Abstract
Background & Objective
Buprenorphine is an underutilized pharmacotherapy that can play a key role in combating the opioid epidemic. Individuals with opioid use disorder (OUD) often struggle to find physicians that prescribe buprenorphine. Many physicians do not have the waiver to prescribe buprenorphine, and a large proportion of physicians that are waivered do not prescribe to capacity. This study aimed to quantitatively understand why physicians do not utilize buprenorphine for the treatment of OUD more frequently.
Methods
Physicians (n=558) with and without the waiver to prescribe buprenorphine were surveyed about perceived drawbacks associated with prescribing buprenorphine. Furthermore, resources were identified that would encourage those without the waiver to obtain it, and those with the waiver to accept more new patients. The survey was distributed online to physicians in the spring/summer of 2016 via the American Society for Addiction Medicine and American Medical Association Listervs.
Results and Conclusions
A logistic regression analysis was used to identify reasons that respondents indicated no willingness to increase prescribing (2(4) = 73.18, p < .001); main reasons were lack of belief in agonist treatment (or 3.98, 95% CI, 1.43 to 11.1, p = .008), lack of time for additional patients (or 5.54, 95% CI, 3.5 to 8.7, p < .001), and belief that reimbursement rates are insufficient (or 2.50, 95% CI, 1.3 to 4.8, p = .006). Differences between non-waivered and waivered physicians concerning attitudes toward buprenorphine treatment as well as resources that would increase willingness to prescribe are also discussed. Identifying barriers to buprenorphine utilization is crucial in expanding treatment options for individuals with OUD.
Keywords: Buprenorphine, Opioid Use Disorder, Opioid Maintenance Treatment, Physician
1. INTRODUCTION
The widespread abuse of both prescription and illicit opioids has had devastating consequences in the Untied States, and have led to public health crises regarding increases in opioid overdose deaths and opioid-related disease transmission (Centers for Disease Control and Prevention (CDC), 2011; Cicero, Ellis, Surratt, & Kurtz, 2014; Cicero et al., 2014; Compton, Jones, & Baldwin, 2016; Hedegaard, Chen, & Warner, 2015; National Center for Health Statistics et al., 2015; Selwyn et al., 1989). Extended maintenance on an opioid agonist is the current standard of care for the treatment of opioid use disorder (OUD) and is endorsed by the World Health Organization as an International Standard for the Treatment of Drug Use Disorders (Gerra, Koutsenok, Saenz, & Busse, 2015).
Two medications are approved for opioid maintenance treatment (OMT) of OUD in the U.S. The first is methadone, a full agonist on the mu opioid receptor with high abuseliability (Drug Enforcement Agency. 2016; Graham, Merlo Goldberger, & Gold, 2008; Winstock & Lea, 2010). Provision of methadone for OMT can be restrictive because federal law requires it be dispensed from authorized clinics and in liquid form. The second medication is buprenorphine (generally sold as buprenorphine/naloxone), which has several pharmacokinetic features that favors its use over methadone in primary care settings. Specifically, buprenorphine has a low ceiling on its agonist effects and a slow dissociation from the receptor, which confers reduced abuseliability relative to methadone while still allowing for once daily dosing to adequately suppress symptoms of withdrawal (Jasinski, Pevnick, & Griffith, 1978; Johnson, Strain, & Amass, 2003). Buprenorphine was approved for the treatment of OUD in 2002 with the requirement that physicians apply for a waiver from the Substance Abuse and Mental Health Services Administration (SAMHSA) in order to prescribe buprenorphine for OUD from primary care settings. Waivered physicians are allowed to prescribe buprenorphine to 30 OUD patients in the first year and 100 patients thereafter–although in 2016 this upper limit was increased to 275 patients (Schuckit, 2016; SAMHSA, 2016). Federal opiate treatment guidelines (SAMHSA, 2015a) also stipulate that patients have reasonable access to services such as counseling and that buprenorphine providers work to reduce the risk of medication diversion (Fudala et al., 2003).
Though it was widely believed that ability to prescribe buprenorphine from a primary care setting would increase the number of patients receiving OMT, physician adoption and utilization of buprenorphine has not been proportional to the magnitude of the opioid epidemic (Blum, Gold, Clark, Dushaj, & Badgaiyan, 2016; Knudsen, Ducharme, Roman, & Link, 2005). A recent survey reported a major shortage in the number of physicians utilizing buprenorphine as a treatment option in the United States; 96% of states (including the District of Columbia) report higher rates of opioid abuse or dependence than buprenorphine treatment capacity ( Jones, Campopiano, Baldwin, & McCance-Katz, 2015). Indeed, a major gap exists between the number of individuals in need of treatment (approximately 2.5 milion) (SAMHSA, 2015b) and the number of OMT providers (Murphy, Fishman, McPherson, Dyck. & Roll, 2014; Rosenblatt, Andriila. Catlin, & Larson, 2015). Further despite approval more than 10 years ago, a 2011 survey reported approximately 43% of counties in the U.S. still have no physicians waivered to prescribe buprenorphine (Stein et al., 2015). Large geographic disparities in buprenorphine availability also exist within counties that have at least one waivered physician, with up to a 30-fold difference in the number of waivered physicians per capita (Stein et al., 2015). These geographical disparities are prevalent in states that have been resistant of the Affordable Care Act (Knudsen, Lofwall Havens, & Walsh, 2015). Lack of waivered physicians is not the only issue affecting buprenorphine, availability. Recent data also suggests the majority of physicians who are waivered are not prescribing to their maximum capacity; for instance, one study reported 48.1% of waivered physicians were prescribing buprenorphine to 5 patients or fewer (Sigmon, 2015). It has been estimated that roughly half of individuals with OUD would be treated if all OMT providers were prescribing to their permitted capacity (Jones et al., 2015; Murphy et al., 2014; Rosenblatt et al., 2015).
Increasing the number of physicians who both receive the buprenorphine waiver and prescribe to capacity is critical to help combat the opioid use epidemic. Previous studies have examined physician attitudes toward buprenorphine as a potential barrier to adoption of OMT, however the few studies that gauged interest in physician resources to increase buprenorphine diffusion were conducted shortly after buprenorphine was approved (Turner, Laine, Lin, & Lynch, 2005). Much of the subsequent research has focused on physicians working with specialty populations such patients; with human immuno defficiency virus (HIV) (Cunningham, Kunins, Roose, Elam, & Sohler, 2007; Turner, Laine, Lin, & Lynch, 2005), or physicians in a specific geographic area (Cunningham, Sohler, McCoy, & Kunins, 2006; DeFlavio, Rolin, Nordstorm, & Kazal Jr, 2015; Kermack, Flannery, Tofighi, McNeely, & Lee, 2017; Walley et al., 2008).
The current study sought to update and expand upon previous research by surveying physicians who do and do not have the buprenorphine prescription waiver to evaluate (a) reasons that physicians don’t receive the waiver, (b) reasons that waivered physicians don’t prescribe to capacity, and (c) what resources might encourage; more physicians to seek the buprenorphine waiver and/or increase their patient load. The goal of this study is to provide insight to the medical community and inform public policy regarding approaches that might increase adoption and prescribing of buprenorphine for OMT.
2. Methods
2.1 Participants
This study was classified as exempt from human research by the Johns Hopkins Institutional Review Board. To be eligible, respondents had to report being a physician currently practicing in the United States and fluent in English. The survey (described below) was delivered to participants from 4/2016 – 5/2016, through listserv postings to the American Medical Association (AMA) and American Society of Addiction Medicine (ASAM). Survey emails were delivered to a total 20,841 email accounts. Which resulted in 604 survey clicks. A total 588 participants (97.4% of those opening the survey) completed the survey. Thirty participants were removed based on responding “yes” to one of two quality control .questions (e.g., “Have you completed this survey before” and “Is there any reason for which we should not use your responses, for instance you were not paying attention, did not answer honestly, or had major computer issues”). The final participant sample size was 558 (92.4% of those: opening the survey).
2.2 Study Measures
Participants received an email with the following instructions “This survey aims to learn about your references for prescribing buprenorphine/naloxone (Suboxone) for the treatment of opioid use disorder, and what barriers you think may exist for prescribing this medication in the United States. We are seeking physicians who DO and DO NOT currently prescribe Suboxone for opioid use disorder. All answers are confidential and anonymous. The survey should not take more than 2 minutes to complete. Please, only complete this survey if you are licensed as a physician in the US.”
Participants then completed a 15-item anonymous self-report survey that was hosted through the online manager Qualtrics (Provo, UT). Since the survey was designed to be brief to encourage completion, detailed demographic information was not collected. Respondents indicated the state in which they practiced, whether they were located in primarily urban, suburban, or rural settings, their primary specialty, and the setting of their practice (e.g., primary care, office based, etc.). Next, participants indicated whether they had completed the waiver necessary to prescribe buprenorphine for the treatment of OUD, the number of patients to which they currently prescribe buprenorphine, and the approximate number of requests for buprenorphine treatment and rejections they process each month. The number of requests and rejections were rated the same on the same ordinal scale, ranging from “0” to “more than 30”.
Waivered respondents were then asked whether they were prescribing to capacity (defined for them as 30 patients in the first year and 100 thereafter), and respondents who selected “No” were provided with a list of potential reasons for not prescribing to capacity. Respondents who were not waivered or were not prescribing to capacity were then presented with a list of potential resources and asked to indicate whether any of the following would increase their willingness to become waivered or prescribe to capacity (1) being paired with an experienced prescriber who can help answer questions/provide guidance on prescribing, (2) being provided with information about counseling resources for patients in their local area, (3) receiving financial assistance to cover the cost of the waiver, (4) having access to more continuing medical education courses on OUD and OUD treatment. Respondents were also allowed to indicate that nothing would increase their willingness to become waivered/prescribe to capacity, and those who selected more than 1 option were next asked to indicate the resource that would MOST increase their willingness to increase prescribing. Finally participants were provided with open-entry boxes to write in any additional information regarding their prescribing practices.
2.4 Data Analysis
The goal of this study was to descriptively characterize reasons that physicians may not be waivered to prescribe buprenorphine, as well as reasons for not prescribing to capacity among waivered physicians. Respondents were separated into the following three groups for comparison: non-waivered, waivered not at capacity, and waivered at capacity. Results were characterized using descriptive statistical and compared across non-waivered and waivered respondents using independent groups t-tests for continuous and chi-squares for dichotomous variables. Data regarding number of patient requests and rejections processed each month were collected on an ordinal scale, therefore a Kruskal-Wallis H test was used to evaluate differences as a function of respondent group and Bonferroni-adjusted pairwise comparisons were used to identify significant group differences. Ordinal regression was then used to identify attitudes associated with rejection of new patient inquires within the waivered respondents. Finally, logistic regression was used to identify whether any of the attitudes listed in the survey were associated with unwillingness to prescribe buprenorphine (yes/no) within both non-waivered and waivered respondents. Alpha levels were set at p<.05 and analyses were conducted using SPSS version 24.0.
3. Results
3.1 Respondents
Respondents were from urban (41.5%), suburban (40.0%), and rural(18.3%) settings (Table, 1). A total of 484 respondents (86.7%) reported having received the waiver. Among those with a waiver, only 43.8% reported prescribing to capacity. Waivered respondents not at capacity reported a mean/median(SD) of 30.6/20.0 (30.6) current buprenorphine patients, while waivered respondents at capacity reported 76.8/97.0 (34.5) current patients (t(478) = −15.52, p<.001; Table 1). Of-the waivered respondents at capacity, 40 (18.7%) reported prescribing to 30 or fewer patients, suggesting that they are either first year prescribers or have not requested additional prescribing privileges from SAMHSA. A Kruskal-Wallis H test revealed a significant differences in the number of patient requests (H(2) = 184.76, p<.001) and patient rejections (H(2) = 106.35, p<.001) between the non-waivered, waivered not at capacity, and waivered at capacity groups. The median number of patients, distribution of responses, and specific groups differences are reported in Figure 1.
Table 1.
Practice characteristics of respondents.
| Total respondents (N = 558) |
Nonwaivered respondents (N = 74) |
Total waivered respondents (N = 484) |
Waivered and not prescribing to capacity (N = 272) |
Waivered and prescribing to capacity (N = 212) |
Total waivered versus nonwaivered (χ2(df), p-value) |
|
|---|---|---|---|---|---|---|
| Patient load | ||||||
| Number of patients (mean, SD) | 44.1 (40.7) | N/A | 50.7 (39.6) | 30.6 (30.6) | 76.8(34.5) | |
| Prescribing to capacity (%) | 39.6 | N/A | 43.8 | 0.0 | 100.0 | |
| Location of practice (%) | ||||||
| Midwest | 19.5 | 27.0 | 18.4 | 17.3 | 19.8 | 4.07(4), 0.40 |
| Northeast | 24.7 | 18.9 | 25.6 | 26.8 | 24.1 | |
| South | 36.7 | 33.8 | 37.2 | 34.2 | 41.0 | |
| West | 18.8 | 20.3 | 18.6 | 21.7 | 14.6 | |
| Speciality (%) | ||||||
| Addiction medicine | 33.5 | 2.7 | 40.5 | 33.5 | 46.9 | 42.49(5), <0.001 |
| Psychiatry | 26.0 | 44.6 | 23.1 | 32.4 | 11.3 | |
| Family medicine | 17.7 | 23.0 | 16.9 | 17.6 | 16.0 | |
| Internal | 9.3 | 12.2 | 8.9 | 8.1 | 9.9 | |
| Other | 10.9 | 16.2 | 10.1 | 8.1 | 12.7 | |
| Practice setting (%) | ||||||
| Urban | 41.8 | 45.9 | 41.1 | 46.0 | 34.9 | 1.43(3), 0.49 |
| Suburban | 40.0 | 40.5 | 39.9 | 37.1 | 43.4 | |
| Rural | 18.3 | 13.5 | 19.0 | 16.9 | 21.7 | |
Outcomes based upon chi-square comparisons. SD = standard deviation.
Figure 1.
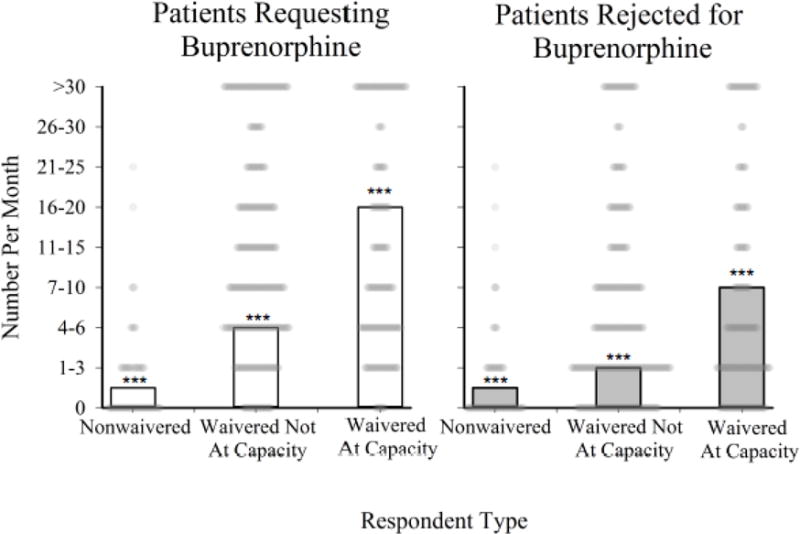
Bar chart representing median number of patients requesting buprenorphine per month (left panel; open bars) and median number of physician requests that are rejected per month (right panel; gray bars). The distribution of reported requests and rejections is overlaid on the bar chart, with each point corresponding to an individual physician respondent. X-axis represents respondent category (non-waivered, waivered not at capacity, waivered at capacity), and the Yaxis represents approximate number of patients as rated on an ordinal scale. Bonferroni-adjusted pairwise comparisons were used to examine differences between the three respondent categories; *** = p<.001 between a respondent category compared to each of the other two categories.
Overall the top cited reasons for not receiving the waiver or prescribing to capacity, collapsed across groups, were not having time for additional patients (19.2% of respondents) and not knowing how to get the waiver (14.0%) (Table 2). Regarding interest in resources, respondents (collapsed across groups) reported interest in receiving information about local counseling resources (12.5% of respondents), being paired with an experienced provider (10.8%), having access to more CME courses for OUD (9.0%), and receiving financial assistance for the waiver (4.7%) (Table 3). The resources rated the most important, collapsed across groups, were information about local counseling resources (40.4%) and being paired with an experienced provider (34.9%). Importantly, 31.2% of all respondents indicated that nothing would increase their willingness to become waivered or prescribe to capacity.
Table 2.
Reasons for not being waivered or not prescribing to capacity.
| Nonwaivered respondents (N = 74) |
Waivered and not prescribing to capacity (N= 272) |
(χ2, p-value) | |
|---|---|---|---|
| No time for more patients (%) | 12.2 | 36.0 | 15.51, <0.001 |
| Reimbursement insufficient (%) | 5.4 | 15.4 | 5.08, =0.02 |
| Concerned about diversion (%) | 25.7 | 10.3 | 11.73, =0.002 |
| Don’t want to be inundated with suboxone requests (%) | 29.7 | 8.8 | 22.06, <0.001 |
| Don’t believe in agonist treatment (%) | 13.5 | 2.9 | 13.16, =0.001 |
| Concerned about precipitating withdrawal (%) | 12.2 | 1.5 | 18.40, <0.001 |
| Not educated enough about Opioid Use Disorder (%) | 14.6 | 1.1 | 28.38, <0.001 |
| Don’t know how to get waiver (%) | 9.5 | <1 | 21.29. <0.001 |
| No problem in my community (%) | 2.7 | <1 | 3.70, =0.12 |
Respondents who were waivered and prescribing to capacity did not answer these questions.
Degrees of freedom = 1 for all comparisons.
Table 3.
What resources will increase receipt of waiver or prescribing to capacity.
| Nonwaivered respondents (N= 74) |
Waivered and not prescribing to capacity (N= 272) |
(χ2, p-value) | |
|---|---|---|---|
| Programs that will increase prescribing (%) | |||
| Nothing will increase my willingness | 33.8 | 54.8 | 10.26. =0.001 |
| Information about local counseling resources | 27.0 | 18.4 | 2.96, =0.10 |
| Being paired with experienced provider | 35.1 | 12.5 | 20.79, <0.001 |
| More CME courses for opioid use disorder | 33.8 | 9.2 | 28.46, <0.001 |
| Financial assistance for waiver | 24.3 | 2.9 | 38.27, <0.001 |
| Program that will most increase prescribing (%)a | |||
| Information about local counseling resources | 11.4 | 54.1 | 20.74 (df = 4), <0.001 |
| Being paired with experienced provider | 45.7 | 29.7 | |
| More CME courses for opioid use disorder | 28.6 | 9.5 | |
| Financial assistance for waiver | 14.3 | 5.4 | |
Waivered respondents who were prescribing to capacity did not answer these questions.
CME = continuing medical education. Degrees of freedom (df) = 1 unless otherwise stated.
Percent of respondents initially endorsing that > 1 program would increase prescribing.
Ordinal regression analysis was used to identify reasons for rejecting new inquiries for buprenorphine OMT, controlling for number of patients and whether respondents were already at capacity. Results indicated that insufficient reimbursement rates (OR 2.47, 95% CI, 1.33 to 4.57, Wald 2(1) = 8.33, p<0.01), not having time for additional patients (OR 2.36, 95% CI, 1.47 to 3.75, Wald 2(1) = 12.67, p<(0.001), and concern about withdrawal/lack of information about induction (OR 6.92, 95% CI, 1.17 to 40.43, Wald 2(1) = 4.62, p=0.03) were associated with greater odds of rejecting patients.
3.1.1 Non-waivered vs. Waivered Respondents
A total of 74 respondents (13.3%) indicated they were not currently waivered to prescribe buprenorphine. Overall, the top cited reasons for not being waivered included not wanting to be inundated with requests for buprenorphine (29.7%) and concerns about diversion (25.7%) (Table 2). Regarding interest in resources, being paired with an experienced provider (35.1%), more CME courses for OUD (33.8%), and information about local counseling services (27%) were rated as the three highest priorities (Table 3).
A total of 33.8% of non-waivered respondents indicated that nothing would increase their willingness to prescribe buprenorphine. A binary logistic regression analysis of non-waivered respondents who indicated no willingness to increase prescribing was significant (2(1) = 5.86, p =0.02). And indicated that this decision was driven by not wanting to be inundated with requests for buprenorphine (OR 3.60, 95% CI, 1.26 to 10.27, p=0.02).
3.1.2 Waivered Respondents Prescribing to Capacity vs. Not Prescribing to Capacity
A total 56.2% (n=272) of waivered respondents indicated they were not currently prescribing to capacity. The single, most cited reason for not prescribing to capacity among waivered respondents was not having time for more patients (36.0%) (Table 2). Regarding interest in resources, information about counseling services (18.4%), being paired with an experienced physician (12.5%), and more CME courses for OUD (9.2%) were rated as the three highest priorities for waivered respondents not prescribing to capacity (Table 3). The resource that was identified as the most likely to increase their willingness to prescribe to capacity was receiving more information about local counseling resources (54.1%).
Importantly, 54.8% of waivered respondents who were not prescribing to capacity indicated that nothing would increase their willingness to prescribe at that level. A binary logistic regression analysis of waivered respondents not at capacity was significant (2(3) = 71.06, p<.001), and indicated that the decision to not prescribe to capacity was driven by lack of belief in agonist treatment (OR 5.02, 95% CI, 1.12 to 22.50, p=0.04), lack of time for additional patients (OR 6.44, 95% CI, 3.97 to 10.45, p<.001), and beliefs that reimbursement rates were insufficient (OR 2.98, 95% CI, 1.51 to 5.88, p<0.01).
4. Discussion
This study surveyed physicians through email postings to the list servs of two major medical organizations (AMA and ASAM) to assess reasons that physicians may not have applied for a waiver to prescribe buprenorphine, and why those who are waivered may not be prescribing to capacity. Understanding physician attitudes towards prescribing buprenorphine is an essential step towards increasing OMT availability in response to the ongoing opioid epidemic (DeFlavio et al., 2015; Molfenier et al. 2015). The findings of this research provide insight into these issues and suggest actionable approaches that could potentially increase adoption of buprenorphine for OMT.
Data from this study indicate that physicians who have not applied for the buprenorphine prescription waiver expressed negative attitudes toward buprenorphine treatment, including concerns about diversion and managing numerous patient requests for OMT. On the other hand, physicians who had received the waiver but were not prescribing to capacity expressed concern with practical barriers with buprenorphine treatment, such as appropriate reimbursement for services and actual time capacity. Overall, survey respondents indicated the resources most likely to increase their willingness to either become waivered or prescribe to capacity were receiving information about local counseling resources, being paired with an experienced provider, and receiving more CME courses on OUD. These results are consistent with previous studies which reported that physicians without access to institutional support or training are likely to see these factors as barriers to prescribing buprenorphine (Hutchinson. Catlin, Andrilla, Baldwin. & Rosenblatt, 2014; Walley et al., 2008).
Buprenorphine is largely underutilized as a treatment option for OUD. A recent study found that waivered physicians in Vermont were only prescribing buprenorphine to an average 14.8 patients per buprenorphine provider (Sigmon. 2015). Although the current study differs in methodology, Table 1 shows that waivered physicians who aren’t prescribing to capacity maintain an average of 30.6 patents; however these same physicians reject approximately half of new patent requests each month (Figure 1). In addition, rejection of new patient inquires among waivered physicians not prescribing, to capacity was associated with lack of time for additional patents, concern about precipitating withdrawal/lack of information about induction, and the belief that reimbursement rates were insufficient. Waivered physicians at capacity also reject about half of patient requests, yet have the highest rates of both new patient requests and rejections (Figure 1). Similar research has found that patients are often turned away because physicians are at capacity (Molfenier, Sherbeck, Zehner, & Starr, 2015). Exploring new paradigms in managing caseloads and expanding the number of patients seen by waivered physicians will likely have an impact on reducing the number of patients rejected for buprenorphine treatment.
The resources that were presented to respondents (e.g., being paired with an experienced provider, information about local counseling resources, financial assistance for the waiver, more CME courses on opioid use disorder) are all programs for which there are existing models that have been implemented to some degree of success. For instance, many of the resources in which respondents reported interest can be addressed with the hub-and-spoke model that has been implemented to increase access to buprenorphine in Vermont. This model links primary care providers with larger OMT programs to provide support and guidance for patient management, and providers a nurse and case manager for primary care clinics (Simpatico, 2015). Together with alearning collaborative (Nordstorm et al., 2016), the: hub-and-spoke approach has shown demonstrable gains in engaging physicians and increasing buprenorphine adoption. A second approach is use of telemedicine or teleconsultation to link inexperienced providers with mentors to help navigate buprenorphine OMT procedures. These approaches are becoming more widely used in general medicine (Biery, Bond, Smith, LeClair, & Foster, 2015; Eaton et al., 2015; Gillis, 2015; Khan et al., 2015; Marcolino, Pereira Afonso Dos Santos, Santos Neves, & Alkmim, 2015), have been associated with reductions in medical errors or referrals to formal treatments (Campanella et al., 2015), and have particular value for remote or rural areas (Saurman, Lyle, Perkins, & Roberts, 2014) for which research has indicated there is a dearth of available opioid treatment options (Blum et al., 2016; Cunningham et al., 2007; Jones et al., 2015; Knudsen et al., 2005; Knudsen, 2015). The Physician Clinical Support System-Buprenorphine(PCSS-B) is a federally funded program that is already in place to pair newly waivered physicians with an experienced provider usually via telephone or email, but possibly with in-person meetings as well (Egan et al., 2010). However, the overall utilization of this program is not known, and data from the current study suggests that some physicians might not known about PCSS-B or might prefer mentor relationships that are strictly face-to-face. Canada has implemented the “Extension for Community Healthcare Outcomes (ECHO)” program to improve chronic pain treatment; this provides a strong model for telementoring programs that could be adapted to enable experienced buprenorphine OMT providers to guide more novice providers (Dubin et al., 2015).
Importantly, 54.8% of waivered physicians that were not prescribing to capacity and 33.8% of non-waivered physicians reported that nothing would increase their willingness to prescribe more buprenorphine. This is a crucial target for future interventions. A study by Thomas et al reported that non-waivered psychiatrists identified lack of time, organizational support, and lack of effectiveness of buprenorphine treatment as reasons not to prescribe (2008). Previous research has also reported that waivered physicians may not be motivated to prescribe buprenorphine due to practical reasons such as logistics, record-keeping, and patient limits (Kissin, McLeod, Sonnefeld, & Stanton, 2006). In the current study, waivered physicians not prescribing to capacity endorsed three attitudes that were significantly associated with a lack of willingness to prescribe buprenorphine lack of belief in agonist treatment, lack of time to see more patients, and reimbursement rates that were perceived as insufficient. While lack of belief in agonist treatment is philosophical .and related to treatment approach, only a small number of waivered physicians endorsed this belief (about 3%). The other two attitudes are related to business models in medicine and could be potentially remedied by increasing office support so that physicians can structure their practice in a way to support OUD patients. This may include team-based or collaborative models that utilize physician assistants and/or nurse practitioners. Future studies should examine ways to make the process of treating OUD patients more efficient, relieving some demand on physicians and increasing the number of patients that can be supported by an office-based medical practice.
This study is limited by the underrepresentation of non-waivered physicians and over representation addiction specialists who responded to the survey. This is partly driven by our method of obtaining the physician sample, although surveying physicians that are also ASAM members ensures that we are targeting an audience that is interested in treating OUD. Similarly, the use of a convenience sample and the brevity of the survey itself are also limitations. Both of these factors were deemed necessary to attract a large enough number of physicians for meaningful data analysis. The survey also did not ask whether physicians were not accepting new patients in general or just not accepting new OUD patients, which is an important distinction that should be made in future research on this topic. In addition, several themes emerged in the open-ended comments sections that were not queried in the entire group, such as the need for more office support or the financial burden of buprenorphine on patents; including these items in future surveys would be important to provide more insight into the variables that are driving provider prescribing practices.
5. Conclusions
The current study assessed physician attitudes associated with administering buprenorphine therapy to individuals with OUD and identified resources that might increase their willingness to prescribe buprenorphine to those patients. These data suggest that increasing the number of waivered physicians without making additional resources available to combat infrastructure concerns is unlikely to have large impact on buprenorphine prescribing. Treatment-seeking individuals with OUD are often hindered by treatment cost and waiting lists for buprenorphine-prescribing physicians (Bazazi, Yokell, Fu, Rich, & Zaller, 2011). Identifying attitudes and programs that are useful in increasing the diffusion of OMT therapy are crucial to address the opioid crisis.
Highlights.
Waivered/non-waivered physicians were surveyed re attitudes toward buprenorphine.
Waivered physicians reported that they did not have time for more patients (36%).
Many waivered physicians were not interested in prescribing to more patients (55%).
Non-waivered were concerned about too many requests for buprenorphine (30%).
Non-waivered were also concerned about diversion of buprenorphine (26%).
Acknowledgments
Funding: NIDA R21 DA035327 (Dunn)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No conflicts of interest to report.
References
- Bazazi AR, Yokell M, Fu JJ, Rich JD, Zaller ND. Illicit use of buprenorphine/naloxone among injecting and noninjecting opioid users. Journal of Addiction Medicine. 2011;5(3):175–180. doi: 10.1097/ADM.0b013e3182034e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biery N, Bond W, Smith AB, LeClair M, Foster E. Using telemedicine techonology to assess physician outpatient teaching. Family Medicine. 2015;47(10):807–810. [PubMed] [Google Scholar]
- Blum K, Gold M, Clark HW, Dushaj K, Badgaiyan RD. Should the United States Government repeal restrictions on buprenorphine/naloxone treatment? Substance Use & Misuse. 2016;51(12):1–6. doi: 10.1080/10826084.2016.1200097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campanella N, Morosini P, Sampaolo G, Catozzo V, Caso A, Ferretti M, et al. Medical teleconsultation to general practitioners reduces the medical error vulnerability of internal medicine patients. European Journal of Internal Medicine. 2015;26(9):675–679. doi: 10.1016/j.ejim.2015.08.010. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Vital signs: Overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR Morbidity and Mortality Weekly Report. 2011;60(43):1487–1492. [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical Prescription-opioid use and heroin use. New England Journal of Medicine. 2016;374(2):154–163. doi: 10.1056/NEJMra1508490. [DOI] [PubMed] [Google Scholar]
- Cunningham CO, Kunins HV, Roose RJ, Elam RT, Sohler NL. Barriers to obtaining waivers to prescribe buprenorphine for opioid addiction treatment among HIV physicians. Journal of General Internal Medicine. 2007;22(9):1325–1329. doi: 10.1007/s11606-007-0264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham CO, Sohler NL, McCoy K, Kunins HV. Attending physicians’ and residents’ attitudes and beliefs about prescribing buprenorphine. at an urban teaching hospital. Family Medicine-Kansas City. 2006;38(5):336. [PubMed] [Google Scholar]
- DeFlavio J, Rolin S, Nordstrom B, Kazal L., Jr Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural and Remote Health. 2015;75(3019) [PubMed] [Google Scholar]
- Drug Enforcement Agency. Schedules of controlled substances. 2016 Retrieved from: Https://WwwDeadiversion.UsdojGov/Pubs/Manuals/Sec/App_lawHtm.
- Dubin RE, Flannery J, Taenzer P, Smith A, Smith K, Fabico R, et al. ECHO ontario chronic pain & opioid stewardship: Providing access and building capacity for primary care providers in underserviced, rural, and remote communities. Studies in Health Technology and Informatics. 2015;209:15–22. [PubMed] [Google Scholar]
- Egan JE, Casadonie P, Garienmann T, Martin J, McCance-Katz EF, Netherland J, Fiellin DA. The Physician Clinical Support System-Buprenorphine(PCSS-B): A novel project to expand/improve buprenorphine treatment. Journal of General Internal Medicine. 2010;25(9):936–941. doi: 10.1007/s11606-010-1377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton JL, Mohr DC, Mohammad A, Kirkhorn S, Gerstel-Santucci C, Mcphaul K, et al. Implementation of a novel. occupational and environmental medicine specialty teleconsultation service: The VHA experience. Journal of Occupational and Environmental Medicine. 2015;57(2):173–177. doi: 10.1097/JOM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- Fudala PJ, Bridge TP, Herbert S, Williford WO, Chiang CN, Jones K, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. New England Journal of Medicine. 2003;349(10):949–958. doi: 10.1056/NEJMoa022164. [DOI] [PubMed] [Google Scholar]
- Gerra G, Koutsenok I, Saenz E, Busse A. International standards in the treatment of drug use. United Nations Office on Drugs and Crime UNODC; Austria: 2015. [Google Scholar]
- Gillis G. Perspectives of champlain BASE specialist physicians: Their motivation, experiences and recommendations for providing eConsultations to primary care providers. Global Telehealth 2015: Integrating Technology and Information for Better Healthcare. 2015;209:38. [PubMed] [Google Scholar]
- Graham NA, Merlo LJ, Goldberger BA, Gold MS. Methadone-and heroin-related deaths in Florida. The American Journal of Drug and Alcohol Abuse. 2008;34(3):347–353. doi: 10.1080/00952990802010892. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Chen LH, Warner M. Drug-poisoning deaths involving heroin: United states, 2000–2013. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.; 2015. [Google Scholar]
- Hutchinson E, Catlin M, Andrilla CH, Baldwin LM, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Annals of Family Medicine. 2014;12(2):128–133. doi: 10.1370/afm.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasinski DR, Pevnick JS, Griffith JD. Human pharmacology and abuse potential of the analgesic buprenorphine: A potential agent for treating narcotic addiction. Archives of General Psychiatry. 1978;35(4):501–516. doi: 10.1001/archpsyc.1978.01770280111012. [DOI] [PubMed] [Google Scholar]
- Johnson RE, Strain EC, Amass L. Buprenorphine: How to use it right. Drug and Alcohol Dependence. 2003;70(2):S59–S77. doi: 10.1016/s0376-8716(03)00060-7. [DOI] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Journal Information. 2015;105(8) doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermack A, Flannery M, Tofighi B, McNeely J, Lee JD. Buprenorphine prescribing practice trends and attitudes among New York providers. Journal of Substance Abuse Treatment. 2017;74:1–6. doi: 10.1016/j.jsat.2016.10.005. [DOI] [PubMed] [Google Scholar]
- Khan NU, Rasheed S, Sharmin T, Ahmed T, Mahmood SS, Khatun F, et al. Experience of using mHealth to link village doctors with physicians: Lessons from Chakaria, Bangladesh. BMC Medical Informatics and Decision Making. 2015;75(1):62. doi: 10.1186/s12911-015-0188-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissin W, McLeod C, Sonnefeld J, Stanton A. Experiences of a national sample of qualified addiction specialists who have and have not prescribed buprenorphine for opioid dependence. Journal of Addictive Diseases. 2006;25(4):91–103. doi: 10.1300/J069v25n04_09. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Ducharme LJ, Roman PM, Link T. Buprenorphine diffusion: The attitudes of substance abuse treatment counselors. Journal of Substance Abuse Treatment. 2005;29(2):95–106. doi: 10.1016/j.jsat.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Lofwall MR, Havens JR, Walsh SL. States’ implementation of the affordable care act and the supply of physicians waivered to prescribe buprenorphine for opioid dependence. Drug and Alcohol Dependence. 2015;157:36–43. doi: 10.1016/j.drugalcdep.2015.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK. The supply of physicians waivered to prescribe buprenorphine for opioid use disorders in the united states: a state-level analysis. Journal of Studies on Alcohol and Drugs. 2015;76(4):644–654. doi: 10.15288/jsad.2015.76.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcolino MS, Pereira Afonso dos Santos J, Santos Neves D, Alkmim MB. Teleconsultation to provide support for primary care practitioners and improve quality of care–the experience of a large scale telehealth service in Brazil. Studies in Health Technology and Informatics. 2015;216:987. [PubMed] [Google Scholar]
- Molfenter T, Sherebeck C, Zehner M, Quanbeck A, McCarty D, Kim J, et al. Implementing buprenorphine in addiction treatment payer and provider perspectives in Ohio. Substance Abuse-Treatment, Prevention, and Policy. 2015;10(1):1. doi: 10.1186/s13011-015-0009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molfenter T, Sherbeck C, Zehner M, Starr S. Buprenorphine prescribing availability in a sample of Ohio specialty treatment organizations. Journal of Addictive Behaviors, Therapy & Rehabilitation. 2015;4(2) doi: 10.4172/2324-9005.1000140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SM, Fishman PA, McPherson S, Dyck DG, Roll JR. Determinants of buprenorphine treatment for opioid dependence. Journal of Substance Abuse Treatment. 2014;46(3):315–319. doi: 10.1016/j.jsat.2013.09.003. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistic’s. Health, United States, 2013 with special feature on prescription drugs. Hyatisville, MD: 2015. Retrieved from: https://www.cdc.gov/nchs/data/hus/husl3.pdf. [PubMed] [Google Scholar]
- Nordstorm BR, Saunders EC, McLeman B, Meier A, Xie H, Lambert-Harris C, et al. Using a learning collaborative strategy with office-based practices to increase access and improve quality of care for patients with opioid use disorder. Journal of Addiction Medicine. 2016;10(2):117–123. doi: 10.1097/ADM.0000000000000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbatt RA, Andrilla CH, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opiod use disorder. Annals of Family Medicine. 2015;13(1):23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurman E, Lyle D, Perkins D, Roberts R. Successful provision of emergency mental health care to rural land remote new south wales: an evaluation of the mental health emergency Care–Rural access program. Australian Health Review. 2014;38(1):58–64. doi: 10.1071/AH13050. [DOI] [PubMed] [Google Scholar]
- Schuckit MA. Treatment of opioid-use disorders. New England Journal of Medicine. 2016;375(4):357–368. doi: 10.1056/NEJMra1604339. [DOI] [PubMed] [Google Scholar]
- Selwyn PA, Hartel D, Lewis VA, Schoenbaum EE, Vermund SH, Klein RS, et al. A prospective study of the risk of tubercllosis among intravenous drug users with human immunodeficiency virus infection. New England Journal of Medicine. 1989;320(9):545–550. doi: 10.1056/NEJM198903023200901. [DOI] [PubMed] [Google Scholar]
- Sigmon SC. The untapped potential office-based buprenorphine. JAMA Psychiatry. 2015;72(4):395–396. doi: 10.1001/jamapsychiatry.2014.2421. [DOI] [PubMed] [Google Scholar]
- Simpatico TA. Vermont responds to its opioid crisis. Preventive Medicine. 2015;80:10–11. doi: 10.1016/j.ypmed.2015.04.002. [DOI] [PubMed] [Google Scholar]
- Stein BD, Pacula RL, Gordon AJ, Burns RM, Leslie DL, Sorbero MJ, et al. Where is buprenorprine dispensed to treat opioid use disorders? The role of private offices, opioid treatment programs, and substance abuse treatment in facilities in urban and rural counties. Milbank Quarterly. 2015;93(3):561–583. doi: 10.1111/1468-0009.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) (SMA) PEP 15-FEDGUIDEOTP. Rockville, MD: 2015a. Federal guidelines for opioid treatment programs HHS publication. Retrieved From: Store.Samhsa.Gov/Shin/ConteNt//PEP15–FEDGUIDEOTP/PEP15-FEDGUIDEOTP.Pdf. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) HHS publication no.(SMA) 13–4795. Rockville, MD: 2015b. Result from the 2014 national survey on drug and health: Summary of national findings (no. NSDUH series H-46) Retrieved from: https://www.samhsa.gov/data/sites/defaults/NSDUH-FRR1-2014/NSDUH-FRR1-2014.pdf. [Google Scholar]
- Thomas CP, Reif S, Haq S, Wallack SS, Hoyt A, Ritter GA. Use of buprenorphine for addiction treatment: Perspectives of addiction specialists and general psychiatrists. Psychiatric Services. 2008;59(8):909–916. doi: 10.1176/ps.2008.59.8.909. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Lin Y, Lynch K. Barriers and facilitators primary care or human immunodeficiency virus clinics providing methadone or buprenorphine for the management of opioid dependence. Archives of Internal Medicine. 2005;165(15):1769–1776. doi: 10.1001/archinte.165.15.1769. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies—tackling the opioid-overdose epidemic. New England Journal of Medicine. 2014;370(22):2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Walley AY, Alperen JK, Cheng DM, Bottichii M, Castro-Donan C, Samet JH, et al. Office-based management of opioid dependence with buprenorphine: Clinical practices and barriers. Journal of General Internai Medicine. 2008;23(9):1393–1398. doi: 10.1007/s11606-008-0686-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstock AR, Lea T. Diversion and injection of methadone and buprenorphine among clients in public optoid treatment clinicians in New Souih Wales, Australia. Substance use & Misuse. 2010;45(1–2):240–252. doi: 10.3109/10826080903080664. [DOI] [PubMed] [Google Scholar]


