Abstract
Background
Little attention has focused on gender differences in cardiac comorbidities and outcomes in patients undergoing orthotropic heart transplant.
Objective
The objective of this study was to investigate gender differences at baseline and during follow-up among heart transplant patients.
Methods
An observational cohort within the NEW HEART study was evaluated to determine gender differences in relation to age, coexisting cardiac comorbidities, and outcomes. Differences were assessed by t-test, Fisher’s exact test, and logistic regression analysis.
Results
Male transplant recipients (n = 238) were significantly older than female recipients (n = 92), with a greater percentage over 60 years of age (45% vs. 24%, p = 0.0006). Males were more likely to have hypertension (63% vs. 49%, p = 0.034), dyslipidemia (62% vs. 45%, p = 0.006), a history of smoking (52% vs. 35%, p = 0.009), and diabetes (42% vs. 21%, p = 0.0002). Analysis of endomyocardial biopsies obtained during the 1-year follow-up period demonstrated that women averaged more episodes of acute rejection than men (3.9 vs. 3.0, p = 0.009). While most episodes of rejection were mild, women were more likely than men to have episodes of moderate or severe rejection (14% vs. 5%, p = 0.012) and to be hospitalized for acute rejection (15% vs. 6%, p = 0.013). There were no significant differences in mortality.
Conclusions
Men were more likely than women to be older and to have diabetes, dyslipidemia, hypertension, and a history of smoking. Women were more likely to experience moderate or severe allograft rejection and to be hospitalized for acute rejection. Future investigation of the reasons for these gender differences is warranted and may improve clinical care of women undergoing cardiac transplantation.
Keywords: ECG monitoring, gender, heart transplant
Introduction
There are currently 2.5 million women with heart failure in the United States, and this number will continue to grow as women live longer with multiple chronic cardiovascular conditions that predispose them to the development of heart failure.1 Specifically, women tend to be older with a non-ischemic etiology for their heart failure, and women also tend to have more comorbidities and worse overall cardiac outcomes than men, regardless of age. Interestingly, although the lifetime risk of heart failure is approximately 20% for both women and men, more women with heart failure have a preserved ejection fraction (>45%) as compared to men.2 The current epidemic of heart failure has continued to increase, as have the number of candidates (predominantly male) actively listed for orthotopic heart transplant (OHT), whereas the number of available donors continues to be limited, highlighting the ever-widening supply–demand mismatch.3,4
Women undergo OHT less frequently than men, a trend that has persisted for decades, with less than a third of heart organs being allocated to women.3–5 The recent literature suggests a number of contributing factors for gender disparities in transplantation, including fewer women being listed for transplant, more women dying while waiting on the transplant list, less aggressive heart failure treatment in women, and increased sensitization in women, limiting the donor pool from which a match can be found.2–8 In fact, the current OHT allocation system in the United States is based primarily on illness severity and not on age and gender.8
A review of transplant data provided evidence to suggest that women may be treated less aggressively and often are not prescribed the same evidence-based heart failure medications as men, which may partially explain why females have increased mortality while waiting to be listed or receiving an OHT.8 Women continue to be underrepresented in clinical trials, and more heart failure-related deaths occur annually in women as compared to men.9,10 Researchers have also shown that gender differences exist in regards to acute myocardial infarction and heart failure symptom recognition among women, and reperfusion and preventive therapies remain underutilized in women, which may also account for their increased mortality.11–16 Yet, the fact remains that women are transplanted less frequently than men, making it critical for researchers to examine why such gender differences continue to exist. Since men and women who have already undergone an OHT should theoretically have similar cardiac illness profiles, examining clinical characteristics and outcomes in those who have undergone OHT may shed light on this continued gender disparity.
The purpose of this study is to investigate gender differences in clinical characteristics at the time of enrollment in the NEW HEART study and outcomes during follow-up among OHT recipients at three large transplant centers in the United States.
Methods
Setting and participants
The NEW HEART study (NINR NR012003) of home ECG monitoring was conducted at three large OHT centers in the United States between 2011 and 2015 (Columbia University Medical Center, University of California Los Angeles, and Cedars-Sinai). The primary aim of the study (currently under data analysis) was to determine whether ECG changes (QT/QTc interval changes) during the first 6 months post-OHT can predict acute allograft rejection. A total of 345 participants were enrolled at three cardiac transplant centers. At the time of this analysis, 330 had complete clinical information necessary for calculating the Charlson comorbidity index (CCI) and are included in the current study (Columbia University Medical Center, n = 132; University of California Los Angeles, n = 128; Cedars-Sinai, n = 70). The remaining 15 participants lacked complete clinical information (data were still being collected and/or validated via medical record review) at the time of this analysis, and so were excluded. Those who were excluded did not differ with respect to age, gender, or race/ethnicity.
After informed consent was obtained, demographic and clinical data were collected by self-report and from medical records. During follow-up, the results of endomyocardial biopsies were recorded using the International Society of Heart and Lung Transplantation (ISHLT) standards for acute rejection; hospitalizations and deaths were also recorded. Institutional Review Board approval was obtained from all three participating institutions.
Details of the protocol used for the NEW HEART study have been published previously.17 Inclusion criteria were:1) ≥18 years of age; 2) having undergone a heart transplant surgery within the past 6 weeks; 3) not enrolled in other research studies that conflict with our study; and 4) clinically stable at time of enrollment. Exclusion criterion for enrollment in the NEW HEART study included those who were unable or unwilling to record and transmit a daily ECG recording for 6 months.
Study design
In order to investigate gender differences in baseline clinical characteristics and comorbidities among OHT recipients, an observational design was utilized with medical record review of cardiac comorbidities present at the time of enrollment in the NEW HEART study. Transplants were performed for end-stage heart failure and patients were followed post-transplant by an interdisciplinary team (nurses, nurse practitioners, cardiologists, social workers, psychiatrists, etc.). The baseline data that were collected included: age, gender, race, heart failure etiology, cardiac risk factors, and comorbidities. Patients were followed for a period of 1 year following OHT in order to assess the frequency of acute rejection on endomyocardial biopsies, hospitalizations (overall and for acute rejection), and all-cause mortality.
Charlson comorbidity index
The CCI is used as a risk stratification measure of patients with end-stage congestive heart failure in order to guide the transplant candidate selection process; the measure is used to predict mortality over 10 years and assigns a score of 1, 2, 3, or 6 to each comorbid condition, which are then summed to generate a total score ranging from 0 to 37.18 The CCI has been shown to be a valid and reliable predictor of mortality; a higher CCI score is associated with a greater predicted mortality in previous cardiovascular clinical trials.19
An age-adjusted CCI was calculated by adding 1 point per decade for patients aged 40 years or greater (adjustment for 40–49 years of age = 1 point, 50–59 years of age = 2 points, 60–69 years of age = 3 points, etc.).18 We expanded upon the cardiac measures captured on CCI (myocardial infarction, congestive heart failure, cerebrovascular disease, and diabetes) and included additional known cardiovascular risk factors (hypertension, hyperlipidemia, smoking, age, and gender). Data were collected via medical record review and were independently verified for accuracy and consistency by the Principal Investigator (PI) at each site.
Endomyocardial biopsies
Biopsies were performed weekly for the first 3 months following OHT and every other week for months 3–6. After 6 months, biopsies were performed monthly. Rejection on endomyocardial biopsies was graded using the ISHLT criteria. Mild rejection consisted of interstitial and/or perivascular infiltrate with no more than a single focus of myocyte damage. The criteria for moderate rejection was two or more foci of infiltrate and accompanying myocyte damage. Severe rejection was defined as biopsies with diffuse infiltrate and multifocal myocyte damage with or without edema, hemorrhage, or vasculitis.
Statistical analyses
Differences between men and women with regards to their underlying clinical characteristics and adverse outcomes were assessed by t-test for continuous variables or Fisher’s exact test for categorical variables. The non-parametric rank-sum test was used to test for differences in the CCI, the number of episodes of allograft rejection, and the number of hospitalizations. Multivariable analyses adjusting for the effects of age and race were performed using logistic regression. SAS 9.4 (SAS Institute, Cary, NC) was used for all analyses, with a p-value < 0.05 being considered to be statistically significant.
Results
The demographic and baseline clinical characteristics of the study population are presented in Table 1. Males comprised 72% of the study population; there were no significant differences among centers with regards to the proportion of male participants. At enrollment, the average age of study participants was 54 years (range 21–75 years). Male OHT recipients were significantly older than female recipients, with a greater percentage being over the age of 60 years (45% vs. 24%, p = 0.0006, respectively). The ethnic and racial composition of the cohort were 49% non-Hispanic whites, 18% non-Hispanic blacks, 20% Hispanics, 12% Asians, and 1% other. Race/ethnicity did not differ significantly by gender. Ischemic cardiomyopathy was more common among men than women (26% vs. 12%, respectively, p = 0.006). At the time of transplant, 32% had a ventricular assist device (VAD) implanted and 39% had an implantable cardioverter defibrillator. These percentages did not differ significantly by gender.
Table 1.
Clinical characteristics of the study population.
| Variable | Overall (n = 330) | Males (n = 238) | Females (n = 92) | p-value |
|---|---|---|---|---|
| Age (mean ± SD, years) | 54 ± 13 | 56 ± 11 | 50 ± 14 | <0.0001 |
| n/total (%) | n/total (%) | n/total (%) | ||
| Diabetes | 120/330 (36%) | 101/238 (42%) | 19/92 (21%) | 0.0002 |
| Hypertension | 193/329 (59%) | 148/237 (63%) | 45/92 (49%) | 0.034 |
| Dyslipidemia | 188/330 (57%) | 147/238 (62%) | 41/92 (45%) | 0.006 |
| History of smoking | 148/315 (47%) | 116/224 (52%) | 32/91 (35%) | 0.009 |
| Dilated cardiomyopathy | 172/316 (54%) | 124/230 (54%) | 48/86 (56%) | 0.80 |
| Ischemic cardiomyopathy | 70/316 (22%) | 60/230 (26%) | 10/86 (12%) | 0.006 |
| Implantable Cardioverter Defibrillator (ICD) | 130/330 (39%) | 86/238 (36%) | 44/92 (48%) | 0.06 |
| Ventricular Assist Device (VAD) | 107/330 (32%) | 84/238 (35%) | 23/92 (25%) | 0.09 |
Baseline cardiovascular risk factors and comorbidities
Cardiovascular risk factors were common within the cohort. Hypertension was most prevalent (59%), followed by dyslipidemia (57%), a history of smoking (47%), and diabetes (36%). These risk factors differed by gender, with males more likely to have hypertension (63% vs. 49%, p = 0.034), dyslipidemia (62% vs. 45%, p = 0.006), a history of smoking (52% vs. 35%, p = 0.009), and diabetes (42% vs. 21%, p = 0.0002). (Table 1).
In multivariable logistic regression analyses of cardiovascular risk factors that included age, race, and gender as independent variables, the effect of male gender remained significant for diabetes (odds ratio (OR) = 2.85, 95% confidence interval [CI) = 1.57–5.17, p= 0.0006), dyslipidemia (OR = 1.72, 95% CI = 1.02–2.90, p = 0.043), and a history of smoking (OR = 1.80, 95% CI = 1.07–3.05, p= 0.028) (Tables 2–5), indicating that males were more likely than females to have these cardiovascular risk factors after accounting for the potential effects of age and race.
Table 2.
Univariate and multivariate logistic regression results for diabetes.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | 95% confidence limits | p-value | Odds ratio | 95% confidence limits | p-value | |
| Age, per decade | 1.27 | 1.05, 1.54 | 0.013 | 1.26 | 1.03, 1.54 | 0.029 |
| Male gender | 2.83 | 1.61, 4.99 | 0.0003 | 2.85 | 1.57, 5.17 | 0.0006 |
| Race (white is reference) | ||||||
| Black | 2.12 | 1.19, 3.80 | 0.011 | 2.79 | 1.50, 5.21 | 0.0012 |
| Asian/other | 1.14 | 0.57, 2.27 | 0.71 | 1.12 | 0.55, 2.28 | 0.76 |
Table 5.
Univariate and multivariate logistic regression results for history of smoking.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | 95% confidence limits | p-value | Odds ratio | 95% confidence limits | p-value | |
| Age, per decade | 1.41 | 1.17, 1.70 | 0.003 | 1.37 | 1.13, 1.67 | 0.0014 |
| Male gender | 1.98 | 1.20, 3.28 | 0.008 | 1.80 | 1.07, 3.05 | 0.028 |
| Race (white is reference) | ||||||
| Black | 1.04 | 0.58, 1.85 | 0.90 | 1.26 | 0.69, 2.31 | 0.45 |
| Asian/other | 0.48 | 0.24, 0.98 | 0.044 | 0.46 | 0.22, 0.96 | 0.038 |
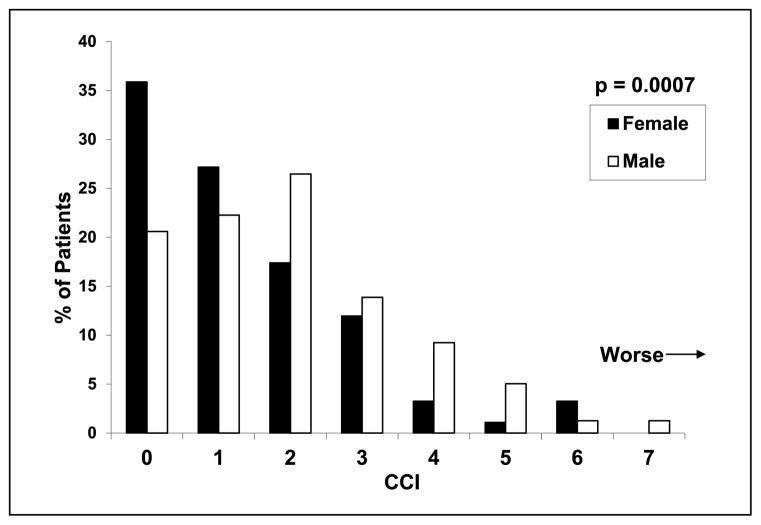
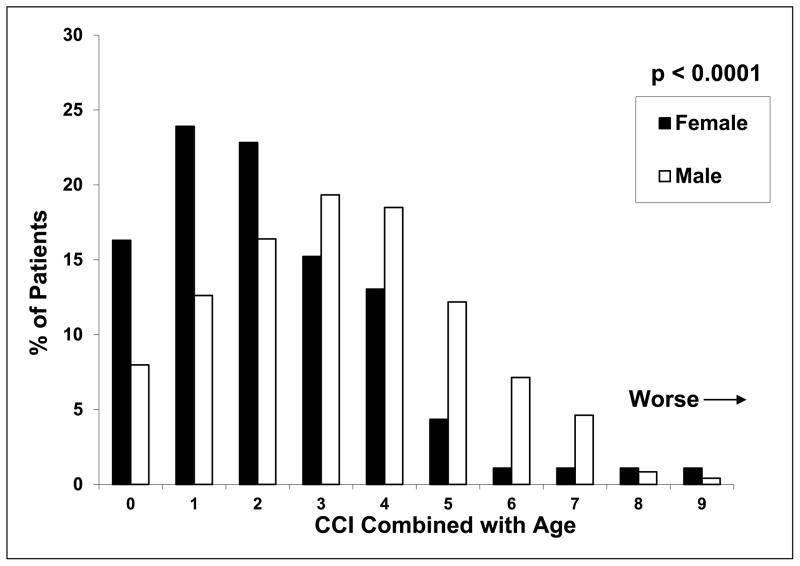
CCI scores were significantly higher in men (p = 0.0007; Figure 1), with 57% of men having a CCI score of 2 or greater versus 37% of women. When the effect of age was included, CCI scores remained significantly higher among men (p < 0.0001; Figure 2); 63% of men had a score of 3 or greater versus 37% of women.
Figure 1.
Charlson comorbidity index (CCI) scores by gender.
Figure 2.
Charlson comorbidity index (CCI) scores combined with age by gender.
Adverse outcomes during follow-up
During the 1-year follow-up period, 266 study participants (81%) had at least one endomyocardial biopsy exhibiting acute allograft rejection, with an average of 3.2 rejections per patient. Despite the large number of abnormal biopsies, most patients had allograft rejection that was classified as mild. Only 23 patients had biopsies showing moderate rejection, while three patients had biopsies showing severe rejection. The overall frequency of having any instance of allograft rejection did not differ significantly by gender (women 87% vs. men 79%). However, women had more episodes of rejection on average than did men (3.9 vs. 3.0, p = 0.009). In addition, women were more likely than men to have episodes of moderate or severe rejection (14% vs. 5%, respectively, p = 0.012). By multivariable logistic regression analysis with age, race, and gender as independent variables, women had increased odds of having episodes of moderate or severe rejection (OR = 2.62, 95% CI = 1.13–6.07, p = 0.025).
The frequency of hospitalizations also differed significantly by gender, with 59% of women and 46% of men being hospitalized at least once during the follow-up period (p = 0.027). The average number of hospitalizations was also greater for women than for men (1.3 vs. 0.9, p = 0.016). Women were hospitalized for acute rejection more frequently than men (15% vs. 6%, p = 0.013) and had a greater average number of hospitalizations for acute rejection (0.22 vs. 0.08, p = 0.006). By multivariable logistic regression analysis, women had increased odds of being hospitalized for acute rejection (OR = 2.35, 95% CI = 1.04–5.28, p = 0.04). Mortality did not differ significantly by gender (women 2% vs. men 5%).
Discussion
Those who received an OHT in the NEW HEART study were predominantly older men (>60 years of age) with multiple chronic underlying cardiovascular risk factors (hypertension, dyslipidemia, diabetes, and smoking). Overall, fewer older women underwent OHT as compared to men at our centers. In fact, the women in our study were younger and were less likely to have ischemic cardiomyopathy as compared to males, as documented in their medical records at the time of OHT. Diabetes, dyslipidemia, and a history of smoking were also observed more frequently in men than in women.
While these results may not be surprising, the findings may be explained by the fact that the prevalence of heart failure is also lower in women in their early years, but by 50 years of age, heart failure prevalence appears to equalize.1,20 Therefore, women may not experience severe heart failure until much later in life, at which point, because of their initial presenting age, they may not be eligible to be listed as candidates for a heart transplant. This may be a factor in why fewer women underwent an OHT at our centers.
Age is a significant variable that may impact the gender-based disparity seen at the time of OHT. Research from the American Heart Association has found that men are younger when they experience their first heart attack, with an average age of 64.7 years as compared to 72.2 years for women.1 Thus, it is likely that older males living with multiple chronic cardiovascular conditions may be under the care of a cardiologist because of their cardiovascular risk factors and thus are evaluated and listed sooner for a OHT as compared to women. The CCI is used as a risk stratification measure of patients with end-stage congestive heart failure and multiple coexisting risk factors in order to guide the transplant candidate selection process.18 Our results showed that 63% of men in the NEW HEART study had a CCI score of 3 or greater versus 37% of women.
However, research has shown that 90% of women have one or more risk factor(s) for developing heart disease, and since 1984, more women than men have died each year from heart disease, highlighting the continued gender difference in survival and the need for the improved recognition and treatment of cardiac risk factors in women. (https://www.goredforwomen.org) Thus, the increased mortality of women on the waiting list is another plausible reason that might explain why fewer women than men underwent an OHT in our study.
Researchers have demonstrated inequalities with clinical care, and determined that women had fewer left ventricular assist devices (LVADs) placed prior to OHT.21 LVADs are an important bridging therapy that maintain cardiac function and viability and improve survival while awaiting a heart transplant. It is possible that reduced use of these adjunctive therapies may result in increased mortality during the pre-transplant waiting period for women. However, the precise reason for this difference is unclear.21 One potential hypothesis is that the difference in body sizes between men and women may have resulted in less aggressive mechanical therapies, such as a VAD, to be placed in the past.21 Since smaller mechanical assist devices that are suitable for implantation in smaller patients have only recently become available and the percentage of women in recent LVAD trials of the much smaller continuous flow pumps has increased from 8% to 25%, we may see this gender difference decrease in the years ahead.21 In the NEW HEART study, we found no significant difference in the percentage of women versus men receiving VADs prior to undergoing their OHT. This may be due to the fact that smaller mechanical devices were commercially available for women during the enrollment period of our study.
Sensitized patients and other high-risk subgroups may have a disparity in heart allocation, accounting for some of the observed gender differences.22 Sensitization is the process by which antibodies are formed against human leukocyte antigens; this can result from a prior pregnancy or exposure to blood products22 and increases the risk of post-transplant rejection.23 Thus, female patients who are highly sensitized may remain on the United Network for Organ Sharing (UNOS) list for a longer period of time due to a smaller donor pool for which they are compatible. However, in Canada, sensitization has been recognized as a significant contributor to patient outcomes, especially in women.24 Sensitized patients have one of the highest priority categories on the heart transplant waiting list.24 One future approach might be providing sensitized women in the United States with a higher priority category on the cardiac waiting list, given the even smaller donor pool from which an eligible match would be available. While our study was not designed to evaluate this variable, the increased prevalence of moderate and severe rejection among women highlights sensitization as an area that needs further investigation, having the potential to impact future clinical care.
Moreover, recent data from the publicly available Scientific Registry of Transplant Recipients (SRTR) and the UNOS databases confirm previous observations that the majority of OHT recipients are older males, similarly to our findings, and that women in the United States have a higher mortality rate than men while awaiting an OHT.3 A recent review of the SRTR database from 2000 to 2009 found greater waiting list mortality for female patients who were status 1A as compared to men.4 The UNOS donor heart allocation system may favor status 1A men over women as heart transplant recipients, with an unclear explanation for this difference.8 Other researchers have also raised the question of whether the United States donor heart allocation system may favor men over women,6,8,23 a view that is supported by the results seen across our three transplant centers in the NEW HEART study. Although the UNOS donor heart allocation policy has undergone revisions (in 1999 and 2006), gender differences still exist, with an unclear explanation.7 The development of risk prediction scores/models has started to be reported in the literature, and the emergence of a scoring system for identifying the specific variables associated with the greatest mortality may be seen in the future.25,26
Other researchers have demonstrated that survival and morality rates do not differ between OHT patients with ischemic cardiomyopathy as compared to those with a dilated cardiomyopathy.27 Thus, even if the underlying severity and etiology of the heart failure differs by gender, as seen in our findings, the question remains as to why more men are transplanted than women.
Conclusions
Gender differences exist in heart transplant patients enrolled in the NEW HEART study. Men undergoing OHT were generally older and had more chronic cardiovascular conditions, while women were more likely to experience moderate or severe allograft rejection and to be hospitalized for acute rejection. Our findings suggest the need for multi-center prospective clinical trials that will examine heart failure cohorts before and after an OHT in order to investigate the reasons for these continued gender differences.
Limitations
This was an observational sub-study of the larger ongoing NEW HEART study. Other factors such as symptoms, social support, mental health status, and medication use may have influenced the findings. Another limitation of this study design was the unavailability of data regarding the duration of heart failure, donor pool information, and the duration of mechanical support prior to cardiac heart transplantation.
Future directions
The need for prospective cohort and registry studies beyond the UNOS is evident. This will allow for gender-specific data (quantitative and qualitative variables related to gender) to be collected and shared between transplantation centers in the United States, as well as internationally.
While the ISHLT has called for more interventional studies in heart transplant recipients, there is a lack of non-interventional studies examining psychological outcomes.28 It also remains to be determined whether psychological gender differences exist among heart transplant recipients and what specific psychosocial interventions may improve outcomes in post-heart transplant recipients.
Future policy recommendations should include the creation of an international task force of experts (i.e., consisting of nurses, physicians, social workers, transplant recipients, etc.) that is focused on gender in order to allow for gender-specific targeted approaches and dialogues to continue between experienced researchers, clinicians, and patients and families, which may identify new or additional underlying reasons that are responsible for existing gender differences. In addition, gender should be carefully examined in ongoing cardiovascular trials and incorporated into clinical risk prediction models.
Taken together, these data suggest multiple areas for future investigation, such as heart failure evaluation and treatment in women, donor matching, and illness severity of recipients, which may help unmask additional reasons for these existing gender differences and provide guidance towards actionable approaches for improving future clinical cardiac care and cardiac transplantation in women.
Table 3.
Univariate and multivariate logistic regression results for hypertension.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | 95% confidence limits | p-value | Odds ratio | 95% confidence limits | p-value | |
| Age, per decade | 1.60 | 1.32, 1.93 | <0.0001 | 1.63 | 1.33, 1.99 | <0.0001 |
| Male gender | 1.74 | 1.07, 2.82 | 0.026 | 1.46 | 0.86, 2.46 | 0.16 |
| Race (white is reference) | ||||||
| Black | 1.78 | 0.96, 3.28 | 0.07 | 2.42 | 1.26, 4.66 | 0.0079 |
| Asian/other | 1.04 | 0.54, 2.03 | 0.90 | 1.10 | 0.55, 2.22 | 0.79 |
Table 4.
Univariate and multivariate logistic regression results for dyslipidemia.
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Odds ratio | 95% confidence limits | p-value | Odds ratio | 95% confidence limits | p-value | |
| Age, per decade | 1.65 | 1.36, 1.99 | <0.0001 | 1.64 | 1.34, 2.01 | <0.0001 |
| Male gender | 2.01 | 1.23, 3.27 | 0.0050 | 1.72 | 1.02, 2.90 | 0.043 |
| Race (white is reference) | ||||||
| Black | 1.38 | 0.76, 2.50 | 0.29 | 1.89 | 1.00, 3.57 | 0.051 |
| Asian/other | 0.69 | 0.36, 1.34 | 0.27 | 0.69 | 0.34, 1.39 | 0.30 |
Implications for practice.
Fewer women than men received a cardiac transplant.
Women who received a cardiac transplant were younger.
Men were older with more cardiovascular risk factors.
More men received an implantable cardioverter defibrillator (ICD) and/or a ventricular assist device prior to transplant.
Acknowledgments
Funding
This work is supported by a grant (R01NR012003) from the National Institute of Health, National Institute of Nursing Research.
Footnotes
Conflict of interest
The authors declare that there are no conflicts of interest.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics – 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Kenchaiah S, Vasan RS. Heart failure in women: insights from the Framingham Heart study. Cardiovasc Drugs Ther. 2015;8(4):377–390. doi: 10.1007/s10557-015-6599-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.OPTN/SRTR 2011 annual data report: heart. US Department of Health and Human Services; Available at: http://srtr.transplant.hrsa.gov/annual_reports/2011/pdf/2011_SRTR_ADR.pdf. [Google Scholar]
- 4.Scientific Registry of Transplant Recipients. Heart: candidates: gender 2000–2009. Available at: http://srtr.transplant.hrsa.gov/annual_reports/2010/iHR_Candidates_gender.htm?o=5&g=1&c=1.
- 5.Frankenstein L, Clark AL, Ribeiro JP. Influence of sex on treatment and outcome in chronic heart failure. Cardiovasc Ther. 2012;30(3):182–192. doi: 10.1111/j.1755-5922.2010.00253.x. [DOI] [PubMed] [Google Scholar]
- 6.Joseph SM. Closing the sex gap in advanced heart failure: reality or illusion? J Card Fail. 2015;21(7):561–563. doi: 10.1016/j.cardfail.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 7.OPTN Policy 3.7. Available at: http://optn.transplant.hrsa.gov/PoliciesandBylaws2/policies/pdfs/policy_9.pdf.
- 8.Hsich EM, Starling RC, Blackstone EH, et al. Does the UNOS heart transplant allocation system favor men over women? JACC Heart Fail. 2014;2(4):347–355. doi: 10.1016/j.jchf.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 9.Melloni C, Berger JS, Wang TY, et al. Representation of women in randomized clinical trials of cardiovascular disease prevention. Circ Cardiovasc Qual Outcomes. 2010;3(2):135–142. doi: 10.1161/CIRCOUTCOMES.110.868307. [DOI] [PubMed] [Google Scholar]
- 10.Maas AH, van der Schouw YT, Regitz-Zagrosek V, et al. Red alert for women’s heart: the urgent need for more research and knowledge on cardiovascular disease in women: proceedings of the workshop held in Brussels on gender differences in cardiovascular disease. Eur Heart J. 2011;32(11):1362–1368. doi: 10.1093/eurheartj/ehr048. [DOI] [PubMed] [Google Scholar]
- 11.Rasmusson K, Brunisholz K, Budge D, et al. Peripartum cardiomyopathy: post-transplant outcomes from the United Network for Organ Sharing Database. J Heart Lung Transplant. 2012;31(2):180–186. doi: 10.1016/j.healun.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 12.Birks EJ, McGee EC, Jr, Aaronson KD, et al. An examination of survival by sex and race in the HeartWare Ventricular Assist Device for the Treatment of Advanced Heart Failure (ADVANCE) Bridge to Transplant (BTT) and Continued Access Protocol trials. J Heart Lung Transplant. 2015;34(6):815–824. doi: 10.1016/j.healun.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Kirklin JK, Naftel DC, Pagani FD, et al. Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant. 2014;33(6):555–564. doi: 10.1016/j.healun.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 14.D’Onofrio G, Safdar B, Lichtman JH, et al. Sex differences in reperfusion in young patients with ST-segment-elevation myocardial infarction: results from the VIRGO study. Circulation. 2015;131(15):1324–1332. doi: 10.1161/CIRCULATIONAHA.114.012293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wenger NK. Are we there yet? Closing the gender gap in coronary heart disease recognition, management and outcomes. Expert Rev Cardiovasc Ther. 2013;11(11):1447–1450. doi: 10.1586/14779072.2013.845526. [DOI] [PubMed] [Google Scholar]
- 16.Lichtman JH, Leifheit-Limson EC, Watanabe E, et al. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2015;8:S31–S38. doi: 10.1161/CIRCOUTCOMES.114.001612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doering LV, Hickey K, Pickham D, et al. Remote noninvasive allograft rejection monitoring for heart transplant recipients: study protocol for the novel evaluation with home electrocardiogram and remote transmission (NEW HEART) study. BMC Cardiovasc Disord. 2012;12:14. doi: 10.1186/1471-2261-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Iorio B, Cillo N, Cirillo M, et al. Charlson comorbidity index is a predictor of outcomes in incident hemodialysis patients and correlates with phase angle and hospitalization. Int J Artif Organs. 2004;27:330–336. doi: 10.1177/039139880402700409. [DOI] [PubMed] [Google Scholar]
- 19.De Groot V, Beckerman H, Lankhorst GJ, et al. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol. 2003;56(3):221–229. doi: 10.1016/s0895-4356(02)00585-1. [DOI] [PubMed] [Google Scholar]
- 20.Zhang Y. Cardiovascular diseases in American women. Nutr Metab Cardiovasc Dis. 2010;20(6):386–393. doi: 10.1016/j.numecd.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller LW, Guglin M. Patient selection for ventricular assist devices: a moving target. J Am Coll Cardiol. 2013;61(12):1209–1221. doi: 10.1016/j.jacc.2012.08.1029. [DOI] [PubMed] [Google Scholar]
- 22.Kobashigawa JA, Patel JK, Kittleson MM, et al. The long-term outcome of treated sensitized patients who undergo heart transplantation. Clin Transplant. 2011;25(1):E61–E67. doi: 10.1111/j.1399-0012.2010.01334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kobashigawa JA. U.S. donor heart allocation bias for men over women?: A closer look. JACC Heart Fail. 2014;2(4):356–357. doi: 10.1016/j.jchf.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Haddad H, Isaac D, Legare JF, et al. Canadian Cardiovascular Society Consensus Conference update on cardiac transplantation: executive summary. Can J Cardiology. 2009;25(4):197–205. doi: 10.1016/s0828-282x(09)70061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sartipy U, Goda A, Mancini DM, et al. Assessment of a University of California, Los Angeles 4-variable risk score for advanced heart failure. J Am Heart Assoc. 2014;3(3):e000998. doi: 10.1161/JAHA.114.000998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moons KG, Kengne AP, Grobbee DE, et al. Risk prediction models: II. External validation, model updating, and impact assessment. Heart. 2012;98(9):691–698. doi: 10.1136/heartjnl-2011-301247. [DOI] [PubMed] [Google Scholar]
- 27.Gungor H, Oguz E, Ayik MF, et al. Comparison of heart transplantation patients with ischemic and idiopathic dilated cardiomyopathy. Transplant Proc. 2011;43(10):3847–3850. doi: 10.1016/j.transproceed.2011.09.073. [DOI] [PubMed] [Google Scholar]
- 28.Conway A, Schadewaldt V, Clark R, et al. The effectiveness of non-pharmacological interventions in improving psychological outcomes for heart transplant recipients: a systematic review. Eur J Cardiovasc Nurs. 2014;13(2):108–115. doi: 10.1177/1474515113519519. [DOI] [PubMed] [Google Scholar]