Abstract
Duane syndrome (DS) is a common form of congenital cranial dysinnervation disorders. The ocular motility pattern lies in a wide clinical spectrum, and the choice of treatment must be individualized depending on the severity of the clinical findings. There is no perfect method of treatment and no real “cure” in DS. In this paper, the aim is to give some guidelines to the reader for selection of the most appropriate treatment method for the patient.
Keywords: Congenital cranial dysinnervation disorders, Duane syndrome, Duane's retraction syndrome, strabismus, synergistic divergence, Y-pattern deviation, Y splitting, paradoxical innervation, periosteal fixation, upshoots and downshoots, vertical retraction syndrome
Introduction
In its original description, Duane syndrome (DS) is defined as an ocular motility disorder characterized with severe abduction deficiency, variable limitation of adduction, globe retraction with narrowing of the palpebral fissure, and oblique elevation or depression on adduction.[1] DS represents 1%–4% of strabismic population; it is more common in females and more common in left eyes.[2] Bilaterality is not uncommon, and nearly 10% of the cases are reported to be familial. In this paper, factors about etiology that may influence surgical results, goals of treatment, and surgical treatment methods with possible results will be reviewed with a decision-making approach.
Etiology and Classification
DS is primarily an innervational disorder with secondary restrictive problems. Electromyographic (EMG) studies revealed paradoxical contraction of lateral rectus (LR) muscle on adduction.[3,4,5] Histopathological studies demonstrated the absence of abducens nucleus and partial innervation of LR muscle by branches of oculomotor nerve.[6,7,8] The number of the cases are limited in histopathological studies. The studies with neuroimaging devices provided information in a large group of patients with broad clinical spectrum and led us to understand the variable manifestations of the abnormal development of ocular motor nerves.[9,10,11] In an early brainstem magnetic resonance imaging (MRI) study, we could only demonstrate the abducens nerve on the normal side of two out of ten patients.[12] However, with new-generation MRI equipment, more reliable data could be obtained in various types of DS. Kim and Hwang[13] demonstrated that the abducens nerve was absent in all cases with Type 1 DS, it was present in all Type 2 patients, and it was either absent or present in Type 3 DS. Studies with MRI also demonstrated that the LR muscle thickness was within normal range as the problem is a dysinnervation, not a “lack” of innervation.[12,14,15] The absence of denervation atrophy may serve as a clue for the differential diagnosis of DS with abducens nerve palsy in cases where there is any confusion.
Familial cases suggested an underlying genetic problem, and the gene mapping is done in familial isolated DS.[16] The associated abnormalities and the association of DS with thalidomide embryopathy suggested a teratogenic effect during second gestational month. However, no common maternal factor could be demonstrated up to date in isolated DS.[17] DS is accepted as the most common form of “congenital cranial dysinnervation syndromes” (CCDD).
In Huber's[2] well-known classification, DS is divided into three types. The features of these three types may be summarized as below:
Type 1: Marked limitation of abduction, normal or slightly defective adduction
Type 2: Marked limitation of adduction, normal or slightly defective abduction
Type 3: Marked limitation of abduction and adduction.
In typical forms, the main EMG abnormality is paradoxical contraction of LR muscle. However, paradoxical contraction of medial rectus (MR), inferior oblique (IO), and vertical rectus muscles was previously reported in typical forms, but the abnormal contraction of these muscles is usually underestimated.[3,4,5,18]
The abnormal innervation of extraocular muscles which does not fit Huber's classification is called as “atypical DS.”
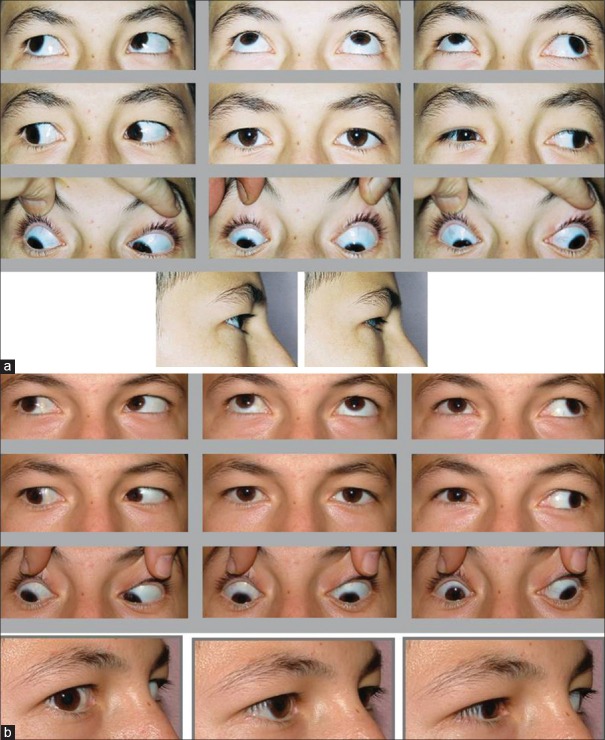
Vertical retraction syndrome is one of these described forms. These patients may have the features of a horizontal DS plus a globe retraction on vertical positions of gaze with or without limitation of vertical eye movements. In a case with Type 1 DS plus globe retraction on adduction, elevation, and depression, we performed EMG [Figure 1]. That case demonstrated paradoxical contraction of vertical recti on elevation, depression, adduction, and on attempted abduction. Scott and Wong[4] demonstrated abnormal activity of superior rectus (SR), inferior rectus (IR), and IO muscles on adduction. However, in the presented case, both vertical recti contracted not only on adduction but also on abduction, elevation, and depression.
Figure 1.
Left type 1 Duane syndrome with globe retraction on adduction, upgaze and downgaze. Both vertical rectus muscles were found to have contraction with electromyography on elevation, depression adduction, and abduction
Synergistic divergence is another form of DS that is characterized with divergence on abduction and limitation of adduction. EMG data demonstrated co-contraction and excessive LR firing on adduction.[19] The unopposed paradoxical contraction of LR with an underacting MR is claimed for this peculiar motility disorder. We reported a group of three patients with synergistic divergence in association with congenital fibrosis of extraocular muscles (CFEOM).[20] Another group of four patients with CFEOM and synergistic divergence is also reported.[21] The fibrotic changes appear secondary to innervational abnormalities both in CFEOM and DS, so it is suggested that these two ocular motility disorders are varieties of the same clinical spectrum as CCDD.
Another form of atypical DS is Y-pattern deviation. Kushner[22] demonstrated paradoxical contraction of LR muscle in Y-pattern deviation and proposed that it was a variant of DS. We reported a group of four patients with Y-pattern deviation, and our results also suggested that it was a variant of DS.[23] However, our results demonstrated that the co-contracting muscle might be the IR muscle as well as the LR muscle.[23,24] The paradoxical contraction of IR rectus muscle was demonstrated either by EMG or kinematic MRI examination.
It is considered that the up and downshoots in adduction are secondary to the leash effect of paradoxically contracting fibrotic LR muscle.[25] We suggested that the mechanism of a Y-pattern with a co-contracting IR muscle might be similar with the mechanism of upshoot on adduction.[24] If a co-contracting LR muscle may cause an upshoot on adduction, then a co-contracting IR muscle may cause abduction on elevation – a similar condition that is 90° turned in clockwise.
In an attempt to demonstrate some common clues among atypical forms of DS, we reported a group of nine patients with atypical forms of DS.[26] There was no globe retraction in four patients, and paradoxical contraction of vertical rectus muscles was found in three of the cases. The findings of our patients suggested that globe retraction is not a common abnormality in atypical forms of DS. It was previously demonstrated that globe retraction may not occur even in typical forms of DS.[27] We concluded that the term retraction syndrome needs to be abandoned. We proposed the addition of atypical forms into Huber's classification as below:[26]
Type 4: Synergistic divergence
Type 5: Vertical retraction syndrome
Type 6: Y-pattern deviation.
Even more atypical forms may be observed in DS. We previously reported a case with λ-pattern exodeviation and globe retraction on adduction.[28] In this case, kinematic MRI examination demonstrated bilateral accessory extraocular muscle below the optic nerve that demonstrated a paradoxical contraction on downgaze. This case also had bilateral IR hypoplasia and was the first documented case with paradoxical contraction in an accessory extraocular muscle.
Although Huber's classification does not perfectly cover all of the cases and there are overlaps, especially in Type 1 and Type 3 cases, it is still useful for an easy documentation of the cases with DS.
Common Clinical Features
The major clinical finding is a limitation of abduction and/or adduction that may be associated with esotropia, exotropia, or orthophoria. Abnormal head posture and globe retraction on adduction are the other common clinical features. Up and downshoots on adduction and alphabetical patterns are also frequent. Children with DS require regular follow-up as amblyopia is a frequent finding. Binocular functions are usually good in most of the patients as many of them have orthophoria in a certain position of gaze with abnormal head posture.
Treatment
The surgeon must be ready for surprises as DS is a dysinnervation plus restriction and the extraocular muscles do not behave as in concomitant strabismus. The general principle is not to operate unless clear-cut indications are present. As a general rule, resections should be avoided, and the normal eye may be operated where necessary. As the predictability of surgical outcome is low compared to conventional strabismus surgery, adjustable sutures are preferable where possible.
The surgeon must be aware that in both typical and atypical forms of DS, there may be a paradoxical contraction in extraocular muscles other than LR muscle, and this paradoxical contraction may even affect accessory extraocular muscle (s).
The goals of treatment are primarily to eliminate the deviation in primary position and abnormal head posture as well as to center the diplopia-free field and to reduce up and downshoots. The secondary goals are to reduce globe retraction and to improve ductions and enlarge binocular field of single vision.
The treatment options are recession of the appropriate horizontal rectus muscle of the affected and/or the sound eye, recession of both horizontal recti (more in one muscle), transposition of vertical recti, and LR inactivation by periosteal fixation.
Recession of one horizontal rectus muscle of the affected eye
Advantages
Decrease in the deviation in primary position
Decrease of abnormal head posture.
Disadvantages
Possible limitation of adduction
Possible decrease of binocular field of single vision
No significant improvement on abduction
No decrease in globe retraction
No decrease in up/downshoot.
Indications
Horizontal deviation
Minimal or no globe retraction
No up/downshoot.
This is the most simple way of management of DS with favorable results; however, it also has some limitations and problems.[29,30,31,32] As most of the patients with DS have some degree of limitation of adduction that may only be identified by a small exotropia on adduction; MR recession causes some degree of limitation of adduction. The decrease of adduction may cause a decrease in binocular field of single vision that may be bothersome for some patients. There is no reliable surgical dose/effect relation for single muscle recession, and the major pitfall is the decision on the amount of recession. If the recession is too much the paradoxical contraction of LR may dominate over the MR contraction, and iatrogenic synergistic divergence may develop in postoperative period.[32] The amount of recession must be determined upon the forced duction test during surgery, and it must be the amount that allows free passive movement of the eye. MR muscle is usually tight, and recession of tight muscles has larger effect on deviation.
If the deviation is large, recession of the appropriate horizontal rectus muscle in the contralateral eye may be considered.[30,33,34] Surgery in the yoke muscle of the sound eye must be regarded with caution. The amount of paradoxical contraction of the LR or the paradoxical contraction of vertical rectus muscles may cause unexpected motility results.[35,36]
Recession of both horizontal recti of the affected eye (more in one muscle)
Advantages
Decrease of the deviation in primary position
Decrease of abnormal head posture
Possible decrease in globe retraction
Possible decrease in up/downshoot
Disadvantages
No significant improvement on abduction
Possible decrease on adduction
Possible decrease of binocular field of single vision
Technical difficulty as the operation is on more posterior site.
Indications
Cases with horizontal deviation and moderate-to-severe globe retraction
Up/downshoots – combined Y splitting of LR muscle should be planned in significant up/downshoots.
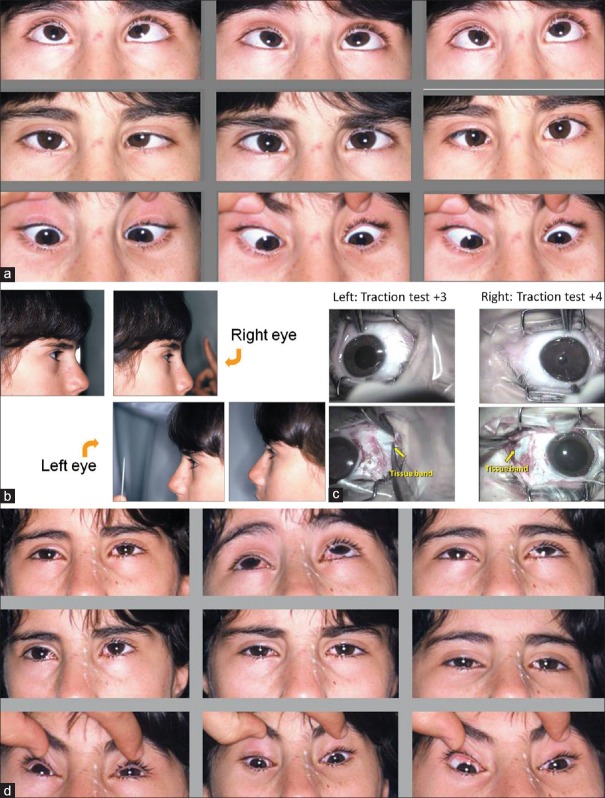
Recession of both horizontal recti in the affected eye has the advantage of combination with Y splitting of LR muscle where necessary.[37,38,39,40,41] In our clinical practice, this is the most commonly used procedure in DS [Figure 2a and b]. Our results demonstrated that recession of both horizontal recti may decrease the globe retraction in 75% of the cases and up/downshoots as well as the deviation in primary position and abnormal head posture [Figure 3].[41] In our series, we concluded that transposition surgery should be kept for those with minimal globe retraction.[41]
Figure 2.
Right type 2 Duane syndrome with up and downshoot and significant globe retraction. (b) Right type 2 after recession of both horizontal recti and Y splitting of lateral rectus muscle. Note the decrease of globe retraction as well as up and downshoot
Figure 3.
(a) Left type 1 Duane syndrome with significant globe retraction on adduction. (b) Note the decrease of globe retraction and esotropia following 10mm recession of medial rectus and 5 mm recession of lateral rectus muscle in the left eye
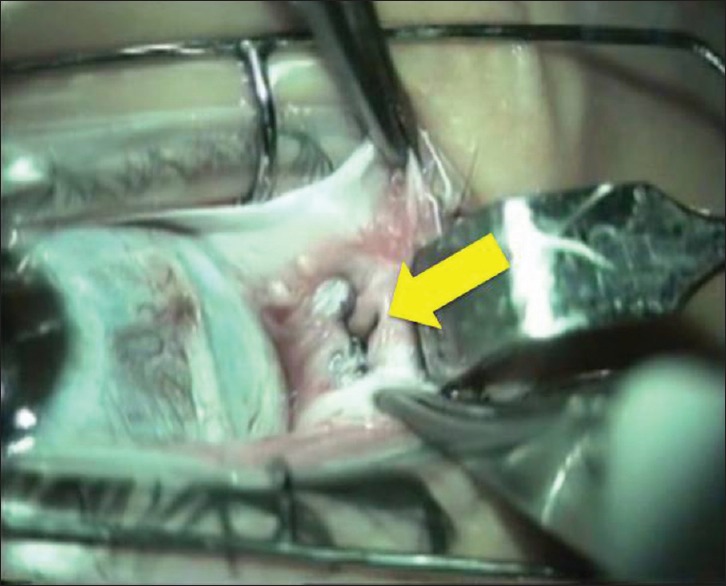
In both single muscle recession and both horizontal rectus recessions, forced duction test must be repeated after disinsertion of the medial or LR muscle. There may be some accessory tissue bands that restrict the ocular movements. Gobin[42] reported the incidence of such bands as 34.3% in cases with DS during surgery. The excision of the tissue band may allow free forced duction test [Figure 4a–d].
Figure 4.
(a) Bilateral type 1 Duane syndrome with esodeviation and severe limitation of abduction. There is mild globe retraction on adduction in both eyes. (b) Bilateral type 1 Duane syndrome with globe retraction on adduction in both eyes. (c) Bilateral type 1 Duane syndrome. Traction test is positive in both eyes (+4 in the right eye and +3 in the left eye). Traction test is still positive after disinsertion of medial rectus muscle, and a tissue band was recognized behind the insertion beneath the medial rectus muscle on both sides. The tissue band is excised during surgery. (d) In primary position, the patient is orthophoric. Note the decrease of adduction on both sides following medial rectus recession and the tissue band excision
Resections of horizontal rectus muscles
The general rule is to avoid resections in DS. However in eso-DS with minimal globe retraction, recess-resect surgery is reported to be successful if the resection is kept within 3.5 mm at most.[43] In our hands, resection of MR muscle may give good results in Type 2 DS with insignificant limitation of adduction. It must be kept in mind that these are very selected cases and the forced duction test must be negative for the muscle that resection is considered. Even a small resection in a paradoxically contracting and fibrotic extraocular muscle may cause unexpected results, and it should better be used by adjustable sutures where possible.
Transposition of vertical recti (usually combined with medial rectus recession)
Advantages
Possible increase of abduction
Possible increase binocular field of single vision.[28]
Disadvantages
Possible increase of globe retraction
Risk of anterior segment ischemia
Possible deterioration of the vertical muscle function
No decrease of up/downshoot
Possible restriction on adduction.
Indications
Cases with horizontal deviations and with minimal or no globe retraction
Severe limitation of abduction
No globe retraction on up and downgaze
No up/downshoot.
Rosenbaum[44] reported that vertical rectus transposition temporally has a greater chance of causing an induced vertical deviation. Augmentation sutures increase the tightening effect.[45,46] Vertical deviations and increase in co-contraction are reported between 8.5% and 30%, and consecutive exotropia rate is reported as 25.5%.[47]
Transposition of SR instead of two vertical rectus transpositions may be performed with or without MR recession.[48,49,50] Augmentation sutures are also possible with this technique. SR transposition is proposed to have a similar effect with both vertical recti transposition. The additional potential problem may be induced incyclotorsion.
Lateral rectus periosteal fixation into the lateral orbital wall
Advantages
Eliminates the effect of paradoxical contraction of LR
Very effective to reduce up/downshoot
Reduces globe retraction.
Disadvantages
Usually requires a combination with vertical rectus transposition surgery
Anterior segment ischemia risk because of transposition surgery
May require secondary surgery
Limited literature data
Technically difficult procedure.
Indications
Severe disfiguring up/down shoot
Synergistic divergence.
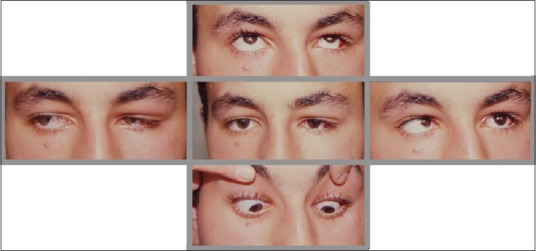
LR periosteal fixation is the most recently described method of treatment for DS[51,52,53,54,55,56,57] [Figure 5]. The idea is to convert DS into 6th nerve palsy by eliminating the junction of the LR muscle with the globe, so it requires a combination with transposition surgery. LR periosteal fixation eliminates the effect of paradoxical contraction of LR, and it is reported to be very effective to reduce up/downshoots as well as globe retraction. Posterior Tenon or lateral canthal tendon fixation of LR muscle are the proposed alternatives to periosteal fixation.[58,59] In synergistic divergence which is the most severe form of exo-DS cases with weak MR function, transposition surgery may be considered as a secondary operation where necessary.[56] In our cases, augmented transpositions caused residual exodeviation and nonaugmented transposition gave better results in exo-DS.[55] In eso-DS, secondary MR recession may be required on a separate session as the fourth rectus muscle. In such cases, the major disadvantage of this technique is the anterior segment ischemia risk despite all the measures such as ciliary artery preserving surgery and partial transposition procedures. In our cases, the up/downshoots significantly reduced in all patients whereas globe retraction decreased but not disappeared. The persistence of globe retraction may be due to the possible subclinical paradoxical contraction in transposed vertical recti or LR muscle may still exert a pulling force through the surrounding soft tissues.
Figure 5.
Lateral rectus periosteal fixation, lateral rectus is sutured at the lateral orbital wall with nonabsorbable sutures
The persistence of globe retraction and residual exodeviations demonstrated that LR orbital wall fixation could not convert the patient into a 6th nerve palsy, and the response of surgery is different than that of 6th nerve palsy.
Methods to reduce up/downshoots
The recommended methods which have already been discussed above for treatment of up and downshoots are recession of both horizontal recti, Y splitting of LR muscle, faden operation of both horizontal recti, vertical muscle recession for innervational up and downshoots, and LR inactivation by periosteal fixation.[37,38,39,40,41,51,52,53,54,55,60,61] “Y” splitting of LR increases the stability of the LR muscle on adduction. Splitting the LR muscle creates some resection effect and should better be combined with a small recession to compensate this.
Treatment of “Y” pattern deviation
In the atypical DS “Y” pattern deviation, surgical treatment is usually not necessary. Pseudo IO overaction does not respond to IO weakening and supraplacement and recession of LR muscle is demonstrated to be effective.[22,23]
Role of botulinum toxin A
Botulinum toxin A (BTXA) may be used for diagnostic purpose in DS to demonstrate the possible postoperative result, and in 53% of cases, long-term reduction of the deviation was obtained out of 88 patients.[62] Young patients may also benefit with BTXA injection and 50% success was reported in a series of eight patients.[63]
Conclusions
During preoperative assessment, the deviation in primary position, abnormal head posture, severity of globe retraction, and presence of up and downshoots must be carefully evaluated for a correct surgical plan for the individual patient.
The traction test results are extremely important during steps of surgery.
The surgeon should consider the individual variables and should keep in mind that the vertical rectus muscles may also have some subclinical dysinnervation problem. Although “cure” is not possible, a satisfactory outcome may usually be achieved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Duane A. Congenital deficiency of abduction, associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. Arch Ophthalmol. 1905;34:133–59. doi: 10.1001/archopht.1996.01100140455017. [DOI] [PubMed] [Google Scholar]
- 2.DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane's retraction syndrome. Surv Ophthalmol. 1993;38:257–88. doi: 10.1016/0039-6257(93)90077-k. [DOI] [PubMed] [Google Scholar]
- 3.Huber A. Electrophysiology of the retraction syndromes. Br J Ophthalmol. 1974;58:293–300. doi: 10.1136/bjo.58.3.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott AB, Wong GY. Duane's syndrome. An electromyographic study. Arch Ophthalmol. 1972;87:140–7. doi: 10.1001/archopht.1972.01000020142005. [DOI] [PubMed] [Google Scholar]
- 5.Strachan IM, Brown BH. Electromyography of extraocular muscles in Duane's syndrome. Br J Ophthalmol. 1972;56:594–9. doi: 10.1136/bjo.56.8.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hotchkiss MG, Miller NR, Clark AW, Green WR. Bilateral Duane's retraction syndrome. A clinical-pathologic case report. Arch Ophthalmol. 1980;98:870–4. doi: 10.1001/archopht.1980.01020030864013. [DOI] [PubMed] [Google Scholar]
- 7.Miller NR, Kiel SM, Green WR, Clark AW. Unilateral Duane's retraction syndrome (Type 1) Arch Ophthalmol. 1982;100:1468–72. doi: 10.1001/archopht.1982.01030040446016. [DOI] [PubMed] [Google Scholar]
- 8.Mulhern M, Keohane C, O’Connor G. Bilateral abducens nerve lesions in unilateral type 3 Duane's retraction syndrome. Br J Ophthalmol. 1994;78:588–91. doi: 10.1136/bjo.78.7.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsa CF, Grant PE, Dillon WP, Jr, du Lac S, Hoyt WF. Absence of the abducens nerve in Duane syndrome verified by magnetic resonance imaging. Am J Ophthalmol. 1998;125:399–401. doi: 10.1016/s0002-9394(99)80158-5. [DOI] [PubMed] [Google Scholar]
- 10.Ozkurt H, Basak M, Oral Y, Ozkurt Y. Magnetic resonance imaging in Duane's retraction syndrome. J Pediatr Ophthalmol Strabismus. 2003;40:19–22. doi: 10.3928/0191-3913-20030101-07. [DOI] [PubMed] [Google Scholar]
- 11.Demer JL, Clark RA, Lim KH, Engle EC. Magnetic resonance imaging evidence for widespread orbital dysinnervation in dominant Duane's retraction syndrome linked to the DURS2 locus. Invest Ophthalmol Vis Sci. 2007;48:194–202. doi: 10.1167/iovs.06-0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Özkan SB, Arıbal E, Orhan M, Sanaç AŞ, Duman S. The results of magnetic resonance imaging in Duane's retraction syndrom. In: Kaufmann H, editor. Transactions 21st Meeting European Strabismological Association. Salzburg: Gahmig Press; 1993. pp. 157–62. [Google Scholar]
- 13.Kim JH, Hwang JM. Presence of the abducens nerve according to the type of Duane's retraction syndrome. Ophthalmology. 2005;112:109–13. doi: 10.1016/j.ophtha.2004.06.040. [DOI] [PubMed] [Google Scholar]
- 14.Kang NY, Demer JL. Comparison of orbital magnetic resonance imaging in duane syndrome and abducens palsy. Am J Ophthalmol. 2006;142:827–34. doi: 10.1016/j.ajo.2006.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ozkan SB, Aribal ME. Comparison of orbital magnetic resonance imaging in Duane syndrome and abducens palsy. Am J Ophthalmol. 2007;143:907. doi: 10.1016/j.ajo.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 16.Graeber CP, Hunter DG, Engle EC. The genetic basis of incomitant strabismus: Consolidation of the current knowledge of the genetic foundations of disease. Semin Ophthalmol. 2013;28:427–37. doi: 10.3109/08820538.2013.825288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aydın P, Mc Gettrick P, Özkan SB, Mc Whinnie H, Nohutçu AF, Sanaç AŞ. A multicentric study on the etiology of Duane's syndrome. International Neuro-Ophthalmological Society Eleventh Meeting, 1996. Neuro-Ophthalmology. 1996;16(Suppl):270. [Google Scholar]
- 18.Saad N, Lee J. Medial rectus electromyographic abnormalities in Duane syndrome. J Pediatr Ophthalmol Strabismus. 1993;30:88–91. doi: 10.3928/0191-3913-19930301-06. [DOI] [PubMed] [Google Scholar]
- 19.Wilcox LM, Jr, Gittinger JW, Jr, Breinin GM. Congenital adduction palsy and synergistic divergence. Am J Ophthalmol. 1981;91:1–7. doi: 10.1016/0002-9394(81)90342-1. [DOI] [PubMed] [Google Scholar]
- 20.Özkan SB, Kır E. Synergistic divergence in association with congenital extraocular muscle fibrosis. In: Lennerstrand G, editor. Advances in Strabismology. Buren, The Netherlands: Aeolous Press; 1998. pp. 150–3. [Google Scholar]
- 21.Brodsky MC. Hereditary external ophthalmoplegia synergistic divergence, jaw winking, and oculocutaneous hypopigmentation: A congenital fibrosis syndrome caused by deficient innervation to extraocular muscles. Ophthalmology. 1998;105:717–25. doi: 10.1016/S0161-6420(98)94029-5. [DOI] [PubMed] [Google Scholar]
- 22.Kushner BJ. Pseudo inferior oblique overaction associated with Y and V patterns. Ophthalmology. 1991;98:1500–5. doi: 10.1016/s0161-6420(91)32098-0. [DOI] [PubMed] [Google Scholar]
- 23.Özkan SB, Kır E. Y pattern exodeviation – A variant of Duane's retraction syndrome. In: Lennerstrand G, editor. Advances in Strabismology. Buren, The Netherlands: Aeolous Press; 1998. pp. 305–8. [Google Scholar]
- 24.Ozkan SB, Aribal EM, Can D, Karaman ZC. Kinematic magnetic resonance imaging in Y pattern exodeviations. J Pediatr Ophthalmol Strabismus. 2003;40:39–43. doi: 10.3928/0191-3913-20030101-12. [DOI] [PubMed] [Google Scholar]
- 25.Jampolsky A. Duane syndrome. In: Rosenbaum A, Santiago AP, editors. Clinical Strabismus Management. Philadelphia: WB Saunders Company; 1999. pp. 325–42. [Google Scholar]
- 26.Özkan SB, Dündar S, Kır E, Dayanır V. Atypical forms of Duane's retraction syndrome – A reappraisal of the classical definition. In: de Faber JT, editor. Transactions 26th Meeting European Strabismological Association. Barcelona: Aeolus Press; 2000. pp. 199–202. [Google Scholar]
- 27.Gross SA, Tien DR, Breinin GM. Aberrant innervational pattern in Duane's syndrome type II without globe retraction. Am J Ophthalmol. 1994;117:348–51. doi: 10.1016/s0002-9394(14)73144-7. [DOI] [PubMed] [Google Scholar]
- 28.Ozkan SB, Ozsunar Dayanir Y, Gökçe Balci Y. Hypoplastic inferior rectus muscle in association with accessory extraocular muscle and globe retraction. J AAPOS. 2007;11:488–90. doi: 10.1016/j.jaapos.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 29.Pressman SH, Scott WE. Surgical treatment of Duane's syndrome. Ophthalmology. 1986;93:29–38. doi: 10.1016/s0161-6420(86)33777-1. [DOI] [PubMed] [Google Scholar]
- 30.Barbe ME, Scott WE, Kutschke PJ. A simplified approach to the treatment of Duane's syndrome. Br J Ophthalmol. 2004;88:131–8. doi: 10.1136/bjo.88.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson LB. Severe adduction deficiency following a large medial rectus recession in Duane's retraction syndrome. Arch Ophthalmol. 1986;104:859–62. doi: 10.1001/archopht.1986.01050180093038. [DOI] [PubMed] [Google Scholar]
- 32.Shiratori A, Kameyama C, Sibasaki K. Adduction deficiency following a large medial rectus recession in Duane's retraction syndrome type 1. J Pediatr Ophthalmol Strabismus. 1999;36:98–100. doi: 10.3928/0191-3913-19990301-12. [DOI] [PubMed] [Google Scholar]
- 33.Saunders RA, Wilson ME, Bluestein EC, Sinatra RB. Surgery on the normal eye in Duane retraction syndrome. J Pediatr Ophthalmol Strabismus. 1994;31:162–9. doi: 10.3928/0191-3913-19940501-08. [DOI] [PubMed] [Google Scholar]
- 34.Farvardin M, Rad AH, Ashrafzadeh A. Results of bilateral medial rectus muscle recession in unilateral esotropic Duane syndrome. J AAPOS. 2009;13:339–42. doi: 10.1016/j.jaapos.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 35.Greenberg MF, Pollard ZF. Poor results after recession of both medial rectus muscles in unilateral small-angle Duane's syndrome, type I. J AAPOS. 2003;7:142–5. doi: 10.1016/mpa.2003.S1091853102420010. [DOI] [PubMed] [Google Scholar]
- 36.Guyton D. Round table discussion – The expert view of difficult strabismus and amblyopia. In: Özkan SB, editor. Update on Strabismology. Ankara: Rotatıp Publisher; 2010. pp. 86–9. [Google Scholar]
- 37.von Noorden GK. Recession of both horizontal recti muscles in Duane's retraction syndrome with elevation and depression of the adducted eye. Am J Ophthalmol. 1992;114:311–3. doi: 10.1016/s0002-9394(14)71796-9. [DOI] [PubMed] [Google Scholar]
- 38.Sprunger DT. Recession of both horizontal rectus muscles in Duane syndrome with globe retraction in primary position. J AAPOS. 1997;1:31–3. doi: 10.1016/s1091-8531(97)90020-3. [DOI] [PubMed] [Google Scholar]
- 39.Rogers GL, Bremer DL. Surgical treatment of the upshoot and downshoot in Duanes’ retraction syndrome. Ophthalmology. 1984;91:1380–3. doi: 10.1016/s0161-6420(84)34137-9. [DOI] [PubMed] [Google Scholar]
- 40.Rao VB, Helveston EM, Sahare P. Treatment of upshoot and downshoot in Duane syndrome by recession and Y-splitting of the lateral rectus muscle. J AAPOS. 2003;7:389–95. doi: 10.1016/s1091-8531(03)00213-1. [DOI] [PubMed] [Google Scholar]
- 41.Ozkan SB, Can D, Arsan AK, Demirci S, Kasim R, Duman S. The results of surgical treatment in Duane's retraction syndrome. Strabismus. 1997;5:5–11. doi: 10.3109/09273979709055053. [DOI] [PubMed] [Google Scholar]
- 42.Gobin MH. Surgical management of Duane's syndrome. Br J Ophthalmol. 1974;58:301–6. doi: 10.1136/bjo.58.3.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kraft SP. Lateral rectus resection strabismus surgery in unilateral Duane syndrome with esotropia and limited abduction. Binocul Vis Strabismus Q. 2010;25:149–57. [PubMed] [Google Scholar]
- 44.Rosenbaum AL. Costenbader lecture. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004;8:409–19. doi: 10.1016/j.jaapos.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 45.Velez FG, Foster RS, Rosenbaum AL. Vertical rectus muscle augmented transposition in Duane syndrome. J AAPOS. 2001;5:105–13. doi: 10.1067/mpa.2001.112677. [DOI] [PubMed] [Google Scholar]
- 46.Akar S, Gokyigit B, Pekel G, Demircan A, Demirok A. Vertical muscle transposition augmented with lateral fixation (Foster) suture for Duane syndrome and sixth nerve palsy. Eye (Lond) 2013;27:1188–95. doi: 10.1038/eye.2013.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Velez FG, Laursen JK, Pineles SL. Risk factors for consecutive exotropia after vertical rectus transposition for esotropic Duane retraction syndrome. J AAPOS. 2011;15:326–30. doi: 10.1016/j.jaapos.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 48.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130:195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tibrewal S, Sachdeva V, Ali MH, Kekunnaya R. Comparison of augmented superior rectus transposition with medial rectus recession for surgical management of esotropic Duane retraction syndrome. J AAPOS. 2015;19:199–205. doi: 10.1016/j.jaapos.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 50.Velez FG, Oltra E, Isenberg SJ, Pineles SL. Assessment of torsion after superior rectus transposition with or without medial rectus recession for Duane syndrome and abducens nerve palsy. J AAPOS. 2014;18:457–60. doi: 10.1016/j.jaapos.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Britt MT, Velez FG, Thacker N, Alcorn D, Foster RS, Rosenbaum AL. Surgical management of severe cocontraction, globe retraction, and pseudo-ptosis in Duane syndrome. J AAPOS. 2004;8:362–7. doi: 10.1016/j.jaapos.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 52.Morad Y, Kowal L, Scott AB. Lateral rectus muscle disinsertion and reattachment to the lateral orbital wall. Br J Ophthalmol. 2005;89:983–5. doi: 10.1136/bjo.2004.051219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Parsa CF. A theoretically optimal and practical surgical approach to Duane syndrome. In: De Faber JT, Souza-Dias C, Goldschmidt M, editors. Strabismus 2006, Proceedings of the Joint Congress. The Xth Meeting of the International Strabismological Association ISA and the First Extraordinary Meeting of the Latin American Council of Strabismus CLADE. Sao Paulo: Cultura Médica; 2006. pp. 315–20. [Google Scholar]
- 54.Andalib D, Javadzadeh A. Lateral rectus muscle disinsertion and reattachment to the lateral orbital wall in exotropic Duane syndrome: A case report. J Med Case Rep. 2008;2:253. doi: 10.1186/1752-1947-2-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Özkan SB, Işıklıgil I. Problems with lateral rectus orbital wall fixation in Duane syndrome. In: Gomez de Liano R, editor. Transactions 32nd Meeting of the European Strabismological Association. Belgrade, Spain: 2009. pp. 149–51. [Google Scholar]
- 56.Özkan SB, editor. Round table discussion – Lateral rectus periosteal fixation. Advances in Strabismology. Ankara: Rotatıp Publishers; 2015. pp. 90–2. [Google Scholar]
- 57.Sharma P, Tomer R, Menon V, Saxena R, Sharma A. Evaluation of periosteal fixation of lateral rectus and partial VRT for cases of exotropic Duane retraction syndrome. Indian J Ophthalmol. 2014;62:204–8. doi: 10.4103/0301-4738.121145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Heo H, Park SW. Rectus muscle posterior tenon fixation as an inactivation procedure. Am J Ophthalmol. 2008;146:310–7. doi: 10.1016/j.ajo.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 59.Sukhija J, Singh M, Singh U. Profound weakening of the lateral rectus muscle with attachment to lateral canthal tendon for treatment of exotropic Duane syndrome. J AAPOS. 2012;16:298–300. doi: 10.1016/j.jaapos.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 60.von Noorden GK, Murray E. Up-and downshoot in Duane's retraction syndrome. J Pediatr Ophthalmol Strabismus. 1986;23:212–5. doi: 10.3928/0191-3913-19860901-03. [DOI] [PubMed] [Google Scholar]
- 61.Mohan K, Saroha V. Vertical rectus recession for the innervational upshoot and downshoot in Duane's retraction syndrome. J Pediatr Ophthalmol Strabismus. 2002;39:94–9. doi: 10.3928/0191-3913-20020301-09. [DOI] [PubMed] [Google Scholar]
- 62.Dawson EL, Maino A, Lee JP. Diagnostic use of botulinum toxin in patients with Duane syndrome. Strabismus. 2010;18:21–3. doi: 10.3109/09273970903580199. [DOI] [PubMed] [Google Scholar]
- 63.Maya JF, de Liaño RG, Catalán MR, Rayward O. Botulinum toxin treatment in patients up to 3 years of age who have esotropic Duane retraction syndrome. Strabismus. 2013;21:4–7. doi: 10.3109/09273972.2012.762530. [DOI] [PubMed] [Google Scholar]