Abstract
Objectives
The relationship between body mass index (BMI) with mortality risk, in particular the BMI category associated with the lowest all-cause and CVD-and-stroke mortality and the BMI threshold for defining overweight or obesity in older persons is controversial. This study investigated the age-dependent associations of BMI categories with all-cause and cardiovascular disease (CVD) and stroke mortality.
Method
Prospective cohort study (Singapore Longitudinal Ageing Studies) of older adults aged 55 and above, followed up from 2003 to 2011. Participants were 2605 Chinese with baseline BMI and other variables. Outcome Measurement: Mortality hazard ratios (HR) for all-cause and CVD and stroke mortality.
Results
Overall, BMI showed a U-shaped relationship with all-cause and CVD and stroke mortality, being lowest at Normal Weight-II category (BMI 23.0–24.9 kg/m2). Most evidently among the middle-aged (55–64 years), all-cause mortality risks relative to Normal Weight-II were elevated for underweight (<BMI 18.5; HR = 4.92, p<0.0138), Normal Weight-I (BMI 18.5–22.9; HR = 3.41, p = 0.0149), and Overweight-Obese (BMI>30.0; HR = 4.05,p = 0.0423). Among the old (≥65 years), however, Overweight and Obese categories were not significantly associated with increased all-cause mortality (HR from 0.98 to 1.29), but Overweight-Obese was associated with increased CVD and stroke mortality (HR = 10.0, p = 0.0086).
Conclusion
BMI showed a U-shaped relationship with mortality. Among older persons aged 65 and above, the overweight-or-obese category of BMI was not associated with excess all-cause mortality.
Introduction
Body mass index (BMI) is known to be associated with a continuum of health risks, with many studies showing a U-shaped relationship. [1–7] Along this continuum, the appropriate BMI cut-off point to define overweight and obesity that is associated with increased mortality risk is controversial. In the 1980’s to 2000’s, the U.S. Dietary Guidelines have variously defined overweight using BMI of 24.9 to 27.1. In 1985, the U.S. National Institutes of Health (NIH) recommended that overweight be defined using BMI 27.8 for men and 27.3 for women. In the 1990s, the definitive guide set by both the NIH and World Health Organization (WHO) was BMI over 25 for overweight and BMI over 30 for obesity.
However, emerging evidence showed that Asian populations are at an increased risk of type 2 diabetes mellitus and cardiovascular diseases at lower BMI levels below 25 kg/m2 than their Western counterparts, and Asians with the same BMI as their Western counterparts have higher body fat percentages and greater abdominal and visceral fat deposition. [8] In 2004 the WHO recommended lowering the BMI cut-offs for Asian adults for overweight from 25 to 23 kg/m2 and for obesity from 30 to 27.5 kg/m2. [9] As there is evidently increased cardio-metabolic disease risk at an even lower BMI among South Asian populations, [10] India has adopted the lower BMI cut-off points of 23 kg/m2 for overweight and 25 kg/m2 for obesity. [11]
Large prospective cohort studies of Western populations variously indicated that the BMI category associated with the lowest all-causes mortality rate was at 22.5 to 25.0 kg/m2, [12] or 20.0 to 25.0 kg/m2, [13] whereas other studies [14–18] showed that BMI category 25-<30 typically associated with overweight, was associated with lower all-causes mortality, compared to normal weight (BMI of 18.5-<25). Reports of mortality risks associated with BMI among Asians were also mixed. [1,2,4,5,7,19–21] The relationship between BMI and all-cause and cardiovascular disease (CVD) and stroke mortality may depend on age, being attenuated or reversed in older age groups. [2, 22–24] Divergent findings may also be due to distortions produced by weight loss because of pre-existing disease (so-called ‘reverse’ causality). It is pertinent to note that the desired level of BMI recommended in clinical guidelines on the management of overweight and obesity in adults were primarily based on studies in young and middle-aged cohorts, [25] and may not be relevant in older persons.
The objectives of this study were to investigate the associations of BMI categories with all-causes and CVD and stroke mortality in a population cohort of middle-aged and older Chinese men and women in Singapore. We used the International Classification recommended by WHO of Underweight (<18.5), Normal weight-I (18.5–22.9), Normal weight-II (23.0–24.99), Overweight Pre-obese-I (25.0–27.49), Overweight-Pre-obese-II (27.5–29.99), Overweight-Obese Class I, II, III (≥30.0), and sought in particular to determine the BMI category associated with the lowest all-cause and CVD-and-stroke mortality, and whether the mortality risk associated with over-weight and obesity was age-dependent for younger middle-aged (55 to 64 years) and older (65 and over) individuals.
Method
Study design
We conducted a prospective follow up study of mortality in a cohort of 2808 participants in the Singapore Longitudinal Ageing Study (SLAS) from September 2003 to December 2011. We excluded those who reported recent loss of weight of 5 kg or more in the last six months (N = 104), and those with missing data on BMI and other variables. The final sample comprised 2604 Chinese participants with BMI data in this study.
Study population
Between September 2003 and December 2005, a whole population of older adults aged 55 years and above who were Singaporean residents in contiguous precincts in the South East region of Singapore were identified from a door-to-door census and invited to participate in the Singapore Longitudinal Ageing Study (SLAS). The response rate was 78.2%. All participants provided written informed consent. The study was approved by National University of Singapore Institutional Review Board. Full details of the survey procedures and baseline variables and data collection are described in previous publications. [26]. Baseline information on demographic and socioeconomic status, medical history, physical activity, and smoking and alcohol history were collected from face-to-face interviews conducted by trained nurses using structured questionnaires at the participants’ home, and physical examination and testing were conducted at a local study site.
Measures
Body mass index (weight divided by height-squared (kg/m2) was determined from measurements of the participant’s weight (in kilogram) and height (in metres). Based on BMI, participants were classified as Underweight (<18.5), Normal weight-I(18.5–22.9), Normal weight-II (23.0–24.99), Overweight Pre-obese-I (25.0–27.49), Overweight-Pre-obese-II (27.5–29.99), Overweight-Obese Class I, II, III (≥30.0), using the International Classification recommended by WHO.
Covariates
Baseline data on sociodemographic and lifestyle variables were collected and categorized for education (>6 years, < = 6 years), smoking status (non-smoker, past smoker, current smoker), alcohol intake (≥1 drinks daily). Physical activity was assessed using questions on the frequency (0 = never or less than once a month; 1 = sometimes, i.e. once a month or more but less than once a week; 2 = often, i.e. at least once a week) of participation in brisk walking, physical workout routines, sports activities, and other physical recreational activities (e.g. taiji and qigong) and summed scores of physical activity score were categorized (0–1, 2–3, 4–8) for analyses.
Mortality follow up
Information on date and cause of death of each study participant during follow up from baseline up to 31 December 2011 was determined using their unique National Registration Identity Card (NRIC) number for computerized record linkage with the National Death Registry through the National Disease Registry Office (NDRO) of the Ministry of Health.
Statistical analyses
Comparison of baseline characteristics between study participants by BMI categories were performed with significance testing using t-test for continuous variables and χ2 for categorical variables. Univariate and multivariate Cox proportionate hazard regression analyses were used to estimate hazard ratio (HR) with 95% confidence intervals (95% C.I.) of all-causes and CVD and stroke mortality risks associated with BMI categories. Age (continuous), sex (men versus women), education (≤6 years versus >6 years), smoking (never, past and current smoking), alcohol intake (>1 drink daily: yes versus no), and physical activity level (scores of 0–1, 2–3, 4–8) were included as adjustment covariates in the Cox models. In stratified analyses, we assessed whether the association between BMI and the risk of death varied according to age group: younger middle-aged (55–64 years and older-aged (≥65 years).
Results
Table 1 shows the demographic and health risk profiles of the study participants by BMI categories. Among the total of 2604 participants, 6.1% had BMI<18.5 (Underweight), 17.9% had BMI: 25.0–27.49 (Overweight Pre-obese-I), 8.6% had BMI: 27.5–29.99 (Overweight-Pre-obese-II) and 4.6% had BMI: ≥30.0 (Overweight Obese Class I, II, and III). Participants who were underweight were significantly older, and more likely to be current smokers at the start of the follow up.
Table 1. Baseline characteristics by BMI status.
| <18.5 Underweight | 18.5–22.9 Normal-I | 23.0–24.99 Normal-II | 25.0–27.49 Overweight Pre Obese-I | 27.5–29.99 Overweight Pre obese-II | ≥30.0 Overweight, Obese Class I, II, III | P | |
|---|---|---|---|---|---|---|---|
| N | 158 | 1039 | 595 | 467 | 224 | 121 | 0.0049 |
| Age (mean, SD) | 67.7 (8.5) | 65.9 (8.0) | 65.9 (7.1) | 66.5 (7.5) | 65.5 (6.9) | 64.4 (7.5) | 0.0017 |
| 55–64 | 63 (40.1) | 526 (50.8) | 295 (49.6) | 225 (48.4) | 113 (50.7) | 70 (58.3) | |
| 65–84 | 87 (55.1) | 484 (46.6) | 295 (49.6) | 235 (50.3) | 109 (48.7) | 51 (42.2) | |
| 85- | 8 (5.1) | 29 (2.8) | 5 (0.8) | 7 (1.5) | 2 (0.9) | 0 | |
| Female | 95 (60.1) | 690 (66.4) | 356 (59.8) | 271 (58.0) | 154 (68.8) | 76 (62.8) | 0.0057 |
| Male | 63 (39.9) | 349 (33.6) | 239 (40.2) | 196 (42.0) | 70 (31.3) | 45 (37.2) | |
| Education: >6 years | 67 (42.4) | 538 (51.8) | 289 (48.6) | 205 (43.9) | 98 (43.8) | 53 (43.8) | 0.0181 |
| < = 6 years | 91 (57.6) | 501 (48.2) | 306 (51.4) | 262 (56.1) | 126 (56.3) | 68 (56.2) | |
| Smoking: Non-smoker | 123 (77.9) | 883 (85.1) | 490 (82.6) | 382 (82.0) | 190 (84.8) | 102 (84.3) | 0.0099 |
| Past smoker | 15 (9.5) | 87 (8.4) | 67 (11.3) | 59 (12.7) | 26 (11.6) | 14 (11.6) | |
| Current smoker | 20 (12.7) | 68 (6.6) | 36 (6.1) | 25 (5.4) | 8 (3.6) | 5 (4.1) | |
| Alcohol: >1 drinks daily | 6 (3.8) | 19 (1.8) | 11 (1.9) | 9 (1.9) | 0 | 2 (1.7) | 0.1703 |
| Physical activity score: | |||||||
| 0–1 | 51 (32.9) | 297 (29.0) | 168 (28.5) | 139 (30.0) | 82 (37.1) | 40 (33.6) | 0.0734 |
| 2–3 | 56 (36.1) | 329 (32.1) | 183 (31.2) | 150 (32.4) | 73 (33.0) | 45 (37/8) | |
| 4–8 | 48 (31.0) | 398 (38.9) | 238 (40.4) | 174 (37.6) | 66 (29.9) | 34 (28.6) |
There were a total of 224 deaths among the 2605 study participants with 8,440 person-years of follow up. The number of deaths from CVD and stroke was 38 (17%) and from non-CVD and stroke was 186 (83%).
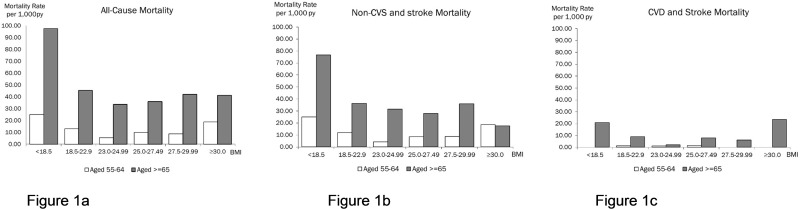
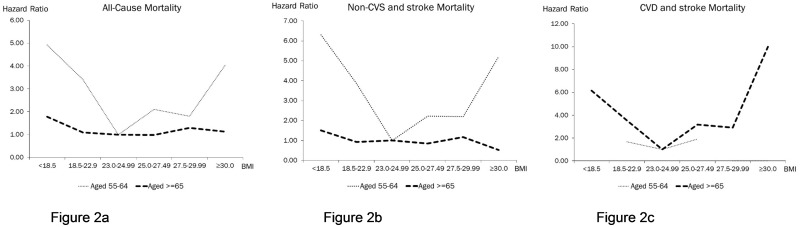
BMI categories and all-cause mortality
The rates and relative risks for all-cause mortality across all categories of BMI showed a U-shaped relationship, being lowest at Normal Weight-II category (BMI 23.0–24.9 kg/m2). (Table 2; Figs 1a and 2a) This was clearly evident among the middle-aged (55–64 years), among whom all-causes mortality risks relative to Normal Weight-II were higher for Underweight (HR = 4.92, p<0.0138), Normal Weight-I (HR = 3.41, p = 0.0149) and Overweight-Obese (HR = 4.05, p = 0.0423).
Table 2. Associations of BMI with total and cardiovascular mortality by age strata.
| Total Mortality | ||||
|---|---|---|---|---|
| BMI categories | Pop/deaths | /1000 p-y | Adj HR | (95% C.I.) |
| Whole cohort | ||||
| <18.5 (Underweight) | 158/33 | 67.7 | 2.06 | (1.27–3.35) |
| 18.5–22.9 (Normal weight) | 1039/92 | 29.1 | 1.32 | (0.90–1.95) |
| 23.0–24.99(Normal-weight-II) | 595/37 | 19.7 | 1.00 | |
| 25.0–27.49 (Overweight Pre-obese-I) | 467/34 | 23.5 | 1.12 | (0.70–1.78) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 224/17 | 25.1 | 1.34 | (0.75–2.38) |
| ≥30.0 (Overweight Obese Class I, II, III) | 121/11 | 28.6 | 1.52 | (0.77–2.98) |
| Middle-aged cohort, 55–64 years | ||||
| <18.5 (Underweight) | 63/5 | 25.0 | 4.92 | (1.38–17.47) |
| 18.5–22.9 (Normal weight) | 526/21 | 13.2 | 3.41 | (1.27–9.17) |
| 23.0–24.99(Normal-weight-II) | 295/5 | 5.4 | 1.00 | |
| 25.0–27.49 (Overweight Pre-obese-I) | 225/7 | 10.0 | 2.10 | (0.66–6.65) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 113/3 | 8.7 | 1.80 | (0.42–7.67) |
| ≥30.0 (Overweight Obese Class I, II, III) | 70/4 | 18.7 | 4.05 | (1.05–15.65) |
| Old cohort, 65+ | ||||
| <18.5 (Underweight) | 95/28 | 97.6 | 1.78 | (1.05–3.02) |
| 18.5–22.9 (Normal weight) | 513/71 | 45.3 | 1.09 | (0.71–1.66) |
| 23.0–24.99(Normal-weight-II) | 300/32 | 33.6 | 1.00 | |
| 25.0–27.49 (Overweight Pre-obese-I) | 242/27 | 35.9 | 0.98 | (0.58–1.65) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 111/14 | 42.0 | 1.29 | (0.68–2.43) |
| ≥30.0 (Overweight Obese Class I, II, III) | 51/7 | 41.2 | 1.13 | (0.50–2.59) |
Fig 1. Mortality rates for All Causes, non-CVS and stroke and CVD and stroke by BMI categories among middle-aged (55–64 years) and old-aged (> = 65 years) participants.
Fig 2. Mortality hazard ratios for All causes, Non-CVS and stroke and CVD and stroke by BMI categories among middle-aged (55–64) and old-aged (> = 65 years) participants.
Among the older participants (≥65 years), however, only Underweight was associated with higher all-cause mortality (HR = 1.78, p = 0.0336), whereas Overweight and Obese categories were not significantly associated with increased all-causes mortality (HR from 0.98 to 1.29).
BMI categories and CVS and stroke mortality
There were small counts of death, and no meaningful relationships were discernible for deaths from CVD and stroke among the young middle-aged. However, among the older participants aged 65 and above, both Underweight (HR = 6.15, p = 0.0299) and Overweight-Obese (HR = 10.0, p = 0.0086) were significantly associated with markedly increased CVD and stroke mortality (Figs 1b, 1c, 2b and 2c).
Discussion
Our study confirms previous findings describing the U-shaped relationship of BMI with all-causes mortality. [1–7] In this population of middle-aged and older Asians, the BMI category associated with the lowest all-cause mortality was 23 to 24.99 kg/m2 (Normal Weight II). This is consistent with meta-analyses indicating that the all-cause mortality rate was lowest at 22.5 to 25.0 kg/m2. [12]
In agreement with previous studies, [6–7, 12] we also observed an age-dependency of associations of BMI with mortality risk in that the relative risk of death associated with BMI was higher among middle-aged persons (aged 55–64) and decreased among older persons (> = 65). For example, the HR of total mortality associated with being underweight was 4.92 in the middle-aged group and 1.78 in the older age group. The HR of total mortality associated with being overweight-obese (BMI> = 30) was 4.05 in the middle-aged group and 1.13 in the older age group
We thus observed that among older persons aged 65 and above, being overweight or obese compared to normal weight was not significantly associated with increased all-cause mortality risks. This agrees with previous studies involving older populations. [2, 15–19] Although among older persons, being overweight or obese was significantly associated with markedly increased CVD and stroke mortality (HR = 10.0, p = 0.0086), CVD and stroke mortality however comprised less than a quarter of deaths among the older participants. Thus the lack of association of overweight-obesity with increased total mortality among the older participants was due to lower mortality predominantly from non-vascular causes of death (cancer, pneumonia, injury, COPD and others).
There are more than a few explanations for the lowered mortality associated with being overweight and obese among older persons. One explanation is the limitation of BMI as an indicator of body fat, as older persons tend to have more body fat at the same BMI as younger adults, with greater BMI possibly reflecting relatively greater fat-free mass, rather than greater body fat. Another explanation is survival bias. Because obese persons were more likely to die earlier at younger ages, those who survived into old age were selectively healthier, commensurate with recent observations of a population subgroup of obese people who are ‘metabolically healthy’. [27–29]. Another explanation is confounding due to disease-associated unintentional weight loss prior to death among obese individuals. This may result in shifting misclassification of obese individuals into the categories of low or normal BMI category. This explanation for our observed association is considered to be less likely as we excluded those who reported recent loss of weight of 5 kg or more in the last six months from various causes. Another possible explanation is the protective effect of adiposity against fatal health outcomes in late life. In opposition to the increased risk of death of persistent weight gain from early life, weight gain late in life may have possible beneficial effects, for example, through its association with increased bone mineral density (BMD), decreased osteoporosis, falls and hip fracture, and decreased mortality risks. [30–32] Elderly patients with chronic heart failure and end-stage renal failure with higher BMI are also known to have all-cause mortality that were lower compared to their non-obese counterparts, [33–36] a phenomenon that is widely referred to as the “obesity paradox”. [37–39]
In this study, underweight was found to be associated with increased all-cause mortality both among middle-aged and older individuals, including increased CVD-and-stroke mortality among older participants. This is expected, and is in agreement with many studies. Among older people, being under-weight largely reflects decreased muscle mass and strength, and is related to an increased risk of sarcopenia and frailty-associated functional limitation and mortality. [40–42] Because we have excluded those who reported significant weight loss prior to follow up, we believe that this reflects the increased risk from leanness, more than the confounding association due to pre-existing disease.
A limitation in this study is the relatively small number of deaths observed in the middle-aged group and for cardiovascular disease and stroke. In particular, there were no deaths due to CVD and stroke recorded in the middle-aged group, and the small number of deaths due this cause of death among the older group could contribute to the very high hazard ratio estimate associated with obesity. Because the estimates of odds ratio were imprecise, the age-differential in vascular disease-related mortality associated with BMI should therefore be interpreted with caution. The limitation of BMI measure to estimate adiposity is widely acknowledged in the literature. Further studies using waist circumference and other metabolic indicators of body composition should provide a much needed clearer understanding of the specific health risks associated with muscle mass and fat mass.
From a clinical standpoint, the controversy over the association between high BMI and lowered mortality in older adults may lead to misinterpretations or confusions regarding the desired level of BMI in older persons. Certainly, it should not be interpreted to mean that obesity conveys a lower mortality risk in older persons compared to younger and middle-aged persons, because the absolute mortality risk associated with increased BMI is still higher in older persons because of the marked increase in mortality with advancing age, as shown in the Table 3 and Fig 1a. However, the desired level of BMI recommended in clinical guidelines on the management of overweight and obesity in adults were primarily based on studies in young and middle-aged cohorts, [25] and may not be relevant in older persons. Among older adults, the health risk of under-weight or weight loss in older persons is a concern, largely reflective of the health risks of sarcopenia and frailty. Certainly, older persons who are obese with metabolic complications may benefit from weight-loss therapy if muscle and bone losses are minimized. [43] Studies have demonstrated the feasibility of exercise-induced reduction in waist circumference and abdominal fat without a corresponding reduction in BMI, [42–44] but more studies are needed.
Table 3. Associations of BMI with total and cardiovascular mortality by age strata.
| Non-Cardiovascular and Stroke Mortality | Cardiovascular and Stroke Mortality | |||||||
|---|---|---|---|---|---|---|---|---|
| BMI categories | Pop/deaths | /1000 p-y | Adj HR | (95% C.I.) | Pop/deaths | /1000 p-y | Adj HR | (95% C.I.) |
| Whole cohort | ||||||||
| <18.5 (Underweight) | 158/27 | 55.4 | 1.89 | (1.12–3.20) | 158/6 | 12.3 | 3.99 | (0.96–16.58) |
| 18.5–22.9 (Normal weight) | 1039/76 | 24.0 | 1.20 | (0.80–1.81) | 1039/16 | 5.1 | 2.73 | (0.79–9.44) |
| 23.0–24.99(Normal-weight-II) | 595/34 | 18.1 | 1 | (referent) | 595/3 | 1.6 | 1 | (referent) |
| 25.0–27.49 (Overweight Pre-obese-I) | 467/27 | 18.6 | 0.99 | (0.60–1.65) | 467/7 | 4.8 | 2.48 | (0.63–9.70) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 224/15 | 22.1 | 1.28 | (0.70–2.36) | 224/2 | 2.9 | 1.89 | (0.31–11.34) |
| ≥30.0 (Overweight Obese Class I, II, III) | 121/7 | 18.2 | 1.05 | (0.47–2.39) | 121/4 | 10.4 | 6.62 | (1.45–30.11) |
| Middle-aged cohort, 55–64 years | ||||||||
| <18.5 (Underweight) | 63/5 | 25.0 | 6.30 | (1.65–24.07) | 63/0 | NA | NA | NA |
| 18.5–22.9 (Normal weight) | 526/19 | 11.9 | 3.85 | (1.29–11.49) | 526/2 | 1.3 | 1.67 | (0.14–20.48) |
| 23.0–24.99(Normal-weight-II) | 295/4 | 4.3 | 1 | (referent) | 295/1 | 1.1 | 1 | (referent) |
| 25.0–27.49 (Overweight Pre-obese-I) | 225/6 | 8.6 | 2.23 | (0.62–7.96) | 225/1 | 1.4 | 1.92 | (0.11–34.76) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 113/3 | 8.7 | 2.20 | (0.48–10.03) | 113/0 | NA | NA | NA |
| ≥30.0 (Overweight Obese Class I, II, III) | 70/4 | 18.7 | 5.22 | (1.26–21.60) | 70/0 | NA | NA | NA |
| Old cohort, 65+ | ||||||||
| <18.5 (Underweight) | 95/22 | 76.7 | 1.50 | (0.84–2.67) | 95/6 | 20.9 | 6.15 | (1.19–31.68) |
| 18.5–22.9 (Normal weight) | 513/57 | 36.3 | 0.93 | (0.59–1.46) | 513/14 | 8.9 | 3.53 | (0.79–15.71) |
| 23.0–24.99(Normal-weight-II) | 300/30 | 31.5 | 1 | (referent) | 300/2 | 2.1 | 1 | (referent) |
| 25.0–27.49 (Overweight Pre-obese-I) | 242/21 | 28.0 | 0.84 | (0.48–1.47) | 242/6 | 8.0 | 3.17 | (0.63–15.93) |
| 27.5–29.99 (Overweight-Pre-obese-II) | 111/12 | 36.0 | 1.17 | (0.60–2.31) | 111/2 | 6.0 | 2.91 | (0.41–20.72) |
| ≥30.0 (Overweight Obese Class I, II, III) | 51/3 | 17.6 | 0.52 | (0.16–1.72) | 51/4 | 23.5 | 10.0 | (1.80–55.67) |
Covariates in in Cox regression model are: age (continuous), sex (men, women), education (≤6, >6 years), smoking, alcohol, physical activities
Acknowledgments
We thank the following voluntary welfare organizations for their support and contributions in kind: Geylang East Home for the Aged, Presbyterian Community Services, St Luke’s Eldercare Services, Thye Hua Kwan Moral Society (Moral Neighbourhood Links), Yuhua Neighbourhood Link, Henderson Senior Citizens’ Home, NTUC Eldercare Co-op Ltd, Thong Kheng Seniors Activity Centre (Queenstown Centre) and Redhill Moral Seniors Activity Centre.
Data Availability
Data are available from the national university of Singapore Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. For data requests, please contact National University of Singapore, Gerontology Research Program, 12 Science Drive 2, Singapore 117549 [pcmgq@nus.edu.sg].
Funding Statement
The study was supported by research grants from the Agency for Science Technology and Research (A*STAR) Biomedical Research Council (BMRC) [Grant: 08/1/21/19/567] and from the National Medical Research Council [Grant: NMRC/1108/2007]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Yuan JM, Ross RK, Gao YT, Yu MC. Body weight and mortality: a prospective evaluation in a cohort of middle-aged men in Shanghai, China. Int J Epidemiol. 1998. October;27(5):824–32. [DOI] [PubMed] [Google Scholar]
- 2.Jee SH, Sull JW, Park J et al. Body-mass index and mortality in Korean men and women. N Engl J Med 2006; 355, 779–787 doi: 10.1056/NEJMoa054017 [DOI] [PubMed] [Google Scholar]
- 3.Orpana HM, Berthelot JM, Kaplan MS et al. (2010) BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring) 2010; 18, 214–218. [DOI] [PubMed] [Google Scholar]
- 4.Tamakoshi A, Yatsuya H, Lin Y, Tamakoshi K, Kondo T, Suzuki S, Yagyu K, Kikuchi S; JACC Study Group. BMI and all-cause mortality among Japanese older adults: findings from the Japan collaborative cohort study. Obesity (Silver Spring). 2010. February;18(2):362–9. [DOI] [PubMed] [Google Scholar]
- 5.Pan WH, Yeh WT, Chen HJ et al. (2012) The U-shaped relationship between BMI and all-cause mortality contrasts with a progressive increase in medical expenditure: a prospective cohort study. Asia Pac J Clin Nutr 2012; 21, 577–587 [PubMed] [Google Scholar]
- 6.Heymsfield SB & Cefalu WT (2013) Does body mass index adequately convey a patient’s mortality risk? JAMA 2013; 309, 87–88. doi: 10.1001/jama.2012.185445 [DOI] [PubMed] [Google Scholar]
- 7.Chung WS, Ho FM, Cheng NC, Lee MC, Yeh CJ. BMI and all-cause mortality among middle-aged and older adults in Taiwan: a population-based cohort study. Public Health Nutr. 2015. July;18(10):1839–46. doi: 10.1017/S136898001400281X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S & Pierson RN (1994): Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am. J. Clin. Nutr. 60, 23–28. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization Expert Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363: 157–163 doi: 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 10.Gray LJ, Yates T, Davies MJ, Brady E, Webb DR, et al. (2011) Defining obesity cut-off points for migrant South Asians. PLoS One 6: e26464 doi: 10.1371/journal.pone.0026464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 12.Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body mass index and cause-specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–96. doi: 10.1016/S0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, Moore SC, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010. December 2;363(23):2211–9. doi: 10.1056/NEJMoa1000367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013. January 2;309(1):71–82. doi: 10.1001/jama.2012.113905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beleigoli AM, Boersma E, Diniz Mde F, Lima-Costa MF, Ribeiro AL. Overweight and class I obesity are associated with lower 10-year risk of mortality in Brazilian older adults: the Bambuí Cohort Study of Ageing. PLoS One. 2012;7(12):e52111 doi: 10.1371/journal.pone.0052111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grabowski DC, Ellis JE. High body mass index does not predict mortality in older people: analysis of the Longitudinal Study of Aging. J Am Geriatr Soc. 2001. July;49(7):968–79. [DOI] [PubMed] [Google Scholar]
- 17.Janssen I. Morbidity and mortality risk associated with an overweight BMI in older men and women. Obesity (Silver Spring). 2007. July;15(7):1827–40. [DOI] [PubMed] [Google Scholar]
- 18.Corrada MM, Kawas CH, Mozaffar F, Paganini-Hill A. Association of body mass index and weight change with all-cause mortality in the elderly. Am J Epidemiol. 2006. May 15;163(10):938–49. doi: 10.1093/aje/kwj114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gu D, He J, Duan X, Reynolds K, Wu X, Chen J, Huang G, Chen CS, Whelton PK. Body Weight and Mortality Among Men and Women in China. JAMA 2006; 295: 776–783. doi: 10.1001/jama.295.7.776 [DOI] [PubMed] [Google Scholar]
- 20.Song Y, Ha M, Sung J. Body mass index and mortality in middle-aged Korean women. Ann Epidemiol 2007; 27: 556–563. [DOI] [PubMed] [Google Scholar]
- 21.Zhang X, Shu XO, Chow WH, Yang G, Li H, Gao J, Gao YT, Zheng W. Body mass index at various ages and mortality in Chinese women: impact of potential methodological biases. Int J Obes 2008; 32: 1130–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagai M, Kuriyama S, Kakizaki M, Ohmori-Matsuda K, Sugawara Y, Sone T, Hozawa A, Tsuji I. Effect of age on the association between body mass index and all-cause mortality: the Ohsaki cohort study. J Epidemiol. 2010;20(5):398–407. doi: 10.2188/jea.JE20090204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tsugane S, Sasaki S, Tsubono Y. Under-and overweight impact on mortality among middle-aged Japanese men and women: a 10-y follow-up of JPHC study cohort I. Int J Obes 2002; 26: 529–537. [DOI] [PubMed] [Google Scholar]
- 24.Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998;338:1–7. doi: 10.1056/NEJM199801013380101 [DOI] [PubMed] [Google Scholar]
- 25.National Institutes of Health. National Heart Lung and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res 1998;6:S51–S210. [PubMed] [Google Scholar]
- 26.Niti M, Yap KB, Kua EH, Tan CH, Ng TP. Physical, social and productive leisure activities, cognitive decline and interaction with APOE-epsilon4 genotype in Chinese older adults. Int Psychogeriatr. 2008. January 11:1–15. [DOI] [PubMed] [Google Scholar]
- 27.Kuk J.L. & Ardern C.I. Are metabolically normal but obese individuals at lower risk for all-cause mortality? Diabetes Care, 2009; 32, 2297–2299. doi: 10.2337/dc09-0574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, Sowers MR. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008. August 11;168(15):1617–24. doi: 10.1001/archinte.168.15.1617 [DOI] [PubMed] [Google Scholar]
- 29.Karelis AD, Brochu M, Rabasa-Lhoret R. Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab. 2004;30: 569–572. [DOI] [PubMed] [Google Scholar]
- 30.Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res 2005;13: 1849–63. doi: 10.1038/oby.2005.228 [DOI] [PubMed] [Google Scholar]
- 31.Slemenda CW, Hui SL, Longcope C, Wellman H, Johnston CC Jr. Predictors of bone mass in perimenopausal women. A prospective study of clinical data using photon absorptiometry. Ann Intern Med 1990;112:96–101. [DOI] [PubMed] [Google Scholar]
- 32.Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 1993;8:567–73. doi: 10.1002/jbmr.5650080507 [DOI] [PubMed] [Google Scholar]
- 33.Landi F, Onder G, Gambassi G, Pedone C, Carbonin P, Bernabei R. Body mass index and mortality among hospitalized patients. Arch Intern Med 2000;160:2641–4. [DOI] [PubMed] [Google Scholar]
- 34.Mosterd A, Cost B, Hoes AW, de Bruijne MC, Deckers JW, Hofman A, Grobbee DE. The prognosis of heart failure in the general population: the Rotterdam Study. Eur Heart J 2001;22: 1318–27. doi: 10.1053/euhj.2000.2533 [DOI] [PubMed] [Google Scholar]
- 35.Lissin LW, Gauri AJ, Froelicher VF, Ghayoumi A, Myers J, Giacommini J. The prognostic value of body mass index and standard exercise testing in male veterans with congestive heart failure. J Card Fail 2002;8:206–15. [DOI] [PubMed] [Google Scholar]
- 36.Davos CH, Doehner W, Rauchhaus M, Cicoira M, Francis DP, Coats AJ, Clark AL, Anker SD. Body mass and survival in patients with chronic heart failure without cachexia: the importance of obesity. J Card Fail 2003;9:29–35. doi: 10.1054/jcaf.2003.4 [DOI] [PubMed] [Google Scholar]
- 37.Bouillanne O, Dupont-Belmont C, Hay P. Fat mass protects hospitalized elderly persons against morbidity and mortality. Am J Clin Nutr 2009; 90, 505–510. doi: 10.3945/ajcn.2009.27819 [DOI] [PubMed] [Google Scholar]
- 38.Chapman IM. (2010) Obesity paradox during aging. Interdiscip Top Gerontol 2010; 37, 20–36. doi: 10.1159/000319992 [DOI] [PubMed] [Google Scholar]
- 39.Lee IM, Paffenbarger RS Jr. Change in body weight and longevity. JAMA 1992; 268: 2045–2049. [PubMed] [Google Scholar]
- 40.Janssen I., Heymsfield S.B. & Ross R. (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 2002; 50, 889–896. [DOI] [PubMed] [Google Scholar]
- 41.Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men-a 22-year follow-up. The study of men born in 1913. Intl J Obes Related Metab Disorders 2000; 24, 33–37. [DOI] [PubMed] [Google Scholar]
- 42.Janssen I, Katzmarzyk PT, Ross R. Body mass index is inversely related to mortality in older people after adjustment for waist circumference. JAGS 53:2112–2118, 2005 [DOI] [PubMed] [Google Scholar]
- 43.Ross R, Janssen I, Dawson J et al. Exercise-induced reduction in obesity and insulin resistance in women: A randomized controlled trial. Obes Res 2004;12: 789–798. doi: 10.1038/oby.2004.95 [DOI] [PubMed] [Google Scholar]
- 44.Ross R, Dagnone D, Jones PJ et al. Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann Intern Med 2000;133: 92–103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the national university of Singapore Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. For data requests, please contact National University of Singapore, Gerontology Research Program, 12 Science Drive 2, Singapore 117549 [pcmgq@nus.edu.sg].