Abstract
Background:
Pedicle screw technique is commonly used treatment of adult spinal trauma, tumor, degeneration. The application of pedicle screws is very challenging in children because children have a fast growing spine and spinal pedicle morphology of children and adult has large difference. 3 D reconstruction individual navigation templates improve the success rate of pediatric pedicle screw system. This study is aimed to provide a precise method for lumbar spine pedicle screw placement in children using computer-aided design and rapid prototyping technology.
Materials and Methods:
Computed tomography (CT) scans of cadaver specimens of 4 children were obtained, and the raw data were reconstructed using three-dimensional reconstruction software. Pedicle screws were placed using the conventional method or by using individually designed navigation templates based on the principles of reverse engineering and rapid prototyping technology.
Results:
We evaluated the accuracy of the pedicle screws placed using the two methods by CT scan. Ten navigation templates were designed for placement of 20 lumbar pedicle screws in the navigation group, and CT scan confirmed that all the screws were placed accurately in the corresponding pedicle. Conversely, of the 20 lumbar pedicle screws placed using the conventional method, 3 screws perforated the pedicle. The findings showed that lumbar pedicle screw placement was successful using navigation templates in children.
Conclusions:
This technique is simple, easy to master, and allows personalized screw placement, thus providing a new and feasible method for lumbar pedicle screw placement in children.
Keywords: Children, navigation template, lumbar spine, cadaver
MeSH terms: Bone screw, spine, cadaver, pediatric surgery, computer assisted
Introduction
Roy-Camille et al. (1970) first reported the use of pedicle screws for the treatment of spinal fractures.1 Excellent three-dimensional (3D) fixation was possible with these screws,2,3 Rapid development of the pedicle screw fixation technique has led to its widespread use in the treatment of spinal trauma, degeneration and tumors. In comparison to adults, lumbar spine injuries in children are relatively rare, and are being mainly treated with nonsurgical alternatives.3 Moreover, the lumbar spine in children is in the growth stage and differs from that in adults in terms of anatomy and biomechanics with respect to the following: (1) There is more collagen tissue in the vertebral body as well as incomplete ossification, which could result in compression fractures of the vertebral body after force, fewer burst fractures, and heavy damage to the endplate; (2) from a structural or morphological perspective, the facet joints are not mature, the angle of the spinal facet joint is small and in a horizontal position, and the vertebral body is wedge shaped, which indicates significantly greater spinal activity than that in adults and the higher likelihood of lateral displacement after force; (3) the interspinous ligaments and the joint capsule are also more loose and the anterior and posterior longitudinal ligaments are flexible, which allows excessive flexion and extension of the spine. Furthermore, in children, development of the spinal cord occurs earlier than the vertebral body. On the other hand, the spinal canal is relatively narrow, the pedicle is small and there is a large variation in anatomical structure, rendering vicinal relations complex in children. For instance, displacement of a fracture is likely to cause a serious direct compression on the spine and the concomitant nerve damage is more serious than that in adults. In addition, a unique mechanism, namely longitudinal traction force, can also aggravate spinal cord injuries in children.
Murakami et al.4 (2008) confirmed the presence of abundant elastic cartilage in the vertebrae of children that contributes to increased spinal elasticity and flexibility. Once injured, however, the spine may exhibit 2 inches of drawing (lengthening) while drawing of the spinal cord is only 0.25 inches. When a longitudinal external force is applied on the spine causing excessive deformation, the spinal cord is pulled or compressed instantaneously; however, the spinal cord and membranes cannot adapt to such high tensile stress induced by the traction injury or laceration. In children, trauma can further aggravate the existing instability of the lumbar spine, which is then also prone to delayed neurological damage. These situations are likely to aggravate spinal cord injuries in children and the clinical manifestations of neurological damage in children are more serious than that in adults.
Although pedicle screw fixation has been reported previously in children under the age of 10 years, especially in young children, the treatment of spinal disorders is not common. Like in adults, pedicle screw fixation is associated with complications in children. Because the morphology of the spine pedicle in children can differ at different ages and in different segments from that in adults, research on the morphological development of spine pedicles in children as well as screw placement using digital 3D reconstruction technology is necessary.5,6 Furthermore, without good technical assurance, the risk of complications in children is higher than that in adults. In the present study, we described a method for lumbar pedicle screw placement in children using computer-aided design and rapid prototyping technology to provide precise positioning.
Materials and Methods
Preparation of specimens
Formalin was selected for perfusion of 2 male and 2 female cadavers aged between 6 and 13 years, the range of specimens was the complete spine. Axial computed tomography (CT) was performed to exclude cases of spinal fractures, tuberculosis, cancer and serious malformations or other diseases. All the experiments in the study were approved by Ethics Committee of our University.
Design and production of the personalized navigation template
The selected four cadavers were scanned using 64-slice spiral CT and the scanning sites were L1–L5. Scanning conditions were as follows: Thickness, 1.25 mm; pitch, 1.25 mm; reconstruction thickness, 0.625 mm; reconstruction pitch, 0.625 mm; Fov, 30 cm × 30 cm; matrix, 512 dpi × 512 dpi; tube voltage, 150 KV; current, 260 mA. CT data were saved in DICOM format and imported to the 3D reconstruction software (Mimics 15.0, Materialise NV, Belgium). A 3D model of the lumbar spine was then created to establish parameters for lumbar pedicle screw placement. For the conventional group, the diameter and length of the screws were defined based on the measurements obtained by CT before surgery; the diameter was 70–80% of the diameter of the pedicle and the length was 80% of the total length of the pedicle channel. For the navigation template group, the diameter and length of the screws for the surgery were selected according to those obtained using Mimics 15.0 software.
Personalized template navigation technology
The CT data of the two cadavers included in the navigation template group were imported to the Mimics 15.0 software in DICOM format for 3D reconstruction of the lumbar spine and then exported in STL format. The reconstructed 3D model was then opened in Geomagic Studio 9 software (Materialise-Technologielaan 15-3001 Leuven-Belgium) to establish a reverse template consistent with the anatomical shape of the lumbar spine in the rear of each lamina and the dorsal root of the spinous process, design simulated screws based on the reconstruction model and determine the direction, length, and diameter of the screws. We mixed the best channel into the nail of the template to form personalized navigation templates for each vertebrae, which had a bilateral positioning guide hole. The vertebral template was then bonded to the rear of the corresponding vertebrae on the 3D reconstruction model of the lumbar spine, and the model was rotated in all directions to observe the corresponding accuracy of the positioning guide hole and pedicle [Figure 1]. Using the SPS350B solid-state laser rapid prototyping machine, the accuracy of the model was 0.1 mm, and using optical assimilation (SLA) technology, an individual physical template (5 mm × 2 mm) was produced. The template was attached to the rear of corresponding lamina and spinous process [Figure 2], and its stability was maintained in the vertebra. Drilled into the anchor point with mouth gag of lumbar through the positioning guide hole, and the distance was consistent with the length of screw. A spherical probe was used to detect the walls, and the screw was placed slowly after smooth and continuous bone was identified [Figure 3].
Figure 1.
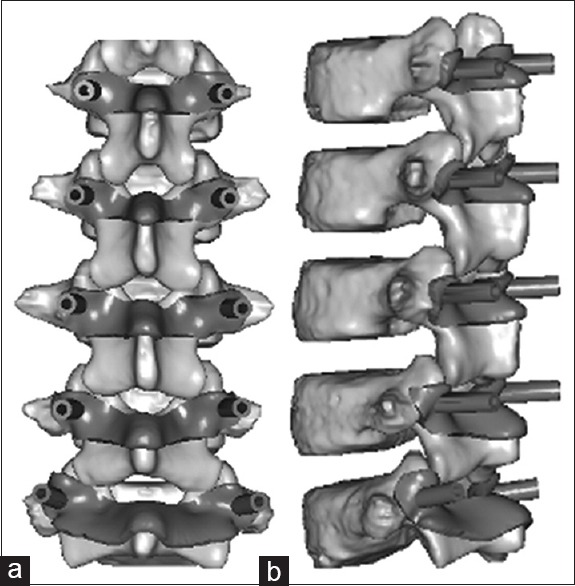
The front and side view of L1–L5 template with computer reconstruction (a: From behind the navigation template; b: Navigation template side view)
Figure 2.

Individual navigation templates bonded tightly to the anatomical structure of corresponding rear of vertebrae
Figure 3.

Individual navigation templates assisted screw placement of lumbar pedicle
Surgical evaluation methods
After surgery, the lumbar spine of the four cadavers was scanned by multislice CT (thickness, 0.625 mm), and the continuous CT data were saved in DICOM format and imported to the Mimics 15.0 software for 3D reconstruction. The position of the screws on the pedicle and vertebra was observed by an orthopedic surgeon in the coronal, horizontal, and sagittal views, respectively. Perforated of the cortex of the pedicle was assessed. The incidence rate of perforation was calculated accordingly, and the feasibility and accuracy of the two methods were evaluated [Figures 4 and 5].
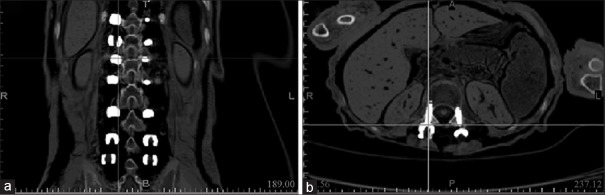
Figure 4.
CT scan coronal (a) and axial cuts (b) showing fixation of L1 screw after the surgery
Figure 5.
Coronal (a) and axial (b) CT scans showing fixation of L3 screw after the surgery
Results
Conventional method of pedicle screw placement
A total of 20 pedicle screws were placed in the conventional group (1 male, 1 female). After imaging acquisition, 2 pedicle screws (50%) were found to have pierced L1, 1 (25%) was found to have pierced L2, and the remaining 17 (85%) were found to be completely placed in the pedicle. With respect to the neck and thoracic pedicles, the lumbar pedicle was large and as such the success rate of screw placement was relatively high [Table 1].
Table 1.
The accuracy rate of screw placement by freehand in children lumbar
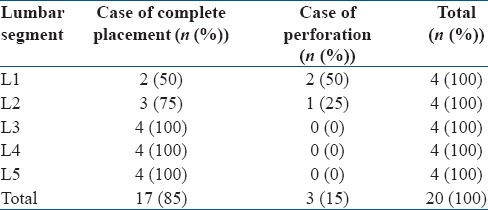
Navigation templates method for screw placement
Under the guidance of the navigation templates, a total of 20 pedicle screws were placed in two cadavers (1 male and 1 female). Following image acquisition, all the 20 pedicle screws were found to be completely placed in the pedicle with 100% accuracy [Table 2].
Table 2.
The accuracy rate of screw placement using children individual template navigation

Discussion
Previous reports indicate that children with spinal injuries account for approximately 1–10% of all patients with spinal injuries, of which 60–80% injury in the cervical and lumbar spine.7 In children, the spine is in growth phase, and in comparison to that in adults, it exhibits distinct characteristics with regard to anatomy, physiology, and biomechanics. In recent years, the pedicle screw fixation technique has developed rapidly exhibiting reasonable biomechanics, high stability, and three characteristic fixation sites. In previous studies,8 this technology has been used in 28 children (age range 1–6 years old) with congenital scoliosis, with satisfactory results.9,10 Successful pedicle screw fixation in the thoracic and lumbar spine11 has also been reported in 10 children aged 1–3 years and 19 children aged <10 years (mean, 6.5 years). Detailed preoperative planning, appropriate diameter selection of the pedicle screws, and flawless surgical technique will make this technique safe and feasible in children.
While clinical 3D reconstruction of the pedicle screw has been reported previously, a majority of these studies are mainly focused on adults. In comparison to adults, however, the morphology of the spinal pedicle is different in children, and can vary based on age and within different segments.12 The use of 3D reconstruction models for pedicle screw placement in children is therefore warranted. Moreover, performing the technique in children based on data in adults is risky, and therefore improving the accuracy and decreasing the error rate of screw placements in children is important.
Emergence of digital medicine has allowed development of digital navigation templates13,14 that are currently used for spinal fixation in adults and have shown improved accuracy. Previous studies comparing the conventional method and digital navigation template method for screw placement15 have confirmed that the rate of successful screw placement and the decrease in surgical time in the digital navigation template group were higher than those in the conventional group. In this study, 20 screws placed in the cadaveric specimens of two children using the navigation template achieved a 100% success rate that was significantly higher than the 85% success rate in the conventional group. The procedures in the two groups were performed by the same doctor. Since this technique is less dependent on the clinical experience of surgeon, the use of navigation templates designed to place screws accurately along the positioning guide hole is easy to master by beginners. The findings of this study demonstrate that this method is simple and requires no particular skills and experience, since it has shown significant accuracy and safety, and that it can be used for lumbar pedicle screw placement in children.
There are, however, limitations associated with this study that must also be taken into consideration. First, since the number of samples were small, the reliability of the data under certain conditions could be questioned. Second, reconstructed lumbar spine model was relatively rough. In this study, preliminary reconstruction was performed by beginners using software, and the 3D digital model reconstructed was rough, which had some influence on the design and production of the navigation templates. Precise design of the navigation template is a key step in successful screw placement and needs to be completed by orthopedic surgeons familiar with the software and with prior experience to ensure accuracy of the screw channel. Third, the material used in the template was relatively soft. Selection of the template material is important because if the material is too soft, angle offset may occur during surgery. In children, the neck and thoracic lumbar pedicle is smaller than that of the lumbar pedicle, and the optimal range of the screw placement angle is smaller, which can easily lead to missed screws; hence, appropriate navigation material is crucial. Fourth, navigation templates may poorly combine with the lamina and spinous process. Use of navigation templates requires soft tissue at the base of the lumbar spine lamina and stripping of the root of the spinous process while avoiding damage to the anatomical structure of the rear of lumbar spine to ensure that the template is tightly attached to the corresponding rear of the lamina and spinous process. Finally, angle offset may occur when the drill is rotated during surgery. When preparing to place screws using the navigation templates, a burr or drill is more appropriate, and shaking during drilling should be minimized to ensure that the passage is completely aligned with the direction of the positioning guide hole. Nevertheless, the use of computer software and the reduced cost of 3D printers can solve these problems.
The diameter, length, anchor point, and direction of the screw are crucial indicators of the success of pedicle screw fixation. The anatomical parameters of the pedicle vary, and there is significant diversity among different ages and segments. To improve the accuracy of pedicle screw placement, the concept of personalization has developed, namely screws are designed for each individual and the different segments, with different anchor points, directions, diameters, and lengths. Although the misplacement rate in clinical applications has consequently reduced, there are still some limitations. In recent years, the use of X-ray machines, with a “C”-shaped arm to guide the screw achieved a successful placement rate of 89.3%.16 The quality of the image, however, affected the accuracy of screw placement, and this technique increased the risk of radiation exposure to both doctors and patients. On the other hand, CT navigation achieved good therapeutic outcomes;17,18,19 however, imaging data are collected before the surgery, the technique is error prone and thus the placement rate could be affected, the time required for doctors to learn is long, it does not allow real-time monitoring, and the operative time is increased. Although, 3D navigation technology has good prospects and is likely to replace other navigation techniques gradually.20,21 System failure during surgery could lead to considerable damage. Since most studies focus on adults, with fewer reports on children, a method for pedicle screw fixation, which is simple, has a high accuracy rate, is easy to use in clinical settings, and feasible in children, is important.
Conclusion
Based on the actual morphology of different segments of the lumbar spine in children, navigation templates were designed using the principles of reverse engineering and rapid prototyping technology.
Financial support and sponsorship
This study was supported by National Natural Science Foundation of China (81260269) and Nature Science Foundation of Inner Mongolia Autonomous Region of China (2012MS1149) and the Youth Innovation Foundation of inner Mongolia Medical University (YKD2013QNCX018).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Roy-Camille R, Saillant G, Mazel C. Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–59. [PubMed] [Google Scholar]
- 2.Zdichavsky M, Blauth M, Knop C, Graessner M, Herrmann H, Krettek C, et al. Accuracy of pedicle screw placement in thoracic spine fractures. Eur J Trauma. 2004;30:234–40. [Google Scholar]
- 3.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: A comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–95. [PubMed] [Google Scholar]
- 4.Murakami S, Mizutani J, Fukuoka M, Kato K, Sekiya I, Okamoto H, et al. Relationship between screw trajectory of C1 lateral mass screw and internal carotid artery. Spine (Phila Pa 1976) 2008;33:2581–5. doi: 10.1097/BRS.0b013e318186b2fd. [DOI] [PubMed] [Google Scholar]
- 5.Karaikovic EE, Yingsakmongkol W, Gaines RW., Jr Accuracy of cervical pedicle screw placement using the funnel technique. Spine (Phila Pa 1976) 2001;26:2456–62. doi: 10.1097/00007632-200111150-00012. [DOI] [PubMed] [Google Scholar]
- 6.Li SG, Sheng L, Zhao H, Zhang JG, Zhai JJ, Zhu Y. Computer-assisted navigation technique in the spinal pedicle screw internal fixation. J Clin Rehabil Tissue Res. 2009;13:3365–9. [PubMed] [Google Scholar]
- 7.Platzer P, Jaindl M, Thalhammer G, Dittrich S, Kutscha-Lissberg F, Vecsei V, et al. Cervical spine injuries in pediatric patients. J Trauma. 2007;62:389–96. doi: 10.1097/01.ta.0000221802.83549.46. [DOI] [PubMed] [Google Scholar]
- 8.Fan Chiang CY, Tsai TT, Chen LH, Lai PL, Fu TS, Niu CC, et al. Computed tomography-based navigation-assisted pedicle screw insertion for thoracic and lumbar spine fractures. Chang Gung Med J. 2012;35:332–8. doi: 10.4103/2319-4170.106137. [DOI] [PubMed] [Google Scholar]
- 9.Ruf M, Harms J. Pedicle screws in 1- and 2-year-old children: Technique, complications, and effect on further growth. Spine (Phila Pa 1976) 2002;27:E460–6. doi: 10.1097/00007632-200211010-00019. [DOI] [PubMed] [Google Scholar]
- 10.Ruf M, Harms J. Posterior hemivertebra resection with transpedicular instrumentation: Early correction in children aged 1 to 6 years. Spine (Phila Pa 1976) 2003;28:2132–8. doi: 10.1097/01.BRS.0000084627.57308.4A. [DOI] [PubMed] [Google Scholar]
- 11.Han W, Gao ZL, Wang JC, Li YP, Peng X, Rui J, et al. Pedicle screw placement in the thoracic spine: A comparison study of computer-assisted navigation and conventional techniques? Orthopedics. 2010;33(8) doi: 10.3928/01477447-20100625-14. doi: 10.3928/01477447-20100625-14. [DOI] [PubMed] [Google Scholar]
- 12.Fuster S, Vega A, Barrios G, Urdaneta I, Ojeda O, Macchia M, et al. Accuracy of pedicle screw insertion in the thoracolumbar spine using image-guided navigation. Neurocirugia (Astur) 2010;21:306–11. doi: 10.4321/s1130-14732010000400003. [DOI] [PubMed] [Google Scholar]
- 13.Gebhard F, Kinzl L, Arand M. Computer-assisted surgery. Unfallchirurg. 2000;103:612–7. doi: 10.1007/s001130050593. [DOI] [PubMed] [Google Scholar]
- 14.Steinmann JC, Mirkovic S, Abitbol JJ, Massie J, Subbaiah P, Garfin SR. Radiographic assessment of sacral screw placement. J Spinal Disord. 1990;3:232–7. [PubMed] [Google Scholar]
- 15.Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, et al. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21:247–55. doi: 10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: A proposed systematic approach to improve accuracy of interpretation. Spine (Phila Pa 1976) 2004;29:767–73. doi: 10.1097/01.brs.0000112071.69448.a1. [DOI] [PubMed] [Google Scholar]
- 17.Mirza SK, Wiggins GC, Kuntz C, 4th, York JE, Bellabarba C, Knonodi MA, et al. Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance: A cadaver study. Spine (Phila Pa 1976) 2003;28:402–13. doi: 10.1097/01.BRS.0000048461.51308.CD. [DOI] [PubMed] [Google Scholar]
- 18.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: A meta-analysis. Spine (Phila Pa 1976) 2007;32:E111–20. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 19.Verma R, Krishan S, Haendlmayer K, Mohsen A. Functional outcome of computer-assisted spinal pedicle screw placement: A systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J. 2010;19:370–5. doi: 10.1007/s00586-009-1258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson AN, Polly DW, Jr, Guidera KJ, Mielke CH, Santos ER, Ledonio CG, et al. The accuracy of navigation and 3D image-guided placement for the placement of pedicle screws in congenital spine deformity. J Pediatr Orthop. 2012;32:e23–9. doi: 10.1097/BPO.0b013e318263a39e. [DOI] [PubMed] [Google Scholar]
- 21.Tian W, Weng C, Liu B, Li Q, Hu L, Li ZY, et al. Posterior fixation and fusion of unstable Hangman's fracture by using intraoperative three-dimensional fluoroscopy-based navigation. Eur Spine J. 2012;21:863–71. doi: 10.1007/s00586-011-2085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]