Abstract
AIM
To address the management of Clostridium difficile (C. difficile) infection (CDI) in the setting of suspected inflammatory bowel disease (IBD)-flare.
METHODS
A systematic search of the Ovid MEDLINE and EMBASE databases by independent reviewers identified 70 articles including a total of 932141 IBD patients or IBD-related hospitalizations.
RESULTS
In those with IBD, CDI is associated with increased morbidity, including subsequent escalation in IBD medical therapy, urgent colectomy and increased hospitalization, as well as excess mortality. Vancomycin-containing regimens are effective first-line therapies for CDI in IBD inpatients. No prospective data exists with regards to the safety or efficacy of initiating or maintaining corticosteroid, immunomodulator, or biologic therapy to treat IBD in the setting of CDI. Corticosteroid use is a risk factor for the development of CDI, while immunomodulators and biologics are not.
CONCLUSION
Strong recommendations regarding when to initiate IBD specific therapy in those with CDI are precluded by a lack of evidence. However, based on expert opinion and observational data, initiation or resumption of immunosuppressive therapy after 48-72 h of targeted antibiotic treatment for CDI may be considered.
Keywords: Biologic therapy, Clostridium difficile, Inflammatory bowel disease, Ulcerative colitis, Crohn’s disease, Corticosteroids
Core tip: Clostridium difficile infection (CDI), common and increasing in inflammatory bowel disease (IBD), is associated with worse outcomes in IBD. Vancomycin-containing regimens are effective first-line therapies for CDI in IBD. Ambiguity exists on the treatment of IBD flare in patients with CDI; however, case reports suggest corticosteroid initiation after appropriate antibiotic therapy may be effective.
INTRODUCTION
Inflammatory bowel disease (IBD), comprised of Crohn’s disease (CD) and ulcerative colitis (UC), are chronic, idiopathic inflammatory gastrointestinal disorders. The pathogenesis of IBD, although incompletely understood, is thought to arise from interactions between environmental and host factors. CD and UC are characterized by recurrent episodes of relapsing inflammation of the gastrointestinal tract with variable clinical manifestations and potentially serious complications including bleeding, perforation and abscess formation[1,2].
Clostridium difficile (C. difficile), a gram-positive spore-forming anaerobe, is highly transmissible through the fecal-oral route and its exotoxins cause a spectrum of disease ranging from mild or moderate diarrhea to fulminant infectious colitis occasionally complicated by toxic megacolon, colonic perforation, sepsis, and death[3].
Several diagnostic assays exist to assess for Clostridium difficile infection (CDI). DNA-based tests or nucleic acid amplification tests via polymerase chain reaction (PCR) for C. difficile toxin genes (tcdA and tcdB) have been found to be more sensitive than toxin A and B enzyme immunoassays (EIA) and are currently recommended as the preferred diagnostic test for CDI[4]. Other, less commonly used diagnostic assays for CDI include EIA for glutamate dehydrogenase (GDH, a protein produced by both toxigenic and non-toxigenic strains) with confirmatory testing via EIA for toxin genes. This has fallen out of favor in view of the more sensitive and rapid PCR assay. The advent of DNA-based testing may partially contribute to the observed increased incidence of CDI. Toxigenic culture is considered to be the gold standard diagnostic assay, albeit the slowest, requiring several days to result and therefore possibly delaying initiation of therapy.
While C. difficile is often pathogenic and accounts for significant morbidity and mortality in the health-care and community setting, it has also been found to colonize the stool of healthy children and adults[5-7]. CDI is most commonly defined as the presence of C. difficile toxin in the context of characteristic clinical manifestations including diarrhea and abdominal pain[4]. CDI rates are increasing in the general population. Health care institutions have seen large outbreaks of CDI as well as the emergence of hypervirulent strains[8-10]. Surveillance of CDI in the United States has demonstrated a shift in the epidemiology to more community-acquired infections. A nationwide study of CDI in the United States using Emerging Infections Program data from the Centers for Disease Control estimated 453000 incident infections in 2011, of which only 24% were identified during hospitalization, as opposed to the outpatient setting[11].
Decreased intestinal microbial diversity along with an inadequate immune response is thought to play a causative role in the development CDI[12-14]. Antibiotic exposure, leading to alterations in the gut microbiota, has been identified as a traditional risk factor for CDI. IBD also predisposes to CDI and accounts for considerable excess morbidity and mortality along with increased systemic costs in IBD patients. Reductions in gut microbial diversity as well as an increase in pro-inflammatory species have been identified in IBD patients[15]. Although a causative role for this dysbiosis in the development of IBD has not been well established, it is plausible that dysbiosis may play a role in increasing CDI risk in IBD patients. Due to an overlap in symptomatology, CDI also gives rise to a series of diagnostic and therapeutic challenges in the IBD population.
This systematic review aims to summarize the management of patients with CDI and concurrent, suspected IBD flares. The epidemiology, risk factors, and methods of diagnosis for CDI in IBD patients are also summarized.
MATERIALS AND METHODS
Data sources and searches
We performed a systematic search of MEDLINE and Ovid EMBASE databases (Figure 1). Eligibility criteria for included studies were decided a priori. Two authors (D’Aoust J and Battat R) independently judged study eligibility. “Clostridium difficile”, “pseudomembranous colitis”, “inflammatory bowel disease”, “Crohn’s disease”, and “ulcerative colitis” were used as search terms. MESH subheadings were combined using the Boolean operators “AND” and “OR” for full articles published in the English language between 1946 and the third week of January 2017. Additional publications were retrieved from included studies and relevant review articles. Publications identified as duplicates were excluded. Cases of disagreement were resolved by discussion and joint analysis of articles by two reviewers (D’Aoust J and Battat R).
Figure 1.
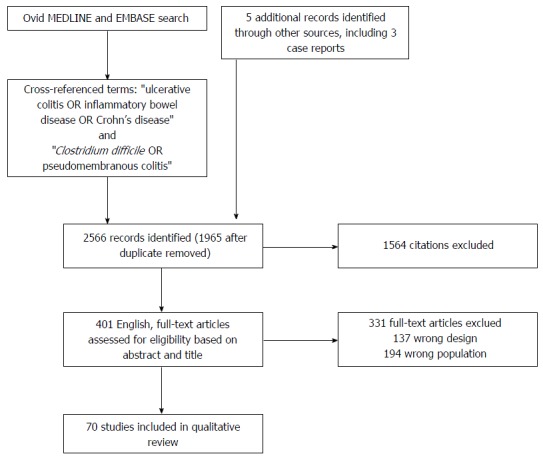
Search strategy for the selection of articles on Clostridium difficile infection in inflammatory bowel disease.
Study selection
Study titles and abstracts obtained from database searches were reviewed to identify those addressing CDI in IBD. Studies analyzing adult and pediatric patients were included. Case reports and case series were included if the management of IBD and CDI was discussed, due to limited data on this topic. Articles not pertaining to this topic in the title or abstract were excluded. Letters, editorials, and review articles were excluded. Data referring to the incidence, risk factors, diagnosis, management, and outcomes of C. difficile infection in patients with IBD were extracted from the articles. Data extraction was performed and agreed on by two authors (D’Aoust J and Battat R).
RESULTS
The search strategy, summarized in Figure 1, revealed 396 full-texts, English-language articles. Sixty-five articles were retained from the database search after applying the exclusion criteria. Two additional articles were retrieved from references. Two case reports discussing the management of CDI with corticosteroids were included. One additional case series on this topic was retrieved from relevant references for inclusion. Articles retained included a total of 932141 IBD patients or IBD-related hospitalizations (526765 UC; 312240 CD; 161 IC; 92 975 not-reported).
DISCUSSION
Epidemiology of CDI in IBD
Both an increasing burden of disease, as well as preponderance for community-acquired infection is reflected in the IBD population. Several studies have documented the changes in CDI epidemiology over time in IBD patients (Table 1). In adult inpatients with IBD, CDI incidence increased two to threefold in the early 2000s and more so in pediatric populations, with the largest rise in incidence among UC patients[16-19]. Several studies demonstrate a disproportionate rise in CDI in the IBD population as compared to the general population[16,17], while others do not[20].
Table 1.
Epidemiology of Clostridium difficile infection in inflammatory bowel disease
| Ref. | Patient population | Sampling time frame | Diagnosis method | Disease activity | Conclusions |
| Keighley[92] (1983) | IBD adult inpatients | 1978-1980 | Stool culture on selective medium + cytotoxicity assay | Active | CDI incidence (%) IBD: 5.7; UC 4.7; CD 6.3 |
| Gurian et al[93] (1983) | IBD adult inpatients and outpatients | 1980-1981 | Stool culture on selective medium + cytotoxicity assay | Active | CDI incidence (%) IBD: 0 |
| Rolny et al[26] (1983) | IBD adult inpatients | 1980-1981 | Stool culture on selective medium + cytotoxicity assay | Active | CDI incidence (%) UC: 5; CD: 7.7 |
| Greenfield et al[21] (1983) | IBD adult inpatients and outpatients | 1980-1981 | Stool culture on selective medium + cytotoxicity assay | Mixed | CDI incidence (%) UC: 13.7; CD: 13.2 |
| Burke et al[94] (1987) | IBD adult outpatients | 1984-1986 | Stool culture on selective medium + cytotoxicity assay | Active | CDI incidence (%) IBD 3.2 |
| Gryboski[95] (1991) | IBD pediatric inpatients and outpatients | 1986-1990 | Stool culture on selective medium + cytotoxicity assay | Active | CDI incidence (%) IBD 16; UC: 18; CD 14 |
| Meyer et al[22] (2004) | IBD adult inpatients and outpatients | 2000-2001 | Immunoassay for Toxin A until 2001 then EIA for Toxin A/B | Active | CDI incidence (%) IBD: 16.7; UC: 12.5; CD: 23.8; IC: 11.1 |
| Mylonaki et al[23] (2004) | IBD adult inpatients and outpatients | 1997-2001 | ELISA for Toxins A/B | Active | CDI incidence (%) IBD: 5.5; CD: 13.2 |
| Issa et al[24] (2007) | IBD adult inpatients and outpatients | 2005 | ELISA for Toxins A/B | Active | CDI incidence (%) UC: 6.1; CD: 4.1 |
| IBD patients accounted for 4% of the total CDI patient cohort in 2003, 7% in 2004, and 16% in 2005 | |||||
| Rodemann et al[16] (2007) | IBD pediatric and adult inpatients (United States) | 1998-2004 | Cell cytotoxic culture | Active | CDI incidence (%) UC: 3.9; CD: 1.6 |
| 2002 onwards C. difficile Toxin A/B immunoassay | CDI incidence increase: UC > CD > non-IBD | ||||
| Non-IBD population: 8.5 to 15.9/1000 admissions | |||||
| CD: 9.5 to 22.3/1000 admissions | |||||
| UC: 18.4 to 57.6/1000 admissions | |||||
| Shen et al[33] (2008) | UC adult outpatients with IPAA | 2005-2006 | ELISA for Toxin A/B | Mixed | CDI incidence (%) UC: 18.3 |
| Bossuyt et al[20] (2009) | IBD and non-IBD CDI adult inpatients | 2000-2008 | EIA for Toxin A until 2005, then EIA for Toxins A/B | Active | All patients: 3.75-fold increase in CDI between 2000-2003 and 2004-2008 |
| Balamurugan et al[96] (2008) | UC adult outpatients | 2004-2005 | PCR for C. difficile | Mixed | CDI incidence (%) UC: 92 |
| Toxin A/B ELISA | |||||
| Ananthakrishnan et al[18] (2008) | IBD and non-IBD CDI adult inpatients | 1998-2004 | N/R | N/R | CDI incidence increase: UC: 24 to 39/1000 discharge ; CD: 8 to 12/1000 discharges |
| Nguyen et al[17] (2008) | IBD and non-IBD adult inpatients | 1998-2004 | N/R | N/R | CDI incidence increase: UC: 26.6 to 51.2/1000 discharges |
| Pascarella et al[35] (2009) | IBD pediatric inpatients | 2005-2007 | Enzyme immunoassay for toxins A/B | Mixed | CDI incidence (%) UC: 21.3; CD: 35 |
| Ricciardi et al[27] (2009) | IBD adult inpatients | 1993-2003 | N/R | Active | CDI incidence (%) UC: 2.8; CD: 1.0 |
| CDI incidence increase: IBD: 12.2 to 21/1000 discharges; CD + colonic involvement: 12.2 to 23.1/1000 discharges | |||||
| Wultańska et al[36] (2010) | IBD pediatric outpatients | 2005-2007 | EIA for Toxins A/B | Mixed | CDI incidence (%) IBD: 60; UC: 61; CD: 59 |
| or PCR | |||||
| Ananthakrishnan et al[58] (2011) | IBD adult inpatients | 1998, 2004, 2007 | N/R | N/R | CDI incidence increase: CD: 0.8 to 1.5% of hospitalizations; UC: 2.4 to 5.3% of hospitalizations |
| Absolute mortality increase in CDI + IBD (5.9% to 7.2%) | |||||
| Kaneko et al[46] (2011) | UC pediatric and adult inpatients and outpatients | 2006-2009 | ELISA for Toxin A | Active | CDI incidence (%) UC inpatient: 36.6; UC outpatient: 41.7 |
| Mezoff et al[37] (2011) | IBD pediatric patients | 2007-2008 | EIA for Toxins A and B | Mixed | CDI incidence (%) UC: 5.8; CD: 7.8; IC: 11.1 |
| Ott et al[28] (2011) | IBD adult inpatients | 2001-2008 | ELISA for Toxins A/B or characteristic histology | Active | CDI incidence (%) IBD: 4.0; CD: 13.2; UC: 4.7 |
| Banaszkiewicz et al[38] (2012) | IBD pediatric inpatients | 2007-2010 | EIA for Toxins A and B | Mixed | CDI incidence (%) IBD: 47 |
| Antonelli et al[29] (2012) | IBD adult inpatients | 2007-2010 | N/R | Active | CDI incidence (%) UC: 11.1; CD: 1.7 |
| Murthy et al[31] (2012) | UC adult inpatients | 2002-2008 | N/R | Active | CDI incidence (%) UC: 9.0 |
| Lamousé-Smith et al[97] (2013) | IBD pediatric inpatients and outpatients (United States) | 2006-2012 | PCR for Toxin B +/- ELISA for Toxin A/B | Mixed | CDI incidence (%) UC: 18.4; CD: 11.6 |
| Masclee et al[47] (2013) | IBD adult outpatients | 2009-2010 | PCR for C. difficile and Toxin A/B | Active | CDI incidence (%) IBD: 4.9; UC: 3.4; CD: 5.9 |
| Mir et al[39] (2013) | IBD pediatric patients | 2010-2012 | EIA or PCR for Toxin A/B | N/R | CDI incidence (%) IBD: 8.1; UC: 5.6; CD: 9.3 ; IBDU: 11.1 |
| No significant variation in IBD incidence over 3 yr | |||||
| Pant et al[98] (2013) | IBD pediatric inpatients | 2000, 2003, 2006, 2009 | N/R | N/R | CDI incidence increase: IBD: 21.7 to 28 cases/1000 IBD cases per year; UC: 28.1 to 42.2/1000 cases per year; CD: 18.3 to 20.3/1000 cases per year |
| Li et al[34] (2013) | IBD adult outpatients with IPAA | 2010-2011 | PCR for Toxin B gene | Active | CDI incidence (%) IBD: 10.7; UC: 10.4; CD: 0; IC: 25.0 |
| Martinelli et al[40] (2014) | IBD pediatric inpatients and outpatients | 2010-2011 | EIA for Toxins A/B | Mixed | CDI incidence (%): IBD: 10.0; UC: 7.5; CD: 11.9 |
| Regnault et al[30] (2014) | IBD adult inpatients | 2008-2010 | Stool culture on selective medium + cytotoxicity assay +/- toxigenic culture | Active | CDI incidence (% hospitalizations): IBD: 7.0; UC: 6.8; CD: 7.2 |
| Negrón et al[32] (2014) | UC adult inpatients | 2000-2009 | EIA for Toxins A/B | Active | CDI incidence (%) UC: 6.1 |
| Hourigan et al[99] (2014) | IBD and non-IBD pediatric and adult inpatients | 1993-2012 | N/R | N/R | CDI incidence increase: IBD: 19.9 to 67/1000 admissions |
| Rate of increase in CDI not significantly different between patients with or without IBD | |||||
| Krishnarao et al[25] (2015) | IBD adult inpatients and outpatients | 2008-2011 | EIA and PCR | Mixed | CDI incidence (%) IBD: 5.1 |
| Sandberg et al[19] (2015) | IBD pediatric inpatients | 1997-2011 | N/R | N/R | Hospitalization rate increase: CDI + IBD: 2.8 to 14.4 per million population per year |
| Rate of increase for UC + CDI = CD + CDI | |||||
| Simian et al[100] (2016) | IBD adult and pediatric inpatients and outpatients | 2014-2015 | PCR | N/R | CDI incidence (%) UC: 5.0; CD: 5.0 |
| Roy et al[101] (2016) | CD adult outpatients on chronic antibiotic therapy > 6 mo | 1992-2015 | N/R | N/R | CDI incidence (%) CD: 2.0 |
IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s Disease; IC: Indeterminate colitis; IBDU: Inflammatory bowel disease unclassified; IPAA: Ileal anal-pouch anastomosis; EIA: Enzyme immunoassay; ELISA: Enzyme linked immunosorbent assay; PCR: Polymerase chain reaction ; N/R: Not reported.
The epidemiological studies of CDI in IBD are heterogeneous with regards to patient population, disease activity, sampling time frame, and diagnostic assay sensitivity. Reported incidences of CDI in pediatric and adult populations reflect this heterogeneity (Table 1). In mixed inpatient and outpatient adult IBD populations, the incidence of CDI ranges between 5.1%-16.7%[21-25].
Studies report the incidence of CDI in CD adult inpatients between 1.0 and 7.7%[26-30]. In adult UC inpatients, the incidence of CDI ranges from 2.8% to 11.1%[26-32]. In adult outpatients with ileal-anal pouch anastomosis (IPAA) for IBD, incidence of CDI is 10.7%-18.3%[33,34]. The incidence of CDI in IBD among pediatric patients is 7.8%-69%, similarly with a higher incidence among patients with UC as opposed to CD[35-40].
Risk factors for CDI in IBD
In patients with CDI and IBD, risk factors are categorized into environmental and host risk factors, including those specific to IBD. Several studies have demonstrated that IBD itself is an independent risk factor for CDI in both adult and pediatric populations[16,35,41].
In the general population, many host and environmental risk factors have been identified. These include antibiotic exposure, specifically broad-spectrum antibiotics, as well as recent hospitalization, immunosuppression, increased age, and comorbidities[42].
In IBD populations, risk factors for CDI appear to be partly distinct (Table 2). Evidence is contradictory regarding antibiotic use as a risk factor for CDI in IBD patients. Three retrospective studies identified recent antibiotic use as a risk factor for CDI and recurrent CDI in both CD and UC[23,43,44]. In one study, antibiotic exposure within 30 d prior to C. difficile testing was associated with a twelve-fold risk of CDI in UC patients (95%CI: 1.2-124.2)[43]. Several others contradict this[30,34,35,43,45-47]. Scarce evidence supports nonsteroidal anti-inflammatories (NSAIDs) and proton pump inhibitors (PPIs) as risk factors for CDI in IBD. One retrospective cohort study of 480 IBD patients hospitalized for a flare who also underwent C. difficile testing, describes NSAID use within two months prior to admission as a predisposing factor for CDI (OR = 3.8, 95%CI: 1.2-12.3, P = 0.02)[30]. No studies have identified gastric acid-suppressive therapy as a risk factor for CDI in the IBD population[30,34,43-46].
Table 2.
Risk factors for Clostridium difficile infection in inflammatory bowel disease
| Ref. | Sampling time frame | Setting | Diagnosis method |
Identified risk factors |
|
| HOST | ENVIRONMENT | ||||
| Razik et al[44] (2016) | 2010-2013 | Inpatient | PCR | Non-ileal CD | Hospitalisation for CDI; recent antibiotic use; biologic therapy; 5-ASA; Steroids |
| McCurdy et al[54] (2016) | 2005-2011 | Inpatient and outpatient | PCR | CMV infection | N/A |
| Seril et al[45] (2014) | 2010-2013 | Inpatient and outpatient | PCR for Toxin B | Post-surgery mechanical intestinal complications; low serum immunoglobulin level | None identified |
| Regnault et al[30] (2014) | 2008-2010 | Inpatient | Stool culture on selective medium + cytotoxicity assay +/- toxigenic culture | None identified | NSAIDs |
| Connelly et al[52] (2014) | N/R | N/R | PCR for Toxin A gene | IL-4 gene associated SNP rs2243250 | Not studied |
| Ananthakrishnan et al[102] (2014) | 1998-2010 | Inpatient | N/R | Low vitamin D concentration | Not studied |
| Ananthakrishnan et al[56] (2013) | N/R | Inpatient and outpatient | ELISA for Toxin A/B | Female sex; pancolitis; IBD-related SNPs | Protective : Anti-TNF therapy |
| Monaghan et al[53] (2013) | 2009-2012 | N/R | Toxigenic culture | Impaired ability to generate: toxin-specific antibody, memory B-cell responses | Not studied |
| Li et al[34] (2013) | 2010-2011 | Outpatient | PCR for Toxin B | None identified | Recent hospitalization |
| Masclee et al[47] (2013) | 2009-2010 | Outpatient | PCR for C. difficile and Toxins A/B | None identified | None identified |
| Kaneko et al[46] (2011) | 2006-2009 | Inpatient and outpatient | ELISA for Toxin A | None identified | None identified |
| Kariv et al[43] (2011) | 2000-2006 | Inpatient and outpatient | EIA for Toxin A/B | Recent surgery | Recent antibiotic use; recent hospitalization |
| Ricciardi et al[27] (2009) | 1993-2003 | Inpatient | N/R | Colonic involvement | Not studied |
| Schneeweiss et al[49] (2009) | 2001-2006 | Inpatient and outpatient | N/R | Not studied | Corticosteroid initiation |
| Nguyen et al[17] (2008) | 1998-2004 | Inpatient | N/R | Colonic involvement | Not studied |
| Comorbidity | |||||
| Issa et al[24] (2007) | 2005 | Inpatient | ELISA for Toxin A/B | Colonic involvement | Maintenance immunomodulator use |
| Rodemann et al[16] (2007) | 1998-2004 | Inpatient | Cell cytotoxic culture | Age | Not studied |
| 2002 onwards C. difficile Toxin A/B immunoassay | Comorbidity | ||||
| Mylonaki et al[23] (2004) | 1997-2001 | Inpatient | ELISA for Toxin A/B | None identified | Recent antibiotic use |
CDI: Clostridium difficile infection; rCDI: Recurrent Clostridium difficile infection; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s Disease; IPAA: Ileal anal-pouch anastomosis; CMV: Cytomegalovirus; CF: Cystic fibrosis; EIA: Enzyme immunoassay; ELISA: Enzyme linked immunosorbent assay; NSAID: Non-steroidal anti-inflammatories PCR: Polymerase chain reaction; N/R: Not reported.
Most studies demonstrate ongoing steroid, biologic, or immunomodulator therapy does not increase the risk of CDI in IBD patients[30,34,35,43,45-47], however, some contradictory evidence exists. A retrospective cohort study of 999 IBD inpatients (737 CD and 262 UC) report a greater than two-fold increased risk of CDI with maintenance immunomodulator use, defined as azathioprine, 6-mercaptopurine, or methotrexate (OR = 2.56, 95%CI: 1.28-5.12, P = 0.008)[24]. In the general population, corticosteroid use increases the risk of CDI[48]. However, when analyzing CDI risk in IBD patients using corticosteroids, studies were observational and did not control for underlying disease activity. A large retrospective cohort study of 10662 IBD inpatients noted a greater than three times increased risk of CDI within 90 d of corticosteroid initiation (RR = 3.4; 95%CI: 1.9-6.1) but no increased risk with preceding biologic therapy. This risk remained constant after 90 d of corticosteroid therapy and was not dose-dependent[49]. Risk factors for recurrent CDI (rCDI), in addition to recent antibiotic use, included preceding steroid and biologic therapy. However, when further stratified, rCDI was associated with infliximab use but not adalimumab or immunomodulator therapy[44].
Although there appears to be more community-acquired CDI in the IBD population compared to the general population, recent hospitalization has also been identified as a risk factor for CDI and rCDI[43,44]. Patients who have undergone colectomy are still at risk of CDI. Ten point seven percent of symptomatic IBD patients with ileal anal-pouch anastomosis (IPAA) were found to be positive for C. difficile toxin in a prospective cohort of 196 patients[34]. A retrospective observational study of 284 UC patients who underwent IPAA found that 64 patients developed pouchitis. Three of the four patients in this cohort with antibiotic-refractory pouchitis were discovered to have CDI that responded to oral vancomycin[50].
Genetic and immunologic risk factors have been identified in IBD patients for the development of CDI[51]. In a retrospective cohort study of 172 IBD patients, an interleukin-4-associated single nucleotide polymorphism (rs2243250) is associated with CDI in IBD[52]. Monaghan et al[53] studied the humoral response to C. difficile toxins A and B in patients with IBD, cystic fibrosis, and healthy controls, finding that an impaired ability to sustain or generate strong toxin-specific antibody and B-cell responses could play a role in CDI development in IBD patients. Furthermore, low serum immunoglobulins were reported as a risk factor for CDI in IBD patients with IPAA[34]. A retrospective case control study of 306 IBD inpatients and outpatients, found that those with CMV infection were at higher risk of being co-infected with C. difficile[54]. As in the general population, patient comorbidities increase the risk of CDI in the IBD population[16,17,55]. While adult IBD patients affected by CDI are younger than those in the general population, increasing age has also been reported as a risk factor for CDI[16].
IBD disease activity is difficult to differentiate from CDI. Therefore, it is not clear that disease activity is an independent risk factor for the development of CDI. Disease location may affect patient risk. CDI is more often identified in those with UC and CD patients with colonic involvement[16,24]. In a retrospective nested case-control analysis of a national hospital discharge database, the prevalence of CDI among IBD patients with only small bowel disease was significantly lower than UC patients or CD patients with ileocolonic disease and only slightly higher than non-IBD patients[17]. Extent of disease in UC patients may be a risk factor for CDI. A prospective cohort study of 319 UC patients found pancolitis to be a risk factor for CDI (OR = 2.52, 95%CI: 1.03-6.17)[56].
Impact of CDI in IBD
CDI negatively impacts short and long-term IBD-related outcomes, including rates of colectomy, escalation in IBD therapy, and mortality. It also results in longer hospitalizations, increased readmission rates, and increased in-hospital expenditures (Table 3).
Table 3.
Outcomes of inflammatory bowel disease patients with Clostridium difficile infection
| Ref. | Patient population | Sampling time frame | Study design | n | Outcomes |
| Razik et al[44] (2016) | Adult CDI | 2010-2013 | Retrospective, single-center, cohort study | 503 | Incidence of rCDI |
| IBD + CDI | IBD > non-IBD [2.04/100 person-months (95%CI: 1.55-2.64) vs 1.25 episodes per 100 person-months (95%CI: 1.05-1.48)] | ||||
| Inpatient | Colectomy | ||||
| IBD > non-IBD (6.4% vs 0.3%) | |||||
| Skowron et al[61] (2016) | Adult IBD + IPAA | 2000-2010 | Retrospective, observational, single-center cohort study | 417 | CDI pre-colectomy associated with post-reconstruction pouch failure (HR = 3.02 95%CI: 1.23-7.44) |
| Inpatient (United States) | |||||
| McCurdy et al[54] (2016) | Adult IBD | 2005-2011 | Retrospective, case-control, single-center, study | 248 | Colectomy-free survival at 1 yr |
| IBD + CMV | IBD + CDI > IBD + CMV + CDI (71.5% vs 30%) | ||||
| IBD + CMV + CDI | IBD + CMV controls > IBD + CMV + CDI (57.1% vs 30%) | ||||
| IBD + CDI | |||||
| Inpatient and outpatient (United States) | |||||
| Negrón et al[32] (2014) | Adult UC | 2000-2009 | Retrospective, case-control, multi-center, database study | 481 | Emergent surgery |
| Inpatient (Canada) | CDI + UC > UC alone [OR = 3.39 (95%CI: 1.02-11.23)] | ||||
| Development of new infectious postoperative complication | |||||
| CDI + UC > UC alone (OR = 4.76, 95%CI: 1.10-20.63) | |||||
| Horton et al[70] (2014) | Adult IBD | 2006-2010 | Retrospective, observational, single-center study | 114 | Readmission: |
| Inpatient (United States) | UC + CDI > CD + CDI (24% vs 10%, P = 0.04) | ||||
| IBD + steroids > no-steroids (29% vs 8%, P < 0.01) | |||||
| Colectomy: | |||||
| UC + CDI > CD + CDI, index admission (27.4% vs 0%, P < 0.01) | |||||
| IBD + steroids > no-steroids (32% vs 6%, P < 0.01) | |||||
| Pant et al[98] (2013) | Pediatric IBD | 2000, 2003, 2006, 2009 | Retrospective, nested case-control, nationwide database study | 12610 | LOS: |
| Inpatient (United States) | CDI + IBD > IBD (8.0 vs 6.0, aRC = 2.1 d, 95%CI: 1.4-2.8) | ||||
| Hospitalization cost: | |||||
| CDI + IBD > IBD alone ($45126 vs $34703, aRC = $11506, 95%CI: 6192-16829) | |||||
| Parenteral nutrition: | |||||
| CDI + IBD > IBD alone (15.9% vs 12.1% aOR = 1.5, 95%CI: 1.1-2.0) | |||||
| Blood transfusions: | |||||
| CDI + IBD > IBD alone (17.7% vs 9.8%, aOR = 1.8, 95%CI: 1.4-2.4). | |||||
| Li et al[34] (2013) | Adult IBD + IPAA | 2010-2011 | Prospective, single-center, cohort study | 196 | 42.9% cured by single course of Vancomycin |
| Outpatient (United States) | 57.1% recurrent/refractory CDI | ||||
| Chu et al[103] (2013) | Adult UC + CDI | 2002-2012 | Retrospective, single-center, observational study | 23 | Morbidity and mortality after colectomy: |
| Inpatient (United States) | UC + CDI + full antibiotic course pre-op = UC + CDI + incomplete antibiotic course pre-op | ||||
| Ananthakrishnan et al[55] (2013) | Adult IBD | 2007 | Retrospective, nested case-control, nationwide database study | 67221 hospitalizations | Mortality: |
| Inpatient (United States) | CDI + IBD vs IBD alone (OR = 3.23, 95%CI: 2.55-4.03). | ||||
| Murthy et al[31] (2012) | Adult UC | 2002-2008 | Retrospective, database, cohort study | 2016 | Mortality: |
| Inpatient (Canada) | CDI + UC > UC alone, 5-yr risk (aHR = 2.40, 95%CI: 1.37-4.20) | ||||
| CDI + UC > UC alone, index hospitalization (aHR = 8.90, 95%CI: 2.80-28.3) | |||||
| CDI + UC > UC alone, 5 years post-discharge (aHR = 2.41, 95%CI: 1.37-4.22) | |||||
| Navaneethan et al[60] (2012) | Adult UC | 2002-2007 | Retrospective, single-center, cohort study | 146 | UC-related ER visits: |
| Inpatient and outpatient (United States) | CDI + UC vs UC alone, 1 yr post index infection (37.8% vs 4%, P < 0.001) | ||||
| Colectomy: | |||||
| CDI + UC vs UC alone, 1 yr post index infection (35.6% vs 9.9%, P < 0.001) | |||||
| CDI associated with colectomy within 1 yr (OR = 10, 95%CI: 2.7-36.3) | |||||
| Escalation in therapy: | |||||
| CDI + UC year after CDI admission vs year prior (55.8% vs 12.9%, P < 0.0001) | |||||
| Jen et al[57] (2011) | Adult IBD | 2002-2008 | Retrospective, nested case-control, nationwide database study | 241478 hospitalizations | Mortality: |
| Inpatient (England) | IBD + CDI (defined as hospital-acquired > IBD alone (aOR = 6.32, 95%CI: 5.67-7.04) | ||||
| LOS: | |||||
| IBD + CDI > IBD alone (27.9 d longer) | |||||
| GI surgery: | |||||
| IBD + CDI > IBD alone (aOR = 1.87, 95%CI: 0.60-5.85) | |||||
| Kariv et al[43] (2011) | Adult UC | 2000-2006 | Single-center | 78 | Colectomy within 3 mo not associated with CDI |
| Inpatient and outpatient (United States) | No UC or CDI associated mortality identified | ||||
| Ananthakrishnan et al[58] (2011) | Adult IBD | 1998, 2004, 2007 | Retrospective, nested case-control, nationwide database study | - | Mortality: |
| Inpatient (United States) | IBD + CDI > IBD alone, from 1998 to 2007 (OR = 2.38, 95%CI: 1.52-3.72 to OR = 3.38, 95%CI: 2.66-4.29). | ||||
| Kelsen et al[62] (2011) | Pediatric IBD | 1997-2007 | Retrospective, nested case-control, single-center study | 315 | rCDI: |
| Inpatient (United States) | CDI + IBD > CDI-alone (34% vs 7.5%, P < 0.0001) | ||||
| Escalation in therapy: | |||||
| IBD + CDI > IBD alone (67% vs 30%, P < 0.001) | |||||
| Jodorkovsky et al[59] (2010) | Adult UC | 2004-2005 | Retrospective, single-center, case-control study | 99 | UC-related hospitalizations: |
| Inpatient (United States) | CDI + IBD > IBD alone, over 1 yr | ||||
| Colectomy: | |||||
| CDI at index admission predictor for colectomy within 1 yr (OR = 2.38, 95%CI: 1.01-5.6) | |||||
| CDI status not a significant predictor for requirement for emergent colectomy at index admission | |||||
| LOS: | |||||
| CDI + IBD = IBD alone | |||||
| Ben-Horin et al[64] (2010) | Adult IBD + CDI | 2000-2008 | Retrospective, multi-center, cohort study | 93 | Morbidity and mortality: |
| Inpatient (Europe/Israel) | IBD + CDI patients + pseudomembranes on endoscopy = IBD + CDI without pseudomembranes | ||||
| Nguyen et al[17] (2008) | IBD and non-IBD controls | 1998-2004 | Retrospective, nested case-control, nationwide database study | 116842 hospitalizations | Mortality: |
| Inpatient (United States) | UC + CDI > CDI alone (OR = 3.79, 95%CI: 2.84-5.06) | ||||
| LOS: | |||||
| CD + CDI > CDI alone | |||||
| Hospitalization cost: | |||||
| UC + CDI > CDI alone |
CDI: Clostridium difficile infection; rCDI: Recurrent clostridium difficile infection; IBD: Inflammatory bowel disease; UC: Ulcerative colitis; CD: Crohn’s disease; IPAA: Ileal anal-pouch anastomosis; CMV: Cytomegalovirus; OR: Odds ratio; aOR Adjusted odds ratio; aRC: Adjusted regression coefficient; LOS: Length of stay.
Increased mortality among IBD patients with CDI has been reported in numerous adult inpatient studies compared to non-IBD patients with CDI[17] and IBD patients without CDI[31,55,57,58]. Furthermore, it appears that this excess mortality is not limited to the index hospitalization. A retrospective cohort study of 2016 adult UC inpatients described increased mortality among patients with CDI compared to those without CDI in the five years post-discharge (HR = 2.41, 95%CI: 1.37-4.22)[31].
Colectomy rates have been reported to be higher in IBD patients with CDI. A retrospective case control study of 99 adult UC inpatients reported CDI at index admission significantly predicted colectomy within one year[59]. Higher rates of colectomy among IBD patients with CDI have been similarly reported in other large adult inpatient studies compared to non-IBD patients with CDI (6.4% vs 0.3%)[44] and IBD patients without CDI (OR = 1.87-10.0) [32,57,59,60] during index admission and up to one year following the initial episode.
IPAA failure also is associated with a history of CDI. A retrospective chart-review study of 417 IBD patients undergoing IPAA found that a history of CDI prior to colectomy in IBD patients was independently associated with IPAA failure (HR = 3.02, 95%CI: 1.23-7.44)[61].
While CDI alone is associated with significant morbidity and mortality, it is thought that CDI may actually lead to a flare in IBD activity resulting in further morbidity. This is supported by a retrospective cohort study of 146 adult UC inpatients and outpatients reporting increased escalation in therapy among patients with CDI in the year after index admission compared to the year prior[60]. A retrospective nested case control study of 238 pediatric IBD inpatients with and without CDI similarly demonstrated significant escalation in therapy among those with CDI as compared to those without after the infection[62].
Diagnosis of CDI in IBD
The overlap in symptomatology between CDI and isolated IBD flare complicates the diagnosis of CDI in IBD patients. CDI and acute inflammatory colitis are clinically indistinguishable. Therefore, a diagnosis relies primarily on laboratory findings, and to a lesser degree endoscopic or histologic findings.
It is recommended to test all patients with acute flares presenting with diarrhea for CDI[63]. Despite its impact on outcome and management, many patients with newly diagnosed IBD or flaring IBD are not tested for CDI. A retrospective cohort study of adult IBD inpatients report that C. difficile testing within 48 h for patients hospitalized for an IBD flare was only performed on 59% of 813 consecutive hospitalizations. A diagnosis of UC or CD with colonic involvement was noted to be independent predictors of CDI testing[30]. In a retrospective cohort study of pediatric patients with newly diagnosed IBD, only 42% of 290 cases had testing for C. difficile around the time of diagnosis[39].
Compared to previously discussed diagnostic methods, pseudomembranes on colonoscopy are specific but not sensitive to diagnose CDI in IBD patients. In a multi-center retrospective study of 93 IBD patients hospitalized with CDI who underwent colonoscopy, only 13% were noted to have pseudomembranes. The presence of pseudomembranes was not found to significantly impact clinical outcomes[64]. A retrospective case-control study of CDI in IBD and non-IBD patients found that none of the IBD-CDI patients had pseudomembranes on endoscopy compared to nearly half of the non-IBD-CDI group[20]. A retrospective study of 37 flaring UC patients assessed histological changes on colonic biopsies with or without CDI. They reported that although those with CDI had significantly more microscopic pseudomembranes than the controls without CDI, less than half of the specimens of CDI patients had this finding[65].
Testing via PCR should only be performed on unformed stools to limit false positives. Asymptomatic carriers of toxigenic C. difficile exist in both IBD patients and the general population. Asymptomatic carriage rates vary significantly with the patient population under study[66]. A rate of 8.2% has been reported in an adult outpatient IBD population with stable disease compared to 1.0% in healthy controls, with higher rates in UC patients compared to those with CD[67]. A prospective case-control study of 163 pediatric outpatients reports a significantly higher carriage rate in those with IBD than in healthy controls (17% vs 3%), which was not associated with recent hospitalization[68]. There are no studies evaluating treatment of the asymptomatic carriage of C. difficile. Evidence is lacking to suggest that treating asymptomatic C. difficile carriers has any future impact on IBD disease activity or the development of symptomatic CDI. However, in the general population, carriage of C. difficile in the absence of symptoms carries a protective effect against future symptomatic CDI[7]. This protective effect has not been studied in the IBD population.
It has been demonstrated that the asymptomatic shedding of C. difficile spores can continue for weeks following the resolution of symptoms[69]. Therefore, test of cure is not recommended. However, in patients with IBD and CDI where symptom overlap creates both diagnostic and therapeutic challenges, repeat testing in patients with ongoing diarrhea may guide management, despite the risk of false-positive results.
Treatment of CDI in IBD patients
In patients with confirmed CDI, distinguishing between symptoms resulting from infection, as opposed to a flare of underlying IBD, creates a management dilemma. There are no randomized controlled trials (RCT) of therapy in IBD patients with CDI to help guide practice. Guidelines outlining the approach to eradication of C. difficile via antibiotic therapy or fecal microbiota transplant (FMT) in the setting of recurrent CDI also include recommendations for the IBD population[3]. IBD outpatients with non-severe CDI can be initially treated with metronidazole, however IBD inpatients regardless of disease severity should receive a vancomycin-containing regimen as first-line therapy (Table 4)[70]. In addition to medical therapy, specific infection control measures should also be put in place, including hand-washing to minimize fecal-oral transmission of C. difficile spores, as well as isolation of patients with CDI under contact-precautions.
Table 4.
| Severity | Criteria | Treatment | Comments |
| First episode | |||
| Stop all non-CDI related antibiotic therapy if possible | |||
| Mild to moderate disease | Diarrhea and symptoms not meeting criteria for severe disease | Metronidazole 500 mg by mouth 3 times per day for 10 d to 14 d | In hospitalized patients with UC and nonsevere CDI, treatment with a vancomycin-containing regimen vs metronidazole alone resulted in fewer readmissions and shorter LOS[70] |
| or | |||
| Vancomycin 125 mg by mouth 4 times per day for 10 to 14 d | |||
| Severe disease | Serum albumin < 3 g/dL AND one of the following: | Vancomycin 125 mg by mouth 4 times per day for 10 to 14 d | |
| WBC ≥ 15000 cells/mm3 | |||
| Abdominal tenderness | |||
| Creatinine ≥ 133 μmol/L | |||
| Severe, complicated disease | Admission to intensive care unit | Vancomycin 500 mg by mouth or nasogastric tube 4 times per day | Consider early surgical consultation |
| Hypotension ± vasopressor requirement | and | ||
| Fever ≥ 38.5 °C | Metronidazole 500 mg IV every 8 h | ||
| Ileus | and, if ileus, | ||
| Mental status changes | Vancomycin 500 mg in 500 mL saline as enema 4 times per day | ||
| WBC ≥ 35000 cells/mm3 or ≤ 2000 cells/mm3 | |||
| Serum lactate ≥ 2.2 mmol/L | |||
| End organ failure | |||
| Recurrent CDI | |||
| First recurrence | Metronidazole 500 mg by mouth 3 times per day for 10 to 14 d | ||
| or | |||
| Vancomycin 125 mg by mouth 4 times per day for 10 to 14 d | |||
| or | |||
| Fidaxomicin 200 mg by mouth 2 times per day for 10 d | |||
| Second recurrence | -Tapered and pulsed vancomycin | ||
| or | |||
| Fidaxomicin 200 mg by mouth 2 times per day for 10 d | |||
| Subsequent recurrence | -Fecal microbiota transplant | ||
LOS: Length of stay; CDI: Clostridium difficile infection; UC: Ulcerative colitis.
Management of IBD flares in patients with CDI
While the treatment of isolated CDI is well studied, the initiation, maintenance or escalation of corticosteroid, immunomodulator or biologic therapy in IBD patient with CDI is not delineated and relies heavily on expert opinion.
Corticosteroids
In the setting of suspected IBD flare in a patient with known CDI, concurrent corticosteroid therapy is reasonable and supported by expert opinion[3,71]. Nevertheless, significant uncertainty exists among practitioners with regards to the initiation of corticosteroid therapy and its safety in the context of an ongoing CDI-mediated colitis. A survey of 169 North American gastroenterologists demonstrated divergence among clinicians with regards to initiating therapy in hospitalized UC patients with CDI; 54% opted for antibiotic monotherapy compared to 46% opting for a combination of antibiotics with either azathioprine or corticosteroids[71]. This concern originates from findings of several observational studies, detailed above, demonstrating increased risk of CDI, rCDI, and worse outcomes among IBD patients receiving corticosteroids[44,49,70]. However, these patients were receiving corticosteroids prior to CDI, and no analysis has been performed for initiation of corticosteroids in IBD patients with CDI on appropriate antimicrobial therapy.
Literature on initiating corticosteroids for IBD flares in patients with concomitant CDI is limited to case reports yielding promising results with patients experiencing remission of symptoms after starting corticosteroid therapy when appropriate antibiotics had failed to do so (Table 5). Similarly, data regarding the initiation of corticosteroids in patients with CDI in the general population is scarce. Corticosteroids have been successfully used as adjunctive therapy to antibiotics in infectious processes such as meningitis, pneumonia, and sepsis[72-74]. While the benefit of corticosteroids seen in these infections may not predict an effect in CDI, it does confer biologic plausibility.
Table 5.
Case reports of corticosteroid initiation in Clostridium difficile infection
| Reference (year of publication) |
Patient data |
Treatment regimen | Outcome | |
| Demographics | Clinical presentation | |||
| Cavagnaro et al[104] (2003) | 5M | Bloody diarrhea (> 10 loose stools/d), tenesmus, abdominal tenderness, fever | Oral vancomycin (40 mg/kg per day divided in 6-hourly doses) and IV metronidazole (20 mg/kg per day divided in 8-hourly doses) × 14 d | Resolution of diarrhea within 24 h of steroid initiation |
| WBC 19000 cells/mm3, albumin 21 g/L | Resolution of endoscopic changes at 6 wk | |||
| Positive C. difficile toxin | IV methyldrnisolone (2 mg/kg per day in two divided doses) on day 14 × 3 d | |||
| Pseudomembranous colitis on flexible sigmoidoscopy on day 14 | Prednisone 2 mg/kg per day tapered over one month | |||
| Sykes et al[105] (2012) | 54F | Moderate CDI that resolved with 10-d course antibiotics | Oral metronidazole × 10 d with resolution of symptoms (doses not specified) | Decreased stool frequency, normalization of vital signs, reduction in CRP to 132 within 48 h of steroid initiation |
| Recurrent diarrhea and abdominal pain 10 d after completion of antibiotics with | Resolution of diarrhea, further reduction in CRP to 15 after 9 d of steroid therapy | |||
| left colonic thickening on CT and positive C. difficile toxin | Oral vancomycin and metronidazole upon admission (doses not specified) × 4 d | Resolution of endosocopic changes at 1 mo | ||
| Fever, tachycardia on day 4 | Sustained clinical response at 5 mo | |||
| with pseudomembranous colitis on flexible sigmoidoscopy | Oral vancomycin 125 mg every 6 h × 9 d | |||
| CRP increased from 149 on admission to 236 on day 4 | IV hydrocortisone 100 mg every 6 h × 9 d | |||
| Prednisolone 30 mg daily with tapering regimen | ||||
| 73F | Moderate-severe CDI that resolved with 10-d course antibiotics | Metronidazole 400 mg every 8 h × 10 d with resolution of symptoms | Resolution of diarrhea, normalization of vital signs, reduction in CRP to 7 within 48 h of steroid initiation | |
| Recurrent moderate CDI 1 wk after completion of antibiotics that resolved with another 10-d course of antibiotics | Complete clinical response at 14 d with no further relapses | |||
| Recurrent CDI 10 d after completion of antibiotics with fever, tachycardia, increased CRP 87 | Oral vancomycin 125 mg every 6 h × 10 d with resolution of symptoms | |||
| Slow response to antibiotics with flexible sigmoidoscopy on day 8 with pseudomembranous colitis | ||||
| Oral vancomycin 125 mg every 6 h × 8 d with tapering regimen over 14 d | ||||
| Prednisolone 30 mg daily × 7 d followed by tapering regimen | ||||
| 91F | Moderate CDI with persistent diarrhea despite courses of metronidazole and vancomycin | Oral metronidazole 400 mg every 8 h × 10 d without resolution of symptoms | Resolution of diarrhea and normalization of CRP within 72 h of steroid initiation | |
| CRP 11 | No further relapses | |||
| Flexible sigmoidoscopy with pseudomembranous colitis | Oral vancomycin 125 mg every 6 h for prolonged course without resolution of symptoms | |||
| Prednisolone 30 mg daily × 14 d with continued vancomycin tapering regimen over 4 wk | ||||
CDI: Clostridium difficile infection; CRP: C-reactive protein.
Conversely, a European retrospective, non-randomized, multi-center study of 155 IBD patients hospitalized with CDI evaluated the effects of antibiotics and immunomodulators compared to antibiotics alone. Immunomodulators were defined as any of the following: corticosteroids at a dose equal to or above 20 mg of prednisone daily, thiopurines at any dose, methotrexate, cyclosporine, tacrolimus, or biologics of any kind. Furthermore, there was no indication of whether therapy was for induction or maintenance of IBD. Conclusions are thus limited by the heterogeneity in the definition of immunomodulator use and antibiotic regimens. Nonetheless, combination of antibiotic and immunomodulator therapy was associated with higher morbidity and mortality compared to antibiotic monotherapy[75]. Most recent AGA practice guidelines suggest postponing escalation of steroids in the setting of acute CDI until 72 to 96 h after the initiation of appropriate antibiotic therapy. However, they refrain from providing further guidance on when to withhold, continue, or escalate corticosteroid therapy given the current absence of prospective data[76].
Immunomodulators and biologic therapy
Recent CDI guidelines suggest, in IBD patients with CDI, maintaining, but not escalating, existing immunosuppressive therapy, including immunomodulators such as azathioprine and methotrexate, as well as biologic agents[3]. Guidelines for the management of opportunistic infections in IBD make no explicit recommendations regarding these therapies in this setting, citing the lack of data available[77]. As described above, conflicting evidence exists regarding immunomodulator and biologic therapies as risk factors for the development of CDI or rCDI. No published data exists regarding when initiation of immunomodulating therapy or biologic therapy is safe in patients with both IBD and CDI. In a study of 14 pediatric patients with predominantly CD being treated with methotrexate and anti-TNF therapy, four patients developed CDI. They were treated with antibiotics with successful clearance of C. difficile but ultimately failed combination therapy[78]. It is difficult to draw conclusions regarding the safety of biologic and immunomodulator therapy from this due to the sample size. Figure 2 summarizes our approach to the patient with IBD who presents with an acute flare in symptoms for which a C. difficile assay is sent, based on existing literature.
Figure 2.
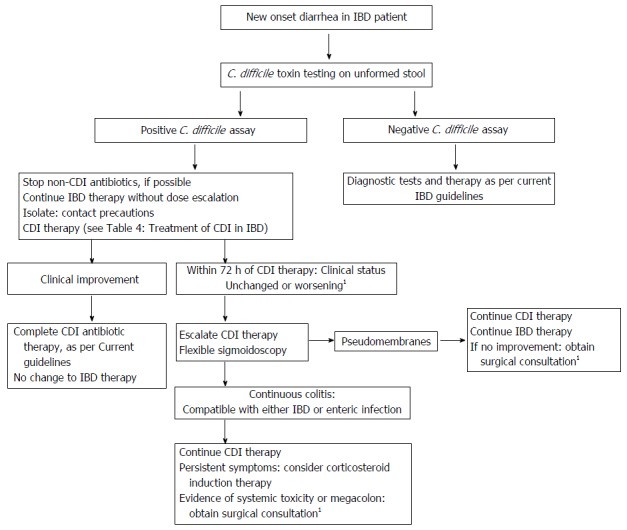
Approach to potential Clostridium difficile infection in inflammatory bowel disease patients. 1Obtain surgical consultation earlier, as dictated by CDI guidelines, should there be evidence of toxic megacolon, or concern for rapid deterioration despite medical therapy. CDI: Clostridium difficile infection; IBD: Inflammatory bowel disease.
Fecal microbiota transplant and recurrent CDI
Existing therapeutic options for rCDI in the general population include vancomycin pulsed and tapered regimens, fidaxomicin, as well as fecal microbiota transplant (FMT). FMT is appealing given the potential to treat both CDI and IBD simultaneously. The risk of rCDI increases with each episode and is higher in IBD patients, as demonstrated in a large retrospective cohort study (32% vs 24%, P < 0.01)[44]. FMT has been demonstrated to be a safe and effective therapy for rCDI in the general population on the basis of several large RCTs[79-81]. Several studies have analyzed treatment of rCDI in IBD patients. A retrospective study of immunosuppressed patients with CDI undergoing FMT included 36 IBD patients, of which 86% were cured of CDI after one transplant and 14% worsened in disease activity[82]. Another retrospective multicenter study of 67 IBD patients (35 CD; 31 UC; 1 IBDU), of which 64% were receiving immunosuppressive therapy at the time of FMT, found that 79% had either resolution of their diarrhea and/or negative CDI testing at week 12 and 46% had improved disease activity at 3 mo. Disease activity at 3 mo remained the same or worsened in 36%, and 18% of patients, respectively[83]. Adverse events occurred in 12% of patients at 3 mo. One patient received a colectomy and two had IBD related hospitalizations. In a prospective study of 35 IBD patients (13 CD; 22 UC) undergoing FMT for rCDI, 54% of patients required escalation of IBD therapy, despite disappearance of C. difficile toxin from the stool[84]. Another retrospective study of 272 IBD and non-IBD patients undergoing one FMT for rCDI demonstrated IBD patients had lower CDI clearance rates than non-IBD patients (74% vs 92% P = 0.0018), independent of immunosuppressive therapy[85]. In follow-up, despite C. difficile toxin clearance, 50% of UC patients worsened in disease activity requiring escalation of therapy[86].
FMT appears to effectively treat rCDI in IBD patients, albeit less-so than in the general population. However, subsequent worsening of disease activity is consistent throughout the literature. Furthermore, the effects of FMT on IBD activity are unclear. Outcomes are heterogeneous regarding FMT as treatment for IBD alone[87,88]. Although several meta-analysis exist[89,90] only 2 RCTs with conflicting results regarding UC patients are included. While one RCT of 70 patients showed FMT induced clinical remission compared to placebo[88], the other did not achieve a stringent composite primary end point of clinical remission and a > 1 point decrease in the endoscopic mayo score in 37 UC patients[87]. More recently, an RCT of intensive multidonor FMT (colonoscopic infusion followed by 5 enemas weekly for 8 wk) in 85 UC patients achieved a primary endpoint of steroid free clinical remission with endoscopic remission or response at week 8[91]. These results, combined with the efficacy of FMT in the treatment of rCDI in IBD patients, necessitates future RCTs analyzing intensive multidonor FMT for rCDI in IBD patients.
In conclusion, CDI commonly complicates the course of IBD but the lack of data precludes formal strong recommendations on the management of IBD in patients with CDI. Initiation of corticosteroids in IBD flares in the context of acute CDI is understudied but seems to be safe. Initiation or resumption of immunosuppressive therapy within 48 to 72 h of targeted antibiotic therapy may be appropriate. To better understand the treatment of IBD flares in the context of acute CDI, further studies are needed to determine the optimal timing and dosing of IBD-specific therapies.
COMMENTS
Background
Clostridium difficile (C. difficile) has been identified as an important nosocomial infection whose traditional risk factors include recent antibiotic use and exposure to a health care institution. Inflammatory bowel disease (IBD) is another important risk factor for Clostridium difficile infection (CDI), likely related to the decreased intestinal microbial diversity and disordered immune response seen in this population. Many observational studies have explored the epidemiology, risk factors, and outcomes of CDI in those with IBD and have reported its negative impact. CDI in IBD patients has been linked to excess morbidity, including longer hospitalization, higher risk of colectomy, and escalation in IBD therapy, as well increased mortality. IBD and CDI-related symptoms are often difficult to distinguish and beyond C. difficile eradication, the appropriate IBD therapy is unclear. This review explored the existing evidence regarding the management of IBD in patients with CDI.
Research frontiers
Prospective studies evaluating the initiation and maintenance of IBD therapeutics in patients with CDI are lacking and are needed to help guide practice.
Innovations and breakthroughs
While the negative impact of developing CDI in those with IBD has been well established, the appropriate management of CDI in the IBD population is less well-defined. Risk factors for the development of CDI in IBD patients identified in this review include recent antibiotic exposure, hospitalization, and colonic involvement. Contradictory evidence exists as to whether maintenance immunosuppressive therapy is a risk factor for the development of CDI. On the basis of data presented in this study, vancomycin should be used as a first-line regimen for CDI. Case reports suggest that corticosteroid initiation, after appropriate antibiotic coverage, may be safe in those with CDI and IBD flare.
Applications
The symptoms of an IBD flare and CDI are often indistinguishable. As such, stool testing for C. difficile should be sent in every flaring IBD patient. Once CDI is diagnosed, a vancomycin-containing antibiotic regimen should be initiated. In the setting of ongoing symptoms, not warranting surgical intervention, it remains unclear when IBD-specific therapy can be initiated. However, case reports and expert opinion may allow for corticosteroid initiation after 3 d of appropriate CDI therapy.
Peer-review
It’s a well done and well written extensive review on the epidemiology and therapy of CDI in IBD patients.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: D’Aoust J and Battat R confirm that there are no conflicts of interest to declare; Bessissow T has received fees as a speaker for Janssen, Shire, Abbvie, Takeda, Ferring, and Pendopharma; Bessissow T has a research grant from Abbvie, Janssen; Bessissow T has consulted for Abbvie, Takeda, Shire.
Peer-review started: March 29, 2017
First decision: April 26, 2017
Article in press: June 19, 2017
P- Reviewer: Begun J, Matowicka-Karna J, Tambuwala M, Zhulina Y S- Editor: Qi Y L- Editor: A E- Editor: Zhang FF
References
- 1.Danese S, Fiocchi C. Ulcerative colitis. N Engl J Med. 2011;365:1713–1725. doi: 10.1056/NEJMra1102942. [DOI] [PubMed] [Google Scholar]
- 2.Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244–250. doi: 10.1097/00054725-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, McFarland LV, Mellow M, Zuckerbraun BS. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–498; quiz 499. doi: 10.1038/ajg.2013.4. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, Pepin J, Wilcox MH; Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA) Infect Control Hosp Epidemiol. 2010;31:431–455. doi: 10.1086/651706. [DOI] [PubMed] [Google Scholar]
- 5.Viscidi R, Laughon BE, Yolken R, Bo-Linn P, Moench T, Ryder RW, Bartlett JG. Serum antibody response to toxins A and B of Clostridium difficile. J Infect Dis. 1983;148:93–100. doi: 10.1093/infdis/148.1.93. [DOI] [PubMed] [Google Scholar]
- 6.Jangi S, Lamont JT. Asymptomatic colonization by Clostridium difficile in infants: implications for disease in later life. J Pediatr Gastroenterol Nutr. 2010;51:2–7. doi: 10.1097/MPG.0b013e3181d29767. [DOI] [PubMed] [Google Scholar]
- 7.Shim JK, Johnson S, Samore MH, Bliss DZ, Gerding DN. Primary symptomless colonisation by Clostridium difficile and decreased risk of subsequent diarrhoea. Lancet. 1998;351:633–636. doi: 10.1016/S0140-6736(97)08062-8. [DOI] [PubMed] [Google Scholar]
- 8.Loo VG, Poirier L, Miller MA, Oughton M, Libman MD, Michaud S, Bourgault AM, Nguyen T, Frenette C, Kelly M, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med. 2005;353:2442–2449. doi: 10.1056/NEJMoa051639. [DOI] [PubMed] [Google Scholar]
- 9.McDonald LC, Killgore GE, Thompson A, Owens RC Jr, Kazakova SV, Sambol SP, Johnson S, Gerding DN. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med. 2005;353:2433–2441. doi: 10.1056/NEJMoa051590. [DOI] [PubMed] [Google Scholar]
- 10.Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN, Goorhuis B, Kuijper EJ, Wilcox MH. The changing epidemiology of Clostridium difficile infections. Clin Microbiol Rev. 2010;23:529–549. doi: 10.1128/CMR.00082-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lessa FC, Winston LG, McDonald LC; Emerging Infections Program C. difficile Surveillance Team. Burden of Clostridium difficile infection in the United States. N Engl J Med. 2015;372:2369–2370. doi: 10.1056/NEJMc1505190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kyne L, Warny M, Qamar A, Kelly CP. Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. N Engl J Med. 2000;342:390–397. doi: 10.1056/NEJM200002103420604. [DOI] [PubMed] [Google Scholar]
- 13.Kyne L, Warny M, Qamar A, Kelly CP. Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhoea. Lancet. 2001;357:189–193. doi: 10.1016/S0140-6736(00)03592-3. [DOI] [PubMed] [Google Scholar]
- 14.Chang JY, Antonopoulos DA, Kalra A, Tonelli A, Khalife WT, Schmidt TM, Young VB. Decreased diversity of the fecal Microbiome in recurrent Clostridium difficile-associated diarrhea. J Infect Dis. 2008;197:435–438. doi: 10.1086/525047. [DOI] [PubMed] [Google Scholar]
- 15.Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146:1489–1499. doi: 10.1053/j.gastro.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodemann JF, Dubberke ER, Reske KA, Seo DH, Stone CD. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:339–344. doi: 10.1016/j.cgh.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 17.Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103:1443–1450. doi: 10.1111/j.1572-0241.2007.01780.x. [DOI] [PubMed] [Google Scholar]
- 18.Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut. 2008;57:205–210. doi: 10.1136/gut.2007.128231. [DOI] [PubMed] [Google Scholar]
- 19.Sandberg KC, Davis MM, Gebremariam A, Adler J. Disproportionate rise in Clostridium difficile-associated hospitalizations among US youth with inflammatory bowel disease, 1997-2011. J Pediatr Gastroenterol Nutr. 2015;60:486–492. doi: 10.1097/MPG.0000000000000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bossuyt P, Verhaegen J, Van Assche G, Rutgeerts P, Vermeire S. Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohns Colitis. 2009;3:4–7. doi: 10.1016/j.crohns.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Greenfield C, Aguilar Ramirez JR, Pounder RE, Williams T, Danvers M, Marper SR, Noone P. Clostridium difficile and inflammatory bowel disease. Gut. 1983;24:713–717. doi: 10.1136/gut.24.8.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meyer AM, Ramzan NN, Loftus EV Jr, Heigh RI, Leighton JA. The diagnostic yield of stool pathogen studies during relapses of inflammatory bowel disease. J Clin Gastroenterol. 2004;38:772–775. doi: 10.1097/01.mcg.0000139057.05297.d6. [DOI] [PubMed] [Google Scholar]
- 23.Mylonaki M, Langmead L, Pantes A, Johnson F, Rampton DS. Enteric infection in relapse of inflammatory bowel disease: importance of microbiological examination of stool. Eur J Gastroenterol Hepatol. 2004;16:775–778. doi: 10.1097/01.meg.0000131040.38607.09. [DOI] [PubMed] [Google Scholar]
- 24.Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, Skaros S, Weber LR, Komorowski RA, Knox JF, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:345–351. doi: 10.1016/j.cgh.2006.12.028. [DOI] [PubMed] [Google Scholar]
- 25.Krishnarao A, de Leon L, Bright R, Moniz H, Law M, Leleiko N, Sands BE, Merrick M, Shapiro J, Wallenstein S, et al. Testing for Clostridium difficile in patients newly diagnosed with inflammatory bowel disease in a community setting. Inflamm Bowel Dis. 2015;21:564–569. doi: 10.1097/MIB.0000000000000309. [DOI] [PubMed] [Google Scholar]
- 26.Rolny P, Järnerot G, Möllby R. Occurrence of Clostridium difficile toxin in inflammatory bowel disease. Scand J Gastroenterol. 1983;18:61–64. doi: 10.3109/00365528309181560. [DOI] [PubMed] [Google Scholar]
- 27.Ricciardi R, Ogilvie JW Jr, Roberts PL, Marcello PW, Concannon TW, Baxter NN. Epidemiology of Clostridium difficile colitis in hospitalized patients with inflammatory bowel diseases. Dis Colon Rectum. 2009;52:40–45. doi: 10.1007/DCR.0b013e31819733fd. [DOI] [PubMed] [Google Scholar]
- 28.Ott C, Girlich C, Klebl F, Plentz A, Iesalnieks I, Schölmerich J, Obermeier F. Low risk of Clostridium difficile infections in hospitalized patients with inflammatory bowel disease in a German tertiary referral center. Digestion. 2011;84:187–192. doi: 10.1159/000324617. [DOI] [PubMed] [Google Scholar]
- 29.Antonelli E, Baldoni M, Giovenali P, Villanacci V, Essatari M, Bassotti G. Intestinal superinfections in patients with inflammatory bowel diseases. J Crohns Colitis. 2012;6:154–159. doi: 10.1016/j.crohns.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 30.Regnault H, Bourrier A, Lalande V, Nion-Larmurier I, Sokol H, Seksik P, Barbut F, Cosnes J, Beaugerie L. Prevalence and risk factors of Clostridium difficile infection in patients hospitalized for flare of inflammatory bowel disease: a retrospective assessment. Dig Liver Dis. 2014;46:1086–1092. doi: 10.1016/j.dld.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 31.Murthy SK, Steinhart AH, Tinmouth J, Austin PC, Daneman N, Nguyen GC. Impact of Clostridium difficile colitis on 5-year health outcomes in patients with ulcerative colitis. Aliment Pharmacol Ther. 2012;36:1032–1039. doi: 10.1111/apt.12073. [DOI] [PubMed] [Google Scholar]
- 32.Negrón ME, Barkema HW, Rioux K, De Buck J, Checkley S, Proulx MC, Frolkis A, Beck PL, Dieleman LA, Panaccione R, et al. Clostridium difficile infection worsens the prognosis of ulcerative colitis. Can J Gastroenterol Hepatol. 2014;28:373–380. doi: 10.1155/2014/914303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shen BO, Jiang ZD, Fazio VW, Remzi FH, Rodriguez L, Bennett AE, Lopez R, Queener E, Dupont HL. Clostridium difficile infection in patients with ileal pouch-anal anastomosis. Clin Gastroenterol Hepatol. 2008;6:782–788. doi: 10.1016/j.cgh.2008.02.021. [DOI] [PubMed] [Google Scholar]
- 34.Li Y, Qian J, Queener E, Shen B. Risk factors and outcome of PCR-detected Clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis. 2013;19:397–403. doi: 10.1097/MIB.0b013e318280fcb9. [DOI] [PubMed] [Google Scholar]
- 35.Pascarella F, Martinelli M, Miele E, Del Pezzo M, Roscetto E, Staiano A. Impact of Clostridium difficile infection on pediatric inflammatory bowel disease. J Pediatr. 2009;154:854–858. doi: 10.1016/j.jpeds.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 36.Wultańska D, Banaszkiewicz A, Radzikowski A, Obuch-Woszczatyński P, Młynarczyk G, Brazier JS, Pituch H, van Belkum A. Clostridium difficile infection in Polish pediatric outpatients with inflammatory bowel disease. Eur J Clin Microbiol Infect Dis. 2010;29:1265–1270. doi: 10.1007/s10096-010-0997-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mezoff E, Mann EA, Hart KW, Lindsell CJ, Cohen MB. Clostridium difficile infection and treatment in the pediatric inflammatory bowel disease population. J Pediatr Gastroenterol Nutr. 2011;52:437–441. doi: 10.1097/MPG.0b013e3181f97209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Banaszkiewicz A, Kowalska-Duplaga K, Pytrus T, Pituch H, Radzikowski A. Clostridium difficile infection in newly diagnosed pediatric patients with inflammatory bowel disease: prevalence and risk factors. Inflamm Bowel Dis. 2012;18:844–848. doi: 10.1002/ibd.21837. [DOI] [PubMed] [Google Scholar]
- 39.Mir SA, Kellermayer R. Clostridium difficile infection in newly diagnosed pediatric inflammatory bowel disease in the mid-southern United States. J Pediatr Gastroenterol Nutr. 2013;57:487–488. doi: 10.1097/MPG.0b013e3182a027c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Martinelli M, Strisciuglio C, Veres G, Paerregaard A, Pavic AM, Aloi M, Martín-de-Carpi J, Levine A, Turner D, Del Pezzo M, Staiano A, Miele E; Porto IBD Working Group of European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Clostridium difficile and pediatric inflammatory bowel disease: a prospective, comparative, multicenter, ESPGHAN study. Inflamm Bowel Dis. 2014;20:2219–2225. doi: 10.1097/MIB.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 41.Kuntz JL, Chrischilles EA, Pendergast JF, Herwaldt LA, Polgreen PM. Incidence of and risk factors for community-associated Clostridium difficile infection: a nested case-control study. BMC Infect Dis. 2011;11:194. doi: 10.1186/1471-2334-11-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015;372:1539–1548. doi: 10.1056/NEJMra1403772. [DOI] [PubMed] [Google Scholar]
- 43.Kariv R, Navaneethan U, Venkatesh PG, Lopez R, Shen B. Impact of Clostridium difficile infection in patients with ulcerative colitis. J Crohns Colitis. 2011;5:34–40. doi: 10.1016/j.crohns.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 44.Razik R, Rumman A, Bahreini Z, McGeer A, Nguyen GC. Recurrence of Clostridium difficile Infection in Patients with Inflammatory Bowel Disease: The RECIDIVISM Study. Am J Gastroenterol. 2016;111:1141–1146. doi: 10.1038/ajg.2016.187. [DOI] [PubMed] [Google Scholar]
- 45.Seril DN, Ashburn JH, Lian L, Shen B. Risk factors and management of refractory or recurrent clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis. 2014;20:2226–2233. doi: 10.1097/MIB.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 46.Kaneko T, Matsuda R, Taguri M, Inamori M, Ogura A, Miyajima E, Tanaka K, Maeda S, Kimura H, Kunisaki R. Clostridium difficile infection in patients with ulcerative colitis: investigations of risk factors and efficacy of antibiotics for steroid refractory patients. Clin Res Hepatol Gastroenterol. 2011;35:315–320. doi: 10.1016/j.clinre.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 47.Masclee GM, Penders J, Jonkers DM, Wolffs PF, Pierik MJ. Is clostridium difficile associated with relapse of inflammatory bowel disease? results from a retrospective and prospective cohort study in the Netherlands. Inflamm Bowel Dis. 2013;19:2125–2131. doi: 10.1097/MIB.0b013e318297d222. [DOI] [PubMed] [Google Scholar]
- 48.Furuya-Kanamori L, Stone JC, Clark J, McKenzie SJ, Yakob L, Paterson DL, Riley TV, Doi SA, Clements AC. Comorbidities, Exposure to Medications, and the Risk of Community-Acquired Clostridium difficile Infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:132–141. doi: 10.1017/ice.2014.39. [DOI] [PubMed] [Google Scholar]
- 49.Schneeweiss S, Korzenik J, Solomon DH, Canning C, Lee J, Bressler B. Infliximab and other immunomodulating drugs in patients with inflammatory bowel disease and the risk of serious bacterial infections. Aliment Pharmacol Ther. 2009;30:253–264. doi: 10.1111/j.1365-2036.2009.04037.x. [DOI] [PubMed] [Google Scholar]
- 50.Suzuki H, Ogawa H, Shibata C, Haneda S, Watanabe K, Takahashi K, Funayama Y, Sasaki I. The long-term clinical course of pouchitis after total proctocolectomy and IPAA for ulcerative colitis. Dis Colon Rectum. 2012;55:330–336. doi: 10.1097/DCR.0b013e3182417358. [DOI] [PubMed] [Google Scholar]
- 51.Hughes M, Qazi T, Berg A, Weinberg J, Chen X, Kelly CP, Farraye FA. Host Immune Response to Clostridium difficile Infection in Inflammatory Bowel Disease Patients. Inflamm Bowel Dis. 2016;22:853–861. doi: 10.1097/MIB.0000000000000696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Connelly TM, Koltun WA, Sangster W, Berg AS, Hegarty JP, Harris L 3rd, Deiling S, Stewart DB. An interleukin-4 polymorphism is associated with susceptibility to Clostridium difficile infection in patients with inflammatory bowel disease: results of a retrospective cohort study. Surgery. 2014;156:769–774. doi: 10.1016/j.surg.2014.06.067. [DOI] [PubMed] [Google Scholar]
- 53.Monaghan TM, Robins A, Knox A, Sewell HF, Mahida YR. Circulating antibody and memory B-Cell responses to C. difficile toxins A and B in patients with C. difficile-associated diarrhoea, inflammatory bowel disease and cystic fibrosis. PLoS One. 2013;8:e74452. doi: 10.1371/journal.pone.0074452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.McCurdy JD, Enders FT, Khanna S, Bruining DH, Jones A, Killian JM, Tariq R, Smyrk TC, Loftus EV Jr. Increased Rates of Clostridium difficile Infection and Poor Outcomes in Patients with IBD with Cytomegalovirus. Inflamm Bowel Dis. 2016;22:2688–2693. doi: 10.1097/MIB.0000000000000939. [DOI] [PubMed] [Google Scholar]
- 55.Ananthakrishnan AN, McGinley EL. Infection-related hospitalizations are associated with increased mortality in patients with inflammatory bowel diseases. J Crohns Colitis. 2013;7:107–112. doi: 10.1016/j.crohns.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 56.Ananthakrishnan AN, Oxford EC, Nguyen DD, Sauk J, Yajnik V, Xavier RJ. Genetic risk factors for Clostridium difficile infection in ulcerative colitis. Aliment Pharmacol Ther. 2013;38:522–530. doi: 10.1111/apt.12425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jen MH, Saxena S, Bottle A, Aylin P, Pollok RC. Increased health burden associated with Clostridium difficile diarrhoea in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33:1322–1331. doi: 10.1111/j.1365-2036.2011.04661.x. [DOI] [PubMed] [Google Scholar]
- 58.Ananthakrishnan AN, McGinley EL, Saeian K, Binion DG. Temporal trends in disease outcomes related to Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:976–983. doi: 10.1002/ibd.21457. [DOI] [PubMed] [Google Scholar]
- 59.Jodorkovsky D, Young Y, Abreu MT. Clinical outcomes of patients with ulcerative colitis and co-existing Clostridium difficile infection. Dig Dis Sci. 2010;55:415–420. doi: 10.1007/s10620-009-0749-9. [DOI] [PubMed] [Google Scholar]
- 60.Navaneethan U, Mukewar S, Venkatesh PG, Lopez R, Shen B. Clostridium difficile infection is associated with worse long term outcome in patients with ulcerative colitis. J Crohns Colitis. 2012;6:330–336. doi: 10.1016/j.crohns.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 61.Skowron KB, Lapin B, Rubin M, Hurst RD, Rubin DT, Hyman NH, Umanskiy K. Clostridium Difficile Infection in Ulcerative Colitis: Can Alteration of the Gut-associated Microbiome Contribute to Pouch Failure? Inflamm Bowel Dis. 2016;22:902–911. doi: 10.1097/MIB.0000000000000710. [DOI] [PubMed] [Google Scholar]
- 62.Kelsen JR, Kim J, Latta D, Smathers S, McGowan KL, Zaoutis T, Mamula P, Baldassano RN. Recurrence rate of clostridium difficile infection in hospitalized pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:50–55. doi: 10.1002/ibd.21421. [DOI] [PubMed] [Google Scholar]
- 63.Bitton A, Buie D, Enns R, Feagan BG, Jones JL, Marshall JK, Whittaker S, Griffiths AM, Panaccione R; Canadian Association of Gastroenterology Severe Ulcerative Colitis Consensus Group. Treatment of hospitalized adult patients with severe ulcerative colitis: Toronto consensus statements. Am J Gastroenterol. 2012;107:179–194; author reply 195. doi: 10.1038/ajg.2011.386. [DOI] [PubMed] [Google Scholar]
- 64.Ben-Horin S, Margalit M, Bossuyt P, Maul J, Shapira Y, Bojic D, Chermesh I, Al-Rifai A, Schoepfer A, Bosani M, Allez M, Lakatos PL, Bossa F, Eser A, Stefanelli T, Carbonnel F, Katsanos K, Checchin D, de Miera IS, Reinisch W, Chowers Y, Moran GW; European Crohn’s and Colitis Organization (ECCO) Prevalence and clinical impact of endoscopic pseudomembranes in patients with inflammatory bowel disease and Clostridium difficile infection. J Crohns Colitis. 2010;4:194–198. doi: 10.1016/j.crohns.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 65.Wang T, Matukas L, Streutker CJ. Histologic findings and clinical characteristics in acutely symptomatic ulcerative colitis patients with superimposed Clostridium difficile infection. Am J Clin Pathol. 2013;140:831–837. doi: 10.1309/AJCP2LBRTTJBF3KD. [DOI] [PubMed] [Google Scholar]
- 66.Viscidi R, Willey S, Bartlett JG. Isolation rates and toxigenic potential of Clostridium difficile isolates from various patient populations. Gastroenterology. 1981;81:5–9. [PubMed] [Google Scholar]
- 67.Clayton EM, Rea MC, Shanahan F, Quigley EM, Kiely B, Hill C, Ross RP. The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol. 2009;104:1162–1169. doi: 10.1038/ajg.2009.4. [DOI] [PubMed] [Google Scholar]
- 68.Hourigan SK, Chirumamilla SR, Ross T, Golub JE, Rabizadeh S, Saeed SA, Elson CO, Kelly CP, Carroll KC, Oliva-Hemker M, et al. Clostridium difficile carriage and serum antitoxin responses in children with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2744–2752. doi: 10.1097/01.MIB.0000435434.53871.36. [DOI] [PubMed] [Google Scholar]
- 69.Sethi AK, Al-Nassir WN, Nerandzic MM, Bobulsky GS, Donskey CJ. Persistence of skin contamination and environmental shedding of Clostridium difficile during and after treatment of C. difficile infection. Infect Control Hosp Epidemiol. 2010;31:21–27. doi: 10.1086/649016. [DOI] [PubMed] [Google Scholar]
- 70.Horton HA, Dezfoli S, Berel D, Hirsch J, Ippoliti A, McGovern D, Kaur M, Shih D, Dubinsky M, Targan SR, et al. Antibiotics for Treatment of Clostridium difficile Infection in Hospitalized Patients with Inflammatory Bowel Disease. Antimicrob Agents Chemother. 2014;58:5054–5059. doi: 10.1128/AAC.02606-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yanai H, Nguyen GC, Yun L, Lebwohl O, Navaneethan U, Stone CD, Ghazi L, Moayyedi P, Brooks J, Bernstein CN, et al. Practice of gastroenterologists in treating flaring inflammatory bowel disease patients with clostridium difficile: antibiotics alone or combined antibiotics/immunomodulators? Inflamm Bowel Dis. 2011;17:1540–1546. doi: 10.1002/ibd.21514. [DOI] [PubMed] [Google Scholar]
- 72.Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2015;(9):CD004405. doi: 10.1002/14651858.CD004405.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Siemieniuk RA, Meade MO, Alonso-Coello P, Briel M, Evaniew N, Prasad M, Alexander PE, Fei Y, Vandvik PO, Loeb M, et al. Corticosteroid Therapy for Patients Hospitalized With Community-Acquired Pneumonia: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;163:519–528. doi: 10.7326/M15-0715. [DOI] [PubMed] [Google Scholar]
- 74.Annane D. Corticosteroids for severe sepsis: an evidence-based guide for physicians. Ann Intensive Care. 2011;1:7. doi: 10.1186/2110-5820-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ben-Horin S, Margalit M, Bossuyt P, Maul J, Shapira Y, Bojic D, Chermesh I, Al-Rifai A, Schoepfer A, Bosani M, Allez M, Lakatos PL, Bossa F, Eser A, Stefanelli T, Carbonnel F, Katsanos K, Checchin D, Miera IS, Chowers Y, Moran GW; European Crohn’s and Colitis Organization (ECCO) Combination immunomodulator and antibiotic treatment in patients with inflammatory bowel disease and clostridium difficile infection. Clin Gastroenterol Hepatol. 2009;7:981–987. doi: 10.1016/j.cgh.2009.05.031. [DOI] [PubMed] [Google Scholar]
- 76.Khanna S, Shin A, Kelly CP. Management of Clostridium difficile Infection in Inflammatory Bowel Disease: Expert Review from the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15:166–174. doi: 10.1016/j.cgh.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 77.Rahier JF, Ben-Horin S, Chowers Y, Conlon C, De Munter P, D’Haens G, Domènech E, Eliakim R, Eser A, Frater J, Gassull M, Giladi M, Kaser A, Lémann M, Moreels T, Moschen A, Pollok R, Reinisch W, Schunter M, Stange EF, Tilg H, Van Assche G, Viget N, Vucelic B, Walsh A, Weiss G, Yazdanpanah Y, Zabana Y, Travis SP, Colombel JF; European Crohn’s and Colitis Organisation (ECCO) European evidence-based Consensus on the prevention, diagnosis and management of opportunistic infections in inflammatory bowel disease. J Crohns Colitis. 2009;3:47–91. doi: 10.1016/j.crohns.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 78.Absah I, Faubion WA Jr. Concomitant therapy with methotrexate and anti-TNF-α in pediatric patients with refractory crohn’s colitis: a case series. Inflamm Bowel Dis. 2012;18:1488–1492. doi: 10.1002/ibd.21885. [DOI] [PubMed] [Google Scholar]
- 79.Cammarota G, Masucci L, Ianiro G, Bibbò S, Dinoi G, Costamagna G, Sanguinetti M, Gasbarrini A. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41:835–843. doi: 10.1111/apt.13144. [DOI] [PubMed] [Google Scholar]
- 80.Lee CH, Steiner T, Petrof EO, Smieja M, Roscoe D, Nematallah A, Weese JS, Collins S, Moayyedi P, Crowther M, et al. Frozen vs Fresh Fecal Microbiota Transplantation and Clinical Resolution of Diarrhea in Patients With Recurrent Clostridium difficile Infection: A Randomized Clinical Trial. JAMA. 2016;315:142–149. doi: 10.1001/jama.2015.18098. [DOI] [PubMed] [Google Scholar]
- 81.van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, Visser CE, Kuijper EJ, Bartelsman JF, Tijssen JG, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 82.Kelly CR, Ihunnah C, Fischer M, Khoruts A, Surawicz C, Afzali A, Aroniadis O, Barto A, Borody T, Giovanelli A, et al. Fecal microbiota transplant for treatment of Clostridium difficile infection in immunocompromised patients. Am J Gastroenterol. 2014;109:1065–1071. doi: 10.1038/ajg.2014.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fischer M, Kao D, Kelly C, Kuchipudi A, Jafri SM, Blumenkehl M, Rex D, Mellow M, Kaur N, Sokol H, et al. Fecal Microbiota Transplantation is Safe and Efficacious for Recurrent or Refractory Clostridium difficile Infection in Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2016;22:2402–2409. doi: 10.1097/MIB.0000000000000908. [DOI] [PubMed] [Google Scholar]
- 84.Chin SM, Sauk J, Mahabamunuge J, Kaplan JL, Hohmann EL, Khalili H. Fecal Microbiota Transplantation for Recurrent Clostridium difficile Infection in Patients With Inflammatory Bowel Disease: A Single-Center Experience. Clin Gastroenterol Hepatol. 2017;15:597–599. doi: 10.1016/j.cgh.2016.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Khoruts A, Rank KM, Newman KM, Viskocil K, Vaughn BP, Hamilton MJ, Sadowsky MJ. Inflammatory Bowel Disease Affects the Outcome of Fecal Microbiota Transplantation for Recurrent Clostridium difficile Infection. Clin Gastroenterol Hepatol. 2016;14:1433–1438. doi: 10.1016/j.cgh.2016.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Newman KM, Rank KM, Vaughn BP, Khoruts A. Treatment of recurrent Clostridium difficile infection using fecal microbiota transplantation in patients with inflammatory bowel disease. Gut Microbes. 2017;8:303–309. doi: 10.1080/19490976.2017.1279377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Rossen NG, Fuentes S, van der Spek MJ, Tijssen JG, Hartman JH, Duflou A, Löwenberg M, van den Brink GR, Mathus-Vliegen EM, de Vos WM, et al. Findings From a Randomized Controlled Trial of Fecal Transplantation for Patients With Ulcerative Colitis. Gastroenterology. 2015;149:110–118.e4. doi: 10.1053/j.gastro.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 88.Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, Armstrong D, Marshall JK, Kassam Z, Reinisch W, et al. Fecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in a Randomized Controlled Trial. Gastroenterology. 2015;149:102–109.e6. doi: 10.1053/j.gastro.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 89.Sun D, Li W, Li S, Cen Y, Xu Q, Li Y, Sun Y, Qi Y, Lin Y, Yang T, et al. Fecal Microbiota Transplantation as a Novel Therapy for Ulcerative Colitis: A Systematic Review and Meta-Analysis. Medicine (Baltimore) 2016;95:e3765. doi: 10.1097/MD.0000000000003765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shi Y, Dong Y, Huang W, Zhu D, Mao H, Su P. Fecal Microbiota Transplantation for Ulcerative Colitis: A Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0157259. doi: 10.1371/journal.pone.0157259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Paramsothy S, Kamm MA, Kaakoush NO, Walsh AJ, van den Bogaerde J, Samuel D, Leong RWL, Connor S, Ng W, Paramsothy R, et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet. 2017;389:1218–1228. doi: 10.1016/S0140-6736(17)30182-4. [DOI] [PubMed] [Google Scholar]
- 92.Keighley MR. Clostridium difficile and inflammatory bowel disease. J Antimicrob Chemother. 1983;11:493–494. doi: 10.1093/jac/11.6.493. [DOI] [PubMed] [Google Scholar]
- 93.Gurian L, Klein K, Ward TT. Role of Clostridium difficile and Campylobacter jejuni in relapses of inflammatory bowel disease. West J Med. 1983;138:359–360. [PMC free article] [PubMed] [Google Scholar]
- 94.Burke DA, Axon AT. Clostridium difficile, sulphasalazine, and ulcerative colitis. Postgrad Med J. 1987;63:955–957. doi: 10.1136/pgmj.63.745.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gryboski JD. Clostridium difficile in inflammatory bowel disease relapse. J Pediatr Gastroenterol Nutr. 1991;13:39–41. doi: 10.1097/00005176-199107000-00007. [DOI] [PubMed] [Google Scholar]
- 96.Balamurugan R, Balaji V, Ramakrishna BS. Estimation of faecal carriage of Clostridium difficile in patients with ulcerative colitis using real time polymerase chain reaction. Indian J Med Res. 2008;127:472–477. [PubMed] [Google Scholar]
- 97.Lamousé-Smith ES, Weber S, Rossi RF, Neinstedt LJ, Mosammaparast N, Sandora TJ, McAdam AJ, Bousvaros A. Polymerase chain reaction test for Clostridium difficile toxin B gene reveals similar prevalence rates in children with and without inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2013;57:293–297. doi: 10.1097/MPG.0b013e3182999990. [DOI] [PubMed] [Google Scholar]
- 98.Pant C, Anderson MP, Deshpande A, Altaf MA, Grunow JE, Atreja A, Sferra TJ. Health care burden of Clostridium difficile infection in hospitalized children with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1080–1085. doi: 10.1097/MIB.0b013e3182807563. [DOI] [PubMed] [Google Scholar]
- 99.Hourigan SK, Oliva-Hemker M, Hutfless S. The prevalence of Clostridium difficile infection in pediatric and adult patients with inflammatory bowel disease. Dig Dis Sci. 2014;59:2222–2227. doi: 10.1007/s10620-014-3169-4. [DOI] [PubMed] [Google Scholar]
- 100.Simian D, Fluxá D, Flores L, Lubascher J, Ibáñez P, Figueroa C, Kronberg U, Acuña R, Moreno M, Quera R. Inflammatory bowel disease: A descriptive study of 716 local Chilean patients. World J Gastroenterol. 2016;22:5267–5275. doi: 10.3748/wjg.v22.i22.5267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Roy A, Lichtiger S. Clostridium difficile Infection: A Rarity in Patients Receiving Chronic Antibiotic Treatment for Crohn’s Disease. Inflamm Bowel Dis. 2016;22:648–653. doi: 10.1097/MIB.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ananthakrishnan AN, Cagan A, Gainer VS, Cheng SC, Cai T, Szolovits P, Shaw SY, Churchill S, Karlson EW, Murphy SN, et al. Higher plasma vitamin D is associated with reduced risk of Clostridium difficile infection in patients with inflammatory bowel diseases. Aliment Pharmacol Ther. 2014;39:1136–1142. doi: 10.1111/apt.12706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chu EW, Ecker BL, Garg M, Divino CM. The surgical management of active ulcerative colitis complicated by Clostridium difficile infection. J Gastrointest Surg. 2013;17:392–396. doi: 10.1007/s11605-012-2031-2. [DOI] [PubMed] [Google Scholar]
- 104.Cavagnaro C, Berezin S, Medow MS. Corticosteroid treatment of severe, non-responsive Clostridium difficile induced colitis. Arch Dis Child. 2003;88:342–344. doi: 10.1136/adc.88.4.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sykes E, McDonald P, Flanagan PK. Corticosteroids in the Treatment of Pseudomembranous Colitis: A Report of 3 Cases. Gastroenterology Res. 2012;5:211–214. doi: 10.4021/gr469w. [DOI] [PMC free article] [PubMed] [Google Scholar]


