Abstract
Background:
The DRAGON score, which includes clinical and computed tomographic (CT) scan parameters, predicts functional outcomes in ischemic stroke patients treated with intravenous tissue plasminogen activator (IV tPA). We assessed the utility of the DRAGON score in predicting functional outcome in stroke patients receiving both IV tPA and endovascular therapy.
Methods:
A retrospective chart review of patients treated at our institution from February 2009 to October 2015 was conducted. All patients with computed tomography angiography (CTA) proven large vessel occlusions (LVO) who underwent intravenous thrombolysis and endovascular therapy were included. Baseline DRAGON scores and modified Rankin Score (mRS) at the time of hospital discharge was calculated. Good outcome was defined as mRS ≤3.
Results:
Fifty-eight patients with LVO of the anterior circulation were studied. The mean DRAGON score of patients on admission was 5.3 (range, 3–8). All patients received IV tPA and endovascular therapy. Multivariate analysis demonstrated that DRAGON scores ≥7 was associated with higher mRS (P < 0.006) and higher mortality (P < 0.0001) compared with DRAGON scores ≤6. Patients with DRAGON scores of 7 and 8 on admission had a mortality rate of 3.8% and 40%, respectively.
Conclusions:
The DRAGON score can help predict better functional outcomes in ischemic stroke patients receiving both IV tPA and endovascular therapy. This data supports the use of the DRAGON score in selecting patients who could potentially benefit from more invasive therapies such as endovascular treatment. Larger prospective studies are warranted to further validate these results.
Keywords: Endovascular thrombectomy, ischemic stroke, large vessel occlusion, tissue plasminogen activator
INTRODUCTION
Intravenous tissue plasminogen activator (IV tPA) has been shown to improve functional outcomes in patients with acute ischemic strokes secondary to large vessel occlusions (LVO).[6] Despite this, IV tPA has a low rate of recanalization, and patients with LVO can further benefit from endovascular therapy.[3] To this end, the DRAGON score was designed to prognosticate patient outcomes after IV tPA therapy, as well as to identify patients who could benefit from further endovascular treatment.[4,12]
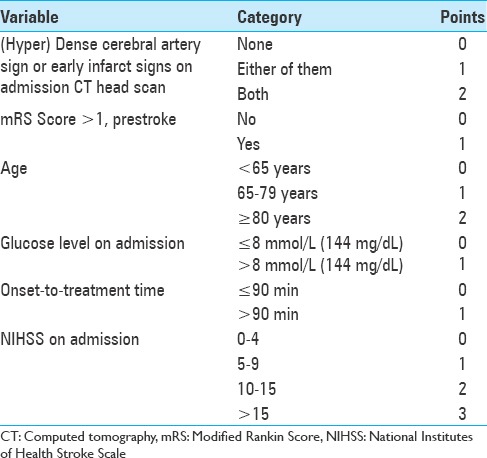
The DRAGON score is a 10-point scoring system based on computed tomography (CT) findings of hypoDensity or a dense MCA sign, prestroke modified Rankin Scale (mRS), Age, Glucose level on admission, Onset-to-treatment time, and initial National Institutes of Health Stroke Score (NIHSS).[12] The score has shown good performance in predicting poor patient outcomes despite administration of IV tPA.[13]
Recent randomized clinical trials using modern endovascular techniques have demonstrated the efficacy of endovascular stroke therapy for treating patients with acute ischemic strokes from LVO.[1,7,11] At present, there is no data to suggest that the DRAGON score can predict functional outcome in stroke patients receiving both IV tPA and endovascular therapy. We sought to assess the utility of the DRAGON score in predicting functional outcome in anterior circulation stroke patients receiving both IV tPA and endovascular therapy.
MATERIALS AND METHODS
Institutional Review Board approval was obtained prior to study initiation. A retrospective chart review was conducted among anterior circulation ischemic stroke patients treated with IV tPA and endovascular therapy, with either the ADAPT technique or stent-triever. The major inclusion criteria were anterior circulation LVO seen on computed tomography angiography (CTA) and age ≥18. Anterior circulation LVO was defined as occlusions of the internal carotid artery (ICA) and M1 and/or M2 segment of the middle cerebral artery (MCA). Baseline DRAGON scores [Table 1], details of the treatment, and clinical outcome at time of hospital discharge were determined.
Table 1.
The DRAGON score
All endovascular interventions were performed on a flat detector-based biplane angiographic system under general anesthesia. Endovascular treatment included mechanical thrombectomy with or without intraarterial thrombolysis (intraarterial tissue plasminogen activator). Mechanical thrombectomy was defined as a stentriever and/or direct aspiration via a large-bore (≥5 Fr) intracranial reperfusion catheter. The degree of recanalization (Thrombolysis in Cerebral Infarction, TICI score) was determined at the end of the case by an endovascular surgeon.
The primary clinical outcome was the modified Rankin Scale (mRS) score at discharge. All mRS scores were reported on physical therapy progress notes and reviewed by stroke neurologists. Good outcome was defined as a mRS score 0–3 and poor outcome as mRS 4–6 (death or dependency).
Univariate analysis for predictors of outcome were determined using the χ2 and Student's t-test. Means were compared using the Student's t-test (two-tailed), and percentages were compared using the χ2 test. P values ≤0.05 were considered significant. Statistical analysis was performed using NCSS Statistical Software Inc V10.0 (Salt Lake City, Utah).
RESULTS
During the study period, a total of 58 patients met the inclusion criteria [Table 2]. The mean patient age was 61.4 years, and the mean National Institutes of Health Stroke Scale (NIHSS) score was 15.6 (range 6–36). In our study population, there were no patients with a DRAGON score of 0–2 and 9–10. There was no significant difference in age or NIHSS between patients with good clinical outcomes (mRS ≤3) and those with poor clinical outcomes (mRS ≥4). Pretreatment DRAGON scores and percentage of good outcomes at discharge are shown in Table 3.
Table 2.
Baseline characteristics of patients
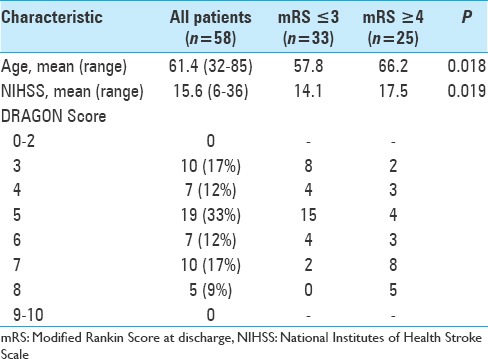
Table 3.
DRAGON Scores, average mRS at discharge, and % good outcome of the 58 patients
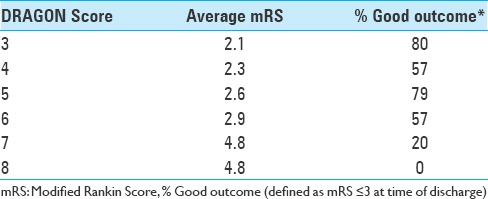
The highest and lowest percentage of good outcomes (mRS ≤ 3) was found in patients with a DRAGON score of 3 and 8, respectively. With increasing DRAGON scores, worse clinical outcome (mRS ≥ 4) was observed [Figure 1]. Mortality rates of 3.8% and 40% were observed in patients with DRAGON scores of 7 and 8, respectively.
Figure 1.
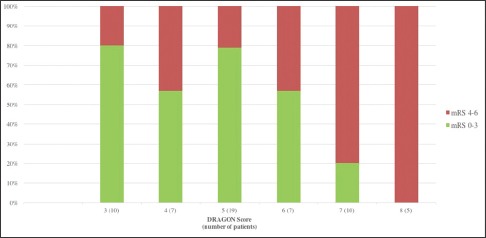
Clinical outcome at discharge according to the DRAGON score
The association between subgroups of DRAGON scores and mRS and mortality rate is shown in Figure 2. DRAGON scores were grouped into high (score of 7–8), intermediate (score of 5–6), and low (score of 3–4) subgroups. High DRAGON scores were associated with higher mRS scores (average 4.8 ± 0.3; P < 0.006) compared with intermediate scores (average mRS 2.6 ± 0.4) and low scores (average mRS 2.2 ± 0.5). High DRAGON scores (7–8) were also associated with higher mortality (40%; P < 0.0001) compared with intermediate and low DRAGON scores (3.8% and 0%, respectively).
Figure 2.
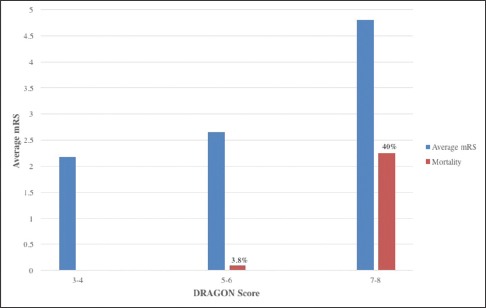
Correlation between DRAGON score and mRS and mortality
DISCUSSION
The DRAGON score was originally proposed as an easy way of identifying patients who should be given additional therapeutic interventions (i.e., endovascular, hypothermia) due to poor functional outcomes after IV tPA.[12] The score takes into account various initial prognosticating factors (age, initial NIHSS, time from onset, CT image findings, and blood sugar levels) and provides relevance based on multivariate logistic regression. Strbian et al. showed the predicative value of their scoring system by demonstrating that patients with DRAGON scores of 8 and 9–10 carried a 70% and 100% proportion of miserable outcomes (mRS ≥5, bedridden, incontinent, requiring constant nursing care, or dead), respectively, compared to patients with lower DRAGON scores.[4] These patients could be suitable for additional rescue therapies such as endovascular intervention.
Although the DRAGON score has been validated by several centers across the world, there are no studies investigating the utility of the score in predicting functional outcomes of patients receiving both IV tPA and endovascular therapy.[2,4,9,13] The results of our study show that patients with a DRAGON score of 7–8 had significantly worse clinical outcomes (mRS ≥4) and higher mortality compared to patients with DRAGON scores ≤6. This demonstrates that the DRAGON score can predict patient clinical outcomes after treatment with IV tPA and endovascular therapy. In addition, the score can be used to select patients who could benefit from endovascular intervention.
There exist a few scoring systems in the literature that have shown promise in predicting the clinical outcome, and thus, appropriately select patients for endovascular therapy. The CTA collateral score, based on the degree of collateral circulation on pretreatment CTA, has been shown to predict smaller infarct volumes and better clinical outcomes in patients after recanalization with endovascular intervention.[5] The Capillary Index Score, based on a preintervention cerebral angiogram, can predict favorable outcomes in patients with ischemic strokes.[8] Similarly, the PRE (Pittsburgh Response to Endovascular therapy) score, which incorporates age, admission NIHSS, and ASPECT score on head CT, can predict outcomes and facilitates selection for patients who could benefit from endovascular intervention.[10]
Compared with other scoring systems, the DRAGON score is (1) fast to obtain, (2) consists of parameters known at admission, and (3) has a low cost; free.[2,4,9,13] Our study results show that the DRAGON score can in fact be applied to endovascular patients who have already received IV tPA.
A few limitations need to be acknowledged in our current study. First, despite controlling for established stroke outcome predictors, we cannot rule out additional baseline confounding variables that can affect patient outcomes. Second, this study uses data from only one center. Our aim was to apply an already established scoring system towards predicting stroke outcomes rather than investigate a novel prognostic tool. Third, as we only included anterior circulation strokes, our study results cannot be applied to posterior circulation strokes. Further data is needed to determine if the DRAGON score can be adapted for posterior circulation strokes.
CONCLUSIONS
The DRAGON score is a fast and easy score to obtain that can predict the functional outcomes of acute ischemic stroke patients treated with IV tPA and endovascular therapy. Larger prospective studies and external validation of the score as it applies to both IV tPA and endovascular therapy is warranted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Arthur Wang, Email: wanga@wcmc.com.
Noorie Pednekar, Email: pednekarn@wcmc.com.
Rachel Lehrer, Email: lehrer@wcmc.com.
Akira Todo, Email: todoa@wcmc.com.
Ramandeep Sahni, Email: sahnir@wcmc.com.
Stephen Marks, Email: markss@wcmc.com.
Michael F. Stiefel, Email: mstiefel@capitalhealth.org.
REFERENCES
- 1.Adeoye O, Hornung R, Khatri P, Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States: A doubling of treatment rates over the course of 5 years. Stroke. 2011;42:1952–5. doi: 10.1161/STROKEAHA.110.612358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baek JH, Kim K, Lee YB, Park KH, Park HM, Shin DJ, et al. Predicting Stroke Outcome Using Clinical versus Imaging-based Scoring System. J Stroke Cerebrovasc Dis. 2015;24:642–8. doi: 10.1016/j.jstrokecerebrovasdis.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke. Stroke. 2010;41:2254–8. doi: 10.1161/STROKEAHA.110.592535. [DOI] [PubMed] [Google Scholar]
- 4.Cooray C, Mazya M, Bottai M, Dorado L, Skoda O, Toni D, et al. External Validation of the ASTRAL and DRAGON Scores for Prediction of Functional Outcome in Stroke. Stroke. 2016;47:1493–9. doi: 10.1161/STROKEAHA.116.012802. [DOI] [PubMed] [Google Scholar]
- 5.Elijovich L, Goyal N, Mainali S, Hoit D, Arthur AS, Whitehead M, et al. CTA collateral score predicts infarct volume and clinical outcome after endovascular therapy for acute ischemic stroke: A retrospective chart review. J Neurointervent Surg. 2016;8:559–62. doi: 10.1136/neurintsurg-2015-011731. [DOI] [PubMed] [Google Scholar]
- 6.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–29. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 7.IST-3 collaborative group, Sandercock P, Wardlaw JM, Lindley RI, Dennis M, Cohen G, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): A randomised controlled trial. Lancet. 2012;379:2352–63. doi: 10.1016/S0140-6736(12)60768-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Labeyrie PE, Redjem H, Blanc R, Labeyrie MA, Bartolini B, Ciccio G, et al. The Capillary Index Score before thrombectomy: An angiographic correlate of favorable outcome. J Neurointervent Surg 2015. 2015:1–4. doi: 10.1136/neurintsurg-2015-011922. [DOI] [PubMed] [Google Scholar]
- 9.Ovesen C, Christensen A, Nielsen JK, Christensen H. External validation of the ability of the DRAGON score to predict outcome after thrombolysis treatment. J Clin Neurosci. 2013;20:1635–6. doi: 10.1016/j.jocn.2013.04.023. [DOI] [PubMed] [Google Scholar]
- 10.Rangaraju S, Aghaebrahim A, Streib C, Sun CH, Ribo M, Muchada M, et al. Pittsburgh Response to Endovascular therapy (PRE) score: Optimizing patient selection for endovascular therapy for large vessel occlusion strokes. J Neurointervent Surg. 2015;7:783–8. doi: 10.1136/neurintsurg-2014-011351. [DOI] [PubMed] [Google Scholar]
- 11.Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007;38:948–54. doi: 10.1161/01.STR.0000257304.21967.ba. [DOI] [PubMed] [Google Scholar]
- 12.Strbian D, Meretoja A, Ahlhelm FJ, Pitkäniemi J, Lyrer P, Kaste M, et al. Predicting outcome of IV thrombolysis-treated ischemic stroke patients: The DRAGON Score. Neurology. 2012;78:427–32. doi: 10.1212/WNL.0b013e318245d2a9. [DOI] [PubMed] [Google Scholar]
- 13.Strbian D, Seiffge DJ, Breuer L, Numminen H, Michel P, Meretoja A, et al. Validation of the DRAGON Score in 12 Stroke Centers in Anterior and Posterior Circulation. Stroke. 2013;44:2718–21. doi: 10.1161/STROKEAHA.113.002033. [DOI] [PubMed] [Google Scholar]


