Abstract
Background:
Inconsistent evidence exists regarding the strength, direction, and moderators in the relationship between obesity and psychiatric disorders.
Aim:
This study aims to summarize the evidence on the association between psychiatric illness and obesity with particular attention to the strength and direction of association and also the possible moderators in each postulated link.
Materials and Methods:
Systematic electronic searches of MEDLINE through PubMed, ScienceDirect, PsycINFO, and Google Scholar were carried out from inception till October 2016. Generated abstracts were screened for eligibility to be included in the review. Study designs that evaluated the strength of relationship between obesity and psychiatric disorders were included in the study. Quality assessment of included studies was done using the Newcastle–Ottawa checklist tool.
Results:
From a total of 2424 search results, 21 eligible articles were identified and reviewed. These included studies on obesity and depression (n = 15), obesity and anxiety (four) and one each on obesity and personality disorders, eating disorder (ED), attention deficit hyperactivity disorder, and alcohol use. Maximal evidence existed for the association between depression and obesity with longitudinal studies demonstrating a bidirectional link between the two conditions. The odds ratios (ORs) were similar for developing depression in obesity (OR: 1.21–5.8) and vice versa (OR: 1.18–3.76) with a stronger association observed in women. For anxiety disorders, evidence was mostly cross-sectional, and associations were of modest magnitude (OR: 1.27–1.40). Among other disorders, obesity, and EDs appear to have a close link (OR: 4.5). Alcohol use appears to be a risk factor for obesity and not vice versa but only among women (OR: 3.84).
Conclusion:
Obesity and depression have a significant and bidirectional association. Evidence is modest for anxiety disorders and inadequate for other psychiatric conditions. Gender appears to be an important mediator in these relationships.
KEY WORDS: Anxiety, depression, metabolic syndrome, obesity, psychiatry, review
Introduction
As per the World Health Organization (WHO) global estimates in 2014, almost 40% of adults are overweight (body mass index [BMI] ≥25 kg/m2) with nearly a third of them obese (BMI ≥30 kg/m2).[1] India, with its rapid urbanization and changing socioeconomic landscape, is experiencing an increase in obesity rates among its population.[2,3,4] In a recent nationally representative study, an estimated 135 million people were found to be suffering from generalized obesity and high prevalence rates were noted in both rural and urban areas.[5] This rising trend has also been reflected in childhood obesity with several Indian and international studies showing alarmingly increasing trends over the last decade.[6,7,8,9] These figures make it clear that obesity is assuming epidemic proportions cutting across age, sociocultural and ethnic boundaries, thus becoming a significant public health issue.
Although the physical comorbidity burden in obesity is well established,[10,11] its relation to mental health is relatively less explored. In the last couple of decades, however, evidence is gradually accumulating on the association between various psychiatric disorders and obesity, particularly among those seeking treatment for the same.[12,13,14] Despite this, knowledge gaps exist with regard to the strength and the direction of the association between obesity and various psychiatric conditions. Further, given the methodological differences between the studies, there is a need to synthesize the available evidence in this area so that clinicians and researchers have a better understanding of the links between obesity and psychiatric disorders. This has the potential to inform clinical evaluation and identify further research targets in this area such as the possible neurobiological links between obesity and psychiatric disorders. From a management perspective, it has been shown that early identification and management of common psychiatric problems can optimize outcomes among obesity patients presenting for surgical treatment. Hence, practicing clinicians need to be well informed about the same.
With this background, we carried out the present systematic review with the objective of summarizing the available evidence on the association between psychiatric illness and obesity with particular attention to the strength and direction of association and also the possible moderators in each postulated link. In this context, moderators refer to those variables that may influence the strength of relationship between two other variables (here, referring to psychiatry and obesity).
Materials and Methods
Inclusion and exclusion criteria
Using the patient, intervention, comparison, outcomes, and study design criteria, all studies that assessed the association between obesity and psychiatric disorders or vice versa were included provided they met the following criteria:
The study provided a quantitative measure of association between obesity (explanatory variable) and specific psychiatric illness (outcome variable) or vice versa. Psychiatric outcomes should, necessarily, have been mentioned as “risk” to be included as it provides a quantitative estimate of the strength of the association
Studies done in populations with no prior medical comorbidities such as diabetes. This was done as chronic medical illness is a major confounder in the relationship between obesity and psychiatric illness[15,16]
Studies that did not use alternate definitions of obesity such as abdominal obesity/sarcopenic obesity
Studies published in English language peer-reviewed journals.
Search strategy and study selection
Electronic searches of MEDLINE through PubMed, ScienceDirect, PsycINFO, and Google Scholar were carried out from inception till October 2016. Our aim as stated above was to identify studies which directly looked into the association between psychiatric illness and obesity. “Psychiatric illness” was defined as any International Classification of Diseases, Tenth Edition coded category between F00 and F99. Obesity was defined as per the WHO definition based on BMI ≥30 kg/m2.[1] For this review, literature search was carried out using random combinations of the following keywords – “obesity”/”overweight”/”weight gain”/”weight changes” and “psychiatry”/”psychiatric illness”/”depression”/”anxiety”/”eating disorders (EDs)”/”binge eating”/”bulimia”/”personality disorders (PDs)”/”substance use”/”alcohol”/”nicotine”/”cannabis.” The initial search was carried out in PubMed, after which a similar search was done in other search engines to identify relevant articles. A supplemental Google Search using random combinations of the above terms was also done to further comb the extant literature. There was no restriction on the date of publication.
The titles and abstracts of the studies that met broad inclusion criteria were examined independently by the two authors (VM and TMR). In case of inadequate information in the abstract, both the authors independently scrutinized the full texts of potentially relevant articles to select those that met the inclusion criteria for the present review. Any disagreements at this stage (e.g., which assessment point to choose in cohorts that were analyzed repeatedly) were sorted out through mutual discussion until consensus. Following this, consolidated list of abstracts was drawn up after removing duplicates. In addition, reference lists of included studies were manually examined to check for potential articles by both the authors independently. Citation indexing services and conference proceedings were not included in the present review, the latter primarily due to concerns about incomplete reporting of data and uncertainty about the study quality.
Data extraction and quality assessment
Quality assessment of included studies was performed concurrently with data extraction by the two authors independently. The data extracted from the articles include the author and year of study, place of conduct of study, characteristics of the study population, sample size, study design, primary objective, fully adjusted measure of association such as risk (either odds ratio [OR]/relative risk [RR]), and any significant moderators/mediators. We used an adapted version of the Newcastle–Ottawa Quality Assessment Scale to critically appraise the selected articles which fell into the category of observational studies. This tool has good psychometric properties such as content validity and inter-rater reliability.[17] It includes items such as representativeness of sampling procedures, validity of assessment measures employed, response rate, and whether the study controlled for at least three essential confounders. Reporting on methodological aspects of a study than numerical scores has been suggested to be more appropriate for nonrandomized observational studies included in systematic reviews and hence this tool was preferred for quality assessment.[18] A response rate of 60% was considered adequate, based on prior systematic reviews of observational studies.[19] We rated the individual components of the quality assessment tool (criteria met, not met, not reported) and derived an overall rating for the quality of every study (high, moderate, poor) included in the review. Quality assessment was not separately done for systematic reviews and meta-analysis included but we relied on the authors’ quality analysis reported in the paper. For effect estimates, we relied on values reported by the authors and did not calculate summary measures or perform additional analysis. We did not attempt a meta-analysis as none of the identified studies were randomized controlled trials.
Results
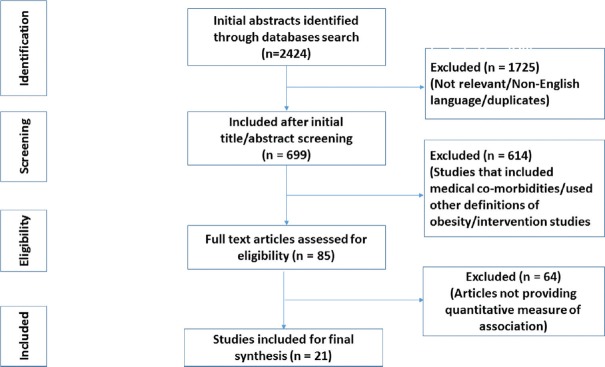
The flowchart for literature search is shown in Figure 1. After applying the inclusion and exclusion criteria, 21 studies were identified for synthesis from an initial search yielding a combined total of 2424 articles. Majority of included studies were on depression (n = 15) while four were on anxiety and one each on PDs, EDs, attention-deficit hyperactivity disorder (ADHD) and alcohol use. Of these, two studies evaluated a range of psychiatric outcomes in obesity and have been described in appropriate sections. Thus, a total of 21 papers were included in the review of which eight were cross-sectional studies, six longitudinal, two systematic reviews, and five were meta-analyses papers. Quality assessment of observational studies showed that four studies were rated high on the quality assessment checklist and others were moderate (n = 10). Data extracted from the selected studies are presented in Table 1.
Figure 1.
Flowchart for literature search
Table 1.
Characteristics of included studies
| Author, Year | Place of conduct | Population Characteristics | Type of study | Primary Objective | Reported Findings | Moderators/Modifiers/other Comments |
|---|---|---|---|---|---|---|
| Depression | ||||||
| Simon et al, 2006†[20] | USA | Adults N=9125 | Cross sectional | Obesity vs psychiatric disorders association | Depression OR-1.21 (1.01-1.35) |
No gender difference Racial difference present |
| Bipolar disorder OR-1.47 (1.12-1.93) |
||||||
| Zhong et al, 2010[21] | USA | General population N=2641 | Cross-sectional | Depression in Obesity | OR=1.6 (1.3-2.0) | - |
| Kim et al, 2010[22] | South Korea | 21-75 yr working population N=8,121 | Cross-sectional | Depression in obesity | OR (female) 1.47 (0.6-3.3) OR (male) 1.94 (1.03-3.62) |
Obesity and underweight risk for depression. Overweight protective |
| Mannan et al, 2016[23] | Australia | Adolescents N=15854 | Meta-analysis (of longitudinal studies) | Obesity vs Depression bidirectional association | O→D* RR-1.4 (1.16-1.7) D→O** RR-1.7 (1.4-2.07) |
Bidirectional link |
| Pan et al, 2011[24] | USA | Women-54-79 years N=65,955 | Longitudinal | Obesity vs Depression bidirectional association | O→D* OR 1.38 (1.2-1.5) D→O** OR 1.1 (1.03-1.18) |
OR corrected for covariates |
| De Wit et al, 2009[25] | Netherlands | N=204,507 | Meta-analysis | Depression in obesity | Pooled OR 1.18 (1.01-1.3) | Female gender- moderator |
| Luppino et al, 2010[26] | Netherlands | N=58,745 | Meta-analysis of longitudinal studies | Obesity vs Depression bidirectional association | O→D* OR-1.55 (1.2-1.98) D→O** OR-1.58 (1.33-1.87) |
Overweight also risk factor for depression |
| Richardson et al, 2003[27] | USA | Adolescents followed up to adulthood N=1037 | Longitudinal | Obesity in depression | RR (Adolescent females)=2.329 (1.29-3.83) | Risk was significant only for adolescent females |
| Marmorstein et al, 2014[28] | USA | Adolescents followed up to adulthood N=1512 | Longitudinal | Prospective risk of obesity in depression and vice-versa | O→D* OR 5.8 (2.3-15.0) D→O** OR 3.76 (1.3-10.5) |
Finding significant only in females |
| Herva et al, 2006[29] | Finland | Adolescents followed up to young adulthood N=8451 | Longitudinal | Prospective risk of depression in obesity | Adjusted OR (males) 1.97 (1.06-3.68) Adjusted OR (females) 1.64 (1.16-2.32) | Being obese both in adolescence and adulthood linked to depression only among females |
| McCarty et al, 2009†[30] | USA | Young Adults N=776 | Longitudinal | Association between obesity, depression and alcohol use | O→D* OR (females) =2.14 | Obesity found to be protective against depression in males |
| Blaine et al, 2008[31] | USA | N>33,000 | Meta-analysis | Obesity in depression | OR=1.18 (1.13-1.23) | Risk more in adolescent females (OR-2.5) |
| Hicken et al, 2013[32] | USA | Women N=3666 | Cross-sectional | Obesity Vs Depression in different ethnic groups | OR- 1.73 (1.19-2.53) | Race/ethnicity- moderator |
| Ma J et al, 2010[33] | USA | Women N=10,348 | Cross sectional | Obesity VS Depression correlation | r=0.49 | Severity of obesity moderator |
| Atlantis et al, 2008[34] | Australia | N=55,387 | Systematic Review | Obesity vs Depression bidirectional association | Evidence weak | . |
| Anxiety | ||||||
| Simon et al, 2006†[20] | USA | Adults N=9125 | Cross sectional | Obesity vs psychiatric disorders association | Panic disorder OR-1.27 (1.01-1.6) |
No gender difference Racial difference present |
| Ejike et al, 2013[35] | Nigeria | General population N=1584 | Cross sectional | BMI Vs Anxiety score correlation | r=0.024(males) r=0.083(females) | Correlation not significant |
| Guedes et al, 2013[36] | Brazil | 18-50 yrs old N=50 | Cross-sectional | BMI Vs Anxiety and depression correlation | Anxiety r=-0.15 Depression r=0.01 | No significant correlation |
| Gariepy et al, 2010[37] | Canada | Pooled N=3,11,968 | Meta-analysis | Anxiety Vs obesity | Pooled OR 1.40 ( 1.23-1.57) | Association significant in women |
| Personality disorder | ||||||
| Gerlach et al., 2015[38] | Germany | 68 included studies Pooled N>1,000,000 |
Systematic review | PD in obesity | Prevalence of Any PD mean=26% (19-71%) | Cluster C predominant |
| Eating disorders | ||||||
| Darby et al, 2009[39] | Australia | General population N=3001 |
Longitudinal | To assess rise in prevalence of comorbid obesity and ED | OR=4.5 (2.8-7.4) | . |
| ADHD | ||||||
| Cortese et al, 2013[40] | USA | Adults N=34,653 |
Cross sectional | Persistent/remitted/lifetime ADHD VS Obesity | OR (persistent ADHD) 1.44 (1.06-1.95) | After adjusting for covariates, significant only in females with lifetime symptoms |
| Alcohol use | ||||||
| McCarty et al, 2009†[30] | USA | Young Adults N=776 |
Longitudinal | Association between obesity, depression and alcohol use | Alcohol use to obesity OR-3.84 in women | Obesity found to be protective against depression in males |
Obesity and depression
From the 15 studies identified in this area, three cross-sectional studies done in general adult population had an average OR of 1.33 for depression in obesity.[20,21,22] This finding was replicated in a meta-analysis of longitudinal studies in adolescents with roughly similar odds of developing depression in obesity (OR: 1.4) and vice versa (OR: 1.7).[23] Thus, the study provided evidence for a bidirectional link between obesity and depression with depressed adolescents having about 70% higher risk for being obese. Broadly, similar findings were also echoed in a 10-year prospective study on older women with obese people having 38% higher risk for developing depression and depressed people having 10% elevated risk for obesity compared to controls.[24] These effect sizes were consistently higher among females (pooled OR: 1.32) than males (pooled OR: 1.00) in community-based studies suggesting a significant moderating role for gender in this relationship.[25] In another exclusive meta-analysis of longitudinal studies, the odds of being depressed in obesity (OR: 1.55) and conversely, odds of obesity in depression (OR: 1.58) was similar.[26] Findings from three longitudinal studies on adolescents/young adults show that the prospective risk of developing depression in obese individuals were significantly higher in females.[27,28,29] One study, interestingly, also noted that obesity had a protective effect against depression in males (OR: 0.31) while it predicted depression among young women (OR: 2.14).[30] Gender as a significant moderator of the obesity-depression association was also observed in the meta-analysis by Blaine, with a significantly higher risk (150%) among females (OR: 2.5).[31] Other studies have noted the role of ethnicity as a possible moderator, wherein only in white women, obesity was associated with significantly greater likelihood of depression.[32] Some evidence for severity of obesity as a possible moderator in the association between depression and obesity has also been observed with one study noting modest correlations between obesity indices and severity of depression (r = 0.49).[33] Interestingly, Atlantis and Baker, in their systematic review of epidemiological studies aimed at determining whether obesity causes depression, have found weak evidence for obesity increasing incidence of depression and point out the need for methodologically rigorous prospective cohort studies in this regard.[34]
Obesity and anxiety
Among the four studies that were reviewed in this area, one found poor correlation between BMI and anxiety across both the genders (r = 0.024 in males and 0.083 in females),[35] while another cross-sectional study also reported a similar lack of association between BMI and both anxiety and depression (r = 0.15 and 0.1, respectively).[36] In a large nationally representative survey, where relationship of different psychiatric disorders in obesity was studied, the authors found that obese people had 27% increased lifetime risks of being diagnosed with panic disorder (OR: 1.27).[20] In a meta-analysis that evaluated both prospective and cross-sectional studies separately,[37] mixed results were observed in the two prospective studies with one study showing significant association between obesity and anxiety disorders only in men (OR for men 1.50 vs. women 0.99) while the other study, carried out only among women, showed an extremely high association (OR: 6.27). Hence, the moderating role of gender was inconclusive here. In the same meta-analysis, the 14 cross-sectional studies showed a positive but varying association (OR: 1.10–2.73). An inconsistency index of 84.3% was noted by the authors pointing toward significant heterogeneity in the results.
Obesity and personality disorders
In the systematic review on 68 studies,[38] the odds of having any PD was greater among obese people (OR: 1.2–1.95) and this relationship was directly proportional to the severity of obesity (24% risk in Class III obesity). Further, the association was more significant among females where the authors noted higher rates of avoidant and antisocial PD in females with severe obesity (38%) when compared to females without obesity (30%). This difference was not significant in men.
Obesity and eating disorders
Darby et al. conducted a study to assess time trends in the prevalence of comorbid ED in obesity over a 10-year period.[39] Their findings showed that comorbid ED and obesity had increased from 1% to 3.5% over the study period. This rise in prevalence was significantly higher than increase in rates of obesity or ED alone.
Obesity and attention deficit hyperactivity disorder
In a large epidemiological study, the authors explored the association between adult obesity and lifetime/remitted/persisting ADHD. Adult persistent ADHD was found to be significantly associated with obesity (OR: 1.44).[40] In women, the association was significant for all the three categories (remitted/persisting/lifetime ADHD). Notably, when corrected for possible confounders, association between obesity and lifetime ADHD continued to be significant only among females (adjusted OR: 1.09) but not in males (adjusted OR: 0.98).
Obesity and alcohol use
One longitudinal study, among young adults, explored prospective three-way association between obesity, depression, and alcohol use. In this study, alcohol use disorders prospectively predicted obesity only among women (OR: 3.84). Obesity, however, did not seem to be a clear risk factor for alcohol use.[30]
Discussion
Although a significant amount of literature is available on obesity and psychiatric illness, the current review has specifically looked into the strength of association of each psychiatric illness with obesity. Clearly, the evidence was more voluminous and strongest for depression, with most of the studies reporting significant association for the presence of depression in obesity.[21,22,23,24,26,28,31,32] However, most of these studies were cross-sectional in nature which cannot conclusively establish the cause-and-effect relationship between the two conditions due to design limitations. This can only be established through longitudinal research designs. Only few such longitudinal studies were available which gave evidence for a reciprocal link between depression and obesity and this was replicated in a meta-analysis paper also which provides stronger evidence of the association.[23,24,26,34] Variability in effect sizes across studies may stem from methodological differences such as the cutoffs used for measuring BMI, methods used to measure psychiatric outcomes such as depression (clinical vs. rating scales), varying lengths of follow-up in longitudinal designs and the nature of effect estimate used (RR vs. absolute risk estimates). Subgroup analysis based on parameters such as age, gender, and differences in measurement methods were reported in a few studies and this may also have contributed to some of the differences observed.
The role of gender as a moderator in this relationship was evident in a handful of studies that showed greater effect sizes in females,[22,25,28] and specifically, in adolescent females.[27,31] The earlier onset of puberty in females and the complex hormonal and biological changes that accompany this phenomenon may result in earlier onset of obesity among females and this may persist from adolescence to adulthood.[41,42] The inherently higher dissatisfaction with their bodies among females combined with societal pressures to remain thin may affect self-esteem and enhance stress, which may further increase the risk of both obesity and depression preferentially among females across life span.[43,44] One study provided preliminary evidence of the role of ethnicity as a possible moderator.[32] Other moderators identified included severity of obesity.[33] A few studies have shown that both overweight and obesity were risk factors for depression,[26] whereas few studies have pointed out that overweight is actually a protective factor against depression.[22] Clearly, this disparity needs to be addressed in future studies with appropriate designs. The mechanisms postulated for depression in obesity include the social dimensions of weight such as negative self-perceptions and stigma as well as the health consequences of being overweight.[45,46,47] Conversely, the mechanisms leading to obesity in depression mostly focus on ethnic and lifestyle factors.[48] Recently, the role of serotonin and particularly, the 5-hydroxytryptamine type 3 receptor has come under scrutiny as a therapeutic target to reduce the burden of comorbid depression and obesity.[49]
For anxiety disorders, the number of studies was comparatively fewer. From the reviewed articles, the correlation between obesity and anxiety appears less robust in comparison to depression.[35,36] One study has shown that obese individuals had a higher odds of lifetime panic disorder.[20] In the meta-analysis that was reviewed, though the pooled OR pointed toward a significant association, the inconsistency index was high.[37] With the exception of specific phobia and social anxiety, evidence is largely mixed in studies which performed subgroup analysis by subtypes of anxiety disorders.[50,51,52,53] The relative lack of longitudinal studies assessing the relationship between anxiety disorders and obesity precludes clear conclusions regarding the direction of association.
The relationship between obesity and PDs appears complex. Few studies have explored specific personality traits in obese individuals and among these, neuroticism and impulsivity has been consistently replicated.[54,55,56] Moreover, among obese people attending a bariatric surgery clinic, roughly a quarter had clinical evidence of borderline PD.[57] Our review shows that the odds of having any PD in obese individuals are high and cluster C traits (avoidant/dependent) are often predominant.[38]
EDs-obesity-other psychiatric illness could form a vicious cycle and many studies have looked into psychiatric illness in the context of comorbid ED and obesity. However, the direct association between ED and obesity has been rarely studied. In the only such study included in this review, the authors have shown that though ED and obesity are increasing in general population, the odds of having comorbid ED and obesity have increased around 4.5 times, indirectly pointing toward an underlying association between these disorders.[39]
One prospective study has reported increased the prevalence of obesity in adults with a childhood history of ADHD.[58] The study included in the present review looked into the strength of association of this relationship and pointed out that persistent ADHD in childhood was associated with obesity later and more so in females.[40] However, as there are very few studies addressing this question, one needs to wait for more evidence before clinical recommendations can be made.
Several neuroimaging studies have implicated a common neurobiology in feeding and substance use such as reinforcement of the reward pathway.[59,60] As such, there has been a trend to consider obesity as a part of “addiction.”[61,62] However, studies that explored the strength of this association are scarce. Here, we have reviewed an article which studied the interaction between obesity-substance use and depression and show that obesity rates were more in those with substance use disorders and this association was stronger in females.[30]
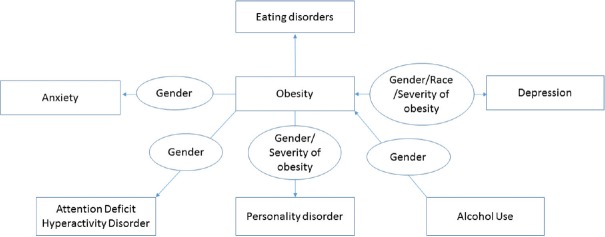
Our findings have important clinical and research implications. With steadily increasing rates of obesity globally, an understanding of the impact of obesity on prevalence rates of mental disorders assumes significance. This may provide inputs from a mental health prevention and promotion standpoint. It may inform the development of prediction tools and better interventions. It may also spur research on the causal pathways and mechanisms mediating the relationship. Figure 2 represents an evidence based model for understanding the association between obesity and psychiatric disorders with key moderators in this relationship and is adapted from earlier works in this field.[63]
Figure 2.
Evidence-based model for association between psychiatric disorders and obesity (moderators shown in ellipse and disorders in rectangle boxes - arrows indicate the direction of association observed)
A growing body of evidence suggests that there may be pathophysiological links between psychiatric disorders such as schizophrenia and metabolic conditions such as obesity and diabetes.[64,65,66,67] Further, obesity (or high BMI) has been identified consistently as a risk factor for metabolic syndrome among psychiatric populations receiving treatment with agents such as clozapine.[68,69] This three-way link between obesity, metabolic syndrome, and psychiatric disorders presents significant opportunities to improve our understanding of pathogenesis of psychiatric disorders and develop newer therapeutic targets.
Psychiatric evaluation may be an important component of comprehensive obesity care and merits further evaluation. This can be expected to optimize therapeutic and functional outcomes. Furthermore, as the bidirectional link becomes apparent, the treatment of the psychiatric illness may bring down the obesity burden and vice versa. Future research opportunities in this area include clarifying the relation between obesity severity and clinical subtypes of depression and anxiety given the heterogeneous nature of these conditions. Researchers should also consider important methodological issues such as measuring obesity through objective rather than self-reported measures and possible confounders such as physical comorbidities to unravel the complex relationship between obesity and psychiatric illness.
Limitations of the present review include the confounding effects of unmeasured medical comorbidities and differences in the way outcomes were assessed. The included studies were quite heterogeneous in characteristics of the study population. As none of the included studies were randomized controlled trials, we did not perform a meta-analysis. We were unable to peruse certain databases due to limitations of institutional access. Furthermore, it is possible that some studies may have been missed as it did not fit our inclusion criteria or remain unpublished or unavailable on academic databases. We tried to keep the studies homogeneous with regard to their design and domains of outcome studied so as to render an interpretation of findings easier and that allied with the quality assessment done are advantages of the present review.
Conclusion
Obesity and psychiatric illness are closely linked, and the evidence is strong and reciprocal for depression, modest, and inconsistent for anxiety disorders and inadequate for other psychiatric conditions. Apart from depression, the causal relationships between obesity and other psychiatric disorders could not be established from available data. Although both genders appeared to be at risk of psychiatric disorders in obesity and vice versa, many of these associations were stronger in females indicating a possible moderating role for gender in this relationship. Based on current evidence, there is a need to carry out a cost-effectiveness analysis of a multidisciplinary approach to the management of obesity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. World Health Statistics 2014. Geneva: World Health Organization; 2014. [Last cited on 2016 Nov 20]. Available from: http://www.apps.who.int/iris/bitstream/10665/112738/1/9789240692671_eng.pdf . [Google Scholar]
- 2.Bhardwaj S, Misra A, Misra R, Goel K, Bhatt SP, Rastogi K, et al. High prevalence of abdominal, intra-abdominal and subcutaneous adiposity and clustering of risk factors among urban Asian Indians in North India. PLoS One. 2011;6:e24362. doi: 10.1371/journal.pone.0024362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mohan V, Deepa R. Obesity and abdominal obesity in Asian Indians. Indian J Med Res. 2006;123:593–6. [PubMed] [Google Scholar]
- 4.Deepa M, Farooq S, Deepa R, Manjula D, Mohan V. Prevalence and significance of generalized and central body obesity in an urban Asian Indian population in Chennai, India (CURES: 47) Eur J Clin Nutr. 2009;63:259–67. doi: 10.1038/sj.ejcn.1602920. [DOI] [PubMed] [Google Scholar]
- 5.Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, et al. Prevalence of generalized and abdominal obesity in urban and rural India- the ICMR – INDIAB Study (Phase-I) [ICMR – INDIAB-3] Indian J Med Res. 2015;142:139–50. doi: 10.4103/0971-5916.164234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranjani H, Mehreen T, Pradeepa R, Anjana R, Garg R, Anand K, et al. Epidemiology of childhood overweight and amp; obesity in India: A systematic review. Indian J Med Res. 2016;143:160. doi: 10.4103/0971-5916.180203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raj M, Kumar RK. Obesity in children and adolescents. Indian J Med Res. 2010;132:598–607. [PMC free article] [PubMed] [Google Scholar]
- 8.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- 10.Kearns K, Dee A, Fitzgerald AP, Doherty E, Perry IJ. Chronic disease burden associated with overweight and obesity in Ireland: The effects of a small BMI reduction at population level. BMC Public Health. 2014;14:143. doi: 10.1186/1471-2458-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 12.Fitzgibbon ML, Stolley MR, Kirschenbaum DS. Obese people who seek treatment have different characteristics than those who do not seek treatment. Health Psychol. 1993;12:342–5. doi: 10.1037//0278-6133.12.5.342. [DOI] [PubMed] [Google Scholar]
- 13.Lykouras L, Michopoulos J. Anxiety disorders and obesity. Psychiatriki. 2011;22:307–13. [PubMed] [Google Scholar]
- 14.Lin HY, Huang CK, Tai CM, Lin HY, Kao YH, Tsai CC, et al. Psychiatric disorders of patients seeking obesity treatment. BMC Psychiatry. 2013;13:1. doi: 10.1186/1471-244X-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sacco WP, Wells KJ, Vaughan CA, Friedman A, Perez S, Matthew R. Depression in adults with type 2 diabetes: The role of adherence, body mass index, and self-efficacy. Health Psychol. 2005;24:630–4. doi: 10.1037/0278-6133.24.6.630. [DOI] [PubMed] [Google Scholar]
- 16.Labad J, Price JF, Strachan MW, Fowkes FG, Ding J, Deary IJ, et al. Symptoms of depression but not anxiety are associated with central obesity and cardiovascular disease in people with type 2 diabetes: The Edinburgh Type 2 Diabetes Study. Diabetologia. 2010;53:467–71. doi: 10.1007/s00125-009-1628-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wells G, Shea B, O’Connell J, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-analysis. 2011. [Last cited on 2017 Feb 24]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
- 18.Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–60. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 19.Wong WC, Cheung CS, Hart GJ. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol. 2008;5:23. doi: 10.1186/1742-7622-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–30. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhong W, Cruickshanks KJ, Schubert CR, Nieto FJ, Huang GH, Klein BE, et al. Obesity and depression symptoms in the Beaver Dam Offspring Study population. Depress Anxiety. 2010;27:846–51. doi: 10.1002/da.20666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim JY, Chang HM, Cho JJ, Yoo SH, Kim SY. Relationship between obesity and depression in the Korean working population. J Korean Med Sci. 2010;25:1560–7. doi: 10.3346/jkms.2010.25.11.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mannan M, Mamun A, Doi S, Clavarino A. Prospective associations between depression and obesity for adolescent males and females – A systematic review and meta-analysis of longitudinal studies. PLoS One. 2016;11:e0157240. doi: 10.1371/journal.pone.0157240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes (Lond) 2012;36:595–602. doi: 10.1038/ijo.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Wit L, Luppino F, van Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res. 2010;178:230–5. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 27.Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157:739–45. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 28.Marmorstein NR, Iacono WG, Legrand L. Obesity and depression in adolescence and beyond: Reciprocal risks. Int J Obes (Lond) 2014;38:906–11. doi: 10.1038/ijo.2014.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herva A, Laitinen J, Miettunen J, Veijola J, Karvonen JT, Läksy K, et al. Obesity and depression: Results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int J Obes (Lond) 2006;30:520–7. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 30.McCarty CA, Kosterman R, Mason WA, McCauley E, Hawkins JD, Herrenkohl TI, et al. Longitudinal associations among depression, obesity and alcohol use disorders in young adulthood. Gen Hosp Psychiatry. 2009;31:442–50. doi: 10.1016/j.genhosppsych.2009.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blaine B. Does depression cause obesity? A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol. 2008;13:1190–7. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 32.Hicken MT, Lee H, Mezuk B, Kershaw KN, Rafferty J, Jackson JS. Racial and ethnic differences in the association between obesity and depression in women. J Womens Health (Larchmt) 2013;22:445–52. doi: 10.1089/jwh.2012.4111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ma J, Xiao L. Obesity and depression in US women: Results from the 2005-2006 National Health and Nutritional Examination Survey. Obesity (Silver Spring) 2010;18:347–53. doi: 10.1038/oby.2009.213. [DOI] [PubMed] [Google Scholar]
- 34.Atlantis E, Baker M. Obesity effects on depression: Systematic review of epidemiological studies. Int J Obes (Lond) 2008;32:881–91. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- 35.Ejike CE. Association between anxiety and obesity: A study of a young-adult Nigerian population. J Neurosci Rural Pract. 2013;4(Suppl 1):S13–8. doi: 10.4103/0976-3147.116429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guedes EP, Madeira E, Mafort TT, Madeira M, Moreira RO, Mendonça LM, et al. Body composition and depressive/anxiety symptoms in overweight and obese individuals with metabolic syndrome. Diabetol Metab Syndr. 2013;23:5–82. doi: 10.1186/1758-5996-5-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gariepy G, Nitka D, Schmitz N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. Int J Obes (Lond) 2010;34:407–19. doi: 10.1038/ijo.2009.252. [DOI] [PubMed] [Google Scholar]
- 38.Gerlach G, Loeber S, Herpertz S. Personality disorders and obesity: A systematic review. Obes Rev. 2016;17:691–723. doi: 10.1111/obr.12415. [DOI] [PubMed] [Google Scholar]
- 39.Darby A, Hay P, Mond J, Quirk F, Buttner P, Kennedy L. The rising prevalence of comorbid obesity and eating disorder behaviors from 1995 to 2005. Int J Eat Disord. 2009;42:104–8. doi: 10.1002/eat.20601. [DOI] [PubMed] [Google Scholar]
- 40.Cortese S, Faraone SV, Bernardi S, Wang S, Blanco C. Adult attention-deficit hyperactivity disorder and obesity: Epidemiological study. Br J Psychiatry. 2013;203:24–34. doi: 10.1192/bjp.bp.112.123299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malina R, Bouchard C, Bar-Or O. Growth, Maturation and Physical Activity. Champaign, IL: Human Kinetics; 2004. Obesity in childhood and adolescent; pp. 535–7. [Google Scholar]
- 42.Slyper AH. The pubertal timing controversy in the USA, and a review of possible causative factors for the advance in timing of onset of puberty. Clin Endocrinol (Oxf) 2006;65:1–8. doi: 10.1111/j.1365-2265.2006.02539.x. [DOI] [PubMed] [Google Scholar]
- 43.Laus MF, Costa TM, Almeida SS. Gender differences in body image and preferences for an ideal silhouette among Brazilian undergraduates. Eat Behav. 2015;19:159–62. doi: 10.1016/j.eatbeh.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 44.Ge X, Natsuaki MN, Conger RD. Trajectories of depressive symptoms and stressful life events among male and female adolescents in divorced and nondivorced families. Dev Psychopathol. 2006;18:253–73. doi: 10.1017/S0954579406060147. [DOI] [PubMed] [Google Scholar]
- 45.Zhao G, Ford ES, Dhingra S, Li C, Strine TW, Mokdad AH. Depression and anxiety among US adults: Associations with body mass index. Int J Obes (Lond) 2009;33:257–66. doi: 10.1038/ijo.2008.268. [DOI] [PubMed] [Google Scholar]
- 46.Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 47.Ross CE. Overweight and depression. J Health Soc Behav. 1994;35:63–79. [PubMed] [Google Scholar]
- 48.Beydoun MA, Wang Y. Pathways linking socioeconomic status to obesity through depression and lifestyle factors among young US adults. J Affect Disord. 2010;123:52–63. doi: 10.1016/j.jad.2009.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kurhe Y, Mahesh R. Mechanisms linking depression co-morbid with obesity: An approach for serotonergic type 3 receptor antagonist as novel therapeutic intervention. Asian J Psychiatr. 2015;17:3–9. doi: 10.1016/j.ajp.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 50.Barry D, Pietrzak RH, Petry NM. Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Ann Epidemiol. 2008;18:458–66. doi: 10.1016/j.annepidem.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008;64:97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 52.Kasen S, Cohen P, Chen H, Must A. Obesity and psychopathology in women: A three decade prospective study. Int J Obes (Lond) 2008;32:558–66. doi: 10.1038/sj.ijo.0803736. [DOI] [PubMed] [Google Scholar]
- 53.Herpertz S, Burgmer R, Stang A, de Zwaan M, Wolf AM, Chen-Stute A, et al. Prevalence of mental disorders in normal-weight and obese individuals with and without weight loss treatment in a German urban population. J Psychosom Res. 2006;61:95–103. doi: 10.1016/j.jpsychores.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 54.Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, et al. Facets of personality linked to underweight and overweight. Psychosom Med. 2009;71:682–9. doi: 10.1097/PSY.0b013e3181a2925b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gerlach G, Herpertz S, Loeber S. Personality traits and obesity: A systematic review. Obes Rev. 2015;16:32–63. doi: 10.1111/obr.12235. [DOI] [PubMed] [Google Scholar]
- 56.Sutin AR, Ferrucci L, Zonderman AB, Terracciano A. Personality and obesity across the adult life span. J Pers Soc Psychol. 2011;101:579–92. doi: 10.1037/a0024286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sansone RA, Sansone LA. The relationship between borderline personality and obesity. Innov Clin Neurosci. 2013;10:36–40. [PMC free article] [PubMed] [Google Scholar]
- 58.Cortese S, Ramos Olazagasti MA, Klein RG, Castellanos FX, Proal E, Mannuzza S. Obesity in men with childhood ADHD: A 33-year controlled, prospective, follow-up study. Pediatrics. 2013;131:e1731–8. doi: 10.1542/peds.2012-0540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Volkow ND, Wang GJ, Fowler JS, Tomasi D, Baler R. Food and drug reward: Overlapping circuits in human obesity and addiction. Curr Top Behav Neurosci. 2012;11:1–24. doi: 10.1007/7854_2011_169. [DOI] [PubMed] [Google Scholar]
- 60.Kenny PJ. Reward mechanisms in obesity: New insights and future directions. Neuron. 2011;24(69):664–79. doi: 10.1016/j.neuron.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stice E, Figlewicz DP, Gosnell BA, Levine AS, Pratt WE. The contribution of brain reward circuits to the obesity epidemic. Neurosci Biobehav Rev. 2013;37(9 Pt A):2047–58. doi: 10.1016/j.neubiorev.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vanbuskirk KA, Potenza MN. The treatment of obesity and its co-occurrence with substance use disorders. J Addict Med. 2010;4:1–10. doi: 10.1097/ADM.0b013e3181ce38e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Markowitz S, Friedman MA, Arent SM. Understanding the relation between obesity and depression: Causal mechanisms and implications for treatment. Clin Psychol Sci Pract. 2008;15:1–20. [Google Scholar]
- 64.Hansen T, Ingason A, Djurovic S, Melle I, Fenger M, Gustafsson O, et al. At-risk variant in TCF7L2 for type II diabetes increases risk of schizophrenia. Biol Psychiatry. 2011;70:59–63. doi: 10.1016/j.biopsych.2011.01.031. [DOI] [PubMed] [Google Scholar]
- 65.Venkatasubramanian G, Chittiprol S, Neelakantachar N, Naveen MN, Thirthall J, Gangadhar BN, et al. Insulin and insulin-like growth factor-1 abnormalities in antipsychotic-naive schizophrenia. Am J Psychiatry. 2007;164:1557–60. doi: 10.1176/appi.ajp.2007.07020233. [DOI] [PubMed] [Google Scholar]
- 66.DE Hert M, Schreurs V, Vancampfort D, VAN Winkel R. Metabolic syndrome in people with schizophrenia: A review. World Psychiatry. 2009;8:15–22. doi: 10.1002/j.2051-5545.2009.tb00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Agarwal SM, Venkatasubramanian G. Metabolic syndrome in schizophrenia: Theoretical, clinical and translational perspectives. Indian J Psychol Med. 2013;35:117–20. doi: 10.4103/0253-7176.116231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lamberti JS, Olson D, Crilly JF, Olivares T, Williams GC, Tu X, et al. Prevalence of the metabolic syndrome among patients receiving clozapine. Am J Psychiatry. 2006;163:1273–6. doi: 10.1176/ajp.2006.163.7.1273. [DOI] [PubMed] [Google Scholar]
- 69.Grover S, Nebhinani N, Chakrabarti S, Avasthi A, Kulhara P. Metabolic syndrome among patients receiving clozapine: A preliminary estimate. Indian J Pharmacol. 2011;43:591–5. doi: 10.4103/0253-7613.84979. [DOI] [PMC free article] [PubMed] [Google Scholar]