Abstract
Teratoma of the orbit is rare; very few cases have been published in literature. A case of orbital teratoma in a neonate is presented where the proptosis was massive enough to obscure the eyeball. Clinically, the diagnosis of teratoma was considered. As there was no possibility of salvaging the eye, exenteration of the orbit was done. Orbital teratomas are generally benign. Histopathological examination revealed the features of malignant teratoma.
KEY WORDS: Histopathology, malignant teratoma, neonate, orbital teratoma, orbital tumor
Introduction
Teratomas are tumors containing elements of all three germ layers: ectoderm, mesoderm, and endoderm. They are common in the gonads, mediastinum, and pineal area. So far, only about 51 cases have been reported in the orbit worldwide. They may present at any time from the fetal stage to adolescence.[1] Orbital teratomas are mostly benign and localized; rarely malignant. Globe is usually not affected but compressed and pushed forward causing marked proptosis at birth.[2] Tissues are usually mature and consist of representation of ectoderm, mesoderm, endoderm, and neuroectoderm. Some cases have intracranial or periorbital involvement and may represent extension of a primary teratoma from these sites.[1] Imaging studies can be performed to ascertain the extent of disease and plan surgical removal. An attempt should be made to save the eye when possible.[2] Here, we report a rare case of malignant orbital teratoma in a newborn girl with histopathological confirmation following exenteration.
Case Report
A 1-day-old female child was brought with massive proptosis on the right side [Figure 1]. She was the first child of nonconsanguineous parents, born of full-term natural delivery, and weighing 2.8 kg. Antenatal period was uneventful. A large multiloculated cystic mass of size 6 cm × 6 cm and quadrangular in shape was seen protruding from the right orbit; cornea and sclera were barely visible on its anterior aspect. The left eye and orbit were normal. Systemic examination and ultrasound did not reveal congenital anomalies elsewhere. Ultrasonography of the right orbit showed a multicystic intraorbital tumor with variegated echogenic pattern, pushing the globe anteriorly. The orbit was grossly distended, but its walls were intact. Computed tomography (CT) scan or magnetic resonance imaging was not done as ultrasound showed that the tumor was localized to the orbit.
Figure 1.
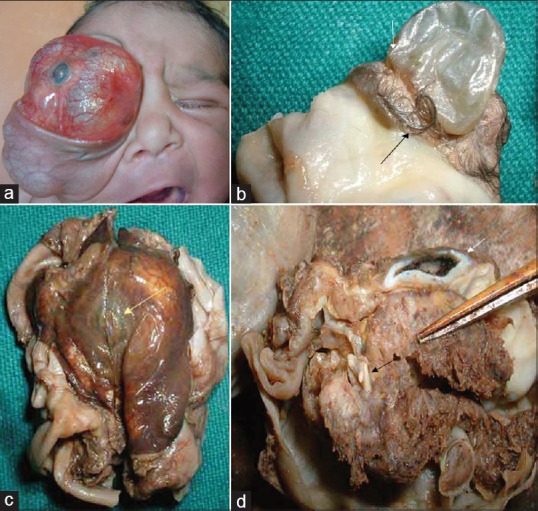
(a) Clinical photograph of the baby showing massive proptosis on the right side. (b) Irregular mass showing cornea (black arrow) on one side and collapsed cyst on the posterior aspect (white arrow). (c) Multiloculated cyst with area resembling skin showing a tuft of hair (white arrow). (d) Cut section of the tumor showing compressed eyeball (white arrow) and brownish tumor mass with a rudimentary tooth (black arrow)
Orbital exenteration was performed under general anesthesia on the 3rd day. Lid-sparing incision was made, and dissection was extended up to the orbital rim circumferentially. The periosteum was incised in a circumlinear fashion. The orbital contents were degloved in the subperiosteal plane. Cautery transection of orbital tissue was begun at the superior orbital fissure and then along the inferior orbital fissure. The tumor was removed in toto. The eyeball was found to be buried within the mass; hence, it could not be dissected free [Figure 1]. Postoperative recovery was uneventful. The irregular mass showed cornea on one side and a cyst on the posterior aspect. Cut section revealed compressed eyeball. Inside the cyst, there was a tumor of size 2.5 cm × 2.0 cm. One area resembled skin with a tuft of hair [Figure 1]. A rudimentary tooth was found in one focus [Figure 1]. Histopathology of the mass showed the following features – skin and its appendages [Figure 2a], intestinal epithelium [Figure 2b], structures resembling choroid plexus [Figure 2c], undifferentiated cells resembling fetal neural tissue [Figure 2d], rosettes [Figure 2e], islands of fat cells, smooth muscle, nerve bundles, and blood vessels. Since tissue elements representing all the 3 germ layers were detected in the mass, the diagnosis of orbital teratoma was made; the presence of fetal neuroepithelium pointed to its malignant nature.
Figure 2.
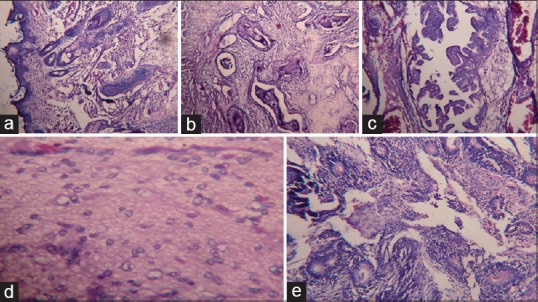
Histopathology of the mass showing: (a) Skin with appendages such as hair follicles (H and E, ×100), (b) intestinal mucosa (H and E, ×100), (c) structures resembling choroid plexus (H and E, ×100), (d) undifferentiated cells resembling fetal neural tissue (H and E, ×100), (e) rosettes (H and E, ×100)
The baby was discharged on the 7th postoperative day but was unfortunately lost for follow-up.
Discussion
Orbital teratomas are unilateral, congenital germ cell tumors, which present at birth with moderate to massive proptosis, leading to exposure keratopathy. They enlarge the orbit diffusely. All grades of complexity in teratomas have been recorded, even up to a partially or completely developed fetus. They are traditionally classified according to the number of germinal layers present and their degree of differentiation. However, knowledge on the spectrum of orbital germ cell tumors has since widened; hence, the old classification is outdated.
Kivelä and Tarkkanen[3] have presented a clinicopathological classification, which emphasizes the diagnostic and therapeutic aspects relevant to their management and prognosis. Teratomas probably arise from pluripotential embryonic stem cells that are carried to the orbit by blood circulation and escape regulatory influence or from primordial germ cells that aim toward the pineal gland. The new classification of orbital teratomas is as follows: (1) primary intraocular teratoma, (2) primary orbital teratoma, (3) combined orbital and extraorbital teratoma, and (4) secondary orbital teratoma.
Orbital teratoma is sufficiently uncommon that individual case reports are usually cited in the literature. In a review of literature in 1980, the authors cited 51 reported cases of true orbital teratoma.[4]
Orbit is a rare but typical location in which primary extragonadal germ cell tumors may arise. Teratomas are the most common of orbital germ cell tumors. They are generally benign, but their true malignant potential may not be readily evident as they are excised rapidly. When the neural tissue appears like fetal neural tissue, it is said to be immature (malignant). This often occurs in primary intracranial teratomas presenting in fetal life with secondary orbital involvement, resulting in death.[1] Our case showed masses of undifferentiated cells resembling primitive neuroepithelium, indicating its malignant nature; however, there was no intracranial involvement. Soares et al.[5] and Mahesh et al.[6] have claimed malignant change in their cases.
Orbital teratomas preferentially affect females and occur with greater frequency in the left orbit. All cases reported in the literature are female babies[7] except one case.[8] Our case was a girl baby with proptosis on the right side. Furthermore, the mass contained a tooth, which is a rare finding in orbital teratoma.[9]
Most tumors are intraconal and stretch the four rectus muscles, resulting in a quadrangular shape and axial proptosis with exposure keratopathy. The eye is normally developed but buried within the tumor. Teratomas are cystic, fluctuant, and transilluminant, but most appear solid clinically. They rapidly enlarge after birth due to the accumulation of secretions in cystic spaces rather than vigorous cell proliferation. The tumor displaces the eyebrow, nose, mouth, and cheek deforming the face.
Clinically, it is difficult to distinguish orbital teratomas from other benign and malignant neoplasms of the orbit. Surgeons now recommend early surgery despite the difficulty in making the diagnosis preoperatively.[10]
Radiology indicates uniform distension of the orbit by the teratoma, without bone defects, destruction, or sclerosis of orbital bones. Ultrasound examination identifies its heterogeneous nature with areas of low- and high-internal reflectivity; cystic spaces and calcification are typical of this condition. Computed tomographic scan reveals a multiloculated cystic mass with focal punctate calcifications and fat; compressed eyeball and displaced optic nerve are also evident. CT scan is necessary to exclude intracranial extension. Routine prenatal ultrasound may or may not detect orbital teratoma.
Although benign, teratomas were formerly treated by orbital exenteration because of their massive size. Now, there are many reports, in which the eye has been saved. Anterior or lateral orbitotomy is useful. Recurrences have not been reported. Early removal ensures the greatest chance of visual preservation. Globe preservation ensures better cosmesis and a growing orbital implant, permitting symmetric orbital growth.[3] In our patient, the tumor was massive and the globe could not be clearly delineated; hence, orbital exenteration was done.
We report this case of malignant orbital teratoma in a newborn, showing mature elements of all the three germ cell layers along with a tooth and also fetal neural tissue, due to its extreme rarity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Salomao DR, Roden AC. Orbital pathology. In: Albert DM, Jakobiec FA, editors. Principles and Practice of Ophthalmology. 3rd ed. Philadelphia: Saunders Elsevier; 2008. p. 3754. [Google Scholar]
- 2.Shields JA, Shields CL. Atlas of Orbital Tumors. Philadelphia: Lippincott Williams and Wilkins; 1999. p. 30. [Google Scholar]
- 3.Kivelä T, Tarkkanen A. Orbital germ cell tumors revisited: A clinicopathological approach to classification. Surv Ophthalmol. 1994;38:541–54. doi: 10.1016/0039-6257(94)90147-3. [DOI] [PubMed] [Google Scholar]
- 4.Chang DF, Dallow RL, Walton DS. Congenital orbital teratoma: Report of a case with visual preservation. J Pediatr Ophthalmol Strabismus. 1980;17:88–95. doi: 10.3928/0191-3913-19800301-07. [DOI] [PubMed] [Google Scholar]
- 5.Soares EJ, Lopes KD, Andrade J. Orbital malignant teratoma: A case report. Orbit. 1983;2:235–42. [Google Scholar]
- 6.Mahesh L, Krishnakumar S, Subramanian N, Babu K, Biswas J. Malignant teratoma of the orbit: A clinicopathological study of a case. Orbit. 2003;22:305–9. doi: 10.1076/orbi.22.4.305.17239. [DOI] [PubMed] [Google Scholar]
- 7.Murty S, Roy S, Rohatgi JN. Congenital teratoma of the orbit. Indian J Ophthalmol. 1980;28:165–6. [PubMed] [Google Scholar]
- 8.Ferry AP. Teratoma of the orbit: A report of two cases. Surv Ophthalmol. 1965;10:434–42. [PubMed] [Google Scholar]
- 9.Baidya KP, Ghosh S, Datta A, Mukhopadhyay S, Bhaduri G. Huge congenital teratoma containing tooth in a three-day-old neonate. Oman J Ophthalmol. 2014;7:13–5. doi: 10.4103/0974-620X.127912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamilarasi DS, Suryababu S, Rao BL, Varralakshmi V, Mallikarjun C. Congenital orbital teratoma: A rare case report with review of literature. J Evol Med Dent Sci. 2015;4:1080–3. [Google Scholar]


