Abstract
We describe a case of entrapment neuropathy of the infrapatellar branch of the saphenous nerve as it pierces sartorius muscle. This is a rare cause of anteromedial knee pain that is easily overlooked and may be mistaken as arising from other anatomical structures in that region. The pain was successfully treated by partially dividing the sartorius muscle and translocating the nerve away from the site of entrapment. It is important to consider entrapment neuropathy of the infrapatellar branch of the saphenous nerve as a differential diagnosis when assessing a patient with anteromedial knee pain.
Keywords: Infrapatellar branch of saphenous nerve, knee pain, nerve entrapment, saphenous nerve, sartorius
MeSH terms: Entrapment neuropathies, knee joint, surgical procedures, operative
Introduction
Entrapment neuropathy of the infrapatellar branch of the saphenous nerve is a rare and often overlooked cause of pain in the anterior and/or medial aspect of the knee. The condition accounts for < 1% of adults presenting with lower extremity pain.1,2 As a result, the symptoms may be mistaken for other more commonly encountered disorders affecting this region, such as patellofemoral pain syndrome, knee joint osteoarthritis, medial meniscus injuries, pes anserine bursitis, and medial collateral ligament injuries.3,4 Failure to recognize this condition can result in delayed diagnosis and the patient may undergo unnecessary investigations or treatment.
We present a case of anteromedial knee pain caused by entrapment of the infrapatellar branch of the saphenous nerve by sartorius. In doing so, we seek to remind the reader of this unusual, but important, cause of anteromedial knee pain and describe its successful treatment by surgical release of the sartorius muscle.
Case Report
A 33 year old male patient presented with complaints of pain in the anteromedial aspect of the right knee. The pain had been ongoing for the last 4 years, but increased in severity for the last 8 months. The pain was exacerbated by movement of the knee joint, particularly when getting up from a chair and climbing or descending stairs. The patient described hypersensitivity in the infrapatellar region and was unable to wear tight fitting trousers, as even the slightest touch aggravated the pain. The patient was otherwise fit and well, with no history of trauma or surgery to the knee. Physical examination revealed a positive Tinel's sign on the medial aspect of the right knee, approximately 6 cm proximal to the joint line. Pressure over this area reproduced the patient's pain, which he described as “shooting” in nature.
Radiographs of the knee joint revealed no bone abnormality. A magnetic resonance scan revealed early degenerative changes within the posterior horn of medial meniscus and a Grade I injury of the medial collateral ligament. The patient was started on a course of physiotherapy and analgesics, but these measures failed to relieve the pain. In view of the specific point tenderness on examination, we considered nerve entrapment or neuroma a possibility and, therefore, decided to explore this area.
At surgery, the infrapatellar branch of the saphenous nerve was found traversing the sartorius muscle at the site of maximum tenderness and making a tight angle on its way to the skin of the infrapatellar area [Figures 1 and 2]. We identified this as the likely cause of pain and partially divided the sartorius muscle in order to free the nerve, so that it lay in a straight line course without any tension or points of compression [Figure 3]. The patient described the relief of his pain immediately postoperatively and this has continued until his most recent followup at 6 months. Initially, he had mild numbness in the infrapatellar region, which has since recovered.
Figure 1.
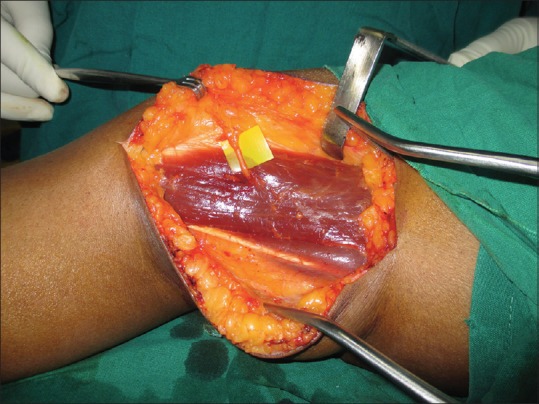
Peroperative photograph showing medial aspect of the patient's left knee undergoing surgical exploration. The infrapatellar branch of saphenous nerve is seen exiting the sartorius muscle on its way to innervating the skin
Figure 2.
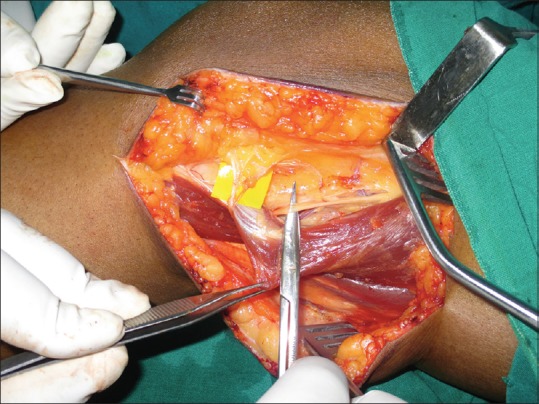
Peroperative photograph showing sartorius muscle being reflected to reveal the straight course of the infrapatellar branch of the saphenous nerve before it pierces sartorius at an acute angle
Figure 3.

Peroperative photograph showing the superior half of the sartorius muscle has been divided to free the infrapatellar branch of the saphenous nerve and allow it to lie in a straight line, away from the site of entrapment
Discussion
The saphenous nerve is well-known to orthopedic surgeons as a possible site of iatrogenic nerve injury; its anatomical course makes it vulnerable during procedures such as knee replacement surgery, hamstring tendon harvest, knee arthroscopy, and tibial nailing.5 However, in those cases with no history of surgery or trauma to the region, the diagnosis of saphenous nerve neuropathy is easy to overlook.
The saphenous nerve is the largest and longest branch of the femoral nerve. It is formed from branches of the L3 and L4 nerve roots and is purely sensory in function. At the level of the medial femoral condyle, the saphenous nerve divides into two branches; the infrapatellar branch, which innervates the skin below the patella as well as the anterior inferior knee capsule and the terminal saphenous branch, which innervates the skin of the anterior and medial lower leg.
Arthornthurasook and Gaew-Im studied the relationship of the infrapatellar branch of the saphenous nerve to the sartorius in 20 cadavers.6 In most (62%) cases, the infrapatellar branch became superficial at the posterior border of the sartorius and crossed the surface of that muscle to the front of the knee. However, in 22% of specimens, as in the case we present, the nerve penetrated the muscle. It is in such cases, the nerve is prone to stretch or compression each time sartorius contracts.
Imaging studies such as magnetic resonance imaging or ultrasound can help define the relationship of the saphenous nerve to the sartorius muscle. However, the surgeon should be wary of ascribing the pain to low grade, asymptomatic pathology which might be revealed elsewhere. Although some authors report that electromyogram or nerve conduction studies are helpful in the diagnosis, others do not feel it offers any diagnostic assistance and prefer local injection of anesthetic to confirm nerve involvement.5,7 Another means of diagnosis is to create tension in the saphenous nerve by placing the patient in a position of hip extension and abduction with full knee flexion. This is reported to reproduce the pain of saphenous nerve entrapment.4
Treatment for saphenous nerve entrapment may be surgical or nonsurgical. We were able to successfully treat the pain by releasing the infrapatellar branch from the sartorius muscle and a handful of reports in the literature describe similar success from surgical decompression.8,9,10 Nonsurgical treatment includes activity modification and various physiotherapy techniques. These include myofascial release, vibration therapy and nerve flossing.4 Alternatively, local anesthetic and corticosteroid injections may be tried, but these only provide temporary relief.5
We describe a rare case of entrapment of the infrapatellar branch of the saphenous nerve, attributable to its anatomical relationship to the sartorius muscle. Clinicians should be aware of this as a possible diagnosis when evaluating patients with pain in the anterior and/or medial aspect of the knee. Clues toward the diagnosis are pain exacerbated using stairs or kneeling, associated with point tenderness at the level of the medial femoral condyle where the infrapatellar branch of the saphenous nerve pierces sartorius. In such cases, surgical release of the nerve by dividing sartorius can successfully treat the pain.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mumenthaler M, Schlaick H. Peripheral Nerve Lesions, Diagnosis and Therapy. New York: Thieme Medical Publishers; 1991. [Google Scholar]
- 2.Pendergrass TL, Moore JH. Saphenous neuropathy following medial knee trauma. J Orthop Sports Phys Ther. 2004;34:328–34. doi: 10.2519/jospt.2004.1269. [DOI] [PubMed] [Google Scholar]
- 3.Morganti CM, McFarland EG, Cosgarea AJ. Saphenous neuritis: A poorly understood cause of medial knee pain. J Am Acad Orthop Surg. 2002;10:130–7. doi: 10.5435/00124635-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Porr J, Chrobak K, Muir B. Entrapment of the saphenous nerve at the adductor canal affecting the infrapatellar branch – A report on two cases. J Can Chiropr Assoc. 2013;57:341–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Trescot AM, Brown MN, Karl HW. Infrapatellar saphenous neuralgia – Diagnosis and treatment. Pain Physician. 2013;16:E315–24. [PubMed] [Google Scholar]
- 6.Arthornthurasook A, Gaew-Im K. Study of the infrapatellar nerve. Am J Sports Med. 1988;16:57–9. doi: 10.1177/036354658801600110. [DOI] [PubMed] [Google Scholar]
- 7.Romanoff ME, Cory PC, Jr, Kalenak A, Keyser GC, Marshall WK. Saphenous nerve entrapment at the adductor canal. Am J Sports Med. 1989;17:478–81. doi: 10.1177/036354658901700405. [DOI] [PubMed] [Google Scholar]
- 8.Lippitt AB. Neuropathy of the saphenous nerve as a cause of knee pain. Bull Hosp Jt Dis. 1993;52:31–3. [PubMed] [Google Scholar]
- 9.House JH, Ahmed K. Entrapment neuropathy of the infrapatellar branch of the saphenous nerve. Am J Sports Med. 1977;5:217–24. doi: 10.1177/036354657700500509. [DOI] [PubMed] [Google Scholar]
- 10.Tennent TD, Birch NC, Holmes MJ, Birch R, Goddard NJ. Knee pain and the infrapatellar branch of the saphenous nerve. J R Soc Med. 1998;91:573–5. doi: 10.1177/014107689809101106. [DOI] [PMC free article] [PubMed] [Google Scholar]


