Abstract
The proportion of tuberculosis (TB) patients tested for the human immunodeficiency virus (HIV) in the state of Ra-jasthan, India, is limited by the availability of HIV testing facilities. Rajasthan implemented a policy of initiating TB-HIV diagnosis at all health institutions in July 2013. The number of TB diagnostic facilities increased from 33 to 63 in Banswara District and from 22 to 68 in Jhunjhunu District, while the number of HIV testing facilities in these districts increased from 1 to 53 and from 10 to 81, respectively, after the policy implementation. The proportion of TB patients tested for HIV increased by respectively 27% and 19%.
Keywords: tuberculosis, HIV, testing, India, underdiagnosis
Abstract
La proportion de patients tuberculeux (TB) testés pour le virus de l'immunodéficience humaine (VIH) dans l'état du Rajasthan, Inde, est limitée par la disponibilité de lieux de tests du VIH. Le Rajasthan a mis en œuvre une politique d'initiation du diagnostic TB dans toutes les structures de santé en juillet 2013. Le nombre de lieux de diagnostic TB a augmenté de 33 à 63 dans le district de Banswara et de 22 à 68 dans le district de Jhunjhunu, tandis que le nombre de lieux de test du VIH a augmenté de 1 à 53 et de 10 à 81, respectivement, après la mise en œuvre de cette politique. La proportion de patients TB testés pour le VIH a augmenté de 27% et 19%, respectivement, dans les deux districts.
Abstract
La proporción de pacientes con tuberculosis (TB) que cuentan con la prueba del virus de la inmunodeficiencia humana (VIH) en el estado de Rajastán en la India se ve limitada por la escasez de establecimientos que la practican. En julio del 2013 se introdujo en Rajastán una política de iniciar el diagnóstico de la TB y el VIH en todos los establecimientos de atención de salud. Después de la introducción de la política, el número de centros de diagnóstico de la TB en el distrito de Banswara aumentó de 33 a 63 y en el distrito Jhunjhunu aumentó de 22 a 68 y la progresión de centros con diagnóstico de la infección por el VIH en Banswazra fue de 1 a 53 centros y en Jhunjhunu de 10 a 81. La proporción de pacientes con TB que cuentan con una prueba del VIH en estos distritos aumentó un 27% y un 19%, respectivamente.
Of the estimated 9 million incident tuberculosis (TB) cases globally in 2013, about 13% were co-infected with the human immunodeficiency virus (HIV).1 The World Health Organization (WHO) recommends offering routine HIV testing to all diagnosed TB patients.2 In 2014, 72% of the approximately 1.4 million TB cases registered for treatment in India knew their HIV status.3 In Rajasthan, however, only 48% of the 94 499 (133 per 100 000 population) diagnosed TB patients knew their HIV status in 2013, due to the limited number of HIV testing facilities available within the general health care services.
To overcome this constraint, the government of Rajasthan in 2013 made it a state-wide policy to establish HIV diagnostic facilities at all peripheral health institutions (PHIs) that were not integrated counselling and testing centres (facilities with a trained counsellor and a laboratory technician) or facility-integrated counselling and testing centres (facilities with a nurse and a laboratory technician trained for counselling and testing), and to provide sputum smear microscopy facilities at all PHIs that were not designated microscopy centres (DMCs). We undertook a study in two districts of Rajasthan to determine whether implementation of this policy led to an increase in the proportion of notified TB cases with known HIV status and in TB notification rates in these districts.
METHODS
This was a descriptive study involving a review of existing records conducted in Banswara and Jhunjhunu districts, selected based on operational convenience, with populations in 2015 of respectively 2.0 and 2.3 million.
To abstract the data, we reviewed the registers routinely maintained by the national TB programme (laboratory register and TB treatment register), the national HIV programme (laboratory register) and the programme reports. Study variables included the projected district population, the number of presumptive TB patients examined for sputum smear microscopy, the number of all types of TB cases diagnosed, the number of TB patients registered for treatment and the number tested for HIV. The data were divided into two periods for the purpose of comparison: 1) the pre-intervention period from 1 July 2012 to 30 June 2013, and 2) the intervention period from 1 July 2013 to 30 June 2014. All data were checked for accuracy and consistency by triangulating information across registers and reports. The number of TB diagnostic facilities increased from 33 to 63 in Banswara District and from 22 to 68 in Jhunjhunu District, while the number of HIV testing facilities in these districts increased from 1 to 53 and from 10 to 81, respectively, from the pre-intervention period to the intervention period.
We calculated the number of presumptive TB cases examined per 100 000, the number of TB cases notified per 100 000, and the proportion of TB patients tested for HIV infection before and after the policy change. The χ2 test was used to assess statistical differences in proportions (P < 0.05).
Ethics approval was obtained from the Ethics Committee of the National Tuberculosis Institute, Bangalore, India, and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France.
RESULTS
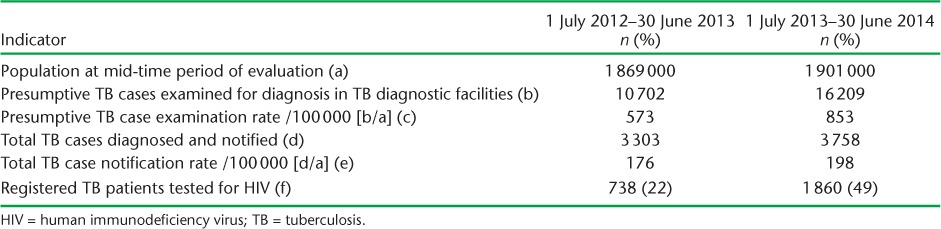
In Banswara District, 10 702 presumptive TB cases were examined in the pre-intervention period and 16 209 in the intervention period, with examination rates of respectively 573/100 000 and 853/100 000 (Table 1). The number of TB cases diagnosed and notified were respectively 3303 and 3758, with total TB case notification rates of 176/100 000 and 198/100 000. The proportions of TB cases tested for HIV were respectively 22% and 49% in the two periods.
TABLE 1.
Comparison of rates of presumptive cases examined, notified and tested for HIV, Banswara District, Rajasthan, India
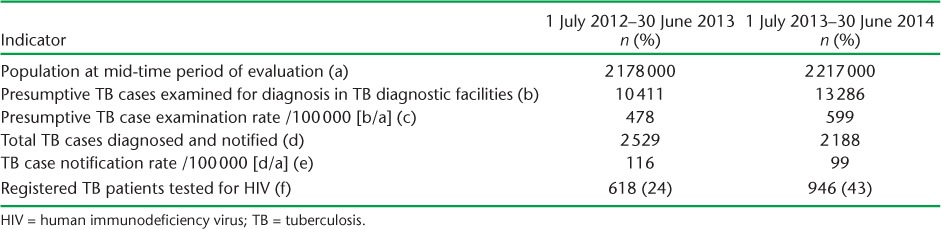
In Jhunjhunu District, 10 411 presumptive TB cases were examined in the pre-intervention period and 13 286 in the intervention period, with examination rates of 478/100 000 and 599/100 000 (Table 2). The number of TB cases diagnosed and notified were respectively 2259 and 2188 and the total TB case notification rates were 116/100 000 and 99/100 000. The proportions of TB cases tested for HIV in the two periods were respectively 24% and 43%.
TABLE 2.
Comparison of rates of presumptive cases examined, notified and tested for HIV, Jhunjhunu District, Rajasthan, India
In both districts, the differences in the number of presumptive TB cases examined and the proportion of registered TB patients tested for HIV between the pre-intervention and the intervention period were statistically significant (P < 0.001). The increase in the TB case notification rate in Banswara District and the decrease in the same rate in Jhunjhunu District were both statistically significant (P < 0.001).
DISCUSSION
The policy change in Rajasthan resulted in a statistically significant increase in the number of presumptive TB cases examined and the proportion of registered TB patients tested for HIV in both districts. A study from West Bengal also found that poor uptake of HIV testing among patients with TB was associated with an absence of HIV testing services at sites providing TB care services, and that increasing the ease of access to HIV testing can increase the uptake of provider-initiated HIV testing and care.4 In Nigeria, it was suggested that ‘HIV services must be fully decentralised and integrated into the fabric of the health system for an AIDS-free generation’.5
Although the total number of TB examinations increased in both districts, the TB case notification rate increased in Banswara District and decreased in Jhunjhunu District. This could be a result of the quality of the TB diagnostic services. Further studies should be conducted, covering all the districts of Rajasthan, to provide more information on the impact of the new policy on the TB case notification rate. Although there has been a significant increase in HIV testing in the state, only half of the TB patients diagnosed knew their HIV status. These data should continue to be monitored, as the proportions of patients HIV tested might continue to improve as medical officers and field staff become sensitised to the new policies.
The study results should be interpreted keeping in mind that during the period after the implementation of the policy, quality assurance for sputum microscopy in PHIs other than DMCs, and for HIV testing in PHIs, was not in place. Trends in case notification should continue to be monitored once quality assurance is implemented.
Our study shows that decentralising HIV testing facilities at all PHIs led to a greater proportion of HIV testing among persons with TB. Ensuring early access to HIV care services may reduce both TB and HIV transmission and TB-HIV related mortality.
Acknowledgments
The study was undertaken as a part of the ‘TB Operations Research Training Project’ conducted by the International Union Against Tuberculosis and Lung Disease (The Union), Paris France, with funding support from The Global Fund to Fight AIDS, Tuberculosis and Malaria, Geneva, Switzerland, through Project Axshya (The Union). This training project was conceived and implemented by The Union South-East Asia Office (New Delhi, India), in collaboration with the Central TB Division (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India), the National TB Institute (Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India, Bangalore, India), the World Health Organization (India Country Office), and the US Centers for Disease Control and Prevention (CDC, Division of TB Elimination, Atlanta, GA, USA). The authors acknowledge the support of the above institutions and also thank the study participants and the staff of the Banswara and Jhunjhunu districts of Rajasthan, India, for their cooperation.
The authors alone are responsible for the views expressed in this publication and these views do not necessarily represent the decisions or policies of the WHO, The Union, or the CDC.
Footnotes
Conflicts of interest: none declared.
References
- 1. World Health Organization. . Global tuberculosis report, 2014. WHO/HTM/TB/2014.08 Geneva, Switzerland: WHO, 2014. [Google Scholar]
- 2. World Health Organization. . WHO policy on collaborative TB/HIV activities: guidelines for national programmes and other stakeholders. WHO/HTM/TB/2012.1 Geneva, Switzerland: WHO, 2012. http://whqlibdoc.who.int/publications/2012/9789241503006_eng.pdf Accessed January 2017. [PubMed] [Google Scholar]
- 3. Central Tuberculosis Division. . TB India. Revised National Tuberculosis Control Programme. Annual Status Report. New Delhi, India: Ministry of Health and Family Welfare, 2015. [Google Scholar]
- 4. Bishnu B, Bhaduri S, Kumar A M V, . et al. What are the reasons for poor uptake of HIV testing among patients with TB in an Eastern India District? PLOS ONE 2013; 8: e55229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oleribe O E, Nwachukwu C E, Akande S F, . et al. An AIDS-free world through the full decentralisation of HIV services: a proof-of-concept study. Lancet 2013; 382 ( Suppl 2): S1. [Google Scholar]


