Abstract
Background and Objective
Effective communication with primary care physicians is important yet incompletely understood for Spanish-speaking parents. We predicted lower satisfaction among Spanish-speaking compared with English-speaking Latino and non-Latino parents.
Methods
Cross-sectional analysis at 2-month well visits within the Greenlight study at 4 pediatric resident clinics. Parents reported satisfaction with 14 physician communication items using the validated Communication Assessment Tool (CAT). High satisfaction was defined as “excellent” on each CAT item. Mean estimations compared satisfaction for communication items among Spanish and English-speaking Latinos and non-Latinos. We used generalized linear regression modeling, adjusted for parent age, education, income, and clinic site. Among Spanish-speaking parents, we compared visits conducted in Spanish with and without an interpreter, and in English.
Results
Compared with English-speaking Latino (N=127) and non-Latino parents (N=432), fewer Spanish-speaking parents (N=303) reported satisfaction with 14 communication items. No significant differences were found between English-speaking Latinos and non-Latinos. Greatest differences were found in: greeting that made the parent comfortable (59.4% of Spanish-speaking Latinos endorsing “Excellent” vs. 77.5% English-speaking Latinos, p<0.01) and discussing follow-up (62.5% of Spanish-speaking Latinos vs. 79.8% English-speaking Latinos, p<0.01). After adjusting for parent age, education, income, and study site, Spanish-speaking Latinos were still less likely to report high satisfaction with these communication items. Satisfaction was not different among Spanish-speaking parents when the physician spoke Spanish versus used an interpreter.
Conclusions
Satisfaction with physician communication was associated with language, but not ethnicity. Spanish-speaking parents less frequently report satisfaction with communication, and innovative solutions to enhance communication quality are needed.
Keywords: Spanish-speaking, parent satisfaction, physician communication
Introduction
In primary care, Latino children constitute a growing demographic group and comprise 24.4% of the U.S. child population. 1 High quality primary care is especially important for Latino children because one-third live in poverty, 1 and Latino families experience barriers to health care2,3 and disparities in health outcomes. 4,5 To deliver high-quality pediatric primary care to diverse populations, effective communication between children’s parents and the medical team is essential, as outlined in the Department of Health and Human Services National Standards for Culturally and Linguistically Appropriate Services (CLAS) 6 and emphasized in Healthy People 2020 objectives on physician communication skills. 7 For Spanish-speaking patients, language barriers may lead to decreased understanding of instructions, 3,8 less family-centered care, 4 and less frequent resolution of medical problems compared with patients who speak English. 9
Detailed investigation of Latino and Spanish-speaking parents’ satisfaction with physician communication has rarely been conducted in pediatric primary care settings. Yet effective physician communication with parents has multiple beneficial effects, including greater parent satisfaction and improved health outcomes.10 Qualitative studies have demonstrated room for improvement in satisfaction with communication; Spanish-speaking mothers have described lack of language services and effective communication as factors influencing their experience of care11 and many expressed frustration.12 Ratings of communication with healthcare providers were low among Spanish-speaking parents in one large state study, 13 and a national study found similar dissatisfaction amongst non-English speaking parents, although specific languages were not examined, nor was the impact of use of interpreters.14
We sought to understand satisfaction with communication with physicians among Spanish and English-speaking parents whose children receive primary care at four university-affiliated clinics in different states. We examined satisfaction with communication at the 2-month well visit, which was selected because of the high attendance rate and likelihood that it would occur with the child’s regular physician; additionally, the larger study involved data collection at 2 months. We hypothesized that the percent of parents who perceived physician communication as excellent would be highest among English-speaking non-Latino parents compared with Spanish-speaking and English-speaking Latino parents. Further, we hypothesized that among Spanish-speaking parents, satisfaction with communication would be highest when language-concordant care was provided by a physician conducting the visit in Spanish, compared with when an interpreter was used.
Methods
We conducted a cross-sectional analysis examining parent perception of physician communication. The sample consists of parents who attended academic medical center clinics (New York, Tennessee, North Carolina, and Florida) and were recruited for the Greenlight study. The parent study, which randomized sites to obesity prevention or active placebo (injury prevention counseling), has been described in detail previously. 15 At 2-month well visits, which were enrollment visits for the trial, baseline measures used in this analysis were collected. Visits were conducted by resident physicians in pediatrics. The study received Institutional Board Review (IRB) approval at all four institutions.
Dependent Variables
Of 1805 parent-child dyads assessed for eligibility for the Greenlight study, 632 were excluded due to parent age under 18, language other than Spanish or English, or plans to relocate; 308 parents declined participation. All parent-child dyads with a 2-month well visit (N=862) were included in the current analysis. Dependent variables were measured by the Communication Assessment Tool (CAT), 16 which was administered in the parent’s preferred language by a bilingual research assistant after the 2-month well visit. The CAT was translated into Spanish, then back-translated into English. The CAT described parent satisfaction with 14 physician communication items and 1 staff communication item. For each CAT item, distributions and descriptive statistics were examined. Satisfaction was defined as “excellent,” versus all other responses (“very good,” “good,” “fair,” and “poor”). This cut point for dichotomization was chosen as recommended16 and used in similar studies. 17,18 Additionally, after examining distributions in this sample and observing skewing toward positive responses, it was necessary to combine all other responses to allow a large enough sample for comparison with “excellent.”
Independent Variables
Parents self-reported their ethnicity and language. Latino parents were those who identified as Hispanic/Latino (N=430). Spanish-speaking (N=303) was defined as answering “Only Spanish” or “More Spanish than English” in response to the question, “In general, what language(s) do you read and speak?” English-speaking (N=127) was defined by responding “both equally,” “more English than Spanish,” or “English only” in response to this question. This cut point for defining Spanish-speaking was chosen in order to identify parents with greater proficiency in Spanish compared with English, similar to previous studies using self-reported proficiency measures.19,20
Additional independent variables were language of visit and interpreter use. Language of visit (English, Spanish, or both) was determined from a separate post-visit, physician-completed questionnaire that was available for only 689 parents due to lack of questionnaire completion by physicians. Interpreter use was reported by resident physicians on the same questionnaire. We used data as reported by physicians at the 4-month visit for 74 patients who were missing this report at 2 months, assuming relative stability in preferred language, and to maximize the sample size. No other 4 month data is included here. All clinic sites had in-person interpreters, and all sites used a language proficiency evaluation process for resident physicians.
Covariates
Additional measures which were examined as potential covariates included the following: nativity (birth in versus outside U.S.), country of origin, mother’s age (categorized as 18–20, 21–25, 26–30, 31–35, ≥ 36 years), whether enrolled child was firstborn (yes/no), receipt of WIC benefits (for mother, infant, or both), parent education (less than high school, high school graduate, some college, college degree), annual household income (<$10,000, $10,000–$19,000, $20,000–$39,000, $40,000–$59,000, ≥ $60,000), parent employment status (not working and not looking for work, working part time, working full time, looking for work), partner working (yes, no, not known), health literacy as measured by STOFHLA (Short Test of Functional Health Literacy in Adults; inadequate, marginal, or adequate).
Analysis
Demographic characteristics were compared using chi-square tests. Mean estimations compared the percent of parents highly satisfied with each item of communication on the CAT among Spanish-speaking Latinos (N=303), English-speaking Latinos (N=127), and English-speaking non-Latinos (N=432). To identify which of the 15 individual aspects of communication on the CAT were associated with high satisfaction, separate generalized linear models were created for each CAT item and compared satisfaction among Spanish and English-speaking Latino parents and non-Latino parents. Models adjusted for the following covariates based on literature supporting their possible relationship to satisfaction with communication 13,14,20–23 and/or hypothesized relationship to satisfaction: primary parent age, household income, WIC participation, parent employment, partner employment, nativity (born in/outside of U.S.), country of origin (Mexico/other), literacy (STOHFLA), education, enrolled child was firstborn, and clinic site. Generalized linear models were selected to facilitate calculation of ratios that are simpler to interpret than odds ratios and require fewer strict statistical assumptions. A three-category independent variable for language and ethnicity (Spanish-speaking Latino, English-speaking Latino, and English-speaking non-Latino) was included in each model. In the final models, we removed WIC participation, parent employment, partner employment, health literacy and firstborn child as these covariates did not change point estimates when entered or removed from model. We also removed nativity and specific country of origin, as these were highly correlated with speaking predominantly Spanish. Regression models included participants with complete data for variables of interest and covariates.
To examine the relationship of interpreter use on satisfaction, we used mean estimations to compare parents whose visits were conducted in Spanish with an interpreter with parents whose visits were conducted without an interpreter or were conducted in English. Separate generalized linear models for each of the fourteen CAT physician items were created, adjusting for the potential covariates described above.
Results
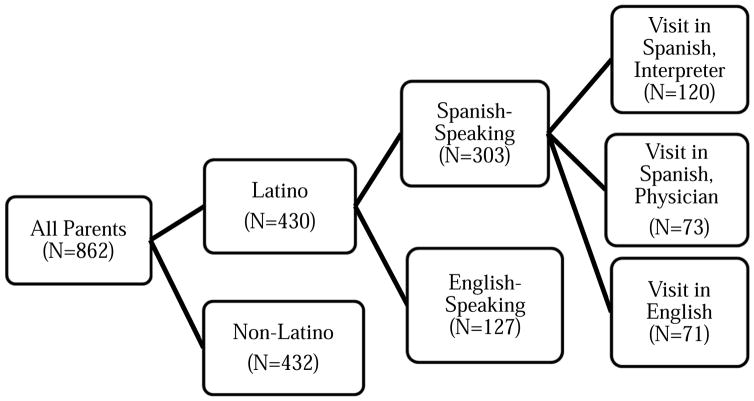
Of 862 parents, 430 identified as Latino; 303 of these were primarily Spanish-speaking (Figure 1). Parents were predominantly low-income, with a majority (81.5%) having annual household incomes <$40,000 and most (85.1%) receiving WIC benefits (Table 1). Multiple statistically significant differences were identified among Spanish-speaking Latinos compared with English-speaking Latinos and non-Latinos, including lower income, education, firstborn child, and health literacy. Spanish-speaking Latinos were much less likely than English-speaking Latinos to have been born in the U.S. (2% versus 53.2%), and more likely to be unemployed (73.9% versus 47.6%) but have an employed partner (80.7%) when compared with English-speaking Latinos (73.6%). Of 430 parents who identified as Latino, 55% (n=236) were born in Mexico and the remainder were born in multiple countries within Central and South America. Clinic sites differed greatly in the percent of parents of Mexican origin, ranging from 6.3% to 64.4%.
Figure 1.
Parent Satisfaction With Physician Communication Analysis Flow Diagram*†
*Spanish speaking was defined as answering “Only Spanish” or “More Spanish than English” in response to the question, “In general, what language(s) do you read and speak?” †N=39 missing values for language of visit and interpreter use due to insufficient information for imputation
Table 1.
Demographic Characteristics Of Parents By Language And Ethnicity (N=862)
| Spanish-Speaking Latino | English-Speaking Latino | English-Speaking Non-Latino | |
|---|---|---|---|
| N=303 (35.2%) | N=127 (14.7%) | N=432 (50.1%) | |
| Parent age, years* | |||
| 18–20 | 15 (5.0%) | 20 (16.0%) | 73 (16.9%) |
| 21–25 | 83 (27.7%) | 45 (36.0%) | 144 (33.4%) |
| 26–30 | 97 (32.3%) | 32 (25.6%) | 106 (24.6%) |
| 30–35 | 68 (22.7%) | 17(13.6%) | 72 (16.7%) |
| >35 | 37 (12.3%) | 11 (8.8%) | 36 (8.4% |
| WIC benefits*† | |||
| Self | 28 (9.3%) | 5 (4.0%) | 31 (7.2%) |
| Child | 42 (13.9%) | 17(13.5%) | 55 (12.9%) |
| Both | 216 (71.3%) | 81 (64.3%) | 254 (59.4%) |
| None | 17 (5.6%) | 23(18.3%) | 88 (20.6%) |
| Parent born in US* | 6 (2.0%) | 67 (53.2%) | 347 (80.9%) |
| Parent education* | |||
| Less than high school degree | 152 (50.2%) | 24 (19.1%) | 49 (11.5%) |
| High school degree | 92 (30.4%) | 37 (29.4%) | 150 (35.1%) |
| Some college | 34 (11.2%) | 34 (27.0%) | 132 (30.8%) |
| College degree | 25 (8.3%) | 31 (24.6%) | 97 (22.7%) |
| Annual household income* | |||
| <$10,000 | 123 (41.7%) | 26 (20.8%) | 115 (27.1%) |
| $10,000–19,999 | 102 (33.8%) | 31 (24.8%) | 95 (22.4%) |
| $20,000–39,999 | 53 (17.6%) | 36 (28.8%) | 113 (26.6%) |
| $40,000-–9,999 | 9 (3.0%) | 17 (13.6%) | 44 (10.4%) |
| ≥$60,000 | 5 (1.7%) | 13 (10.4%) | 44 (10.4%) |
| Parent employment* | |||
| Not working or looking | 224 (73.9%) | 60 (47.6%) | 184 (43.0%) |
| Working part time | 25 (8.3%) | 17 (13.5%) | 47 (111.0%) |
| Working full time | 27 (8.9%) | 33 (26.2%) | 128 (29.9%) |
| Looking for work | 27 (8.9%) | 16 (12.7%) | 69 (16.1%) |
| Parent’s partner employed* | 243 (80.7%) | 92 (73.6%) | 284 (66.4%) |
| Parent health literacy (STOFHLA)* ‡ | |||
| Inadequate | 44 (14.6%) | 5 (4.0%) | 18(4.2%) |
| Marginal | 12 (4.0%) | 1 (1.0%) | 14 (3.3%) |
| Adequate | 245 (81.4%) | 119 (95.2%) | 396 (92.5%) |
| Firstborn child* | 96 (31.7%) | 53 (42.1%) | 193 (45.0%) |
| Site* | |||
| Vanderbilt | 53 (17.5%) | 25 (19.7%) | 152 (35.2%) |
| New York University | 130 (42.9%) | 50 (39.4%) | 49 (11.3%) |
| University of North Carolina | 77 (25.4%) | 20 (15.8%) | 158 (36.6%) |
| Miami | 43 (14.2%) | 32 (25.2%) | 73 (16.9%) |
Indicates p-value <0.01 for difference between Spanish-speaking Latino, English-speaking Latino, and English-speaking non-Latino parents
WIC: Special Supplemental Nutrition Program for Women, Infants, and Children
STOFHLA: Short Test of Functional Health Literacy in Adults
Compared with English-speaking Latino (N=127) and non-Latino parents (N=432), fewer Spanish-speaking parents (N=303) reported high satisfaction with all 15 communication items (Table 2). No significant differences in satisfaction were found between English-speaking Latinos and non-Latinos. Spanish-speaking Latino parents were less likely than English-speaking Latino parents to report that the provider used a greeting that made the parent comfortable (59.4% vs. 77.5%, p<0.01) or discussed follow-up plans (62.5% vs. 79.8%, p<0.01). After adjusting for parent age, education, income, and clinic site, Spanish-speaking Latinos were still less likely than both English-speaking Latinos and non-Latinos to report high satisfaction with 6 of 14 physician communication items (Table 3). Likelihood of satisfaction with several aspects of communication was significantly higher for both English-speaking Latinos and non-Latinos compared with Spanish-speaking Latinos, including: the way the physician greeted them, treated them with respect, was interested in their ideas, gave as much information as they wanted, discussed next steps, and spent the right amount of time with them (Table 3).
Table 2.
Parent Satisfaction With Physician and Staff Communication By Language And Ethnicity (N=862)
| Spanish-Speaking Latino (N=303) | English-Speaking Latino (N=127) | English-Speaking Non-Latino (N=432) | |
|---|---|---|---|
| Physician Communication | |||
| Greeted me in a way that made me feel comfortable* | 59.4% | 77.5% | 79.0% |
| Treated me with respect* | 66.1% | 84.9% | 84.1% |
| Interested in my ideas about my health* | 63.5% | 81.5% | 81.1% |
| Understood my main health concerns* | 65.6% | 83.2% | 83.1% |
| Paid attention to me* | 69.9% | 84.9% | 85.1% |
| Let me talk without interruptions* | 68.9% | 84.0% | 84.1% |
| Gave me as much information as I wanted* | 68.5% | 82.4% | 85.6% |
| Talked in terms I could understand* | 68.2% | 79.8% | 83.6% |
| Checked to be sure I understood everything* | 66.7% | 78.2% | 79.7% |
| Encouraged me to ask questions* | 66.1% | 73.1% | 79.0% |
| Involved me in decisions as much as I wanted* | 64.0% | 78.2% | 79.7% |
| Discussed next steps, including any follow-up plans* | 62.5% | 79.8% | 83.4% |
| Showed care and concern* | 66.8% | 84.9% | 83.9% |
| Spent the right amount of time with me* | 62.8% | 79.0% | 80.7% |
| Staff Communication | |||
| The doctor’s staff treated me with respect* | 65.0% | 80.8% | 80.9% |
Indicates p-value <0.01 for difference between Spanish-speaking Latino, English-speaking Latino, and English-speaking non-Latino parents
Table 3.
Adjusted* Incidence Rate Ratios Of Parent Satisfaction With Physician and Staff Communication For Spanish-Speaking Latinos Compared With English-Speaking Latino And Non-Latino Parents
| Spanish-Speaking Latino (N=303) | English-Speaking Latino (N=127) | English-Speaking Non-Latino (N=432) | |
|---|---|---|---|
| Physician Communication | |||
| Greeted me in a way that made me feel comfortable† | Referent | 1.29 (1.13, 1.48) | 1.15 (1.02, 1.29) |
| Treated me with respect | Referent | 1.24 (1.11, 1.40) | 1.14 (1.03, 1.27) |
| Interested in my ideas about my health | Referent | 1.27 (1.11, 1.45) | 1.16 (1.04, 1.31) |
| Understood my main health concerns | Referent | 1.22 (1.08, 1.38) | 1.09 (0.98, 1.22) |
| Paid attention to me | Referent | 1.18 (1.06, 1.33) | 1.05 (0.95, 1.16) |
| Let me talk without interruptions | Referent | 1.19 (1.06, 1.33) | 1.06 (0.96, 1.16) |
| Gave me as much information as I wanted | Referent | 1.18 (1.05, 1.32) | 1.11 (1.01, 1.23) |
| Talked in terms I could understand | Referent | 1.11 (0.98, 1.26) | 1.05 (0.95, 1.17) |
| Checked to be sure I understood everything | Referent | 1.15 (1.01, 1.31) | 1.07 (0.96, 1.19) |
| Encouraged me to ask questions | Referent | 1.08 (0.94, 1.24) | 1.05 (0.94, 1.17) |
| Involved me in decisions as much as I wanted | Referent | 1.20 (1.05, 1.38) | 1.11 (0.99, 1.25) |
| Discussed next steps, including any follow- up plans | Referent | 1.20 (1.06, 1.37) | 1.14 (1.03, 1.28) |
| Showed care and concern | Referent | 1.24 (1.11, 1.40 | 1.10 (0.99, 1.22) |
| Spent the right amount of time with me | Referent | 1.24 (1.08, 1.42) | 1.13 (1.01, 1.27) |
| Staff Communication | |||
| The doctor’s staff treated me with respect | Referent | 1.22 (1.08, 1.38) | 1.09 (0.98, 1.21) |
Adjusted for: primary parent age, parent education, household income, site of enrollment.
Italics denote items for which Spanish-speaking Latinos are significantly less likely to have high satisfaction compared with both English-speaking Latinos and English-speaking non-Latinos
Satisfaction was not significantly different among Spanish-speaking parents whose physicians spoke Spanish, used an interpreter, or spoke English (Table 4). We repeated this analysis, adjusting for parent age, education, income, and clinic site, and results were similar (not shown).
Table 4.
Spanish-Speaking Parent Perception of Excellent Physician and Staff Communication By Language of Visit and Interpreter Use
| Visit in Spanish, Interpreter Used* (N=120) | Visit in Spanish, Provider Spoke Spanish* (N=73) | Visit in English (N=71)* | p-value† | |
|---|---|---|---|---|
| Physician Communication | % rating communication as excellent* | |||
| Greeted me in a way that made me feel comfortable | 62.6% | 58.5% | 60.6% | 0.58 |
| Treated me with respect | 71.3% | 64.2% | 66.7% | 0.33 |
| Interested in my ideas about my health | 65.2% | 63.7% | 66.7% | 0.84 |
| Understood my main health concerns | 66.9% | 67.1% | 66.2% | 0.97 |
| Paid attention to me | 73.9% | 71.4% | 65.2% | 0.72 |
| Let me talk without interruptions | 74.8% | 70.0% | 65.2% | 0.49 |
| Gave me as much information as I wanted | 71.3% | 74.3% | 65.2% | 0.66 |
| Talked in terms I could understand | 68.7% | 72.9% | 66.7% | 0.55 |
| Checked to be sure I understood everything | 69.3% | 67.1% | 68.2% | 0.76 |
| Encouraged me to ask questions | 70.4% | 67.1% | 65.2% | 0.64 |
| Involved me in decisions as much as I wanted | 67.0% | 67.1% | 63.6% | 0.98 |
| Discussed next steps, including any follow-up plans | 64.0% | 67.1% | 62.1% | 0.67 |
| Showed care and concern | 68.7% | 68.6% | 68.2% | 0.99 |
| Spent the right amount of time with me | 64.3% | 68.6% | 63.6% | 0.56 |
| Staff Communication | ||||
| The doctor’s staff treated me with respect | 66.0% | 68.5% | 66.0% | 0.73 |
Language of visit and interpreter use were reported by physician on post-visit questionnaire
p-value for difference between visit in Spanish with interpreter, in Spanish by physician, and in English
Discussion
This investigation in four pediatric primary care clinics demonstrated lowest satisfaction with physician communication among Spanish-speaking Latino parents, compared with English-speaking Latino and non-Latino parents. Comparing parents by both language and ethnicity allowed us to demonstrate that language, rather than ethnicity, was specifically associated with lower satisfaction. Spanish-speaking Latino parents experienced lower satisfaction with multiple aspects of visits, including having as much information as desired, being treated respectfully, and discussing next steps and follow-up.
Given the potentially powerful influence of language on communication with physicians, it is not surprising that Spanish-speaking parents reported lower satisfaction. This is consistent with findings in adults 24 and similar to reports of lower overall satisfaction among Latino parents of children with special health care needs. 23 While both linguistic and cultural barriers can affect the health care of Latino children, 3 the current study reinforces prior reports in identifying language, rather than ethnicity, as the key differentiator between families who experience low satisfaction with physician communication.
The sample included parents from four different states and different countries of origin. We considered, but were not able to identify, differences between Latino subgroups in perceptions of communication, similar to previous work in adults. 25 Lower satisfaction among Spanish-speaking Latinos persisted after we adjusted for clinic site, which was strongly associated with country of origin. The involved clinic sites are located in regions with different migration histories; two sites are major urban areas with long histories of Latino immigration, and two experienced more recent immigration waves with dramatic growth in Latino populations. 26 Even after adjusting for clinic site, which would take into account differences in national origin and different degrees of acculturation in these different Latino subgroups, Spanish-speaking Latinos still experienced lower satisfaction with physician communication.
We expected, but did not find, differences in Spanish-speaking parents’ satisfaction when using an interpreter, compared with when physicians conducted the visit themselves in Spanish. Professional interpreter services are important for quality of care, and better communication is generally achieved with a professional interpreter or a bilingual provider. 27,28 Language concordance between physician and patient could potentially be associated, as described in adults, with improved communication due to less frustration and confusion. 20 We did not observe such improved satisfaction with communication in these clinics when care was by language-concordant physicians. There may be multiple reasons for not detecting this difference. First, though physicians conducted the visit in Spanish, they may have varied in proficiency. Second, we do not have information about physician ethnicity, country of origin, and whether or not they were native Spanish speakers, and we are unable to determine whether or not there was cultural as well as linguistic concordance between parent and physician, which may also influence parent perceptions of communication. Finally, it is likely that factors other than language concordance were important in shaping parents’ perceptions about communication. For example, family centeredness, but not language concordance, has been associated with parent perception of higher quality care. 21 Finally, the questions on the CAT are not particularly sensitive to language concordance (e.g. greeting, showing respect, care and concern), and this may have limited our ability to detect differences between groups.
We also observed that visits were commonly reported to have been conducted in English for families who were primarily Spanish-speaking. Clinic sites in this study had access to professional interpreters, consistent with language access requirements to protect persons with limited English proficiency from discrimination under Title VI of the Civil Rights Act. 29 We do not have information about why visits were not conducted in Spanish through an interpreter. Several hypotheses may explain this observation. An English-speaking relative may have been present, which, alongside limited availability of language interpreters, may have allowed the provider to feel more comfortable conducting the visit in English. Alternatively, parents’ limited English may have been judged by either the parent or the physician as superior to the physician’s Spanish proficiency. Providing care in English for Spanish-speaking patients raises quality concerns, especially since subjective assessment of language proficiency had been shown to differ from objectively assessed proficiency. 30 The similarity in satisfaction ratings of Spanish-speaking parents whose visits were conducted with a Spanish-speaking provider, with an interpreter, or in English further highlights that language is likely not the only variable affecting responses on the CAT.
These analyses compared parents’ perceptions of communication as “excellent” with all perceptions less than “excellent.” As described by CAT developers, responses were positively skewed, making it necessary to dichotomize the satisfaction variables as “excellent” versus all other in order to have sufficient sample size for comparisons. Although it is difficult to ascertain the absolute clinical significance of a communication rating of “excellent” versus other ratings, our analyses demonstrate a relative difference in “excellent” ratings for Spanish-speaking versus English-speaking parents. Though there may be limits to the clinical significance of using “excellent” as a cutpoint for dichotomization, it allows identification of Spanish-speaking parents as a group with relatively lower satisfaction.
There are some additional limitations of this study. First, satisfaction was measured at a single point in infancy, and this analysis does not include information on parent perceptions at other time points. Second, the CAT may be subject to social desirability bias, and reflects only parent perception, in contrast to other methods of assessing quality of communication. Third, additional factors, such as maternal depression, could also have influenced results. Fourth, the sample included parents of infants who enrolled in a study; therefore, parent perceptions may not be fully generalizable to the entire clinic populations. Last, this study included pediatric resident physicians and generalizability to other physicians may be limited. Communication with resident physicians may be especially important to understand, however, since the communication patterns that physicians establish during their careers may start during this period. Additionally, conducting this study in clinic settings where residents practice allowed us to include a large sample of low-income families, whose communication with physicians is particularly important to understand because of the great challenges to health and healthcare access that these children face.
Conclusions
For Spanish-speaking parents, conducting visits in Spanish via a language-concordant provider or interpreter is an essential step toward quality medical care, yet may not be sufficient to yield high parent satisfaction with communication quality. Cultural differences, such as patient activation, may influence the quality of patient-physician communication. 19 Innovative approaches are needed to address both the linguistic and cultural needs of Spanish-speaking Latino parents. For example, models of care delivery that align Latino patients with linguistically and culturally concordant providers have reported improved satisfaction and understanding. 31,32 Another strategy for improving communication, suggested by Latina mothers, is investing more in relationships with families. 11 Finally, non-physician personnel could be used to address some of the gaps identified in satisfaction for Spanish-speaking Latino parents in this sample, including having as much information as desired, being treated respectfully, and discussing follow-up. Patient navigators, for example, could help reduce these linguistic and cultural barriers to care. 33 While this study focused on satisfaction among parents with limited English proficiency, the results apply to all parents bringing children for pediatric primary care, regardless of language barriers. Universal efforts to improve clear communication with parents are an acknowledged goal of pediatric quality initatives. 34,35 Improving parent satisfaction with physician communication in pediatric primary care, in fact, may be a first step to improving primary care for all children.
What’s New.
Spanish-speaking Latino parents experience lower satisfaction with primary care physician communication, compared with both English-speaking Latino and non-Latino parents. Parents’ satisfaction with communication was not significantly different between language-concordant care and care using an interpreter.
Acknowledgments
FUNDING: All phases of this study were supported by the Eunice Kennedy Shriver National Institute of Child Health and Development (grant R01 HD049794), with supplemental funding from the Centers for Disease Control and Prevention and Office of Behavioral and Social Science Research (grants R01HD059794-04S1 and R01HD059794-04S2). Parts of the study were supported by the National Institutes of Health’s National Center for Advancing Translational Sciences through its Clinical and Translational Science Awards Program, grants 1UL1RR029893, UL1TR000445, and UL1RR025747, as well as the National Institutes of Health DK56350 to fund the Nutrition Obesity Research Center at the University of North Carolina, Chapel Hill. Dr Yin is supported by a grant from the Health Resources and Services Administration (12-191-1077 Academic Administrative Units in Primary Care). National Institutes of Health (NIH).
Abbreviations
- CAT
Communication Assessment Tool
- IRB
Institutional Review Board
- STOFHLA
Short Test of Functional Health Literacy in Adults
- WIC
Special Supplemental Nutrition Program for Women, Infants, and Children
- IRR
Incidence rate ratio
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have indicated they have no potential conflicts of interest to disclose.
Clinical Trial Registration: This trial has been registered at www.clinicaltrials.gov (identifier NCT01040897).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. Census Bureau, Population Division. [Accessed 3/6, 2016];America's children: Key national indicators of well-being. 2015 http://www.childstats.gov/americaschildren/tables.asp.
- 2.DeCamp LR, Choi H, Davis MM. Medical home disparities for Latino children by parental language of interview. J Health Care Poor Underserved. 2011;22(4):1151–1166. doi: 10.1353/hpu.2011.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flores G, Abreu M, Olivar MA, Kastner B. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med. 1998;152(11):1119–1125. doi: 10.1001/archpedi.152.11.1119. [DOI] [PubMed] [Google Scholar]
- 4.Eneriz-Wiemer M, Sanders LM, Barr DA, Mendoza FS. Parental limited English proficiency and health outcomes for children with special health care needs: A systematic review. Acad Pediatr. 2014;14(2):128–136. doi: 10.1016/j.acap.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Flores G, Olson L, Tomany-Korman SC. Racial and ethnic disparities in early childhood health and health care. Pediatrics. 2005;115(2):e183–93. doi: 10.1542/peds.2004-1474. [DOI] [PubMed] [Google Scholar]
- 6.Office of Minority Health, editor. National standards for culturally and linguistically appropriate services in health and health care: A blueprint for advancing and sustaining CLAS policy and practice. Washington, DC: Department of Health and Human Services; Apr, 2013. [Google Scholar]
- 7.U.S. Department of Health and Human Services. HealthyPeople.gov. [Accessed 12/2016];Health communication and health information technology Web site. 2016 https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology/objectives. Updated 2016.
- 8.Arthur KC, Mangione-Smith R, Meischke H, et al. Impact of English proficiency on care experiences in a pediatric emergency department. Acad Pediatr. 2015;15(2):218–224. doi: 10.1016/j.acap.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Welty E, Yeager VA, Ouimet C, Menachemi N. Patient satisfaction among Spanish-speaking patients in a public health setting. J Healthc Qual. 2012;34(5):31–38. doi: 10.1111/j.1945-1474.2011.00158.x. [DOI] [PubMed] [Google Scholar]
- 10.Clark NM, Cabana MD, Nan B, et al. The clinician-patient partnership paradigm: Outcomes associated with physician communication behavior. Clin Pediatr (Phila) 2008;47(1):49–57. doi: 10.1177/0009922807305650. [DOI] [PubMed] [Google Scholar]
- 11.DeCamp LR, Kieffer E, Zickafoose JS, et al. The voices of limited English proficiency Latina mothers on pediatric primary care: Lessons for the medical home. Matern Child Health J. 2013;17(1):95–109. doi: 10.1007/s10995-012-0951-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinberg EM, Valenzuela-Araujo D, Zickafoose JS, Kieffer E, DeCamp LR. The “battle” of managing language barriers in health care. Clin Pediatr (Phila) 2016 doi: 10.1177/0009922816629760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seid M, Stevens GD, Varni JW. Parents' perceptions of pediatric primary care quality: Effects of race/ethnicity, language, and access. Health Serv Res. 2003;38(4):1009–1031. doi: 10.1111/1475-6773.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halfon N, Inkelas M, Mistry R, Olson LM. Satisfaction with health care for young children. Pediatrics. 2004;113(6 Suppl):1965–1972. [PubMed] [Google Scholar]
- 15.Sanders LM, Perrin EM, Yin HS, Bronaugh A, Rothman RL Greenlight Study Team. “Greenlight study”: A controlled trial of low-literacy, early childhood obesity prevention. Pediatrics. 2014;133(6):e1724–37. doi: 10.1542/peds.2013-3867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makoul G, Krupat E, Chang CH. Measuring patient views of physician communication skills: Development and testing of the communication assessment tool. Patient Educ Couns. 2007;67(3):333–342. doi: 10.1016/j.pec.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Myerholtz L. Assessing family medicine residents' communication skills from the patient's perspective: Evaluating the communication assessment tool. J Grad Med Educ. 2014;6(3):495–500. doi: 10.4300/JGME-D-13-00347.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.White RO, Chakkalakal RJ, Presley CA, et al. Perceptions of provider communication among vulnerable patients with diabetes: Influences of medical mistrust and health literacy. J Health Commun. 2016;21(sup2):127–134. doi: 10.1080/10810730.2016.1207116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alegria M, Sribney W, Perez D, Laderman M, Keefe K. The role of patient activation on patient-provider communication and quality of care for US and foreign born Latino patients. J Gen Intern Med. 2009;24(Suppl 3):534–541. doi: 10.1007/s11606-009-1074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzalez HM, Vega WA, Tarraf W. Health care quality perceptions among foreign-born Latinos and the importance of speaking the same language. J Am Board Fam Med. 2010;23(6):745–752. doi: 10.3122/jabfm.2010.06.090264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arauz Boudreau AD, Fluet CF, Reuland CP, Delahaye J, Perrin JM, Kuhlthau K. Associations of providers' language and cultural skills with Latino parents' perceptions of well- child care. Acad Pediatr. 2010;10(3):172–178. doi: 10.1016/j.acap.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Clemans-Cope L, Kenney G. Low income parents' reports of communication problems with health care providers: Effects of language and insurance. Public Health Rep. 2007;122(2):206–216. doi: 10.1177/003335490712200210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ngui EM, Flores G. Satisfaction with care and ease of using health care services among parents of children with special health care needs: The roles of race/ethnicity, insurance, language, and adequacy of family-centered care. Pediatrics. 2006;117(4):1184–1196. doi: 10.1542/peds.2005-1088. [DOI] [PubMed] [Google Scholar]
- 24.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14(7):409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wallace LS, DeVoe JE, Rogers ES, Protheroe J, Rowlands G, Fryer GE., Jr Digging deeper: Quality of patient-provider communication across hispanic subgroups. BMC Health Serv Res. 2009;9 doi: 10.1186/1472-6963-9-240. 240-6963-9-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kochhar R, Suro R, Tafoya S, editors. The new Latino south: The context and consequences of rapid population growth. Washington, DC: Pew Hispanic Center; 2005. [Google Scholar]
- 27.Flores G. The impact of medical interpreter services on the quality of health care: A systematic review. Med Care Res Rev. 2005;62(3):255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 28.Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen AH, Youdelman MK, Brooks J. The legal framework for language access in healthcare settings: Title VI and beyond. J Gen Intern Med. 2007;22(Suppl 2):362–367. doi: 10.1007/s11606-007-0366-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson DA, Hernandez RG, Cowden JD, Sisson SD, Moon M. Caring for patients with limited English proficiency: Are residents prepared to use medical interpreters? Acad Med. 2013;88(10):1485–1492. doi: 10.1097/ACM.0b013e3182a3479d. [DOI] [PubMed] [Google Scholar]
- 31.Cowden JD, Thompson DA, Ellzey J, Artman M. Getting past getting by: Training culturally and linguistically competent bilingual physicians. J Pediatr. 2012;160(6):891–892.e1. doi: 10.1016/j.jpeds.2012.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Dunlap JL, Jaramillo JD, Koppolu R, Wright R, Mendoza F, Bruzoni M. The effects of language concordant care on patient satisfaction and clinical understanding for hispanic pediatric surgery patients. J Pediatr Surg. 2015;50(9):1586–1589. doi: 10.1016/j.jpedsurg.2014.12.020. [DOI] [PubMed] [Google Scholar]
- 33.Robert Wood Johnson Foundation. [Accessed 1/28, 2015];Finding answers: Disparities research for change. http://www.solvingdisparities.org/tools/roadmap. Updated 2015.
- 34.American Academy of Pediatrics. [Accessed 6/5, 2016];National center for medical home implementation. https://medicalhomeinfo.aap.org/tools-resources/Pages/For-Practices.aspx.
- 35.DeWalt DA, Callahan LF, Hawk VH, Broucksou KA, Hink A, Rudd R, Brach C, editors. Health literacy universal precautions toolkit. Rockville, MD: Agency for Healthcare Research and Quality; 2010. AHRQ Publication No. 10-0046-EF ed. Prepared by North Carolina Network Consortium, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, under Contract No. HHSA290200710014, ed. [Google Scholar]