Abstract
This study aimed to determine if active feedback gait retraining to produce a medial weight transfer at the foot significantly reduces the knee adduction moment in subjects with medial compartment knee osteoarthritis. Secondarily, changes in peak knee flexion moment, frontal plane knee and ankle kinematics, and center of pressure were investigated. Ten individuals with medial compartment knee osteoarthritis (9 males; age: 65.3±9.8 years; BMI: 27.8±3.0 kg/m2) were tested at self-selected normal and fast speeds in two conditions: intervention, with an active feedback device attached to the shoe of their more affected leg, and control, with the device de-activated. Kinematics and kinetics were assessed using a motion capture system and force plate. The first peak, second peak, and impulse of the knee adduction moment were significantly reduced by 6.0%, 13.9%, and 9.2%, respectively, at normal speed, with reductions of 10.7% and 8.6% in first peak and impulse at fast speed, respectively, with the active feedback system, with no significant effect on the peak knee flexion moment. Significant reductions in peak varus knee angle and medialized center of pressure in the first half of stance were observed, with reductions in peak varus knee angle associated with reductions in the knee adduction moment. This study demonstrated that active feedback to produce a medial weight-bearing shift at the foot reduces the peaks and impulse of the knee adduction moment in patients with medial compartment knee osteoarthritis. Future research should determine the long-term effect of the active feedback intervention on joint loading, pain, and function.
Keywords: Knee, Osteoarthritis, Gait Modification, Knee Adduction Moment, Active Feedback
Introduction
Given the scope and magnitude of the chronic physical disability caused by osteoarthritis (OA)1, and the high prevalence of OA of the knee2,3, there is an unmet need for low cost and effective interventions for knee OA. Load-modifying interventions that address the medial compartment of the knee are of particular importance, as there is a 10-fold greater incidence4 of medial compartment knee OA versus lateral compartment knee OA, believed to be due to the greater distribution of loading on the medial compartment of the knee.5 While direct measurement of load on the medial knee compartment is not feasible, the observation that an external parameter measured during walking can be associated with load on the medial compartment has enabled the assessment of load-modifying interventions for knee OA. Specifically, the greater distribution of loading on the medial compartment has been related to an increase in the external knee adduction moment (KAM).6,7 Thus, the KAM provides a measureable parameter that describes the internal medial/lateral distribution of loading at the knee.
The first peak of the KAM and KAM impulse (integration of KAM over stance time) have shown clinical relevance, being associated with the presence8, severity9, and rate of progression of medial compartment knee OA.10-12 As a result, reducing the KAM offers an attractive target for interventions to potentially reduce medial compartment joint loading and slow the rate of progression and reduce painful symptoms of the disease. However, attempts to introduce non-surgical load-modifying interventions have been met with limited success. While most approaches to load-modifying interventions have reported a reduction in the KAM13-15, the general adoption of this type of intervention has been limited for a variety of reasons. For example, patient discomfort with braces14 and lateral wedges16 has led to poor compliance. Further, such interventions require continual use of specialized equipment for an effect to be seen.
Gait retraining, or modifying walking style, has also been shown to reduce the KAM using techniques such as increased ipsilateral trunk sway17, change in foot progression angle18-20, medial weight transfer at the foot21, change in walking speed22, and medial thrust gait wherein the knee is medialized during stance phase.23,24 It has also been shown that several combinations of modifications can be trained at once.18 Visual or haptic feedback can also increase the ability of subjects to perform and internalize the modifications through training.25 An overall perspective of both the physical and gait retraining approaches to load modification suggests that the more extreme the change introduced by the intervention the less likely the patient will sustain the change. Also, the load modification may induce changes in other factors, such as the knee flexion moment (KFM), that can have a substantial influence on the total load acting the knee.26 Thus, there remains a need for an approach that provides sufficient changes to the KAM without causing unwanted changes to other load components such as the KFM.27
One such approach is medial weight transfer at the foot, a simple, promising gait modification which has been shown to reduce the KAM immediately by 14.2% in healthy young subjects with use of an active feedback system incorporating vibration.21 This work built upon a prior study which demonstrated that a medial shift in foot pressure caused by a lateral wedge was related to a reduction in the KAM.28 A recent study investigating the relationship between changes in KAM and changes in foot center of pressure caused by medial thrust gait23 has further suggested that medializing plantar pressure should be investigated with the aim of reducing the KAM in those with medial knee OA.
Thus the purpose of this study was to determine if active feedback gait retraining to produce a medial weight transfer at the foot will significantly reduce the KAM in subjects with symptoms of medial compartment knee OA. Specifically, we tested the following primary hypothesis: 1) Gait retraining to produce a medial weight-bearing shift via an active feedback system will reduce the KAM (first peak, second peak, and impulse) compared to untreated control. Secondarily, we also tested the following hypothesis: 2) The peak KFM will not change relative to an untreated control in subjects using a medial weight-bearing shift via an active feedback system. We also sought to understand the effects of the active feedback gait retraining on frontal plane knee kinematics (peak varus knee angle during loading), ankle kinematics (peak ankle eversion in stance), and foot center of pressure (COP), including if changes in the KAM (first and second peaks) are associated with the changes in the frontal plane knee and ankle kinematics and foot COP.
Methods
Study Design and Level of Evidence
Level 3, Cross-Sectional Study Design
Subjects
Ten individuals with symptoms of medial compartment knee OA and physician-diagnosed radiographic medial compartment knee OA (Kellgren-Lawrence grade ≥ 1) participated in this study after giving written consent in accordance with Institutional Review Board approval. Subjects were recruited from the orthopedic clinic or from the community after responding to an advertisement and were enrolled after meeting the inclusion/exclusion criteria. Inclusion criteria included: persistent medial compartment knee joint pain, age between 18 and 80 years, full weight-bearing status, and ability to provide informed consent. Exclusion criteria included: body mass index (BMI) > 35 kg/m2, use of walking aid, nerve or muscle disease associated with walking difficulty, and foot neuropathy. An a priori sample size calculation was performed for comparing the KAM between conditions based on preliminary data for percent changes in first peak KAM with the gait modification from a cohort of healthy subjects.21 Using an alpha level of 0.05, a power of 0.8, and a mean percent change of 14%, 10 subjects were needed to adequately power the study for changes in KAM.
Testing Procedure
The testing protocol involved testing subjects with their own low-top athletic sneakers in two conditions: intervention and control.
Intervention
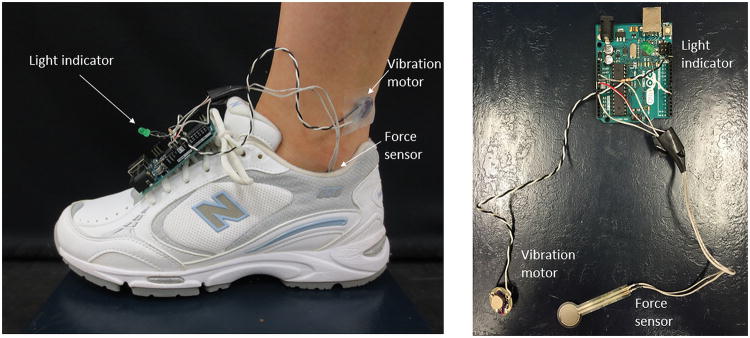
The subjects wore an active feedback device (Figure 1) attached to the shoe of their more affected leg, as determined by self-reported pain. The device, similar to the one used in a previous study of healthy subjects21, measured pressure under the lateral side of the heel (sensor placed in the shoe) and activated a vibration motor if the loading crossed a set threshold. The threshold was determined individually for each subject prior to intervention trial testing by adjusting the system so that the sensor was activated during normal walking resulting in vibration, but the subject was able to stop vibration by producing a medial shift at the foot during walking. The vibration motor was placed in contact with the skin at the foot/ankle, with the location of the vibration motor customized for each subject to achieve maximal sensitivity. Subjects were instructed to walk in a manner to keep the device from activating the vibration, by shifting weight medially at the foot. Prior to measurement with the active feedback device, subjects were given as much time as necessary to get used to the new gait condition. The incorporation of a light indicator allowed researchers to see if the subject was able to successfully stop vibration with the medial weight transfer at the foot.
Figure 1.
The active feedback gait modification intervention, incorporating a force sensor placed under the lateral side of the heel, a vibration motor placed in contact with the skin on the foot/ankle, and a light indicator to indicate activation of the vibration motor.
Control
The subjects were tested with an inactive feedback system attached to the shoe of their more affected leg, to accommodate for any potential effect of wearing the system itself. Control trials were collected prior to intervention trial practice and collection.
Subjects performed five successful walking trials at self-selected normal and fast speeds in each of the two conditions, for a total of 20 trials per subject. For fast speed trials, subjects were instructed to walk at a self-selected pace that was faster than their self-selected normal pace. A faster-than-normal speed was collected, in addition to subject's self-selected pace, for comparison to previous work in a healthy population21, as subjects with symptoms of medial compartment knee OA are known to walk at a slower pace than healthy subjects.9,29 Kinematic data were collected using a multi-camera motion capture system (Qualisys Medical, Gothenburg, SE) and the point cluster technique, which uses a redundant set of 21 reflective markers.30 Ground reaction forces were collected using a multicomponent force plate embedded in the ground (Bertec Corporation, Columbus, OH). The systems were synchronized and recorded data at 120 Hz. A trial was considered successful if the foot of the test leg fully stepped on the force plate. Lower-limb kinematics and kinetics were calculated using the software application BioMove (Stanford University, Stanford, CA) as described briefly below. The position and orientation of the foot, shank, and thigh segments were calculated using clusters of reflective markers fixed to the participant.30,31 Anatomical landmarks were identified by palpation, and these landmarks were used to define the anatomical frame of the lower-limb segments following a previously described procedure31 during a standing reference pose collected before the walking trials. Knee angles were calculated according to the joint coordinate system.32 The peak varus knee angle during loading and peak ankle eversion angle in stance were extracted for analysis. Knee moments were calculated using an inverse dynamics approach33 with the foot, lower leg, and thigh segments idealized as rigid bodies and their scaled inertial properties taken from the literature34, and were expressed as external moments relative to the tibial anatomical frame and normalized to percent bodyweight and height (Bw*Ht). The first and second peak KAMs were defined as the maximum moments during the first and second half of stance phase, respectively, and the KAM angular impulse was calculated as the time integral of the KAM curve during the entire stance phase. The peak KFM was defined as the maximum moment during the first half of stance phase. Average foot COP during the first (COP1) and second (COP2) halves of stance in the medial/lateral direction were calculated with respect to a reference line connecting the heel and 5th metatarsal foot markers, where a more positive value in COP indicates a more medial COP.
Data Analysis
All statistical analyses were completed in SPSS version 23.0 (SPSS Inc., Chicago, IL). Differences in the first peak KAM, second peak KAM, KAM impulse, peak KFM, peak varus knee angle during loading, peak ankle eversion angle, and COP between experimental conditions were analyzed using two-way repeated measures analysis of variance (ANOVA) with intervention and speed as between-test factors. Upon a significant result of the ANOVA, post hoc paired Student's t-tests were used for analyses. Relationships between changes (intervention – control) in first and second peak KAM and changes in peak varus knee angle during loading, peak ankle eversion, and COP were assessed by the calculation of Pearson correlation coefficients. P-values <0.05 were considered significant.
Results
The study participants included 9 males and 1 female, with an average (± standard deviation) age of 65.3 ± 9.8 years and BMI of 27.8 ± 3.0 kg/m2. The participant's average self-reported daily medial knee pain on a 0-10 scale (0 indicating no pain and 10 worst pain) was 3.2 ± 3.6. Five participants had previously undergone medial meniscectomy surgery and all participants had radiographic medial compartment knee OA (Kellgren-Lawrence grade ≥ 1) in the study knee.
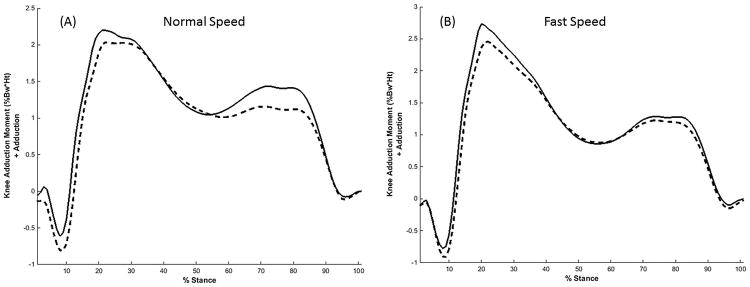
There was a significant effect of the intervention on the first peak KAM (p=0.001), second peak KAM (p=0.005), and KAM impulse (p=0.009), irrespective of walking speed. The first peak of the KAM was significantly reduced both at normal and fast walking speeds, with reductions of 6.0% (p=0.040) and 9.2% (p<0.001), respectively, with the active feedback system as compared to control (Table 1; Figure 2). The second peak KAM was significantly reduced at normal walking speed, with a reduction of 13.9% (p<0.001), with no significant reduction at fast speed (p=0.244) (Table 1; Figure 2). The KAM impulse was also significantly reduced at both normal and fast walking speeds with the active feedback system as compared to control, with reductions of 10.7% (p=0.012) and 8.6% (p=0.026), respectively (Table 1). There was no significant interaction effect of walking speed and intervention on either the first peak KAM (p=0.129) or KAM impulse (p=0.405), while a significant interaction effect was seen for the second peak KAM (p=0.024).
Table 1.
Mean (± standard deviation) of the first peak KAM, second peak KAM, KAM impulse, peak KFM, peak varus knee angle during loading, COP, and walking speed in the control and active feedback gait retraining intervention conditions. P-values presented are from post-hoc paired t-tests. Bold indicates significance at the 0.05 level.
| Variable | Condition | Normal Speed | Fast Speed |
|---|---|---|---|
| First Peak KAM (%Bw*Ht) | Control | 2.41 ± 1.10 | 2.90 ± 1.28 |
| Active Feedback | 2.26 ± 1.04 | 2.63 ± 1.35 | |
| P-value | 0.040 | <0.001 | |
| Second Peak KAM (%Bw*Ht) | Control | 1.71 ± 1.01 | 1.58 ± 1.11 |
| Active Feedback | 1.47 ± 0.96 | 1.50 ± 1.13 | |
| P-value | <0.001 | 0.244 | |
| KAM Impulse (%Bw*Ht*s) | Control | 0.77 ± 0.48 | 0.71 ± 0.47 |
| Active Feedback | 0.69 ± 0.51 | 0.65 ± 0.51 | |
| P-value | 0.012 | 0.026 | |
| Peak KFM (%Bw*Ht) | Control | 2.48 ± 1.38 | 3.20± 1.53 |
| Active Feedback | 2.51 ± 1.42 | 3.25 ± 1.79 | |
| P-value | 0.898 | 0.741 | |
| Peak Varus Knee Angle in Loading (◦) | Control | 0.99 ± 4.90 | 1.33 ± 4.79 |
| Active Feedback | 0.29 ± 4.65 | 0.75 ± 4.98 | |
| P-value | 0.046 | 0.039 | |
| Peak Ankle Eversion Angle in Stance (◦) | Control | 13.9 ± 5.4 | 14.1 ± 5.4 |
| Active Feedback | 14.7 ± 5.3 | 14.7 ± 5.4 | |
| P-value | 0.193 | 0.148 | |
| COP1 (mm) | Control | 43.1 ± 5.6 | 43.9 ± 6.0 |
| Active Feedback | 49.0 ± 7.6 | 47.5 ± 6.7 | |
| P-value | 0.011 | 0.006 | |
| COP2 (mm) | Control | 28.3 ± 9.5 | 29.1 ± 10.5 |
| Active Feedback | 31.8 ± 13.7 | 30.8 ± 11.7 | |
| P-value | 0.079 | 0.141 | |
| Speed (m/s) | Control | 1.28 ± 0.14 | 1.53 ± 0.18 |
| Active Feedback | 1.31 ± 0.12 | 1.50 ± 0.15 | |
| P-value | 0.183 | 0.374 |
Figure 2.
Average KAM curves of control gait (solid line) and of medial weight transfer gait (dashed line) during stance phase at (A) normal and (B) fast speeds.
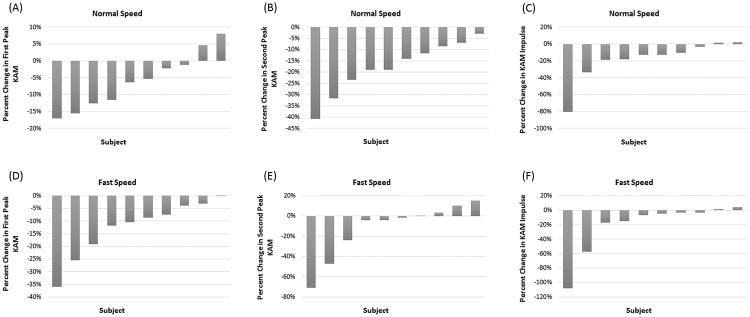
The magnitude of change in the KAM varied between individuals, where 60% to 100% of subjects had a reduced first peak KAM, second peak KAM, or KAM impulse with the active feedback intervention (Figure 3). Forty percent of subjects had a reduction in first peak KAM greater than 10% and 70% of subjects had a reduction in second peak KAM and KAM impulse greater than 10% at normal speed. While the majority of subjects had a reduction in first peak KAM, there was a small percentage of the study population (20% at normal speed) with an increase in loading with the active-feedback gait intervention. However, nearly all patients showed a reduction in the first peak KAM when asked to walk at a fast speed.
Figure 3.
Individual subject percent changes (ordered from largest to smallest) in the first peak KAM (A and D), second peak KAM (B and E), and KAM impulse (C and F) at normal (top row) and fast (bottom row) speeds with active feedback gait retraining versus control.
Importantly, the active feedback intervention did not have a significant effect on the peak KFM (p=0.805, Table 1) relative to control. The KFM was unchanged relative to control for both the normal and fast walking speeds (Table 1). There was no difference in walking speed at either normal or fast speeds with active feedback intervention as compared to control (normal: p=0.183, fast: p=0.374, Table 1). Further, no significant increases in peak ankle eversion angle during stance with active feedback were observed (p=0.167, Table 1) relative to control at either normal or fast speeds.
There was a significant effect of the active feedback intervention on the peak varus knee angle during loading (p=0.030), irrespective of walking speed, with significant reductions in peak varus knee angle at both normal (p=0.046) and fast (p=0.039) walking speeds (Table 1). There was also a significant effect of active feedback intervention on the foot COP in the first half of stance phase (p=0.005), irrespective of walking speed, with significant medialization of the COP in the first half of stance at both normal (p=0.011) and fast (p=0.006) walking speeds (Table 1). Medialization in COP in the second half of stance did not reach statistical significance at either normal (p=0.079) or fast (p=0.141) walking speeds (Table 1).
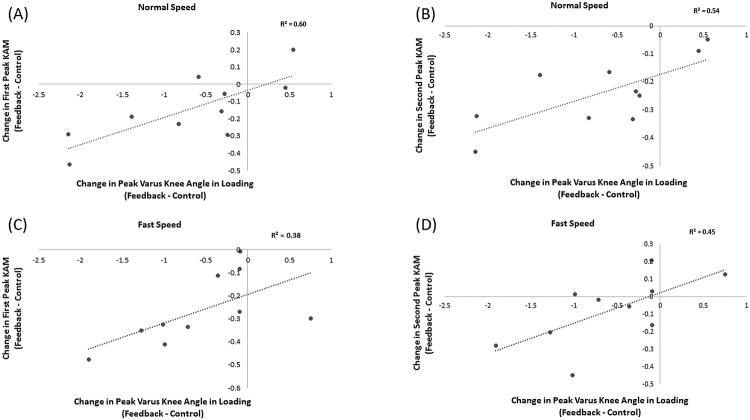
Analysis of associations between changes in first peak KAM and second peak KAM and changes in knee and ankle kinematics and foot COP are presented in Table 2. The reductions in varus knee angle during loading were associated with changes in first peak KAM and second peak KAM (Figure 4). Specifically, at normal speed, subjects with greater reductions in peak varus knee angle during loading had greater reductions in first peak KAM and second peak KAM (Table 2). At fast speed, subjects with greater reductions in varus knee angle during loading had greater reductions in second peak KAM, with a trend towards an association between greater reduction in peak varus knee angle during loading and greater reduction in first peak KAM (Table 2). No significant associations were observed between the change in COP in the first half of stance and change in first peak KAM, nor were any associations found between the change in COP in the second half of stance and change in second peak KAM. Further, no associations were observed between changes in ankle eversion angle and either the first or second peak KAM at normal or fast speeds (Table 2).
Table 2.
Associations between changes (intervention – control) in KAM (first peak and second peak) and changes (intervention – control) in peak varus knee angle during loading, peak ankle eversion angle in stance, and COP (first and second halves of stance). Pearson correlation coefficients (95% confidence intervals) and p-values are presented. Bold indicates significance at the 0.05 level.
| Variable | First Peak KAM | Second Peak KAM | ||
|---|---|---|---|---|
| R (95% CI) | P-value | R (95% CI) | P-value | |
| Peak Ankle Eversion Angle in Stance | ||||
| Normal Speed | -0.230 (-0.751, 0.468) | 0.522 | 0.050 (-0.599, 0.659) | 0.892 |
| Fast Speed | -0.188 (-0.731, 0.501) | 0.746 | 0.219 (-0.476, 0.746) | 0.543 |
| Peak Varus Knee Angle in Loading | ||||
| Normal Speed | 0.773 (0.278, 0.943) | 0.009 | 0.735 (0.195, 0.933) | 0.016 |
| Fast Speed | 0.619 (-0.017, 0.898) | 0.056 | 0.671 (0.071, 0.914) | 0.034 |
| COP1 | ||||
| Normal Speed | -0.247 (-0.453, 0.759) | 0.492 | --- | --- |
| Fast Speed | 0.045 (-0.602, 0.656) | 0.901 | --- | --- |
| COP2 | ||||
| Normal Speed | --- | --- | -0.304 (-0.783, 0.403) | 0.393 |
| Fast Speed | --- | --- | 0.276 (-0.428, 0.771) | 0.439 |
Figure 4.
Associations between individual subject changes (intervention – control) in the first peak KAM (A and C) and second peak KAM (B and D) and changes in peak varus knee angle during loading at normal (top row) and fast (bottom row) speeds with active feedback gait retraining versus control. Reductions in first peak KAM, second peak KAM, and peak varus knee angle with active feedback are shown as negative values.
Discussion
The results of this study support the primary hypothesis and demonstrate that an active feedback gait retraining intervention to produce a subtle medial weight-bearing shift at the foot reduces the KAM (first peak, second peak, and KAM angular impulse) in subjects with symptoms of medial compartment knee OA. The majority of patients were able to reduce the KAM. While these reductions were smaller than reported in healthy subjects,21 where a mean reduction of 14.2% in first peak KAM was seen using the active feedback intervention, the symptomatic subjects in this study walked at a slower self-selected pace (mean speed of 1.30 m/s) than the healthy subjects (mean speed of 1.43 m/s). While there was not a statistically significant difference in magnitude of reduction of the first peak KAM between normal and fast speeds in this study (p=0.129), the results suggest that the amount of reduction in the KAM is likely partially dependent on walking speed since the reduction in first peak KAM in the current study at the faster-than-normal pace (mean speed of 1.5 m/s) was closer to the reduction seen previously in healthy subjects. Thus, assessing interventions of this nature should account for the walking speed of the target population.
Another important finding of this study was that the peak KFM was unchanged with this intervention. This is important as the KFM will influence the total force acting on the medial compartment of the knee.5,26 Specifically, the KFM acts to balance the flexor and extensor muscle force at the joint, and a change in the KFM can be interpreted to reflect a change in the muscle force. Given that the muscles contribute the major portion of the total force across the knee, a reduction in KAM associated with an intervention might not reflect a reduction in the load on the medial compartment if there is a change in the KFM.26 The importance of the KFM in the context of knee OA is further supported by recent work where the peak KFM was associated with disease progression in knee OA.11 Thus, any condition that causes a substantial change in the pattern of locomotion should be evaluated for an unanticipated response to other factors that influence joint loading such as the KFM.
While the majority of subjects had a reduction in KAM, there was a substantial range of change in the KAM peaks and KAM impulse among patients. Further, several subjects were non-responders to the intervention, and increased their KAM with the gait modification. Subject specific characteristics such as disease severity, lower limb alignment, neuromuscular control, muscle strength, age, and BMI may influence the ability of the active feedback intervention to affect joint loading in the patient population, and should be investigated in a larger study as the study design at this stage was not powered for such an analysis. Further, the sustainability of the gait retraining and tolerability for longer-term clinical implementation requires future consideration. Neurological literature showing reorganization of the motor cortex due to repetitive training35,36 suggests the potential for such a gait retraining intervention to have durable effects after a period of extended use. While the results are promising, and the gait modification was readily achieved, a longitudinal study would be required to determine the feasibility of the gait modification to improve joint loading in the long term as well as evaluate potential improvements in clinical outcomes such as pain and function. While no change in peak KFM was observed in this study, future larger studies will also ensure adequate statistical power for secondary outcomes such as changes in peak KFM.
The force threshold used for the gait modification intervention was set using an iterative manner, such that during normal walking the vibration was activated and each subject's threshold was set once they were able to turn off the vibration with a medial weight shift at the foot. Higher thresholds requiring greater subject modifications were not attempted once this threshold was reached. As real-time calculation of the reduction in KAM was not available with the current testing protocol, it was not possible to determine an ‘optimal’ reduction in force producing an ‘optimal’ reduction in KAM (i.e. to determine if requiring the subject to perform a more exaggerated modification would result in a greater reduction in KAM). Future work could consider using a more quantitative approach to setting the threshold to determine if greater reductions in KAM could be achieved with greater subject modifications.
The reductions in peak KAM and KAM impulse are of similar magnitude to other non-invasive gait modification interventions in subjects with symptoms of medial compartment knee OA, including changes in foot progression angle19,20, medial thrust gait23, and ipsilateral trunk lean17. The reductions in KAM in the current study are not as large as those reported previously for gait modification with haptic feedback in a healthy population at a single testing session37, which reached reductions of greater than 30% through subject-specific alterations in multiple gait parameters. However, the applicability of such a multi-parameter modification to the knee OA population is unclear, as they may not have the necessary endurance or learning abilities as a young, healthy population. Further, although the reductions observed in this study were not as large as reductions seen following surgical interventions such as high tibial osteotomy38, the intervention used in the current study is non-invasive, and due to the continued feedback has the potential for a sustained effect with continued use, repetitive practice, and internalization of the new movement pattern.35,36 In addition, since there was no significant increase in peak KFM with the active feedback intervention in this study, the results of this study suggest that the reductions observed in KAM reflect reductions in medial compartment joint loading, and therefore may have the potential to affect clinical outcomes such as pain and function with sustained use.
The kinematic analyses aid in understanding the mechanism for the reduction in the KAM produced by a medial weight-bearing shift at the foot. Specifically, there was significant medialization in foot COP in the first half of stance phase and a significant reduction in peak varus knee angle during the loading phase of stance. A medial shift in COP is somewhat counterintuitive, when considering the effect independently. If all other variables remained constant, one would expect a medial shift in COP would result in an increase in the moment arm of the ground reaction force about the knee center. However, as also described, the intervention resulted in a significant reduction in peak varus knee angle, which would tend to reduce the lever arm. While no significant associations were found between medialization in foot COP and changes in KAM, significant associations between reductions in peak varus knee angle were observed with reductions in KAM peaks. As the KAM is the product of the ground reaction force and the moment arm of the ground reaction force in the frontal plane, the reduction of the varus knee angle due to the gait modification likely resulted in a reduction of the frontal plane moment arm39, leading to significant reductions in KAM. No significant effect of the intervention was seen in this study on frontal plane ankle kinematics, which may be a positive finding and should be confirmed in a larger future study, as increased eversion angles may increase stresses on the medial ankle and arch, which could lead to discomfort with longer-term use.
In conclusion, this study demonstrated that active feedback (vibration) can modify gait to produce a medial weight-bearing shift at the foot that reduces the KAM peaks and KAM impulse in patients with medial compartment knee OA. In particular, the simple feedback used in this study has the advantage that it could potentially be utilized in a clinical or home setting, as it does not require specialized equipment such as a motion capture system. The results suggest that a substantial portion of the change in KAM could be explained by a reduction in the frontal plane varus knee angle. It is also important to note that the reductions in KAM were achieved without an increase in peak KFM. Such a gait modification may be a simple intervention for medial compartment knee OA, and future research is needed to determine the long-term effect of the active feedback intervention on joint loading as well as clinical outcomes of pain and function.
Acknowledgments
This work was supported by the NIH (grant R01 AR052784-CRC) and a National Science Foundation Fellowship. The funding sources had no role in the study design, collection or analysis of data, or manuscript preparation or submission.
Footnotes
Author Contributions Statement: Dr. Erhart-Hledik participated in design of the research study, acquisition, analysis, and interpretation of the data, and drafting of the manuscript. Drs. Andriacchi and Chu each participated in interpretation of the data and revising of the manuscript. Ms. Asay and Ms. Clancy each participated in acquisition and analysis of the data and revising of the manuscript. Dr. Erhart-Hledik takes responsibility for content of the manuscript. All authors have read and approved the final submitted manuscript.
Conflict of Interest Statement: The authors declare no conflict of interest that could influence the content of the presented work.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oliveria SA, Felson DT, Reed JI, et al. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995;38:1134–41. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahlback S. Osteoarthritis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;277(Suppl):7–72. [PubMed] [Google Scholar]
- 5.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–9. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 6.Erhart JC, Dyrby CO, D'Lima DD, et al. Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. J Orthop Res. 2010;28:1548–53. doi: 10.1002/jor.21183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao D, Banks SA, Mitchell KH, et al. Correlation between the knee adduction moment torque and medial contact force for a variety of gait patterns. J Orthop Res. 2007;25:789–97. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]
- 8.Baliunas AJ, Hurwitz DE, Ryals AB, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10:573–9. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 9.Mündermann A, Dyrby CO, Hurwitz DE, et al. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: Reduced walking speed. Arthritis Rheum. 2004;50:1172–78. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 10.Miyazaki T, Wada M, Kawahara H, et al. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–22. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(11):1833–9. doi: 10.1016/j.joca.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang AH, Moisio KC, Chmiel JS, et al. External knee adduction and flexion moments during gait and medial tibiofemoral disease progression in knee osteoarthritis. Osteoarthritis Cartilage. 2015;23(7):1099–106. doi: 10.1016/j.joca.2015.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnold JB, Wong DX, Jones RK, et al. Lateral wedge insoles for reducing biomechanical risk factors for medial knee osteoarthritis progression: A systematic review and meta-analysis. Arthritis Care Res. 2016;68(7):936–51. doi: 10.1002/acr.22797. [DOI] [PubMed] [Google Scholar]
- 14.Moyer RF, Birmingham TB, Bryant DM, et al. Biomechanical effects of valgus knee bracing: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(2):178–88. doi: 10.1016/j.joca.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Radzimski AO, Mündermann A, Sole G. Effect of footwear on the external knee adduction moment - A systematic review. Knee. 2012;19(3):163–75. doi: 10.1016/j.knee.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Kerrigan DC, Lelas JL, Goggins J, et al. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2002;83:889–93. doi: 10.1053/apmr.2002.33225. [DOI] [PubMed] [Google Scholar]
- 17.Simic M, Hunt MA, Bennell KL, et al. Trunk lean gait modification and knee joint load in people with medial knee osteoarthritis: the effect of varying trunk lean angles. Arthritis Care Res. 2012;64(10):1545–53. doi: 10.1002/acr.21724. [DOI] [PubMed] [Google Scholar]
- 18.Shull PB, Silder A, Shultz R, et al. Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis. J Orthop Res. 2013;31(7):1020–5. doi: 10.1002/jor.22340. [DOI] [PubMed] [Google Scholar]
- 19.Shull PB, Shultz R, Silder A, et al. Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis. J Biomech. 2013;46:122–8. doi: 10.1016/j.jbiomech.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 20.Simic M, Wrigley TV, Hinman RS, et al. Altering foot progression angle in people with medial knee osteoarthritis: the effects of varying toe-in and toe-out angles are mediated by pain and malalignment. Osteoarthritis Cartilage. 2013;21(9):1272–80. doi: 10.1016/j.joca.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Dowling AV, Fisher DS, Andriacchi TP. Gait modification via verbal instruction and an active feedback system to reduce peak knee adduction moment. J Biomech Eng. 2010;132:071007–1. doi: 10.1115/1.4001584. [DOI] [PubMed] [Google Scholar]
- 22.Robbins SM, Maly MR. The effect of gait speed on the knee adduction moment depends on waveform summary measures. Gait Posture. 2009;30(4):543–6. doi: 10.1016/j.gaitpost.2009.08.236. [DOI] [PubMed] [Google Scholar]
- 23.Ferrigno C, Wimmer MA, Trombley RM, et al. A reduction in the knee adduction moment with medial thrust gait is associated with a medial shift in center of plantar pressure. Med Eng Phys. 2016;38(7):615–21. doi: 10.1016/j.medengphy.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Fregly BJ, D'Lima DD, Colwell CW. Effective Gait Patterns for Offloading the Medial Compartment of the Knee. J Orthop Res. 2009;27(8):1016–1021. doi: 10.1002/jor.20843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hunt MA, Simic M, Hinman RS, et al. Feasibility of a gait retraining strategy for reducing knee joint loading: increased trunk lean guided by real-time biofeedback. J Biomech. 2011;44:943–7. doi: 10.1016/j.jbiomech.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 26.Walter JP, D'Lima DD, Colwell CW, Fregly BJ. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res. 2010;28:1348–54. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andriacchi T. Valgus alignment and lateral compartment knee OA: A biomechanical paradox or new insight into knee OA? Arthritis Rheum. 2013;65(2):310–3. doi: 10.1002/art.37724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Erhart JC, Mündermann A, Mündermann L, Andriacchi TP. Predicting changes in knee adduction moment due to load-altering interventions from pressure distribution at the foot in healthy subjects. J Biomech. 2008;41:2989–94. doi: 10.1016/j.jbiomech.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 29.Kumar D, Manal KT, Rudolph KS. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(2):298–305. doi: 10.1016/j.joca.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andriacchi TP, Alexander EJ, Toney MK, et al. A point cluster method for in vivo motion analysis: applied to a study of knee kinematics. J Biomech Eng. 1998;120:743–749. doi: 10.1115/1.2834888. [DOI] [PubMed] [Google Scholar]
- 31.Dyrby CO, Andriacchi TP. Secondary motions of the knee during weight bearing and non-weight bearing activities. J Orthop Res. 2004;22:794–800. doi: 10.1016/j.orthres.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–44. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 33.Andriacchi TP, Johnson TS, Hurwitz DE, Nataraja RN. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Huiskes R, editors. Basic Orthopaedic Biomechanics and Mechano-Biology. 3rd. Lippin- cott Williams & Wilkins; Philadelphia, PA: 2005. pp. 91–122. [Google Scholar]
- 34.Dempster WT, Gaughran GRL. Properties of body segments based on size and weight. Am J Anat. 1967;120:33–54. [Google Scholar]
- 35.Karni A, Meyer G, Jezzard P, et al. Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature. 1995;377(6545):155–8. doi: 10.1038/377155a0. [DOI] [PubMed] [Google Scholar]
- 36.Ungerleider LG, Doyon J, Karni A. Imaging brain plasticity during motor skill learning. Neurobiol Learn Mem. 2002;78(3):553–64. doi: 10.1006/nlme.2002.4091. [DOI] [PubMed] [Google Scholar]
- 37.Shull PB, Lurie K, Cutkosky MR, et al. Training multi-parameter gaits to reduce the knee adduction moment with data-driven models and haptic feedback. J Biomech. 2011;44:1605–1609. doi: 10.1016/j.jbiomech.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 38.Wada M, Imura S, Nagatani K, et al. Relationship between gait and clinical results after high tibial osteotomy. Clin Orthop Relat Res. 1998;354:180–188. doi: 10.1097/00003086-199809000-00022. [DOI] [PubMed] [Google Scholar]
- 39.Jenkyn TR, Erhart JC, Andriacchi TP. An analysis of the mechanisms for reducing the knee adduction moment during walking using a variable stiffness shoe in subjects with knee osteoarthritis. J Biomech. 2011;44:1271–1276. doi: 10.1016/j.jbiomech.2011.02.013. [DOI] [PubMed] [Google Scholar]