Abstract
Being one of the most successful surgeries in the history of medicine, the indications for total hip arthroplasty have widened and are increasingly being offered to younger and fitter patients. This has also led to high expectations for longevity and outcomes. Acetabular cup position has a significant impact on the results of hip arthroplasty as it affects dislocation, abductor muscle strength, gait, limb lengths, impingement, noise generation, range of motion (ROM), wear, loosening, and cup failure. The variables in cup position are depth, height, and angular position (anteversion and inclination). The implications of change in depth of center of rotation (COR) are medialized versus anatomical positioning. As opposed to traditional medialization with beneficial effects on joint reaction force, the advantages of an anatomical position are increasingly recognized. The maintained acetabular offset offers advantages in terms of ROM, impingement, cortical rim press fit, and maintaining medial bone stock. The height of COR influences muscle activity and limb lengths and available bone stock for cup support. On the other hand, ideal angular position remains a matter of much debate and reliably achieving a target angular position remains elusive. This is not helped by variations in the way we describe angular position, with operative, radiologic, or anatomic definitions being used variably to describe anteversion and inclination. Furthermore, pelvic tilt plays a major role in functional positions of the acetabulum. In addition, commonly used techniques of positioning often do not inform us of the real orientation of the pelvis on operating table, with possibility of significant adduction, flexion, and external rotation of the pelvis being possibilities. This review article brings together the evidence on cup positioning and aims to provide a systematic and pragmatic approach in achieving the best position in individual cases.
Keywords: Acetabular cup position, angular position, anteversion, depth, height, inclination, mediolateral, pelvic tilt, superoinferior
MeSH terms: Acetabulum, replacement, arthroplasty, hip, biomechanics
Introduction
Total hip arthroplasty (THA) has become one of the most successful and cost-effective interventions in the history of medicine.1 Over time patient demands have increased significantly, with a greater focus on range of motion and function as well as pain relief. Due to its success, surgery is now offered to younger and fitter patients and thus achieving longevity for the implant has become a bigger challenge.
Accurate biomechanical reconstruction of the joint is essential to achieve function and longevity, with acetabular positioning being a key factor. The consequences of malposition include instability,2 increased wear,3,4,5 impaired muscle function,6 reduced range of motion (ROM),7 impingement,7,8,9 bearing-related noise generation,10,11 poor functional outcomes,12 limb length discrepancy,13,14 and loosening and cup failure.15,16,17 Despite advances in technique, accuracy of cup placement remains variable. This review aims to bring together the evidence on cup positioning and discuss a pragmatic approach to applying these principles.
Section I – Defining Cup Position
Variables defining acetabular positioning are:
Depth or mediolateral position
Height or superoinferior position
Angular placement including inclination and version.
Depth of cup
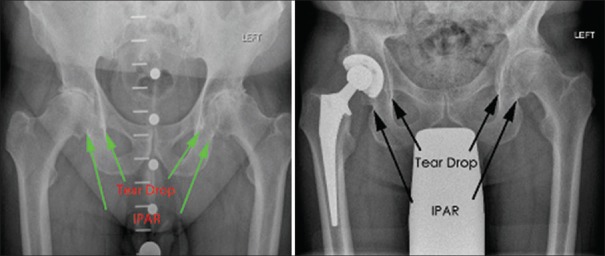
Mediolateral position determines the lever arms of body weight and abductor force and thus joint reaction force (JRF) [Figure 1]. It contributes to offset, a reduction, in which can result in a reduced ROM,7 increased dislocation risk,18 impaired gait,6,19 and accelerated bearing wear [Figure 1].3,4,5
Figure 1.
X-ray pelvis with both hip joints anteroposterior view showing importance of mediolateral position in determining joint reaction force. Medialization reduces body weight lever arm and increases abductor lever arm reducing joint reaction force which is calculated as JRF = BWxB – AbxA. Right side shows femoral offset, acetabular offset, and their contribution to global offset. BW – Body weight, Ab – Abductor force, A – Abductor moment arm, B – Body weight moment arm, JRF – Joint reaction force, AO – Acetabular offset, FO – Femoral offset
The traditional Charnley approach20 advocates medialization of acetabular component to reduce JRF. However, medialization can reduce global offset which is the sum of femoral offset (perpendicular distance from the center of rotation [COR] of femoral head to the central axis of femur) and acetabular offset (distance between COR of femoral head and inner wall of quadrilateral plate/true floor) [Figure 1]. Medialization reduces acetabular contribution to global offset and to restore it, a stem with offset greater than the natural offset of femur is required.
Bonnin et al.9 examined three scenarios of acetabular and femoral offset, namely, medialization of cup with native femoral offset, medialization with increased femoral offset to restore global offset, and anatomic position of cup with femoral offset increased. Medialization resulted in the least stress at cup-head interface and abductor muscles, with optimum outcome when femoral offset was increased to restore the global offset. The increased JRF seen with decreased medialization has been implicated in increased wear in hard-on-hard bearings and squeaking in ceramic-on-ceramic (CoC) bearings.10,11
Downsides of medialization includes reduced ROM, increased risk of bony impingement, risk of microseparation if global offset is not restored resulting in accelerated wear, particularly in hard-on-hard bearings,21,22 loss of bone medially that may have implications for revision surgery, change in working length of muscles, and changed proprioception due to nonanatomic positioning.6
Impingement can be component-to-component (CCI), bone-to-bone (BBI), or component-to-bone impingement.23 Excessive medialization may lead to impingement, especially when peripheral osteophytes are not removed, due to premature contact between proximal femur and pelvic bone/soft tissue (BBI).7,8,9 Conversely, excessively lateral placement of cup, especially in a horizontal position with lateral uncoverage, can also lead to impingement between metal femoral neck and cup liner (CCI) leading to early loosening.24 Simulation studies of ROM before bony impingement found that decreased global offset and length reduce ROM7 with acetabular offset and height having a greater effect than femoral offset and height. Restoring offset by increasing femoral offset or osteophyte removal did not fully restore ROM before impingement. Thus, anatomic positioning of cup, preserving acetabular offset has been proposed.8,24
Component containment is another important consideration when choosing depth of cup. Press-fit uncemented components rely on a rim of peripheral cortical bone for their initial stability.23,25 Medialization past this supportive rim into cancellous bone can increase the risk of loosening. An over-lateralized cup is also at the risk of loosening due to inadequate superolateral bony support.23,24 In contrast, a cemented component will require greater medialization to containment.
Despite traditionally espoused benefits, medialization has deleterious effects too. Attention to acetabular offset and restoration of an anatomic COR has advantages in terms of impingement, ROM, global offset restoration, cortical rim press-fit, and maintaining medial bone stock. We would recommend an individualized approach to each patient, considering each of these factors, rather than routine medialization for all.
Height of cup
The superoinferior position of cup affects limb length and JRF.
A change in cup height can cause limb length discrepancy. Clinical consequences include gait disturbance, low back pain, neurological symptoms, and instability of hip.13 Although the usual problem is a high COR with shortening, lower placement of COR has been described as a cause of lengthening. Parvizi et al.14 have described revision THA for lengthening caused by the cup extending below the level of teardrop.
Araised COR causes higher JRF, increasing risk of premature wear, aseptic loosening, and implant failure.15,16,17 Raising the COR reduces perpendicular distance to abductors and Asayama et al.6 showed that it negatively correlates with abductor strength. They recommended a slight inferomedial position of COR with a slight increase in femoral offset to optimize abductor function. In dysplastic hips with a superiorly displaced COR, the best outcomes are associated with reconstruction of the anatomic COR. This results in a reduction in JRF and abductor muscle force.15,16,19
During THA, the acetabular reaming vector can cause minor displacements of COR superiorly and posteriorly. It is believed that superior displacements of up to 13 mm (and medial of 7.5 mm)24 have no clinical consequence. However, more recent work suggests that when COR is raised >3 mm (and medialized >5 mm) restoration of offset within 5 mm becomes difficult.26,27
Angular position of cup
Angular position includes anteversion and inclination (abduction angle) of cup.
A variety of values has been recommended to help reduce wear, bearing-related noise, impingement, and risk of dislocation. Inclination past 45° has been shown to increase wear rate,28,29 metal-on-metal bearings with inclinations past 55° have shown raised blood levels of metal ions,30 CoC bearings outside a zone of 35°–45° inclination, and 15°–35° anteversion are 29 times more likely to squeak.11 However, the vast majority of studies relate to dislocation, with a wide range of recommended values. The most commonly quoted study is by Lewinnek et al.2 He found an increased dislocation rate in cups placed outside anteversion angles of 5°–25° and 30°–50° of inclination. To a certain extent, the variation in recommended angles can be attributed to different ways of measuring these angles. An understanding of this is vital in achieving optimum cup placement.
Quantifying angular position
Angular position is the angle subtended by acetabular axis, which passes through the center of socket and is perpendicular to plane of the socket face (Calandruccio, 1987). In practical terms, this is represented by the inserter handle of an uncemented socket. The angle of this axis can be measured in three different ways, depending on the plane or the axis from which it is measured. Inclination and anteversion can thus be operative, radiologic, or anatomic [Table 1].31
Table 1.
Definitions of operative, radiographic and anatomic inclination
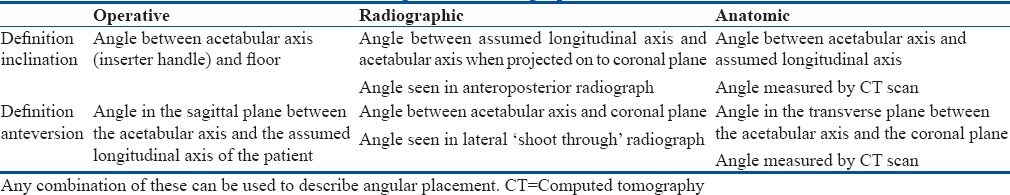
Operative and radiographic angles are the most relevant surgically in lateral position of the patient. Due to anteversion, the radiographic inclination is higher than operative inclination and increases with increasing anteversion. To achieve a target radiographic anteversion, the operative angle should be higher.
During surgery in lateral position, operative inclination is assessed by looking from a point perpendicular to the plane of anteversion of the cup inserter. Radiographic inclination can be assessed by standing directly behind the patient and looking (from a point perpendicular to the coronal plane) at the insertion angle with floor [Figure 2]. The radiographic projection will be greater than this due to anteversion. The operative anteversion is assessed by looking down, to project the insertion angle onto sagittal plane, and measuring against the longitudinal axis. This angle will be greater than the projected radiographic angle [Figure 2].
Figure 2.
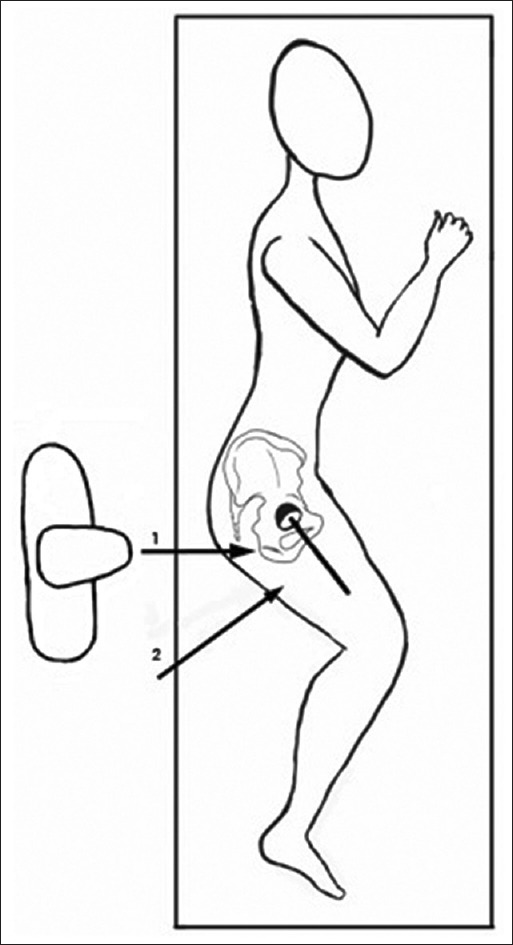
Schematic diagram showing surgeon position to assess radiographic and operative inclination. Position 1 assesses the projection of the operative inclination on the coronal plane, and therefore, the radiographic angle. Position 2 perpendicular to the vertical plane passing through inserter handle assesses operative inclination
An illustration of these differences is the interpretation of Lewinnek's safe zone by Murray.31 Lewinnek et al.2 reported 25° as the upper limit of anteversion beyond which 15% hips dislocated. This is a radiographic angle and, on conversion, equivalent to 38° operative anteversion, above which 21% hips dislocated. Therefore, Murray recommends that Lewinnek's statement should have been interpreted as - hips should be inserted at < 35° of operative anteversion to avoid dislocations.
Pelvic tilt and functional acetabular positions
The angle between the coronal plane of the patient and the anterior pelvic plane (APP) (plane passing through both anterior superior iliac spines [ASIS] and pubic tubercles) is called pelvic tilt [Figure 3].32 It can be judged on radiographs by looking at symphysis pubis to sacrococcygeal distance with normal values of 32 mm (range 8–50 mm) in women and 47 mm (range 15-72 mm) in men.33 The distance increases with forward tilt and decreases when tilted backward. The average pelvis has a posterior tilt, −12° and −8° in standing and supine, respectively,34 that tilts further back when sitting [Figure 3].
Figure 3.
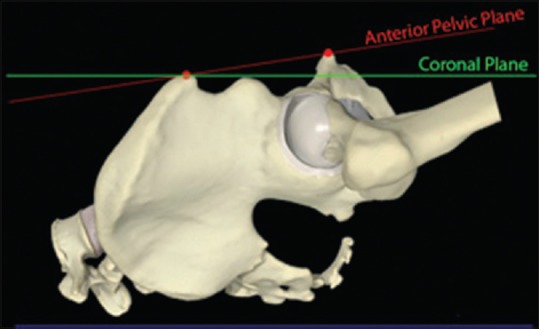
Schematic representation on saw bones demonstrating pelvic tilt - the difference between the anterior pelvic plane and the coronal plane
Dynamic changes to pelvic tilt affects radiographic anteversion,35 with 0.7°–0.8° increase for each degree of posterior tilt.36,37 There is a mean increase in anteversion of 7° (range −2° to 18°) in standing compared to supine, with 52% of patients having more than 5° increase.36 There is a larger change moving from standing to sitting with an average increase of 15.6°.38
Forward or anteriorpelvic tilt causes a decrease in inclination and vice versa.37 Although the mean change is not significant (mean 2°),39 as the change in inclination happens in a nonlinear manner, patients with larger posterior tilts have a larger change in inclination (mean change 0.29° per degree of posterior pelvic tilt as opposed to 0.47° per degree when patient has 15° posterior tilt).40
Safe zone considering differing angular measurements and reference frames
There is controversy whether a generic safe zone exists for cup position as some researchers have found that a significant proportion of cups that dislocate lie within defined safe zones.41,42,43,44,45 As previously discussed, there is large variation in recommended values46,47,48,49,50,51,52,53 partly due to the use of different reference frames and angular definitions.
Yoon et al.32 have attempted to resolve these inconsistencies by amalgamating data from nine different papers recommending safe zones and computed angles to a unified system by transferring to a pelvic reference plane (based on a pelvic tilt of −8° standing and −4° lying34). Using their common reference, the averaged target orientation is 41° inclination and 16° anteversion for radiographic angles. This equates to operative angles of 39° inclination and 21° anteversion. Based on the evidence so far, this seems to be a good generalization that can be offered to minimize the incidence of dislocation.
Section II - Planning and Execution in Cup Positioning
Callanan et al.54 studied the accuracy of cup positioning and concluded that only 50% of hips were within the targeted safe zone for both anteversion and inclination (63% for inclination and 79% for version). Surgeon volume and high body mass index (BMI) were independent risk factors, with obesity, low volume surgeons, and minimally invasive surgery conferring a 1.3-fold, 2-fold, and 6-fold higher risk of malposition, respectively. Techniques that can be used to improve the accuracy of positioning are discussed below.
Templating
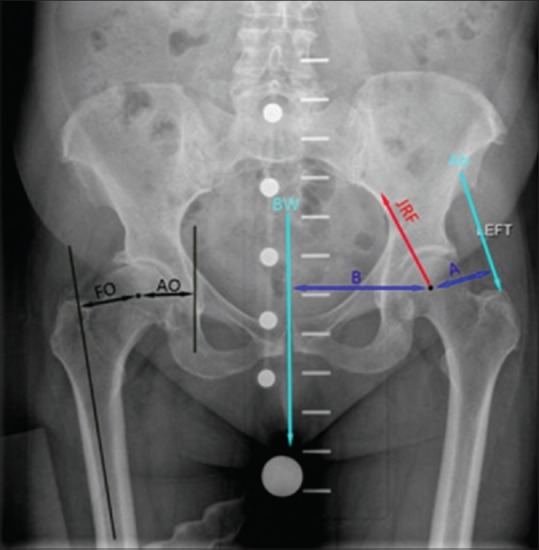
Templating is an essential step in the THA surgical process. Two-dimensional templating is the most common method, and while, this does have limitations, it provides enough information to carry out uncomplicated primary THAs [Figure 4].
Figure 4.
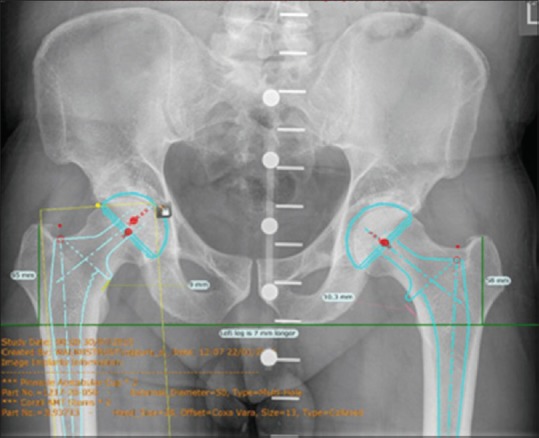
X-ray pelvis with hip joints and proximal 1/3rd of femur anteroposterior view showing templating for an uncemented total hip arthroplasty
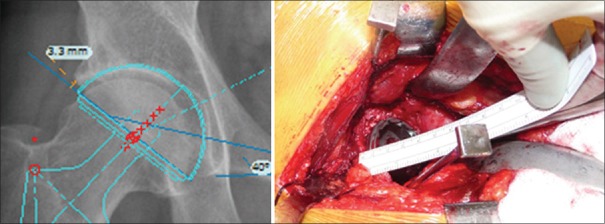
Predicting implant size from templating is imprecise, with correct size prediction ranging from 16%–62%,55,56 improving to 52%–98% if a range of sizes one above and below is accepted. Some of this inaccuracy has been attributed to differences in magnification, poor placement of calibrating ball, and distortion due to projection.57 Work from our institution58 suggest that a major factor is incorrect placement of cup template on radiographs and that an understanding of relationship between teardrop and the most inferior extent of posterior acetabular rim (IPAR) may help to improve sizing.
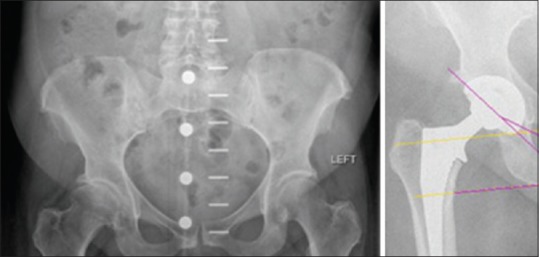
The “teardrop” is a radiographic landmark created by superimposition of the most distal part of the medial wall of the acetabulum and the tips of the anterior and posterior horns. A line drawn between both teardrops can be used as a reference from which to measure inclination and leg length. However, rather than teardrop, it is the posterior and inferior part of the semilunar weight bearing bone of the acetabulum that is the most inferior and we call this IPAR [Figure 5]. The IPAR and teardrop were at different levels in 86% cases, and the inferior extent of most cups tends to sit between the radiographic projection of IPAR and teardrop on postoperative X-rays. Placing template at the level of teardrop would tend to undersize and placing at IPAR would oversize the component [Figure 5].
Figure 5.
X-ray pelvis with both hip joints and proximal 1/3rd of femur anteroposterior view showing the difference in position between teardrop and inferior extent of posterior acetabular rim. To size the acetabulum accurately in templating as well as to understand cup positioning, it's important to recognize the distance between the two
However, the aim of templating is not to predict implant sizes (other than in extreme situations), as this can be done easily during surgery, but to predict cup position in terms of restoring COR and height, depth, and angular position [Figure 4].
Computerized navigation – passing fad or lasting benefits?
Navigation can lead to more reliable cup placement within safe zones.59 An evidence-based analysis60 showed that though there was no significant difference in mean angles between navigated and nonnavigated cups (though with less variation in the navigated group), a significantly higher number were placed within safe zone (80.75% vs. 62.34%) and had lower dislocation rate (1.03% vs. 2.49%) using navigation. A meta-analysis of cup position in navigated versus nonnavigated groups61 showed that a significantly lower number of cups were outliers with regard to the safe position in the navigated group (10.7% vs. 41.8%).
There is active, semi-active, and passive navigation. Active navigation uses robots to implant cups. Semi-active systems allow the surgeons to move the robotic arms but do not allow the arm to move beyond a milling boundary that has been determined by preoperative three-dimensional imaging. The data from robotic THA is only starting to come through and is not presented here. Passive navigation only guides the surgeon to implant in the right position and consists of three types of navigation - imageless navigation, computed tomography-based navigation, and fluoroscopic navigation.
Most passive navigation systems use APP as the reference plane. Although this aids accurate placement of cup in relation to the pelvis, it does not consider pelvic tilt. Babisch et al.62 produced a nomogram for pelvic tilt and used it to adjust for pelvic tilt during navigation resulting in 98% accuracy of cup placement. Although current navigation systems consider mean pelvic tilt, the future lies in adjusting cup position according to functional pelvic position of each individual.
Despite these advantages, navigation is not commonly used due to cost and operative time implications.
Patient positioning and its significance
Supine positioning, with the use of anterior, anterolateral, or direct lateral approaches, has the advantage that it is easier to assess whether the pelvis is square and to assess limb lengths. In addition, surgery takes place in the coronal plane which is the functional plane.
However, the vast majority of THA uses lateral decubitus position using posterior, anterolateral, anterior, or the newer direct superior approach. Here, pelvic position tends to have wide variation at setup. Pelvic tilt can range from 25° posterior to 20° anterior (55% hips having posterior tilt, 38% anterior) with 16.1% patients having a tilt of 10° or greater.39 Therefore, while we tend to think that the pelvis is aligned with the coronal plane of the patient when positioned on operating table, the truth is that we do not know its real orientation.
While maximum variation is for pelvic tilt, 8° (2 standard deviation [SD] ± 32°), it is also adducted, −4° (2SD ± 12°), and externally rotated, −8° (2SD ± 14°).63 It is recommended that while positioning, both ASIS and pubic tubercles are considered, and position of posterior support in craniocaudal direction is used to control pelvic tilt.64 To control pelvic obliquity, a helpful method described by Beverland et al.65 is to draw parallel lines at lumbosacral region using a spirit level with the patient seated preoperatively. In the lateral position, these lines then demonstrate the degree of pelvic adduction before application of posterior support. This may not be as helpful in high BMI patients.
How to Achieve Target Depth
Individualized depth of cup placement is based on achieving optimum cup fixation as the priority, with the main variable being adequate cup coverage. Where there is an adequate acetabulum an anatomic position, with its associated advantages, can be chosen [Figure 6]. Care should be exercised in choosing a medialized position in a person with large native offset, as medialization can result in medial movement of COR up to 14 mm27 making it difficult to find a stem that would restore global offset. Similarly, in a person with a deep acetabulum further medialization can lead to impingement and loss of ROM. On the other hand, in an acetabulum that is shallow or tending toward dysplasia, the anatomical position would lead to lateral uncoverage, and therefore, a medialized position should be chosen [Figures 6 and 7].
Figure 6.

X-ray pelvis with both hip joints and proximal half of femur, anteroposterior view in this patient, an anatomical position has been chosen for the cup. Reducing the acetabular offset would mean that a femoral stem with greater offset would have been required. Risk of impingement and reduced range of movement could result from medialization
Figure 7.
Preoperative and postoperative radiographs of pelvis with both hips and proximal femur anteroposterior view in a patient with shallow acetabulum where the medialized position has been chosen. Choosing the anatomic position in this patient would have resulted in lateral uncoverage of the cup
Ifan anatomic position is chosen, the transverse acetabular ligament (TAL) and labrum can be used to define the cup not only in version but also its depth of placement.64,66 Beverland et al.65 has described his technique of reaming the acetabulum conservatively to no more than 4 mm bigger than femoral head size until the final reamer is cradled by labrum and TAL. The depth, version, and height (not inclination) of a hemispherical cup is guided by this.
If medialization is chosen, reamer/osteotomes are used to expose the true floor. Care must be taken to restore global offset, as conventional reaming displaces COR medially by a mean of 5 mm and elevates it by 3.7 mm, compared to the anatomic position which displaces it by a mean of < 1 mm in each direction.27 In planning, stem offset should be measured from intended final position of hip COR (based on final cup position) rather than COR of femoral head. The profile of the lesser trochanter (LT) should also be noted, as an externally rotated hip, as evidenced by a prominent LT can cause a 20% reduction in measurement of femoral offset19 on templating.
To check global offset intraoperatively, there are several techniques described. Jigs are available to measure from a fixed point above acetabulum before hip dislocation, measuring length, and offset. The senior author has described his technique of using a suture from a Judd pin inserted into the illium just superior to acetabulum to measure intraoperative leg length [Figure 8].67,68 The angle of this suture, with respect to the floor, can also be used to determine the restoration of global offset. For this technique, it is necessary to accurately place the limb in same position each time, as any change in angular position of the limb can affect measurement significantly. Another technique is direct measurement of the distance from COR of the femoral head to greater trochanter before neck resection and restoring it along with the length of any medialization. The use of a caliper to measure diameter of the resected head and using this measurement to estimate the distance to the prosthetic head from fixed points on greater trochanter and resected neck to accurately reproduce femoral offset and height when an anatomic COR is chosen has been described [Figure 8].69
Figure 8.
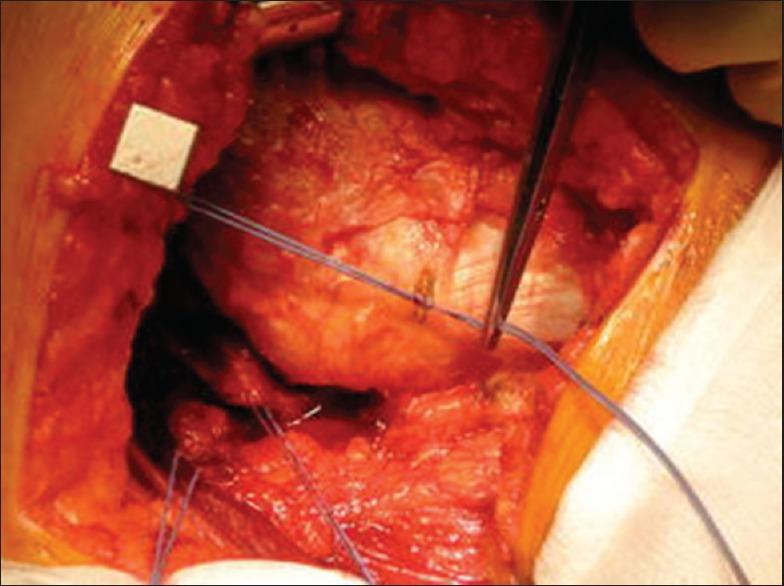
Peroperative photograph showing a Judd pin is inserted at the supraacetabular level, and the suture with a knot is used to mark the distance to a fixed point on the greater trochanter before dislocation. This suture can be used to assess leg length and offset intraoperatively
How to Achieve Target Height
The TAL can also be used to determine height.64 Ideally, the reamer should be cradled by TAL and labrum66 which ensures that the cup will not migrate proximally. The effect of medialization must be considered as it can elevate COR by up to 18.9 mm.24 The inferior extent of the cotyloid fossa is projected as teardrop on radiographs, and at the correct inclination, the inferior extent of the cup should not be above this. However, in dysplasia, sometimes medialization and elevation of COR ID required to achieve good lateral coverage.
How to Achieve Target Angular Position
Due to the disparity between operative and radiographic angles, Grammatopoulos et al.63 recommended implanting the cup in 5° less inclination and 8° more anteversion to achieve the target radiographic position. The most common technique used to guide angular position remains the use a jig during cup insertion. In smaller incisions and high BMI patients, care must be taken to ensure that inclination is not changed by abutment of the cup inserter against soft tissues (angled/offset inserter is useful in such situations). However, orthopedic surgeons are not very good at visually estimating angles subtended by Jigs.66 A digital protractor placed on the inserter handle can help improve the accuracy of insertion angles.70
Achieving the correct angle between inserter handle and the floor or the operating table does not ensure satisfactory cup inclination. Hill et al.71 reported a 12.7° variation between implanted inclination angle and final position on radiographs despite careful implantation. They indicated that although this is in large part related to the difference between operative and radiographic inclination, it is also partly due to adduction of the pelvis on operating table. They, therefore, recommend an operative inclination target of 35° to prevent outliers at above what is seen as a critical inclination of 50° of radiographic inclination.
We have discussed variability of pelvic position at setup. There is also significant intraoperative movement of the pelvis during surgery. Factors influencing movement include surgeon, pelvic supports (two ASIS supports better), approach (posterior more movement than anterolateral), and procedure type (resurfacing more than THA).62 Such pelvic movement during surgery can affect cup position. A solution is to use internal landmarks that are independent of patient position. The relationship between the superolateral most point of the bony acetabulum and the lateral extent of the templated acetabular cup can be used for this purpose. The distance between these points can be measured during templating and can then be recreated intraoperatively to guide inclination [Figure 9].
Figure 9.
X-ray (L) hip joint anteroposterior view and peroperative photograph showing measuring the lateral overhang of template and reproducing it intraoperatively to achieve correct cup inclination
The use of TAL to guide anteversion has been reported to reduce dislocation rates to 0.6%.64 Another intrapelvic guide to cup version is the acetabular notch or psoas groove. Especially in anatomical position of cup, care should be exercised that there should be adequate anteversion so that the anterior margin of cup is deep to the notch to prevent psoas irritation.
Where it is suspected that the femoral version is abnormal, the version of the implanted stem should be considered, before the definitive cup is implanted. In these cases, the use of combined anteversion angle is recommended.24,25 It is beyond the scope of this article to discuss this technique in detail, however, it is recommended that the surgeon is familiar with this concept where abnormal femoral anatomy is encountered.
Spinopelvic Interaction
It has long been recognized that severe hip arthritis and its treatment with arthroplasty can change the alignment of the spine. Recently, there has been more focus on the relationship between functional cup position and spinopelvic kinematics. Due to changes in lumbar lordosis and resultant pelvic tilt, a cup positioned within conventionally defined safe zones may become unstable with activities such as sitting and standing.
In people with normal spine/pelvis mobility, there is a posterior tilt of 20°–35°, moving from standing to sitting, with a mean of 4° less in stiffer spines, and 13° less than those with hypermobile spines.72
This has implications in patients undergoing THA with stiffer spines or spinal fusions. Such patients are not able to tilt when sitting and therefore tend toward anterior impingement in sitting, increasing the risk of posterior instability while patients with unbalanced spines tend to extend their spine and hip to retain balance and tend to get posterior impingement in standing.
Phan et al.73 divide these patients into four groups and have suggested cup anteversion options: for flexible balanced spines, the cup is placed within a standard safe zone; a rigid balanced spine (anterior impingement in sitting) should be compensated by placing the cup in greater anteversion; a flexible unbalanced spine (posterior impingement) should have spinal surgery first or a cup in less anteversion; finally, the rigid unbalanced spine should have spinal surgery first or a cup placed in a standard safe zone.
Conclusion
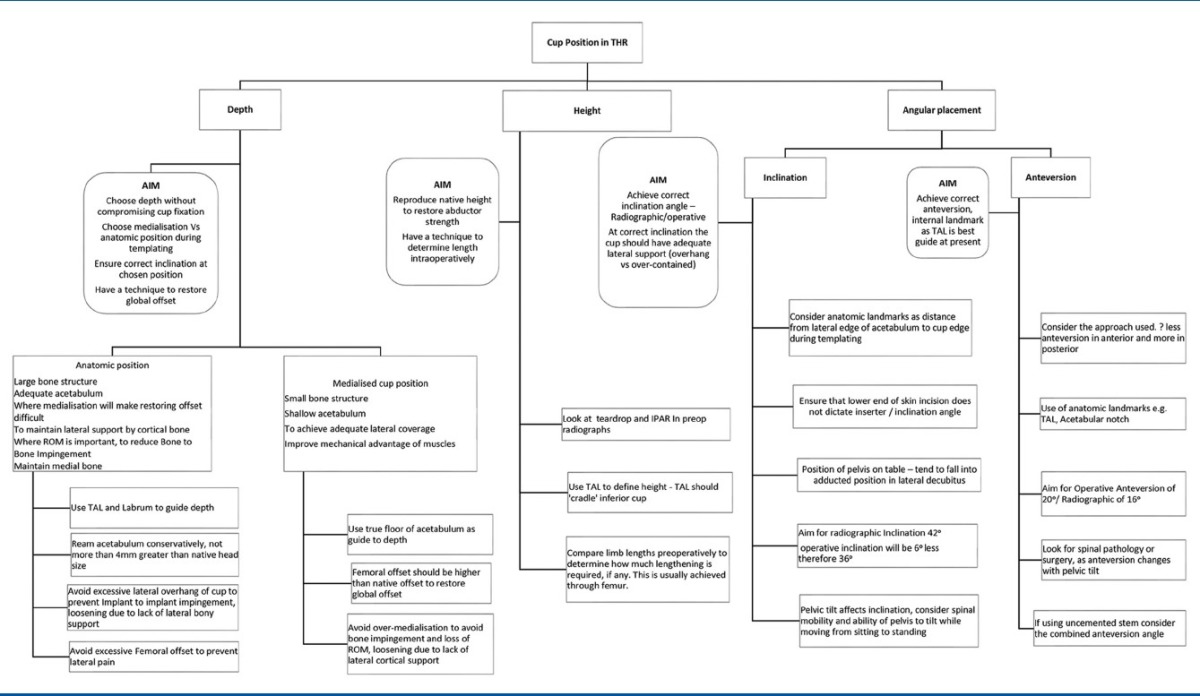
We have discussed the range of factors that play a role in achieving planned cup position. The anatomy of the pelvis, stiffness of spinopelvic junction, functional positions of pelvis, its position at setup and movement during surgery, reference frames used, the way angles are measured and surgical technique, all have an impact on cup position [Table 2]. An improved understanding of these factors may necessitate a move away from the traditional technique of trying to place cup within the same defined safe zone for every patient. The future may lie in individualized target positions, taking into account functional pelvic movement, to reduce dislocation risk, and improve outcomes.
Table 2.
A pragmatic approach to cup positioning
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: A health economic analysis. Bone Joint J. 2013;95-B:115–21. doi: 10.1302/0301-620X.95B1.29835. [DOI] [PubMed] [Google Scholar]
- 2.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 3.Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467:2895–900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–34. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Schmalzried TP, Shepherd EF, Dorey FJ, Jackson WO, dela Rosa M, Fa’vae F, et al. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20:414–20. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz WB, Ecker TM, Reichmann WM, Murphy SB. Factors affecting bony impingement in hip arthroplasty. J Arthroplasty. 2010;25:624–34.e1-2. doi: 10.1016/j.arth.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 8.Bonnin MP, Archbold PH, Basiglini L, Fessy MH, Beverland DE. Do we medialise the hip centre of rotation in total hip arthroplasty? Influence of acetabular offset and surgical technique. Hip Int. 2012;22:371–8. doi: 10.5301/HIP.2012.9350. [DOI] [PubMed] [Google Scholar]
- 9.Bonnin MP, Archbold PH, Basiglini L, Selmi TA, Beverland DE. Should the acetabular cup be medialised in total hip arthroplasty. Hip Int. 2011;21:428–35. doi: 10.5301/HIP.2011.8582. [DOI] [PubMed] [Google Scholar]
- 10.Sexton SA, Yeung E, Jackson MP, Rajaratnam S, Martell JM, Walter WL, et al. The role of patient factors and implant position in squeaking of ceramic-on-ceramic total hip replacements. J Bone Joint Surg Br. 2011;93:439–42. doi: 10.1302/0301-620X.93B4.25707. [DOI] [PubMed] [Google Scholar]
- 11.Walter WL, O’toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: The importance of acetabular component orientation. J Arthroplasty. 2007;22:496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 12.Cassidy KA, Noticewala MS, Macaulay W, Lee JH, Geller JA. Effect of femoral offset on pain and function after total hip arthroplasty. J Arthroplasty. 2012;27:1863–9. doi: 10.1016/j.arth.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Frueh WW, Hozack WJ. Management of limb length discrepancy after total hip arthroplasty. Semin Arthroplasty. 2005;16:127–31. [Google Scholar]
- 14.Parvizi J, Sharkey PF, Bissett GA, Rothman RH, Hozack WJ. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am. 2003;85-A:2310–7. doi: 10.2106/00004623-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Abolghasemian M, Samiezadeh S, Jafari D, Bougherara H, Gross AE, Ghazavi MT. Displacement of the hip center of rotation after arthroplasty of Crowe III and IV dysplasia: A radiological and biomechanical study. J Arthroplasty. 2013;28:1031–5. doi: 10.1016/j.arth.2012.07.042. [DOI] [PubMed] [Google Scholar]
- 16.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33:397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Traina F, De Fine M, Biondi F, Tassinari E, Galvani A, Toni A. The influence of the centre of rotation on implant survival using a modular stem hip prosthesis. Int Orthop. 2009;33:1513–8. doi: 10.1007/s00264-008-0710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robinson M, Bornstein L, Mennear B, Bostrom M, Nestor B, Padgett D, et al. Effect of restoration of combined offset on stability of large head THA. Hip Int. 2012;22:248–53. doi: 10.5301/HIP.2012.9283. [DOI] [PubMed] [Google Scholar]
- 19.Sariali E, Klouche S, Mouttet A, Pascal-Moussellard H. The effect of femoral offset modification on gait after total hip arthroplasty. Acta Orthop. 2014;85:123–7. doi: 10.3109/17453674.2014.889980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Charnley J. Low Friction Arthroplasty of the Hip – Theory and Practice. Berlin, Heidelberg: Springer-Verlag; 1979. [Google Scholar]
- 21.Nevelos J, Ingham E, Doyle C, Streicher R, Nevelos A, Walter W, et al. Microseparation of the centers of alumina-alumina artificial hip joints during simulator testing produces clinically relevant wear rates and patterns. J Arthroplasty. 2000;15:793–5. doi: 10.1054/arth.2000.8100. [DOI] [PubMed] [Google Scholar]
- 22.Wroblewski BM, Siney PD, Fleming PA. Microseparation, fluid pressure and flow in failures of metal-on-metal hip resurfacing arthroplasties. Bone Joint Res. 2012;1:25–30. doi: 10.1302/2046-3758.13.2000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Widmer KH. Containment versus impingement: Finding a compromise for cup placement in total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S29–33. doi: 10.1007/s00264-007-0429-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–42. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 25.Ranawat CS, Maynard MJ. Modern techniques of cemented total hip arthroplasty. Tech Orthop. 1991;6:17–25. [Google Scholar]
- 26.Dastane M, Dorr LD, Tarwala R, Wan Z. Hip offset in total hip arthroplasty: Quantitative measurement with navigation. Clin Orthop Relat Res. 2011;469:429–36. doi: 10.1007/s11999-010-1554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meermans G, Doorn JV, Kats JJ. Restoration of the centre of rotation in primary total hip arthroplasty: The influence of acetabular floor depth and reaming technique. Bone Joint J. 2016;98-B:1597–603. doi: 10.1302/0301-620X.98B12.BJJ-2016-0345.R1. [DOI] [PubMed] [Google Scholar]
- 28.Hirakawa K, Mitsugi N, Koshino T, Saito T, Hirasawa Y, Kubo T. Effect of acetabular cup position and orientation in cemented total hip arthroplasty. Clin Orthop Relat Res. 2001;388:135–42. doi: 10.1097/00003086-200107000-00020. [DOI] [PubMed] [Google Scholar]
- 29.Patil S, Bergula A, Chen PC, Colwell CW, Jr, D’Lima DD. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A(Suppl 4):56–63. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 30.De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291–7. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]
- 31.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–32. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 32.Yoon YS, Hodgson AJ, Tonetti J, Masri BA, Duncan CP. Resolving inconsistencies in defining the target orientation for the acetabular cup angles in total hip arthroplasty. Clin Biomech (Bristol, Avon) 2008;23:253–9. doi: 10.1016/j.clinbiomech.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 33.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–8. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 34.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–23. doi: 10.1080/17453670510041501. [DOI] [PubMed] [Google Scholar]
- 35.Tannast M, Fritsch S, Zheng G, Siebenrock KA, Steppacher SD. Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res. 2015;473:1255–66. doi: 10.1007/s11999-014-3936-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polkowski GG, Nunley RM, Ruh EL, Williams BM, Barrack RL. Does standing affect acetabular component inclination and version after THA? Clin Orthop Relat Res. 2012;470:2988–94. doi: 10.1007/s11999-012-2391-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mellano CR, Spitzer AI. How does pelvic rotation or tilt affect radiographic measurement of acetabular component inclination angle during THA? J Orthop. 2015;12:222–7. doi: 10.1016/j.jor.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lazennec JY, Boyer P, Gorin M, Catonné Y, Rousseau MA. Acetabular anteversion with CT in supine, simulated standing, and sitting positions in a THA patient population. Clin Orthop Relat Res. 2011;469:1103–9. doi: 10.1007/s11999-010-1732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu J, Wan Z, Dorr LD. Quantification of pelvic tilt in total hip arthroplasty. Clin Orthop Relat Res. 2010;468:571–5. doi: 10.1007/s11999-009-1064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maratt JD, Esposito CI, McLawhorn AS, Jerabek SA, Padgett DE, Mayman DJ. Pelvic tilt in patients undergoing total hip arthroplasty: When does it matter? J Arthroplasty. 2015;30:387–91. doi: 10.1016/j.arth.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res. 2016;474:386–91. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esposito CI, Gladnick BP, Lee YY, Lyman S, Wright TM, Mayman DJ, et al. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015;30:109–13. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grammatopoulos G, Thomas GE, Pandit H, Beard DJ, Gill HS, Murray DW. The effect of orientation of the acetabular component on outcome following total hip arthroplasty with small diameter hard-on-soft bearings. Bone Joint J. 2015;97-B:164–72. doi: 10.1302/0301-620X.97B2.34294. [DOI] [PubMed] [Google Scholar]
- 44.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–10. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 45.Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–8. [PubMed] [Google Scholar]
- 46.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after total hip arthroplasty: The effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–9. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 47.Dorr LD, Wan Z. Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res. 1998;355:144–51. doi: 10.1097/00003086-199810000-00015. [DOI] [PubMed] [Google Scholar]
- 48.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. J Arthroplasty. 2002;17:282–8. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 49.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, et al. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30:26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–70. [PubMed] [Google Scholar]
- 51.Seki M, Yuasa N, Ohkuni K. Analysis of optimal range of socket orientations in total hip arthroplasty with use of computer-aided design simulation. J Orthop Res. 1998;16:513–7. doi: 10.1002/jor.1100160418. [DOI] [PubMed] [Google Scholar]
- 52.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–21. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 53.Yoshimine F. The influence of the oscillation angle and the neck anteversion of the prosthesis on the cup safe-zone that fulfills the criteria for range of motion in total hip replacements. The required oscillation angle for an acceptable cup safe-zone. J Biomech. 2005;38:125–32. doi: 10.1016/j.jbiomech.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 54.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: Risk factors for cup malpositioning: Quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–29. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.González Della Valle A, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop. 2008;32:289–94. doi: 10.1007/s00264-006-0317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Knight JL, Atwater RD. Preoperative planning for total hip arthroplasty. Quantitating its utility and precision. J Arthroplasty. 1992;7:403–9. doi: 10.1016/s0883-5403(07)80031-3. [DOI] [PubMed] [Google Scholar]
- 57.Scheerlinck T. Primary hip arthroplasty templating on standard radiographs. A stepwise approach. Acta Orthop Belg. 2010;76:432–42. [PubMed] [Google Scholar]
- 58.Edakalathur J, Bhaskar D, Thomas S, Board TN, Rajpura A. IPAR (Inferior edge of the posterior acetabular rim) and Its Relevance in Positioning of the Cup. Oral Presentation At: European Hip Society, Munich; 07 September. 2016 [Google Scholar]
- 59.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–9. doi: 10.1097/BLO.0b013e3181560c51. [DOI] [PubMed] [Google Scholar]
- 60.Moskal JT, Capps SG. Acetabular component positioning in total hip arthroplasty: An evidence-based analysis. J Arthroplasty. 2011;26:1432–7. doi: 10.1016/j.arth.2010.11.011. [DOI] [PubMed] [Google Scholar]
- 61.Gandhi R, Marchie A, Farrokhyar F, Mahomed N. Computer navigation in total hip replacement: A meta-analysis. Int Orthop. 2009;33:593–7. doi: 10.1007/s00264-008-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–65. doi: 10.2106/JBJS.F.00628. [DOI] [PubMed] [Google Scholar]
- 63.Grammatopoulos G, Pandit HG, da Assunção R, Taylor A, McLardy-Smith P, De Smet KA, et al. Pelvic position and movement during hip replacement. Bone Joint J. 2014;96-B:876–83. doi: 10.1302/0301-620X.96B7.32107. [DOI] [PubMed] [Google Scholar]
- 64.Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: An aid to orientation of the acetabular component during primary total hip replacement: A preliminary study of 1000 cases investigating postoperative stability. J Bone Joint Surg Br. 2006;88:883–6. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 65.Beverland DE, O’Neill CK, Rutherford M, Molloy D, Hill JC. Placement of the acetabular component. Bone Joint J. 2016;98-B(1 Suppl A):37–43. doi: 10.1302/0301-620X.98B1.36343. [DOI] [PubMed] [Google Scholar]
- 66.Beverland D. The transverse acetabular ligament: Optimizing version. Orthopedics. 2010;33:631. doi: 10.3928/01477447-20100722-22. [DOI] [PubMed] [Google Scholar]
- 67.Desai A, Barkatali B, Dramis A, Board TN. A simple intraoperative technique to avoid limb length discrepancy in total hip arthroplasty. Surgeon. 2010;8:119–21. doi: 10.1016/j.surge.2009.10.023. [DOI] [PubMed] [Google Scholar]
- 68.Desai AS, Dramis A, Board TN. Leg length discrepancy after total hip arthroplasty: A review of literature. Curr Rev Musculoskelet Med. 2013;6:336–41. doi: 10.1007/s12178-013-9180-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hill JC, Archbold HA, Diamond OJ, Orr JF, Jaramaz B, Beverland DE. Using a calliper to restore the centre of the femoral head during total hip replacement. J Bone Joint Surg Br. 2012;94:1468–74. doi: 10.1302/0301-620X.94B11.29144. [DOI] [PubMed] [Google Scholar]
- 70.Meermans G, Goetheer-Smits I, Lim RF, Van Doorn WJ, Kats J. The difference between the radiographic and the operative angle of inclination of the acetabular component in total hip arthroplasty: Use of a digital protractor and the circumference of the hip to improve orientation. Bone Joint J. 2015;97-B:603–10. doi: 10.1302/0301-620X.97B5.34781. [DOI] [PubMed] [Google Scholar]
- 71.Hill JC, Gibson DP, Pagoti R, Beverland DE. Photographic measurement of the inclination of the acetabular component in total hip replacement using the posterior approach. J Bone Joint Surg Br. 2010;92:1209–14. doi: 10.1302/0301-620X.92B9.24476. [DOI] [PubMed] [Google Scholar]
- 72.Kanawade V, Dorr LD, Wan Z. Predictability of acetabular component angular change with postural shift from standing to sitting position. J Bone Joint Surg Am. 2014;96:978–86. doi: 10.2106/JBJS.M.00765. [DOI] [PubMed] [Google Scholar]
- 73.Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J. 2015;97-B:1017–23. doi: 10.1302/0301-620X.97B8.35700. [DOI] [PubMed] [Google Scholar]