Abstract
Since its initial outbreak in 1976, Ebola virus disease (EVD) has affected thousands of people, causing severe illness with high mortality rates. In the absence of a vaccine or effective specific treatment, as well as the lack of early diagnostic and detective methods, the EVD outbreak has generated a significant worldwide health concern. Insufficient health-care system resources, deficient infection control measures, and the shortage of appropriate personal protective equipment acted as amplifiers of the outbreak extension, especially in poorly resourced and unprepared communities. Operating on the frontlines, health-care workers must be familiar, not only with the identification of the disease, but also with the ability to protect themselves and initiate the appropriate response. This review seeks to provide essential information required to identify and manage the disease, with an emphasis on pathogenesis, transmission, diagnosis, treatment, and prevention. We conducted a literature search in MEDLINE/PubMed and Google Scholar using the following keywords: “Ebola, Ebola virus disease, Hemorrhagic Fever, Outbreak.” We included all types of publications. To augment our study, we searched the reference lists of identified reviews.
Key words: Ebola (MeSH), Ebola vaccines (MeSH), Ebola virus (MeSH), hemorrhagic fever
INTRODUCTION
On June 2016, the World Health Organization (WHO) declared the end of the most recent outbreak of Ebola virus disease (EVD) in Guinea and Liberia.[1] The EVD outbreak in West Africa was a global health threat resulting in 28,616 total suspected, probable, and confirmed cases with >11,310 total deaths recorded since December 2013 according to the WHO situation report.[1]
The global concerns are justified by the challenge of early diagnosis, the lack of specific treatment and vaccines, the endemic nature of poor communities, and the high number of fatalities.[2,3] However, many epidemiologists view EVD as a challenge to the health-care system rather than a scientific challenge. In favor of this view is the wide variation in the mortality rate ranging from 20% to 80% in developed and developing countries, respectively.[4]
Ebola virus (EV) was named after a river in Northwestern Zaire, now the Democratic Republic of Congo, where the first documented outbreak emerged in 1976.[3,5,6] The virus, like Marburg virus, is an enveloped, nonsegmented, negative sense, single-stranded RNA virus. Together, they form the genera of Filoviruses. EV has five distinct species, namely, Zaire, Sudan, Tai forest, Bundibugyo, and Reston, which greatly differ in their characteristics and fatality.[7] Mortality rates range from 80% with Zaire species, the causative agent of the recent outbreak in West Africa, to 40% with Bundibugyo species. However, most of the past outbreaks were caused by the Sudan species. Reston species is the only identified Asian species of EV with no human cases reported.[8]
Since 1976, many outbreaks occurred in Sudan, central and West Africa. Nevertheless, the recent outbreak, hitting three countries simultaneously; Guinea, Liberia, and Sierra Leone, stands out for the longest duration, the largest numbers infected, and its relatively high fatality rate.[9] In addition, it is the first outbreak in a densely populated urban area with many cases in the capitals of the affected countries.[10] Once it crossed the borders, affecting the United States and Europe,[11,12] with four U.S citizens infected,[13] EVD gained much more attention. On August 2014, the WHO declared this outbreak as a Public Health Emergency of International Concern (PHEIC) seeking greater efforts to fight against this fatal disease.
We conducted a literature search in MEDLINE/PubMed and Google Scholar using the following keywords: “Ebola, EVD, Hemorrhagic Fever, Outbreak.” Through this review, we aim at providing simple, yet comprehensive overview of EVD with an emphasis on pathogenesis, transmission, diagnosis, treatment, and prevention. Because they operate on the frontlines, health-care workers' (HCWs) preparedness is essential to prevent and manage the next outbreaks, especially in resource-limited communities.
PATHOGENESIS
Definitive pathogenesis of EVD is still unknown due to the lethal nature of the virus and rarity of human studies.[14] Concurrent transmission of EVD occurs through two main routes; animal-to-human and human-to-human contacts.[3,15] Animal-to-human transmission occurs through handling bush meat[10,16] or direct contact with infected nonhuman primates[17] (such as chimpanzees, gorillas, fruit bats,[18] and monkeys[10]). However, human-to-human transmission is the main route and occurs through intimate contact with infected cases (i.e., family-based transmission) or exposure to the blood and other body fluids of patients exhibiting clinical manifestations, or even after the handling of the dead bodies. Blood, semen, and vomitus are the most infectious body fluids.[19] Despite its detection in breast milk, breastfeeding is not a confirmed route for EV transmission, which is the case for droplet, air, and mosquito and insect bites as well.[10]
On initial infection, EV invades through breaks in the skin, causing cells such as monocytes, macrophages, and dendritic cells to modulate their genes, undergo apoptosis, and release viral particles to extracellular tissue. Viral particles migrate from the infected cells to the regional lymph nodes causing lymphadenopathy. Bloodstream dissemination to the liver and spleen induces an active inflammatory response[4] associated with hepatocellular necrosis and lymphopenia. EV then induces release of pro-inflammatory mediators such as cytokines (interfe1 interleukin) and chemokines that cause dysregulation of the immune system. Released cytokines and tumor necrosis factor-α from infected macrophages disturb the vasculature system integrity resulting in disseminated intravascular coagulation (DIC) and multiple organ failure.[16]
DIAGNOSIS
The early clinical diagnosis of EVD is challenging due to the vague presentation that usually overlaps with multiple differential diagnoses, including malaria, dengue fever, typhoid fever, meningococcemia, and other bacterial infections.[20] The presentation of the disease usually starts after an incubation period that ranges from 3 to 21 days with an average 12.7 ± 4.3 days, according to Eichner et al.[21] The disease itself usually lasts from 4 to 15 days.[22]
Patients usually develop symptoms abruptly in three phases [Table 1]. Most cases initially present with sudden, nonspecific symptoms of fever, chills, headache, myalgia, and general malaise for a few days. These symptoms are usually followed within the first week by progressive gastrointestinal symptoms such as anorexia, nausea, and abdominal discomfort followed by excessive watery diarrhea and vomiting which may lead to severe fluid loss and intravascular volume depletion. During the second phase, the patient either recovers or deteriorates to the third stage, in which the patient may develop neurological symptoms and collapse.[23]
Table 1.
Symptoms and signs of Ebola virus disease
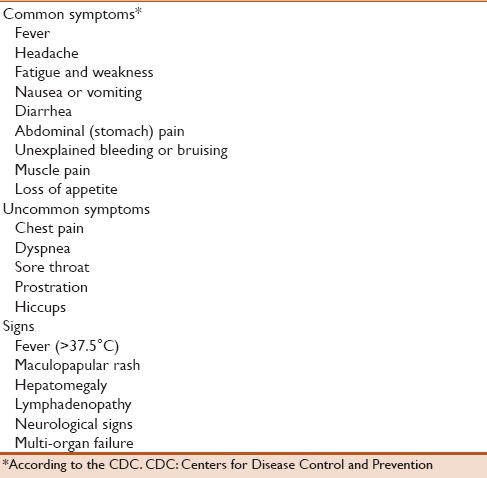
In the 2014 outbreak, the most commonly reported symptoms were fever (87.1%), vomiting (67.6%), fatigue (76.4%), diarrhea (65.6%), loss of appetite (64.5%), headache (53.4%), and abdominal pain (44.3%).[24] Bleeding (in the form of petechiae, ecchymosis, oozing from venipuncture sites, pregnancy-related hemorrhage, and/or mucosal hemorrhage) was detected in 30%–36% of cases in previous outbreaks.[3] However, it was reported in only 18% of the recent outbreaks with blood-in-stool presentation in about 6% of cases.[24] Major bleeding occurs late in the course of the disease in most cases.
Physical examination of patients with suspected EV infection should be done with precautionary isolation procedures and personal protective equipment (PPE) usage. It should include assessment of vital data and other possible findings such as maculopapular rash, bleeding, hepatomegaly, lymphadenopathy, and neurological signs.[14] Fever (>37.5°C) is usually a presenting sign and should raise concern in any patient with suspected epidemiological risks.[24,25] However, normal temperature or even hypothermia may occur, especially in late stages.[6,26] Pulse–temperature dissociation has been noted in the prior and recent outbreaks. Bradycardia is usually present in the initial stages of the disease, in contrast to tachycardia which occurs later in the fatal infections. Hypotension is usually present in the preterminal and shock stages. Tachypnea occurs in the severe infection, and it is explained by the respiratory compensation of the metabolic acidosis rather than the infection itself.[6]
A nonpruritic, erythematous, maculopapular rash usually develops early in 25%–52% of patients by days 5–7 that involves neck, trunk, and arms.[6,27,28] However, in the 2014 outbreak, it was not a prominent feature (5% of patients).[3] It may start as a focal lesion and then become diffuse and confluent. Tender hepatomegaly and lymphadenopathy are rarely reported.[3]
Neurological signs such as confusion, depressed consciousness, and seizures are rare,[14] and may be due to encephalitis, metabolic problems, or sepsis-induced encephalopathy.[29,30] Multi-organ failure (acute kidney injury, pancreatitis, acute adrenal failure, and hepatic failure) and shock are common in advanced infections due to massive fluid loss and sepsis.[14] Patients die typically between days 6 and 16 after the onset of symptoms.[31]
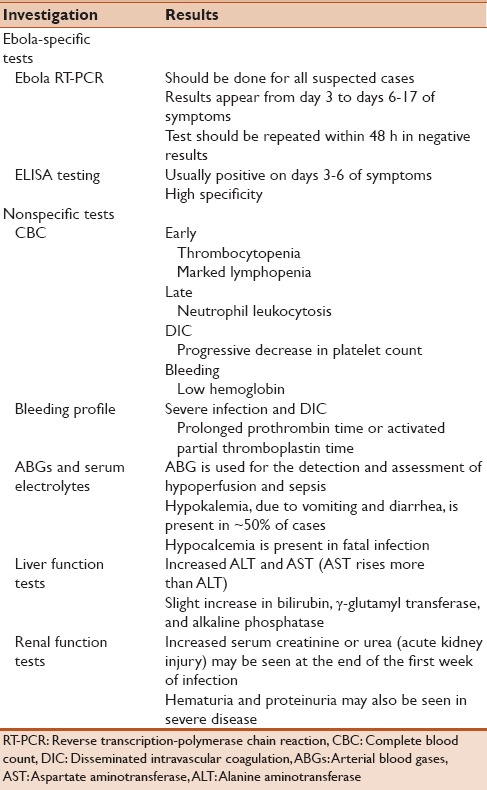
Regarding laboratory diagnosis [Table 2],[20] it is important to confirm infection with EV due to the clinical similarity in symptoms with other endemic diseases. However, laboratory tests take time and are not specific and thus need to be correlated with the clinical findings.[20] Laboratory diagnosis of the virus can be achieved through assessing two points; host-specific immune responses to the virus and detection of viral particles or their components in blood after the onset of symptoms. While viral particles can be detected by reverse transcription-polymerase chain reaction in the blood after 3–10 days of symptoms, it may take months to be detected in other body fluids such as semen. Negative tests should be repeated after 48 h to avoid early false-negative results. Testing for malaria is routine for any suspected case.[20,32]
Table 2.
Specific and nonspecific investigations of Ebola virus disease
PREVENTION
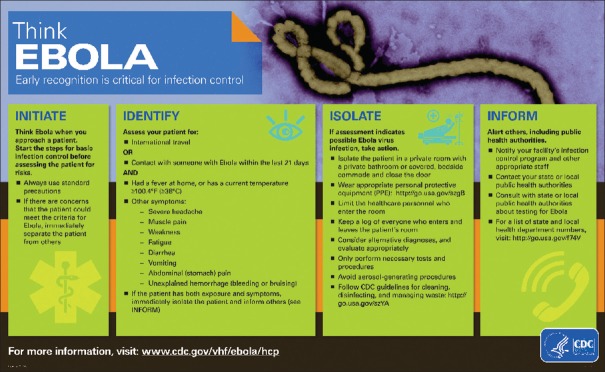
The lack of specific treatment for EVD makes prevention the cornerstone in the fight against Ebola. Immediate isolation of suspected cases with prompt notification of health authorities is very important before proceeding in any investigation to decrease transmission to HCWs and other patients.[14,33] Figure 1 demonstrates “Think Ebola” which is a tool, developed by the Centers for Disease Control and Prevention (CDC), to help HCWs to early diagnose and report suspected cases of Ebola.
Figure 1.
The Centers for Disease Control and Prevention's four steps to early diagnose the cases of Ebola virus disease
During the 2014 outbreak, 509 of 874 infected HCWs died from the virus.[34] Therefore, strict infection control measures by HCWs should be carried out. They should avoid any direct contact with the patients' bodies or their fluids without using PPE. In addition, it is important to maintain close monitoring of individuals who have been exposed to patients with EV to identify any symptom or sign as early as possible.[35]
Once the diagnosis of EVD is confirmed, HCWs should follow the guidelines of the CDC and WHO while managing their patients through isolation in special rooms, hand hygiene, standard contact and droplet precautions, and the appropriate use of PPE.[36]
Women with suspected or confirmed Ebola should avoid close contact with their children, including breastfeeding, especially if the infant can receive adequate care and nutrition in other ways according to the CDC. In resource-limited settings, as there is no clear evidence about virus transmission through breast milk, it is important to weigh the risk of virus transmission against the risk of malnutrition development if there are no other safe alternative feeding options.[37]
Regarding sexual transmission, the CDC and WHO advise against sexual activities for EVD survivors until their semen has twice tested negative. This is because the virus may persist in body fluids, even after its disappearance from the blood. If abstinence is not possible, a condom can be used.[38]
Unfortunately, to date, there are no Food and Drug Administration (FDA)-approved vaccines to prevent the spread of Ebola.[39] Experimental vaccines have proved their success in protecting laboratory primates against lethal EV challenge. These include cAd3-ZEBOV (chimpanzee-adenovirus vector type three encoding for Ebola glycoprotein [GP]), rVSV-ZEBOV (recombinant vesicular stomatitis vector encoding for Ebola GP), recombinant adenovirus type five vector encoding for Ebola Zaire and Sudan GP, a virus-like particle vaccine, and recombinant adenovirus alone.[40] Multiple human trials have been initiated in many countries including Africa. However, the WHO expert panel in September 2014 informed that cAd3-ZEBOV and rVSV-ZEBOV are the most advanced candidates to fight the West African outbreak. Studies on healthy volunteers to evaluate cAd3-ZEBOV and rVSV-ZEBOV vaccines indicated that both low and high doses were immunogenic and relatively safe.[41] During 2014 outbreak, rVSV-ZEBOV vaccine was administered as postexposure prophylaxis to four HCWs, and none of them developed the disease.[42] In addition, it was given to another six cases in West Africa, and all patients experienced self-limited symptoms and did not develop the disease.[43]
TREATMENT
The absence of FDA-approved drugs for EVD amplifies the role of prevention and early detection of cases, especially in affected areas where advanced care is not readily available. The first step in the management of suspected cases is appropriate isolation in Ebola Treatment Centers (ETCs) with strict infection control measures by trained teams followed by screening all contacts of the suspected case.[20] In ETCs, the mainstay in the treatment of EVD is supportive and symptomatic in nature, gaining time for an appropriate immune response to occur. Continuous monitoring of vital signs (temperature, respiratory rate, pulse and blood pressure), urine output, and serum electrolytes is essential. Invasive diagnostic or therapeutic maneuvers should be avoided when possible.[4,44]
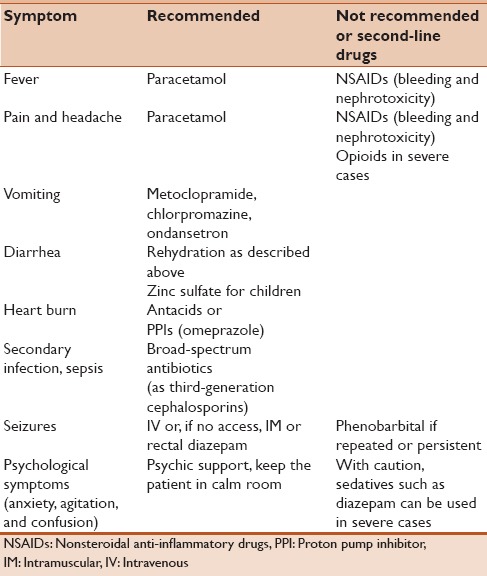
Patients mostly die from dehydration and electrolyte imbalance caused by vomiting and diarrhea. Rehydration, by oral rehydration solution (ORS) or intravenous (IV) fluids, with daily electrolyte monitoring can prevent vascular collapse and maintain electrolyte balance. Volume replacement is determined based on the degree of dehydration assessed by clinical signs and by following the plans A, B, and C for mild, moderate, and severe dehydration, respectively. ORS is commonly preferred in patients with no or mild dehydration. For IV fluids, lactated Ringer's solution is preferred to normal saline, and it is associated with less mortality. Follow-up can be done through assessment of clinical signs of dehydration, fluid input and output, serum electrolytes, and lactate levels.[4,45] Table 3 shows a simplified guide for symptomatic treatment of EVD based on the WHO and Canadian Critical Care guidelines.
Table 3.
Simplified guide for symptomatic treatment of Ebola virus disease
Throughout the period of care, monitoring for EVD complications with prompt treatment in tertiary care centers is of top priority. Renal insufficiency is suspected in anuric patients and is confirmed by laboratory tests. Renal replacement therapy should be promptly started. Although uncommon, major bleeding can be managed by whole blood transfusion. Septic shock needs close monitoring of vital signs, central venous pressure, and urine output in concordance with oxygen flow, IV fluids, and broad-spectrum antibiotics. DIC management should be customized for each patient with plasma/clotting factor transfusion recommended only in patients with active bleeding.[21,45]
Antiviral drugs, such as interferon and ribavirin, were investigated for a potential role in EVD. However, their use in EVD patients remains unclear while the current studies continue to explore their potential benefits.[46] Convalescent-phase plasma/blood transfusion with whole blood collected from patients recovered from EVD was approved by the WHO as a treatment choice in the recent outbreak. Theoretically, the ready-made antibodies could attack the viral particles and eliminate the disease from the current patient. It was reported to reduce mortality to 12% in eight cases during the Kikwit epidemic in 1995.[47,48] However, the practice remains controversial and requires further investigation.
There are huge rising efforts to develop specific EV therapy. Among dozens of tested drugs, ZMapp and TKM-Ebola are the most promising. ZMapp is a combination of three monoclonal antibodies that target specific viral GPs, while TKM-Ebola interferes with viral RNA polymerase L and two other proteins essential for replication.[49] Both drugs have shown effectiveness in animals and nonhuman primates. ZMapp was provided to two American patients during the recent outbreak with promising results.[50] However, none of the potential therapies are even close to FDA approval. Extensive studies on humans involving close ethical consideration will need to be carried out to address the safety and efficacy of these potential new drugs.[20,51]
CONCLUSION
During the past 3 years, multiple efforts have been done in the battle against EVD in West Africa. Despite the success to put an end to the current outbreak, it may not be the last outbreak. It is imperative that more efforts are required to develop vaccines and specific treatments to prevent future threats. However, the fact that the trials to develop such vaccines or treatments are still far away necessitates emergency preparedness for early detection and control.
Operating on the frontlines, HCWs are considered the master players in the prevention of the onward spread of the epidemic. Establishing good clinical knowledge about the disease and infection control measures is the main weapon to fight against the next outbreaks. Therefore, it is necessary to develop training programs to increase awareness about the diseases among HCWs, especially in the afflicted areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Ebola Virus Situation Report. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 2.Leroy EM, Gonzalez JP, Baize S. Ebola and Marburg haemorrhagic fever viruses: Major scientific advances, but a relatively minor public health threat for Africa. Clin Microbiol Infect. 2011;17:964–76. doi: 10.1111/j.1469-0691.2011.03535.x. [DOI] [PubMed] [Google Scholar]
- 3.Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet. 2011;377:849–62. doi: 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fowler RA, Fletcher T, Fischer WA, 2nd, Lamontagne F, Jacob S, Brett-Major D, et al. Caring for critically ill patients with ebola virus disease. Perspectives from West Africa. Am J Respir Crit Care Med. 2014;190:733–7. doi: 10.1164/rccm.201408-1514CP. [DOI] [PubMed] [Google Scholar]
- 5.Feldmann H, Jones S, Klenk HD, Schnittler HJ. Ebola virus: From discovery to vaccine. Nat Rev Immunol. 2003;3:677–85. doi: 10.1038/nri1154. [DOI] [PubMed] [Google Scholar]
- 6.Kortepeter MG, Bausch DG, Bray M. Basic clinical and laboratory features of filoviral hemorrhagic fever. J Infect Dis. 2011;204(Suppl 3):S810–6. doi: 10.1093/infdis/jir299. [DOI] [PubMed] [Google Scholar]
- 7.Ramanan P, Shabman RS, Brown CS, Amarasinghe GK, Basler CF, Leung DW. Filoviral immune evasion mechanisms. Viruses. 2011;3:1634–49. doi: 10.3390/v3091634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feldmann H. Ebola – A growing threat? N Engl J Med. 2014;371:1375–8. doi: 10.1056/NEJMp1405314. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Ebola Response Roadmap Situation Report. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 10.Dixon MG, Schafer IJ. Centers for Disease Control and Prevention (CDC). Ebola viral disease outbreak – West Africa, 2014. MMWR Morb Mortal Wkly Rep. 2014;63:548–51. [PMC free article] [PubMed] [Google Scholar]
- 11.Bausch DG, Rojek A. West Africa 2013: Re-examining Ebola. Microbiol Spectr. 2016;4:3. doi: 10.1128/microbiolspec.EI10-0022-2016. [DOI] [PubMed] [Google Scholar]
- 12.Parra JM, Salmerón OJ, Velasco M. The first case of Ebola virus disease acquired outside Africa. N Engl J Med. 2014;371:2439–40. doi: 10.1056/NEJMc1412662. [DOI] [PubMed] [Google Scholar]
- 13.Whiteside LK, Fernandez R, Bammer J, Nichol G. Perception of the risks of Ebola, enterovirus-E68 and influenza among emergency department patients. West J Emerg Med. 2016;17:391–5. doi: 10.5811/westjem.2016.5.29981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Ebola Virus Disease. 2016. [Last accessed on 2016 Sep 01]. Available from: http://www.who.int/mediacentre/factsheets/fs103/en/
- 15.Osterholm MT, Moore KA, Kelley NS, Brosseau LM, Wong G, Murphy FA, et al. Transmission of Ebola viruses: What we know and what we do not know. MBio. 2015;6:e00137. doi: 10.1128/mBio.00137-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ansari AA. Clinical features and pathobiology of Ebolavirus infection. J Autoimmun. 2014;55:1–9. doi: 10.1016/j.jaut.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 17.Olival KJ, Hayman DT. Filoviruses in bats: Current knowledge and future directions. Viruses. 2014;6:1759–88. doi: 10.3390/v6041759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Marburg Haemorrhagic Fever. 2012. [Last accessed on 2016 Sep 01]. Available from: http://www.who.int/mediacentre/factsheets/fs_marburg/en/
- 19.World Health Organization. What We Know About Transmission of the Ebola Virus among Humans. 2014. [Last accessed on 2016 Sep 01]. Available from: http://www.who.int/mediacentre/news/ebola/06-october-2014/en/
- 20.Beeching NJ, Fenech M, Houlihan CF. Ebola virus disease. BMJ. 2014;349:g7348. doi: 10.1136/bmj.g7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eichner M, Dowell SF, Firese N. Incubation period of ebola hemorrhagic virus subtype zaire. Osong Public Health Res Perspect. 2011;2:3–7. doi: 10.1016/j.phrp.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chippaux JP, Boyer LV, Alagón A. Post-exposure treatment of Ebola virus using passive immunotherapy: Proposal for a new strategy. J Venom Anim Toxins Incl Trop Dis. 2015;21:3. doi: 10.1186/s40409-015-0003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chertow DS, Kleine C, Edwards JK, Scaini R, Giuliani R, Sprecher A. Ebola virus disease in West Africa – Clinical manifestations and management. N Engl J Med. 2014;371:2054–7. doi: 10.1056/NEJMp1413084. [DOI] [PubMed] [Google Scholar]
- 24.WHO Ebola Response Team. Ebola virus disease in West Africa – The first 9 months of the epidemic and forward projections. N Engl J Med. 2014;371:1481–95. doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dananché C, Bénet T, Vanhems P. Ebola: Fever definitions might delay detection in non-epidemic areas. Lancet. 2014;384:1743. doi: 10.1016/S0140-6736(14)61787-6. [DOI] [PubMed] [Google Scholar]
- 26.Mupere E, Kaducu OF, Yoti Z. Ebola haemorrhagic fever among hospitalised children and adolescents in Northern Uganda: Epidemiologic and clinical observations. Afr Health Sci. 2001;1:60–5. [PMC free article] [PubMed] [Google Scholar]
- 27.Bwaka MA, Bonnet MJ, Calain P, Colebunders R, De Roo A, Guimard Y, et al. Ebola hemorrhagic fever in Kikwit, Democratic Republic of the Congo: Clinical observations in 103 patients. J Infect Dis. 1999;179(Suppl 1):S1–7. doi: 10.1086/514308. [DOI] [PubMed] [Google Scholar]
- 28.Formenty P, Hatz C, Le Guenno B, Stoll A, Rogenmoser P, Widmer A. Human infection due to Ebola virus, subtype Côte d'Ivoire: Clinical and biologic presentation. J Infect Dis. 1999;179(Suppl 1):S48–53. doi: 10.1086/514285. [DOI] [PubMed] [Google Scholar]
- 29.Denizot M, Neal JW, Gasque P. Encephalitis due to emerging viruses: CNS innate immunity and potential therapeutic targets. J Infect. 2012;65:1–16. doi: 10.1016/j.jinf.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 30.Sonneville R, Verdonk F, Rauturier C, Klein IF, Wolff M, Annane D, et al. Understanding brain dysfunction in sepsis. Ann Intensive Care. 2013;3:15. doi: 10.1186/2110-5820-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Ebola Virus Disease Information for Clinicians in US Healthcare Settings. 2016. [Last accessed on 2016 Sep 01]. Available from: https://www.cdc.gov/vhf/ebola/healthcare-us/preparing/clinicians.html .
- 32.World Health Organization. Laboratory Guidance for the Diagnosis of Ebola Virus Disease: Interim Recommendations. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 33.Fletcher TE, Brooks TJ, Beeching NJ. Ebola and other viral haemorrhagic fevers. BMJ. 2014;349:g5079. doi: 10.1136/bmj.g5079. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Think Ebola: Early Recognition is Critical for Infection Control. 2016. [Last accessed on 2016 Sep 01]. Available from: http://www.cdc.gov/vhf/ebola/healthcare-us/evaluating-patients/think-ebola.html .
- 35.Centers for Disease Control and Prevention. Interim U.S. Guidance for Monitoring and Movement of Persons with Potential Ebola Virus Exposure. 2015. [Last accessed on 2016 Sep 01]. Available from: https://www.cdc.gov/vhf/ebola/exposure/monitoring-and-movement-of-persons-with-exposure.html .
- 36.Centers for Disease Control and Prevention. Infection Prevention and Control Recommendations for Hospitalized Patients under Investigation (PUIs) for Ebola Virus Disease (EVD) in U.S. Hospitals. 2015. [Last accessed on 2016 Sep 01]. Available from: http://www.cdc.gov/vhf/ebola/healthcare-us/hospitals/infection-control.html .
- 37.Centers for Disease Control and Prevention. Recommendations for Breastfeeding/Infant Feeding in the Context of Ebola. 2016. [Last accessed on 2016 Sep 01]. Available from: http://www.cdc.gov/vhf/ebola/hcp/recommendations-breastfeeding-infant-feeding-ebola.html .
- 38.World Health Organization. Sexual and Reproductive Health Interim Advice on the Sexual Transmission of the Ebola Virus Disease. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 39.Galvani AP, Ndeffo-Mbah ML, Wenzel N, Childs JE. Ebola vaccination: If not now, when? Ann Intern Med. 2014;161:749–50. doi: 10.7326/M14-1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, et al. Chimpanzee adenovirus vaccine generates acute and durable protective immunity against ebolavirus challenge. Nat Med. 2014;20:1126–9. doi: 10.1038/nm.3702. [DOI] [PubMed] [Google Scholar]
- 41.Ledgerwood JE, DeZure AD, Stanley DA, Novik L, Enama ME, Berkowitz NM, et al. Chimpanzee adenovirus vector ebola vaccine – Preliminary report. N Engl J Med. 2014 doi: 10.1056/NEJMoa1410863. [In press] [DOI] [PubMed] [Google Scholar]
- 42.Jacobs M, Aarons E, Bhagani S, Buchanan R, Cropley I, Hopkins S, et al. Post-exposure prophylaxis against Ebola virus disease with experimental antiviral agents: A case-series of health-care workers. Lancet Infect Dis. 2015;15:1300–4. doi: 10.1016/S1473-3099(15)00228-5. [DOI] [PubMed] [Google Scholar]
- 43.Wong KK, Davey RT, Hewlett AL, Kraft CS, Mehta AK, Mulligan MJ, et al. Use of post-exposure prophylaxis after occupational exposure to Zaire ebolavirus. Clin Infect Dis. 2016;63:376–9. doi: 10.1093/cid/ciw256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ebola Clinical Care Guidelines – A Guide for Clinicians in Canada. Ontario, Canada: Canadian Critical Care Society; 2014. Canadian Critical Care Society; pp. 1–62. [Google Scholar]
- 45.World Health Organization. Clinical Management of Patients with Viral Haemorrhagic Fever: A Pocket Guide for Front-line Health Workers. Geneva, Switzerland: World Health Organization; 2016. [Google Scholar]
- 46.World Health Organization. Potential Ebola Therapies and Vaccines. 2014. [Last accessed on 2016 Sep 01]. Available from: http://www.who.int/csr/resources/publications/ebola/potential-therapies-vaccines/en/
- 47.World Health Organization. Use of Convalescent Whole Blood or Plasma Collected from Patients Recovered from Ebola Virus Disease for Transfusion, as an Empirical Treatment during Outbreaks. 2014. [Last accessed on 2016 Sep 01]. Available from: http://www.apps.who.int/iris/handle/10665/135591 .
- 48.Mupapa K, Massamba M, Kibadi K, Kuvula K, Bwaka A, Kipasa M, et al. Treatment of Ebola hemorrhagic fever with blood transfusions from convalescent patients. International Scientific and Technical Committee. J Infect Dis. 1999;179(Suppl 1):S18–23. doi: 10.1086/514298. [DOI] [PubMed] [Google Scholar]
- 49.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature. 2014;514:47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lyon GM, Mehta AK, Varkey JB, Brantly K, Plyler L, McElroy AK, et al. Clinical care of two patients with Ebola virus disease in the United States. N Engl J Med. 2014;371:2402–9. doi: 10.1056/NEJMoa1409838. [DOI] [PubMed] [Google Scholar]
- 51.Bishop BM. Potential and emerging treatment options for Ebola virus disease. Ann Pharmacother. 2015;49:196–206. doi: 10.1177/1060028014561227. [DOI] [PubMed] [Google Scholar]
- 52.Sridhar S, Brouqui P, Fontaine J, Perivier I, Ruscassier P, Gautret P, et al. Risk perceptions of MSF healthcare workers on the recent Ebola epidemic in West Africa. New Microbes New Infect. 2016;12:61–8. doi: 10.1016/j.nmni.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]