Abstract
Carthamin yellow (CY), which is a flavonoid compound isolated from safflower, has various pharmacological effects including promoting blood circulation to remove blood stasis and alleviating pain. CY is a herb used in Chinese traditional medicines. Intervertebral disc degeneration (IDD) is a common spinal disorder and degeneration of nucleus pulposus (NP) cells and inflammation are significant parts of the pathological cascade. The curative effect of CY on NP cells in association with degeneration and inflammation remains to be elucidated. In the present study, rat NP cells were isolated, cultured and used to detect the suppressive effects of CY on lipopolysaccharide (LPS)-induced genetic expression variation and the expression of matrix degradation enzymes, including matrix metallopeptidase-3, ADAM metallopeptidase with thrombospondin type 1 motif (ADAMTS)-4 and ADAMTS-5. A protective effect of CY on NP cells was observed against LPS-induced matrix degradation and inflammation. Western blotting results demonstrated that pretreatment with CY significantly suppressed the LPS-induced activation of the mitogen activated protein kinase (MAPK) pathway. The results of the present study suggested that CY exerted anti-degenerative and anti-inflammatory effects on NP cells via inhibition of MAPK pathway activation. Therefore, CY may be a potential therapeutic drug for the treatment of IDD in the future.
Keywords: carthamins yellow, intervertebral disc, nucleus pulposus cells, degeneration, inflammation
Introduction
Intervertebral disc degeneration (IDD) is a common spinal disorder and is characterized by clinical signs ranging from low back pain (LBP) to neurological deficits. In addition, LBP is one of the most common musculoskeletal complaints in the world, and it has become a severe socioeconomic and health issue influencing of our society. Previous studies have exhibited that the mechanism of IDD includes a complicated biochemical process. One of the most important characteristics of IDD is the deficiency of proteoglycan (PG) content in intervertebral discs (IVDs). This process is closely related to the gene expression of ADAMTSs (activity of disintegrins and metalloproteinases with thrombospondin motifs), MMPs (matrix metalloproteinases) and TIMPs (tissue inhibitors of metalloproteinases) (1–7). As a strong inflammatory stimulation factor, previous researches have revealed that lipopolysaccharide (LPS) can lead to gene upregulation and the secretion of diverse proinflammatory cytokines and matrix-degrading enzymes, including ADAMTSs and MMPs in NP cells, thereout causing a decrease in PG volume and IDD (8,9). Moreover, proinflammatory cytokines such as tissue necrosis factor-α (TNF-α) also play important parts in IDD (10,11). Cell factors do not affect the IVD like ADAMTSs or MMPs do directly; instead of that, they expedite IDD by inducing the production of inflammatory factors by the intervertebral disc cells. As a TLR ligand, LPS can initiate TLR signaling in intervertebral disc cells, resulting in the up-regulated expression of proinflammatory cytokines and MMPs. Apart from MMPs and ADAMTSs, cytokines can also promote the chemokine ligand (CCL) expression in intervertebral disc cells. In terms of previous studies, CCLs can induce macrophage migration into the IVD, deteriorating the inflammatory stage and causing pain (12–17).
Traditional Chinese medicines (TCMs) are experience-based remedies derived from hundreds or thousands of years of clinical use in China. Most TCMs are extracted from one or more medicinal herbs. The existence of multiple bioactive ingredients makes many TCMs potential novel resources for the discovery of new anti-inflammatory and anti-matrix degradation drugs (18,19). Thus far, many naturally occurring phytochemicals were reported to possess anti-inflammatory and anti-matrix degradation effect and got considerable research attention.
Carthamins yellow (CY), which is the flavonoid compounds derived from safflower, has been extensively used as a natural food color additive in China. Safflower is known as the herb used in traditional medicines that promotes blood circulation to remove blood stasis and alleviate pain (20,21). Safflower injection has been used clinically for cerebrovascular disease, coronary heart disease, and angiitis in China (22,23). However, the effects and potential mechanisms of CY in inflammation and matrix degradation in the intervertebral disc desease has not yet been illuminated. Therefore, the purpose of our study was to evaluate the anti-inflammatory and anti-matrix degradation effect of CY in the IDD and investigate its potential mechanisms.
Materials and methods
Main reagents
CY and LPS was purchased from Sigma-Aldrich (St. Louis, MO, USA). CY was dissolved in DMSO at concentrations of 1 mol/l. And it was stored at −20°C. The additional proportion of DMSO in the culture medium was less than 0.05%. LPS was dissolved in PBS at concentrations of 1 mg/ml and was stored at 4°C. The P-ERK, ERK, P-JNK, JNK, P-P38, P38 and GAPDH antibody and secondary antibody were purchased from Cell Signaling Technology, Inc. (Beverly, MA, USA). Collagen II and aggrecan were purchased from Abcam (Cambridge, UK). The IHC secondary antibody was MaxVision TM HRP-Polymer kit from Maixin Bio (Fuzhou, China).
NP cell isolation and culture
The present study was conducted in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. NP cells were isolated from the lumbar spines of Sprague Dawley rats (6–8 weeks old, mixed male and female), using standard enzymatic digestion and culture in complete media (high-glucose DMEM with 10% FBS, 100 U/ml penicillin and 100 mg/ml streptomycin) up to passage 2–3 at 37°C in a humidifed atmosphere with 5% CO2.
Cell cytotoxicity assay
A cell counting kit-8 (CCK8) (Dojindo, Kumamoto, Japan) was used to test the viability of NP cells after CY treatment for 1 day according to previously reported methods (24). Approximately 5×103 NP cells were seeded on each film and transferred to 96-well plates. incubated with various concentrations of CY for 24 h. The conditioned culture medium was removed before CCK8 examination. Subsequently, 100 µl of DMEM and 10 µl of CCK8 solution were added to each well, followed by CCK8 incubation at 37°C for 2.5 h. The optical density (OD) at 450 nm was determined using a microplate reader (BioTek, Winooski, VT, USA). Cell viability was calculated as follows: Cell viability to control (%)=(ODdrug-treated group-ODblank)/(ODcontrol group-ODblank).
Apoptosis assay
Cell apoptosis was measured by flow cytometry using Annexin V/propidium iodide (PI) double-immunofluorescent staining according to previously reported methods (25). NP cells were cultured with 200 µM CY and/or 1 µg/ml LPS for 24 h. Then the cells were washed with cold PBS and resuspended with 1X Annexin-binding buffer. After that, all cells were stained with Annexin V-FITC and Propidium iodide according to the manufacturer's protocols. The apoptosis rate was measured by flow cytometry (FCM). Apoptotic events were indicated as a combination of fluorescein isothiocyanate (FITC)+/PI- (early apoptotic) and FITC+/PI+ (late apoptotic or dead) events. The final results are expressed as the percentage of early, late and total apoptotis.
Gene expression
NP cells were incubated with different concentrations of CY and 1 µg/ml LPS for 24 h. LPS could induce inflammation and matrix degradation in IVD. Total RNA was isolated by the AxyPrep™ Multisource Total RNA Miniprep kit (Axygen Biosciences, Union City, CA, USA). Then 1 µg RNA was converted into complementary DNA (cDNA) with PrimeScript™ RT reagent kit (Takara Bio, Inc., Otsu, Japan). Quantitative PCR was performed using an ABI 7500 Sequencing Detection System and SYBR® Premix Ex Taq™ (Takara Bio, Inc.). Cycling conditions were as follows: 40 cycles at 95°C for 5 sec and 60°C for 34 sec. The primers were used to amplify target genes are listed in Table I. The primers were designed and selected using blast in pubmed, and GAPDH was used as the internal control.
Table I.
Sequences of primers used in quantitative PCR.
| Gene | Primer sequences (5′-3′) |
|---|---|
| TNF-α | Forward: GGCTTTCGGAACTCACTGGA |
| Reverse: GGGAACAGTCTGGGAAGCTC | |
| Collagen II | Forward: GGCCAGGATGCCCGAAAATTA |
| Reverse: ACCCCTCTCTCCCTTGTCAC | |
| Aggrecan | Forward: CAGATGGCACCCTCCGATAC |
| Reverse: GACACACCTCGGAAGCAGAA | |
| ADAMT-4 | Reverse: ACCGATTACCAGCCTTTGGG |
| Forward: CCGACTCCGGATCTCCATTG | |
| ADAMT-5 | Forward: CCGAACGAGTTTACGGGGAT |
| Reverse: TGTGCGTCGCCTAGAACTAC | |
| MMP3 | Forward: TTTGGCCGTCTCTTCCATCC |
| Reverse: GCATCGATCTTCTGGACGGT | |
| GAPDH | Forward: TGCCACTCAGAAGACTGTGG |
| Reverse: TTCAGCTCTGGGATGACCTT |
Western blotting
For signaling pathway protein assay, the cells were treated with various concentrations of CY and/or 1 µg/ml LPS for 24 h. For aggrecan and collagen II protein assay, the cells were treated with various concentrations of CY and/or 1 µg/ml LPS for 5 or 8 days. Cell total proteins were extracted using NE-PER® Nuclear and Cytoplasmic Extraction Reagents according to the manufacturer's instructions. 20 µg protein (each sample) was loaded into gel, and separated by 7.5–12.5% SDS-PAGE, then transferred to 0.22-µm PVDF membranes (Millipore Corp., Billerica, MA, USA). The membranes were blocked with 5% fat-free milk at room temperature for 1 h and subsequently incubated with primary antibodies overnight at 4°C (1:1,000 dilution, Cell Signaling Technology). After three washes in TBST, the membranes were probed with the corresponding secondary antibody for 1 h at room temperature. The membranes were washed again in TBST, and the protein bands were visualized using an Odyssey Infrared Imaging System (LI-COR Biosciences, Lincoln, NE, USA). Positive immunoreactive bands were densitometrically quantified and normalized to GAPDH.
Immunohistochemistry staining
2×104/ml cells were seeded in 24-well plates, and these NP cells were cultured with diverse CY concentrations and/or 1 µg/ml LPS for 5 or 8 days. Cells were fixed with 4% paraformaldehyde before making cells slides. After fixation, NP cells were treated with 0.1% Triton X-100 for 15 min. Then the cells were blocked with 2% bovine serum albumin (Sigma-Aldrich) for 1 h. Then, cells slides were incubated with the corresponding antibody, including anti-collagen II and anti-aggrecan antibody (1:200 dilution; Abcam) overnight at 4°C. For immunohistochemistry, the secondary antibody was used for 15 min at room temprature. The DAB (Maixin Bio) solution was used as the chromogen. We used an inverted microscope microscopy (Olympus, Tokyo, Japan) to acquire the images. The integral optical density (IOD) of every photo was measured using the Image-Pro Plus 6.0 software (Media Cybernetics, Inc., Rockville, MD, USA).
Statistical analysis
The statistical package for the social sciences (SPSS) version 19.0 was used to analyze the data. The significance of differences between experimental groups and controls were assessed using the Student's t-test or one-way analysis of variance (ANOVA) as appropriate. The data are expressed as the mean ± SD. P<0.05 was considered to indicate a statistically significant difference.
Results
Cell viability of NP cells after CY treatment
To study the potential cytotoxicity of CY, we measured the cell viability of NP cells. After incubating with different concentrations of CY for 24 h, we used CCK-8 to assay the cell viability of NP cells. As shown in Fig. 1, CY did not inhibit proliferation of NP cells at concentration of 50, 100 and 200 µM.
Figure 1.
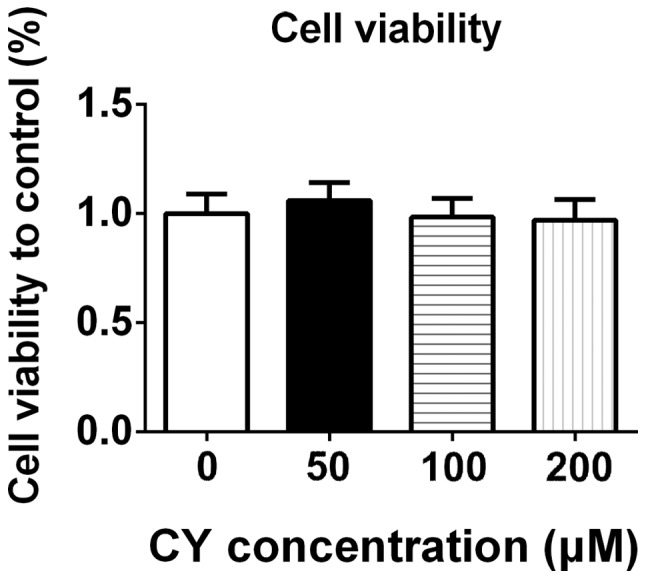
Cell viability assay of NP cells. 5×103/ml cells were seeded onto 96-well plates, and these cells were cultured with various concentrations of CY for 24 h after adherence. Then, we used CCK-8 to measure the cell viability of NP cells. CY had no effect in NP cells following 24 h treatment. Data are presented as the means ± SD. All data were obtained from at least three independent experiments.
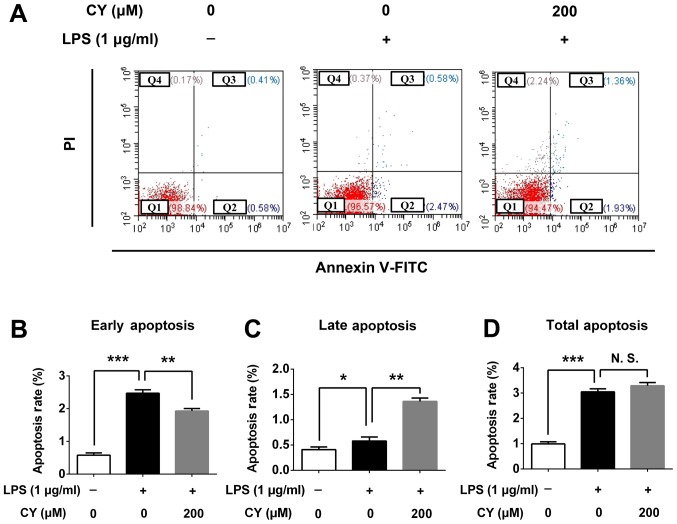
Apoptosis analysis of NP cells following CY treatment
To verify the cytotoxicity of CY, we examined the apoptosis rate of NP cells after treating with CY for 24 h. CY could decrease the early apoptosis rate at 200 µM with 1 µg/ml LPS (2.47% in 1 µg/ml LPS vs. 1.93% which were treated with CY of 200 µM and 1 µg/ml LPS, P<0.05), and CY could increase the late apoptosis rate at 200 µM with 1 µg/ml LPS (0.58% in 1 µg/ml LPS vs. 1.36% which were treated with CY of 200 µM and 1 µg/ml LPS, P<0.05), but the total apoptosis has no difference between two groups (Fig. 2A). And quantitative data of early, late and total apoptosis rate was consistant with this phenomenon (Fig. 2B-D).
Figure 2.
Apoptosis assay of NP cells following CY treatment. (A) After stimulation with or without 1 µg/ml LPS and 200 µM CY for 24 h, cells were stained with Annexin V-FITC and Propidium iodide and the apoptosis rate was measured via flow cytometry. (B-D) The early, late and total apoptosis rate was calculated and compared. The data are presented as the means ± SD. ***P<0.001; **P<0.01; *P<0.05. All data were obtained from at least three independent experiments.
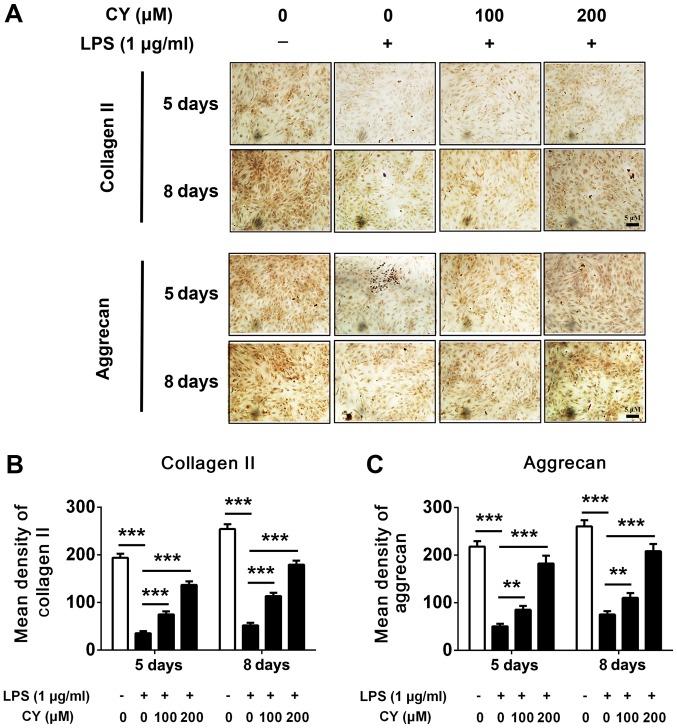
CY inhibited LPS induced matrix-degradation in NP cells
NP cells were incubated with 1 µg/ml LPS in the various concentration of CY (100 or 200 µM) for 5 or 8 days. After that, we detected extracellular matrix content by cell immunohistochemistry. Our results indicated that the expression of collagen II and aggrecan increased over time in NP cells, while LPS strikingly decreased the aggrecan and collagen II amount (Fig. 3A). Immunohistochemistry staining showed CY significantly increased the content of aggrecan and collagen II compared to the LPS groups (Fig. 3A). The quantification of IOD also indicated that the CY group gained more aggrecan and collagen II staining (Fig. 3B and C).
Figure 3.
Immunohistochemistry staining of NP cells after CY treatment. (A) 2×104/ml cells were seeded in a 24-well plates, and these cells were cultured with different concentrations of CY and/or 1 µg/ml LPS for 5 or 8 days, then cells were fixed with 4% paraformaldehyde and performed immunohistochemistry staining of collagen II and aggrecan. (B and C) The immunohistochemistry staining of collagen II and aggrecan were quantified by integrated optical density (IOD). The data are presented as the means ± SD. ***P<0.001, **P<0.01. All data were obtained from at least three independent experiments.
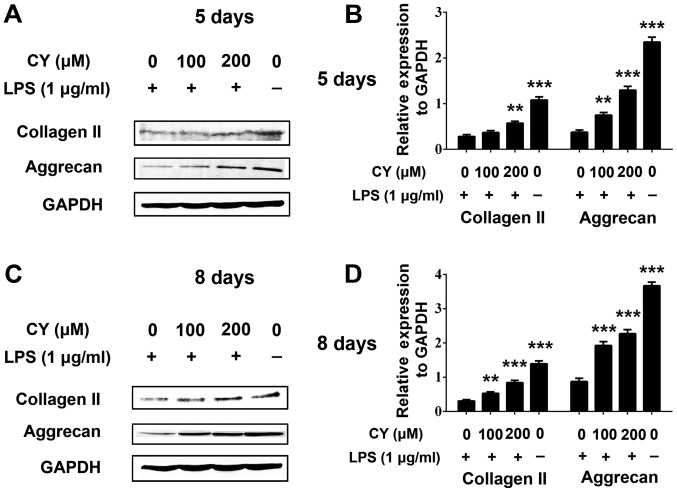
After incubated with LPS and various concentration of CY for 5 or 8 days, we also used western blotting to measure the collagen II and aggrecan protein content. The result was similar with immunohistochemistry staining. As shown in Fig. 4, LPS induced collagen II and aggrecan protein down-expression, and CY significantly attenuated the collagen II and aggrecan loss at day 5 and 8. This effect was more obvious at day 8 (Fig. 4).
Figure 4.
Matrix related protein expression of NP cells after CY treatment. Western blotting used to measure aggrecan and collagen II protein expression of NP cells. Cells were cultured with different concentrations of CY and/or 1 µg/ml LPS for 5 or 8 days, then total protein of cells were extracted and performed western blotting. (A and C) Expression of collagen II and aggrecan at 5 and 8 days. (B and D) Positive immunoreactive bands were densitometrically quantified and normalized to GAPDH. The data are presented as the means ± SD. ***P<0.001, **P<0.01. All data were obtained from at least three independent experiments.
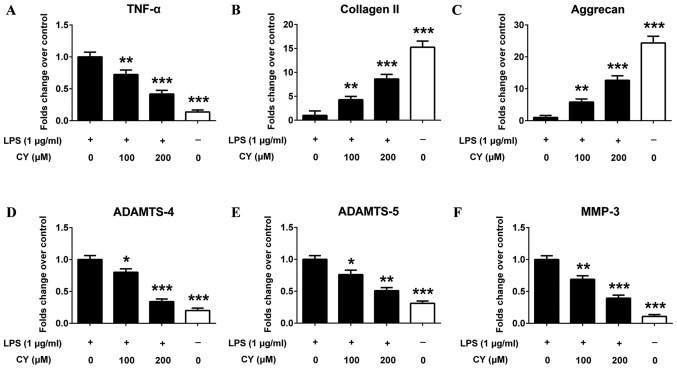
CY reversed LPS induced gene expression changes in NP cells
NP cells were stimulated with 1 µg/ml LPS and 0, 100 or 200 µM CY, followed by quantitative PCR assay. PCR results showed that LPS significantly up-regulated the gene expression of proinflammatory cytokines TNF-α (Fig. 5A). LPS also down-regulated the gene expression of collagen II and aggrecan in NP cells, which was reversed by CY (Fig. 5B and C). And CY also inhibited multiple matrix-degrading enzymes (MMP-3, ADAMTS-4 and ADAMTS-5) gene overexpression induced by LPS in NP cells (Fig. 5D-F).
Figure 5.
Gene expression changes in NP cells following CY treatment. (A-F) NP cells were treated with or without 1 µg/ml LPS and various concentrations of CY for 24 h. Then the gene expression of TNF-α, collagen II, aggrecan, ADAMTS-4, ADAMTS-5 and MMP-3 were measured by quantitative PCR. GAPDH was used as the internal control. The data are presented as the means ± SD. ***P<0.001, **P<0.01, *P<0.05. All data were obtained from at least three independent experiments.
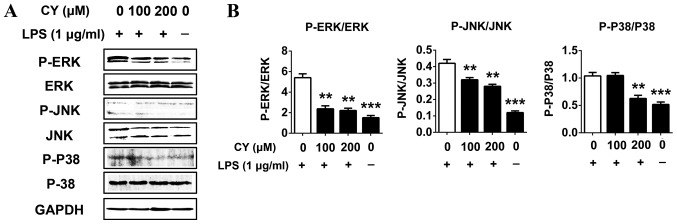
CY inhibited the LPS-induced activation of the MAPK pathway in NP cells
We measured the activation of the MAPKs pathway related proteins by western blotting to evaluate the potential mechanisms of effects of CY on LPS induced NP cells. Cells were pretreated with various concentrations of CY for 2 h, then treated with or without 1 µg/ml LPS for 30 min. The results showed that 1 µg/ml LPS significantly activated the MAPKs pathways by promoting JNK, ERK and P38 protein phosphorylation (Fig. 6). And CY could inhibit the phosphorylation of JNK, ERK and P38 in a dose dependent manner (Fig. 6). This result indicated the MAPKs pathway was involved while CY exerted anti-inflammatory effect in NP cells.
Figure 6.
Effect of CY on LPS induced activation of MAPK pathway in NP cells. (A) NP cells were pretreated with various concentrations of CY for 2 h, then treated with or without 1 µg/ml LPS for 30 min. The expression of MAPKs pathway proteins was measured by western blotting. (B) Positive immunoreactive bands were densitometrically quantified and the results were expressed as the ratio of P-ERK to ERK, P-JNK to JNK and P-P38 to P38. The data are presented as the means ± SD. ***P<0.001, **P<0.01. All data were obtained from at least three independent experiments.
Discussion
At present, CY has already been widely used as a bioactive natural products and food additive in China (26). However, there is no study focus on the potential therapeutic effect of CY in intervertebral disc degeneration. In our study, we tested the cytotoxicity of CY to NP cells by CCK8 and apoptosis assay firstly. The results showed that CY did not inhibit proliferation of NP cells at different concentration, and there is a statistically significant difference between different treatment in early and late apoptosis, but the apoptosis rate could be ignored as the apoptosis rate is too little in different treatment. As the total apoptosis rate has no difference between LPS and LPS with CY group, there is no cytotoxicity of CY to NP cells. Furthermore, our research showed that CY produced pharmacological anti-inflammatory reaction and anti-degeneration results in LPS-induced NP cells for the first time. And our study also evidenced that CY could block the LPS-induced activation of the MAPK pathway in NP cells.
The gene expression of ADAMTSs and MMPs has been a wide range of researches in the stage of IVD degeneration (27). According to many researches, MMP-3 are not expressed in normal human intervertebral discs but have up-regulated expression in degenerated human intervertebral discs. Besides, the protein expression of MMP-3 has a positive correlation with IVD histomorphological degenerative studies (28). The upregulated expression of ADAMTSs has also been detected in degenerative intervertebral discs. ADAMTS-4 and ADAMTS-5 have been revealed as the most important aggrecanases because of their strong abilties in cleaving aggrecan among the 20 various ADAMTSs (29). Inhibitors of ADAMTSs and MMPs have a therapeutic action on IDD in vitro and in vivo studies (30). Aggrecan and collagen II are the main elements of nucleus pulposus, and the decrease of collagen II content is highly correlated with IVD degeneration (31). Our research shows that CY can both prevent LPS-induced collagen II and aggrecan loss and induce their synthesis.
We also demonstrated that CY could inhibit LPS-induced inflammation of NP cells. Previous studies suggested that LPS markedly induced gene upregulation and the production of various proinflammatory cytokines in NP cells (32). TNF-α secreted from inflammatory cells and IVD cells triggers MMPs expression which ends up in vicious cycle of cell apoptosis and matrix degradation (33). The result of the current study demonstrated CY can down-regulate TNF-α expression. TNF-α blocker is now widely used in the treatment of inflammatory arthritis and in certain cases of IVD herniation (34). The MAPK pathways play important roles in the regulation of the inflammatory response (35). The effect of inhibiting p38 expression in NP cells was tested in previous study, the result indicated that inflammatory cytokines induced caveolin-1/β-catenin signalling in rat nucleus pulposus cell apoptosis through the p38 MAPK pathway (36). The role of the ERK pathway had also been investigated in human intervertebral disc, and exogenous and autocrine growth factors could stimulate human intervertebral disc cell proliferation via the ERK and Akt pathways (37). And another research showed that crocin exerts anti-inflammatory and anti-catabolic effects on rat intervertebral discs by suppressing the activation of JNK. And JNK is a critical MAPK pathway for intervertebral disc degeneration (15). Though MAPK pathway is related to NP cell death, CCK8 and apoptosis assay showed that there was no impact on NP cell proliferation and total apoptosis following CY treatment. That revealed that there may be other signaling influencing NP cell death. And in our study, MAPK pathway was activated after inflammatory stimulation, so MAPK pathway is more related to inflammatory. Our western blotting results showed that CY inhibited the activation of MAPK pathway in NP cells, thus exerting anti-inflammation effect. So the inhibitory effect of CY on LPS induced inflammation of NP cells was through suppressing MAPK pathway.
As the above, we are honored to report the role of CY in LPS-induced inflammatory and matrix degradation in the intervertebral disc. We found that CY could indirectly or directly affect the vitality of MAPK signaling and PG content of intervertebral discs. However, more investigations should conducted following this basal research. Firstly, the in-depth molecular mechanisms controlling the CY-mediated transformations to inflammatory- and PG-related signaling pathways should be better stated. Secondly, animal experients should be constructed to verify the therapeutic effect of CY in vivo. Finally, our results should be verified by patient treatment.
Taken together, our study reveals that CY could exhibit a strong anti-inflammatory and anti-degeneration effect by suppressing LPS-induced MAPK activation in NP cells. CY may be a potential new traditional Chinese medicine for curing IDD in the future. However, more and further studies are required to confirm this.
Acknowledgements
This study was supported by grants from Research project of Shanghai municipal health and Family Planning Commission (grant no. 201640304).
References
- 1.Li Y, Li K, Mao L, Han X, Zhang K, Zhao C, Zhao J. Cordycepin inhibits LPS-induced inflammatory and matrix degradation in the intervertebral disc. PeerJ. 2016;4:e1992. doi: 10.7717/peerj.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Y, Li K, Han X, Mao C, Zhang K, Zhao T, Zhao J. The imbalance between TIMP3 and matrix-degrading enzymes plays an important role in intervertebral disc degeneration. Biochem Biophys Res Commun. 2016;469:507–514. doi: 10.1016/j.bbrc.2015.12.020. [DOI] [PubMed] [Google Scholar]
- 3.Campbell RJ, Mobbs RJ, Phan K. Evidence update-association between CILP and degeneration of the intervertebral disc: A meta-analysis. J Spine Surg. 2016;2:242–243. doi: 10.21037/jss.2016.07.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ye S, Ju B, Wang H, Lee KB. Bone morphogenetic protein-2 provokes interleukin-18-induced human intervertebral disc degeneration. Bone Joint Res. 2016;5:412–418. doi: 10.1302/2046-3758.59.BJR-2016-0032.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Feng Y, Egan B, Wang J. Genetic factors in intervertebral disc degeneration. Genes Dis. 2016;3:178–185. doi: 10.1016/j.gendis.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teichtahl AJ, Urquhart DM, Wang Y, Wluka AE, O'Sullivan R, Jones G, Cicuttini FM. Lumbar disc degeneration is associated with modic change and high paraspinal fat content-a 3.0T magnetic resonance imaging study. BMC Musculoskelet Disord. 2016;17:439. doi: 10.1186/s12891-016-0934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine (Phila Pa 1976) 1995;20:11–19. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Liu MC, Chen WH, Wu LC, Hsu WC, Lo WC, Yeh SD, Wang MF, Zeng R, Deng WP. Establishment of a promising human nucleus pulposus cell line for intervertebral disc tissue engineering. Tissue Eng Part C Methods. 2014;20:1–10. doi: 10.1089/ten.tec.2013.0048. [DOI] [PubMed] [Google Scholar]
- 9.Kim JS, Ellman MB, Yan D, An HS, Kc R, Li X, Chen D, Xiao G, Cs-Szabo G, Hoskin DW, et al. Lactoferricin mediates anti-inflammatory and anti-catabolic effects via inhibition of IL-1 and LPS activity in the intervertebral disc. J Cell Physiol. 2013;228:1884–1896. doi: 10.1002/jcp.24350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang B, Wang D, Yan T, Yuan H. MiR-138-5p promotes TNF-α-induced apoptosis in human intervertebral disc degeneration by targeting SIRT1 through PTEN/PI3K/Akt signaling. Exp Cell Res. 2016;345:199–205. doi: 10.1016/j.yexcr.2016.05.011. [DOI] [PubMed] [Google Scholar]
- 11.Liu XG, Hou HW, Liu YL. Expression levels of IL-17 and TNF-α in degenerated lumbar intervertebral discs and their correlation. Exp Ther Med. 2016;11:2333–2340. doi: 10.3892/etm.2016.3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang W, Yu XH, Wang C, He WS, Zhang SJ, Yan YG, Zhang J, Xiang YX, Wang WJ. Interleukin-1β in intervertebral disk degeneration. Clin Chim Acta. 2015;450:262–272. doi: 10.1016/j.cca.2015.08.029. [DOI] [PubMed] [Google Scholar]
- 13.Hu B, Shi C, Xu C, Cao P, Tian Y, Zhang Y, Deng L, Chen H, Yuan W. Heme oxygenase-1 attenuates IL-1β induced alteration of anabolic and catabolic activities in intervertebral disc degeneration. Sci Rep. 2016;6:21190. doi: 10.1038/srep21190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang F, Jiang D. IL-1β/HMGB1 signalling promotes the inflammatory cytokines release via TLR signalling in human intervertebral disc cells. Biosci Rep. 2016;36(pii):e00379. doi: 10.1042/BSR20160118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li K, Li Y, Ma Z, Zhao J. Crocin exerts anti-inflammatory and anti-catabolic effects on rat intervertebral discs by suppressing the activation of JNK. Int J Mol Med. 2015;36:1291–1299. doi: 10.3892/ijmm.2015.2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y, Liu L, Wang S, Zhao Y, Liu Y, Li J, Nie L, Cheng L. Production of CCL20 on nucleus pulposus cells recruits IL-17-producing cells to degenerated IVD tissues in rat models. J Mol Histol. 2016;47:81–89. doi: 10.1007/s10735-015-9651-2. [DOI] [PubMed] [Google Scholar]
- 17.Karli P, Martlé V, Bossens K, Summerfield A, Doherr MG, Turner P, Vandevelde M, Forterre F, Henke D. Dominance of chemokine ligand 2 and matrix metalloproteinase-2 and −9 and suppression of pro-inflammatory cytokines in the epidural compartment after intervertebral disc extrusion in a canine model. Spine J. 2014;14:2976–2984. doi: 10.1016/j.spinee.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 18.Cheng CY, Lee YC. Anti-inflammatory effects of traditional Chinese medicines against ischemic injury in in vivo models of cerebral ischemia. Evid Based Complement Alternat Med. 2016;2016:5739434. doi: 10.1155/2016/5739434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu F, Yin L, Ji L, Yang F, Zhang G, Shi L, Xu L. Suppressive effect of Sanmiao formula on experimental gouty arthritis by inhibiting cartilage matrix degradation: An in vivo and in vitro study. Int Immunopharmacol. 2016;30:36–42. doi: 10.1016/j.intimp.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Wang CC, Choy CS, Liu YH, Cheah KP, Li JS, Wang JT, Yu WY, Lin CW, Cheng HW, Hu CM. Protective effect of dried safflower petal aqueous extract and its main constituent, carthamus yellow, against lipopolysaccharide-induced inflammation in RAW264.7 macrophages. J Sci Food Agric. 2011;91:218–225. doi: 10.1002/jsfa.4172. [DOI] [PubMed] [Google Scholar]
- 21.Kohno Y, Totsuka K, Ikoma S, Yoda K, Shibata M, Matsushima R, Tomita Y, Maeda Y, Kobayashi K. Photostability enhancement of anionic natural dye by intercalation into hydrotalcite. J Colloid Interface Sci. 2009;337:117–121. doi: 10.1016/j.jcis.2009.04.065. [DOI] [PubMed] [Google Scholar]
- 22.Fan S, Lin N, Shan G, Zuo P, Cui L. Safflower yellow for acute ischemic stroke: A systematic review of randomized controlled trials. Complement Ther Med. 2014;22:354–361. doi: 10.1016/j.ctim.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Zhou MX, Fu JH, Zhang Q, Wang JQ. Effect of hydroxy safflower yellow A on myocardial apoptosis after acute myocardial infarction in rats. Genet Mol Res. 2015;14:3133–3141. doi: 10.4238/2015.April.10.24. [DOI] [PubMed] [Google Scholar]
- 24.Han XG, Li Y, Mo HM, Li K, Lin D, Zhao CQ, Zhao J, Tang TT. TIMP3 regulates osteosarcoma cell migration, invasion, and chemotherapeutic resistances. Tumour Biol. 2016;37:8857–8867. doi: 10.1007/s13277-015-4757-4. [DOI] [PubMed] [Google Scholar]
- 25.Han XG, Du L, Qiao H, Tu B, Wang YG, Qin A, Dai KR, Fan QM, Tang TT. CXCR1 knockdown improves the sensitivity of osteosarcoma to cisplatin. Cancer Lett. 2015;369:405–415. doi: 10.1016/j.canlet.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 26.Li HX, Han SY, Wang XW, Ma X, Zhang K, Wang L, Ma ZZ, Tu PF. Effect of the carthamins yellow from Carthamus tinctorius L. on hemorheological disorders of blood stasis in rats. Food Chem Toxicol. 2009;47:1797–1802. doi: 10.1016/j.fct.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 27.Vo NV, Hartman RA, Yurube T, Jacobs LJ, Sowa GA, Kang JD. Expression and regulation of metalloproteinases and their inhibitors in intervertebral disc aging and degeneration. Spine J. 2013;13:331–341. doi: 10.1016/j.spinee.2012.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weiler C, Nerlich AG, Zipperer J, Bachmeier BE, Boos N. 2002 SSE award competition in basic science: Expression of major matrix metalloproteinases is associated with intervertebral disc degradation and resorption. Eur Spine J. 2002;11:308–320. doi: 10.1007/s00586-002-0472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gendron C, Kashiwagi M, Lim NH, Enghild JJ, Thøgersen IB, Hughes C, Caterson B, Nagase H. Proteolytic activities of human ADAMTS-5: Comparative studies with ADAMTS-4. J Biol Chem. 2007;282:18294–18306. doi: 10.1074/jbc.M701523200. [DOI] [PubMed] [Google Scholar]
- 30.Leckie SK, Bechara BP, Hartman RA, Sowa GA, Woods BI, Coelho JP, Witt WT, Dong QD, Bowman BW, Bell KM, et al. Injection of AAV2-BMP2 and AAV2-TIMP1 into the nucleus pulposus slows the course of intervertebral disc degeneration in an in vivo rabbit model. Spine J. 2012;12:7–20. doi: 10.1016/j.spinee.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Y, Li K, Hu Y, Xu B, Zhao J. Piperine mediates LPS induced inflammatory and catabolic effects in rat intervertebral disc. Int J Clin Exp Pathol. 2015;8:6203–6213. [PMC free article] [PubMed] [Google Scholar]
- 32.Iwata M, Ochi H, Asou Y, Haro H, Aikawa T, Harada Y, Nezu Y, Yogo T, Tagawa M, Hara Y. Variations in gene and protein expression in canine chondrodystrophic nucleus pulposus cells following long-term three-dimensional culture. PloS One. 2013;8:e63120. doi: 10.1371/journal.pone.0063120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kang YM, Hong SH, Yang JH, Oh JC, Park JO, Lee BH, Lee SY, Kim HS, Lee HM, Moon SH. Pamidronate down-regulates tumor necrosis factor-alpha induced matrix metalloproteinases expression in human intervertebral disc cells. J Bone Metab. 2016;23:165–173. doi: 10.11005/jbm.2016.23.3.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams LM, Lali F, Willetts K, Balague C, Godessart N, Brennan F, Feldmann M, Foxwell BM. Rac mediates TNF-induced cytokine production via modulation of NF-kappaB. Mol Immunol. 2008;45:2446–2454. doi: 10.1016/j.molimm.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 35.Goldring MB, Otero M, Plumb DA, Dragomir C, Favero M, El Hachem K, Hashimoto K, Roach HI, Olivotto E, Borzì RM, Marcu KB. Roles of inflammatory and anabolic cytokines in cartilage metabolism: Signals and multiple effectors converge upon MMP-13 regulation in osteoarthritis. Eur Cell Mater. 2011;21:202–220. doi: 10.22203/eCM.v021a16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J, Chen H, Cao P, Wu X, Zang F, Shi L, Liang L, Yuan W. Inflammatory cytokines induce caveolin-1/β-catenin signalling in rat nucleus pulposus cell apoptosis through the p38 MAPK pathway. Cell Prolif. 2016;49:362–372. doi: 10.1111/cpr.12254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pratsinis H, Constantinou V, Pavlakis K, Sapkas G, Kletsas D. Exogenous and autocrine growth factors stimulate human intervertebral disc cell proliferation via the ERK and Akt pathways. J Orthop Res. 2012;30:958–964. doi: 10.1002/jor.22017. [DOI] [PubMed] [Google Scholar]