Abstract
Septoplasty alone is not always sufficient to correct nasal obstruction. Various techniques have been employed to repair nasal valve collapse and improve airflow.
This article aimed to evaluate outcomes and quality of life following nasal valve reconstruction using a titanium implant in patients with nasal valve collapse.
This is a single-center retrospective study that consisted of a telephone questionnaire of 37 quality-of-life measures and questions related to the surgical procedure and recovery process to evaluate postsurgical outcomes.
Fifteen patients completed the survey. There was a significant improvement in nasal blockage/obstruction, breathing through the nose, sleeping, breathing through nose during exercise, the need to blow nose, sneezing, facial pain/pressure, fatigue, productivity, and restlessness/irritability after surgery. Overall, 100% of patients were satisfied with the results and would recommend this procedure. The most common postoperative complaints were pain (33%) and difficulty breathing (33%). Patients noticed no increase (20%) or a slight increase (73%) in the size of their nose. Sixty percent of patients cannot see the implant and 13% report the implant is barely noticeable.
Nasal valve repair with a titanium implant was successful at improving symptoms of nasal obstruction and other quality-of-life issues. Satisfaction was high among all patients. The implants are palpable, thought to be visible by some patients, yet accepted by the majority of patients. This approach may be especially important in patients with prior nasal surgery but continue to experience refractory symptoms.
Keywords: nasal valve collapse, titanium implant, nasal valve reconstruction, patient satisfaction
Every functional rhinoplasty surgeon understands that sometimes septoplasty is just not enough. Septoplasty is a commonly performed procedure, where in general the majority of patients achieve the desired outcome, improvement in nasal airflow. 1 2 The procedure is in theory ideal—no resulting change in the shape of the nose and all incisions are hidden. However, sometimes septoplasty alone is not sufficient to correct nasal airway obstruction. While the reason for the failure of septoplasty may be due to the presence of an inflammatory process, the most common reason for failure is related to the structure of the nasal valve. The internal nasal valve is that area of the nose defined by the junction of the septum and the lateral nasal sidewall, where the septum, the inferior turbinate, and the caudal edge of the upper lateral cartilage meet. 3 This nasal valve collapse (NVC) or nasal valve dysfunction could have been present prior to septoplasty or could have been a result of the septoplasty, and can also be a consequence of rhinoplasty. 4
There is no single test or examination that, by itself, defines NVC. When used appropriately, many tests may be helpful including standard axial CT imaging; anterior rhinoscopy; physical exam maneuvers such as the Cottle maneuver, cheek elevation maneuvers, nasal speculum or Q-tip, or a trial of an external nasal dilator; and patient questionnaires. 5 6 7 8
There is no standard treatment for NVC. Literature offers many novel techniques offering alternative methods for treatment of the nasal valve. Traditionally, one of the most common techniques is the use of the nasal spreader graft. 9 10 11 12 Many other clever methods to lateralize the upper lateral cartilages from the nasal septum have been reported, including suture techniques, 13 14 onlay-type spreader grafts, 15 H-graft technique, 16 lateral crural flaps, 17 18 nasal batten grafts, 19 20 auto spreader flap, 21 22 intranasal Z-plasty transposition flaps, 23 24 and the butterfly graft. 25 26 The fact that so many new techniques are being developed demonstrates that no technique is perfect.
Optimally, correcting a NVC should result in an improvement in function, while achieving a cosmetically acceptable outcome. Improving function, in terms of decreased nasal airway resistance, has been reported using techniques including use of the spreader graft and flaring sutures. 27 However, gain of function often comes at the expense of the cosmetic result. Many of the previously discussed techniques require some type of a graft, frequently a cartilage graft, either from the septum or, in cases of revision surgery, from the conchal bowl or ribs. A consideration with cartilage grafting, other than requiring a second surgical site, is to provide a significant amount of structural support, relatively larger and thicker grafts may be required. Chaiet and Marcus, for example, quantified the increase in volume caused by the use of the very powerful onlay butterfly graft as a mean 6.4% increase in nasal tip width. They further reported up to 19% dissatisfaction with the increase in cosmetic results. 26
Chaiet and Marcus' findings support what has been observed clinically, good functional outcome of onlay butterfly grafts but disappointing results aesthetically with the significant change in nasal tip size, and led the author (N.D.G.) of this study to consider an alternative approach using the same structural concept. Instead of using a cartilage graft, a titanium plate, from traditional trauma plating systems, was chosen. The goal of using a titanium plate in nasal valve reconstruction was to provide better cosmesis using a lower profile implant, while providing better structural support than the previously described techniques. The implant functions the same way as an external nasal dilator. Hurbis described a similar procedure using the Monarch Nasal Implant, made of either an expanded polytetrafluoroethylene or a silicone casing surrounding a titanium core. 28 29 Various other alternatives to using a cartilage graft have been described, including the use of grafts made of synthetic materials such as nonresorbable high-density porous polyethylene 9 and resorbable polymer of polyglycolic and polylactic acid. 10
The objective of this study is to evaluate patient-reported outcomes after placement of the titanium implants, in place of cartilage grafts alone, in nasal valve reconstruction. Outcome measures such as changes in pre- and postoperative symptoms related to nasal obstruction and changes in nose size will be assessed to help both patients and surgeons in the future determine which nasal valve repair technique is most appropriate in regard to functional and cosmetic outcomes. Additionally, surgical and postoperative complications will be assessed.
Methods
This was a single-center retrospective study evaluating outcomes, morbidity, and improvement in quality-of-life issues as well as perioperative recovery in patients undergoing nasal valve repair using a titanium implant. This study consisted of a telephone questionnaire of 37 quality-of-life measures and or questions related to the surgical procedure and recovery process. Data on surgical and postoperative complications were also obtained from chart review. Approval for this study was obtained from Wake Forest School of Medicine Institutional Review Board.
Participants
Medical records were searched from December 2005 to September 2011 to identify and recruit all patients aged 18 and older who underwent nasal valve reconstruction by a single surgeon (author N.D.G.) at Department of Otolaryngology, Wake Forest Baptist Medical Center. Patients were called with a scripted telephone message inviting them to participate in the questionnaire titled “Nasal Valve Reconstruction Quality-of-Life Assessment.” Verbal consent was obtained from patients who agreed to participate. These patients were then offered a choice to answer the questions over the phone or to have the survey mailed to them. Three attempts were made to contact each potential candidate. If the patient could not be contacted or refused to participate, they were not further contacted to participate in this study.
Nasal Valve Reconstruction Quality-of-Life Assessment
This questionnaire consisted of a combination of questions that asked subjects to rate perioperative symptoms and morbidities, as well as comparisons of symptoms before and after surgery. Subjects were first asked 13 questions regarding the worst part of the recovery period, suggested time off of work after surgery, change in size of their nose, subjects' thoughts on their nose, other's thoughts about the subject's nose, if an implant was used and whether it is visible/palpable, whether titanium implant is sensitive to cold weather, if a graft was taken from an ear is there pain or change in shape of the ear, overall satisfaction with the procedure, changes in airway, whether they would recommend the surgery, and whether others undergoing this procedure should be concerned about a postsurgical nose that is too large. Additionally, patients were asked to rate 25 symptoms before and after surgery on a 5-point scale (1 = no problem, 3 = moderate problem, 5 = severe problems), including headache, sneezing, need to blow nose, difficulty breathing through nose, nasal discharge, nasal blockage, sleeping difficulty, and fatigue. Additional questions including sadness, embarrassment, asthma, reduced concentration, dizziness, and ear pain which are unrelated to outcomes of nasal valve repair were included as internal controls. A two-sample t -test was used to compare the average responses between preoperative and postoperative outcomes.
Nasal Valve Reconstruction Procedure
In all patients who underwent nasal valve reconstruction, an open approach was used to access the nasal valve. A transcolumellar incision and release of the septal mucoperichondrial flaps on both sides of the septum and off the undersurface of the upper lateral cartilage provided total mobility and control of the valve ( Fig. 1 ).
Fig. 1.
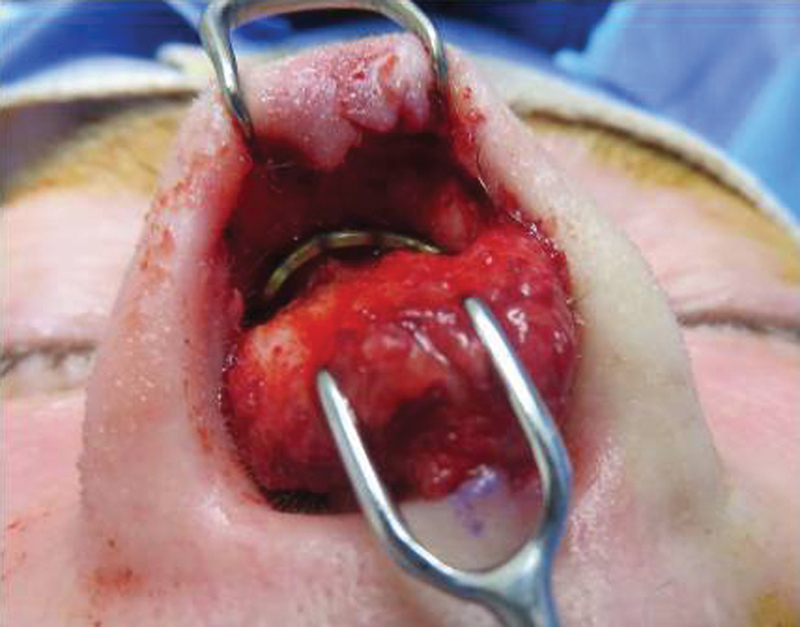
Access to nasal valve and placement of titanium plate. A transcolumellar incision is made and the septal mucoperichondrial flaps on both sides of the septum and off the undersurface of the upper lateral cartilage are released.
The titanium implants used were standard trauma plates from Synthes (Synthes, Inc., West Chester, PA). Most procedures used the 0.4- or 0.5-mm low-profile straight or rectangular plates from the midface plating system. No single standard shape or length was chosen ( Fig. 2 ). While these plates are FDA-approved medical devices, they were used off label in this setting. They were placed subcutaneously in a pocket just above the nasal valve at the cephalic margin of the lower lateral cartilages and the caudal end of the upper lateral cartilage from just above the pyriform aperture on one side to the pyriform aperture on the opposite side. No bony fixation was performed; all plates were mobile and free floating in the soft tissue of the nose ( Figs. 1 and 3 ). The septal mucosal flaps were closed with a mattress suture to minimize the chance of hematoma and to maintain the integrity of septal flaps that may have been compromised from previous surgery. When turbinectomies were performed, they were done by removing the lateral bone and mucosa, and attempting to maintain an intact medial mucosa.
Fig. 2.
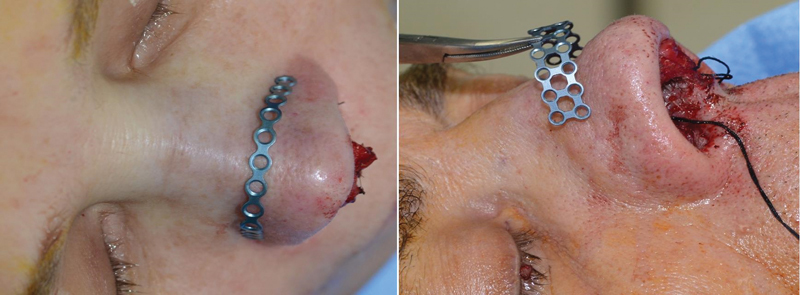
Examples of various titanium implants used for nasal valve reconstruction. Various implants were used, with size dependent on skin thickness and individual patient needs. Placement is demonstrated in desirable location above skin; surgically implant is secured in a pocket subcutaneously.
Fig. 3.
CT imaging of titanium implant in place after naval valve reconstruction. Titanium implant is in place subcutaneously after naval valve reconstruction.
Patients who underwent nasal valve reconstruction were casted with an external thermal splint left in position for 5 to 7 days. Nasal septal splints of silicone sheeting were used for 5 to 7 days.
No implants were placed in patients who had a significant disruption of the nasal mucosal envelope, as it was felt to be too risky with regard to potential infection or extrusion. To reduce the potential visibility of the implanted plate, skin flaps were made as thick as possible to lift all the soft tissues off the lower lateral cartilage and upper lateral cartilage. Antibiotics were given preoperatively and continued for 5 days postoperatively.
Results
Participants
A total of 16 patients who underwent nasal valve reconstruction with a titanium implant and met inclusion criteria were contacted and 15 agreed to participate in the study. Six females and nine males, with an average age of 58 years (SD: 11.2), completed the questionnaire. Eleven of 15 patients (73.33%) had previous nasal surgery. Average follow-up from the time the procedure was performed to when the survey was administered was 23 months (range: 1–57 months). Five patients had follow-up of 6 months or less and eight patients had follow-up of 24 months or less. The remaining seven patients had follow-up of more than 24 months, with two of these patients having follow-up of more than 48 months. Patients were offered a titanium implant to maximally improve their airways, and frequently had a combination of other procedures including columellar strut (53%), septoplasty or revision septoplasty (100%), turbinate reduction (53%), and ear cartilage graft (20%).
Questionnaire
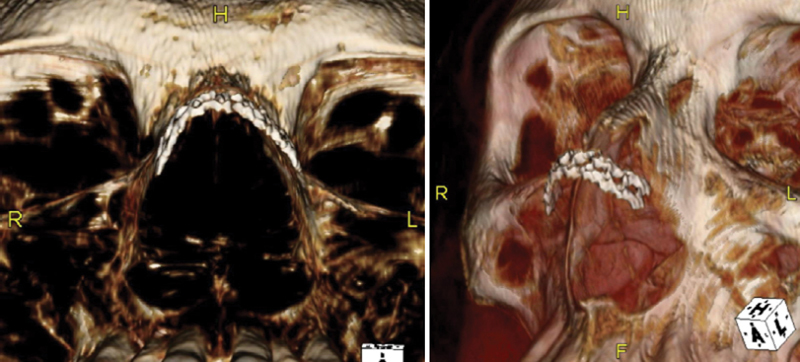
Subjects reported that the worst part of the recovery period was difficulty breathing (33%) and pain (33%), followed by swelling and bruising (27%). Subjects were least likely to rate bleeding (7%) as the worst part of recovery. When asked how much time they suggest patients should take off work or usual activities, 47% suggested 2 weeks ( Fig. 4 ).
Fig. 4.
Patients' responses to symptoms experienced during postoperative recovery period and how much time they felt was needed for recovery. Patient-reported pain and bleeding were the worse symptoms during the recovery period. Two weeks of time was the most common response needed for recovery.
When subjects were asked if they noticed a change in the size of their nose postoperatively, the majority of patients (73%) reported that their nose was slightly larger and 20% noticed no change ( Fig. 5 ). Of those patients who noticed that their nose was larger ( N = 12), 42% either thought about it once or occasionally; while 17% reported that they thought about it daily. More than half of these subjects (58%) reported that no one commented on their nose being larger and 33% reported rarely receiving a comment on the size ( Fig. 6 ).
Fig. 5.
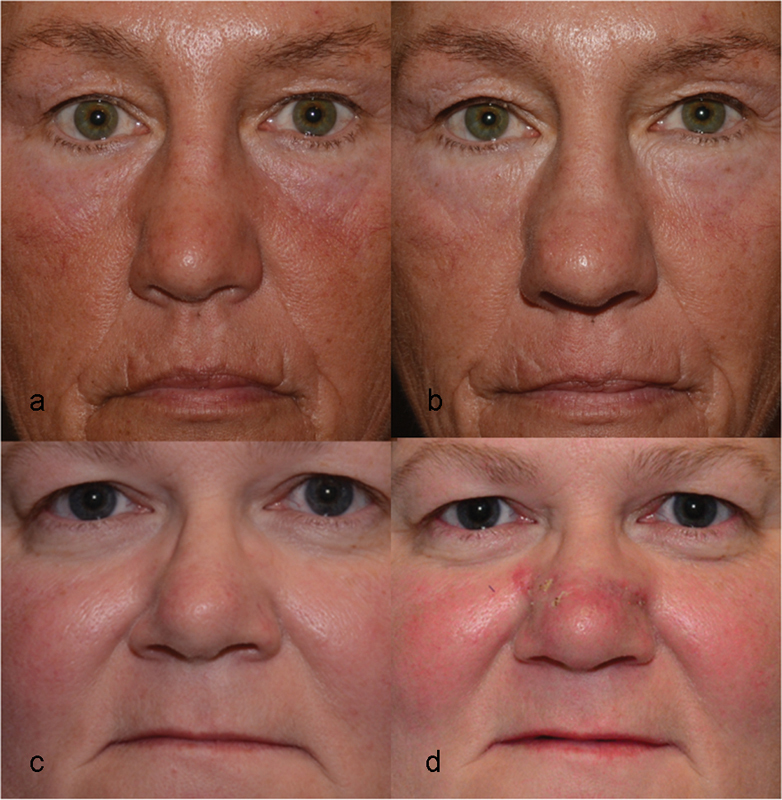
Before and after pictures. ( a and c ) Before nasal valve reconstruction and placement of titanium plate. ( b ) 1 year postoperative showing a larger, wider nose and with the plate nearly visible. ( d ) 3 weeks postoperative showing a wider nose, partially attributed to postoperative swelling, and with the plate nearly visible.
Fig. 6.
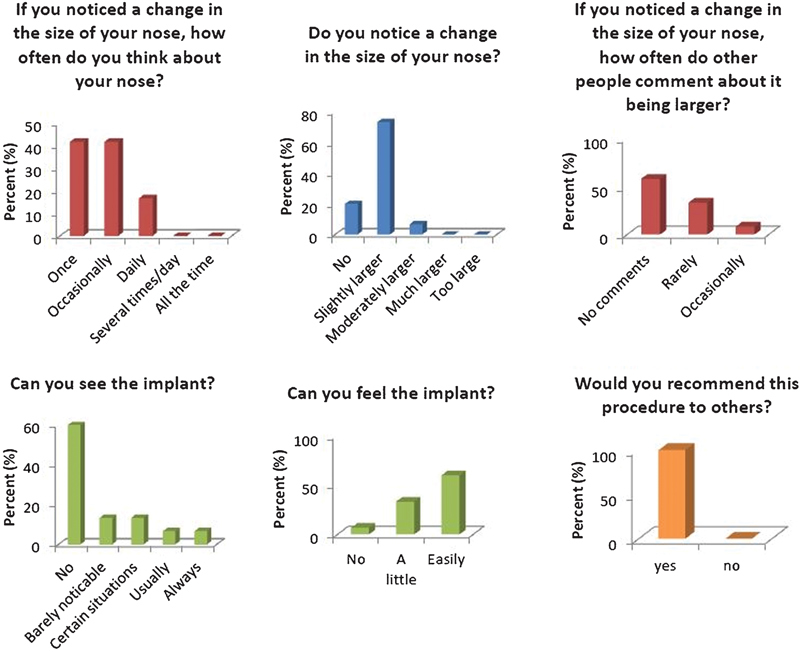
Patients' responses to questions related to whether they felt the titanium implant changed the size of their nose and whether the implant was visible or palpable. All patients responded they would recommend this procedure to others.
A majority of subjects reported that they could not see the implant (60%), but that the implant could be easily felt (60%). Most patients (73%) reported no sensitivity to cold weather with the implant (the study was conducted in North Carolina and outcomes may differ in colder climates). Patients overwhelmingly (100%) would recommend the procedure despite the implants being palpable and/or occasionally visible ( Fig. 6 ).
Subjects reported a statistically significant improvement in nasal blockage or obstruction, trouble breathing through the nose, trouble sleeping, and difficulty breathing through the nose during exercise after nasal valve reconstruction compared with before surgery ( Fig. 7 ). Statistically significant improvement was also noted with the need to blow the nose, sneezing, facial pressure/pain, difficulty breathing through the nose, difficulty falling asleep, waking at night, lack of a good night sleep, waking up tired, fatigue, reduced productivity, and feeling frustrated/restless/irritable ( Table 1 ).
Fig. 7.
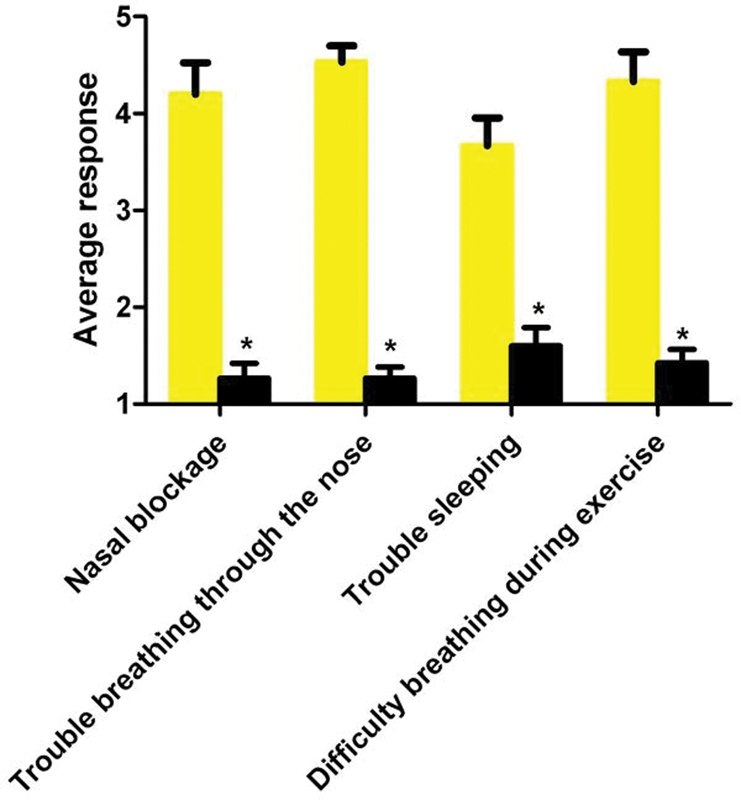
Patient reported improvement in symptoms. Patients reported significant improvement in all symptoms including problems with nasal blockage or obstruction, trouble breathing through nose, trouble sleeping, and difficulty breathing through nose during exercise. *p < 0.001.
Table 1. Patients' grading of symptoms before and after nasal valve reconstruction with placement of a titanium implant on a 5-point scale (1 = no problem, 3 = moderate problem, 5 = severe problems).
| Preoperative | Postoperative | ||||||
|---|---|---|---|---|---|---|---|
| Average | ± | SEM | Average | ± | SEM | p -Value | |
| Need to blow nose | 3.33 | ± | 0.35 | 1.13 | ± | 0.32 | <0.0001 |
| Sneezing | 1.93 | ± | 0.47 | 0.67 | ± | 0.36 | 0.04 |
| Facial pain/pressure | 1.67 | ± | 0.44 | 0.53 | ± | 0.27 | 0.04 |
| Difficulty breathing through the nose | 4.07 | ± | 0.34 | 0.60 | ± | 0.21 | <0.0001 |
| Difficulty falling asleep | 2.00 | ± | 0.54 | 0.60 | ± | 0.25 | 0.03 |
| Waking up at night | 2.67 | ± | 0.41 | 1.13 | ± | 0.34 | 0.007 |
| Lack of good night sleep | 3.07 | ± | 0.44 | 1.20 | ± | 0.33 | 0.002 |
| Wake up tired | 2.87 | ± | 0.47 | 1.13 | ± | 0.31 | 0.005 |
| Fatigue | 2.47 | ± | 0.41 | 1.13 | ± | 0.34 | 0.02 |
| Reduced productivity | 1.93 | ± | 0.48 | 0.73 | ± | 0.30 | 0.04 |
| Frustrated/restless/irritable | 2.27 | ± | 0.45 | 0.73 | ± | 0.23 | 0.005 |
Notes: Symptoms not listed which did not significantly change include runny nose, postnasal discharge, thick nasal discharge, dizziness, ear pain, decreased sense of smell, reduced concentration, sadness, embarrassment, and asthma. Unrelated symptoms, such as sadness, added to the survey as a control, also did not significantly change adding to the reliability of data reporting.
There was no statistically significant change in the following outcomes: dizziness, ear pain, reduced concentration, sadness, embarrassment, asthma, runny nose, postnasal discharge, thick nasal discharge, and decreased sense of smell.
Surgical and Postoperative Complications
Postoperatively, in 2 of the 16 patients who underwent nasal valve reconstruction with placement of a titanium plate, extrusion of the implant at the marginal incision occurred. In one patient, this occurred at 4 months postoperatively; dates of other complications were not recorded in the data collection. This complication was managed by opening a small portion of the marginal incision, cutting off one to two holes of partially exposed plate, and reclosing a mucosal flap over the plate, thus salvaging the original plate. No plates extruded at any site other than the marginal incision. One plate broke postoperatively. This plate was removed and replaced in a simple outpatient procedure done under local anesthesia with no further morbidity. Additionally, one infection of the plate was reported.
Discussion
Implants have been used in facial reconstruction to improve both cosmetic and functional deficiencies. The results of our study support the use of titanium implants in nasal valve reconstruction, with improved outcomes in function and results that are cosmetically acceptable. Overall, patients are highly satisfied with the procedure and would recommend it to others. The goal of this procedure is to improve symptomatic nasal obstruction and statistically significant improvement was reported in related symptoms such as difficulty breathing through the nose, trouble sleeping, and facial pain/pressure. While the majority of patients did notice that their nose was slightly larger after surgery, 20% of patients did not notice a change in size, and no patients reported their nose was much larger or too large. Furthermore, of these patients who felt their nose was larger, in general it does not appear to affect their quality of life, as most reported that they only thought about it once or occasionally. These findings are encouraging from both a functional and cosmetic standpoint.
The benefits of nasal valve reconstruction must be weighed against any potential risk. The complications in this patient population were limited and the procedure appears to be well tolerated. The two cases of implant extrusion were likely a result of surgical technique, as the marginal incision was not closed, a technique adapted from primary rhinoplasties. This may be avoidable by closing the pocket when implants are placed. However, Hurbis similarly reported extrusion of implants using the Monarch Nasal Implant at a rate of 3 out of 39 patients, despite closing the marginal incisions. 28 To prevent the implant breaking, which occurred in one patient, the risk of using a smaller thinner plate that may be more cosmetically appealing must be balanced against using a larger stronger plate that will tolerate the stress of deformation longer or withstand trauma. The longevity of the implant is a concern when using titanium implants in the nose. Patients were counseled prior to placement by informing them that these implants, like other implants (joint replacement, valve replacement, breast augmentation), have a limited lifespan. As the longest follow-up in our patient population was 57 months, we cannot comment on the longevity of these implants; however, the hope is that they will last 8 to 10 years. In the two patients who had follow-up over 48 months, there were no complications with the plates. However, patients undergoing this procedure should be followed up annually to assess implant viability and to allow for implant adjustments if needed; the titanium plate can be physically maneuvered and adjusted appropriately. Patients are instructed to not attempt adjusting the plates themselves.
Patients overall appeared to tolerate the procedure well. Difficulty breathing and pain were most commonly reported as the worst part of the recovery period. However, almost half of the subjects felt that 2 weeks' time was sufficient to recover. Bleeding was not a common postoperative complaint which was expected as the nose was packed preoperatively with splints and nonstick packing.
Limitations of this study include recall bias. Follow-up from the time of procedure to when the survey was administered was as long as 57 months and subjects therefore may have had difficulty recalling specifics of the recovery period and preoperative versus postoperative symptoms. However, a longer follow-up period, 5 to 10 years, would be beneficial to better assess complications and longevity of the implants, especially given that over half of the patients (8 out of 15 patients) had follow-up of 24 months or less. Not all patients evaluated for nasal valve reconstruction were offered titanium implants, creating preselection bias. Initially, patients who had significant and serious comorbidities and would most benefit from this procedure in regard to improved function were selected. Younger patients were typically not offered these implants due to concern that aesthetically they would not tolerate them. However, this is true of most nasal valve repairs, which can be bulky and result in increased nasal size, such as onlay grafts, butterfly graphs, or large spreader graphs. Clearly, there was a subset of patients who would have been less than satisfied with the outcome of a bulky nasal implant or graft who made this very clear prior to their surgical intervention. Had this group of patients been included in the study it would have likely resulted in poorer overall patients' satisfaction. Finally, confounding is evident in this study, as most patients had additional procedures performed concurrently with the nasal valve repair. Furthermore, the majority of patients had various prior nasal surgeries and therefore it was impossible to control for patient variability in terms of both reported functional and cosmetic outcomes.
Conclusion
Nasal valve reconstruction with the use of titanium implants appears to be a suitable option in appropriate patients. Overall, patients are satisfied with the procedure, achieving improved functional outcomes and acceptable cosmetic results. The procedure was in general well tolerated with limited complications. It should be emphasized that the use of the Synthes titanium plates for nasal valve reconstruction is off label and should be reserved for surgeons with extensive experience placing these implants. Future prospective, randomized controlled trials may be needed to further support our findings. Studies comparing outcomes of this procedure to other commonly performed procedures such as the nasal spreader graft and auto spreader graft may offer guidance to both surgeons and patients and help establish standards for treatment of nasal valve dysfunction.
References
- 1.Stewart M G, Smith T L, Weaver E M et al. Outcomes after nasal septoplasty: results from the Nasal Obstruction Septoplasty Effectiveness (NOSE) study. Otolaryngol Head Neck Surg. 2004;130(03):283–290. doi: 10.1016/j.otohns.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Bezerra T F, Stewart M G, Fornazieri M A et al. Quality of life assessment septoplasty in patients with nasal obstruction. Rev Bras Otorrinolaringol (Engl Ed) 2012;78(03):57–62. doi: 10.1590/S1808-86942012000300011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta A, Brooks D, Stager S, Lindsey W H. Surgical access to the internal nasal valve. Arch Facial Plast Surg. 2003;5(02):155–158. doi: 10.1001/archfaci.5.2.155. [DOI] [PubMed] [Google Scholar]
- 4.Ballert J A, Park S S. Functional considerations in revision rhinoplasty. Facial Plast Surg. 2008;24(03):348–357. doi: 10.1055/s-0028-1083088. [DOI] [PubMed] [Google Scholar]
- 5.Moche J A, Cohen J C, Pearlman S J. Axial computed tomography evaluation of the internal nasal valve correlates with clinical valve narrowing and patient complaint. Int Forum Allergy Rhinol. 2013;3(07):592–597. doi: 10.1002/alr.21128. [DOI] [PubMed] [Google Scholar]
- 6.Rhee J S, Weaver E M, Park S S et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg. 2010;143(01):48–59. doi: 10.1016/j.otohns.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cannon D E, Rhee J S. Evidence-based practice: functional rhinoplasty. Otolaryngol Clin North Am. 2012;45(05):1033–1043. doi: 10.1016/j.otc.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 8.Murrell G L. Components of the nasal examination. Aesthet Surg J. 2013;33(01):38–42. doi: 10.1177/1090820X12469626. [DOI] [PubMed] [Google Scholar]
- 9.Gürlek A, Celik M, Fariz A, Ersöz-Oztürk A, Eren A T, Tenekeci G. The use of high-density porous polyethylene as a custom-made nasal spreader graft. Aesthetic Plast Surg. 2006;30(01):34–41. doi: 10.1007/s00266-005-0119-8. [DOI] [PubMed] [Google Scholar]
- 10.Stal S, Hollier L.The use of resorbable spacers for nasal spreader grafts Plast Reconstr Surg 200010604922–928., discussion 929–931 [PubMed] [Google Scholar]
- 11.de Pochat V D, Alonso N, Mendes R R, Cunha M S, Menezes J V. Nasal patency after open rhinoplasty with spreader grafts. J Plast Reconstr Aesthet Surg. 2012;65(06):732–738. doi: 10.1016/j.bjps.2011.11.059. [DOI] [PubMed] [Google Scholar]
- 12.Yoo D B, Jen A. Endonasal placement of spreader grafts: experience in 41 consecutive patients. Arch Facial Plast Surg. 2012;14(05):318–322. doi: 10.1001/archfacial.2012.173. [DOI] [PubMed] [Google Scholar]
- 13.Rizvi S S, Gauthier M G. Lateralizing the collapsed nasal valve. Laryngoscope. 2003;113(11):2052–2054. doi: 10.1097/00005537-200311000-00037. [DOI] [PubMed] [Google Scholar]
- 14.Rizvi S S, Gauthier M G. Lateralizing the collapsed nasal valves simplified: 10-year survey of a simple concealed suture technique. Laryngoscope. 2011;121(03):558–561. doi: 10.1002/lary.21350. [DOI] [PubMed] [Google Scholar]
- 15.Alsarraf R, Marakami C S. The saddle nose deformity. Facial Plast Surg Clin North Am. 1999;7:303–310. [Google Scholar]
- 16.Tastan E, Demirci M, Aydin E et al. A novel method for internal nasal valve reconstruction: H-graft technique. Laryngoscope. 2011;121(03):480–486. doi: 10.1002/lary.21437. [DOI] [PubMed] [Google Scholar]
- 17.Sazgar A A, Woodard C, Most S P. Preservation of the nasal valve area with a lateral crural hinged flap: a cadaveric study. Aesthetic Plast Surg. 2012;36(02):244–247. doi: 10.1007/s00266-011-9797-6. [DOI] [PubMed] [Google Scholar]
- 18.Apaydin F. Lateral crural turn-in flap in functional rhinoplasty. Arch Facial Plast Surg. 2012;14(02):93–96. doi: 10.1001/archfacial.2011.798. [DOI] [PubMed] [Google Scholar]
- 19.Sufyan A, Ziebarth M, Crousore N, Berguson T, Kokoska M S. Nasal batten grafts: are patients satisfied? Arch Facial Plast Surg. 2012;14(01):14–19. doi: 10.1001/archfacial.2011.1187. [DOI] [PubMed] [Google Scholar]
- 20.Sufyan A S, Hrisomalos E, Kokoska M S, Shipchandler T Z. The effects of alar batten grafts on nasal airway obstruction and nasal steroid use in patients with nasal valve collapse and nasal allergic symptoms: a prospective study. JAMA Facial Plast Surg. 2013;15(03):182–186. doi: 10.1001/jamafacial.2013.974. [DOI] [PubMed] [Google Scholar]
- 21.Gruber R P, Park E, Newman J, Berkowitz L, Oneal R. The spreader flap in primary rhinoplasty. Plast Reconstr Surg. 2007;119(06):1903–1910. doi: 10.1097/01.prs.0000259198.42852.d4. [DOI] [PubMed] [Google Scholar]
- 22.Yoo S, Most S P. Nasal airway preservation using the autospreader technique: analysis of outcomes using a disease-specific quality-of-life instrument. Arch Facial Plast Surg. 2011;13(04):231–233. doi: 10.1001/archfacial.2011.7. [DOI] [PubMed] [Google Scholar]
- 23.Dutton J M, Neidich M J. Intranasal Z-plasty for internal nasal valve collapse. Arch Facial Plast Surg. 2008;10(03):164–168. doi: 10.1001/archfaci.10.3.164. [DOI] [PubMed] [Google Scholar]
- 24.Weeks D M, Walker D D, Dutton J M. Anatomical comparison of minimally invasive nasal valve procedures. Arch Facial Plast Surg. 2012;14(03):189–192. doi: 10.1001/archfacial.2012.24. [DOI] [PubMed] [Google Scholar]
- 25.Clark J M, Cook T A. The ‘butterfly’ graft in functional secondary rhinoplasty. Laryngoscope. 2002;112(11):1917–1925. doi: 10.1097/00005537-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Chaiet S R, Marcus B C. Nasal tip volume analysis after butterfly graft. Ann Plast Surg. 2014;72(01):9–12. doi: 10.1097/SAP.0b013e3182586b5d. [DOI] [PubMed] [Google Scholar]
- 27.Jalali M M. Comparison of effects of spreader grafts and flaring sutures on nasal airway resistance in rhinoplasty. Eur Arch Otorhinolaryngol. 2015;272(09):2299–2303. doi: 10.1007/s00405-014-3327-5. [DOI] [PubMed] [Google Scholar]
- 28.Hurbis C G. An adjustable implant for nasal valve dysfunction: a 3-year experience. Ear Nose Throat J. 2012;91(08):E5–E12. [PubMed] [Google Scholar]
- 29.Hurbis C G. An adjustable, butterfly-design, titanium-expanded polytetrafluoroethylene implant for nasal valve dysfunction: a pilot study. Arch Facial Plast Surg. 2006;8(02):98–104. doi: 10.1001/archfaci.8.2.98. [DOI] [PubMed] [Google Scholar]


