Abstract
The results of modern cemented and uncemented total hip arthroplasties are outstanding and both systems have their advantages and disadvantages. This paper aims to examine the designs of different types of prostheses, some history behind their development and the reported results. Particular emphasis is placed on cemented stem design and the details of cementing technique.
Keywords: Cemented stem, prostheses, total hip arthroplasty, uncemented stem
MeSH terms: Arthroplasty, replacement, hip, joint, prosthesis, bone cements
Introduction
Total hip arthroplasty (THA) can be broadly divided into those hips fixed with cement and those fixed without. Cemented THA use polymethylmethacrylate (PMMA) to function as a grout, producing an interlocking fit between cancellous bone and prosthesis. Uncemented hips rely on biological fixation of bone to a surface coating on the prosthesis. Initial fixation is achieved by inserting a prosthesis slightly larger than the prepared bone-bed, generating compression hoop stresses, and obtaining a so-called “press-fit.”
Debate regarding the relative merits of cemented versus uncemented hips continues today as vehemently as it has done since their introduction. Modern fixation techniques and implants using cement have resulted in better outcome than older cemented and historical uncemented series.1 However, uncemented devices over the past 30 years have shown improved stability equal, in many cases, to cemented fixation. In spite of this, the authors’ preference is to use a fully cemented hip replacement in the majority of cases and a cemented femoral stem in all cases. Our these reasons form the substance of the following review article.
Features of Cemented and Uncemented Arthroplasty Designs
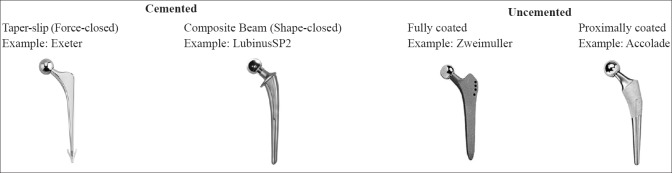
Cemented stems fall into two broad categories: taper-slip or “force-closed” and composite beam or “shape-closed.” Taper-slip stems, such as the Exeter stem, are collarless and have a highly polished surface finish. They achieve stability through micromotion at the prosthesis-cement interface promoting slight subsidence of the stem within the cement mantle, the generation of radial stresses, and ultimately compression at the bone-cement and prosthesis-cement interfaces.2 Composite beam stems, such as the later versions of the Charnley Stem, aim to achieve stability through a solid bond between stem, cement and bone, maintaining the position of the stem within the mantle. Design features including rough surface finish and the presence of a collar are intended to improve stability at the prosthesis-cement interface.2
Cemented sockets tend to be thick-walled polyethylene cups. They usually have grooves in the outer surface to increase stability within the cement mantle, and an embedded wire marker to allow the assessment of position on postoperative X-rays. Modern designs such as the Exeter Contemporary flanged acetabular cup have PMMA spacer beads to ensure a uniform cement mantle and avoid “bottoming out” which results in a thin discontinuous cement mantle. A flange at the rim of the component aids in cement pressurization during cup insertion.
Uncemented stems exhibit a large range of designs, employing wedged, tapered, cylindrical, modular and anatomic shapes, and with the addition of proximal fins and ribs for added stability, and splines, flutes, and slots to reduce modulus of elasticity.3 [Figure 1] More recently, shorter stem designs have been introduced with the aim of creating a more “physiological” loading of the proximal femur and reducing the problems of stress shielding.4 Whatever the stem design, the aims are the same: To maximize initial stability and osseous contact, to hold the prosthesis steady while the surrounding bone adheres onto or into it, over subsequent weeks, months, or years.5,6 Initial stability is crucial because the degree of micromotion at this stage influences the tissue that forms at the bone prosthesis interface. Micromotion of greater than 150 μm leads to the formation of fibrous tissue, between 40 and 150 μm results in a mixture of bone and fibrous tissue and below 20 μm results predominantly in bone formation.7,8,9
Figure 1.
Examples of different cemented and uncemented femoral stem designs
Uncemented prostheses are surface-engineered in one of two ways, encouraging bony interlock either by on- or in-growth. On-growth surfaces are created by grit blasting or plasma spraying hydroxyapatite (HA) onto the component to create a textured surfaced, with multiple indentations onto which bone can grow.3,10 In-growth surfaces are created using sintered beads, fiber mesh and porous metals, which create microscopic pores into which bone can grow. Optimum pore size for bony in-growth is 50–400 μm.11,12,13 Optimum percentage of voids within the coating should be 30%–50% to maintain mechanical strength.13,14,15
The potential for improved bonding, and thus stability, through coating prostheses with bioactive materials such as HA and tricalcium phosphate, has attracted increasing interest. These compounds actively stimulate osteoblasts, rather than just providing a scaffold for adherence. Some studies have shown improved weight transfer and radiographic appearance in the short term1,16,17,18,19 while others have found no advantages.20 No improvement has been demonstrated with regard to revision rate or long-term outcomes.21,22
Component coating can be complete or partial. Complete coating presents a large surface area for rigid fixation, but this may reduce loading of the proximal bone, leading to stress-shielding. Proximal coating only, channels the forces of weight bearing through the femoral metaphysis, but provides a smaller area for stable fixation. In either case, circumferential coating provides a barrier to the ingress of joint fluid and particulate debris and thus to the development of osteolysis.18,23,24,25
Uncemented sockets have porous coating over their whole circumference, with fixation using screws, pegs, or spikes to achieve initial stability. Most systems use a metal shell with a polyethylene liner fastened securely inside it. Various locking mechanisms have been designed to facilitate this. Motion between the shell and liner can be a source of particle debris, so-called “backside wear”.
A Brief History of Cementing
German surgeon Themistocles Gluck (1891) who, proposed the use of bone-cement in arthroplasty. The previous year in Berlin, he had performed the first total joint replacement using a hinged, ivory prosthetic knee. He had also developed models for shoulder, elbow, and wrist arthroplasties. To secure these to bone, he experimented with a variety of materials including copper amalgam, plaster of Paris, and stone putty.26 Although his efforts were remarkably successful in the short-term, they invariably failed due to infection or loosening, and ultimately he gave up his work on prosthetics to pursue other areas of medical research.
Pioneering work in the field of PMMA technology is credited to German Chemist Otto Röhm, who patented “Plexiglas” in 1933. In the lead up to World War One, interest in this material and its use in submarine periscopes, gun turrets, and aeroplane canopies grew significantly.27 In 1936, the German Kultzer Company found that a mixture of methyl methacrylate monomer and ground polymer produced a dough that could be molded and polymerized to a solid mass by heating in the presence of benzoyl peroxide.28,29 They went on to develop cold-cured PMMA, which hardens at room temperature. Following this, the use of acrylic resins for dentures and cranioplasty prostheses developed during the 1940s.29
During the 1950s, the use of cement in joint arthroplasty became a viable possibility. In 1951 Sven Kiaer and Knud Jansen of Copenhagen attached plastic cups to the femoral head using acrylic cement. They reported their technique at an international orthopedics meeting, attended by Sir John Charnley, whose work in the area of cemented hip arthroplasty is well known.30 In 1953, Edward Haboush, working at the Hospital for Joint Disease in New York, published a report of his work with a hip prosthesis and acetabular cup both held in place with dental acrylic.31 It was Charnley, though, who is credited with popularizing the use of PMMA bone-cement in arthroplasty.32 He had meticulously studied the properties of PMMA outside the body and in 1958, he performed his first arthroplasty in Manchester. In his pivotal report of his first six cases in the Journal of Bone and Joint Surgery in 1960,33 he emphasized that the cement dough acted as a grout rather than a glue, achieving its fixation by interlock rather than adhesion, and that the cement should be forced into every crevice in the interior of the femur so that the weight of the body was dispersed over a large area of bone.30,34
Although Charnley's hip arthroplasties did well, with an incidence of mechanical failure at the cement-bone interface of only 2.2% at 8 years,35 other surgeons had less successful outcomes. Unfortunately, the failure of many early, cemented, THAs was attributed to the cement itself, rather than cementing technique or implant design. Space was therefore created for the development of uncemented alternatives.
McKee and Watson-Farrar documented an early model of an uncemented artificial hip joint between 1956 and 1960. They trialed it in 40 patients and reported 51% “good” or “fair” clinical results.36 Despite the outcomes of early uncemented THA being poor, uncemented prostheses gained favor and their use, particularly in the United States of America, increased.
In 1981, on the basis of human retrieval studies, Albrektsson et al. described “osseointegration” as “the attachment of lamellar bone to implants without intervening fibrous tissue.”14 It became understood that the amplitude of micromotion was directly related to the type of tissue that adhered to the prosthesis; where micromotion was very low bone would form, and where higher, it would be fibrous tissue.7,8,9 It was also established that micromotion could be minimized with adequate osseous contact and firm fixation of the implant.5 The first uncemented implant, the anatomic medullary locking implant, was approved by the American Food and Drug Administration in 1983. In 2012, 93% of THA in the US were uncemented. Despite an increasing trend toward the use of uncemented fixation, evidence is still weighted in favor of cement.36
First generation cementing techniques were fairly crude and involved antegrade filling of an unplugged femoral canal. The second generation introduced the use of a femoral restrictor to improve cementing pressures. Retrograde filling of the femoral canal marked the third generation of cementation. Modern, fourth generation cementation with canal plug, serial high-pressure pulse lavage, retrograde filling of the femoral canal followed by proximal pressurization and late insertion of an implant into viscous cement is widely practiced and can be considered the gold standard in modern cemented arthroplasty practice.
Properties of Acrylic Cement
Bone-cement is supplied as a powder and a liquid. The powder includes the cement (acrylic) polymer along with an initiator (di-benzoyl peroxide), a radio-opacifier (zirconium oxide or barium sulfate) and often an antibiotic. The liquid contains the monomer along with a stabilizer (hydroquinone) to prevent premature polymerization, and an activator or accelerator (dimethyl-para-toluidine) to encourage polymerization at room temperature.37,38 As the powdered polymer and liquid monomer are mixed, polymerization occurs, and a viscous dough is formed. It is the viscosity of cement that determines its handling and working properties.
The term “bone-cement” is something of a misnomer. Bone-cement has no adhesive properties, rather, it acts as grout, forming a close mechanical interlock between the bone interstices and the prosthesis, such that physiological loads can be evenly distributed through it and transmitted to the bone.37,39 The creation of a strong and extensive micro-interlock is the key to success with cemented prostheses. Such interlock optimizes load-carriage to the bone and reduces the amplitude of repeated cycles of loading and unloading. This, in turn, minimizes the formation of a cellular layer and subsequent fibrous tissue at the bone-cement interface, and thus the risk of loosening.39 Clearly the success of a cemented stem depends on good surgical technique, and hence, it is perhaps reasonable to provide a brief summary of the key points.
Optimum Cementing Technique
The excellent survival rates seen with modern cemented THA are due to rigorous implementation of modern cementing techniques. Optimizing the mechanical interlock at the bone-cement interface can be achieved by ensuring good cement penetration secondary to good pressurization.40,41,42,43,44 Experiments in Exeter45 and elsewhere,46,47 confirmed that improved cementing is associated with better postoperative radiographs.
In the early days of hip replacement, little significance was attributed to the technique of cementation. Work from Robin Ling in Exeter and John Charnley in Wrightington furthered understanding of the mechanical properties of bone-cement and the importance of surgical technique in improving outcomes in THA. It became clear that to deeply and densely interdigitate cement into trabecular bone, and to form a strong mechanical interlock, effort had to be made to first clear the bone interstices of fat and blood. Viscous cement could then be inserted into dry, clean bone and pressurized, maintaining the pressure, before, during and after the insertion of the prosthesis. The key stages are as follows: Before cementation and indeed after each instrumentation of the femur, the femoral canal is cleaned with pulse lavage and suctioned, to remove fat, blood, and other debris. Brushes are not used as this risks damaging the strong cancellous bone into which cement is inserted. Lavage is also important to reduce the pulmonary physiological disturbance and embolic load, and it should be carried out before any instrumentation of the medullary cavity.48,49,50,51,52 Following lavage, the femoral canal is plugged at an appropriate depth using a well-fitting cement restrictor. This ensures good filling and pressurization and reduces physiological disturbance during cement and prosthesis insertion.53,54 Gauze soaked in saline or hydrogen peroxide is then packed into the femoral canal while the cement is being prepared.
Cement is mixed in a vacuum for the purpose of fume extraction.37 Vacuum mixing also serves to reduce cement porosity, but, although reference is often made to this fact in the literature, it has little effect on fixation (porosity predominantly affects the tensile strength of cement while the main force to which cement is subjected in THA is compression, in which it is strongest). Cement is introduced into the femoral canal in a retrograde manner using a cement gun with a proximal seal to maintain pressure in the femoral canal. The pressure applied to the cement has to exceed blood pressure to prevent the cement from being pushed back out of the cancellous bone by bleeding. This pressure needs to be maintained until the viscosity is sufficient to resist extrusion.
At the optimum time, usually 4–5 min into polymerization, the stem is inserted in the desired anteversion and to the preplanned depth as judged by preoperative templating. The taper design of many successful polished cemented stems came about because Clive Lee and Robin Ling, inventors of the Exeter Hip, recognized that a taper was the ideal shape to pressurize cement during stem insertion. This pressure (and also the alignment of the stem in the femoral canal), can be improved by placing a thumb over the calcar during insertion. A proximal seal is then held around the neck of the stem to maintain pressure until cement polymerization is complete.
Acetabular cementing follows the same principles. The labrum and surrounding osteophytes are removed and the acetabulum is decorticated, along with any cysts, to reveal trabecular bone. Milled bone graft is placed in cysts and on the medial wall in order to enhance fixation and to prevent cement extrusion under the transverse acetabular ligament.55 Multiple drill holes are made to maximize macro-interlock. The bone of the acetabulum is then washed with pulse lavage and packed with a swab soaked in saline or hydrogen peroxide to create a dry surface for cementing. Cement is introduced and pressurized until it is optimal for component implantation.
Benefits of Cemented Total Hip Arthroplasty
There are a number of ways in which cemented THAs outperform their uncemented relatives:
Survivorship
At The Princess Elizabeth Orthopaedic Centre (PEOC), Exeter, we have reported excellent survivorship of cemented components in THA. Kaplan–Meier survivorship of the Exeter contemporary flanged cemented acetabular component, at 12.5 years with aseptic loosening as the end point was 100%,56 as was survivorship of the cemented Exeter Universal femoral stem at 17 years.57 Similar results have been reported by other units, both in the UK and internationally.58,59
The 2014 report from the National Joint Registry of England and Wales found Kaplan–Meier estimates of cumulative percentage probability of revision 10 years following primary operation to be 3.13 (3.00–3.26) for cemented hips, compared to 7.60 (7.35–7.85) for uncemented hips.60 The Swedish Hip Arthroplasty Register also demonstrates superior survivorship of cemented over uncemented THAs with revision free component survival at 10 years of 94% versus 85% (P < 0.001).61 No age or diagnosis group was found to benefit from the use of uncemented THA.61
The New Zealand Joint Registry reports that the overall all-cause revision rate is lower in cemented than uncemented THA, although, in contrast to the larger registries above, they found uncemented acetabular components performed better in the medium term (9 years) across all age groups.62 The combined Nordic Arthroplasty Database found that in patients aged 65–74 and 75 or older, the 10-year survival of cemented implants was higher than that of uncemented, hybrid and reverse-hybrid implants. In patients aged 55–64, survivorship of cemented and uncemented implants was found to be similar.63
An alternative way of looking at data from arthroplasty registers is to consider the revision burden; the proportion of THAs that are revisions as opposed to primary procedures. In the United States, where the vast majority of stems are uncemented, the revision burden is approximately 18%, whereas in Sweden, where the vast majority of stems are cemented, this figure is 6%.64 Revision burden is a particularly worthy of scrutiny when one considers that mortality following revision surgery is more than double the rate after primary surgery. Avoiding revision surgery thus has implications for the mortality associated with THA.65,66,67
A number of meta-analyses and literature reviews have concluded that cemented fixation is gold standard in THA in terms of re-operation rate in older patients68 or in all patients regardless of age.69,70 Two reviews looking particularly at acetabular fixation, found cemented acetabular components to have the lowest all-cause re-operation rate and to demonstrate more reliable performance beyond the first postoperative decade.71,72
The British Medical Journal in 2015 published a report on revision rates in THA following an analysis of registry evidence. This concludes that cemented devices have better revision performance than uncemented devices and that “greater use of cementless as opposed to cemented devices does not reflect the apparent superior performance of cemented devices.”73
Optimum positioning
A cemented stem can be considered to be customized for the patient and can be used in almost all situations, including where there is femoral deformity. The cement mantle allows components to be positioned optimally with respect to the patient's anatomy and leg length. Version and offset can all be altered independently to ensure good restoration of anatomy and a stable, well-functioning hip replacement.64
Specific bone physiology
Cemented components are especially beneficial in osteopenic or osteoporotic bone where deeper penetration of cement provides excellent fixation across a wide surface area, in irradiated bone where biology may be impaired, and in the Dorr C stovepipe femur74 where the enlarged metaphyseal region makes it difficult to gain adequate purchase with an uncemented component.64 Cement also allows the local delivery of antibiotics where indicated. Uncemented stems are less forgiving and may be contra-indicated where bone stock and quality are poor, or where there is abnormal proximal femoral morphology.
Short-term clinical outcomes
While discussion of survivorship and revision reflects the long-term performance of THA, the patients’ experience in the short-term is also of utmost importance. Uncemented stems are associated with a significant risk of thigh pain due to a modulus mismatch between the stiff cobalt chrome stem and the more compliant cortical and cancellous bone.36,64 Multiple studies have demonstrated better pain relief and short-term clinical outcomes, including earlier weight bearing, with cemented THAs. A detailed review of these can be found in the meta analysis of randomized controlled trials comparing cemented and uncemented hips by Abdulkarim et al.75 Some studies have found contrary results; however, a recent review by Rolfson et al. of patients on the Swedish Hip Arthroplasty Register found patient reported outcome measures in the 1st postoperative year were better in uncemented than cemented hips.76
Peri-prosthetic fracture
Thien et al. studied the incidence of periprosthetic fracture around the femoral component in cemented and uncemented hips in the 2 years following implantation. They found a rate of 0.07% for cemented stems and 0.47% for uncemented stems; a relative risk of 8.72 (95% confidence interval, 7.37–10.32); P < 0.0005, albeit in the context of a low absolute risk.77
Femoral impaction grafting
Femoral impaction grafting works better in cemented THA. A medium-term follow-up of 100 stems using a long stem proximally coated uncemented prosthesis demonstrated a 50% failure rate and 10% incidence of aseptic loosening.78 In contrast, a series from PEOC, using polished-tapered stems and the technique described by Steele et al.79 found a rate of aseptic loosening of 1%.80
Ease of revision
Revising cemented polished taper-slip THAs is relatively straightforward. If access is needed to the acetabulum then the stem can easily be knocked out and a new stem re-cemented into the original mantle at the end of the procedure.64 If the stem requires revision to allow change in version or offset, this can be done using the cement-in-cement technique.45
Costs
Uncemented prostheses are generally more expensive than cemented or hybrid options, and their increasing use has contributed to a large increase in the cost of THA. Pennington et al. who carried out a cost-analysis study concluded that uncemented prostheses do not improve health outcomes sufficiently to justify their higher costs.81
Concerns Regarding Cemented Total Hip Arthroplasty
Bone-cement implantation syndrome and mortality
Bone-cement implantation syndrome (BCIS) is a poorly understood phenomenon that currently has no agreed definition.82 It is characterized by a number of clinical features from hypoxia, hypotension, and cardiac arrhythmias to increased peripheral vascular resistance and cardiac arrest.83 It is most commonly associated with, but not restricted to, hip arthroplasty, where it generally occurs at one of five stages femoral reaming, acetabular or femoral cement implantation, insertion of the prosthesis, and joint reduction.83
The pathophysiology of BCIS is unclear. Initial theories focused on the release of methyl methacrylate into the circulation causing vasodilation. More recent research has suggested micro-embolisation of fat, forced out of the marrow and into the bloodstream. Several other mechanisms including histamine release,84 complement activation,85 and endogenous cannabinoid-mediated vasodilatation have also been proposed.86
While there is no clear evidence with regards the effect of anesthetic technique on BCIS, the general principles of management include pre operative identification of high-risk patients, optimization of their cardiovascular reserve before surgery and intra operative maintenance of normovolemia and high inspired oxygen concentrations.82 BCIS is a reversible time limited phenomenon so aggressive resuscitation and supportive treatment are essential to reduce associated morbidity and mortality.82
There is no accurate data regarding rates of BCIS in hip arthroplasty but overall mortality rates have been studied. Sierra, in his review of mortality and contemporary cementing techniques during cemented THA with the Exeter stem, reported one operative death in a series of 9082 total hips over a 17-year period: A 0.01% prevalence of sudden death. With current contemporary cementing techniques and a specialized anesthetic protocol, he suggested the incidence of sudden death during cemented THA should be “near zero.”87 Pennington et al. found no difference in mortality following THA across prosthesis types after adjusting for potential confounders (age, sex, American Society of Anaesthesiologists grade, body mass index, articulation type, funding source, and date of surgery). The hazard rate for mortality after total hip replacement using cemented versus uncemented prostheses was 1.01 (P = 0.75).81 Jämsen et al. in their review of the Finnish hip registry showed no difference in mortality in 4509 octogenarian patients having cemented, uncemented and hybrid hip replacement for primary osteoarthritis.88 Hunt et al. revealed, using data from the National Joint Registry of England and Wales, that the use of cement was unrelated to mortality in 409096 patients undergoing total hip replacement.89 Costa et al. reviewed 16496 femoral neck fractures treated with hemiarthroplasty or total hip replacement and showed that “overall peri-operative mortality is significantly lower when cement is used.”90 However, to achieve good outcomes, attention to surgical details as outlined above is essential.
Conclusion
Cemented THA is an operation with abundant evidence of excellent outcomes. Registry data and reports confirm excellent survivorship and low revision rates. The stem can be placed in the optimum position for a patient's anatomy with length, rotation and offset, all independently determined by the surgeon. It can be used in patients with femoral deformity, osteoporotic bone, or following radiotherapy, and in young or old alike. Short-term clinical outcomes in terms of pain relief and early mobilisation are good. Femoral impaction grafting has shown better results in combination with cemented THA, and revision in cemented THA is straightforward using the cement-in-cement technique.
Many of the reasons that may have caused surgeons in the past to move away from the use of cemented implants have been found to be unwarranted and the evidence does not support the increasing using of uncemented implants. In particular, the risk of mortality in cemented THA has not been found to be higher than uncemented THA, and importantly in today's economic climate, economic analysis confirms that cemented THA is a highly cost-effective option.
Financial support and sponsorship
The senior author's institution receives research funding from Stryker Corporation, Mahwah, NJ, USA
Conflicts of interest
The senior author receives royalties from Stryker Corporation, Mahwah, NJ, USA
References
- 1.Thanner J. The acetabular component in total hip arthroplasty. Evaluation of different fixation principles. Acta Orthop Scand Suppl. 1999;286:1–41. [PubMed] [Google Scholar]
- 2.Davies N, Jackson W, Price A, Rees J, Lavy C. FRCS Trauma and Orthopaedics Viva. Oxford: Oxford University Press; 2012. [Google Scholar]
- 3.Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011;93:500–9. doi: 10.2106/JBJS.J.00774. [DOI] [PubMed] [Google Scholar]
- 4.Castelli CC, Rizzi L. Short stems in total hip replacement: Current status and future. Hip Int. 2014;24(Suppl 10):S25–8. doi: 10.5301/hipint.5000169. [DOI] [PubMed] [Google Scholar]
- 5.Galante J, Rostoker W, Lueck R, Ray RD. Sintered fiber metal composites as a basis for attachment of implants to bone. J Bone Joint Surg Am. 1971;53:101–14. [PubMed] [Google Scholar]
- 6.Zweymüller KA, Lintner FK, Semlitsch MF. Biologic fixation of a press-fit titanium hip joint endoprosthesis. Clin Orthop Relat Res. 1988;235:195–206. [PubMed] [Google Scholar]
- 7.Engh CA, O’Connor D, Jasty M, McGovern TF, Bobyn JD, Harris WH. Quantification of implant micromotion, strain shielding, and bone resorption with porous-coated anatomic medullary locking femoral prostheses. Clin Orthop Relat Res. 1992;285:13–29. [PubMed] [Google Scholar]
- 8.Pilliar RM, Lee JM, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res. 1986;208:108–13. [PubMed] [Google Scholar]
- 9.Jasty M, Bragdon C, Burke D, O’Connor D, Lowenstein J, Harris WH. In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Joint Surg Am. 1997;79:707–14. doi: 10.2106/00004623-199705000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Mirza SB, Dunlop DG, Panesar SS, Naqvi SG, Gangoo S, Salih S. Basic science considerations in primary total hip replacement arthroplasty. Open Orthop J. 2010;4:169–80. doi: 10.2174/1874325001004010169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook SD, Thomas KA, Haddad RJ., Jr Histologic analysis of retrieved human porous-coated total joint components. Clin Orthop Relat Res. 1988;234:90–101. [PubMed] [Google Scholar]
- 12.Spector M. Historical review of porous-coated implants. J Arthroplasty. 1987;2:163–77. doi: 10.1016/s0883-5403(87)80024-4. [DOI] [PubMed] [Google Scholar]
- 13.Berry DJ. Primary total hip arthroplasty. In: Chapman MW, editor. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott: Williams and Wilkins; 2001. pp. 2769–90. [Google Scholar]
- 14.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–70. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 15.Haddad RJ, Jr, Cook SD, Thomas KA. Biological fixation of porous-coated implants. J Bone Joint Surg Am. 1987;69:1459–66. [PubMed] [Google Scholar]
- 16.Abrahams TG, Crothers OD. Radiographic analysis of an investigational hydroxyapatite-coated total hip replacement. Invest Radiol. 1992;27:779–84. [PubMed] [Google Scholar]
- 17.Chambers B, St. Clair SF, Froimson MI. Hydroxyapatite-coated tapered cementless femoral components in total hip arthroplasty. J Arthroplasty. 2007;22(4 Suppl 1):71–4. doi: 10.1016/j.arth.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 18.Dorr LD, Wan Z, Song M, Ranawat A. Bilateral total hip arthroplasty comparing hydroxyapatite coating to porous-coated fixation. J Arthroplasty. 1998;13:729–36. doi: 10.1016/s0883-5403(98)90023-7. [DOI] [PubMed] [Google Scholar]
- 19.Thanner J, Kärrholm J, Herberts P, Malchau H. Porous cups with and without hydroxylapatite-tricalcium phosphate coating: 23 matched pairs evaluated with radiostereometry. J Arthroplasty. 1999;14:266–71. doi: 10.1016/s0883-5403(99)90050-5. [DOI] [PubMed] [Google Scholar]
- 20.Rothman RH, Hozack WJ, Ranawat A, Moriarty L. Hydroxyapatite-coated femoral stems. A matched-pair analysis of coated and uncoated implants. J Bone Joint Surg Am. 1996;78:319–24. doi: 10.2106/00004623-199603000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Paulsen A, Pedersen AB, Johnsen SP, Riis A, Lucht U, Overgaard S. Effect of hydroxyapatite coating on risk of revision after primary total hip arthroplasty in younger patients: Findings from the Danish Hip Arthroplasty Registry. Acta Orthop. 2007;78:622–8. doi: 10.1080/17453670710014310. [DOI] [PubMed] [Google Scholar]
- 22.Camazzola D, Hammond T, Gandhi R, Davey JR. A randomized trial of hydroxyapatite-coated femoral stems in total hip arthroplasty: A 13-year follow-up. J Arthroplasty. 2009;24:33–7. doi: 10.1016/j.arth.2008.01.129. [DOI] [PubMed] [Google Scholar]
- 23.Emerson RH, Jr, Sanders SB, Head WC, Higgins L. Effect of circumferential plasma-spray porous coating on the rate of femoral osteolysis after total hip arthroplasty. J Bone Joint Surg Am. 1999;81:1291–8. doi: 10.2106/00004623-199909000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Sinha RK, Dungy DS, Yeon HB. Primary total hip arthroplasty with a proximally porous-coated femoral stem. J Bone Joint Surg Am. 2004;86-A:1254–61. doi: 10.2106/00004623-200406000-00019. [DOI] [PubMed] [Google Scholar]
- 25.Urban RM, Jacobs JJ, Sumner DR, Peters CL, Voss FR, Galante JO. The bone-implant interface of femoral stems with non-circumferential porous coating. J Bone Joint Surg Am. 1996;78:1068–81. doi: 10.2106/00004623-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Eynon-Lewis NJ, Ferry D, Pearse MF. Themistocles Gluck: An unrecognised genius. BMJ. 1992;305:1534–6. doi: 10.1136/bmj.305.6868.1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nottrott M. Acrylic bone cements: Influence of time and environment on physical properties. Acta Orthop Suppl. 2010;81:1–27. doi: 10.3109/17453674.2010.487929. [DOI] [PubMed] [Google Scholar]
- 28.Arora M, Chan EK, Gupta S, Diwan AD. Polymethylmethacrylate bone cements and additives: A review of the literature. World J Orthop. 2013;4:67–74. doi: 10.5312/wjo.v4.i2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cabraja M, Klecan J, Phillips GO. Polymethyl methacrylate: An acceptable material for tissue augmentation and reconstruction. In: Phillips GO, editor. Legal Basis of Global Tissue Banking: A Proactive Clinical Perspective. New Jersey, London, Singapore, Beijing, Shanghai, Hong Kong, Chennai: World Scientific; 2016. pp. 253–74. [Google Scholar]
- 30.Draenert K, Draenert Y, Garde U, Ulrich CH. Manual of Cementing Technique. Berlin: Berlin Heidelberg, Springer-Verlag; 1999. [Google Scholar]
- 31.Haboush EJ. A new operation for arthroplasty of the hip based on biomechanics, photoelasticity, fast-setting dental acrylic, and other considerations. Bull Hosp Joint Dis. 1953;14:242–77. [PubMed] [Google Scholar]
- 32.Peltier LF. Orthopaedics: History and Iconography. San Francisco: Norman Publishing; 1993. [Google Scholar]
- 33.Charnley J. Anchorage of the femoral head prosthesis to the shaft of the femur. J Bone Joint Surg Br. 1960;42-B:28–30. doi: 10.1302/0301-620X.42B1.28. [DOI] [PubMed] [Google Scholar]
- 34.Gomez PF, Morcuende JA. A historical and economic perspective on Sir John Charnley, Chas F. Thackray Limited, and the early arthoplasty industry. Iowa Orthop J. 2005;25:30–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Griffith MJ, Seidenstein MK, Williams D, Charnley J. Eight year results of Charnley arthroplasties of the hip with special reference to the behavior of cement. Clin Orthop Relat Res. 1978;13:724–36. [PubMed] [Google Scholar]
- 36.Yamada H, Yoshihara Y, Henmi O, Morita M, Shiromoto Y, Kawano T, et al. Cementless total hip replacement: Past, present, and future. J Orthop Sci. 2009;14:228–41. doi: 10.1007/s00776-008-1317-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaishya R, Chauhan M, Vaish A. Bone cement. J Clin Orthop Trauma. 2013;4:157–63. doi: 10.1016/j.jcot.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fenton P, Rampurada A, Quereshi F. USM Orthopaedic. [Last accessed on 2016 Dec 29]. Available from: https://www.usmorthopaedic.wordpress.com/2009/08/24/bone-cement-its-history-its-properties-anddevelopments-in-its-use/2009 .
- 39.Fagan M, Ling RS. Principles of cemented implant fixation. In: Ling RS, Lee AJ, GIe GA, Timperley AJ, Hubble MJ, Howell JR, et al., editors. The Exeter Hip: 40 Year of Innovation in Total Hip Arthroplasty. Exeter, UK: Exeter Hip Publishing; 2010. pp. 13–23. [Google Scholar]
- 40.Halawa M, Lee AJ, Ling RS, Vangala SS. The shear strength of trabecular bone from the femur, and some factors affecting the shear strength of the cement-bone interface. Arch Orthop Trauma Surg. 1978;92:19–30. doi: 10.1007/BF00381636. [DOI] [PubMed] [Google Scholar]
- 41.Krause WR, Krug W, Miller J. Strength of the cement-bone interface. Clin Orthop Relat Res. 1982;163:290–9. [PubMed] [Google Scholar]
- 42.Panjabi MM, Goel VK, Drinker H, Wong J, Kamire G, Walter SD. Effect of pressurization on methylmethacrylate-bone interdigitation: An in vitro study of canine femora. J Biomech. 1983;16:473–80. doi: 10.1016/0021-9290(83)90061-1. [DOI] [PubMed] [Google Scholar]
- 43.Lee AJ, Ling RS. A device to improve the extrusion of bone cement into the bone of the acetabulum in the replacement of the hip joint. Biomed Eng. 1974;9:522–4. [PubMed] [Google Scholar]
- 44.Markolf KL, Amstutz HC. Penetration and flow of acrylic bone cement. Clin Orthop Relat Res. 1976;121:99–102. [PubMed] [Google Scholar]
- 45.Ling RS, Lee AJ, Gie GA, Timperley AJ, Hubble MW, Howell JR, et al. The Exeter Hip: 40 Years of Innovation in Total Hip Arthoplasty. 1st ed. Exeter: Exeter Hip Publishing; 2010. [Google Scholar]
- 46.Barrack RL, Mulroy RD, Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A -year radiographic review. J Bone Joint Surg Br. 1992;74:385–9. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 47.Ritter MA, Zhou H, Keating CM, Keating EM, Faris PM, Meding JB, et al. Radiological factors influencing femoral and acetabular failure in cemented Charnley total hip arthroplasties. J Bone Joint Surg Br. 1999;81:982–6. doi: 10.1302/0301-620x.81b6.9634. [DOI] [PubMed] [Google Scholar]
- 48.Byrick RJ, Bell RS, Kay JC, Waddell JP, Mullen JB. High-volume, high-pressure pulsatile lavage during cemented arthroplasty. J Bone Joint Surg Am. 1989;71:1331–6. [PubMed] [Google Scholar]
- 49.Christie J, Robinson CM, Singer B, Ray DC. Medullary lavage reduces embolic phenomena and cardiopulmonary changes during cemented hemiarthroplasty. J Bone Joint Surg Br. 1995;77:456–9. [PubMed] [Google Scholar]
- 50.Breusch SJ, Reitzel T, Schneider U, Volkmann M, Ewerbeck V, Lukoschek M. Cemented hip prosthesis implantation – Decreasing the rate of fat embolism with pulsed pressure lavage. Orthopade. 2000;29:578–86. doi: 10.1007/s001320050496. [DOI] [PubMed] [Google Scholar]
- 51.Clarius M, Heisel C, Breush SJ. Breusch SJ, Malchau H, editors. Cemented hip prosthesis implantation – Decreasing the rate of fat embolism with pulsed pressure lavage. Orthopade. 2000;29:578–86. doi: 10.1007/s001320050496. [DOI] [PubMed] [Google Scholar]
- 52.Malchau H, Herberts P, Soderman P, Oden A. Prognosis of Total Hip Replacements. Update and Validation of Results from the Swedish National Hip Arthroplasty Register 1979-1998; Presented at the 67th Annual Meeting of the American Academy of Orthopaedic Surgeons, Orlando, March 15-19. 2000 [Google Scholar]
- 53.Heisel C, Norman T, Rupp R, Pritsch M, Ewerbeck V, Breusch SJ. In vitro performance of intramedullary cement restrictors in total hip arthroplasty. J Biomech. 2003;36:835–43. doi: 10.1016/s0021-9290(03)00017-4. [DOI] [PubMed] [Google Scholar]
- 54.McCaskie AW, Barnes MR, Lin E, Harper WM, Gregg PJ. Cement pressurisation during hip replacement. J Bone Joint Surg Br. 1997;79:379–84. doi: 10.1302/0301-620x.79b3.7301. [DOI] [PubMed] [Google Scholar]
- 55.Acharya A, Petheram T, Hubble M, Howell J. Sealing the acetabular notch in cemented total hip arthroplasty. A radiological review of 380 cases. Acta Orthop Belg. 2010;76:199–204. [PubMed] [Google Scholar]
- 56.Maggs JL, Smeatham A, Whitehouse SL, Charity J, Timperley AJ, Gie GA. The exeter contemporary flanged cemented acetabular component in primary total hip arthroplasty. Bone Joint J. 2016;98-B:307–12. doi: 10.1302/0301-620X.98B3.35901. [DOI] [PubMed] [Google Scholar]
- 57.Carrington NC, Sierra RJ, Gie GA, Hubble MJ, Timperley AJ, Howell JR. The Exeter Universal cemented femoral component at 15 to 17 years: An update on the first 325 hips. J Bone Joint Surg Br. 2009;91:730–7. doi: 10.1302/0301-620X.91B6.21627. [DOI] [PubMed] [Google Scholar]
- 58.Hook S, Moulder E, Yates PJ, Burston BJ, Whitley E, Bannister GC. The Exeter Universal stem: A minimum ten-year review from an independent centre. J Bone Joint Surg Br. 2006;88:1584–90. doi: 10.1302/0301-620X.88B12.18345. [DOI] [PubMed] [Google Scholar]
- 59.Fujita H, Katayama N, Iwase T, Otsuka H. Multi-center study of use of the Exeter stem in Japan: Evaluation of 100 primary THA. J Orthop Sci. 2012;17:370–6. doi: 10.1007/s00776-012-0237-5. [DOI] [PubMed] [Google Scholar]
- 60.The NJR Centre. National Joint Registry for England and Wales. 11th Annual Report. The NJR Centre, Hemel Hempstead. 2014 [Google Scholar]
- 61.Hailer NP, Garellick G, Kärrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hooper GJ, Rothwell AG, Stringer M, Frampton C. Revision following cemented and uncemented primary total hip replacement: A seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–8. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 63.Mäkelä KT, Matilainen M, Pulkkinen P, Fenstad AM, Havelin L, Engesaeter L, et al. Failure rate of cemented and uncemented total hip replacements: Register study of combined Nordic database of four nations. BMJ. 2014;348:7592. doi: 10.1136/bmj.f7592. [DOI] [PubMed] [Google Scholar]
- 64.Murray DW. Cemented femoral fixation: The North Atlantic divide. Bone Joint J. 2013;95-B(11 Suppl A):51–2. doi: 10.1302/0301-620X.95B11.32976. [DOI] [PubMed] [Google Scholar]
- 65.Sharkey PF, Shastri S, Teloken MA, Parvizi J, Hozack WJ, Rothman RH. Relationship between surgical volume and early outcomes of total hip arthroplasty: Do results continue to get better? J Arthroplasty. 2004;19:694–9. doi: 10.1016/j.arth.2004.02.040. [DOI] [PubMed] [Google Scholar]
- 66.Doro C, Dimick J, Wainess R, Upchurch G, Urquhart A. Hospital volume and inpatient mortality outcomes of total hip arthroplasty in the United States. J Arthroplasty. 2006;21(6 Suppl 2):10–6. doi: 10.1016/j.arth.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 67.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–33. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]
- 68.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: The uncemented paradox. Clin Orthop Relat Res. 2013;471:2052–9. doi: 10.1007/s11999-013-2941-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: A systematic review. PLoS One. 2010;5:e13520. doi: 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM., Jr Comparison of cemented and uncemented fixation in total hip replacement: A meta-analysis. Acta Orthop. 2007;78:315–26. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 71.Clement ND, Biant LC, Breusch SJ. Total hip arthroplasty: To cement or not to cement the acetabular socket? A critical review of the literature. Arch Orthop Trauma Surg. 2012;132:411–27. doi: 10.1007/s00402-011-1422-2. [DOI] [PubMed] [Google Scholar]
- 72.Toossi N, Adeli B, Timperley AJ, Haddad FS, Maltenfort M, Parvizi J. Acetabular components in total hip arthroplasty: Is there evidence that cementless fixation is better? J Bone Joint Surg Am. 2013;95:168–74. doi: 10.2106/JBJS.K.01652. [DOI] [PubMed] [Google Scholar]
- 73.Kandala NB, Connock M, Pulikottil-Jacob R, Sutcliffe P, Crowther MJ, Grove A, et al. Setting benchmark revision rates for total hip replacement: Analysis of registry evidence. BMJ. 2015;350:h756. doi: 10.1136/bmj.h756. [DOI] [PubMed] [Google Scholar]
- 74.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993;14:231–42. doi: 10.1016/8756-3282(93)90146-2. [DOI] [PubMed] [Google Scholar]
- 75.Abdulkarim A, Ellanti P, Motterlini N, Fahey T, O’Byrne JM. Cemented versus uncemented fixation in total hip replacement: A systematic review and meta-analysis of randomized controlled trials. Orthop Rev (Pavia) 2013;5:e8. doi: 10.4081/or.2013.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rolfson O, Garellick G, Kärrholm J, Donahue GS, Hallsten M, Nemes S, et al. Patient-reported outcomes in cemented and uncemented total hip replacements. Hip Int. 2016;26:451–7. doi: 10.5301/hipint.5000371. [DOI] [PubMed] [Google Scholar]
- 77.Thien TM, Chatziagorou G, Garellick G, Furnes O, Havelin LI, Mäkelä K, et al. Periprosthetic femoral fracture within two years after total hip replacement: Analysis of 437,629 operations in the nordic arthroplasty register association database. J Bone Joint Surg Am. 2014;96:e167. doi: 10.2106/JBJS.M.00643. [DOI] [PubMed] [Google Scholar]
- 78.Nickelsen TN, Erenbjerg M, Retpen JB, Solgaard S. Femoral revision with impaction allografting and an uncemented femoral component. Hip Int. 2008;18:278–85. doi: 10.1177/112070000801800403. [DOI] [PubMed] [Google Scholar]
- 79.Steele R, Lamberton TD, Gie GA. Revision of the femoral component: Impaction grafting. In: Ling RS, Lee AJ, Gie GA, Timperley AJ, Hubble MJ, Howell JR, et al., editors. The Exeter Hip: 40 Years of Innovation in Total Hip Arthroplasty. Exeter: Exeter Hip Publishing; 2010. pp. 321–8. [Google Scholar]
- 80.Wilson MJ, Hook S, Whitehouse SL, Timperley AJ, Gie GA. Femoral impaction bone grafting in revision hip arthroplasty: 705 cases from the originating centre. Bone Joint J. 2016;98-B:1611–9. doi: 10.1302/0301-620X.98B12.37414. [DOI] [PubMed] [Google Scholar]
- 81.Pennington M, Grieve R, Sekhon JS, Gregg P, Black N, van der Meulen JH. Cemented, cementless, and hybrid prostheses for total hip replacement: Cost effectiveness analysis. BMJ. 2013;346:f1026. doi: 10.1136/bmj.f1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Khanna G, Cernovsky J. Bone cement and the implications for anaesthesia. Br J Anaesth. 2012;12:213–216. [Google Scholar]
- 83.Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009;102:12–22. doi: 10.1093/bja/aen328. [DOI] [PubMed] [Google Scholar]
- 84.Tryba M, Linde I, Voshage G, Zenz M. Histamine release and cardiovascular reactions to implantation of bone cement during total hip replacement. Anaesthesist. 1991;40:25–32. [PubMed] [Google Scholar]
- 85.Lewis RN. Some studies of the complement system during total hip replacement using bone cement under general anaesthesia. Eur J Anaesthesiol. 1997;14:35–9. doi: 10.1046/j.1365-2346.1997.00084.x. [DOI] [PubMed] [Google Scholar]
- 86.Motobe T, Hashiguchi T, Uchimura T, Yamakuchi M, Taniguchi N, Komiya S, et al. Endogenous cannabinoids are candidates for lipid mediators of bone cement implantation syndrome. Shock. 2004;21:8–12. doi: 10.1097/01.SHK.0000094766.36694.49. [DOI] [PubMed] [Google Scholar]
- 87.Sierra RJ, Timperley JA, Gie GA. Contemporary cementing technique and mortality during and after Exeter total hip arthroplasty. J Arthroplasty. 2009;24:325–32. doi: 10.1016/j.arth.2008.01.301. [DOI] [PubMed] [Google Scholar]
- 88.Jämsen E, Eskelinen A, Peltola M, Mäkelä K. High early failure rate after cementless hip replacement in the octogenarian. Clin Orthop Relat Res. 2014;472:2779–89. doi: 10.1007/s11999-014-3641-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hunt LP, Ben-Shlomo Y, Clark EM, Dieppe P, Judge A, MacGregor AJ, et al. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: A retrospective analysis. Lancet. 2013;382:1097–104. doi: 10.1016/S0140-6736(13)61749-3. [DOI] [PubMed] [Google Scholar]
- 90.Costa ML, Griffin XL, Pendleton N, Pearson M, Parsons N. Does cementing the femoral component increase the risk of peri-operative mortality for patients having replacement surgery for a fracture of the neck of femur? Data from the National Hip Fracture Database. J Bone Joint Surg Br. 2011;93:1405–10. doi: 10.1302/0301-620X.93B10.26690. [DOI] [PubMed] [Google Scholar]