet Gynecol 109: 168–180. doi: 10.1097/01.AOG.0000249609.04831.7c [DOI] [PubMed] [Google Scholar]
- 61.Romero R, Nien JK, Espinoza J, Todem D, Fu W, Chung H, et al. (2008) A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J Matern Fetal Neonatal Med 21: 9–23. doi: 10.1080/14767050701830480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bujold E, Romero R, Chaiworapongsa T, Kim YM, Kim GJ, Kim MR, et al. (2005) Evidence supporting that the excess of the sVEGFR-1 concentration in maternal plasma in preeclampsia has a uterine origin. J Matern Fetal Neonatal Med 18: 9–16. doi: 10.1080/14767050500202493 [DOI] [PubMed] [Google Scholar]
- 63.Bdolah Y, Lam C, Rajakumar A, Shivalingappa V, Mutter W, Sachs BP, et al. (2008) Twin pregnancy and the risk of preeclampsia: bigger placenta or relative ischemia? Am J Obstet Gynecol 198: 428 e421–426. [DOI] [PubMed] [Google Scholar]
- 64.Cohen A, Lim KH, Lee Y, Rana S, Karumanchi SA, Brown F (2007) Circulating levels of the antiangiogenic marker soluble FMS-like tyrosine kinase 1 are elevated in women with pregestational diabetes and preeclampsia: angiogenic markers in preeclampsia and preexisting diabetes. Diabetes Care 30: 375–377. doi: 10.2337/dc06-1514 [DOI] [PubMed] [Google Scholar]
- 65.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. (2006) Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 355: 992–1005. doi: 10.1056/NEJMoa055352 [DOI] [PubMed] [Google Scholar]
- 66.Rajakumar A, Powers RW, Hubel CA, Shibata E, von Versen-Hoynck F, Plymire D, et al. (2009) Novel soluble Flt-1 isoforms in plasma and cultured placental explants from normotensive pregnant and preeclamptic women. Placenta 30: 25–34. doi: 10.1016/j.placenta.2008.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sela S, Itin A, Natanson-Yaron S, Greenfield C, Goldman-Wohl D, Yagel S, et al. (2008) A novel human-specific soluble vascular endothelial growth factor receptor 1: cell-type-specific splicing and implications to vascular endothelial growth factor homeostasis and preeclampsia. Circ Res 102: 1566–1574. doi: 10.1161/CIRCRESAHA.108.171504 [DOI] [PubMed] [Google Scholar]
- 68.Gilbert JS, Babcock SA, Granger JP (2007) Hypertension produced by reduced uterine perfusion in pregnant rats is associated with increased soluble fms-like tyrosine kinase-1 expression. Hypertension 50: 1142–1147. doi: 10.1161/HYPERTENSIONAHA.107.096594 [DOI] [PubMed] [Google Scholar]
- 69.Maynard SE, Venkatesha S, Thadhani R, Karumanchi SA (2005) Soluble Fms-like tyrosine kinase 1 and endothelial dysfunction in the pathogenesis of preeclampsia. Pediatr Res 57: 1R–7R. doi: 10.1203/01.PDR.0000159567.85157.B7 [DOI] [PubMed] [Google Scholar]
- 70.Levine RJ, Thadhani R, Qian C, Lam C, Lim KH, Yu KF, et al. (2005) Urinary placental growth factor and risk of preeclampsia. JAMA 293: 77–85. doi: 10.1001/jama.293.1.77 [DOI] [PubMed] [Google Scholar]
- 71.Aggarwal PK, Jain V, Sakhuja V, Karumanchi SA, Jha V (2006) Low urinary placental growth factor is a marker of pre-eclampsia. Kidney Int 69: 621–624. doi: 10.1038/sj.ki.5000075 [DOI] [PubMed] [Google Scholar]
- 72.Crispi F, Dominguez C, Llurba E, Martin-Gallan P, Cabero L, Gratacos E (2006) Placental angiogenic growth factors and uterine artery Doppler findings for characterization of different subsets in preeclampsia and in isolated intrauterine growth restriction. Am J Obstet Gynecol 195: 201–207. doi: 10.1016/j.ajog.2006.01.014 [DOI] [PubMed] [Google Scholar]
- 73.Schlembach D, Wallner W, Sengenberger R, Stiegler E, Mortl M, Beckmann MW, et al. (2007) Angiogenic growth factor levels in maternal and fetal blood: correlation with Doppler ultrasound parameters in pregnancies complicated by pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol 29: 407–413. doi: 10.1002/uog.3930 [DOI] [PubMed] [Google Scholar]
- 74.Rajakumar A, Cerdeira AS, Rana S, Zsengeller Z, Edmunds L, Jeyabalan A, et al. (2012) Transcriptionally active syncytial aggregates in the maternal circulation may contribute to circulating soluble fms-like tyrosine kinase 1 in preeclampsia. Hypertension 59: 256–264. doi: 10.1161/HYPERTENSIONAHA.111.182170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chaiworapongsa T, Romero R, Korzeniewski SJ, Kusanovic JP, Soto E, Lam J, et al. (2013) Maternal plasma concentrations of angiogenic/antiangiogenic factors in the third trimester of pregnancy to identify the patient at risk for stillbirth at or near term and severe late preeclampsia. Am J Obstet Gynecol 208: 287 e281–287 e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maynard SE, Crawford SL, Bathgate S, Yan J, Robidoux L, Moore M, et al. (2013) Gestational angiogenic biomarker patterns in high risk preeclampsia groups. Am J Obstet Gynecol 209: 53 e51–59. [DOI] [PubMed] [Google Scholar]
- 77.von Dadelszen P, Magee LA, Roberts JM (2003) Subclassification of preeclampsia. Hypertens Pregnancy 22: 143–148. doi: 10.1081/PRG-120021060 [DOI] [PubMed] [Google Scholar]
- 78.Vatten LJ, Skjaerven R (2004) Is pre-eclampsia more than one disease? Bjog 111: 298–302. [DOI] [PubMed] [Google Scholar]
- 79.Valensise H, Vasapollo B, Gagliardi G, Novelli GP (2008) Early and late preeclampsia: two different maternal hemodynamic states in the latent phase of the disease. Hypertension 52: 873–880. doi: 10.1161/HYPERTENSIONAHA.108.117358 [DOI] [PubMed] [Google Scholar]
- 80.Crispi F, Llurba E, Dominguez C, Martin-Gallan P, Cabero L, Gratacos E (2008) Predictive value of angiogenic factors and uterine artery Doppler for early- versus late-onset pre-eclampsia and intrauterine growth restriction. Ultrasound Obstet Gynecol 31: 303–309. doi: 10.1002/uog.5184 [DOI] [PubMed] [Google Scholar]
- 81.Junus K, Centlow M, Wikstrom AK, Larsson I, Hansson SR, Olovsson M (2012) Gene expression profiling of placentae from women with early- and late-onset pre-eclampsia: down-regulation of the angiogenesis-related genes ACVRL1 and EGFL7 in early-onset disease. Mol Hum Reprod 18: 146–155. doi: 10.1093/molehr/gar067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vatten LJ, Eskild A, Nilsen TI, Jeansson S, Jenum PA, Staff AC (2007) Changes in circulating level of angiogenic factors from the first to second trimester as predictors of preeclampsia. Am J Obstet Gynecol 196: 239.e231–236. [DOI] [PubMed] [Google Scholar]
- 83.Soto E, Romero R, Kusanovic JP, Ogge G, Hussein Y, Yeo L, et al. (2012) Late-onset preeclampsia is associated with an imbalance of angiogenic and anti-angiogenic factors in patients with and without placental lesions consistent with maternal underperfusion. J Matern Fetal Neonatal Med 25: 498–507. doi: 10.3109/14767058.2011.591461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Parra-Cordero M, Rodrigo R, Barja P, Bosco C, Rencoret G, Sepulveda-Martinez A, et al. (2013) Prediction of early and late pre-eclampsia from maternal characteristics, uterine artery Doppler and markers of vasculogenesis during first trimester of pregnancy. Ultrasound Obstet Gynecol 41: 538–544. doi: 10.1002/uog.12264 [DOI] [PubMed] [Google Scholar]
- 85.Tranquilli AL, Brown MA, Zeeman GG, Dekker G, Sibai BM (2013) The definition of severe and early-onset preeclampsia. Statements from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Pregnancy Hypertens 3: 44–47. doi: 10.1016/j.preghy.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 86.Cheng YW, Kaimal AJ, Bruckner TA, Halloran DR, Caughey AB (2011) Perinatal morbidity associated with late preterm deliveries compared with deliveries between 37 and 40 weeks of gestation. Bjog 118: 1446–1454. doi: 10.1111/j.1471-0528.2011.03045.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kramer MS, Demissie K, Yang H, Platt RW, Sauve R, Liston R (2000) The contribution of mild and moderate preterm birth to infant mortality. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. Jama 284: 843–849. [DOI] [PubMed] [Google Scholar]
- 88.Robertson PA, Sniderman SH, Laros RK Jr., Cowan R, Heilbron D, Goldenberg RL, et al. (1992) Neonatal morbidity according to gestational age and birth weight from five tertiary care centers in the United States, 1983 through 1986. Am J Obstet Gynecol 166: 1629–1641; discussion 1641–1625. [DOI] [PubMed] [Google Scholar]
- 89.Kenneth L, Hall DR, Gebhardt S, Grove D (2010) Late onset preeclampsia is not an innocuous condition. Hypertens Pregnancy 29: 262–270. doi: 10.3109/10641950902777697 [DOI] [PubMed] [Google Scholar]
- 90.Moldenhauer JS, Stanek J, Warshak C, Khoury J, Sibai B (2003) The frequency and severity of placental findings in women with preeclampsia are gestational age dependent. Am J Obstet Gynecol 189: 1173–1177. [DOI] [PubMed] [Google Scholar]
- 91.Sebire NJ, Goldin RD, Regan L (2005) Term preeclampsia is associated with minimal histopathological placental features regardless of clinical severity. J Obstet Gynaecol 25: 117–118. doi: 10.1080/014436105400041396 [DOI] [PubMed] [Google Scholar]
- 92.van der Merwe JL, Hall DR, Wright C, Schubert P, Grove D (2010) Are early and late preeclampsia distinct subclasses of the disease—what does the placenta reveal? Hypertens Pregnancy 29: 457–467. doi: 10.3109/10641950903572282 [DOI] [PubMed] [Google Scholar]
- 93.Ogge G, Chaiworapongsa T, Romero R, Hussein Y, Kusanovic JP, Yeo L, et al. (2011) Placental lesions associated with maternal underperfusion are more frequent in early-onset than in late-onset preeclampsia. J Perinat Med 39: 641–652. doi: 10.1515/JPM.2011.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mifsud W, Sebire NJ (2014) Placental pathology in early-onset and late-onset fetal growth restriction. Fetal Diagn Ther 36: 117–128. doi: 10.1159/000359969 [DOI] [PubMed] [Google Scholar]
- 95.Odegard RA, Vatten LJ, Nilsen ST, Salvesen KA, Austgulen R (2000) Preeclampsia and fetal growth. Obstet Gynecol 96: 950–955. [PubMed] [Google Scholar]
- 96.Yu CK, Khouri O, Onwudiwe N, Spiliopoulos Y, Nicolaides KH (2008) Prediction of pre-eclampsia by uterine artery Doppler imaging: relationship to gestational age at delivery and small-for-gestational age. Ultrasound Obstet Gynecol 31: 310–313. doi: 10.1002/uog.5252 [DOI] [PubMed] [Google Scholar]
- 97.Jelin AC, Cheng YW, Shaffer BL, Kaimal AJ, Little SE, Caughey AB (2010) Early-onset preeclampsia and neonatal outcomes. J Matern Fetal Neonatal Med 23: 389–392. doi: 10.1080/14767050903168416 [DOI] [PubMed] [Google Scholar]
- 98.Lisonkova S, Joseph KS (2013) Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol 209: 544.e541–544.e512. [DOI] [PubMed] [Google Scholar]
- 99.Espinoza J, Romero R, Nien JK, Gomez R, Kusanovic JP, Goncalves LF, et al. (2007) Identification of patients at risk for early onset and/or severe preeclampsia with the use of uterine artery Doppler velocimetry and placental growth factor. Am J Obstet Gynecol 196: 326.e321–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Melchiorre K, Wormald B, Leslie K, Bhide A, Thilaganathan B (2008) First-trimester uterine artery Doppler indices in term and preterm pre-eclampsia. Ultrasound Obstet Gynecol 32: 133–137. doi: 10.1002/uog.5400 [DOI] [PubMed] [Google Scholar]
- 101.Llurba E, Carreras E, Gratacos E, Juan M, Astor J, Vives A, et al. (2009) Maternal history and uterine artery Doppler in the assessment of risk for development of early- and late-onset preeclampsia and intrauterine growth restriction. Obstet Gynecol Int 2009: 275613 doi: 10.1155/2009/275613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Poon LC, Staboulidou I, Maiz N, Plasencia W, Nicolaides KH (2009) Hypertensive disorders in pregnancy: screening by uterine artery Doppler at 11–13 weeks. Ultrasound Obstet Gynecol 34: 142–148. doi: 10.1002/uog.6452 [DOI] [PubMed] [Google Scholar]
- 103.Tobinaga CM, Torloni MR, Gueuvoghlanian-Silva BY, Pendeloski KP, Akita PA, Sass N, et al. (2014) Angiogenic factors and uterine Doppler velocimetry in early- and late-onset preeclampsia. Acta Obstet Gynecol Scand 93: 469–476. doi: 10.1111/aogs.12366 [DOI] [PubMed] [Google Scholar]
- 104.Muresan D, Rotar IC, Stamatian F (2016) The usefulness of fetal Doppler evaluation in early versus late onset intrauterine growth restriction. Review of the literature. Med Ultrason 18: 103–109. doi: 10.11152/mu.2013.2066.181.dop [DOI] [PubMed] [Google Scholar]
- 105.Eskild A, Romundstad PR, Vatten LJ (2009) Placental weight and birthweight: does the association differ between pregnancies with and without preeclampsia? Am J Obstet Gynecol 201: 595 e591–595. [DOI] [PubMed] [Google Scholar]
- 106.Espinoza J, Lee W, Martin SR, Belfort MA (2014) Customized growth curves for identification of large-for-gestational age neonates in pre-eclamptic women. Ultrasound Obstet Gynecol 43: 165–169. [DOI] [PubMed] [Google Scholar]
- 107.Rasmussen S, Irgens LM, Espinoza J (2014) Maternal obesity and excess of fetal growth in pre-eclampsia. BJOG 121: 1351–1357. doi: 10.1111/1471-0528.12677 [DOI] [PubMed] [Google Scholar]
- 108.Verlohren S, Melchiorre K, Khalil A, Thilaganathan B (2014) Uterine artery Doppler, birth weight and timing of onset of pre-eclampsia: providing insights into the dual etiology of late-onset pre-eclampsia. Ultrasound Obstet Gynecol 44: 293–298. doi: 10.1002/uog.13310 [DOI] [PubMed] [Google Scholar]
- 109.Wikstrom AK, Larsson A, Eriksson UJ, Nash P, Norden-Lindeberg S, Olovsson M (2007) Placental growth factor and soluble FMS-like tyrosine kinase-1 in early-onset and late-onset preeclampsia. Obstet Gynecol 109: 1368–1374. doi: 10.1097/01.AOG.0000264552.85436.a1 [DOI] [PubMed] [Google Scholar]
- 110.Chaiworapongsa T, Romero R, Kusanovic JP, Mittal P, Kim SK, Gotsch F, et al. (2010) Plasma soluble endoglin concentration in pre-eclampsia is associated with an increased impedance to flow in the maternal and fetal circulations. Ultrasound Obstet Gynecol 35: 155–162. doi: 10.1002/uog.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Myatt L, Clifton RG, Roberts JM, Spong CY, Wapner RJ, Thorp JM Jr., et al. (2013) Can changes in angiogenic biomarkers between the first and second trimesters of pregnancy predict development of pre-eclampsia in a low-risk nulliparous patient population? BJOG 120: 1183–1191. doi: 10.1111/1471-0528.12128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Allen RE, Rogozinska E, Cleverly K, Aquilina J, Thangaratinam S (2014) Abnormal blood biomarkers in early pregnancy are associated with preeclampsia: a meta-analysis. Eur J Obstet Gynecol Reprod Biol 182: 194–201. doi: 10.1016/j.ejogrb.2014.09.027 [DOI] [PubMed] [Google Scholar]
- 113.Perales A, Delgado JL, De La Calle M, Garcia-Hernandez JA, Escudero AI, Campillos JM, et al. (2016) sFlt-1/PlGF for early-onset pre-eclampsia prediction: STEPS (Study of Early Pre-eclampsia in Spain). Ultrasound Obstet Gynecol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kusanovic JP, Romero R, Chaiworapongsa T, Erez O, Mittal P, Vaisbuch E, et al. (2009) A prospective cohort study of the value of maternal plasma concentrations of angiogenic and anti-angiogenic factors in early pregnancy and midtrimester in the identification of patients destined to develop preeclampsia. J Matern Fetal Neonatal Med 22: 1021–1038. doi: 10.3109/14767050902994754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Erez O, Romero R, Espinoza J, Fu W, Todem D, Kusanovic JP, et al. (2008) The change in concentrations of angiogenic and anti-angiogenic factors in maternal plasma between the first and second trimesters in risk assessment for the subsequent development of preeclampsia and small-for-gestational age. J Matern Fetal Neonatal Med 21: 279–287. doi: 10.1080/14767050802034545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Villa PM, Hamalainen E, Maki A, Raikkonen K, Pesonen AK, Taipale P, et al. (2013) Vasoactive agents for the prediction of early- and late-onset preeclampsia in a high-risk cohort. BMC Pregnancy Childbirth 13: 110 doi: 10.1186/1471-2393-13-110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Abdelaziz A, Maher MA, Sayyed TM, Bazeed MF, Mohamed NS (2012) Early pregnancy screening for hypertensive disorders in women without a-priori high risk. Ultrasound Obstet Gynecol 40: 398–405. doi: 10.1002/uog.11205 [DOI] [PubMed] [Google Scholar]
- 118.Akolekar R, Zaragoza E, Poon LC, Pepes S, Nicolaides KH (2008) Maternal serum placental growth factor at 11 + 0 to 13 + 6 weeks of gestation in the prediction of pre-eclampsia. Ultrasound Obstet Gynecol 32: 732–739. doi: 10.1002/uog.6244 [DOI] [PubMed] [Google Scholar]
- 119.Akolekar R, Syngelaki A, Sarquis R, Zvanca M, Nicolaides KH (2011) Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11–13 weeks. Prenat Diagn 31: 66–74. doi: 10.1002/pd.2660 [DOI] [PubMed] [Google Scholar]
- 120.Akolekar R, Syngelaki A, Poon L, Wright D, Nicolaides KH (2013) Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn Ther 33: 8–15. doi: 10.1159/000341264 [DOI] [PubMed] [Google Scholar]
- 121.Myers JE, Kenny LC, McCowan LM, Chan EH, Dekker GA, Poston L, et al. (2013) Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: a predictive test accuracy study. BJOG 120: 1215–1223. doi: 10.1111/1471-0528.12195 [DOI] [PubMed] [Google Scholar]
- 122.Poon LC, Syngelaki A, Akolekar R, Lai J, Nicolaides KH (2013) Combined screening for preeclampsia and small for gestational age at 11–13 weeks. Fetal Diagn Ther 33: 16–27. doi: 10.1159/000341712 [DOI] [PubMed] [Google Scholar]
- 123.Crovetto F, Figueras F, Triunfo S, Crispi F, Rodriguez-Sureda V, Dominguez C, et al. (2015) First trimester screening for early and late preeclampsia based on maternal characteristics, biophysical parameters, and angiogenic factors. Prenat Diagn 35: 183–191. doi: 10.1002/pd.4519 [DOI] [PubMed] [Google Scholar]
- 124.Poon LC, Kametas NA, Maiz N, Akolekar R, Nicolaides KH (2009) First-trimester prediction of hypertensive disorders in pregnancy. Hypertension 53: 812–818. doi: 10.1161/HYPERTENSIONAHA.108.127977 [DOI] [PubMed] [Google Scholar]
- 125.Akolekar R, Minekawa R, Veduta A, Romero XC, Nicolaides KH (2009) Maternal plasma inhibin A at 11–13 weeks of gestation in hypertensive disorders of pregnancy. Prenat Diagn 29: 753–760. doi: 10.1002/pd.2279 [DOI] [PubMed] [Google Scholar]
- 126.O'Gorman N, Wright D, Rolnik DL, Nicolaides KH, Poon LC (2016) Study protocol for the randomised controlled trial: combined multimarker screening and randomised patient treatment with ASpirin for evidence-based PREeclampsia prevention (ASPRE). BMJ Open 6: e011801 doi: 10.1136/bmjopen-2016-011801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Romero R, Espinoza J, Gotsch F, Kusanovic JP, Friel LA, Erez O, et al. (2006) The use of high-dimensional biology (genomics, transcriptomics, proteomics, and metabolomics) to understand the preterm parturition syndrome. BJOG 113 Suppl 3: 118–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Romero R, Chaemsaithong P, Xu Z, Docheva N, Chaiyasit N, Chaiworapongsa T, et al. (2015) Abstract O-0278, The Maternal Plasma Proteome Changes As A Function Of Gestational Age In Normal Pregnancy: A Longitudinal Study. 12th World Congress of Perinatal Medicine, Madrid, Spain
- 129.Ngo D, Sinha S, Shen D, Kuhn EW, Keyes MJ, Shi X, et al. (2016) Aptamer-Based Proteomic Profiling Reveals Novel Candidate Biomarkers and Pathways in Cardiovascular Disease. Circulation 134: 270–285. doi: 10.1161/CIRCULATIONAHA.116.021803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mehan MR, Ayers D, Thirstrup D, Xiong W, Ostroff RM, Brody EN, et al. (2012) Protein signature of lung cancer tissues. PLoS One 7: e35157 doi: 10.1371/journal.pone.0035157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ostroff RM, Mehan MR, Stewart A, Ayers D, Brody EN, Williams SA, et al. (2012) Early detection of malignant pleural mesothelioma in asbestos-exposed individuals with a noninvasive proteomics-based surveillance tool. PLoS One 7: e46091 doi: 10.1371/journal.pone.0046091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mehan MR, Williams SA, Siegfried JM, Bigbee WL, Weissfeld JL, Wilson DO, et al. (2014) Validation of a blood protein signature for non-small cell lung cancer. Clin Proteomics 11: 32 doi: 10.1186/1559-0275-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Webber J, Stone TC, Katilius E, Smith BC, Gordon B, Mason MD, et al. (2014) Proteomics analysis of cancer exosomes using a novel modified aptamer-based array (SOMAscan) platform. Mol Cell Proteomics 13: 1050–1064. doi: 10.1074/mcp.M113.032136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Hathout Y, Brody E, Clemens PR, Cripe L, DeLisle RK, Furlong P, et al. (2015) Large-scale serum protein biomarker discovery in Duchenne muscular dystrophy. Proc Natl Acad Sci U S A 112: 7153–7158. doi: 10.1073/pnas.1507719112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Drolet DW, Green LS, Gold L, Janjic N (2016) Fit for the Eye: Aptamers in Ocular Disorders. Nucleic Acid Ther. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.(2002) ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol 99: 159–167. [DOI] [PubMed] [Google Scholar]
- 137.(1998) NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Obesity in Adults (US). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda (MD): National Heart, Lung, and Blood Institute.
- 138.Gold L, Ayers D, Bertino J, Bock C, Bock A, Brody EN, et al. (2010) Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS One 5: e15004 doi: 10.1371/journal.pone.0015004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Davies DR, Gelinas AD, Zhang C, Rohloff JC, Carter JD, O'Connell D, et al. (2012) Unique motifs and hydrophobic interactions shape the binding of modified DNA ligands to protein targets. Proc Natl Acad Sci U S A 109: 19971–19976. doi: 10.1073/pnas.1213933109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.SomaLogic. SOMAmer Technical notes: http://www.somalogic.com/somalogic/media/Assets/PDFs/SSM-017-Rev-3-SOMAmer-Technical-Note-3-7-15.pdf.
- 141.Bates D, Maechler M, Bolker B, Walker S (2014) lme4: Linear mixed-effects models using Eigen and S4. http://arxivorg/abs/14065823
- 142.Tarca AL, Than N. G., Romero R. (2013) Methodological approach from the Best Overall Team in the sbv IMPROVER Diagnostic Signature Challenge. Systems Biomedicine 1. [Google Scholar]
- 143.Tarca AL, Lauria M, Unger M, Bilal E, Boue S, Kumar Dey K, et al. (2013) Strengths and limitations of microarray-based phenotype prediction: lessons learned from the IMPROVER Diagnostic Signature Challenge. Bioinformatics 29: 2892–2899. doi: 10.1093/bioinformatics/btt492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dayarian A, Romero R, Wang Z, Biehl M, Bilal E, Hormoz S, et al. (2014) Predicting protein phosphorylation from gene expression: top methods from the IMPROVER Species Translation Challenge. Bioinformatics. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Smyth GK (2012) Limma: linear models for microarray data In: Gentleman R, Carey VJ, Huber W, Irizarry RA, Dudoit S, editors. Bioinformatics and Computational Biology Solutions Using R and Bioconductor: Springer; pp. 397–420. [Google Scholar]
- 146.Gentleman RC, Carey VJ, Bates DM, Bolstad B, Dettling M, Dudoit S, et al. (2004) Bioconductor: open software development for computational biology and bioinformatics. Genome Biol 5: R80 doi: 10.1186/gb-2004-5-10-r80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Maglott D, Ostell J, Pruitt KD, Tatusova T (2005) Entrez Gene: gene-centered information at NCBI. Nucleic Acids Res 33: D54–58. doi: 10.1093/nar/gki031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Ashburner M, Ball CA, Blake JA, Botstein D, Butler H, Cherry JM, et al. (2000) Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nat Genet 25: 25–29. doi: 10.1038/75556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Romero R, Erez O, Maymon E, Chaemsaithong P, Xu Z, Pacora P, et al. (2017) The maternal plasma proteome changes as a function of gestational age in normal pregnancy: a longitudinal study. Accepted. Am J Obstet Gynecol. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sibai BM (1990) The HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets): much ado about nothing? Am J Obstet Gynecol 162: 311–316. [DOI] [PubMed] [Google Scholar]
- 151.Mbah AK, Kornosky JL, Kristensen S, August EM, Alio AP, Marty PJ, et al. (2010) Super-obesity and risk for early and late pre-eclampsia. BJOG 117: 997–1004. doi: 10.1111/j.1471-0528.2010.02593.x [DOI] [PubMed] [Google Scholar]
- 152.Ornaghi S, Tyurmorezova A, Algeri P, Giardini V, Ceruti P, Vertemati E, et al. (2013) Influencing factors for late-onset preeclampsia. J Matern Fetal Neonatal Med 26: 1299–1302. doi: 10.3109/14767058.2013.783807 [DOI] [PubMed] [Google Scholar]
- 153.Durst JK, Tuuli MG, Stout MJ, Macones GA, Cahill AG (2016) Degree of obesity at delivery and risk of preeclampsia with severe features. Am J Obstet Gynecol 214: 651 e651–655. [DOI] [PubMed] [Google Scholar]
- 154.Burke B (2004) The role of matrix metalloproteinase 7 in innate immunity. Immunobiology 209: 51–56. doi: 10.1016/j.imbio.2004.04.005 [DOI] [PubMed] [Google Scholar]
- 155.Wilson CL, Ouellette AJ, Satchell DP, Ayabe T, Lopez-Boado YS, Stratman JL, et al. (1999) Regulation of intestinal alpha-defensin activation by the metalloproteinase matrilysin in innate host defense. Science 286: 113–117. [DOI] [PubMed] [Google Scholar]
- 156.Beckmann I, Efraim SB, Vervoort M, Visser W, Wallenburg HC (2004) Tumor necrosis factor-alpha in whole blood cultures of preeclamptic patients and healthy pregnant and nonpregnant women. Hypertens Pregnancy 23: 319–329. doi: 10.1081/PRG-200030334 [DOI] [PubMed] [Google Scholar]
- 157.Schiff E, Friedman SA, Baumann P, Sibai BM, Romero R (1994) Tumor necrosis factor-alpha in pregnancies associated with preeclampsia or small-for-gestational-age newborns. Am J Obstet Gynecol 170: 1224–1229. [DOI] [PubMed] [Google Scholar]
- 158.Goncalves I, Bengtsson E, Colhoun HM, Shore AC, Palombo C, Natali A, et al. (2015) Elevated Plasma Levels of MMP-12 Are Associated With Atherosclerotic Burden and Symptomatic Cardiovascular Disease in Subjects With Type 2 Diabetes. Arterioscler Thromb Vasc Biol 35: 1723–1731. doi: 10.1161/ATVBAHA.115.305631 [DOI] [PubMed] [Google Scholar]
- 159.Pelisek J, Rudelius M, Zepper P, Poppert H, Reeps C, Schuster T, et al. (2009) Multiple biological predictors for vulnerable carotid lesions. Cerebrovasc Dis 28: 601–610. doi: 10.1159/000247605 [DOI] [PubMed] [Google Scholar]
- 160.Abbas A, Aukrust P, Russell D, Krohg-Sorensen K, Almas T, Bundgaard D, et al. (2014) Matrix metalloproteinase 7 is associated with symptomatic lesions and adverse events in patients with carotid atherosclerosis. PLoS One 9: e84935 doi: 10.1371/journal.pone.0084935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Halpert I, Sires UI, Roby JD, Potter-Perigo S, Wight TN, Shapiro SD, et al. (1996) Matrilysin is expressed by lipid-laden macrophages at sites of potential rupture in atherosclerotic lesions and localizes to areas of versican deposition, a proteoglycan substrate for the enzyme. Proc Natl Acad Sci U S A 93: 9748–9753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Katabuchi H, Yih S, Ohba T, Matsui K, Takahashi K, Takeya M, et al. (2003) Characterization of macrophages in the decidual atherotic spiral artery with special reference to the cytology of foam cells. Med Electron Microsc 36: 253–262. doi: 10.1007/s00795-003-0223-2 [DOI] [PubMed] [Google Scholar]
- 163.Kim YM, Chaemsaithong P, Romero R, Shaman M, Kim CJ, Kim JS, et al. (2015) The frequency of acute atherosis in normal pregnancy and preterm labor, preeclampsia, small-for-gestational age, fetal death and midtrimester spontaneous abortion. J Matern Fetal Neonatal Med 28: 2001–2009. doi: 10.3109/14767058.2014.976198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Smith SD, Dunk CE, Aplin JD, Harris LK, Jones RL (2009) Evidence for immune cell involvement in decidual spiral arteriole remodeling in early human pregnancy. Am J Pathol 174: 1959–1971. doi: 10.2353/ajpath.2009.080995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Vettraino IM, Roby J, Tolley T, Parks WC (1996) Collagenase-I, stromelysin-I, and matrilysin are expressed within the placenta during multiple stages of human pregnancy. Placenta 17: 557–563. [DOI] [PubMed] [Google Scholar]
- 166.Maymon E, Romero R, Pacora P, Gervasi MT, Edwin SS, Gomez R, et al. (2000) Matrilysin (matrix metalloproteinase 7) in parturition, premature rupture of membranes, and intrauterine infection. Am J Obstet Gynecol 182: 1545–1553. doi: 10.1067/mob.2000.107652 [DOI] [PubMed] [Google Scholar]
- 167.Reister F, Kingdom JC, Ruck P, Marzusch K, Heyl W, Pauer U, et al. (2006) Altered protease expression by periarterial trophoblast cells in severe early-onset preeclampsia with IUGR. J Perinat Med 34: 272–279. doi: 10.1515/JPM.2006.052 [DOI] [PubMed] [Google Scholar]
- 168.Martinez-Fierro ML, Perez-Favila A, Garza-Veloz I, Espinoza-Juarez MA, Avila-Carrasco L, Delgado-Enciso I, et al. (2017) Matrix metalloproteinase multiplex screening identifies increased MMP-2 urine concentrations in women predicted to develop preeclampsia. Biomarkers: 1–7. [DOI] [PubMed] [Google Scholar]
- 169.Chaiworapongsa T, Chaemsaithong P, Korzeniewski SJ, Yeo L, Romero R (2014) Pre-eclampsia part 2: prediction, prevention and management. Nat Rev Nephrol 10: 531–540. doi: 10.1038/nrneph.2014.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Chaiworapongsa T, Romero R, Korzeniewski SJ, Kusanovic JP, Soto E, Lam J, et al. (2013) Maternal plasma concentrations of angiogenic/antiangiogenic factors in the third trimester of pregnancy to identify the patient at risk for stillbirth at or near term and severe late preeclampsia. Am J Obstet Gynecol 208: 287.e281–287.e215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Chaiworapongsa T, Romero R, Savasan ZA, Kusanovic JP, Ogge G, Soto E, et al. (2011) Maternal plasma concentrations of angiogenic/anti-angiogenic factors are of prognostic value in patients presenting to the obstetrical triage area with the suspicion of preeclampsia. J Matern Fetal Neonatal Med 24: 1187–1207. doi: 10.3109/14767058.2011.589932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chaiworapongsa T, Romero R, Whitten AE, Korzeniewski SJ, Chaemsaithong P, Hernandez-Andrade E, et al. (2015) The use of angiogenic biomarkers in maternal blood to identify which SGA fetuses will require a preterm delivery and mothers who will develop pre-eclampsia. J Matern Fetal Neonatal Med: 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Romero R, Chaiworapongsa T (2013) Preeclampsia: a link between trophoblast dysregulation and an antiangiogenic state. J Clin Invest 123: 2775–2777. doi: 10.1172/JCI70431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Levine RJ, Lam C, Qian C, Yu KF, Maynard SE, Sachs BP, et al. (2006) Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N Engl J Med 355: 992–1005. doi: 10.1056/NEJMoa055352 [DOI] [PubMed] [Google Scholar]
- 175.(2016) Practice Bulletin No. 163 Summary: Screening for Fetal Aneuploidy. Obstet Gynecol 127: 979–981. doi: 10.1097/AOG.0000000000001439 [DOI] [PubMed] [Google Scholar]
- 176.(2016) Practice Bulletin No. 162: Prenatal Diagnostic Testing for Genetic Disorders. Obstet Gynecol 127: e108–122. [DOI] [PubMed] [Google Scholar]
- 177.Baer RJ, Flessel MC, Jelliffe-Pawlowski LL, Goldman S, Hudgins L, Hull AD, et al. (2015) Detection Rates for Aneuploidy by First-Trimester and Sequential Screening. Obstet Gynecol 126: 753–759. doi: 10.1097/AOG.0000000000001040 [DOI] [PubMed] [Google Scholar]
- 178.Dashe JS (2016) Aneuploidy Screening in Pregnancy. Obstet Gynecol 128: 181–194. doi: 10.1097/AOG.0000000000001385 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Protein abundance data for each sample (rows) and each of the 1125 proteins is given in this table. ID: anonymized identifier indicator of the patient, GA: gestational age at sample, LatePE: is 1 for late preeclampsia and 0 for normal pregnancy. Protein symbol and names provide by Somalogic, Inc, are included above the protein accession numbers.
(CSV)
Thirty-six proteins that were significant (Sig.) (q<0.25 and fold change >1.1) in at least one interval are shown. Adjustment was performed for BMI, maternal age, parity and smoking. FC: linear fold change, with negative values denoting lower while positive values denoting higher level in cases than in controls, p: p-value, q: adjusted p-value, GA: gestational age. The column labeled as “Changes with GA” indicates whether the protein abundance changes with gestational age [128].
(XLS)
Data Availability Statement
All relevant data are included within the paper and its Supporting Information files.